Introduction
Hemangioma is a common benign vascular tumor usually
observed in the liver, skin, eyes and central nervous system.
However, intramuscular hemangiomas (IHs) are extremely rare,
accounting for <1% of all hemangiomas (1). IH frequently occurs in the extremities,
particularly the lower limbs. Since the majority of lesions are
small, isolated and asymptomatic, the true incidence of hemangioma
is very difficwult to calculate (2).
Chronic pain and novel mass development comprise the most common
symptoms of IH and hemangioma in general (3). Diagnostic methods for IH and hemangioma
include clinical and laboratory examination, plain radiographs,
ultrasound, computed tomography (CT), angiography and magnetic
resonance imaging (MRI) (4). There
are several treatment methods available for IH and hemangioma,
including conservative therapy, systemic corticosteroids,
embolization, radiation, sclerotherapy and surgical excision.
Treatment for IH and hemangioma should be individualized (5). In the present study, the patient was
mistakenly diagnosed with a common traumatic femoral fracture. The
missed diagnosis of IH led to the rupture of an incision following
open reduction and internal fixation (ORIF), which was accompanied
by extensive blood loss. A careful review of the patient's history
and detailed clinical examination are important for the
identification of fractures, particularly in cases without a
definite history of trauma. In the present study, CT and
arteriography confirmed the diagnosis of pathological femoral
fracture with IH; however, the misdiagnosis of the patient's
condition resulted in a markedly high cost and suffering for the
patient. The present study was approved by the Ethics Review
Committee of The First Affiliated Hospital of Nanchang University
(Nanchang, China), and written informed consent was obtained from
the patient.
Case report
A 46-year-old male patient visited the Orthopedic
Clinic of a local hospital (Yichun City Chinese Medicine Hospital,
Yichun, China) in December 2014, complaining of severely painful
swelling in his right thigh, which was preceded by a mild sprain
that occurred whilst lifting heavy weights. Plain film radiographs
(Kodak DirectView DR9000; Kodak, Rochester, NY, USA) performed at
the local general hospital revealed a traumatic femoral fracture,
which was treated by ORIF. The patient was discharged without any
complications 2 weeks later, after the incision had healed.
However, 20 days following surgery, gradual swelling and soreness
with no obvious cause was observed around the incision. Eventually,
the incision ruptured during squatting for bowel movement, which
resulted in marked blood loss. The patient was referred to the
Department of Orthopedics of The First Affiliated Hospital of
Nanchang University for further treatment and was admitted in
January 2015. A series of laboratory tests were performed shortly
following admission: Blood hemoglobin levels were 66 g/l (normal
ranges, 120–160g/l), while inflammatory and tumor markers were
within the normal ranges. Coagulant function was normal. The
patient was diagnosed with severe hemorrhagic anemia, and required
a transfusion of 12 units red blood cell suspensions, 18 units
fresh frozen plasma, 13 units platelets and 20 units
cryoprecipitate within 2 days of hospital admission. However,
hemoglobin levels were only slightly increased to ~80 g/l, and
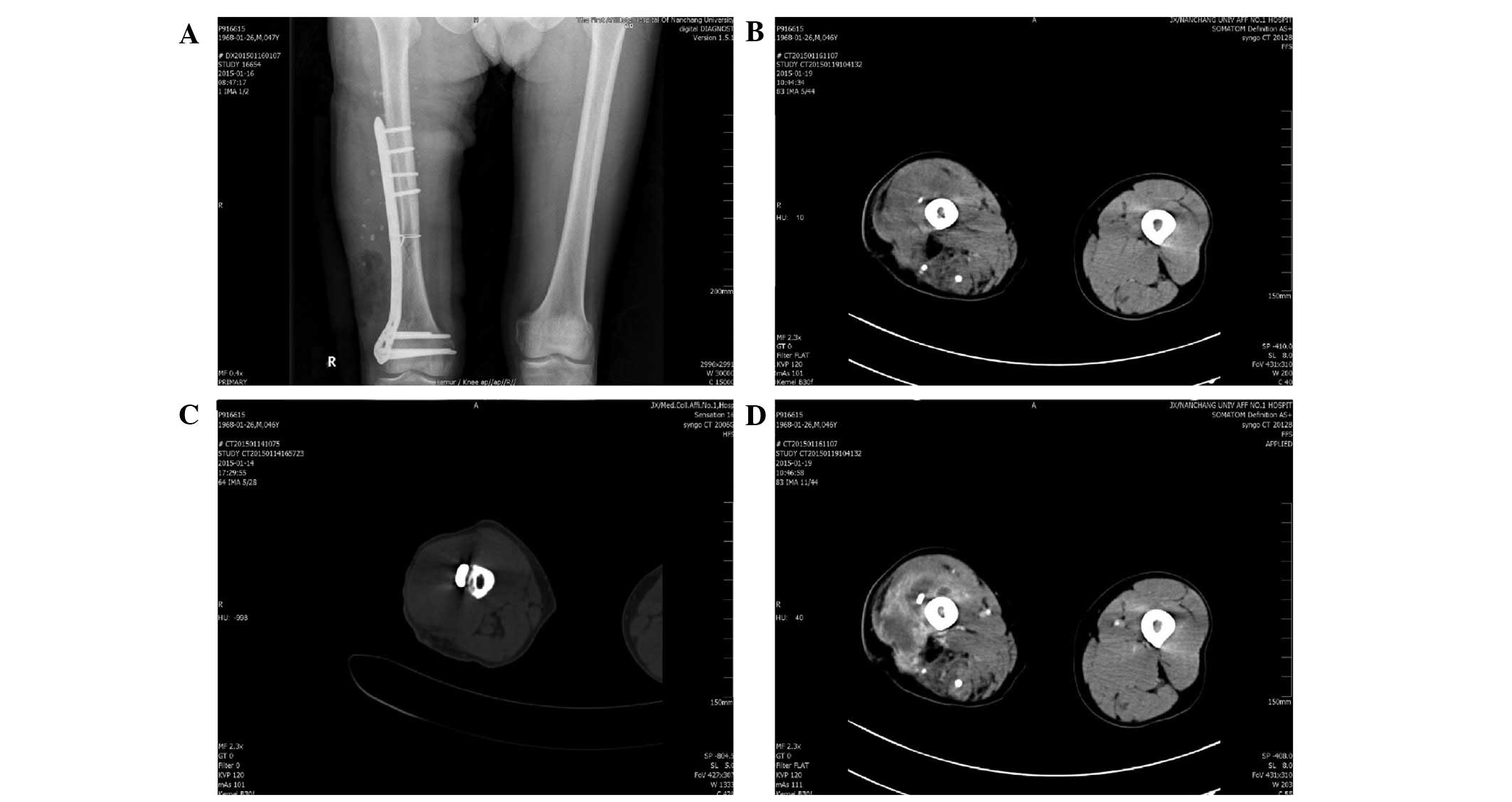
heavy bleeding due to the ruptured incision was observed. Plain
radiographs revealed the presence of multiple radiopaque calcified
bodies around the fracture (Fig. 1).
In addition, they showed that the fracture had been considerably
reduced following ORIF at the Yichun City Chinese Medicine Hospital
(Fig 2A). A diagnosis of inter- or IH
with calcification was considered; however, the differential
diagnosis for the patient's condition was extensive, including
parenchymal foreign bodies, myositis ossifications, aggressive
fibromatosis and postoperative infection. CT (SOMATOM Definition AS
CT Scanner; Siemens Healthcare, Henkestr, Germany) revealed an
irregularly low-density mass shadow surrounding the femoral shaft
in the anterolateral muscles of the right middle and distal thigh,
and punctate calcification was observed (Fig. 2B). Following careful observation of
the scans, cortical thinness and bone destruction was identified in
the fracture ends (Fig. 2C). Enhanced
CT demonstrated clear peripheral enhancement of the mass (Fig. 2D).
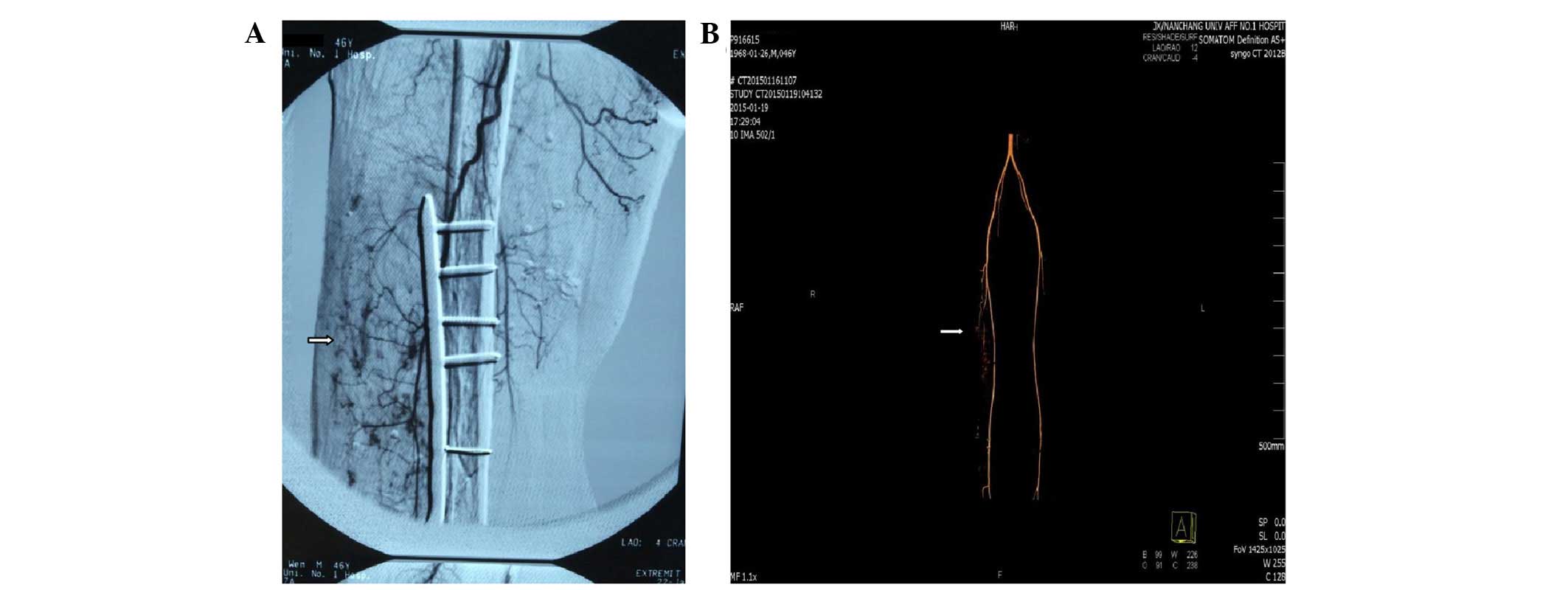
Based on the aforementioned findings, IH with
pathological femoral fracture was suspected, and femoral artery
arteriography was performed. Selective angiography (Axiom Artis BA
DSA; Siemens Healthcare) demonstrated that the deep femoral artery
was the feeder vessel of the IH (Fig. 3A
and B); therefore, the patient underwent selective embolization
of the deep femoral artery. Several days following treatment, the
condition of the patient improved and the bleeding gradually
stopped. The diagnosis of IH with pathological femoral fracture was
confirmed based on these observations. The patient was discharged
without complications 1 week subsequent to arterial embolization,
when the patient's hemoglobin levels had reached 110 g/l. The
patient was monitored by plain radiograph and CT scan during the 6
months of postoperative follow-up and by plain radiograph and MRI
scan (Magnetom Trio Tim 3.0; Siemens AG, Munich, Germany) for 9
months after that; no sign of recurrence was observed and the
patient returning to work. At the time of writing the fracture had
healed. Rigorous monitoring of patients with pathological femoral
fracture with IH is essential in order to detect any local
recurrence or non-union of the femoral shaft.
Discussion
Hemangiomas are benign vascular tumors that are most
likely to arise from the embryonic rest of unipotent angioblastic
cells that have failed to develop into normal blood vessels.
Hemangiomas account for 7–10% of all soft-tissue tumors (6,7). IH is the
most common type of deep soft-tissue hemangioma, one of the most
common types of deep-seated soft tissue tumors, as well as the most
common type of benign tumors of muscle (5). The majority of IHs originate in the
skeletal muscle of the extremities, particularly the lower
extremities. IH accounts for <1% of all hemangiomas, and are
primarily observed in young adults aged <30 years (8,9). Chronic
pain and novel mass development are the most common symptoms of IH
(3). Pain has been recorded in 60% of
cases, and is most frequent in long and narrow muscles. Pain is
often aggravated by exercise of the involved muscles, since
vascular dilation and increased regional blood flow leads to
swelling and compressive pain (10,11). A
palpable tender mass is observed in the majority of IH cases. Large
hemangiomas are identified by the detection of a vascular murmur or
tremor upon palpation (2,12). Superficial vein dilation may also be
observed with cutaneous extension, and the tumor is generally
long-standing, large and slowly-growing (4). Complications have been reported, such as
nerve compression and compartment-like syndromes (13,14). In
general, IH is rarely considered in the differential diagnosis of
musculoskeletal pain. The average duration of symptoms at initial
presentation is 13 months, and so chronic extremity pain should
increase suspicion for the presence of IH (2,15). IH
presenting with pathological fracture is extremely rare. It is
essential that IH is considered in the differential diagnosis of
parenchymal foreign bodies, myositis ossifications, aggressive
fibromatosis and postoperative infection, when multiple radiopaque
calcified bodies are observed around the fracture using plain
radiographs. A diagnosis of IH is usually based on medical history,
clinical examination and a combination of imaging studies.
The pathophysiology of these lesions has not been
fully determined, but information may be gained from their
underlying vascular nature. Isolated lesions are benign tumors that
do not metastasize, but enlarge and involute over time (16). There are 3 histological types of
hemangiomas: Capillary, cavernous and mixed. The majority of IHs
are capillary, although, sometimes, mixed IHs may also have a
dominant capillary component (17).
The present case was a capillary IH, according to the findings of
the deep femoral artery arteriography. Pathology was not performed
as it was not necessary for the diagnosis.
IHs are evaluated with plain radiographs,
ultrasound, CT, angiography and MRI. MRI is the preferred
diagnostic modality, as it effectively differentiates between
hemangiomas and malignant tumors without a biopsy. On T2-weighted
images IH exhibits a high-signal intensity compared to skeletal
muscle, which suggests the presence of dilated vascular spaces
filled with stagnant blood. On T1-weighted images, 70% of IHs
exhibit mildly hyperintense signals compared to skeletal muscle,
while 30% are hyperintense (4,18,19). On plain radiographs, rounded
soft-tissue calcifications, known as ‘phleboliths’ or ‘venous
stones’, may be observed in certain hemangiomas. Musculoskeletal
ultrasound may reveal a mass, and is effective in the workup of IH.
However, ultrasound does not reliably identify pathognomonic
features of hemangiomas, but it does reveal abnormal Doppler flow
patterns or features consistent with phleboliths (20). CT is helpful in excluding other types
of masses from diagnosis, but is not always reliable in defining
hemangiomas. Occasionally, angiography is required to demonstrate
the fine vascular details of a hemangioma. This may be helpful in
cases where embolization or surgical resection of complex lesions
is considered. The majority of imaging modalities may identify
certain features of IH, and therefore biopsy is rarely required to
rule out malignancy. However, if diagnostic uncertainty remains
following clinical examination and imaging, open or needle biopsy
is recommended (18,21). A definitive diagnosis is only
demonstrated following histopathological evaluation of the entire
tumor.
Several treatment methods have been proposed for IH,
including conservative management, systemic corticosteroids,
embolization, radiation, sclerotherapy and surgical excision. Each
individual case requires thorough consideration of the unique
characteristics of the lesion and degree of functional impairment.
Conservative management is the preferred treatment option for
nearly all isolated IHs; however, complete surgical excision of the
lesion is the mainstay of IH treatment in the presence of rapid
tumor growth, intense pain, risk of local skin necrosis, cosmetic
or functional impairment or suspicion of malignancy. However,
recurrence rates, particularly following incomplete surgical
excision are between 18 and 61% (5,22).
Surgical margins and tumor size have been reported as risk factors
for recurrence. Selective embolization is feasible as large caliber
vessels, which feed IH, are available for the procedure, as
demonstrated by the present case. In addition, preoperative
embolization is also performed for diffuse hemangiomas, when
arteriography highlights tributary arteries of sufficient diameter
(23). Additional treatments, such as
corticosteroids, radiation and sclerotherapy, are available, but
are rarely used due to side-effects and less successful long-term
outcomes: Side-effects of corticosteroids include elevated blood
pressure, changes to cholesterol levels, mood swings, acne and
premature balding; side-effects of radiation include nausea,
vomiting, inhibition of hematopoiesis and skin ulcers, and
side-effects of sclerotherapy include tissue necrosis and pulmonary
embolism (2,24). Surgical excision is occasionally
impractical; not all patients are recommended for surgery, and
complex high-risk infiltrating lesions exist. In these cases,
sclerotherapy, corticosteroids or radiation therapy may be
beneficial.
In conclusion, the present study reports the case of
a 46-year-old male patient who suffered from IH of the right thigh
and presented with a pathological femoral fracture. Initially, the
patient was misdiagnosed with traumatic femoral fracture, and
routine open reduction and internal fixation were performed;
however, based on the patient's medical history, plain radiographs,
CT and artery arteriography, the diagnosis of pathological femoral
fracture with IH was eventually made. In conclusion, a differential
diagnosis of IH with pathological fracture should be considered
when multiple radiopaque calcified bodies are observed around the
fracture. In the present study, after 6 months of follow-ups, the
patient was symptom-free, with CT demonstrating no evidence of
recurrence. As the risk of tumor recurrence is high in IH,
long-term follow-up is required.
Acknowledgements
This study was supported by the Gan-Po Talents
Project 555 of Jiangxi Province and the Support Plan of Science and
Technology Department of Jiangxi Province (grant no.
20112BBG70020).
References
|
1
|
Zide BM and Levine SM: Hemangioma update:
Pearls from 30 years of treatment. Ann Plast Surg. 69:99–103. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wierzbicki JM, Henderson JH, Scarborough
MT, Bush CH, Reith JD and Clugston JR: Intramuscular hemangiomas.
Sports Health. 5:448–454. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kryzak TJ and DeGroot H III: Adult onset
flatfoot associated with an intramuscular hemangioma of the
posterior tibialis muscle. Orthopedics. 31:2802008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Griffin N, Khan N, Thomas JM, Fisher C and
Moskovic EC: The radiological manifestations of intramuscular
haemangiomas in adults: Magnetic resonance imaging, computed
tomography and ultrasound appearances. Skeletal Radiol.
36:1051–1059. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tang P, Hornicek FJ, Gebhardt MC, Cates J
and Mankin HJ: Surgical treatment of hemangiomas of soft tissue.
Clin Orthop Relat Res. 399:205–210. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Jahn H and Nissen HM: Haemangioma of the
urinary tract: Review of the literature. Br J Urol. 68:113–117.
1991. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rigopoulou A and Saifuddin A: Intraosseous
hemangioma of the appendicular skeleton: Imaging features of 15
cases and a review of the literature. Skeletal Radiol.
41:1525–1536. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brown RA, Crichton K and Malouf GM:
Intramuscular haemangioma of the thigh in a basketball player. Br J
Sports Med. 38:346–348. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wu JL, Wu CC, Wang SJ, Chen YJ, Huang GS
and Wu SS: Imaging strategies in intramuscular haemangiomas: An
analysis of 20 cases. Int Orthop. 31:569–575. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wild AT, Raab P and Krauspe R: Hemangioma
of skeletal muscle. Arch Orthop Trauma Surg. 120:139–143. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ranero-Juárez AG, Rosales-Galindo VM,
León-Takahashi AM, Arenas-Guzmán R and García C: Intramuscular
hemangiomas of the extremities: Report of six cases. Int J
Dermatol. 48:875–878. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jamshidi K, Jafari D, Ramezan Shirazi M,
Pahlevansabagh A and Shoushtaryzadeh T: An unusual presentation of
ossified intramuscular hemangioma: A case report. Acta Med Iran.
52:319–322. 2014.PubMed/NCBI
|
|
13
|
Downey-Carmona FJ, González-Herranz P, De
La Fuente-González C and Castro M: Acute compartment syndrome of
the foot caused by a hemangioma. J Foot Ankle Surg. 45:52–55. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nazzi V, Messina G, Dones I, Ferroli P and
Broggi G: Surgical removal of intramuscular arteriovenous
hemangioma of the upper left forearm compressingradial nerve
branches. J Neurosurg. 108:808–811. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wisniewski SJ, Newcomer K and Stanson AW:
Intramuscular hemangioma of the foot: A diagnostic dilemma. Med Sci
Sports Exerc. 37:1655–1657. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Henderson J, Wierzbicki J, Clugston J and
Patel N: Ten years of lower leg pain: Intramuscular hemangioma. Med
Sci Sports Exer. 42:52010.
|
|
17
|
Lee JK and Lim SC: Intramuscular
hemangiomas of the mylohyoid and sternocleidomastoid muscle. Auris
Nasus Larynx. 32:323–327. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Buetow PC, Kransdorf MJ, Moser RP Jr,
Jelinek JS and Berrey BH: Radiologic appearance of intramuscular
hemangioma with emphasis on MR imaging. AJR Am J Roentgenol.
154:563–567. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Teo EL, Strouse PJ and Hernandez RJ: MR
imaging differentiation of soft tissue hemangiomas from malignant
soft-tissue masses. AJR Am J Roentgenol. 174:1623–1628. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
McNeill TW, Chan GE, Chapek V and Ray RD:
The value of angiography in the surgical management of deep
hemangiomas. Clin Orthop Relat Res. 101:176–181. 1974.PubMed/NCBI
|
|
21
|
Greenspan A, McGahan JP, Vogelsang P and
Szabo RM: Imaging strategies in the evaluation of soft-tissue
hemangiomas of the extremities: Correlation of the findings of
plain radiography, angiography, CT, MRI and ultrasonography in 12
histologically proven cases. Skeletal Radiol. 21:11–18. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Bella G, Manivel J, Thompson RC Jr,
Clohisy DR and Cheng EY: Intramuscular hemangioma: Recurrence risk
related to surgical margins. Clin Orthop Relat Res. 459:186–191.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Holzapfel BM, Geitner U, Diebold J, Glaser
C, Jansson V and Dürr HR: Synovial hemangioma of the knee joint
with cystic invasion of the femur: A case report and review of the
literature. Arch Orthop Trauma Surg. 129:143–148. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zide BM and Levine SM: Hemangioma update:
Pearls from 30 years of treatment. Ann Plast Surg. 69:99–103. 2012.
View Article : Google Scholar : PubMed/NCBI
|