Introduction
Leiomyomas are benign, soft tissue tumors that
originate from smooth muscle and account for ~3.8% of all benign
soft tissue tumors (1). The most
common gynecological leiomyoma is uterine leiomyoma. The exact
causes underlying the development of these lesions are not known.
Uterine leiomyomas are speculated to be hormonally responsive
neoplasms, and it has been suggested that estrogen and progesterone
may stimulate susceptible uterine fibromuscular elements. The
expression of progesterone receptor (PR) and estrogen receptor (ER)
is significantly increased in the tissues of uterine leiomyoma
(2). Vulval leiomyomas primarily
develop in premenopausal women and usually occur in the clitoris,
and labia majora and minora (3). As
for premenopausal perineal leiomyoma, only 3 cases have been
reported in the literature (Table I).
To the best of our knowledge, there are currently no cases
describing the presence of perineal leiomyomas in postmenopausal
woman.
 | Table I.Summary of perineal leiomyoma cases in
the literature. |
Table I.
Summary of perineal leiomyoma cases in
the literature.
| Author, year | Age, years | Mass and
symptoms | Menopausal | Pathology | Prognosis | Refs. |
|---|
| Roy et al,
1998 | 47 | Palpable soft, cystic
masses in the vulva and perineum with no pain | No | Negative for
malignant cells | No recurrence in 2
years | (14) |
| Koc et al,
2010 | 47 | Palpable solid,
cystic mass with a painless perineal swelling | No | N/A | No recurrence in 1
year | (15) |
| Oliveira Brito et
al, 2011 | 36 | Palpable soft, cystic
mass with perineal tenderness and local pain | No | Benign mesenchymal
tumor | No recurrence | (1) |
The present case describes a postmenopausal woman
who presented with tenderness, lumbosacral radiating pain and a
perineal mass, which was eventually diagnosed as a
hormone-independent perineal leiomyoma. The discussion of the case
is followed by a brief review of the available literature.
Case report
A 60-year-old Chinese female (gravida 4, para 4) was
admitted to the Department of Gynecology, First Affiliated
Hospital, Xi'an Jiaotong University (Xi'an, China) in May 2014
after experiencing perineal tenderness for the last year, in
addition to lumbosacral radiating pain, which occurred 6 months
previously. The patient had a history of surgical sterilization and
went through the menopause 12 years previously. The patient had no
history of hormone replacement treatment. During physical
examination, palpation identified a movable, tender, hard mass
(~1×1×1 cm) that extended from the rear of the left labia majora to
the frenulum of the labia minora near the anus. Doppler
ultrasonography of the uterus and uterine adnexa was considered
satisfactory for the patient's age. It was decided that local mass
resection would be performed. During surgery, a solid and
well-demarcated mass was removed without invasion of the
surrounding tissues. Histopathological analysis confirmed the
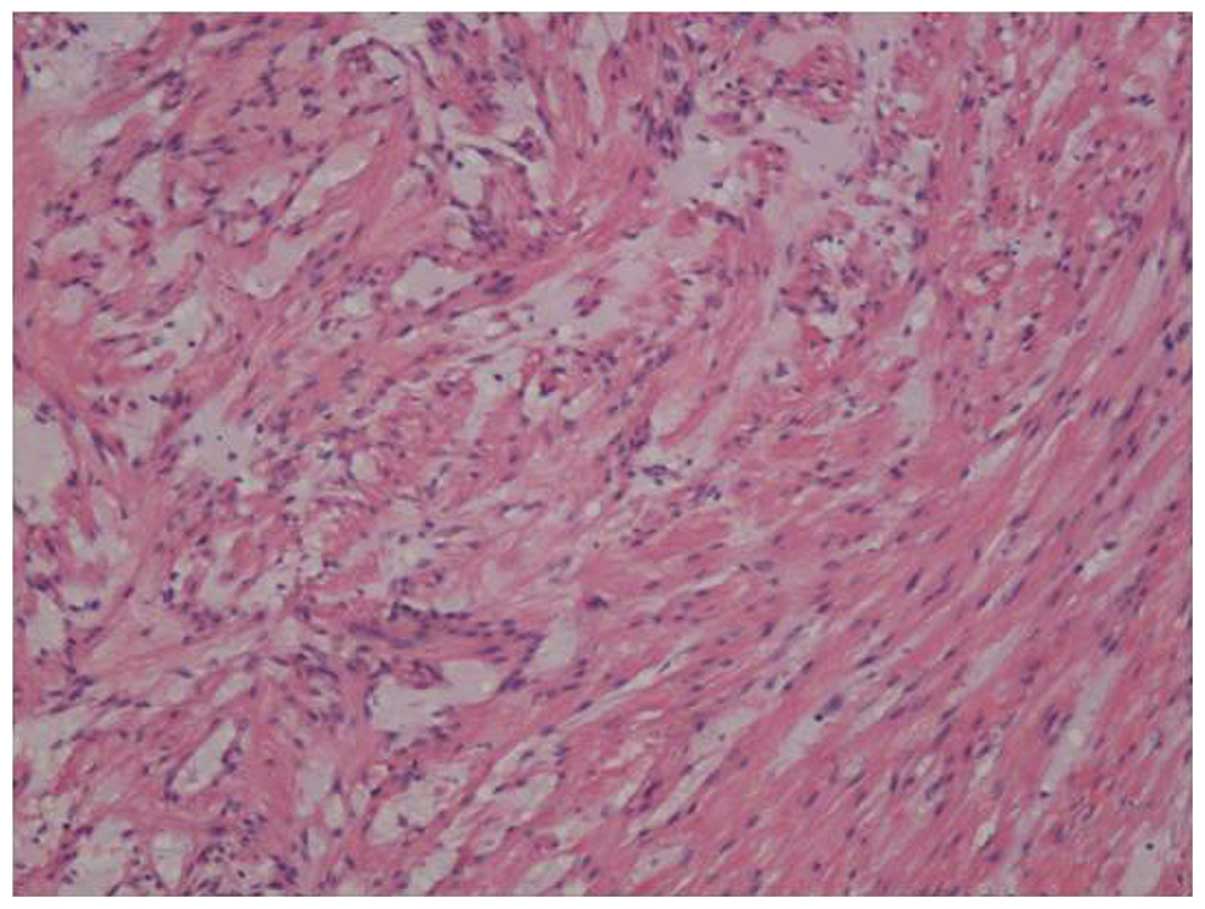
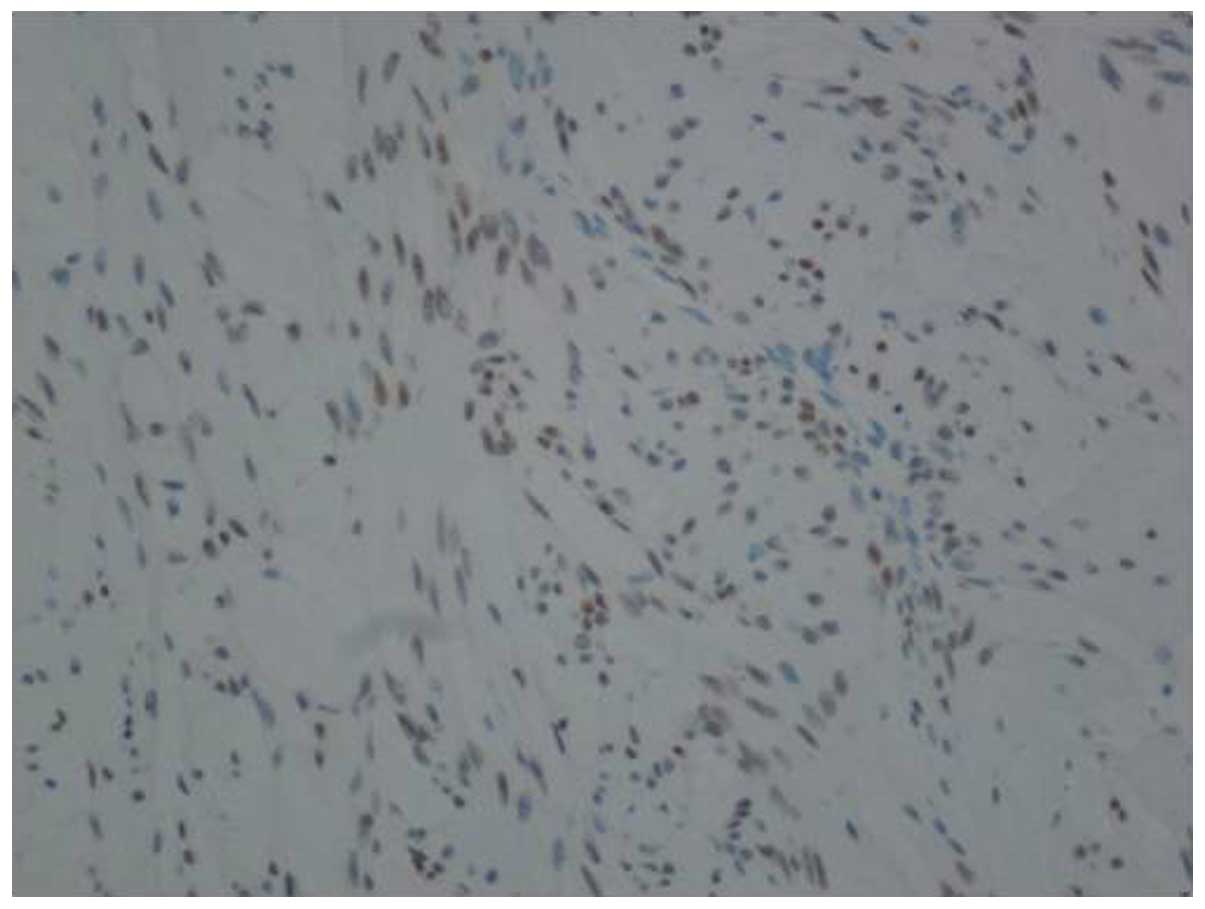
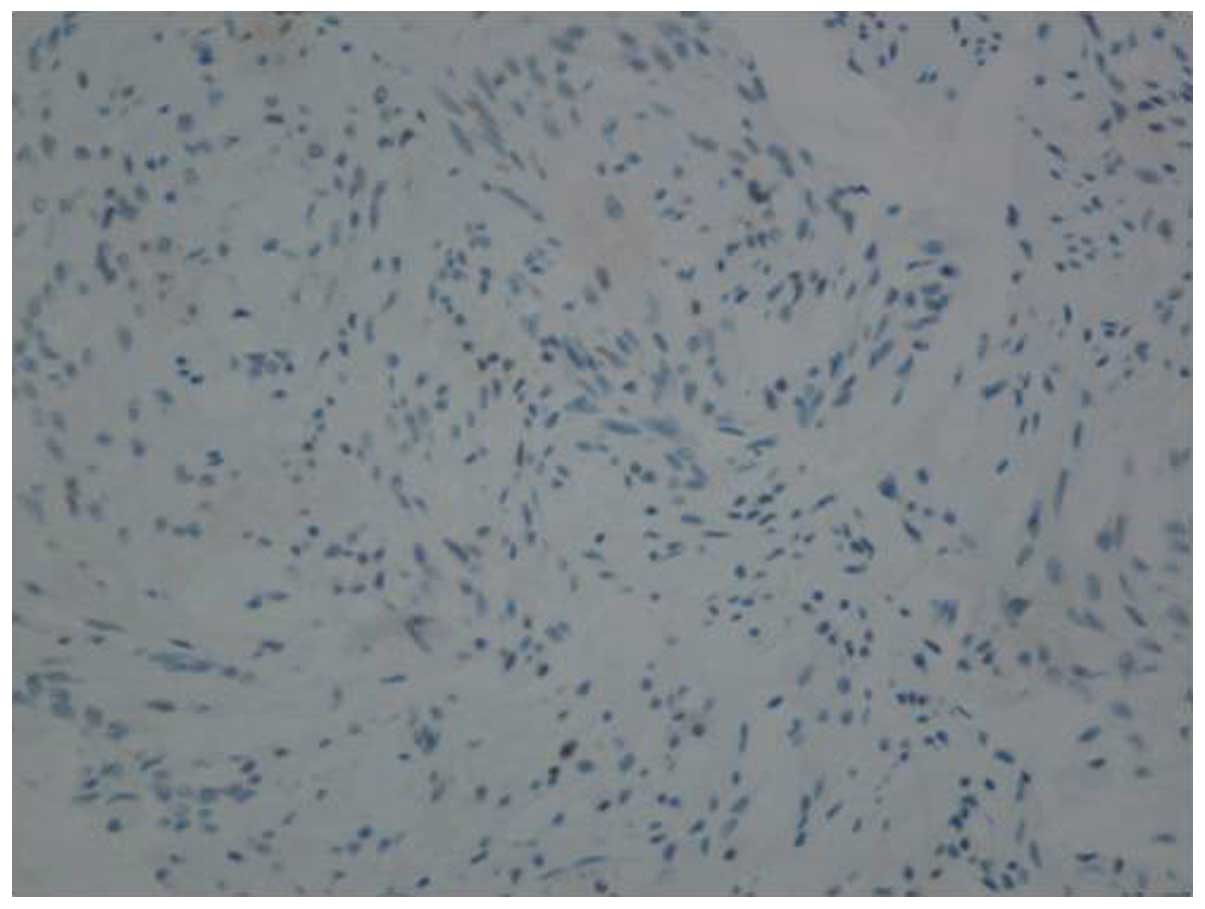
presence of a benign perineal leiomyoma (Fig. 1). Immunohistochemical staining with
antibodies against ER and PR identified that the lesion was
positive for ER expression (+2, 40%) (Fig. 2) and negative for PR (Fig. 3). The patient was followed up for 1
year with no recurrence, pain or fecal incontinence.
Discussion
Leiomyomas, which are typically hormone sensitive,
develop most commonly in females during their reproductive years
and often regress following menopause (4). Only 1 case of vulval leiomyoma has been
reported in a postmenopausal women by Celik et al (4), and 3 cases of perineal leiomyoma in
premenopausal women have been reported (Table I). The 3 patients were all
menstruating and <50 years old. To the best of our knowledge, no
studies describing the continued growth of perineal leiomyomas in
the postmenopausal period without hormone replacement therapy were
reported in the literature.
The specific etiology of leiomyoma remains unknown.
For uterine leiomyomas, the expression of PR and ER is usually
positive, and estrogen- and progesterone-induced tumor growth is
accepted as the likely cause (5). The
expression of PR in leiomyomas is significantly higher than that of
ER, regardless of menstrual cycle phase (6). In the present case, the patient was
postmenopausal, and although ER expression was positive, the role
of estrogen cannot be over emphasized as estrogen levels are
significantly lower in postmenopausal women compared with
premenopausal women (7). It has been
reported that other possible factors underlying the development of
these lesions may include stress, infection, and environmental and
dietary factors (8). Infection may
result in oncogenesis due to subsequent injury and/or inflammation
resulting in cell proliferation, increased extracellular matrix and
reduced apoptosis, apropos of abnormal tissue repair (9,10). A
number of molecular researchers presented a model depicting myoma
development based on an abnormal response to tissue repair,
resulting in formation of an altered extracellular matrix and
disordered healing (9).
Nielsen et al (11) studied 25 cases of vulval leiomyoma and
observed that the primary symptom is a painless mass, with less
common symptoms including pain, itching and erythema. Two of the
masses described in Table I are soft
and cystic, while the other is solid. One case presented with
perineal tenderness and local pain following a right-sided
mediolateral episiotomy, which occurred 1 year previously (1). However, in the current case, the patient
presented with a painful and solid mass associated with lumbosacral
radiating pain, the combination of which, to the best of our
knowledge, has not yet been reported in any extensive review of the
literature. The authors propose that the pain experienced by the
current patient may be due to the lesion stimulating peripheral
nerves. However, unanswered questions remain regarding the factors
that induce leiomyoma development in postmenopausal women.
Leiomyomas of the vulva typically present with three
different histological patterns: i) Spindled; ii) epithelioid; and
iii) myxohyaline, which may be mixed or pure (12). The myxohyaline pattern is commonly
associated with the epithelioid pattern, and a combination of
spindle and epithelioid cells is often observed (11). The tumor in the present case was a
benign, epithelioid perineal leiomyoma and did not exhibit any
myxoid changes. Recurrence is extremely rare (13) and close follow-up is seldom
required.
In conclusion, leiomyomas of the perineal occur most
commonly in the fourth and fifth decades of life (11). The most common principle action of
perineal leiomyoma is a painless mass (4,14,15). Before a preoperative diagnosis,
endoscopic ultrasound and MRI are suggested to be taken to aid
differential diagnosis from Bartholin cysts, aggressive
angiomyxoma. Perineal leiomyomas, exhibit three principal
histological patterns-spindled, epithelioid and myxoid (12). Spindled is the most common. The
excision of perineal leiomyomas is the most useful surgical option
to cure leiomyomas completely (4,11,16,17).
Though the recurrence is uncommon, a short-time follow-up is still
suggested.
Acknowledgements
The authors would like to thank Mrs. Hui-ting Liu
from the First Affiliated Hospital, Xi'an Jiaotong University
(Xi'an, China), for grammatically revising the original
manuscript.
References
|
1
|
Oliveira Brito LG, Falcão Motoki L,
Magnani PS, Sabino-de-Freitas MM, et al: Giant perineal leiomyoma
incidentally manifested at a recent episiotomy site: Case report. J
Minim Invasive Gynecol. 18:267–269. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Massart F, Becherini L, Marini F, Noci I,
Piciocchi L, Del Monte F, Masi L, Falchetti A, Tanini A, Scarselli
G and Brandi L: Analysis of estrogen receptor (ERalpha and ERbeta)
and progesterone receptor (PR) polymorphisms in uterine leiomyomas.
Med Sci Monit. 9:BR25–BR30. 2003.PubMed/NCBI
|
|
3
|
Pandey D, Shetty J, Saxena A and Srilatha
PS: Leiomyoma in vulva: A diagnostic dilemma. Case Rep Obstet
Gynecol. 2014:3864322014.PubMed/NCBI
|
|
4
|
Celik H, Bildircin FD, Kefeli M, Yavuz E
and Kokcu A: Labial leiomyoma growing gradually in the vulva of an
elderly woman. J Obstet Gynaecol. 32:8162012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Reyad MM, Gazvani MR and Khine MM: A rare
case of primary leiomyoma of the vulva. J Obstet Gynaecol.
26:73–74. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zasławski R, Surowiak P, Dziegiel P,
Pretnik L and Zabel M: Analysis of the expression of estrogen and
progesteron receptors, and of PCNA and Ki67 proliferation antigens,
in uterine myomata cells in relation to the phase of the menstrual
cycle. Med Sci Monit. 7:908–913. 2001.PubMed/NCBI
|
|
7
|
Unfer TC, Figueiredo CG, Zanchi MM, Maurer
LH, Kemerich DM, Duarte MM, et al: Estrogen plus progestin increase
superoxide dismutase and total antioxidant capacity in
postmenopausal women. Climacteric. 18:379–388. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Khan AT, Shehmar M and Gupta JK: Uterine
fibroids: Current perspectives. Int J Womens Health. 6:95–114.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Leppert PC, Catherino WH and Segars JH: A
new hypothesis about the origin of uterine fibroids based on gene
expression profiling with microarrays. Am J Obstet Gynecol.
195:415–420. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rogers R, Norian J, Malik M, Christman G,
Abu-Asab M, Chen F, Korecki C, Iatridis J, Catherino WH, Tuan RS,
et al: Mechanical homeostasis is altered in uterine leiomyoma. Am J
Obstet Gynecol. 198:474.e1–e11. 2008. View Article : Google Scholar
|
|
11
|
Nielsen GP, Rosenberg AE, Koerner FC,
Young RH and Scully RE: Smooth-muscle tumors of the vulva. A
clinicopathological study of 25 cases and review of the literature.
Am J Surg Pathol. 20:779–793. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nucci MR and Fletcher CD: Vulvovaginal
soft tissue tumours: Update and review. Histopathology. 36:97–108.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Goyal LD, Kaur H, Kaur K and Kaur S: An
unusual case of vaginal myoma presenting with postmenopausal
bleeding. J Family Reprod Health. 7:103–104. 2013.PubMed/NCBI
|
|
14
|
Roy KK, Mittal S and Kriplani A: A rare
case of vulval and perineal leiomyoma. Acta Obstet Gynecol Scand.
77:356–357. 1998.PubMed/NCBI
|
|
15
|
Koc O, Sengul N and Gurel S: Perineal
leiomyoma mimicking complex Bartholin mass. Int Urogynecol J.
21:495–497. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Newman PL and Fletcher CD: Smooth muscle
tumours of the external genitalia: clinicopathological analysis of
a series. Histopathology. 18:523–529. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ngo Q and Haertsch P: Vulvar leiomyoma in
association with gastrointestinal leiomyoma. Aust N Z J Obstet
Gynaecol. 51:468–469. 2011. View Article : Google Scholar : PubMed/NCBI
|