Introduction
Granulocytic sarcoma (GS) is a rare form of tumor
consisting of extramedullary leukemic infiltrations. GS can develop
at various sites, including the skin, orbital region, central
nervous system (CNS), lymph nodes and spleen (1). GS may present at an initial leukemia
diagnosis, during disease progression or relapse, or after
hematopoietic stem cell transplantation (SCT) (2). The symptoms of GS depend on its size and
location, and include tenderness or abnormal bleeding. The
incidence of GS in acute myeloid leukemia (AML) is 2.5–9.1%
(3), but it is less frequent in
chronic myelogenous leukemia and other myeloproliferative
diseases.
Chronic myelomonocytic leukemia (CMMoL) is a subtype
of myelodysplastic/myeloproliferative neoplasm (4). The clinical presentation of CMMoL is
often non-specific, including fatigue, dyspnea, petechiae,
hemorrhage, skin lesions or splenomegaly. Diagnostic criteria
include monocytosis of >1,000 cells/mm3 for >3
months, exclusion of all possible infectious etiologies and no
specific gene rearrangements or mutations (5).
Cauda equina syndrome is associated with compression
of the lumbosacral nerve roots below the level of the conus
medullaris, which presents as tenderness and sphincter dysfunction
(6). The current study presents a
rare case of lower back pain and monocytosis as the initial
presentation. Radiographic and immunohistochemical studies
confirmed a diagnosis of CMMoL with granulocytic sarcoma located at
the sacral region.
Case report
A 62 year-old woman presented with a 1-year history
of mild lower back pain with soreness radiating to the left leg.
The patient had previously taken over-the-counter analgesics and
had intermittently undergone physical therapy. However, the
tenderness persisted and then worsened, with the development of
weakness of the left lower leg on February 28, 2015. Other
pertinent symptoms included urinary retention, stool incontinence
and left gum swelling, prompting referral to the Emergency
Department of the Tri-Service General Hospital (Taipei, Taiwan).
Upon physical examination, the patient exhibited swelling and
tenderness of the left posterior mandibular region. A neurological
examination showed hypoesthesia over the L3–5 and S1 dermatomes,
along with a loose anal sphincter and unsteady gait. Bilateral
muscle power was grade 4 (7), and the
Babinski sign was absent. A peripheral blood smear revealed
monocytosis, anemia and thrombocytopenia: White blood cell count,
80,030/µl; hemoglobin, 10.7 g/dl; platelets, 32,000/µl; monocytes,
38.2%; and metamyelocytes, 2.9%. An enlarged spleen was palpable 5
cm below the left costal margin, but no pulmonary or breast masses
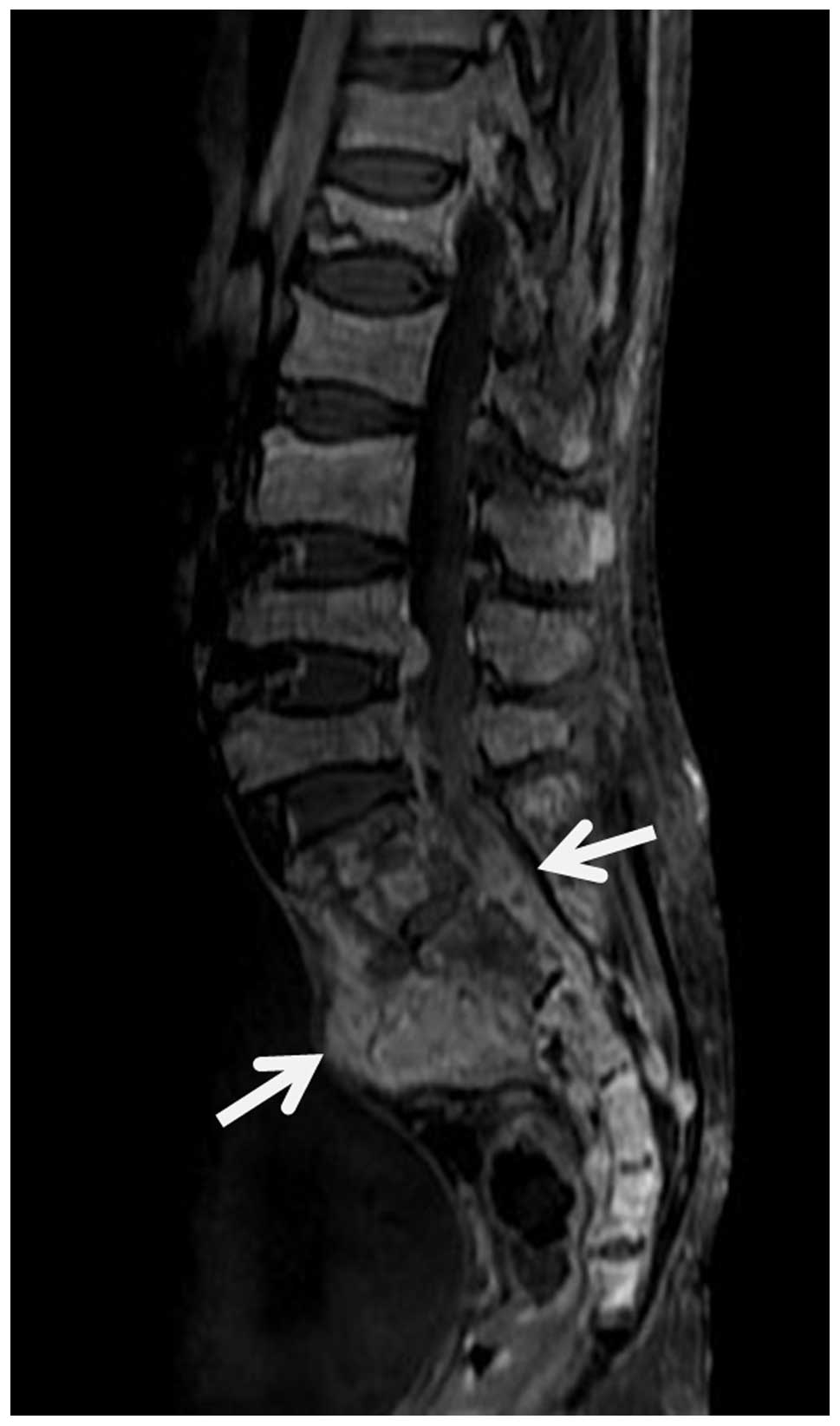
were found. Spine magnetic resonance imaging showed several
heterogeneously contrast-enhancing masses up to 5.6 cm in diameter,
located at the S1 to S3 vertebrae. Multiple enhancing nodules were
identified in the spinal canals from L4 to the caudal end (Fig. 1). The patient was immediately admitted
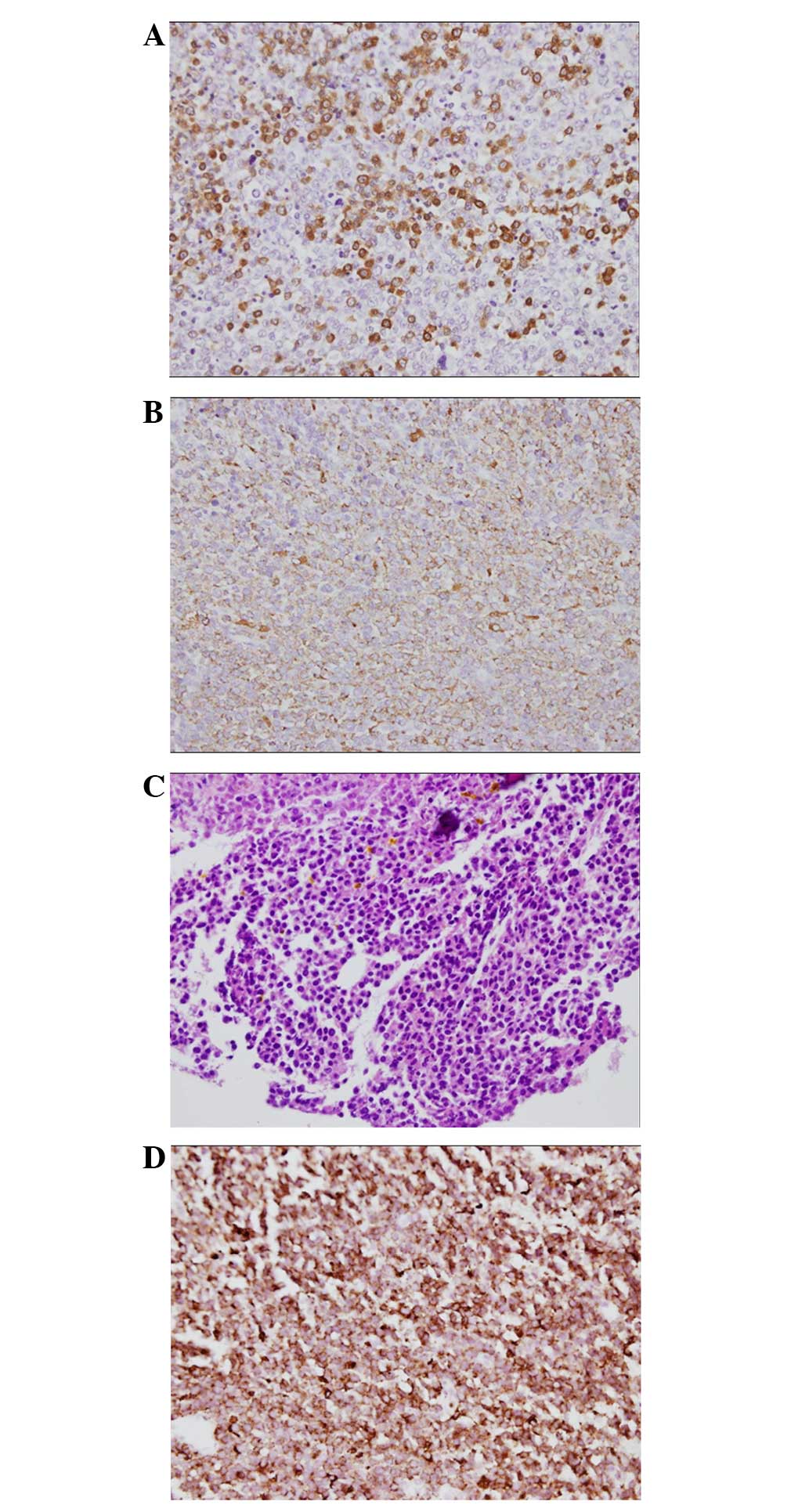
with a diagnosis of cauda equina syndrome. A bone marrow biopsy and
spine biopsy were performed. The bone marrow was hypercellular and
demonstrated dysplastic megakaryocytes with hyposegmentation,
left-shifted myeloid hyperplasia and an increased myeloid:erythoid
ratio (>10/1). Cluster of differentiation (CD)34 (mouse
anti-human CD34 class II monoclonal antibody; 1:100 dilution;
clone, QBEnd 10; Dako, Glostrup, Denmark), was positive in ~15% of
cells, and there was also increased numbers of CD68-positive cells
(mouse anti-human CD68 monoclonal antibody; 1:100 dilution; clone,
PG-M1; Dako). The two pathology reports indicated CMMoL with spine
involvement (Fig. 2A-D). Cytogenetic
studies were normal (46XX). Flow cytometry revealed 18% of
monoblasts lacking the expression of cluster of differentiation
(CD)14, CD34 and CD117, and with increased expression of CD56. The
patient was therefore diagnosed with CMMoL, intermediate-2,
according to the CMMoL-specific prognostic scoring system (8), and treated with low-dose cytosine
arabinoside (10 mg/m2 every 12 h) for 10 days.
Palliative radiotherapy was also arranged, but was not performed as
the condition of the patient deteriorated. The patient succumbed to
severe sepsis half a month later.
Discussion
In patients who complain of lower back pain, a
thorough survey of all possible underlying systemic diseases, with
an evaluation of neurological signs, should be undertaken,
particularly in elderly patients. A total of 5–14% of cancer
patients develop spinal metastasis with cord compression (9). Lung, breast, prostate, renal and
gastrointestinal tumors are all prone to progress to or present
with spinal metastasis (10). A
detailed workup should be performed to search for the primary
etiology. In addition to solid tumors, metastatic spinal lesions of
hematological origin should be taken into consideration,
particularly in patients with an abnormal hemogram.
The incidence and prevalence of CMMoL are not high,
and the exact frequencies are unknown (11). Granulocytic sarcoma is more common in
acute leukemia and less common in chronic leukemia (1). Leukemia cutis is the most common type of
GS that presents in CMMoL, accounting for 10.2% of cases during
disease progression (12). Certain
cases transform to AML rapidly. The remaining sites of involvement
are the pericardium, jejunum and testis, respectively (13–16).
Extramedullary involvement of the CNS is rare, and only one
pediatric patient has been reported following SCT (17). This juvenile CMMoL patient experienced
bone marrow relapse 8 months after GS formation in the CNS.
According to the aforementioned findings, it is known that the
presence of GS in CMMoL patients indicates a dismal outcome and a
possible sign of blastic crisis. The treatment for CMMoL varies
depending on the severity of the disease status and the specifics
of the presentation. Patients with a lower blast count (<5%) may
initially require only supportive care if their symptoms are mild.
However, conventional chemotherapy, hypomethylating agents or
allogeneic SCT may be required for those with bone marrow blast
counts of >10% or for those who exhibit other signs of advanced
or aggressive disease. The treatment response of hypomethylating
agents is 25–70% (5). Patients may
also require >4 cycles of therapy to reach a clinical response,
which is similar to myelodysplastic syndrome (18).
The present study reported a case with an unusual
presentation of back pain that was finally diagnosed as a
hematological malignancy. In conclusion, GS should be taken into
consideration for patients with a spinal mass and abnormal
hemogram. The presence of GS in CMMoL predicts a poor outcome. A
prompt biopsy is important to ensure the correct diagnosis and to
guide the appropriate treatment, thus preventing rapid progression
of the disease.
Acknowledgements
The authors would like to thank Mr. Chian-Ming Chen,
Miss Hsin-Yi Liu and Dr Wen-Chuan Tsai from the Tri-Service General
Hospital for their expertise in analyzing the patient's bone marrow
smear, spinal biopsy specimen and flow cytometry results. The
authors would also like to thank Dr Anthony Janckila (Department of
Microbiology and Immunology, University of Louisville, Louisville,
KY, USA) for providing a critical review of the manuscript.
References
|
1
|
Yilmaz AF, Saydam G, Sahin F and Baran Y:
Granulocytic sarcoma: A systematic review. Am J Blood Res.
3:265–270. 2013.PubMed/NCBI
|
|
2
|
Avni B and Koren-Michowitz M: Myeloid
sarcoma: Current approach and therapeutic options. Ther Adv
Hematol. 2:309–316. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bakst RL, Tallman MS, Douer D and Yahalom
J: How I treat extramedullary acute myeloid leukemia. Blood.
118:3785–3793. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Arber DA, Orazi A, Hasserjian R, Thiele J,
Borowitz MJ, Le Beau MM, Bloomfield CD, Cazzola M and Vardiman JW:
The 2016 revision to the World Health Organization classification
of myeloid neoplasms and acute leukemia. Blood. 127:2391–2405.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Patnaik MM, Parikh SA, Hanson CA and
Tefferi A: Chronic myelomonocytic leukaemia: A concise clinical and
pathophysiological review. Br J Haematol. 165:273–286. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fraser S, Roberts L and Murphy E: Cauda
equina syndrome: A literature review of its definition and clinical
presentation. Arch Phys Med Rehabil. 90:1964–1968. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bickley LS and Szilagyi PG: BATES' Pocket
Guide to Physical Examination and History Taking. 5th. Lippincott
Williams & Wilkins; Philadelphia: pp. 3132007
|
|
8
|
Such E, Germing U, Malcovati L, Cervera J,
Kuendgen A, Porta MG Della, Nomdedeu B, Arenillas L, Luño E, Xicoy
B, et al: Development and validation of a prognostic scoring system
for patients with chronic myelomonocytic leukemia. Blood.
121:3005–3015. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kaloostian PE, Yurter A, Zadnik PL,
Sciubba DM and Gokaslan ZL: Current paradigms for metastatic spinal
disease: An evidence-based review. Ann Surg Oncol. 21:248–262.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Coleman RE: Skeletal complications of
malignancy. Cancer 80 (8 Suppl). 1588–1594. 1997. View Article : Google Scholar
|
|
11
|
Parikh SA and Tefferi A: Chronic
myelomonocytic leukemia: 2013 update on diagnosis, risk
stratification, and management. Am J Hematol. 88:967–974. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mathew RA, Bennett JM, Liu JJ, Komrokji
RS, Lancet JE, Naghashpour M, Messina JL, List AF, Moscinski LC and
Zhang L: Cutaneous manifestations in CMML: Indication of disease
acceleration or transformation to AML and review of the literature.
Leuk Res. 36:72–80. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bradford CR, Smith SR and Wallis JP:
Pericardial extramedullary haemopoiesis in chronic myelomonocytic
leukaemia. J Clin Pathol. 46:674–675. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Craig JW and Lin RJ: Paraneoplastic
autoimmunity associated with testicular myeloid sarcoma and chronic
myelomonocytic leukemia. Case Rep Hematol.
2013:6565432013.PubMed/NCBI
|
|
15
|
Fukushima M, Ono Y and Imai Y:
Granulocytic sarcoma of the small intestine in a patient with
chronic myelomonocytic leukemia. Dig Endosc. 26:757–758. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hyams ES, Gupta R, Melamed J, Taneja SS
and Shah O: Renal involvement by chronic myelomonocytic leukemia
requiring nephroureterectomy. Rev Urol. 11:33–37. 2009.PubMed/NCBI
|
|
17
|
Wilson DB, Michalski JM, Grossman WJ and
Hayashi RJ: Isolated CNS relapse following stem cell
transplantation for juvenile myelomonocytic leukemia. J Pediatr
Hematol Oncol. 25:910–913. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Silverman LR, McKenzie DR, Peterson BL,
Holland JF, Backstrom JT, Beach CL and Larson RA: Cancer and
Leukemia Group B: Further analysis of trials with azacitidine in
patients with myelodysplastic syndrome: Studies 8421, 8921, and
9221 by the Cancer and Leukemia Group B. J Clin Oncol.
24:3895–3903. 2006. View Article : Google Scholar : PubMed/NCBI
|