Introduction
Colorectal cancer (CRC) is the fifth leading cause
of cancer-associated mortality in China (1). Surgery is the first-line treatment for
patients with early-stage and localized tumors, but certain
patients with recurrent or metastatic disease are inoperable when
they arrive at the hospital. Chemotherapy and radiotherapy could be
adopted for such patients, yet the adverse effects can be
unbearable and the 5-year survival rate remains low (2). Therefore, novel treatment approaches
with acceptable toxicity levels are required to improve the
therapeutic efficacy and survival rate of inoperable patients.
Since the 1990s, certain novel achievements towards
improving the prognosis of patients with advanced CRC were
established, including an immunotherapy strategy based on
antigen-targeted therapy via monoclonal antibodies (mAbs). mAbs,
including panitumumab, bevacizumab and cetuximab, have been
recently approved by the Food and Drug Administration for
first-line treatment of advanced CRC (3). In addition, the adoptive transfer of
natural killer (NK) cells is also an emerging method to eliminate
the metastasis of CRC (4,5).
Cetuximab, a human-mouse chimerized anti-epidermal
growth factor receptor (EGFR) immunglobulin G1 (IgG1) monoclonal
antibody, has been previously used to specifically combine with
EGFR on the cell surface and intercept downstream signal
conduction; as a result, tumor cell proliferation, invasion,
metastasis, angiogenesis were inhibited and tumor cell apoptosis
were promoted (6–8). In addition, cetuximab may target tumor
cells by antibody dependent cell mediated cytotoxicity (ADCC)
activity (9). However, data
accumulated from clinical studies indicate that metastatic CRC
showed limited responses to cetuximab, when used as a monotherapy
(10).
The use of NK cells, the most powerful type of
innate immune cell, is another immunotherapy option for patients
with advanced CRC. NK cells were previously demonstrated to
directly kill human tumor cells that had been freshly isolated from
gastric, renal cell and colon carcinomas (11). The cytotoxicity of NK cells is
regulated by a series of activating or inhibiting signals, which
may improve the sensitivity of NK cells to affecting tumor cells
(9,12,13).
Activated NK cells can kill tumor cells directly through the
release of intracellular toxic substances, including perforin and
granzyme (14). Furthermore, NK cells
produce cytokines, such as interferon-γ (IFN-γ), tumor necrosis
factor-α and interleukin-2 (IL-2), to enhance the antitumor effects
and mediate tumor cell apoptosis via the FasL/Fas apoptosis pathway
(15,16). NK cells can also induce ADCC activity
in order to lyse tumor cells (14).
Although the results of NK cell therapy have been promising in
vitro, adoptive NK cell therapy in vivo possesses
certain limitations, including the immunosuppressive environment of
CRC or a lack of specificity (17).
ADCC activity is regulated by a complex balance of
activating and inhibiting signals, including membrane coreceptors
and serum proteins, such as cytokines, chemokines and hormones
(18). NK cells only express
activated cluster of differentiation (CD)16a (also called Fc
fragment of IgG receptor IIIa), and are widely accepted as the key
immune cells to mediate ADCC antitumor activity (19). The Fc receptor of NK cells can
identify the constant region of tumor-bound antibodies, which
allows NK cells to kill antibody-coated target cells via ADCC
activity specifically (20). Siokawa
et al (15) confirmed that
rituximab could significantly enhance the ADCC activity and improve
the killing effects of NK cells towards leukemia xenograft cells in
immune deficient NOG mice. Elotuzumab, a monoclonal antibody, was
shown to enhance NK cell-mediated ADCC activity in SLAM family
member 7-expressing myeloma cells (21). Roda et al (22) found that after combining with
cetuximab, NK cells would enhance IFN-γ secretion by 3–10 times.
These studies demonstrate that the combination of NK cell therapy
with antibody-based immunotherapy may be an effective way to
enhance the antitumor activity towards CRC.
In a previous study, the ADCC activity of NK cells
was demonstrated to be important in cetuximab-induced cytotoxicity
in EGFR-positive colon cancer cells in vitro (23). In addition, Yang et al
(24) suggested that cetuximab could
mediate ADCC activity through NK cells in vivo. However, the
ADCC activity of adoptive NK cells, induced by cetuximab in a nude
mouse CRC xenograft model, has not been previously reported. In the
present study, healthy human NK cells were regarded as effector
cells, and the ADCC activity or antitumor effects of cetuximab
combined with adoptive NK cells were observed in CRC xenograft
models with varying degrees of EGFR expression. The present study
was conducted in order to explore a potential immunotherapy for
advanced CRC, based on the combination of cetuximab and adoptive NK
cells.
Materials and methods
Animals and cell lines
In total, 60 BALB/c nude mice (female; weight, 17–18
g; age, 4–5 weeks) were purchased from the Shanghai Laboratory
Animal Center Laboratory Animal Co., Ltd. [Shanghai, China; animal
quality certificate code, SCXK (Shanghai) 2007-000528569]. All mice
were bred in specific pathogen-free (SPF) conditions at the Fujian
Medical University [Fuzhou, China; environmental license, SYXK
(Fujian) 2008-0001], and were housed at constant temperature
(24±2°C) and 60% relative humidity, with a 10:14 h light-dark
cycle. Mice had ad libitum access to food and autoclaved
water. All the animal procedures were approved by the Animal Ethics
Committee of Fujian Medical University (Fuzhou, China). LOVO and
SW620 cell lines were obtained from the Cell Bank of Type Culture
Collection of Chinese Academy of Sciences (Shanghai, China).
Antibodies and reagents
Cetuximab was purchased from Merck Millipore
(Darmstadt, Germany). The antibodies used in the present study were
mouse anti-human CD3-fluorescein isothiocyanate (FITC; monoclonal;
1:100; cat. no. 55539; BD Biosciences, Franklin Lakes, NJ, USA),
mouse anti-human CD56-phycoerythrin (PE) (monoclonal; 1:100; cat.
no. 555516; BD Biosciences); human immunoglobulin G (hIgG;
polyclonal; 1:200; cat. no. bs-0297P; Beijing Biosynthesis
Biotechnology Co., Ltd., Beijing, China), rabbit anti-human EGFR
(polyclonal; 1:200; cat. no. Sc-03AC; Santa Cruz Biotechnology,
Inc.) rabbit anti-human Ki-67 (monoclonal; 1:200; cat. no ZA-0502;
OriGene Technologies, Inc., Beijing, China). The PV-9000 polymer
detection system for immunohistological staining, apoptosis
detection kits in situ and diaminobenzidine color reagent
were purchased from OriGene Technologies, Inc. The WST-1 cell
proliferation reagent was purchased from Roche Diagnostics (Basel,
Switzerland). RPMI-1640 and 0.25% ethylenediaminetetraacetic acid
pancreatin were purchased from Takara Bio, Inc. (Otsu, Japan), and
Ficoll-paque lymphocyte separation medium was purchased from GE
Healthcare Life Sciences (Chalfont, UK). Recombinant IL-2 was
purchased from Beijing Four Rings Biopharmaceutical Co., Ltd.
(Beijing, China). Cells were analyzed by Moflow XDP flow cytometry
with Summit version 5.2 software (Beckman Coulter, Inc., Brea, CA,
USA).
Cancer cells culture
Human CRC SW620 and LOVO cells were cultured in
RPMI-1640 medium containing 10% fetal bovine serum (FBS; Gibco;
Thermo Fisher Scientific, Inc., Waltham, MA, USA) in an incubator
at 37°C with 5% CO2.
NK cell isolation and cultivation
A 40 ml sample of peripheral blood was obtained from
five healthy human donors between April and August 2013, which was
approved by the Ethics Committee of Fujian Provincal Cancer
Hospital (Fuzhou, China) and written informed consent was obtained.
Peripheral blood mononuclear cells (PBMCs) were isolated using
Ficoll-paque lymphocyte separation medium and then washed twice
with phosphate-buffered saline (PBS). The PBMCs were resuspended in
100 µl PBS, stained with 10 ul CD3-FITC and 10 ul CD56-PE
monoclonal antibodies and then incubated at 4°C for 30 min in
darkness. The cells were then washed twice using PBS, prior to
being evaluated by the MoflowXDP flow cytometry and sorted into
CD3−CD56+ NK cells. The NK cells were
cultured in RPMI-1640 medium containing 20% fetal bovine serum,
recombinant IL-2 (1,000 units (U)/ml), streptomycin (100 µg/ml) and
penicillin (100 U/ml) for 10 days.
ADCC activity assay of NK cells in
vitro
After 14 days of culture, NK cells were analyzed and
collected. A small portion of NK cells (~106 cells) were
analyzed by Moflow XDP flow cytometry, while the remaining NK cells
were washed twice with PBS and resuspended at a density of
4×104 cells/ml in RPMI-1640 medium containing 10% FBS.
LOVO and SW620 cells (104 cells) were seeded in a
96-well plate for 24 h and then cocultured with NK cells for 48 h
at effector-to-target ratios of 40:1, 20:1, 10:1 and 5:1. Following
coculture, the cells were marked by incubating with WST-1 for 4 h
at 37°C in 5% CO2. The lysis of cells was measured by
examining optical density (OD) at 450 nm, and the ADCC activity of
NK cells was calculated using the following formula: Killing effect
(%) = [1 - (OD value of experimental group - OD value of effect
cells)/OD of target cells] × 100.
Establishment of nude mouse xenograft
model
After one week of breeding in the SPF conditions,
logarithmic phase LOVO or SW620 cells (5×106 cells) were
subcutaneously injected into the mice via the left axillary (LOVO
group, n=30; SW620 group, n=30). Tumorigenicity was observed, by
assessing the tumor volume over time.
Experimental groups and
intervention
When the volume of the tumors had reached ~200
mm3 (7–8 mm in diameter), the 30 mice were divided into
6 groups and received the following interventions: i)
Intraperitoneal injection of 0.2 ml PBS; ii) intraperitoneal
injection of cetuximab (1 mg/kg); iii) intraperitoneal injection of
hIgG (1 mg/kg); iv) intravenous injection of NK cells
(2×106 cells) through the caudal vein; v)
intraperitoneal injection of hIgG (1 mg/kg) and intravenous
injection of NK cells (2×106); or vi) intraperitoneal
injection of cetuximab (1 mg/kg) and intravenous injection of NK
cells (2×106). These interventions were executed 3 times
per week, for 4 weeks.
Nude mouse xenograft tumor assay
To observe the tumor growth in the mice, tumor
diameter was measured 2 times per week using vernier calipers, and
tumor volume was calculated with the formula: Volume = 0.5 × long
diameter × (short diameter)2. Subsequent to data
collection, a tumor growth curve was drawn. All the mice sacrificed
by CO2 inhalation 3 days following the end of treatment
and tumors were resected and weighed. The antitumor rate was
evaluated with the formula: Antitumor rate (%) = (average tumor
weight of control group - average tumor weight of experimental
group)/average tumor weight of control group × 100. Pathological
changes to the tumor tissues were observed by immunohistochemistry
(IHC) and terminal deoxynucleotidyl transferase dUTP nick end
labeling (TUNEL). IHC was used to detect the expression of EGFR and
Ki-67, whereas xenograft cell apoptosis was analysed by TUNEL.
Human CRC specimens obtained from CRC patients who provided written
informed consent at Fujian Provincal Cancer Hospital (Fuzhou,
China) in September 2013 were used as positive controls, while PBS
was used as a negative control. The expression level of EGFR or
Ki-67 was assessed by randomly selecting 5 non-overlap ping fields
of view in an optical microscope, and counting 100 tumor cells per
field. The percentage of positive cells or apoptosis cells was
regarded as the labeling index (LI) or apoptosis index (AI),
respectively. An expression score of 0–10% was regarded as negative
(−), 10–25% as weak positive (+), 26–50% as positive (++) and
50–100% as strong positive (+++).
Statistical analysis
SPSS 19.0 (IBM SPSS, Armonk, NY, USA) was used for
the analysis of all statistics. Data were presented as the mean ±
standard error of the mean. One-way analysis of variance was used
to determine the differences between multiple groups. Various
groups were compared using the Bonferroni test. P<0.05 was
considered to indicate a statistically significant difference.
Results
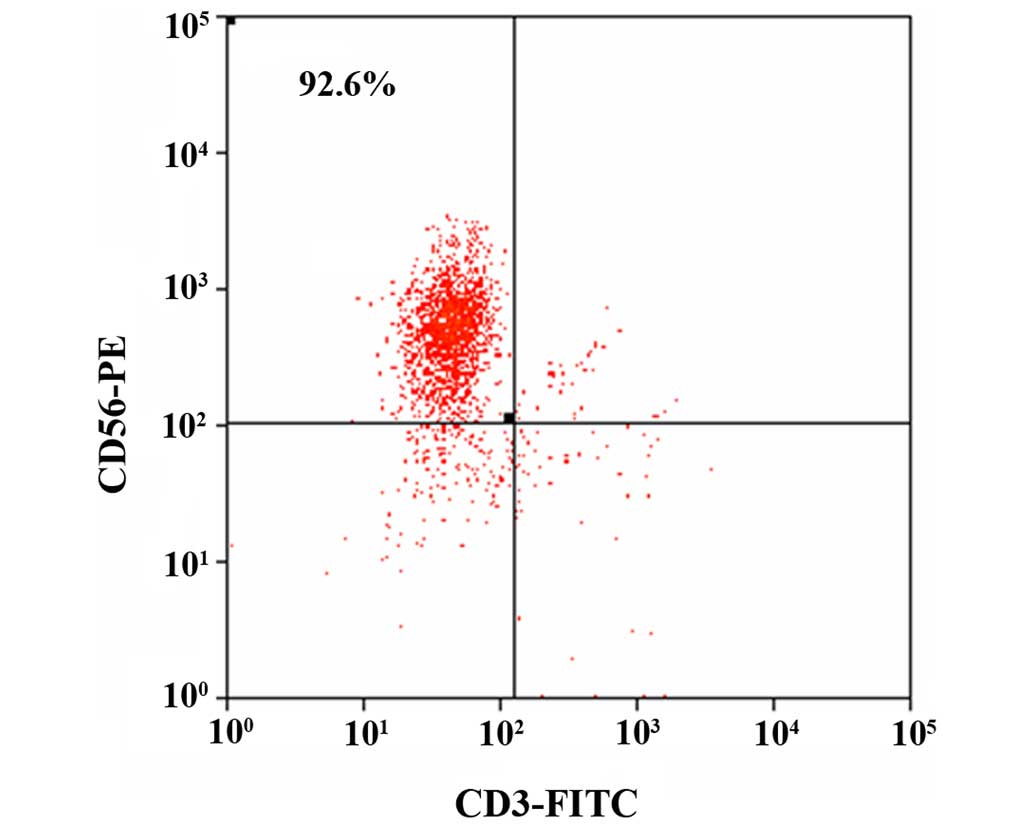
Purity of NK cells
After 14 days of culture, the percentage of NK cells
(CD3−CD56+) cells was 92.60±3.83% (Fig. 1), which met the requirements for the
following experiments.
ADCC activity of NK cells in
vitro
The inhibition rate of CRC cells is shown on
Table I. NK cells had a marked
inhibitory effect towards the LOVO and SW620 cells, and the
inhibitory rate was positively associated with the
effector-to-target ratios (r=0.994, P=0.006; r=0.972, P=0.028). In
addition, the inhibitory rate was greater in the LOVO cells
compared with the SW620 cells (P=0.003).
 | Table I.Antibody dependent cell mediated
cytotoxicity activity of natural killer cells towards LOVO and
SW620 cells in vitro, expressed as the inhibition rate of
LOVO or SW620 cells (%). |
Table I.
Antibody dependent cell mediated
cytotoxicity activity of natural killer cells towards LOVO and
SW620 cells in vitro, expressed as the inhibition rate of
LOVO or SW620 cells (%).
|
| Effector-target
ratios |
|---|
|
|
|
|---|
| Cell line | 40:1 | 20:1 | 10:1 | 5:1 |
|---|
| LOVO | 52.14±1.45 | 29.91±1.03 | 19.62±0.78 | 8.80±1.38 |
| SW620 | 20.34±0.88 | 14.05±1.10 |
5.02±0.75 | 3.07±0.45 |
Mouse weight and xenograft tumor
volume prior to treatment
After 5 days of subcutaneous implantation, the
xenograft tumors grew well in the nude mice, and the tumor size
grew to ~200 mm3 after 14 days. For each group of mice,
the weight and xenograft tumor volume was analyzed prior to
treatment, and no statistically significant difference was shown
(P=0.132 and P=0.880, respectively).
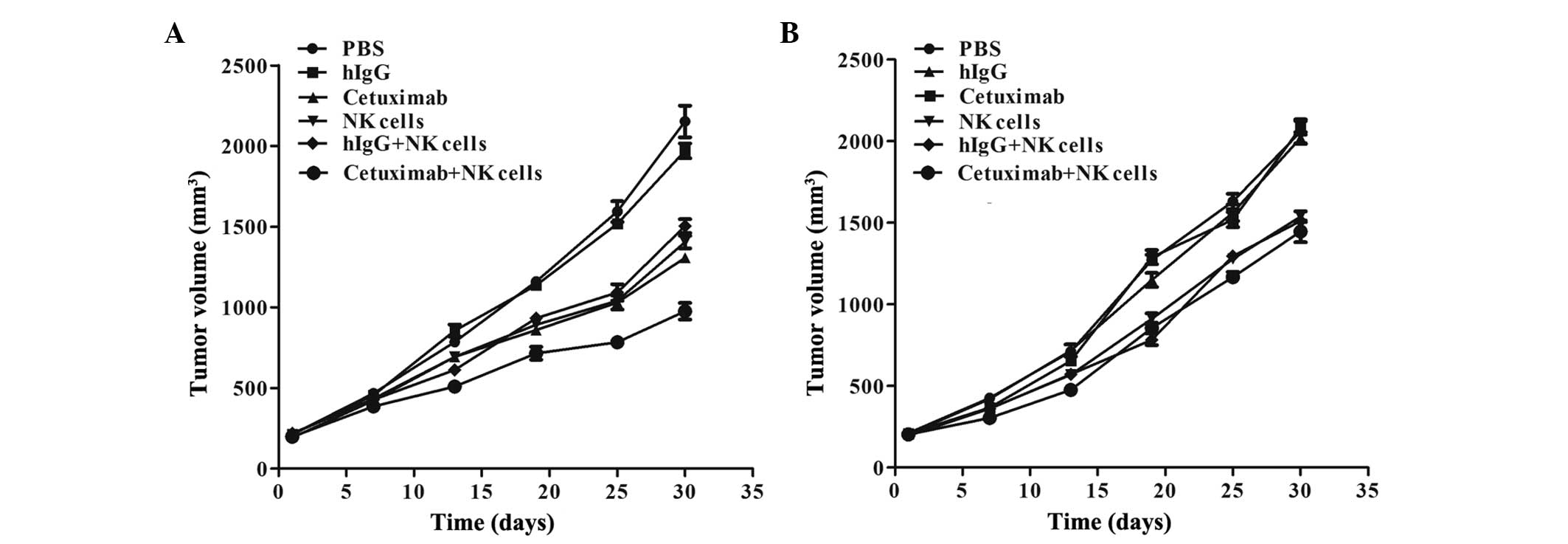
Xenograft tumor growth curve
The tumor growth curve showed that the LOVO
xenograft underwent a growth restriction following the injection of
cetuximab plus NK cells, and the average tumor volume was evidently
decreased compared with other groups (P<0.0001 compared with the
PBS group, P<0.0001 compared with the hIgG group, P=0.004
compared with the cetuximab group, P=0.02 compared with the NK
cells group and P=0.01 compared with the hIgG plus NK cells group).
Furthermore, the tumor growth was also inhibited in the cetuximab
only, NK cells only and NK cells plus hIgG groups, with similar
inhibitory effects in each (P=0.113). The tumor volume was
inhibited, but no statistically significantly difference was found,
among the cetuximab plus NK cells, NK cells and NK cells plus hIgG
groups of the SW620 xenograft models (P=0.374), and tumor growth
was not inhibited in the cetuximab group (Fig. 2).
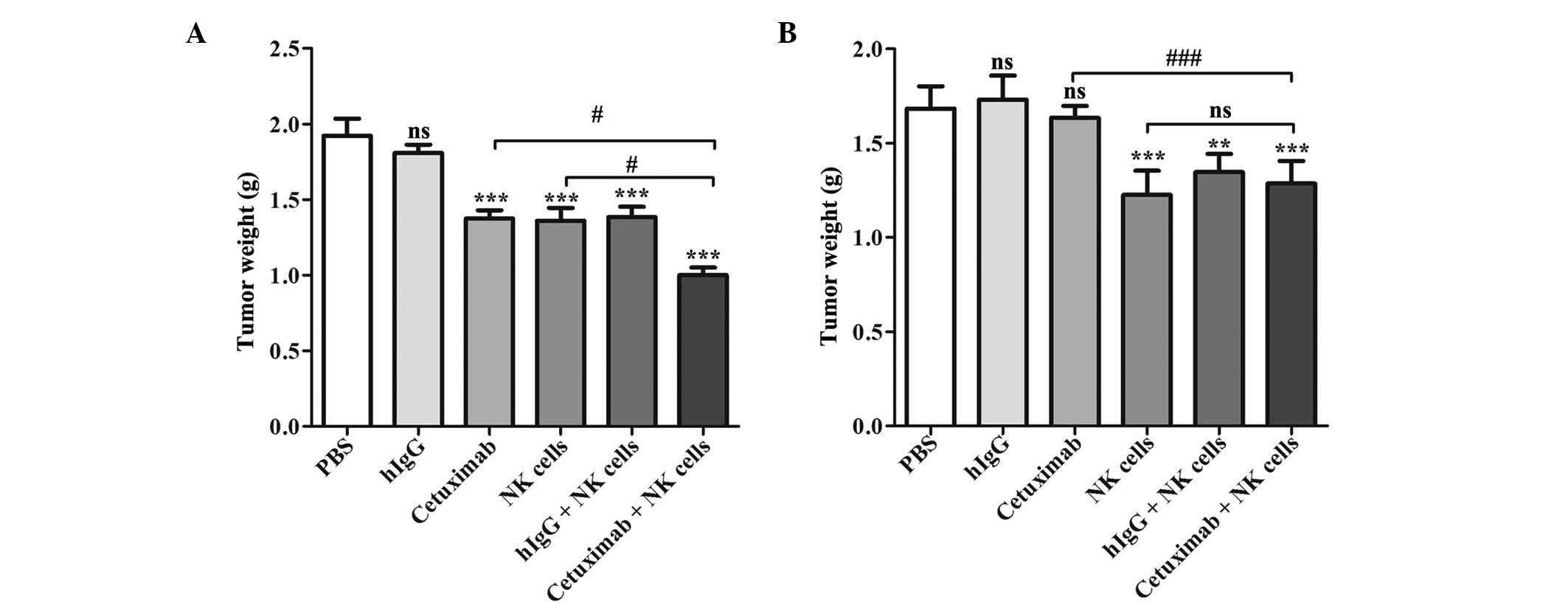
Xenograft tumor weight
At the end of experiment, the average LOVO xenograft
tumor weight of the cetuximab plus NK cells group was decreased
compared with any of the other groups (P<0.0001 compared with
the PBS group, P<0.0001 compared with the hIgG group, P=0.004
compared with the cetuximab group, P=0.047 compared with the NK
cells group and P=0.005 compared with the hIgG plus NK cells
group), and the inhibition rate was 47.92%, which was ~60%
increased compared with the cetuximab or NK cells groups. The
cetuximab, NK cells and NK cells plus hIgG groups also demonstrated
an antitumor effect compared with PBS group (P=0.0002, P=0.0004 and
P=0.0004, respectively), but their tumor weights were increased
compared with combination group (P=0.014, P=0.017 and P=0.023,
respectively). In SW620 xenograft models, the tumor weight showed
no statistical differences among the cetuximab plus NK cell group,
NK cells group and NK cells plus hIgG group (P=0.299), but their
tumor weights were decreased compared the control group (P=0.008,
P=0.004 and P=0.001, respectively). Tumor weight was not affected
by cetuximab only in the SW620 cell xenograft models (P=0.430;
Fig. 3; Table II).
 | Table II.Inhibitory rates of tumor weight in
xenografts. |
Table II.
Inhibitory rates of tumor weight in
xenografts.
|
| LOVO
xenografts | SW620
xenografts |
|---|
|
|
|
|
|---|
| Group | Weight, g | Inhibitory rate,
% | Weight, g | Inhibitory rate,
% |
|---|
| Phosphate-buffered
saline | 1.92±0.11 | – | 1.68±0.05 | – |
| hIgG | 1.81±0.06 |
5.73 | 1.73±0.06 | −3.00 |
| Cetuximab | 1.37±0.05 | 28.65 | 1.63±0.03 |
3.00 |
| NK cells | 1.36±0.09 | 29.17 | 1.23±0.06 | 26.79 |
| hIgG+NK cells | 1.38±0.07 | 28.13 | 1.35±0.04 | 19.64 |
| Cetuximab+NK
cells | 1.00±0.05 | 47.92 | 1.29±0.05 | 23.21 |
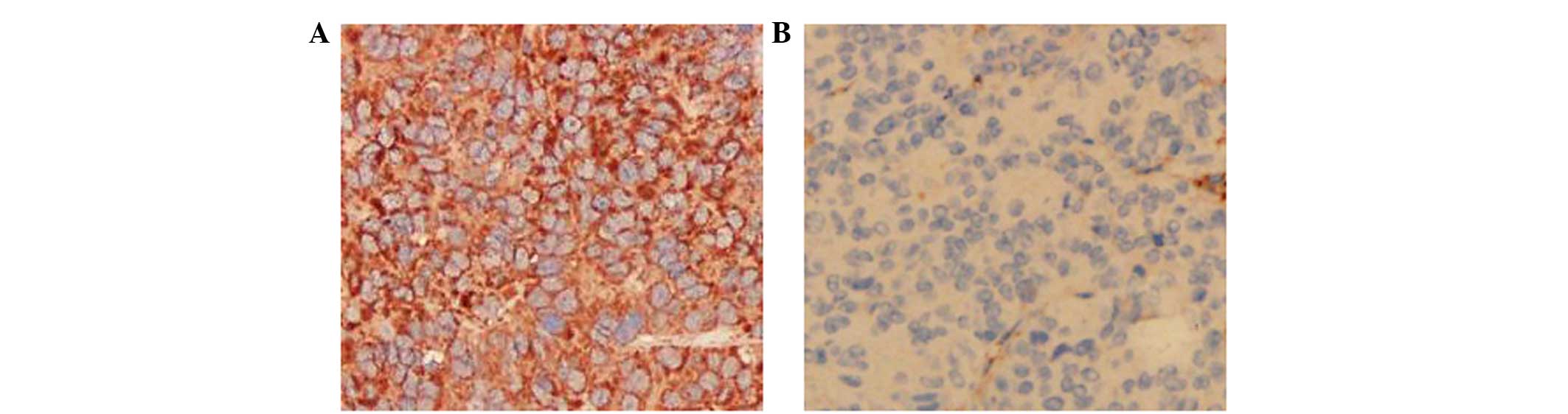
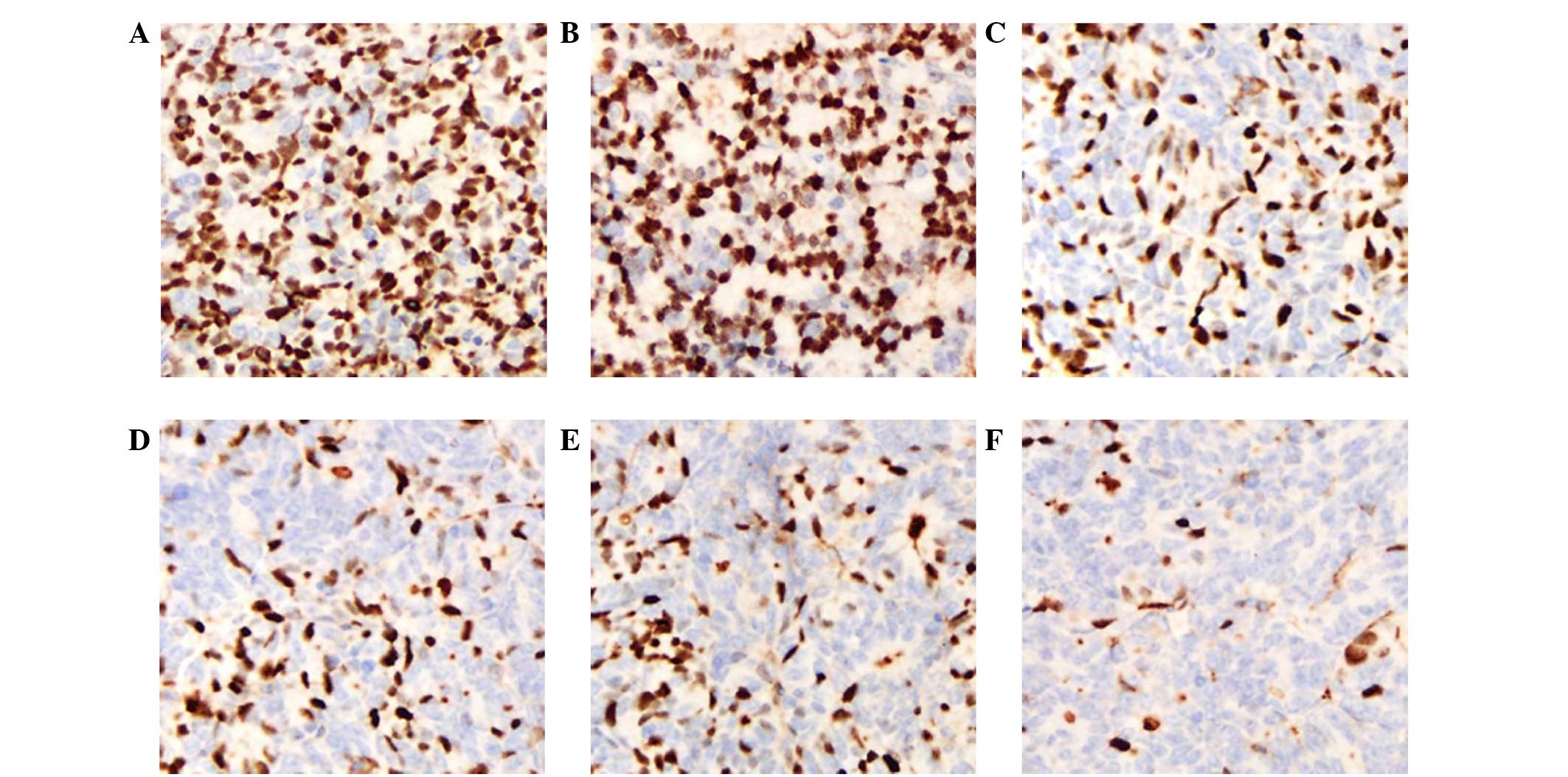
EGFR staining
As shown in Fig. 4,
IHC staining showed that EGFR was mainly expressed in the tumor
cell membrane. The EGFR expression in the LOVO xenograft models was
strong positive (+++), whereas the expression in the SW620
xenograft models was negative (−).
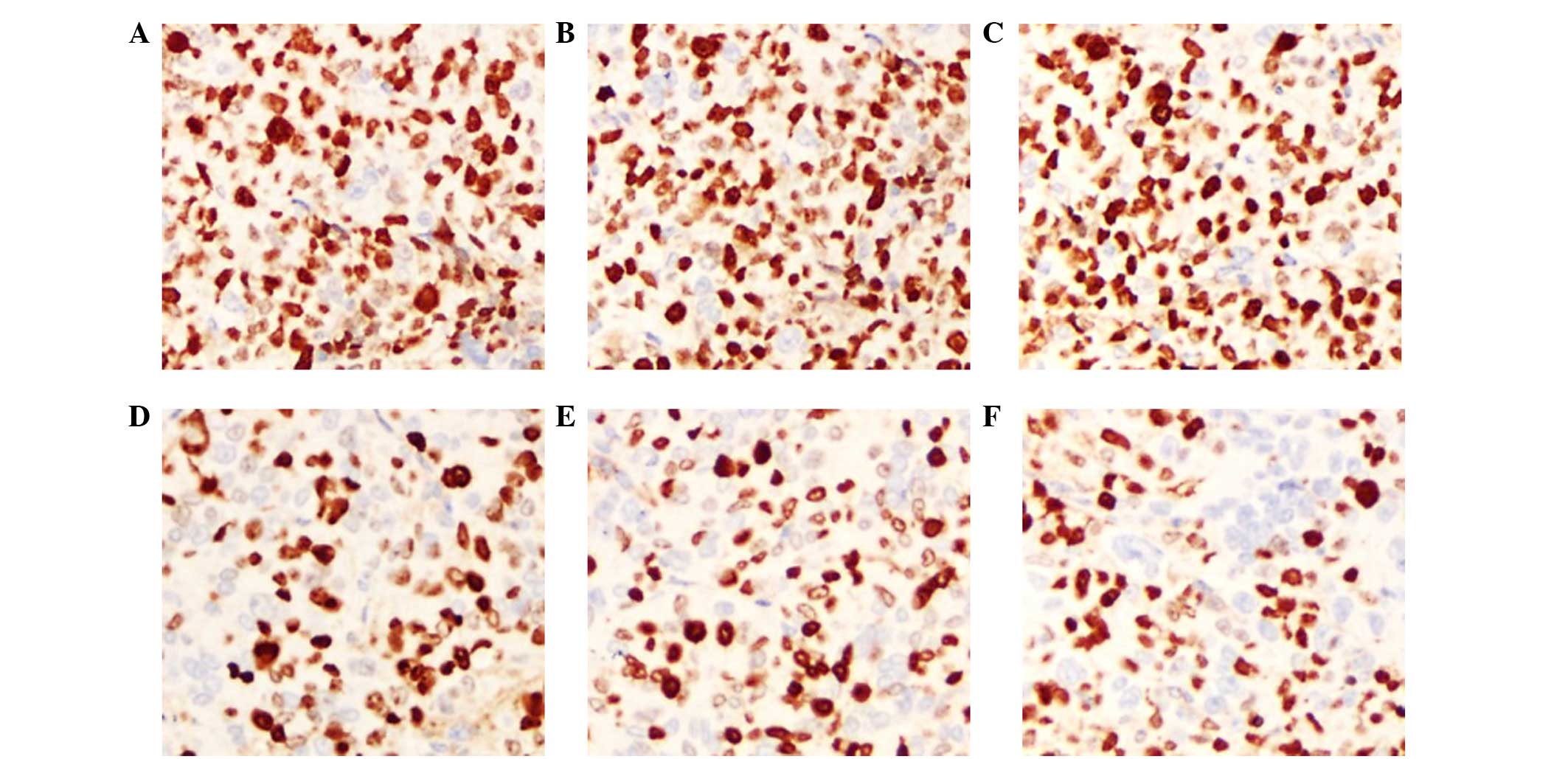
Ki-67 staining
Ki-67 is an indicator of cell proliferation and is
mainly expressed in the cell nucleus. IHC staining showed that the
Ki-67 expression of LOVO xenograft tumors in the cetuximab plus NK
cells group was 23.8±3.89%, which was decreased compared with the
NK cells and cetuximab groups (P=0.003 and P=0.002, respectively).
The expression of Ki-67 in the cetuximab plus NK cells group was
weak positive (+), whereas the expression in the control groups
(PBS and hIgG) was strong positive (+++). In the SW620 xenograft
tumor models, the Ki-67 expression in the cetuximab plus NK cells
group was not decreased compared with the NK cells group (P=0.173).
In addition, the Ki-67 expression in the cetuximab group also
showed no significant difference compared with the control group
(P=0.862). These results indicate that cetuximab or adoptive NK
cells may inhibit the proliferation of tumor cells in LOVO
xenografts, and that the combination of cetuximab and NK cells
significantly improved this effect. Nevertheless, cell
proliferation remained active and was not affected by cetuximab in
the SW620 cell xenograft tumors (Figs.
5 and 6; Table III).
 | Table III.Labeling index of Ki-67 in
xenografts. |
Table III.
Labeling index of Ki-67 in
xenografts.
|
| Ki-67 labelling
index, % |
|---|
|
|
|
|---|
| Group | LOVO
xenografts | SW620
xenografts |
|---|
| Phosphate-buffered
saline | 85.40±1.72 | 83.80±4.14 |
| hIgG | 83.80±2.27 | 88.40±1.12 |
| Cetuximab | 55.00±5.89 | 83.00±1.67 |
| NK cells | 52.20±5.49 | 66.60±4.08 |
| hIgG+NK cells | 54.00±7.07 | 67.40±3.01 |
| Cetuximab+NK
cells | 23.80±3.89 | 59.20±2.97 |
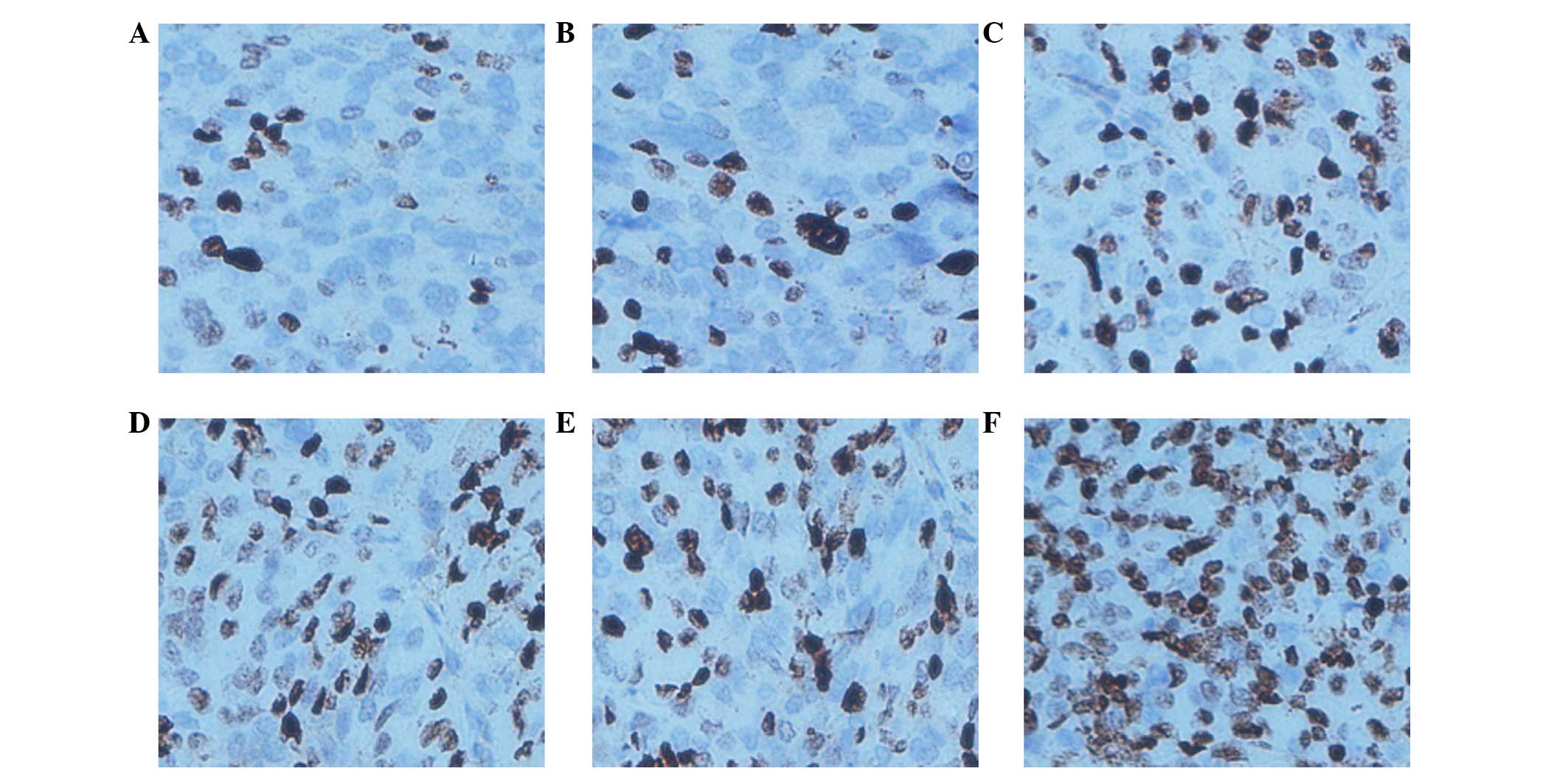
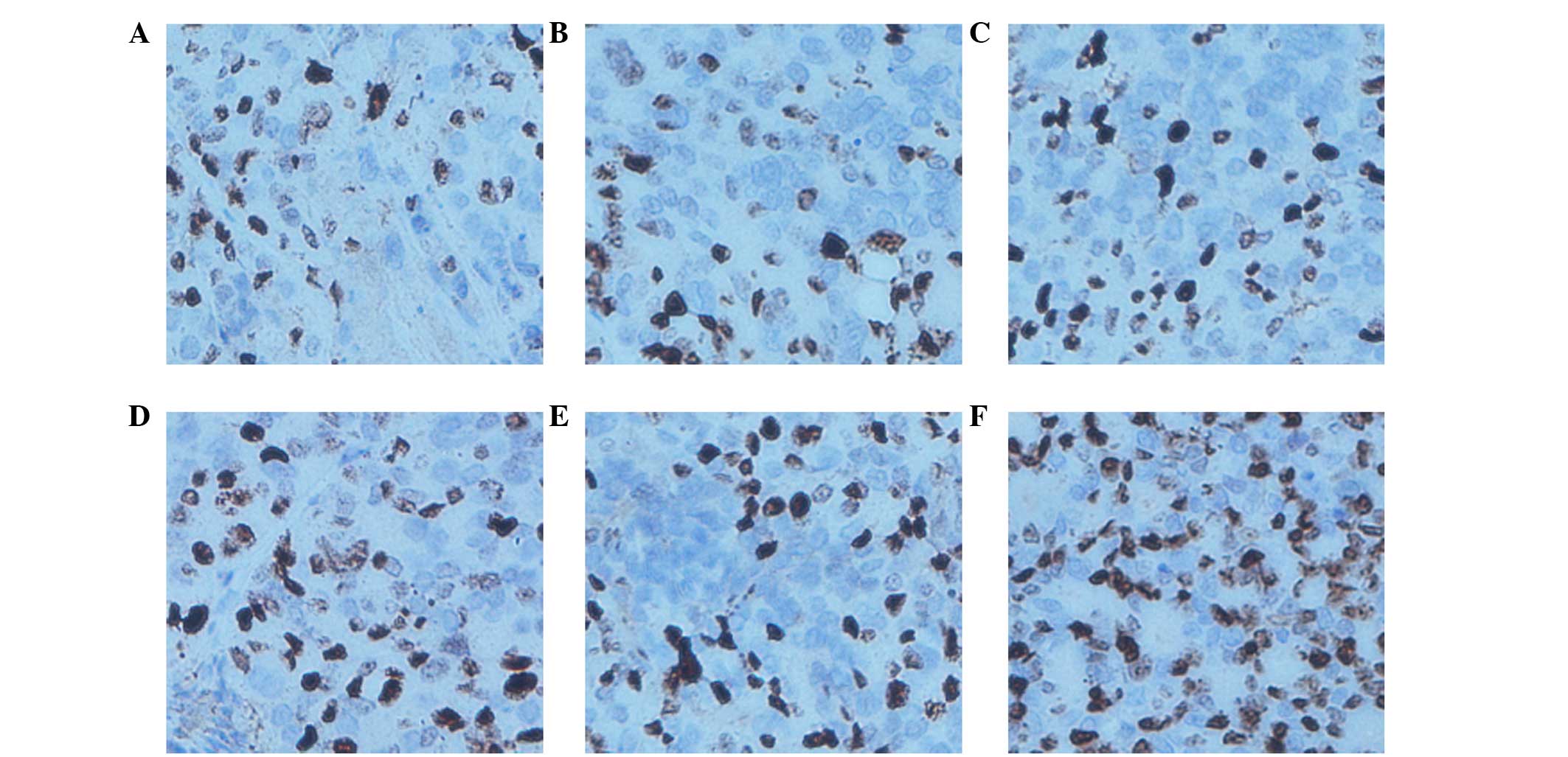
TUNEL assay
TUNEL assays are an indicator of cell apoptosis, in
which the nuclei are stained brown in positively staining cells.
The results showed that the AI of the LOVO xenograft tumors was
73.80±4.35% in the cetuximab combined with NK cells group, which
was evidently increased compared with other groups (P<0.0001
compared with the PBS group, P<0.0001 compared with the hIgG
group, P=0.008 compared with the cetuximab group, P=0.008 compared
with the NK cells group and P=0.002 compared with the hIgG plus NK
cells group). The AI in the cetuximab, NK cells and NK cells plus
hIgG groups increased compared with the PBS control group
(P=0.0009, P=0.0009 and P=0.0003, respectively). The AI of the
SW620 xenograft tumors in the cetuximab combined with NK cells, the
NK cells and the NK cells plus hIgG groups were increased compared
with the PBS control group (P=0.018, P=0.004 and P=0.0007,
respectively); however no significant difference was identified
between the 3 (non-control) groups (P=0.533). The AI in the
cetuximab group was similar to the control group (P=0.780). These
results suggest that NK cells may promote LOVO xenograft tumor cell
apoptosis in vivo, and that the effects are increased by the
participation of cetuximab. However, SW620 xenograft tumor cell
apoptosis was not influenced by cetuximab (Figs. 7 and 8;
Table IV).
 | Table IV.Apoptosis index in xenografts. |
Table IV.
Apoptosis index in xenografts.
|
| Apoptosis index,
% |
|---|
|
|
|
|---|
| Group | LOVO
xenografts | SW620
xenografts |
|---|
| Phosphate-buffered
saline | 24.20±1.46 | 25.40±2.91 |
| hIgG | 23.40±2.91 | 20.00±1.52 |
| Cetuximab | 50.60±4.91 | 24.20±2.96 |
| NK cells | 50.80±4.97 | 49.60±6.14 |
| hIgG+NK cells | 47.40±3.47 | 46.60±4.31 |
| Cetuximab+NK
cells | 73.80±4.35 | 54.00±2.55 |
Discussion
The present preclinical study has focused on the
ADCC activity of adoptive NK cells in combination with cetuximab in
nude mice xenograft models. The results suggested that NK cells
alone could inhibit tumor growth in the LOVO and SW620 xenografts.
Following combination with cetuximab, NK cells had a stronger
inhibiting effect on the growth of LOVO xenografts compared with NK
cell therapy or cetuximab therapy. However, adding cetuximab to NK
cells did not enhance the ADCC activity towards SW620 xenografts.
Pathological changes demonstrated that the varied EGFR expression
levels of the two tumor cells were responsible for these
conflicting results.
NK cells, discovered ~40 years ago, are considered
to be the most effective cytotoxic lymphocytes for counteracting
cancer (25). Mandal and Viswanathan
(25) reported that adoptive NK cell
transfer was applied to advanced CRC patients that were refractory
to standard therapy, and was demonstrated to be efficacious and
safe. The data from the present study also verified that the
adoptive injection of NK cells can inhibit LOVO or SW620 xenograft
tumor cell proliferation and promote apoptosis compared with a PBS
control. However, the effect was not particularly strong and the
tumor volume and weight remained at a relatively high level.
Cetuximab has been approved for the first-line
treatment of EGFR-positive metastatic CRC and somewhat demonstrates
therapeutic efficacy when used as a monotherapy in metastatic CRC
patients for which chemotherapy has failed. In the present study,
cetuximab alone also showed considerable antitumor activity in LOVO
xenografts compared with the hIgG control group, and had a similar
effect to NK cells. However, cetuximab did not show a significant
tumor inhibitory effect in the SW620 xenografts.
The therapeutic target of cetuximab is EGFR, which
is a transmembrane glycoprotein (molecular weight, 170 KD) that is
composed by extracellular, transmembrane and intracellular
tyrosinekinase domains. EGFR is widely expressed in human cell
membranes and highly expressed by a variety of epithelial tumor
cells, including 60–80% CRCs (26).
The overexpression of EGFR will lead to uncontrolled cell growth
and proliferation (3,27,28), which
can result in disease progression, metastasis and recurrence and is
associated with a poor outcome of CRC (10). Using IHC staining, the present study
confirmed that the LOVO cells were EGFR-positive (+++) and that the
SW620 cells were EGFR-negative (−), which was consistent with in
vitro experiments reported in the literature (12,29). This
finding indicated that LOVO or SW620 cells transplanted into nude
mice retained the EGFR-positive or -negative biological
characteristics. Seo et al (30) verified that cetuximab-mediated ADCC
activity was strongly and significantly correlated with the cell
surface expression level of EGFR. After completely binding to EGFR,
cetuximab can inhibit of the downstream signals induced by its
natural ligands, epidermal growth factor and transforming growth
factor-α, exposing the cancer cells to the to immune system
(12). NK cells can then lyse the
tumor cells bound to cetuximab via ADCC activity (12). Furthermore, the extent of the
activation of NK cells by cetuximab has also been found to
correlate with the level of EGFR expression (12). Therefore, EGFR-negative SW620
xenografts did not respond to cetuximab and adding cetuximab to NK
cells did not enhance the tumor inhibitory effect of adoptive NK
cells in the present study.
The combination of cetuximab with irinotecan,
fluorouracil (5-FU) and folinic acid chemotherapy or oxaliplatin,
5-FU and folinic acid chemotherapy was shown to be effective in a
previous study (10), yet conflicting
results were found in the COIN (31)
and NORDIC VII (32) trials when
cetuximab was combined with oxaliplatin-based chemotherapy. One of
the most important aspects was the adverse side effects of
chemotherapy. Thus, the present study sought for a safer and more
effective way utilize cetuximab for the treatment of metastatic
CRC. Pahl et al (12) reported
that cetuximab enhances the ADCC activity of NK cells towards
osteosarcoma, and the present in vitro study demonstrates
that cetuximab may significantly enhance NK-mediated ADCC activity
in CRC cell lines. Therefore, cetuximab was combined with adoptive
NK cells in vivo and, as expected, cetuximab was found to
intensify the ADCC activity of adoptive NK cells towards LOVO
xenografts. In agreement with previous studies (10,33), the
present study found that NK cell-mediated ADCC activity could be a
crucial antitumor mechanism of cetuximab in vivo.
Previously, however, certain studies expressed
diverging opinions. Wild et al (34) reported that the effect of cetuximab
in vivo did not necessarily associate with EGFR expression
on the target cell surface, or was affected by a variety of factors
in vivo. Similarly, Kurai et al (9) claimed that even low EGFR expression was
sufficient for maximum ADCC activity. These reports indicate that
the ADCC activity is affected by numerous factors. The ultimate
purpose of the present study is to improve therapeutic efficacy and
decrease the toxicity of cetuximab or adoptive NK cells for
advanced CRC; however, numerous problems remain to be solved,
including the suitable amount of NK cells and the minimum dosage of
cetuximab required to induce maximal anticancer ADCC activity.
Thus, the specific clinical application of this combination also
requires additional studies.
In conclusion, the present study suggests that
cetuximab combined with adoptive NK cells may be a potential
immunotherapy for advanced CRC patients with increased EGFR
expression, particularly for patients that are not sensitive to
isolated NK cell or cetuximab therapies. The expression of EGFR on
tumor cells may be useful as a prediction index for evaluating the
efficacy of the combination therapy. In addition, the present study
elucidates a novel strategy for promoting cancer treatment by
combining molecular target therapy with adoptive cell therapy;
however, additional preclinical studies and clinical trials are
required in order to focus on their efficacy in combination.
Acknowledgements
The present study was supported by the Medical
Innovation Project of Fujian Province (Fujian, China; grant no.
2011-CX-17). The authors would like to thank Miss Qinying Liu for
assistance in manipulating the figures, Miss Yangmei Xu for
modification of the manuscript and the healthy donors that agree to
be involved in the present study.
References
|
1
|
Chen W, Zheng R, Zhang S, Zhao P, Zeng H
and Zou X: Report of cancer incidence and mortality in China, 2010.
Ann Transl Med. 2:612014.PubMed/NCBI
|
|
2
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Noguchi T, Ritter G and Nishikawa H:
Antibody-based therapy in colorectal cancer. Immunotherapy.
5:533–545. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kuppen PJ, Gorter A, Hagenaars M, Jonges
LE, Giezeman-Smits KM, Nagelkerke JF, Fleuren G and van de Velde
CJ: Role of NK cells in adoptive immunotherapy of metastatic
colorectal cancer in a syngeneic rat model. Immunol Rev.
184:236–243. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Barkholt L, Alici E, Conrad R, Sutlu T,
Gilljam M, Stellan B, Christensson B, Guven H, Björkström NK,
Söderdahl G, et al: Safety analysis of ex vivo-expanded NK
and NK-like T cells administered to cancer patients: A phase I
clinical study. Immunotherapy. 1:753–764. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
de Castro-Carpeño J, Belda-Iniesta C,
Casado Sáenz E, Hernández Agudo E, Feliu Batlle J and González
Barón M: EGFR and colon cancer: A clinical view. Clin Transl Oncol.
10:6–13. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Huether A, Höpfner M, Baradari V, Schuppan
D and Scherübl H: EGFR blockade by cetuximab alone or as
combination therapy for growth control of hepatocellular cancer.
Biochem Pharmacol. 70:1568–1578. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Troiani T, Zappavigna S, Martinelli E,
Addeo SR, Stiuso P, Ciardiello F and Caraglia M: Optimizing
treatment of metastatic colorectal cancer patients with anti-EGFR
antibodies: Overcoming the mechanisms of cancer cell resistance.
Expert Opin Biol Ther. 13:241–255. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kurai J, Chikumi H, Hashimoto K, Yamaguchi
K, Yamasaki A, Sako T, Touge H, Makino H, Takata M, Miyata M, et
al: Antibody-dependent cellular cytotoxicity mediated by cetuximab
against lung cancer cell lines. Clin Cancer Res. 13:1552–1561.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sotelo Lezama MJ, Sastre Valera J and
Díaz-Rubio García E: Impact of cetuximab in current treatment of
metastatic colorectal cancer. Expert Opin Biol Ther. 14:387–399.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bachanova V and Miller JS: NK cells in
therapy of cancer. Crit Rev Oncog. 19:133–141. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pahl JH, Ruslan SE, Buddingh EP, Santos
SJ, Szuhai K, Serra M, Gelderblom H, Hogendoorn PC, Egeler RM,
Schilham MW and Lankester AC: Anti-EGFR antibody cetuximab enhances
the cytolytic activity of natural killer cells toward osteosarcoma.
Clin Cancer Res. 18:432–441. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kohrt HE, Colevas AD, Houot R, Weiskopf K,
Goldstein MJ, Lund P, Mueller A, Sagiv-Barfi I, Marabelle A, Lira
R, et al: Targeting CD137 enhances the efficacy of cetuximab. J
Clin Invest. 124:2668–2682. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cheng M, Chen Y, Xiao W, Sun R and Tian Z:
NK cell-based immunotherapy for malignant diseases. Cell Mol
Immunol. 10:230–252. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shiokawa M, Takahashi T, Murakami A, Kita
S, Ito M, Sugamura K and Ishii N: In vivo assay of human
NK-dependent ADCC using NOD/SCID/gamma(null) (NOG) mice. Biochem
Biophys Res Commun. 399:733–737. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lee SC, Srivastava RM, López-Albaitero A,
Ferrone S and Ferris RL: Natural killer (NK): Dendritic cell (DC)
cross talk induced by therapeutic monoclonal antibody triggers
tumor antigen-specific T cell immunity. Immunol Res. 50:248–254.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ogbomo H, Cinatl J Jr, Mody CH and Forsyth
PA: Immunotherapy in gliomas: Limitations and potential of natural
killer (NK) cell therapy. Trends Mol Med. 17:433–441. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ottaiano A, Scala S and Iaffaioli VR:
Cetuximab-dependent ADCC in cancer: Dream or reality? Cancer
Immunol Immunother. 59:1607–1608. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Qu YH and Li Y: Progress of study on
antitumor effects of antibody dependent cell mediated
cytotoxicity-review. Zhongguo Shi Yan Xue Ye Xue Za Zhi.
18:1370–1375. 2010.(In Chinese). PubMed/NCBI
|
|
20
|
Srivastava RM, Lee SC, Andrade Filho PA,
Lord CA, Jie HB, Davidson HC, López-Albaitero A, Gibson SP, Gooding
WE, Ferrone S and Ferris RL: Cetuximab-activated natural killer and
dendritic cells collaborate to trigger tumor antigen–specific
T-cell immunity in head and neck cancer patients. Clin Cancer Res.
19:1858–1872. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Balasa B, Yun R, Belmar NA, Fox M, Chao
DT, Robbins MD, Starling GC and Rice AG: Elotuzumab enhances
natural killer cell activation and myeloma cell killing through
interleukin-2 and TNF-α pathways. Cancer Immunol Immunother.
64:61–73. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Roda JM, Joshi T, Butchar JP, McAlees JW,
Lehman A, Tridandapani S and Carson WE III: The activation of
natural killer cell effector functions by cetuximab-coated,
epidermal growth factor receptor-positive tumor cells is enhanced
by cytokines. Clin Cancer Res. 13:6419–6428. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
JD H, JW Y, RM C, MG Y and QH Z: The ADCC
function of NK cells combined with cetuximab on colon cancer cell.
Fu Jian Yi Ke Da Xue Xue Bao. 46:20–27. 2012.(In Chinese).
|
|
24
|
Yang X, Zhang X, Mortenson ED,
Radkevich-Brown O, Wang Y and Fu YX: Cetuximab-mediated tumor
regression depends on innate and adaptive immune responses. Mol
Ther. 21:91–100. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Mandal A and Viswanathan C: Natural killer
cells: In health and disease. Hematol Oncol Stem Cell Ther.
8:47–55. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Vincenzi B, Zoccoli A, Pantano F, Venditti
O and Galluzzo S: Cetuximab: From bench to bedside. Curr Cancer
Drug Targets. 10:80–95. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Baselga J: Why the epidermal growth factor
receptor? The rationale for cancer therapy. Oncologist. 7(Suppl 4):
S2–S8. 2002. View Article : Google Scholar
|
|
28
|
Goldberg RM and Gill S: Recent phase III
trials of fluorouracil, irinotecan, and oxaliplatin as chemotherapy
for metastatic colorectal cancer. Cancer Chemother Pharmacol.
54(Suppl 1): S57–S64. 2004.PubMed/NCBI
|
|
29
|
Holubec L, Liska V, Matejka VM, Fiala O,
Dreslerova J, Mrazkova P, Treska V and Finek J: The role of
cetuximab in the treatment of metastatic colorectal cancer.
Anticancer Res. 32:4007–4011. 2012.PubMed/NCBI
|
|
30
|
Seo Y, Ishii Y, Ochiai H, Fukuda K,
Akimoto S, Hayashida T, Okabayashi K, Tsuruta M, Hasegawa H and
Kitagawa Y: Cetuximab-mediated ADCC activity is correlated with the
cell surface expression level of EGFR but not with the KRAS/BRAF
mutational status in colorectal cancer. Oncol Rep. 31:2115–2122.
2014.PubMed/NCBI
|
|
31
|
Maughan TS, Adams RA, Smith CG, Meade AM,
Seymour MT, Wilson RH, Idziaszczyk S, Harris R, Fisher D, Kenny SL,
et al: MRC COIN Trial Investigators: Addition of cetuximab to
oxaliplatin-based first-line combination chemotherapy for treatment
of advanced colorectal cancer: Results of the randomised phase 3
MRC COIN trial. Lancet. 377:2103–2114. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tveit KM, Guren T, Glimelius B, Pfeiffer
P, Sorbye H, Pyrhonen S, Sigurdsson F, Kure E, Ikdahl T, Skovlund
E, et al: Phase III trial of cetuximab with continuous or
intermittent fluorouracil, leucovorin, and oxaliplatin (Nordic
FLOX) versus FLOX alone in first-line treatment of metastatic
colorectal cancer: The NORDIC-VII study. J Clin Oncol.
30:1755–1762. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li S, Schmitz KR, Jeffrey PD, Wiltzius JJ,
Kussie P and Ferguson KM: Structural basis for inhibition of the
epidermal growth factor receptor by cetuximab. Cancer Cell.
7:301–311. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wild R, Fager K, Flefleh C, Kan D, Inigo
I, Castaneda S, Luo FR, Camuso A, McGlinchey K and Rose WC:
Cetuximab preclinical antitumor activity (monotherapy and
combination based) is not predicted by relative total or activated
epidermal growth factor receptor tumor expression levels. Mol
Cancer Ther. 5:104–113. 2006. View Article : Google Scholar : PubMed/NCBI
|