Introduction
Colorectal cancer, which includes colon and rectal
cancer, is a common digestive tract tumor. In recent years, there
is an upward trend in the incidence of colorectal cancer in China
(1). The incidence of colorectal
cancer in China is ranked fourth in men and third in women
(2). Acute left-sided mechanical
intestinal obstruction needs to be addressed. Traditional surgical
treatment is utilized for gastrointestinal fistula, followed by
staging tumor resection (3). Tumor
resection is primarily used to treat patients. Although it is
generally considered successful, there are disadvantages to
consider, including the length of course of treament, the
considerable pain experienced by patients and high cost.
Middle-aged and elderly patients often experience a high percentage
of water and electrolyte disorders, reulting in an increased risk
of emergency surgery. There is also a high incidence of
postoperative complications, such as anastomotic fistula (4).
Use of the ileal tube for bowel decompression has
become increasingly common (5). The
decompression tube was inserted into the proximal colon of
obstruction point through anus to effectively alleviate and
eliminate any obstruction in patients with symptoms, thereby
avoiding emergency surgery. It also allows for intestinal cleaning,
relieves swelling (edema) of the intestinal wall, creating
conditions for tumor I stage radical excision anastomosis. Left
colon obstruction may be treated by placing an ileal tube during
colonoscopy and having patients undergo a single-stage anastomosis
following colonic decompression and lavage, which reduces
experience of pain (6–8). This process can cause secondary pain
during treatment because of the ileal tube placement. Transanal
placement of the ileal tube to treat left colon obstruction through
X-ray monitoring has been widely used in Xuzhou Central Hospital
since 2011. Patients readily accept this procedure as it is
virtually painless, has a high success rate, and fewer
complications.
The present study was undertaken to examine the
clinical value of transanal ileal tube placement under X-ray
monitoring.
Patients and methods
Patients
Thirty-six patients were diagnosed with left colon
cancer obstruction in Xuzhou Central Hospital between July 2014 and
February 2011. Of the 36 cases, 21 were men, and 15 were women,
with an age range of 45–93 years and a median age of 73.5 years.
The course of the disease was 1–7 days with an average of 3 days.
All 36 patients were diagnosed with left-sided malignant tumor and
obstruction through X-ray and computed tomography, including 8
cases of left-sided intestinal obstruction, 14 cases of descending
colon obstruction, 10 cases of sigmoid colon obstruction and 4
cases of upper rectal obstruction. Patients had a different degree
of abdominal distension and pain prior to treatment. Any patients
with intestinal strangulation were excluded from the study.
Instruments
The Philips Tele-Diagnost digital gastrointestinal
machine (Philips, The Netherlands) was used to produce X-ray and
guide the technical operation. The (0.97 mm) 2.6 m long guidewire
was purchased from Terumo (China) Holding Corp. (Tokyo, Japan). The
4.2 m long intestinal guidewire (MTN-QF medical non-vascular
guidewire) was purchased from Micro-Tech Co., Ltd. (Nanjing,
China). The 5F single-curve catheter (1.25 m long) was purchased
from Cordis Corp. (Miami Lakes, FL, USA) and intestinal lavage
syringes (100 ml) were purchased from Shandong Weigao Group Medical
Polymed Co., Ltd. (Weihai, China).
Methods
Patients underwent conventional abdominal vertical
perspective to observe the obstruction site. The patient lay in the
left lateral recumbent position, and the loach guidewire and 5F
single-curve catheter were inserted through the rectum and gently
guided via X-ray monitoring. If the guidewire did not perforate, a
single bend duct and iohexol were used to observe whether any
contrast agent was diffused. If any contrast agent was detected, a
different angle was used to follow the path of further insertion of
the guidewire catheter. However, when no difference was observed in
the vessels, repeated exploration using a combination of the
guidewire and catheter was performed. The loach guidewire was
withdrawn following perforation of the obstruction site. The
contrast agent was injected by transcatheter to confirm that the
catheter tip was located in the dilated colon. The site and length
of obstruction were observed at the same time. The hard guidewire
was then inserted, and the single-curve catheter was withdrawn. A
dilatation catheter was inserted together with the intestinal
guidewire for pre-expansion.
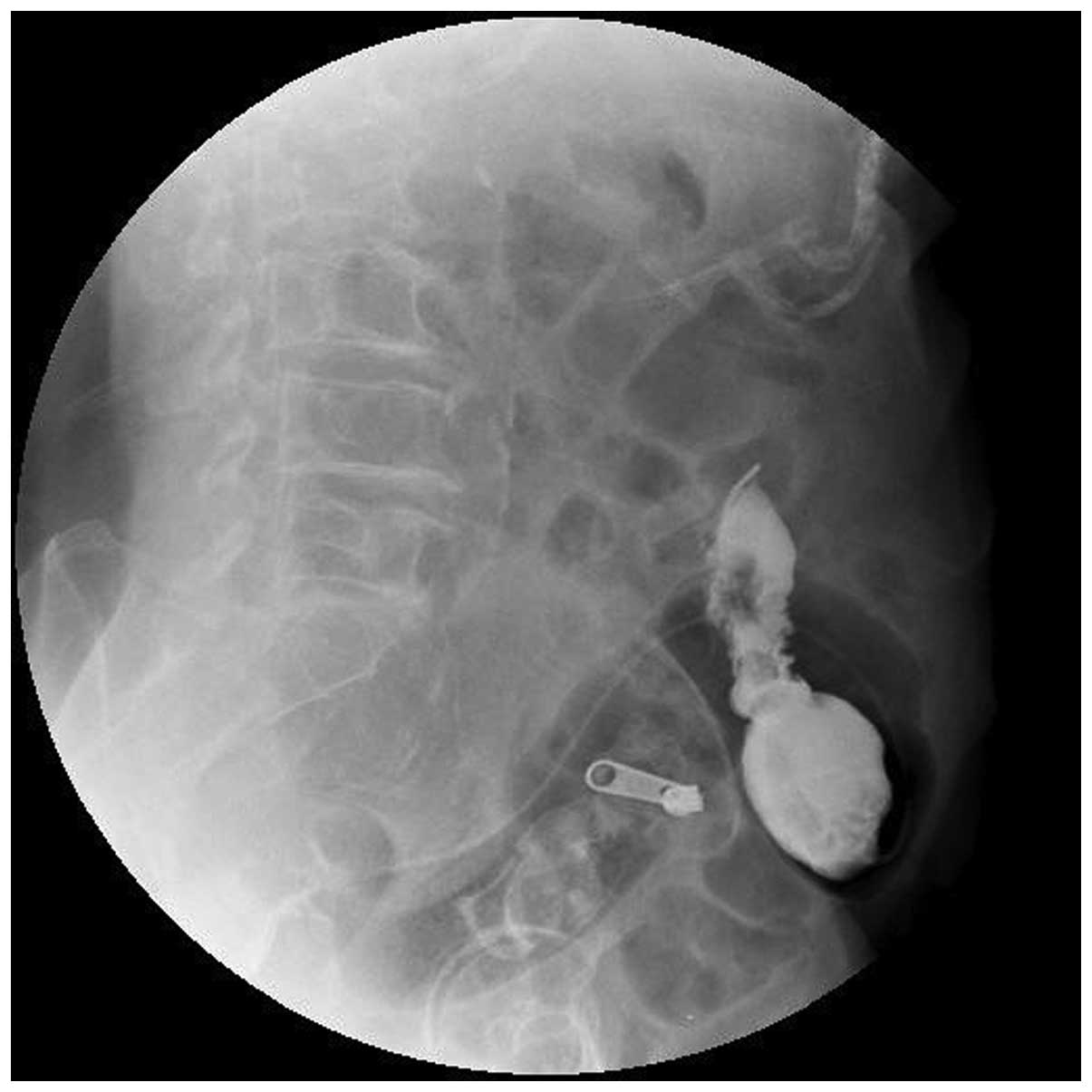
An ileal decompression tube coated with paraffin oil
on the front was inserted along with the hard guidewire. When the
balloon of the ileal decompression tube encountered the stenosis as
confirmed by X-ray, the tube was inserted for a further 10 cm to
prevent necrosis of the bowel wall regions caused by stenosis
compression following infusion of water into the balloon. A total
of 30 ml in sterile distilled water was injected into the balloon
to prevent prolapse of the intestinal obstruction decompression
catheter. The Y-type joint was connected, and the contrast agent
was again injected to confirm that the decompression tube was
located in the colon (Figs.
1–5). The medical adhesive tape
was used to fasten the rectum catheter postoperatively. Continuous
suction was applied following the procedure and intermittent
suction was applied on the second day. At the same time, full colon
irrigation with warm water (500 ml/times) was applied 4–6 times a
day (4). Abdominal pain, bloating,
and other symptoms were carefully observed postoperatively.
Properties of the drainage fluid were observed to confirm the
drainage catheter patency.
Results
Thirty-two patients underwent successful transanal
ileal decompression tube under X-ray monitoring. Thirty-one
patients underwent decompression, intestinal lavage drainage and
stage 1 intestinal resection and anastomosis. No cases of
anastomotic leakage or death due to surgery were identified.
However, incision infection was evident in one patient. One patient
preferred non-surgical therapy (stenting) subsequent to the lifting
of intestinal obstruction symptoms due to age.
Decompression time of catheter indwelling in 31
patients was 4–9 days (median 5 days, average 5.61 days). The
catheter drainage observed after 24 h was yellow, brown sticky
stool, mixed with a substantial amount of gas. Waste volume was
2,000–4,000 ml with an average of 2,800 ml. Abdominal pain, and
abdominal distension symptoms of all the patients were apparently
alleviated. Colonic expansion was significantly improved (Fig. 6).
The guidewire perforated the bowel in two patients
during exploration of the obstruction. Contrast agent diffusion
into the abdominal cavity was evident after injection with the
contrast agent. The catheter and guidewire were subsequently
withdrawn and patients immediately underwent surgery. The repeated
exploration guidewire did not perforate the obstruction site in two
patients and tube indwelling was abandoned.
Discussion
Colonic obstruction is a serious complication of
colorectal cancer indicating poor prognosis in patients. The
primary option for colorectal cancer patients is surgery. For
right-sided colonic cancer obstruction or chronic partial
obstruction, stage 1 whole resection and anastomosis is preferred
following sufficient preoperative bowel preparation (9,10).
Regarding left-sided colon cancer, stage 1 complete
resection and anastomosis potentially induce infection and
anastomotic fistula due to prominent edema and dilatation of the
proximal colon, poor blood supply, large amount of bacteria, and
complexity of the bacteria (11).
Tumor obstruction of the colon frequently occurs in elderly
patients with further complications in multiple organs,
compensatory dysfunction, immune dysfunction, reduced surgical
tolerance, further surgical complications and high mortality rate
(12). The traditional treatment
approach is the Hartmann procedure (abdominal resection of rectal
cancer, with a proximal colonic stoma and distal closure
operation), followed by closure of the stoma in selective surgery
(3,9).
However, this procedure involves a long period of recuperation
time, significant pain, and high cost. In addition, patient quality
of life is inevitably affected owing to the existence of the stoma.
Stage 1 anastomosis can be performed when the bowel is prepared
preoperatively. The ileus tube may be guided by an endoscope to
provide lavage and obtain good results (6,13).
However, the endoscopic catheter requires preparation including
enema bowel cleaning prior to insertion, as well as gas injection
during colonoscopy which causes considerable pain (14). Consequently, this procedure is not
preferred by patients. Transanal ileal tube placement under X-ray
monitoring is more readily accepted by patients due to a lower
amount of pain, high success rate, and observation of the direction
of the catheter and the guidewire at any point.
In the present study, the path of the guidewire
during exploration was different to that in the normal human colon.
The contrast agent was injected through a single-curve catheter. If
perforation of the catheter was confirmed, colonic investigation
continued until the expanded colon was reached. In two cases,
contrast agent diffusion following injection confirmed that the
catheter had penetrated the abdominal cavity. The catheter and
guidewire were withdrawn in a timely manner causing no visible
peritonitis or other serious consequences.
Repeated exploration resistance of the guidewire and
catheter indicates stenosis. Transcatheter injection of the
contrast agent was used to determine whether the contrast agent was
diffused, which would allow for insertion of the guidewire or
catheter. No contrast agent diffusion indicated a short stenosis
time and that the site of stenosis was not infiltrated or fused
completely, but had a small gap in the majority of cases. The
contrast agent was used by pressure injection to observe contrast
agent infiltration. The majority of patients exhibited a small
amount of contrast agent penetration. If contrast agent
infiltration was successful, exploration involved guidewire
combined with catheter, whereas if there was no contrast agent
infiltration, careful inspection using guidewire and catheter
individually was required. The guidewire guided the catheter in the
exploration process. The contrast agent was injected in a timely
manner every 2–3 cm, to ensure that the front section of the
catheter is in the middle of the colon. At the same time, the site
and length of the obstruction were observed.
When the ileus tube was inserted, the catheter tip
was coated with paraffin oil to facilitate its insertion. The
catheter was inserted a further 10 cm after the decompression
catheter balloon across the stenosis to prevent necrosis of the
bowel wall caused by the water injection to the balloon. Since
stools in the colon tend to be thick in general, leading to a fecal
mass in some cases, the catheter must remain unobstructed. If
blockage occurs, the timely use of an intestinal lavage syringe
dredge is necessary. The dredging method involves the infusion of
500 ml warm saline water into the intestine and is then suspended
for 30 min after drainage. Warmed saline water was used for
dredging the following day and retained for approximately 30 min to
soften the stools. Attention was paid to water-electrolyte and
acid-base balance in patients subsequent to insertion of the
catheter.
In summary, transanal placement of the ileus tube
under X-ray monitoring effectively alleviates left-sided colonic
obstruction symptoms following preoperative preparation. Thus, the
present study has identified a safe, effective, economical
treatment method that may be utilized for colon cancer and readily
accepted by patients.
References
|
1
|
Chen W, Zheng R, Zeng H, Zhang S and He J:
Annual report on status of cancer in China, 2011. Chin J Cancer
Res. 27:2–12. 2015.PubMed/NCBI
|
|
2
|
Jie H and Wanqing C: China tumor
registration report. Military Medical Science Press; Beijing: pp.
31–56. 2012
|
|
3
|
Breitenstein S, Rickenbacher A, Berdajs D,
Puhan M, Clavien PA and Demartines N: Systematic evaluation of
surgical strategies for acute malignant left-sided colonic
obstruction. Br J Surg. 94:1451–1460. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pavlidis TE, Marakis G, Ballas K,
Rafailidis S, Psarras K, Pissas D, Papanicolaou K and Sakantamis A:
Safety of bowel resection for colorectal surgical emergency in the
elderly. Colorectal Dis. 8:657–662. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nozoe T and Matsumata T: Usefulness of
preoperative colonic lavage using transanal ileus tube for
obstructing carcinoma of left colon: device to perform one-stage
operation safely. J Clin Gastroenterol. 31:156–158. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dekovich AA: Endoscopic treatment of
colonic obstruction. Curr Opin Gastroenterol. 25:50–54. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fischer A, Schrag HJ, Goos M, Obermaier R,
Hopt UT and Baier PK: Transanal endoscopic tube decompression of
acute colonic obstruction: experience with 51 cases. Surg Endosc.
22:683–688. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Araki Y, Isomoto H, Matsumoto A, Kaibara
A, Yasunaga M, Hayashi K, Yatsugi H and Yamauchi K: Endoscopic
decompression procedure in acute obstructing colorectal cancer.
Endoscopy. 32:641–643. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Villar JM, Martinez AP, Villegas MT,
Muffak K, Mansilla A, Garrote D and Ferron JA: Surgical options for
malignant left-sided colonic obstruction. Surg Today. 35:275–281.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ohnita K, Shikuwa S, Isomoto H, Yamaguchi
N, Okamoto K, Nishiyama H, Fukuda E, Nakamura T, Mizuta Y and Kohno
S: A new thin endoscopic method of transanal drainage tube
insertion for acute colonic obstruction due to colorectal cancer.
Dig Endosc. 21:252–254. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Leong QM, Aung MO, Ho CK and Sim R:
Emergency colorectal resections in Asian octogenarians: Factors
impacting surgical outcome. Surg Today. 39:575–579. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Merkel S, Meyer C, Papadopoulos T, Meyer T
and Hohenberger W: Urgent surgery in colon carcinoma. Zentralbl
Chir. 132:16–25. 2007.(In German). PubMed/NCBI
|
|
13
|
Morino M, Bertello A, Garbarini A, Rozzio
G and Repici A: Malignant colonic obstruction managed by endoscopic
stent decompression followed by laparoscopic resections. Surg
Endosc. 16:1483–1487. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Keränen I, Lepistö A, Udd M, Halttunen J
and Kylänpää L: Stenting for malignant colorectal obstruction: a
single-center experience with 101 patients. Surg Endosc.
26:423–430. 2012. View Article : Google Scholar : PubMed/NCBI
|