Introduction
Parathyroid carcinoma (PTCA) is a rare malignancy,
accounting for 0.005% of all cancers (1,2), and
ectopic PTCA is particularly rare. The incidence of ectopic
parathyroid glands in healthy individuals is ~6% (3), and are located in the anterior superior
mediastinum (4), either within or
outside the thymus and along the esophagus, into the posterior
superior mediastinum (5). Therefore,
ectopic PTCA is particularly rare.
Although the etiology of PTCA is unknown, history of
neck radiation (6) and secondary and
tertiary hyperparathyroidism caused by chronic renal failure
(7) are known risk factors for PTCA.
In addition, PTCA has been associated with hyper-functioning
parathyroid glands (8). Of all types
of parathyroid cancer, ~95% are hormonally functional, and
frequently exhibit profound symptoms of hyperparathyroidism with
marked hypercalcemia and elevated parathyroid hormone (PTH) levels.
These symtpoms include polydipsia or polyuria, myalgia or
arthralgia, nephrolithiasis, weakness, fatigue, nervousness,
depression, renal insufficiency, pancreatitis, peptic ulcer disease
or weight loss. Bone pain, osteopenia, osteofibrosis and
pathological fractures were the prominent manifestation of skeletal
involvement in PTCA (9).
Parathyroid hormone-related peptide (PTHrP) causes
hypercalcemia via increased calcium absorption at the kidney and
increased bone resorption. PTHrP is widely expressed at low levels
throughout the body in healthy individuals (10), and is also ectopically secreted at
much higher levels by certain solid tumors and in several
hematological malignancies (11).
However, to the best of our knowledge, there are no previous
reports about co-expression of PTH and PTHrP contributing to
hypercalcemia in PTCA. The present study reports a unique case of a
patient with an ectopic mediastinal PTCA coproducing PTH and
PTHrP.
Case report
A 53-year-old man presented to Qilu Hospital of
Shandong University (Jinan, China) on December 2011 with fatigue
(with a 1-year history), intermittent chest pain and dizziness
(with a 2-day history), and intermittent muscular soreness (with a
9-hour history). The patient also had a 2-year history of polyuria,
night sweats and renal stones. There was no family history of renal
stones or any other kidney disease. The patient had been healthy
previously, with the exception of a surgery performed due to
abdominal trauma caused by an accident.
A physical examination revealed an average body type
(height, 175 cm; body weight, 76.3 kg) with fatigue and stable
vital signs [body temperature, 36.7°C (normal range, 36–37°C;
respiratory rate, 18 breaths/min (normal range, 16–20 breaths/min);
blood pressure, 129/83 mmHg (normal range, 120/80 mmHg); and heart
rate, 76 beats/min (normal range 60–100 beats/min), with a regular
rhythm and no pathological murmurs]. Serum calcium (Ca) on the date
of admission was 3.4 mmol/l (normal range, 2.0–2.6 mmol/l).
Alkaline phosphatase (AKP) was increased to 722 U/l (normal range,
15–112 U/l), and the levels of PTH in plasma were 2,630 pg/ml
(normal range, 15–65 pg/ml), as measured by VITROS® ECiQ
Immunodiagnostic System (Ortho Clinical Diagnostics; Johnson &
Johnson, New Brunswick, NJ, USA). However, other laboratory
parameters were normal.
Neck ultrasound (CX50 CompactXtreme; Philips
Healthcare, DA Best, The Netherlands) was negative for any
significantly abnormal thyroid nodules or parathyroid adenoma and
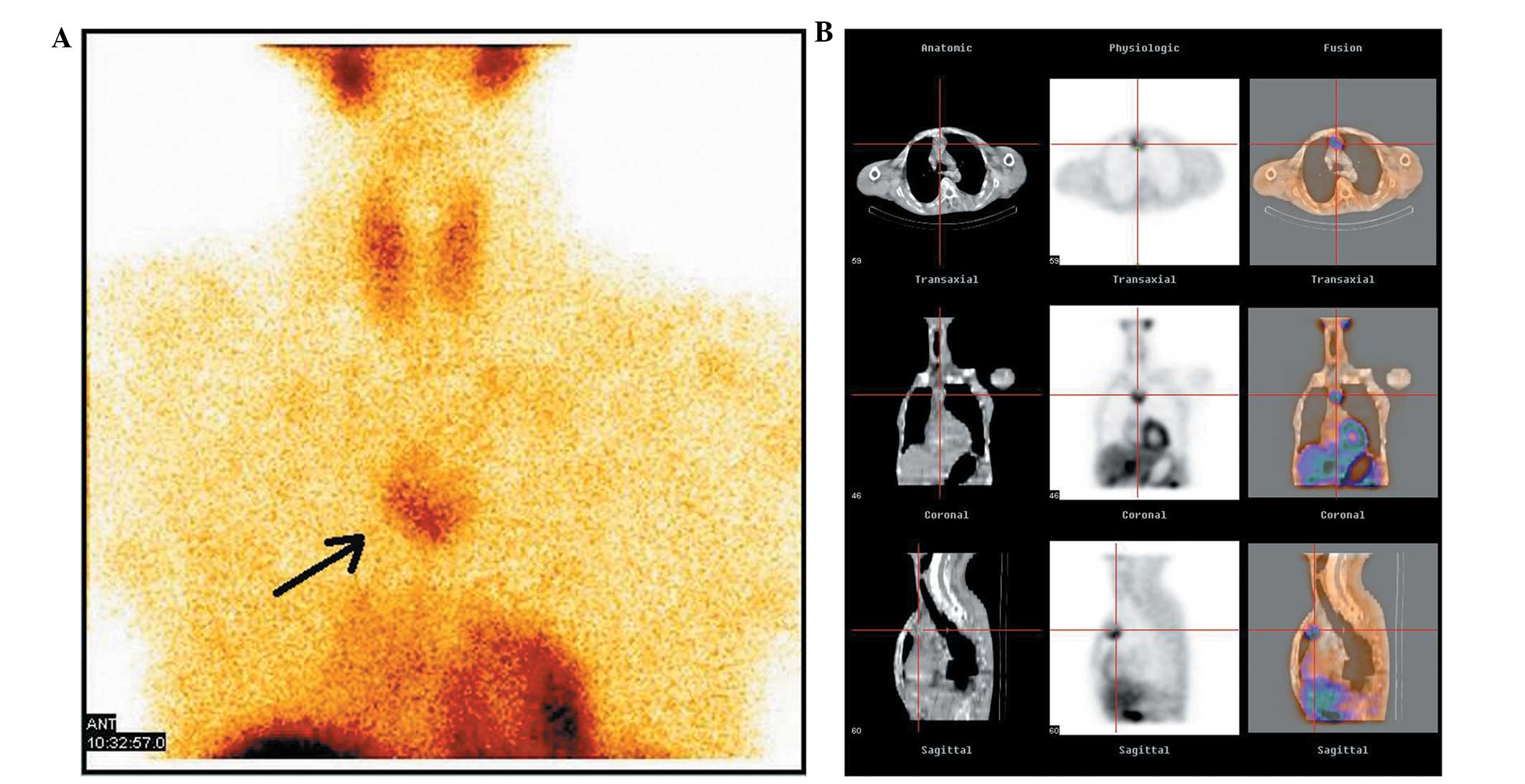
Tc99m methoxyisobutylisonitrile (Tc99m-MIBI) scintigraphy scanning
of the parathyroid confirmed the findings of the neck ultrasound.
Computed tomography (CT) of the chest, which was performed with an
IQon Spectral CT (Philips Healthcare), revealed a 3.5×3.0 cm mass
originating in the anterior mediastinum, and Tc99m-MIBI scanning
demonstrated increased uptake of Tc99m-MIBI on the mass, which
indicated an ectopic mediastinal parathyroid adenoma (PTA; Fig. 1). Enhanced CT scanning produced a
low-density image of the costal bone, right humerus and partial
vertebral body. However, no widespread bone metastasis was
observed.
Subsequently, the patient received intravenous
hydration (10–12 l/day of 0.9% normal saline) and combined
treatment with calcitonin (100 IU, i.h, q.d.; Novartis, Basel,
Switzerland), alendronate sodium tablets (10 mg, p.o., q.d.;
Instituto Gentili S.p.A., Milan, Italy), pamidronate disodium (30
mg, i.v. drop infusion, q.d.; Shenzhen Haiwang Pharmaceutical Co.
Ltd., Guangzhou, China) and furosemide (20 mg, i.v. injection,
q.d.; Huanggang Yinhe Aarti Pharmaceutical Co.,Ltd., Huangzhou,
China). The day prior to surgery, the patient's serum Ca reduced to
2.42 mmol/l. Therefore, all treatment that aimed to reduce serum Ca
was halted. The patient underwent transthorascopic surgery to
remove the giant mass in the anterior mediastinum. Surgical
exploration revealed a large mass (5×3×3 cm in size) that adhered
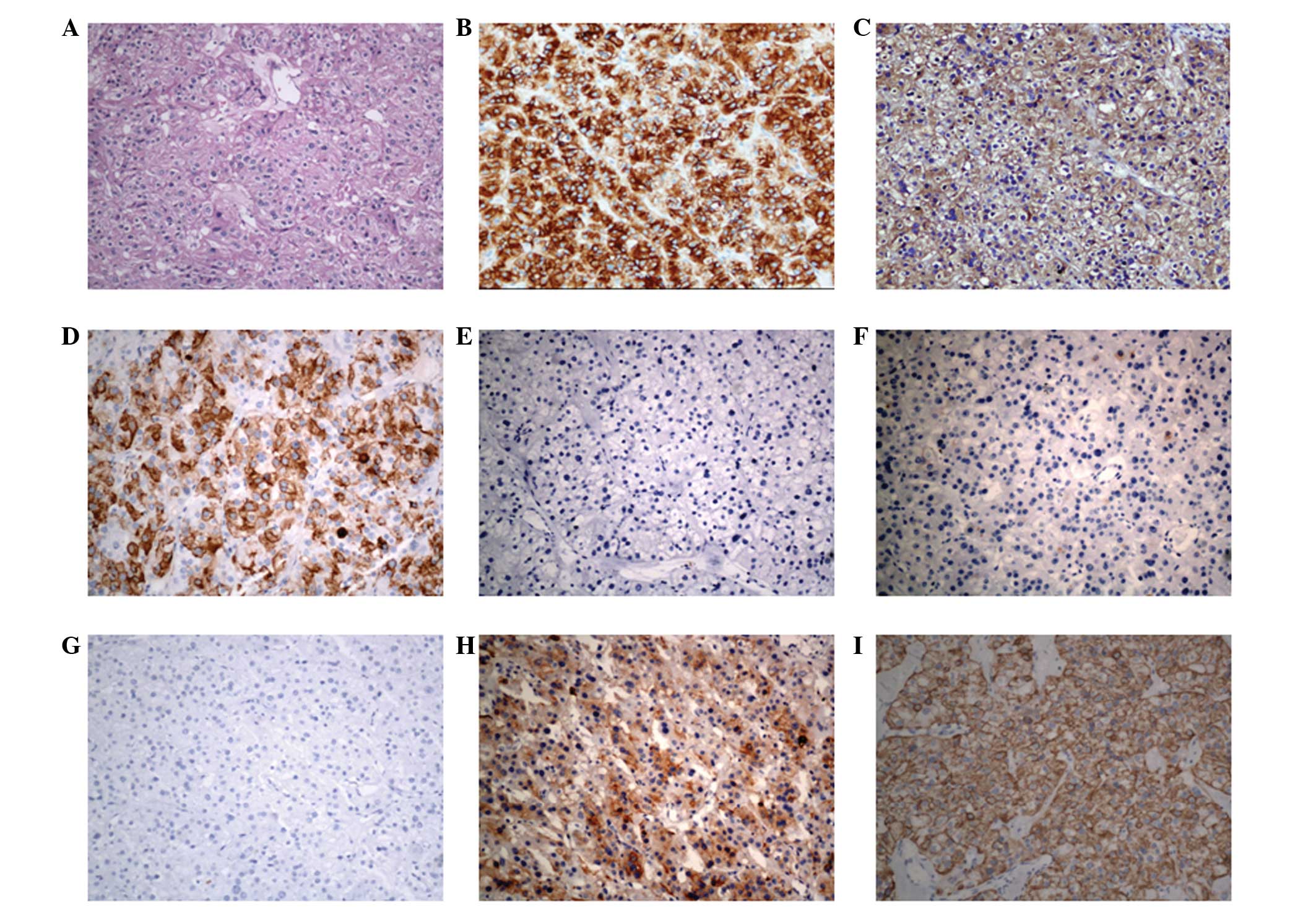
to the superior vena cava and azygos vein. Histopathological
examination revealed a parathyroid carcinoma. Hematoxylin (C0107;
Biyuntian Biotech Co., Ltd.) and eosin (C0109; Biyuntian Biotech
Co., Ltd.) staining and immunohistochemistry (IHC) results are
presented in Fig. 2, and were as
follows: Cytokeratin+ (mouse monoclonal antibody;
dilution 1:600; ab668; Abcam, Cambridge, UK),
synaptophysin+ (rabbit monoclonal antibody; dilution
1:600; ab32127; Abcam), chromogranin+ (rabbit polyclonal
antibody; dilution 1:400; ab15160; Abcam), human melanoma
black-45− (mouse monoclonal antibody; dilution 1:50;
ab787; Abcam), Melan-A− (rabbit monoclonal antibody;
dilution 1:200; ab51061; Abcam) and epithelial membrane
antigen− (rabbit monoclonal antibody; dilution 1:100;
ab136615; Abcam). PTH (rabbit polyclonal antibody; dilution 1:100;
ab40630; Abcam) and PTHrP (mouse monoclonal antibody; dilution
1:200; ab79539; Abcam) were additionally identified by IHC in the
tumor (Fig. 2).
A total of 2 days subsequent to surgery, the patient
developed perioral numbness and tingling in his extremities, and
serum Ca was 1.81 mmol/l. Subsequently, the patient was
administered calcium carbonate and vitamin D3 tablets (600 mg,
p.o., q.d.; Pfizer Inc., New York City, NY, USA), calcitriol soft
capsules (0.25 µg, p.o., q.d..; Fritz Hoffmann-La Roche AG, Basel,
Switzerland) and calcium gluconate (1 g, i.v. injection, t.i.d.;
Jinling Pharmaceutical Co., Ltd., Nanjing, China). With these
drugs, the symptoms of numbness and tingling were resolved, and 2
months later, the patient's PTH was 65.8 pg/ml and serum Ca was
1.96 mmol/l. There was no tumor recurrence at a 3-year follow-up
appointment, and serum Ca and PTH levels remained within normal
ranges. The patient is currently under follow-up.
Written informed consent was obtained from the
patient for publication of the present case report and any
accompanying images.
Discussion
PTCA is a rare cause of hypercalcemia, accounting
for <1% of patients with primary hyperparathyroidism (2). In contrast to PTA, the prevalence of men
is equal to women in patients with PTCA (12). The mean age at diagnosis is between 45
and 59 years, which is 10 years younger than patients with PTA
(6). A total of 20–25% of parathyroid
glands are in ectopic sites, and the neck and mediastinum are
common ectopic sites (13).
Therefore, PTCA has also been deemed as a mediastinal fifth
parathyroid gland. (14).
The present study described the presentation and
management of a patient with PTCA. PTCA and PTA have similar
clinical and biochemical symptoms, and histological features alone
often cannot entirely distinguish between them, therefore it may be
difficult to diagnose PTCA (15).
However, patients with PTCA have severe hypercalcemia (>15
mg/dl; normal range, 8.02–10.42 mg/dl) and markedly elevated PTH
(>300 pg/ml; normal range, 15–65 pg/ml) (2). In addition, PTCA is larger than PTA
(median size, 3.3 cm vs. 1.5 cm) (16). Furthermore, the mean levels of AKP in
PTCA are typically elevated by three-fold or more (17). According to these parameters, the
present patient could be diagnosed as PTCA prior to surgery. The
rapid postoperative normalization of PTH levels and prolonged
hypocalcemia of the present patient was most likely due to ‘hungry
bone syndrome’, which is characterized by prolonged (>4 days
following parathyroidectomy) hypocalcemia (serum calcium levels,
<8.4 mg/dl) or severe primary hyperparathyroidism as a result of
extensive remineralization of bone tissue (18). In consequence, the patient received
medical treatment of calcium gluconate, vitamin D3 and calcitriol.
Increased PTH levels following postoperative normalization may
reveal tumor recurrence. Therefore, the PTH level should be
monitored during patient follow-up.
PTHrP caused hypercalcemia is widely observed in
various malignancies, including lung cancer (19), breast carcinoma (20), hematological malignancies (21) and squamous cell carcinomas of the head
and neck. PTHrP protein has been observed in normal parathyroid,
adenomas and hyperplasia (22).
However, PTHrP has not yet been reported in PTCA to the best of our
knowledge. The present study is the first report that the tumor
tissue of PTCA is able to express PTHrP, which contributes to the
pathogenesis of hypercalcemia in PTCA with hypersecretion of PTH.
Furthermore, PTHrP may cause hypercalcemia with normal levels of
PTH (23).
The majority of clinicians recommend en bloc
resection at the initial surgery to offer the best chance for cure
(5), but it requires accurate
positioning prior to the operation and to ascertain its nature.
Although markedly elevated serum Ca, PTH, AKP and tumor size
indicate the presence of tumor tissue (2), clinicians have to decide the origin of
the ectopic mass. Ultrasound is widely applied in routine
inspection of the thyroid and parathyroid (24), but it could not diagnose parathyroid
malignancy. However, the sensitivity of Tc99m-MIBI scintigraphy
scanning combined with ultrasound is considered as high as 95% for
the diagnosis of parathyroid carcinoma (25), and this technique is able to
discriminate parathyroid masses from thyroid masses and higher
sensitivity to distinguish malignancy from benign tumor. Diagnosis
of malignant tumor, in conjunction with detailed images of enhanced
CT provide, the initial surgical approach was established. Complete
surgical resection is associated with an 8% local recurrence rate
and a long-term overall survival rate of 89% (mean follow-up time,
69 months) (26). Adjuvant radiation
therapy following surgical resection is an area of ongoing
investigation due to the common local recurrence (12).
PTCA is an extremely rare disease, but it should be
considered in patients with severe hypercalcemia (>15 mg/dl),
markedly elevated PTH (>300 pg/ml), large tumor size (median
size, 3.3 cm), AKP levels elevated by threefold or greater and
various symptoms of hyperparathyroidism. Tc99m-MIBI scintigraphy
scanning combined with ultrasound may assist with the
identification of tumor origin and nature in an ectopic mass.
In summary, the present case reported a patient with
ectopic mediastinal parathyroid carcinoma cosecreting PTHrP and
PTH, which contributed to hypercalcemia. It will be necessary to
continue monitoring the plasma levels of PTHrP and PTH in the
present patient and to perform further analyses on the different
roles of PTHrP and PTH in PTCA. Currently, surgery remains the sole
curative treatment for PTCA, although close clinical and
radiological follow-up is advocated, due to the high risk of
relapse.
Glossary
Abbreviations
Abbreviations:
|
PTCA
|
parathyroid carcinoma
|
|
Tc99m-MIBI
|
Tc99m methoxyisobutylisonitrile
|
|
PTA
|
parathyroid adenoma
|
|
AKP
|
alkaline phosphatase
|
|
CT
|
computed tomography
|
|
IHC
|
immunohistochemistry
|
|
Ca
|
calcium
|
References
|
1
|
Dudney WC, Bodenner D and Stack BC Jr:
Parathyroid carcinoma. Otolaryngol Clin North Am. 43:441–453. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Fortson JK, Su R, Patel VG and Lawrence
GE: Parathyroid carcinoma presenting with pathologic fracture: Case
report and review of the literature. Head Neck. 37:E139–E141. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kettle AG and O'Doherty MJ: Parathyroid
imaging: How good is it and how should it be done? Semin Nucl Med.
36:206–211. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Damadi A, Harkema J, Kareti R and Saxe A:
Use of pre-operative 99mTc-sestamibi scintigraphy and
intraoperative parathyroid hormone monitoring to eliminate neck
exploration in mediastinal parathyroid adenocarcinoma. J Surg Educ.
64:108–112. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tseng CW, Lin SZ, Sun CH, Chen CC, Yang
AH, Chang FY, Lin HC and Lee SD: Ectopic mediastinal parathyroid
carcinoma presenting as acute pancreatitis. J Chin Med Assoc.
76:108–111. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al-Kurd A, Mekel M and Mazeh H:
Parathyroid carcinoma. Surg Oncol. 23:107–114. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Khan MW, Worcester EM, Straus FH II, Khan
S, Staszak V and Kaplan EL: Parathyroid carcinoma in secondary and
tertiary hyperparathyroidism. J Am Coll Surg. 199:312–319. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Harari A, Waring A, Fernandez-Ranvier G,
Hwang J, Suh I, Mitmaker E, Shen W, Gosnell J, Duh QY and Clark O:
Parathyroid carcinoma: A 43-year outcome and survival analysis. J
Clin Endocrinol Metab. 96:3679–3686. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shane E: Clinical review 122: Parathyroid
carcinoma. J Clin Endocrinol Metab. 86:485–493. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McCauley LK and Martin TJ: Twenty-five
years of PTHrP progress: From cancer hormone to multifunctional
cytokine. J Bone Miner Res. 27:1231–1239. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Henderson JE, Shustik C, Kremer R, Rabbani
SA, Hendy GN and Goltzman D: Circulating concentrations of
parathyroid hormone-like peptide in malignancy and in
hyperparathyroidism. J Bone Miner Res. 5:105–113. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wei CH and Harari A: Parathyroid
carcinoma: Update and guidelines for management. Curr Treat Options
Oncol. 13:11–23. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Lumachi F, Zucchetta P, Varotto S,
Polistina F, Favia G and D'Amico D: Noninvasive localization
procedures in ectopic hyperfunctioning parathyroid tumors. Endocr
Relat Cancer. 6:123–125. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wynne AG, van Heerden J, Carney JA and
Fitzpatrick LA: Parathyroid carcinoma: Clinical and pathologic
features in 43 patients. Medicine (Baltimore). 71:197–205. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Minisola S, Cipriani C, Diacinti D,
Tartaglia F, Scillitani A, Pepe J and Scott-Coombes D: Imaging of
the parathyroid glands in primary hyperparathyroidism. Eur J
Endocrinol. 174:D1–D8. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mittendorf EA and McHenry CR: Parathyroid
carcinoma. J Surg Oncol. 89:136–142. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hofbauer LC, Spitzweg C, Arnholdt H,
Landgraf R and Heufelder AE: Mediastinal parathyroid tumor: Giant
adenoma or carcinoma? Endocr Pathol. 8:161–166. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ebina K, Miyoshi Y, Izumi S, Hashimoto J,
Naka N, Tsukamoto Y, Kashii M, Kaito T and Yoshikawa H: A case of
adolescent giant parathyroid adenoma presenting multiple osteolytic
fractures and postoperative hungry bone syndrome. Clin Case Rep.
3:835–840. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Okagawa T and Hiramatsu Y: Parathyroid
hormone-related peptide (PTHrP) producing lung cancer presenting
hypercalcemia; report of a case. Kyobu Geka. 68:237–239. 2015.(In
Japanese). PubMed/NCBI
|
|
20
|
Boras-Granic K and Wysolmerski JJ: PTHrP
and breast cancer: More than hypercalcemia and bone metastases.
Breast Cancer Res. 14:3072012. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Clines GA and Guise TA: Hypercalcaemia of
malignancy and basic research on mechanisms responsible for
osteolytic and osteoblastic metastasis to bone. Endocr Relat
Cancer. 12:549–583. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kitazawa R, Kitazawa S, Maeda S and
Kobayashi A: Expression of parathyroid hormone-related protein
(PTHrP) in parathyroid tissue under normal and pathological
conditions. Histol Histopathol. 17:179–184. 2002.PubMed/NCBI
|
|
23
|
Gurrado A, Marzullo A, Lissidini G,
Lippolis A, Rubini D, Lastilla G and Testini M: Substernal oxyphil
parathyroid adenoma producing PTHrP with hypercalcemia and normal
PTH level. World J Surg Oncol. 6:242008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kunstman JW, Kirsch JD, Mahajan A and
Udelsman R: Clinical review: Parathyroid localization and
implications for clinical management. J Clin Endocrinol Metab.
98:902–912. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gawrychowski J, Gabriel A, Kluczewska E,
Buła G and Lackowska B: Mediastinal parathyroid carcinoma: A case
report. Endokrynol Pol. 63:143–146. 2012.PubMed/NCBI
|
|
26
|
Koea JB and Shaw JH: Parathyroid cancer:
Biology and management. Surg Oncol. 8:155–165. 1999. View Article : Google Scholar : PubMed/NCBI
|