Introduction
T-Lymphoblastic lymphoma (T-LBL) is a rare and
aggressive subtype of adult non-Hodgkin's lymphoma (NHL) (1). The unique clinical and biological
characteristics of T-LBL, including a male predominance and a high
incidence of mediastinal tumors, differ from those of diffuse large
B-lymphoblastic lymphoma, which is the most common type of NHL
(1). In addition, T-LBL has a poor
long-term survival rate with standard cyclophosphamide,
doxorubicin, vincristine and prednisolone-like chemotherapy
(2).
Fluorine-18 fluorodeoxyglucose positron emission
tomography (FDG-PET) has been widely used for the evaluation of
lymphoma, including NHL (3). With
FDG-PET, it is possible to assess the lymphoma burden in the entire
body, as FDG-PET is a more sensitive and specific diagnostic tool
compared with other imaging modalities, such as computed tomography
(3). Malignant and aggressive
lymphomas typically exhibit a higher FDG uptake on FDG-PET scans
(3). In addition, certain studies
have reported the FDG-PET findings of lymphoma subtypes (4). However, only a few studies have
described the FDG-PET findings in T-LBL patients (4,5).
The aim of the present study was to evaluate FDG-PET
images in patients with a specific subtype of lymphoma, T-LBL.
Patients and methods
Patients
In total, 9 patients (8 men and 1 woman; mean age,
30±8.3 years) with initially histopathologically confirmed T-LBL at
the Korean Institute of Radiological and Medical Sciences, Seoul,
Republic of Korea, between January 2000 and December 2005, were
retrospectively enrolled in the present study. The present study
was approved by the Ethics Committee of the Korean Institute of
Radiological and Medical Sciences (Institutional Review Board no.
K-1507-002-026).
Histopathological diagnosis
Specimens obtained by lymph node or tumor biopsy
were assessed by histological or cytological examination. Specimens
were embedded with paraffin and fixed with formalin, and then cut
into 2-mm thick sections. Bone marrow (BM) involvement or leukemic
transformation (LT) was confirmed by iliac crest marrow biopsy and
peripheral blood blast count.
FDG-PET image acquisition
FDG-PET scans were acquired at the initial
pre-therapeutic period. Images were obtained with conventional PET
scanners (GE Advance Scanner; GE Medical Systems, Waukesha, WI,
USA; or ECAT EXACT HR+ Scanner; Siemens, Knoxville, TN, USA). All
patients fasted for at least 6 h and serum glucose levels were
<180 mg/dl prior to scanning. At 60 min after the intravenous
injection of 370–555 MBq FDG, the image acquisition was
started.
Image analysis
Two experienced nuclear physicians assessed the
FDG-PET images using visual analysis and maximum standardized
uptakes (SUVmax). In the visual analysis, an increased tracer
uptake pattern (diffuse, nodular or localized) and uptake intensity
(mild, moderate or intense) were considered for assessment. The SUV
was calculated as follows: SUV = mean activity [region of interest
(ROI)] (MBq/ml) / injected dose (MBq) / total body weight(g). Among
these SUVs from the targeted ROI, the SUVmax were defined as the
highest SUVs of pixels in the ROI.
Results
As shown in Table I, 8
patients presented with BM involvement; 7 showed LT and 1 patient
showed BM involvement without LT at the initial diagnosis.
 | Table I.Characteristics of the 9 T-LBL
patients. |
Table I.
Characteristics of the 9 T-LBL
patients.
|
|
|
|
|
|
|
| Nodal FDG uptake |
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Case no. | Gender/age | Histological
type | Ki-67 index | BM | LT | PET pattern | Intensity | SUVmax | Mediastinal FDG
uptake | Clinical outcome |
|---|
| 1 | M/33 | T-LBL | 30 | + | + | Diffuse | Mild | 3.97 | + | CR (22 mo+) |
| 2 | M/33 | T-LBL | X | + | + | Diffuse | Intense | 11.1 | + | Early death |
| 3 | M/19 | T-LBL | 60 | − | − | Localize | Intense | 12.2 | + | CR in death |
| 4 | M/40 | T-LBL | 40 | + | − | Nodular | Intense | 8.37 | − | CR (30 mo+) |
| 5 | F/37 | T-LBL | 50 | + | + | Diffuse | Moderate | 6.354 | + | PR in death |
| 6 | M/23 | T-LBL | 60 | + | + | Diffuse | Mild | 3.72 | + | CR (16 mo+) |
| 7 | M/29 | T-LBL | 90 | + | + | Diffuse | Intense | 8.11 | + | CR (7 mo+) |
| 8 | M/30 | T-LBL | 70 | + | + | Diffuse | Mild | 4.58 | + | Early death |
| 9 | M/15 | T-LBL | 30 | + | + | Diffuse | Mild | 4.2 | + | CR (7 mo+) |
All lymphoma involvement lesions were FDG-avid and
the intensity of nodal FDG uptake was variable (mild in 4,
moderated in 1 and intense in 4 patient). The mean SUVmax was
6.4±3.3 (range, 3.7–12.2). As shown in Table I and Fig.
1, 8 out of 9 patients presented with hypermetabolic lesions in
the mediastinum and intense splenic uptake was noted in 4 patients.
A high Ki-67 index was associated with relatively intense and
increased SUVmax values. All the images of the enrolled patients
are presented in Fig. 1.
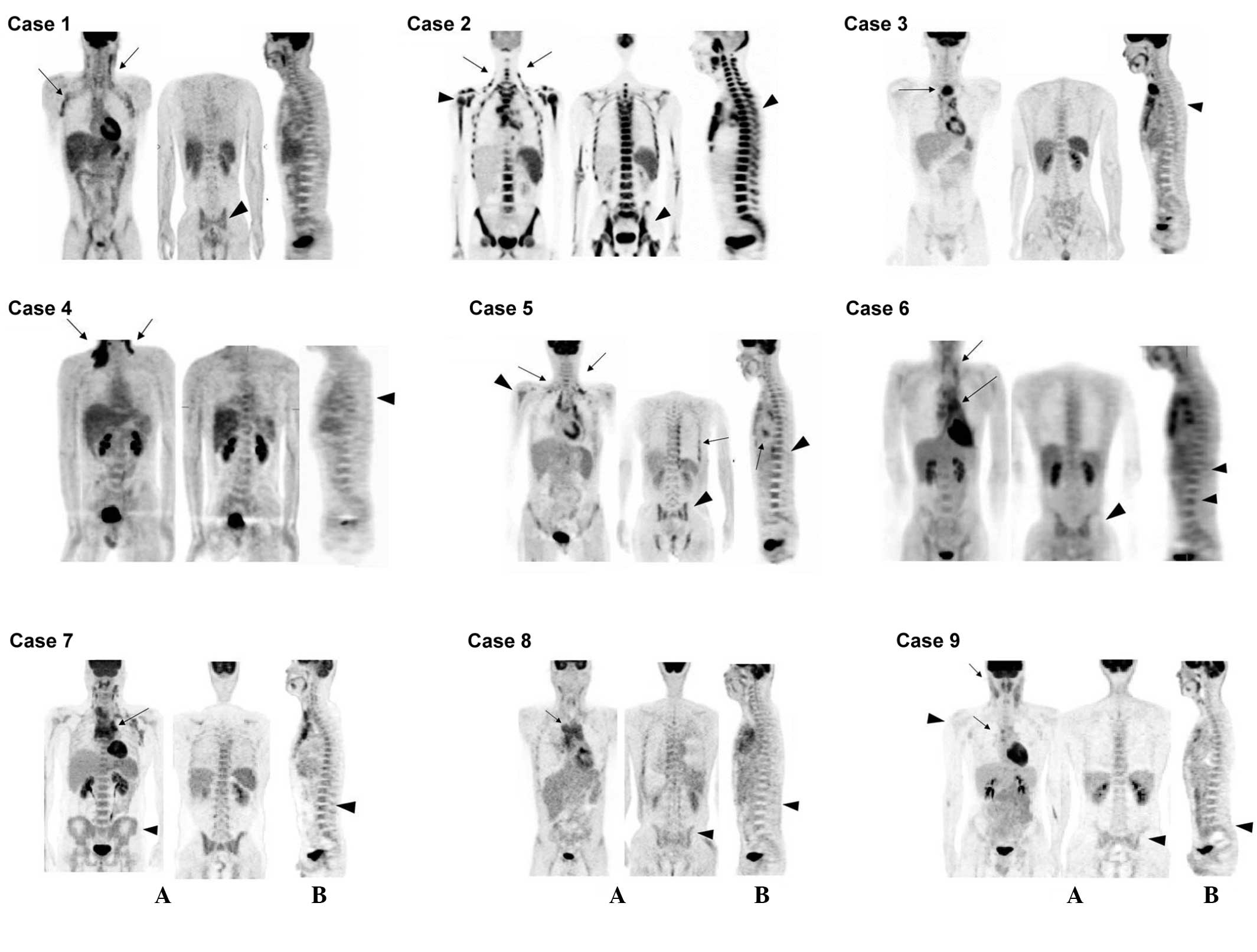
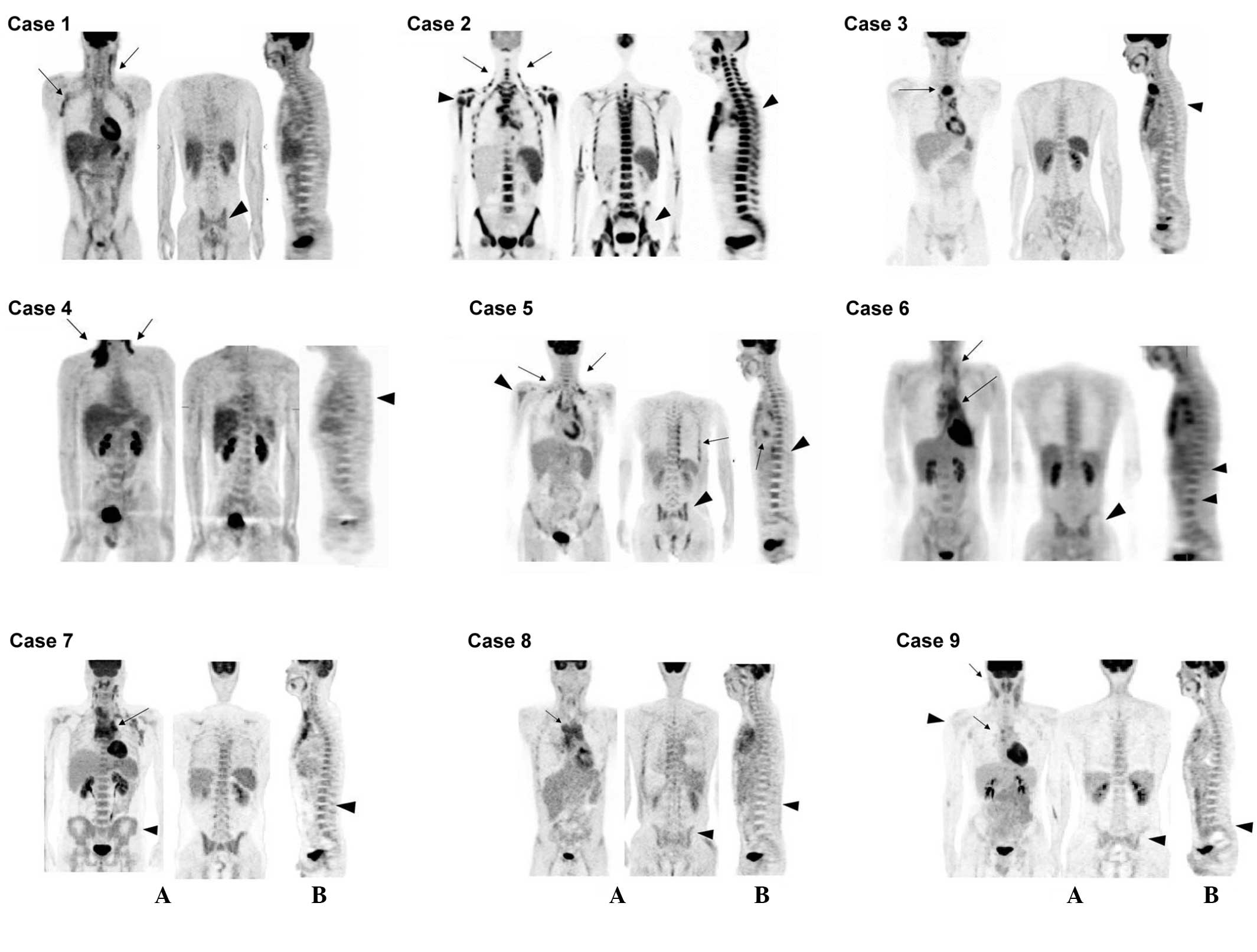 | Figure 1.Fluorine-18 fluorodeoxyglucose
positron emission tomography, (A) coronal and (B) sagittal images.
Case 1: Confluent nodal activity is present in the bilateral neck
and axilla (arrows), with diffuse and non-uniform BM activity
(arrowhead). Case 2: Diffuse, hyperintense BM activity consistent
with BM involvement. Activity is so extensive it is nearly
confluent in areas (arrowhead). The bilateral jugular chains of the
neck are shown (arrows). Case 3: Intense activity within the
mediastinal mass (arrow). BM activity shows localized uptake
(arrowhead). Case 4: Hyperintense activity within the neck and
supraclavicular regions (arrows), with nodular BM activity at the
level of the mid-T spines (arrowhead). Case 5: Nodal activities in
the supraclavicular region, left axilla, mediastinum, bilateral
pleura and pericardium (arrows), with diffuse and non-uniform BM
activity (arrowhead). Case 6: Supraclavicular (arrow) and
mediastinal leukemic transformation (arrows). BM shows
heterogeneous hyperactivity, mainly in the thoraco-lumbar spine and
hip (arrowhead). Case 7: Heterogneous nodal activity in the
mediastinum (arrow) and supraclavicular area, with diffuse and
non-uniform BM activity (arrowhead). Case 8: Triangular-shaped
prevascular mediastinal activity (arrow) and diffuse BM
hyperactivity (arrowhead). Case 9: Mild to moderate degree of
hyperactivity in the neck, aortopulmonary window and subcarinal
region (arrow). BM shows diffuse hyperactivity (arrowhead). BM,
bone marrow. |
Discussion
The present study found two notable points in the
FDG-PET imaging. First, all T-LBL patients with involvement of the
BM showed diffuse or nodular BM FDG uptake. However, patients with
no bone involvement showed localized marrow uptake (case 3;
Fig. 1;). Second, with regard to LT,
the LT patients presented with diffuse BM FDG uptake (mean SUVmax,
3.7±2.9), while the single patient with marrow involvement without
LT showed nodular FDG uptake in the BM (SUVmax, 2.7) (case 4;
Fig. 1). In the present study, all
lymphomas involving lymph nodes and mediastinal lesions were
FDG-avid. These results were concordant with previous studies
(4,5).
In addition, the present study provides a more detailed FDG uptake
pattern with BM involvement and LT status. In conclusion, it is
possible to use FDG-PET for the evaluation of the disease extent of
T-LBL. Furthermore, it could provide a diagnostic clue for BM
involvement or LT in T-LBL patients.
References
|
1
|
Hoelzer D, Gökbuget N, Digel W, Faak T,
Kneba M, Reutzel R, Romejko-Jarosinska J, Zwolinski J and Walewski
J: Outcome of adult patients with T-lymphoblastic lymphoma treated
according to protocols for acute lymphoblastic leukemia. Blood.
99:4379–4385. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ellin F, Jerkeman M, Hagberg H and
Relander T: Treatment outcome in T-cell lymphoblastic lymphoma in
adults - a population-based study from the Swedish Lymphoma
Registry. Acta Oncol. 53:927–934. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Seam P, Juweid ME and Cheson BD: The role
of FDG PET scans in patients with lymphoma. Blood. 110:3507–3516.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Weiler-Sagie M, Bushelev O, Epelbaum R,
Dann EJ, Haim N, Avivi I, Ben-Barak A, Ben-Arie Y, Bar-Shalom R and
Israel O: (18)F-FDG Avidity in lymphoma readdressed: A study of 766
patients. J Nucl Med. 51:25–30. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Xiang X, Wang X, Yi Q, Lin L, Zhang X,
Liang H and Yang J: Precursor T-cell lymphoblastic lymphoma
extensively involving the mediastinum, pleura and pericardium: A
case report. Mol Clin Oncol. 2:945–948. 2014.PubMed/NCBI
|