Introduction
Laryngeal carcinoma is the second most prevalent
malignancy located in the head and neck region (1). Chemotherapy is a common therapeutic
approach for patients with advanced or metastatic laryngeal
carcinoma; however, multidrug resistance (MDR) has been a major
contributor to the failure of chemotherapy in patients presenting
with this disease (2,3). The pathogenetic mechanisms underlying
the regulation of MDR in laryngeal cancer cells currently remain
unclear.
Hypoxia has been considered as an essential feature
in human solid tumors, such as laryngeal cancer, and it affects a
number of biological cell behaviors, including angiogenesis,
apoptosis and resistance to therapy, occurring through the
regulation of gene expression and modification of certain proteins
(4). It has been reported that
hypoxia induces drug resistance in various solid tumors (5–7).
Similarly, it was confirmed in a previous study that hypoxia has an
effect on the regulation of MDR in human laryngeal carcinoma cells
(8). Therefore, hypoxia serves as a
major obstacle in the development of cancer chemotherapy.
Currently, further research is required to fully understand the
regulatory mechanisms of MDR in hypoxic laryngeal cancer cells.
Multidrug resistance 1 (MDR1)/P-glycoprotein (P-gp),
a plasma membrane glycoprotein encoded by the MDR1 gene, is a
member of the adenosine triphosphate-binding cassette (ABC)-type
transporter family. In a previous study, the upregulation of
MDR1/P-gp expression was associated with a poorer prognosis in
patients with human laryngeal cancer (9). It is understood that MDR1/P-gp serves a
crucial role in regulating intracellular drug concentrations,
consequently determining the drug sensitivity of human cells.
Recently, MDR1/P-gp has been elucidated to be involved in the
regulation of MDR in human laryngeal cancer cells (10,11), with
the inhibition of MDR1/P-gp expression having been confirmed as an
effective method to reverse MDR in such cells (11). Furthermore, previous data have
demonstrated that MDR1/P-gp expression is significantly upregulated
in response to hypoxia in laryngeal cancer cells (12). To the best of our knowledge, there are
currently no existing studies that focus on the function and
mechanism of MDR1/P-gp in the hypoxia-induced MDR observed in
laryngeal cancer cells.
The present study aimed to investigate the role of
MDR1/P-gp in the hypoxia-induced MDR of human laryngeal carcinoma
cells and elucidate the mechanisms underlying this.
Materials and methods
Cell culture
Human laryngeal cancer Hep-2 and AMC-HN8 cell lines
were obtained from the American Type Culture Collection (Manassas,
VA, USA) and the Asan Medical Center, Ulsan University College of
Medicine (Seoul, Korea), respectively. Each cell line was cultured
in Dulbecco's modified Eagle's medium (DMEM; Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA), supplemented with 10% fetal
bovine serum (HyClone; GE Healthcare Life Sciences, Logan, UT,
USA), 100 IU/ml penicillin and 100 IU/ml streptomycin at 37°C with
5% CO2.
Exposure to hypoxia
For hypoxic exposure, the Hep-2 and AMC-HN8 cells
were incubated in a NU-4750 US Autoflow CO2
Water-Jacketed Incubator (NuAire, Plymouth, MN, USA) at 37°C, with
1% O2 and 5% CO2 balanced by nitrogen.
Transfection of small interfering RNA
(siRNA)
The double strand siRNA oligonucleotide obtained to
target the human MDR1 gene (sense, 5′-GGAAAAGAAACCAACUGUCTT-3′; and
anti-sense, 5′-GACAGUUGGUUUCUUUUCCTT-3′) was synthesized by
Shanghai GenePharma Co. Ltd. (Shanghai, China), as previously
described (13). As a negative
control, the cells were transfected with a non-specific control
siRNA (sense, 5′-UUCUCCGAACGUGUCACGUTT-3′; and antisense,
5′-ACGUGACACGUUCGGAGAATT-3′; Shanghai GenePharma Co. Ltd.), which
had no homology to any human transcripts on record. The cells were
cultured in antibiotic-free medium for 24 h prior to transfection
with 100nM siRNA using Lipofectamine® 2000 (Invitrogen;
Thermo Fisher Scientific, Inc.). The cells were harvested and
examined following a 24-h transfection period.
Reverse transcription-quantitative
polymerase chain reaction (PCR) analysis
Total RNA was extracted from the laryngeal carcinoma
cells using TRIzol® Reagent (Invitrogen; Thermo Fisher
Scientific, Inc.) according to the manufacturer's protocols.
Subsequently, the isolated RNA was reverse-transcribed into
complementary DNA (cDNA) using the PrimeScript® RT
Reagent kit (Takara Bio, Inc., Otsu, Japan), as previously
described (14). The primers used
were as follows: MDR1 sense, 5′-CTTCAGGGTTTCACATTTGGC-3′ and
antisense, 5′-GGTAGTCAATGCTCCAGTGG-3′; and glyceraldehyde
3-phosphate dehydrogenase (GAPDH) sense, 5′-CATCTTCCAGGAGCGAGA-3′
and antisense, 5′-TGTTGTCATACTTCTCAT-3′. PCR amplification was
performed in a 20-µl final reaction mixture, including a diluted
cDNA solution, 10 µM of each primer and 10 µl SYBR®
Green PCR Master Mix (Thermo Fisher Scientific, Inc.) using the ABI
7900HT Real-Time PCR system (Applied Biosystems; Thermo Fisher
Scientific, Inc.). The thermal cycling conditions were as follows:
One cycle at 95°C for 10 min and 40 cycles at 95°C for 15 sec and
60°C for 60 sec. The data were analyzed using the 2−ΔΔCq
method, as previously described (15).
Western blot analysis
The laryngeal cancer Hep-2 and AMC-HN8 cells were
harvested and lysed with cold radioimmunoprecipitation assay buffer
(Sigma-Aldrich, St. Louis, MO, USA) for 30 min. Equal amounts of
protein extract (25 µg total protein) were loaded into sodium
dodecyl sulfate polyacrylamide gel electrophoresis (5% stacking gel
and 8% separating gel), followed by separation at 80 V for ~2 h and
transferal onto Immobilon®-P PVDF Membranes (EMD
Millipore, Billerica, MA, USA), blocked with 4% skimmed milk for
1.5 h at room temperature. Protein extracts were incubated
overnight at 4°C with the primary antibodies [mouse monoclonal
anti-human MDR1/P-gp (catalog no., ab3366; 1:200; Abcam, Cambridge,
UK) and mouse monoclonal anti-human GAPDH (1:1,000;
Sigma-Aldrich)], followed by incubation for 1 h with the secondary
antibodies [horseradish peroxidase-conjugated anti-mouse secondary
antibodies (1:5,000; Sigma-Aldrich)]. Finally, protein bands were
detected by electrogenerated chemiluminescence according to the
manufacturer's protocols (GE Healthcare Bio-Sciences, Pittsburgh,
PA, USA).
Cell cytotoxicity assay
The sensitivity of the Hep-2 and AMC-HN8 cells to
fluorouracil (5-FU), cisplatin, doxorubicin, paclitaxel and
gemcitabine was determined using a cell counting kit 8 (CCK-8)
assay. The cells were plated in 96-well culture panels (Hep-2,
5×103 cells/well; and AMC-HN8, 8×103
cells/well), and following 12 h, the cells were treated with
relevant doses of chemotherapeutic agents (5-fluorouracil: 0.1, 1,
10, 100 and 1000 µg/ml; gemcitabine: 0.032, 0.32, 3.2, 32 and 320
µg/ml; cisplatin: 0.03, 0.3, 3.0, 30 and 300µg/ml); adriamycin:
0.004, 0.04, 0.4, 4 and 40 µg/ml); and paclitaxel: 0.09, 0.9, 9, 90
and 900 µg/ml) and incubated for 48 h under normoxic or hypoxic
conditions. The sensitivity of the cells to each agent was detected
using CCK-8 assay, and the IC50 was calculated as the
concentration of each drug required to produce a 50% reduction in
the number of cells.
Annexin-V/propidium iodide (PI)
apoptosis assay
The apoptotic indices of the Hep-2 and AMC-HN8 cells
were examined by flow cytometry (FCM). Cells in the log phase were
grown in 6-well plates (Hep-2, 3×105 cells/well; and
AMC-HN8, 4×105 cells/well) and cultured overnight at
37°C. The culture medium was then renewed, and the cells were
incubated in normoxic or hypoxic conditions for 12 h. Cisplatin was
added to each well with a final concentration of
2.5×10−9 M, and the cells were cultured in normoxic or
hypoxic conditions for 48 h. Subsequently, 5 µl (50 µg/ml)
Annexin-V-fluorescein isothiocyanate (FITC) was added to each well,
and the cells were incubated for a further 10 min. The cells were
washed twice with DMEM and then resuspended in 190 µl
Tris-hydrochloride buffer. Next, 5 µl (20 µg/ml) PI was added to
the resuspended cells and cultured at 4°C for a further 10 min. The
mean fluorescence intensity of Annexin-V-FITC/PI was measured by
FCM. Finally, the apoptotic indices of the Hep-2 and AMC-HN8 cells
were calculated by the mean fluorescence intensity.
Rhodamine 123 (Rh123) accumulation
assay
Rh123 accumulation in the Hep-2 and AMC-HN8 cells
was analyzed by FCM, which was performed as previously described
(16). The cell suspension was
detected by a FACSCalibur Flow Cytometer (BD Biosciences, Franklin
Lakes, NJ, USA) using 488 nm excitation. All the data were analyzed
using CellQuest™ software (BD Biosciences).
Statistical analysis
Each experiment was repeated at least three times,
and the data are presented as the mean ± standard deviation.
Comparisons of quantitative variables were performed using
Student's t-test or a one-way analysis of variance using SPSS
software, version 13.0 (SPSS, Inc., Chicago, IL, USA). P<0.05
was considered to indicate a statistically significant
difference.
Results
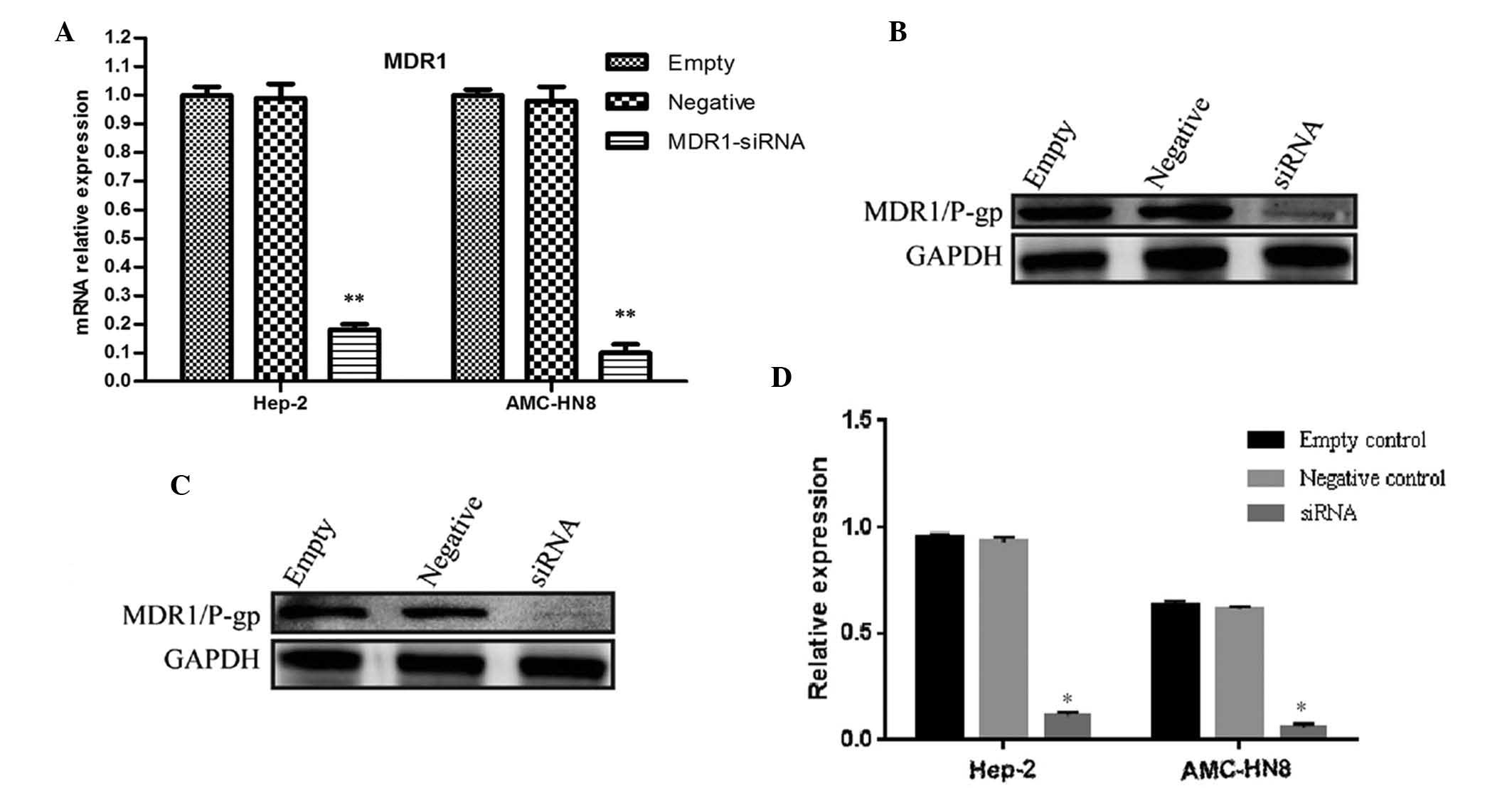
Inhibition of MDR1 gene expression by
RNA interference
In a previous study, it was confirmed that MDR1 gene
expression in human laryngeal cancer cells was upregulated by
hypoxia (12). In the present study,
the Hep-2 and AMC-HN8 cells were transfected with either
non-specific control siRNA (scrambled siRNA) or a double-strand
siRNA oligonucleotide that targeted the MDR1 gene (MDR1-siRNA) for
24 h, followed by a 24-h incubation in hypoxic conditions. As
presented in Fig. 1, compared with
the negative or untreated controls, the protein and mRNA levels of
the MDR1 gene in the hypoxic laryngeal cancer cells were
significantly reduced following transfection with MDR1-siRNA
(P<0.05).
Inhibition of MDR1/P-gp expression
suppresses MDR in hypoxic laryngeal carcinoma cells
It has been previously demonstrated that hypoxia
upregulates the sensitivity of human laryngeal cancer cells to
multiple chemotherapeutic agents (8).
In the present study, to allow for the investigation of the role of
MDR1/P-gp in hypoxia-induced MDR, the Hep-2 and AMC-HN8 cells were
transfected with MDR1-siRNA or scrambled siRNA for 24 h prior to
incubation in hypoxic conditions. Subsequently, the drug
sensitivity of the MDR1-siRNA group was compared to that of the
negative or untreated control groups using a CCK-8 assay. As
presented in Tables I and II, the sensitivity of the hypoxic laryngeal
carcinoma cells to cisplatin, gemcitabine, paclitaxel, 5-FU and
doxorubicin was significantly upregulated following the suppression
of MDR1/P-gp expression (P<0.05).
 | Table I.Effect of MDR1/P-gp expression
inhibition on the chemosensitivity of hypoxic Hep-2 cells. |
Table I.
Effect of MDR1/P-gp expression
inhibition on the chemosensitivity of hypoxic Hep-2 cells.
|
| IC50,
µg/ml |
|---|
|
|
|
|---|
| Drug | Untreated
control | Negative control | MDR1-siRNA |
|---|
| Paclitaxel |
3.90×10−2±0.21×10−2 |
3.85×10−2±0.26×10−2 |
7.61×10−3±0.39×10−3a |
| 5-FU |
240.81±0.32 |
238.90±0.21 |
78.24±0.48a |
| Doxorubicin |
3.94±0.15 |
3.96±0.24 |
2.24±0.27a |
| Gemcitabine |
39.26±0.16 |
39.18±0.28 |
28.26±0.35a |
| Cisplatin |
9.10±0.10 |
8.82±0.12 |
4.48±0.36a |
 | Table II.Effect of MDR1/P-glycoprotein
expression inhibition on the chemosensitivity of hypoxic AMC-HN8
cells. |
Table II.
Effect of MDR1/P-glycoprotein
expression inhibition on the chemosensitivity of hypoxic AMC-HN8
cells.
|
| IC50,
µg/ml |
|---|
|
|
|
|---|
| Drug | Untreated
control | Negative control | MDR1-siRNA |
|---|
| Paclitaxel |
35.54×10−3±0.36×10−3 |
36.04×10−3±0.17×10−3 |
7.23×10−3±0.58×10−3a |
| 5-FU |
230.34±0.64 |
232.48±0.92 |
71.53±0.82a |
| Doxorubicin |
3.72±0.22 |
3.87±0.35 |
2.12±0.19a |
| Gemcitabine |
36.40±0.32 |
35.58±0.29 |
21.48±0.13a |
| Cisplatin |
8.83±0.58 |
8.64±0.26 |
3.35±0.27a |
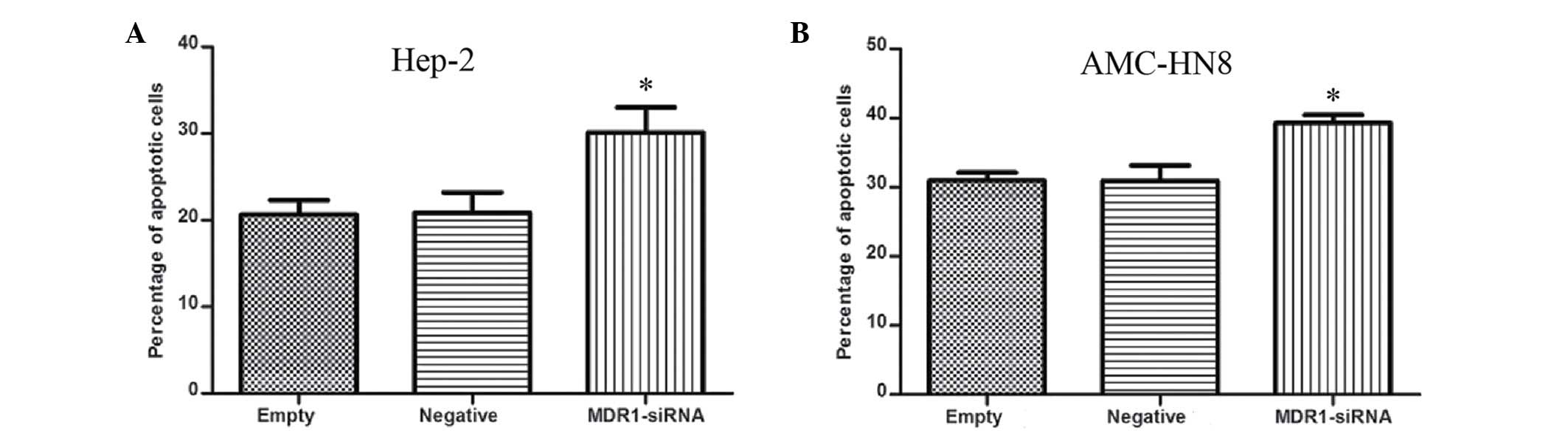
MDR1/P-gp protects hypoxic laryngeal
cancer cells from cisplatin-induced apoptosis
A previous study demonstrated that hypoxia enhances
the rate of chemotherapy-induced apoptosis in laryngeal cancer
cells (8). In the present study, FCM
with Annexin-V/PI staining was utilized to assess the role of
MDR1/P-gp in the hypoxic protection of Hep-2 and AMC-HN8 cells from
cisplatin-induced apoptosis. It was observed that the rate of
cisplatin-induced apoptosis was significantly increased under
hypoxic conditions in the MDR1-siRNA transfected cells compared
with the untreated or negative controls (P<0.05; Fig. 2).
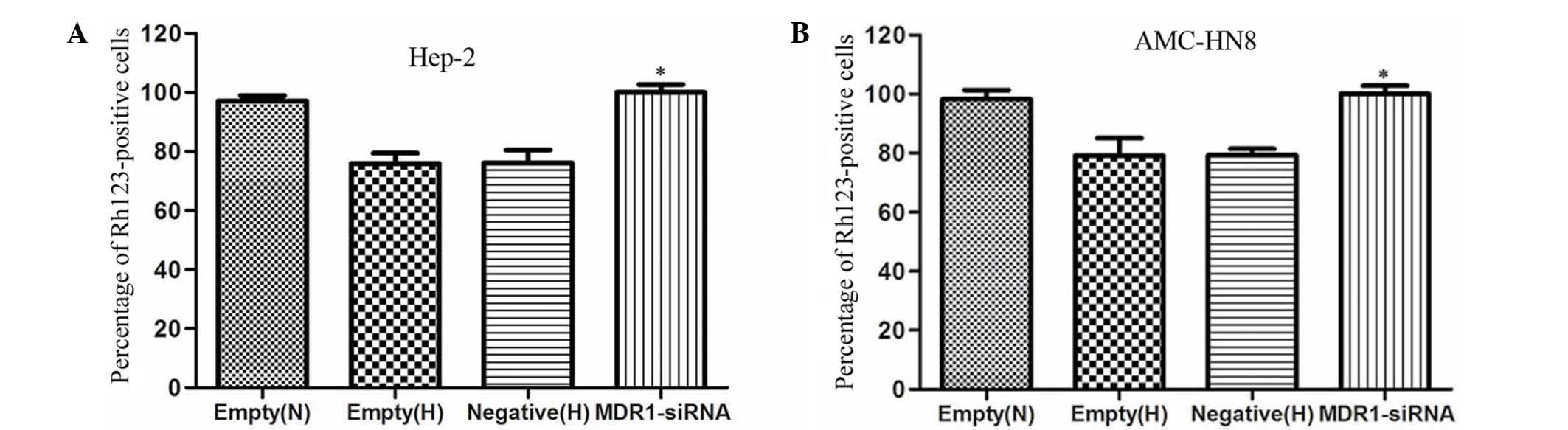
MDR1/P-gp downregulates drug
accumulation in hypoxic laryngeal cancer cells
A previous study demonstrated that hypoxia
significantly reduces the intracellular drug accumulation in
laryngeal carcinoma cells (8). In the
current study, the effect of MDR1/P-gp expression on intracellular
drug accumulation in hypoxic Hep-2 and AMC-HN8 cells was evaluated
using FCM to detect the fluorescence intensity of intracellular
Rh123 accumulation. As presented in Fig.
3, the laryngeal carcinoma cells exposed to hypoxic conditions
had significantly decreased Rh123 accumulation (P<0.05).
Furthermore, the inhibition of MDR1/P-gp expression in the hypoxic
Hep-2 and AMC-HN8 cells transfected with MDR1-siRNA significantly
increased the intracellular accumulation of Rh123 (P<0.05;
Fig. 3).
Discussion
Despite the wide application of chemotherapeutic
agents for the treatment of human laryngeal cancer, MDR remains a
major therapeutic obstacle. The hypoxic microenvironment has been
recognized as a common phenomenon in the tissues of human solid
tumors. Currently, there is increasing evidence suggesting that
hypoxic cells are somewhat resistant to conventional chemotherapy
in various human malignancies (7,17,18). A previous study confirmed that the
sensitivity of laryngeal cancer cells to multiple chemotherapeutic
drugs may be reduced by hypoxia (8).
However, the regulatory mechanism underlying hypoxia-induced MDR in
human laryngeal carcinoma cells remains to be identified.
MDR1/P-gp is a member of the ABC-type transporter
family and has been considered as a biofunctional regulator of MDR
in a series of human tumor cells (19–21). In a
previous study, it was demonstrated that the expression of
MDR1/P-gp in human laryngeal cancer tissues was associated with
malignant progression and metastasis (9). Furthermore, several studies have
reported that MDR1/P-gp may serve a crucial role in the regulation
of MDR in laryngeal cancer cells (10,11).
Zhigang et al (11) observed
that the inhibition of MDR1/P-gp expression served as an effective
method to reverse MDR in laryngeal cancer cells. Similarly, certain
studies have identified that hypoxia may contribute to MDR through
the upregulation of MDR1/P-gp expression in human tumor cells
(22,23). By contrast, Song et al
(24) indicated that MDR1/P-gp may
not be involved in hypoxia-induced MDR in non-small cell lung
cancer cells. Another previous study confirmed that hypoxia
significantly enhances the expression of MDR1/P-gp in laryngeal
carcinoma cells (12), and the
current study demonstrated that the inhibition of MDR1/P-gp
expression significantly increased the sensitivity of laryngeal
cancer cells to multiple drugs in hypoxic environments. Therefore,
further research has verified that the inhibition of MDR1/P-gp
expression upregulates the apoptosis rate of hypoxic laryngeal
cancer cells induced by chemotherapy. This suggests that MDR1/P-gp
may be partly involved in the hypoxia-induced MDR observed in
laryngeal cancer cells, and the suppression of MDR1/P-gp expression
may be considered as an effective approach to achieve MDR reversal.
The differences noted between the aforementioned studies may be due
to intrinsic differences in the regulatory mechanisms of MDR in
numerous types of tumor cells.
Theoretically, MDR1/P-gp, as an energy-dependent
membrane efflux pump, has an effect on the drug sensitivity of
human cells by regulating intracellular drug concentrations
(25,26). In a previous study, it was
demonstrated that hypoxia markedly reduced drug accumulation in
laryngeal cancer cells (8). In
practice, the results of the present study indicated that
inhibition of MDR1/P-gp expression results in the downregulation of
the transport function in hypoxic laryngeal cancer cells, leading
to increased intracellular drug concentration and suppression of
hypoxia-induced MDR. Similar to the results of Wartenberg et
al (22) and Xia et al
(23), the data from the current
study suggested that MDR1/P-gp may partly contribute to
hypoxia-induced MDR in human laryngeal cancer cells through the
regulation of drug transport. However, further research is
necessary to determine the regulatory mechanisms underlying
MDR1/P-gp expression in hypoxic laryngeal cancer cells.
In conclusion, the present study indicates that
MDR1/P-gp expression serves an important role in the mediation of
MDR in hypoxic laryngeal carcinoma cells. The results have provided
evidence that a decrease in intracellular drug concentration may
explain how MDR1/P-gp contributes to the MDR of hypoxic laryngeal
cancer cells. Therefore, targeting the MDR1 gene may be a
potentially beneficial therapeutic strategy for the reversal of
hypoxia-induced MDR in human laryngeal cancer cells.
Acknowledgements
The authors would like to thank Professor Jin-ke
Cheng and Professor Xue-mei Tong, from the Department of
Biochemistry and Molecular Biology, Shanghai Jiao Tong University
School of Medicine (Shanghai, China), for providing technical
assistance. This study was funded by the China Postdoctoral Science
Foundation (grant no. 2013M541466).
References
|
1
|
Chu EA and Kim YJ: Laryngeal cancer:
Diagnosis and preoperative work-up. Otolaryngol Clin North Am.
41:673–695, v. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Liu HC, Chen GG, Vlantis AC, Tong MC and
van Hasselt CA: Chemotherapy for laryngeal cancer - an apoptotic
approach. Curr Drug Targets. 9:878–886. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bar-Ad V, Palmer J, Yang H, Cognetti D,
Curry J, Luginbuhl A, Tuluc M, Campling B and Axelrod R: Current
management of locally advanced head and neck cancer: The
combination of chemotherapy with locoregional treatments. Semin
Oncol. 41:798–806. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wang GL, Jiang BH, Rue EA and Semenza GL:
Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS
heterodimer regulated by cellular O2 tension. Proc Natl
Acad Sci USA. 92:5510–5514. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wohlkoenig C, Leithner K, Deutsch A,
Hrzenjak A, Olschewski A and Olschewski H: Hypoxia-induced
cisplatin resistance is reversible and growth rate independent in
lung cancer cells. Cancer Lett. 308:134–143. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yoshiba S, Ito D, Nagumo T, Shirota T,
Hatori M and Shintani S: Hypoxia induces resistance to
5-fluorouracil in oral cancer cells via G(1) phase cell cycle
arrest. Oral Oncol. 45:109–115. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huang L, Ao Q, Zhang Q, Yang X, Xing H, Li
F, Chen G, Zhou J, Wang S, Xu G, et al: Hypoxia induced paclitaxel
resistance in human ovarian cancers via hypoxia-inducible factor
1alpha. J Cancer Res Clin Oncol. 136:447–456. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li DW, Dong P, Wang F, Chen XW, Xu CZ and
Zhou L: Hypoxia induced multidrug resistance of laryngeal cancer
cells via hypoxia-inducible factor-1α. Asian Pac J Cancer Prev.
14:4853–4858. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li DW, Gao S, Shen B and Dong P: Effect of
apoptotic and proliferative indices, P-glycoprotein and survivin
expression on prognosis in laryngeal squamous cell carcinoma. Med
Oncol. 28(Suppl 1): S333–S340. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li L, Jiang AC, Dong P, Wan Y and Yu ZW:
The characteristics of Hep-2 cell with multiple drug resistance
induced by Taxol. Otolaryngol Head Neck Surg. 137:659–664. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhigang H, Qi Z, Jugao F, Xiaohong C, Wei
Z, Hong W, Hu H, Na M, Zheng Y and Demin H: Reverse multidrug
resistance in laryngeal cancer cells by knockdown MDR1 gene
expression. J Otolaryngol Head Neck Surg. 38:440–448.
2009.PubMed/NCBI
|
|
12
|
Xie J, Li DW, Chen XW, Wang F and Dong P:
Expression and significance of hypoxia-inducible factor-1α and
MDR1/P-glycoprotein in laryngeal carcinoma tissue and hypoxic Hep-2
cells. Oncol Lett. 6:232–238. 2013.PubMed/NCBI
|
|
13
|
Sowter HM, Raval RR, Moore JW, Ratcliffe
PJ and Harris AL: Predominant role of hypoxia-inducible
transcription factor (Hif)-1alpha versus Hif-2alpha in regulation
of the transcriptional response to hypoxia. Cancer Res.
63:6130–6134. 2003.PubMed/NCBI
|
|
14
|
Li DW, Zhou L, Jin B, Xie J and Dong P:
Expression and significance of hypoxia-inducible factor-1α and
survivin in laryngeal carcinoma tissue and cells. Otolaryngol Head
Neck Surg. 148:75–81. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(−Delta Delta C(T)) Method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ludescher C, Thaler J, Drach D, Drach J,
Spitaler M, Gattringer C, Huber H and Hofmann J: Detection of
activity of P-glycoprotein in human tumour samples using rhodamine
123. Br J Haematol. 82:161–168. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhu H, Chen XP, Luo SF, Guan J, Zhang WG
and Zhang BX: Involvement of hypoxia-inducible factor-1-alpha in
multidrug resistance induced by hypoxia in HepG2 cells. J Exp Clin
Cancer Res. 24:565–574. 2005.PubMed/NCBI
|
|
18
|
Liu L, Ning X, Sun L, Zhang H, Shi Y, Guo
C, Han S, Liu J, Sun S, Han Z, et al: Hypoxia-inducible factor-1
alpha contributes to hypoxia-induced chemoresistance in gastric
cancer. Cancer Sci. 99:121–128. 2008.PubMed/NCBI
|
|
19
|
Huang C, Xu D, Xia Q, Wang P, Rong C and
Su Y: Reversal of P-glycoprotein-mediated multidrug resistance of
human hepatic cancer cells by Astragaloside II. J Pharm Pharmacol.
64:1741–1750. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hao YX, He ZW, Zhu JH, Shen Q, Sun JZ, Du
N and Xiao WH: Reversal of multidrug resistance in renal cell
carcinoma by short hairpin RNA targeting MDR1 gene. Chin Med J
(Engl). 125:2741–2745. 2012.PubMed/NCBI
|
|
21
|
Jia M, Hu J, Li W, Su P, Zhang H, Zhang X
and Zhou G: Trps1 is associated with the multidrug resistance of
osteosarcoma by regulating MDR1 gene expression. FEBS Lett.
588:801–810. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wartenberg M, Ling FC, Müschen M, Klein F,
Acker H, Gassmann M, Petrat K, Pütz V, Hescheler J and Sauer H:
Regulation of the multidrug resistance transporter P-glycoprotein
in multicellular tumor spheroids by hypoxia-inducible factor
(HIF-1) and reactive oxygen species. FASEB J. 17:503–505.
2003.PubMed/NCBI
|
|
23
|
Xia S, Yu SY, Yuan XL and Xu SP: Effects
of hypoxia on expression of P-glycoprotein and multidrug resistance
protein in human lung adenocarcinoma A549 cell line. Zhonghua Yi
Xue Za Zhi. 84:663–666. 2004.(In Chinese). PubMed/NCBI
|
|
24
|
Song X, Liu X, Chi W, Liu Y, Wei L, Wang X
and Yu J: Hypoxia-induced resistance to cisplatin and doxorubicin
in non-small cell lung cancer is inhibited by silencing of
HIF-1alpha gene. Cancer Chemother Pharmacol. 58:776–784. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kimura Y, Matsuo M, Takahashi K, Saeki T,
Kioka N, Amachi T and Ueda K: ATP hydrolysis-dependent multidrug
efflux transporter: MDR1/P-glycoprotein. Curr Drug Metab. 5:1–10.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ueda K: Molecular mechanisms for drug
transport by MDR1/P-glycoprotein. Tanpakushitsu Kakusan Koso.
42:1263–1272. 1997.(In Japanese). PubMed/NCBI
|