Introduction
Craniopharyngioma is a common benign tumor of the
sella region and it grows in the midline position of the
sella-hypothalamus and is closely associated with the peripheral
brain tissues, important nerves and blood vessel structures
(1). It is difficult to achieve gross
total removal of craniopharyngioma, thus, during the postoperative
period, a considerable number of patients suffer from a high rate
of mortality, tumor recurrence and postoperative complications
(2). Selecting an appropriate
surgical approach that allows preservation of vital structures
including the hypothalamus is the key to achieving gross total
removal and reduce postoperative complications (3,4). It has
been reported that, fronto-basal interhemispheric approach achieves
a high rate of gross total removal of tumor and pituitary stalk
preservation (5) and is being widely
applied in clinical setting.
In the present study, the fronto-basal
interhemispheric approach was employed in removing
craniopharyngioma in 20 patients from January, 2012 to January,
2015.
Patients and methods
Patients
In this retrospective study, radiological images,
operative studies and postoperative clinical follow-up data of 20
patients who underwent resection for craniopharyngioma via a
fronto-basal interhemispheric approach between January, 2012 to
January, 2015, were analyzed. Of the 20 patients, 12 were men and 8
women aged 15–65 years, with an average of 42.5 years. The course
of disease ranged from 1 to 36 months. Comorbid conditions such as
headache were present in 18 patients, 10 patients had visual acuity
and visual field disorders, 2 patients had polydipsia and polyuria,
8 patients had nausea and vomiting, 5 patients had retardation and
4 patients had memory loss. All the patients underwent magnetic
resonance imaging (MRI) or computed tomography (CT) scan prior to
and following resection of craniopharyngioma.
Surgical technique
To perform resection using fronto-basal
interhemispheric approach, the patient was positioned supine and
the back was elevated 20° to facilitate venous drainage. A coronal
skin incision behind the hairline was carried out. Craniotomy was
performed including the inner side of the frontal bone flap and
lower end of arcus superciliaris and basis crania after making a
single midline burrhole. The dura was cut open in an arc-shaped
manner that allowed the dissection of basal interhemispheric
fissure. This procedure exposed the end plate, optic chiasma and
anterior communicating artery from the genus of corpus callosum.
The tumor was exposed by opening of the end plate of the expanding
hole. Subsequently, the craniopharyngioma tumor was removed under
direct vision of the surgeon. The tumor that grew in the sella
region was removed after abrading the olivary eminence via
pneumatic drill and a large bone wax was used to seal the opened
sphenoid sinus. During the surgery, bipolar coagulation was used as
little as possible to preserve the pituitary stalk.
Results
Pre-operative radiological
diagnoses
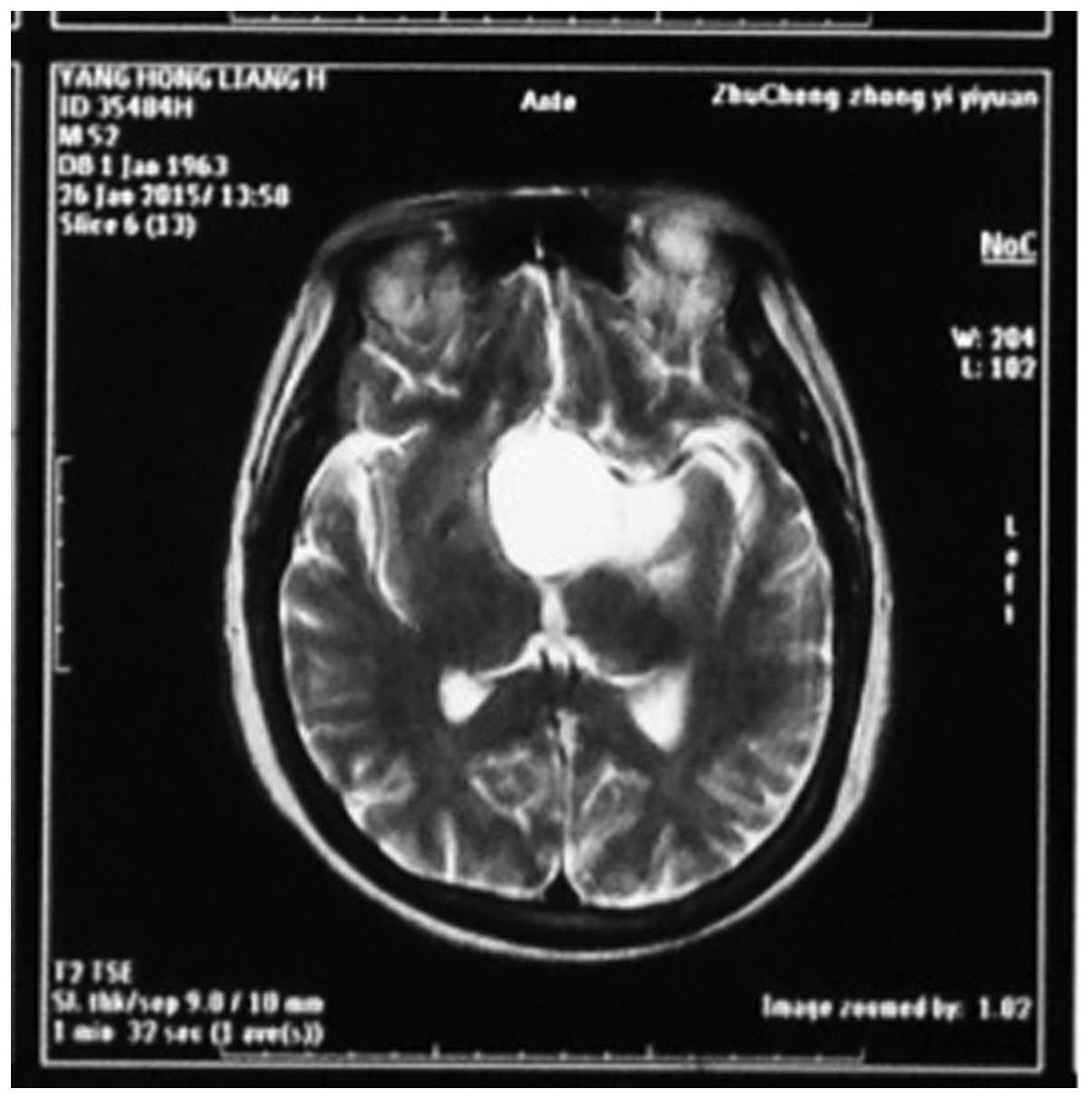
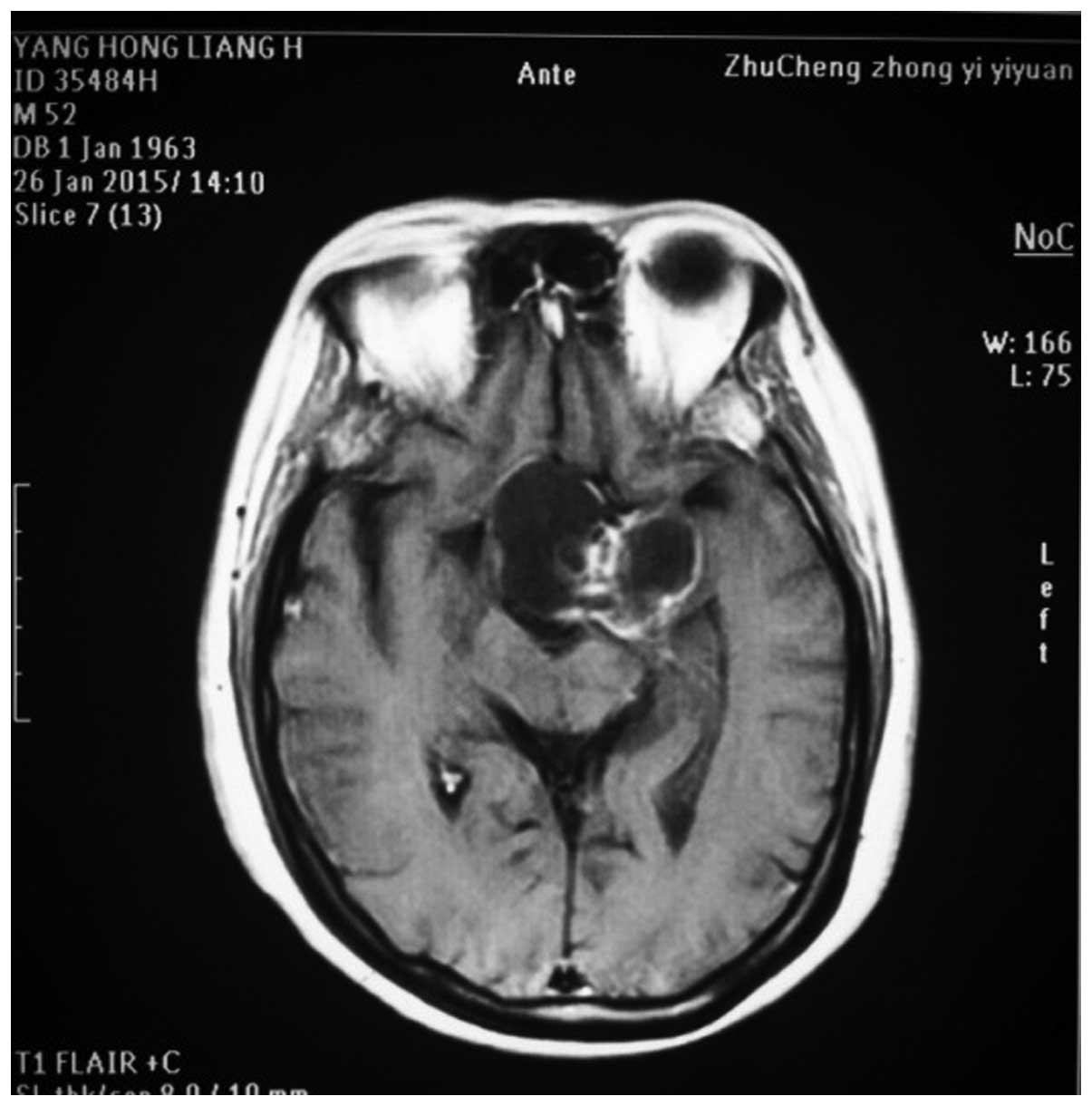
The MRI and CT investigations identified tumors in
the sellar-hypothalamus region in 10 patients, sellar-anterior
third ventricle in 5 patients, interior sellar-sellar region in 2
patients and brainstem in 3 patients. The tumors were cystic and
solid in structure in 13 patients, cystic in 4 patients and solid
in 3 patients (Figs. 1 and 2).
Post-operative radiological
diagnoses
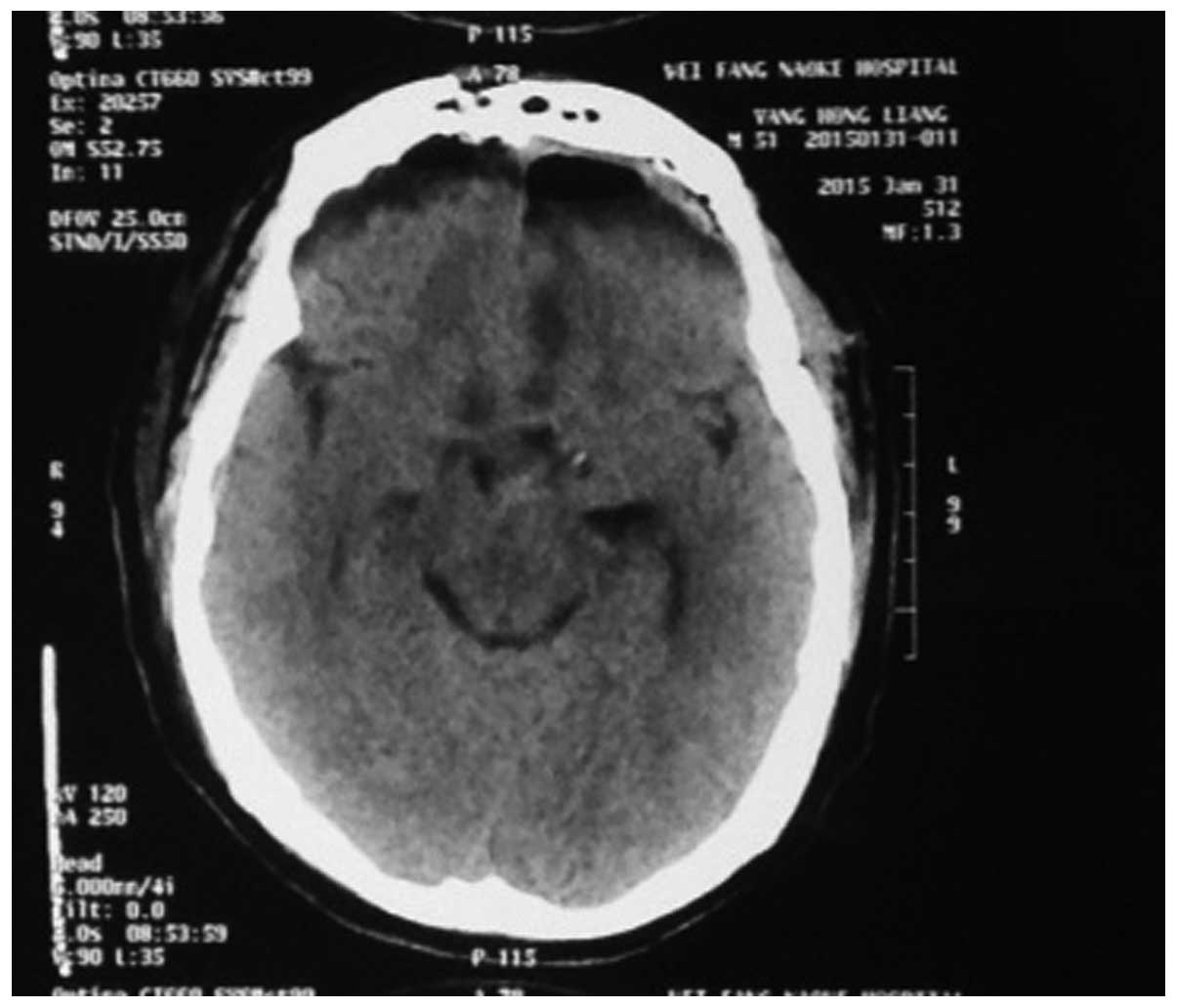
The MRI and CT investigations of patients who
underwent resection of craniopharyngioma revealed gross total
removal of tumor was achieved in 18 cases (Fig. 3), tumor residue was present in 2
patients, and the pituitary stalk was preserved in 18 patients.
Fig. 4 shows the incision of the
fronto-basal interhemispheric approach. In the immediate
post-operative period, vision was recovered or improved in 10
patients. The complications observed were polydipsia and polyuria
in 15 patients and blood electrolyte disorder in 15 patients. A
patient succumbed and the autopsy results confirmed that the
patient due to large area pulmonary embolism.
Discussion
Craniopharyngioma is a common benign epithelial
tumor and many studies have revealed that, patients can be cured if
gross total removal of tumor is achieved. Nevertheless,
craniopharyngioma is physically closely associated with
hypothalamus and important blood vessels, which makes gross total
removal difficult. Furthermore, partial removal is always
accompanied with a higher recurrence rate in comparison with gross
total removal (6).
Previously, craniopharyngioma was treated by surgery
using the pterional and callosum interhemispheric approach. The
pterional interhemispheric approach is time-consuming, and causes
serious injury and profuse bleeding. Thus, its curative effects for
tumors that invade sella, anterior third ventricle, brainstem and
posterior circulation are poor. Furthermore during surgery, it
inevitably involves the traction of internal carotid artery and
optic nerves, which may lead to hemiplegia or even coma due to
spasm of the internal carotid artery (7). The callosum interhemispheric approach
may cause damage to the bilateral fornices in the anterior corpus
callosum and when resection is carried out using this approach, it
is difficult to discern the boundary of the tumor, sella region and
optic chiasma. Thus, this approach leaves tumor residues, thereby
achieving gross total removal of tumor is less effective. Hori
et al (8) reported that the
benefits of pterional and callosum interhemispheric approaches are
limited in comparison with the fronto-basal interhemispheric
approach.
Craniopharyngioma occurs in the pituitary stalk of
the midline and grows along the midline. Since fronto-basal
interhemispheric approach can reach the endplate and chiasmatic
cistern (9) directly, it is a
convenient way to approach the tumor. In the present study, during
surgical resection, no significant structural damage occurred.
The fronto-basal interhemispheric approach was
effective in removing the tumors that grow from the sellar region
to the anterior third ventricle and even for tumors that extended
into the third ventricle. In the present study, two patients had a
tumor in their anterior third ventricle and were successfully
resected and the operative field was good. Even a large tumor that
pressed the interpeduncular cistern and grew into the anterior
pontine cistern of dorsum sella was gross totally removed under
direct vision of the surgeon.
In the present study, one patient who had tumor
closely attached to the top and branches of basal artery and showed
bulk-shaped calcification had gross total removal and no recurrence
occurred after surgery. For the tumors that grow towards the
interior sella, the fronto-basal interhemispheric approach provides
a relatively large visual angle from below and anterior direction.
If the tumors grow towards the sphenoid sinus via expanded sella
turcica, it results in a visual blind area in the anterior wall of
sella turcica. A pneumatic drill can be used to abrade the
tuberculum sellae to remove the tumor inside the sellar region. In
the current study, three patients had tumors growing towards
sphenoid sinus and the tuberculum sellae was abraded to achieve
tumor removal, but two patients showed tumor residues after
surgery. The results showed that, for the large craniopharyngioma
in the midline area of the sella region, double frontal craniotomy
combined with the fronto-basal interhemispheric approach provides
more surgical space. Sometimes, the tumor protrudes towards
internal carotid or spreads across internal carotid artery. In such
situations, use of subfrontal approach creates a larger visual
field for the surgeon.
Craniopharyngioma originates from the pituitary
stalk and tumor residues in this area are always the source of
tumor recurrence. The gross total removal of the tumors, while
preserving the pituitary stalk has been a burden to surgeons for a
long time (10). The fronto-basal
interhemispheric approach is useful for the removal of tumor
tissues in the pituitary stalk from below and posterior area or
anterior area of chiasma opticum. The retention rate of the
pituitary stalk of pterion approach was approximately 33% (11). However, in the present study using the
fronto-basal interhemispheric approach, the retention rate of the
pituitary stalk reached 90% (18 patients) and most patients
experienced diabetes insipidus after surgery in a transient
manner.
In comparison with the pterion or callosum
approaches, the fronto-basal interhemispheric approach requires
experienced surgeons. This approach involves stretching of cerebral
tissues, thus damage arising from stretching the hypothalamus were
mild but for the frontal lobe were severe. In the immediate
post-operative period, the patients experienced mental problems.
During all the surgeries, the surgeon was careful in protecting the
fine perforating arteries that originate from the anterior
communicating artery and supplying blood to the hypothalamus and
basal ganglia.
In conclusion, the fronto-basal interhemispheric
approach is safer and provides more direct surgical vision that is
benefiical in identifying the pituitary stalk and reducing damage
to the olfactory nerve, optic nerve, internal carotid artery,
hypothalamus and other important structures. The immediate
post-operative complications are also fewer and this favors rapid
recovery of patients.
References
|
1
|
Liu JK, Christiano LD, Gupta G and Carmel
PW: Surgical nuances for removal of retrochiasmatic
craniopharyngiomas via the transbasal subfrontal translamina
terminalis approach. Neurosurg Focus. 28:E62010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kassam AB, Prevedello DM, Thomas A,
Gardner P, Mintz A, Snyderman C and Carrau R: Endoscopic endonasal
pituitary transposition for a transdorsum sellae approach to the
interpeduncular cistern. Neurosurgery. 62:57–72. 2008.PubMed/NCBI
|
|
3
|
Pettorini BL, Frassanito P, Caldarelli M,
Tamburrini G, Massimi L and Di Rocco C: Molecular pathogenesis of
craniopharyngioma: switching from a surgical approach to a
biological one Neurosurg. Focus. 28:E12010.
|
|
4
|
Campbell PG, McGettigan B, Luginbuhl A,
Yadla S, Rosen M and Evans JJ: Endocrinological and
ophthalmological consequences of an initial endonasal endoscopic
approach for resection of craniopharyngiomas. Neurosurg Focus.
28:E82010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kassam AB, Gardner PA, Snyderman CH,
Carrau RL, Mintz AH and Prevedello DM: Expanded endonasal approach,
a fully endoscopic transnasal approach for the resection of midline
suprasellar craniopharyngiomas: a new classification based on the
infundibulum. J Neurosurg. 108:715–728. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nishimoto A, Matsuhisa T, Kunishio K,
Maeshiro T, Furuta T and Ohmoto T: Craniopharyngioma: Early and
long term recurrence after partial removal. J Neurol Neurosurg
Psychiatry. 58:111–112. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kunihiro N, Goto T, Ishibashi K and Ohata
K: Surgical outcomes of the minimum anterior and posterior combined
transpetrosal approach for resection of retrochiasmatic
craniopharyngiomas with complicated conditions. J Neurosurg.
120:1–11. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hori T, Kawamata T, Amano K, Aihara Y, Ono
M and Miki N: Anterior interhemispheric approach for 100 tumors in
and around the anterior third ventricle. Neurosurgery. 66:65–74.
2010.PubMed/NCBI
|
|
9
|
Jung TY, Jung S, Choi JE, Moon KS, Kim IY
and Kang SS: Adult craniopharyngiomas: surgical results with a
special focus on endocrinological outcomes and recurrence according
to pituitary stalk preservation. J Neurosurg. 111:572–527. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Garrè ML and Cama A: Craniopharyngioma:
modern concepts in pathogenesis and treatment. Curr Opin Pediatr.
19:471–479. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shi XE, Wu B, Zhou ZQ, Fan T and Zhang YL:
Microsurgical treatment of craniopharyngiomas: report of 284
patients. Chin Med J (Engl). 119:1653–1663. 2006.PubMed/NCBI
|