Introduction
The incidence of differentiated thyroid carcinoma
(DTC) is very frequent in clinic, accounting for 90–95% of all
thyroid carcinoma clinical incidence (1). With increasing number of cancer cases in
the early stage of diagnosis, excision is becoming the first choice
of treatment. Moreover, biological nature of differentiated thyroid
cancer determines its low degree of malignancy and late lymphatic
metastasis.
Total thyroidectomy and subtotal thyroidectomy are
generally considered optimal options (2). However, some studies have suggested that
based on lymph node partitions, the act of clearing the most
suspicious lymph node does not increase the surgical complications,
but reduces the possibility of tumor recurrence and second surgery
(3).
In the present study, we studied the preoperative
high-frequency color ultrasonography for the removal and range of
the lymph nodes and obtained favorable results.
Patients and methods
Patients
In total 80 patients diagnosed with DTC at The
Second Affiliated Hospital of Harbin Medical University
(Heilongjiang, China) from March 2012 to March 2014 were
successively included in the study. The patients suffered from
hoarseness, drinking cough and diminishing physique of unknown
origin or remained relatively asymptomatic. The patients were
examined for thyroid nodule in their physical inspection, and were
diagnosed with DTC after ultrasound guided fine needle puncture
biopsy. The inclusion criteria for the study were: i) According to
DTC diagnostic criteria; ii) age ≥18 years, <75 years; and iii)
no systemic metastasis. The exclusion criteria for the study were:
i) Pregnancy; ii) combined hyperthyroidism, Hashimoto's thyroiditis
and severe hypothyroidism; iii) patients with severe heart, liver,
kidney and other organ dysfunction, or with mental disorder; and
iv) patients with poor compliance or patients who refused to
participate in the research.
After approval of the ethics committee of The Second
Affiliated Hospital of Harbin Medical University and informed
consent was obtained from patients or relatives, the cases were
divided into the control group (n=36 cases) and observation group
(n=44 cases). There were 14 male patients and 22 female patients in
the control group, aged 37–66 years, with an average age of
46.9±12.3 years. There were 32 cases of papillary carcinoma, and 4
cases of follicular carcinoma. The tumor diameter was 0.6–2.2 cm,
with an average of 1.4±0.3 cm. There were 20 male patients and 24
female patients in the observation group, aged 35–68 years with an
average of 48.7±13.4 years. Furthermore, there were 39 cases of
papillary carcinoma, 5 cases of follicular carcinoma, and the tumor
diameter was 0.7–2.5 cm with an average of 1.6±0.5 cm. A comparison
of the differences of the gender, age, pathological type and tumor
size showed no statistical significance (P>0.05).
Test methods
The patients in both groups underwent total
thyroidectomy or subtotal thyroidectomy, the standard of which
complied with the 2012 guideline for the diagnosis and treatment of
thyroid cancer. Notably, attention was paid not to damage the
parathyroid during surgery, and the combination of tracers e.g.,
methylene blue and nano carbon and micro-technique were applied if
necessary. The surrounding tissue and structures were carefully
separated and the recurrent laryngeal nerve was protected. However,
in the control group, patients underwent preoperative
high-frequency color ultrasonography, and the surgeons cleared the
most suspicious lymph node according to experience. In the
observation group, patients underwent preoperative high-frequency
color ultrasonography, and the surgeons cleared the lymph node of
the widest range. The difference in clinical effects and prognosis
of the two groups were compared.
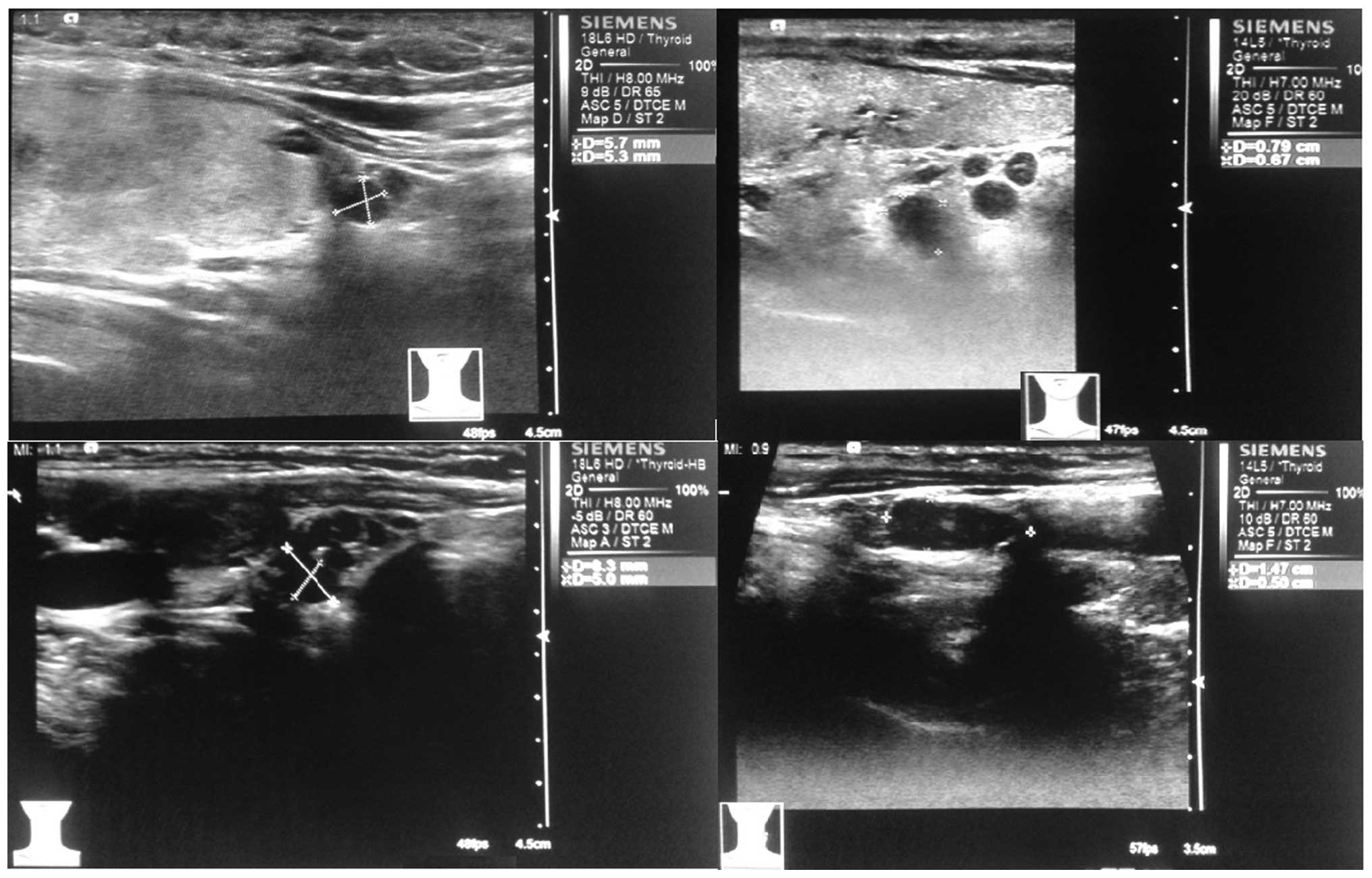
The ultrasound equipment used was Philips IU22 G4
high-frequency Doppler ultrasound with linear array wide-band
probe, and the probe frequency was 7.5–10 MHz. Cervical lymph node
metastasis standard diagnosed by ultrasound were (4): i) Change of aspect in ratio of lymph
nodes >1; ii) irregular blood flow signals with lymph nodes;
iii) irregular or blurred borders; iv) uneven internal echo; v)
internal calcification; vi) unclear cortex and medulla boundaries;
and vii) disappeared or cystic degeneration of hilar structure.
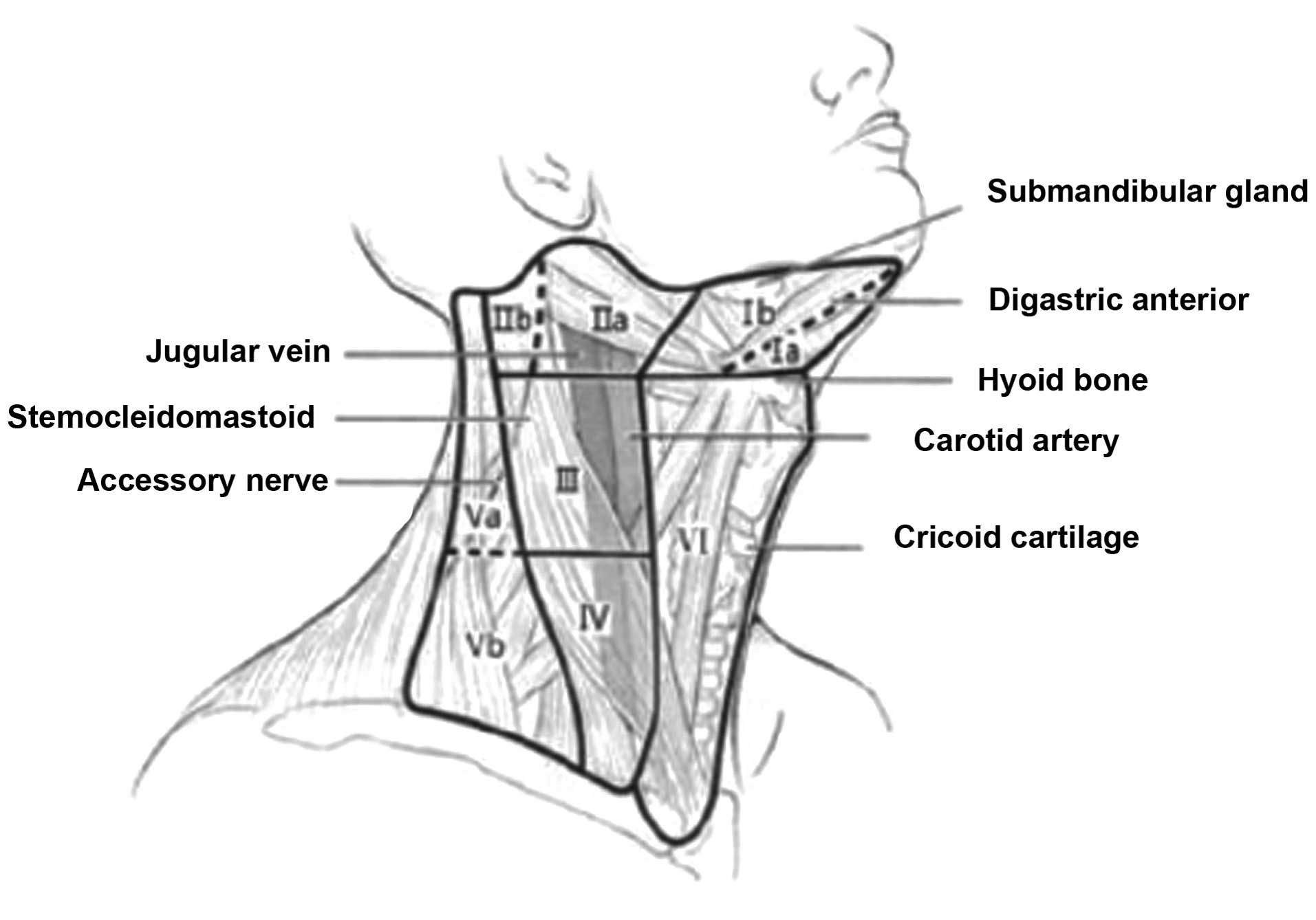
All the operations were performed by two Ultrasound
experts. The ultrasound cervical lymph node partition referred to
the dividing method of lymph nodes in the American Academy of
Otolaryngology-Head and Neck. It was divided into seven areas
(5): area I included submental area
and submandibular lymph nodes, area II contained the internal
jugular vein lymph node group lymph nodes, area III was middle
jugular lymph nodes, area IV was lower jugular lymph nodes, area V
was the carotid triangle jugular lymph nodes, area VI was anterior
jugular lymph nodes (also known as central zone jugular lymph
nodes), area VII was upper mediastinal lymph node (Figs. 1 and 2).
Observation index
The difference between the two groups was analyzed
for tumor recurrence rate and survival rate as well as the rate of
surgery complications after nearly a year's follow-up observation.
After the comparison of the judgement of lymphatic metastases by
preoperative high-frequency color ultrasonic results of definite
diagnoses during surgery in the observation group, we obtained the
sensitivity, specificity, positive predictive value and negative
predictive value of ultrasonic diagnosis.
Statistical analysis
SPSS 20.0 statistical software (IBM SPSS, Armonk,
NY, USA) was used for analysis and data was expressed as mean ±
standard deviation. Comparisons between groups were made using the
t-test. The enumeration data were expressed as percentage (%).
Comparisons between groups were made using the χ2 test.
P<0.05 was considered to indicate a statistically significant
difference.
Sensitivity was calculated as: True positive
listings/(number of true-positive + number of false-negative) ×
100%. Specificity was calculated as: Number of true
negative/(number of true-negative + number of false-positive) ×
100%.
Positive predictive value was calculated as the
number of true positive/(number of true-positive + false positive
number) × 100%, and the negative predictive value was calculated as
the number of true negatives/(true-negative + number of
false-negative number) × 100%. P<0.05 was considered
statistically significant.
Results
Comparison of tumor recurrence rate
and survival rate in the two groups
The tumor recurrence rate of the observation group
was significantly lower than that of the control group and the
survival rate of the observation group was significantly higher
than that of the control group (P<0.05). The recurrence of
tumor, and the time of death, of the two groups was not
statistically significant (P>0.05; Table I).
 | Table I.A comparison of tumor recurrence rate
and survival rate in the two groups [n (%)]. |
Table I.
A comparison of tumor recurrence rate
and survival rate in the two groups [n (%)].
| Group | No. of cases | Tumor recurrence
rate | Recurrence time
(month) | Survival rate | Death (month) |
|---|
| Control | 36 | 11 (30.6) | 10.5±2.3 | 28 (77.8) | 11.6±3.3 |
| Observation | 44 | 5
(11.4) | 11.6±3.4 | 42 (95.5) | 11.9±3.6 |
| t
(χ2) |
| 4.558 | 0.624 | 4.156 | 0.925 |
| P-value |
| 0.033 | 0.329 | 0.041 | 0.748 |
Comparison of the rate of surgery
complications
The rate of surgery complications and comparative
difference of the two patient groups was not statistically
significant (P>0.05) as shown in Table II.
 | Table II.Comparison of the rate of surgery
complications [n (%)]. |
Table II.
Comparison of the rate of surgery
complications [n (%)].
| Group | No. of cases | Parathyroid
injury | Recurrent laryngeal
nerve | Superior laryngeal
nerve | Others | Rate of surgery
complications |
|---|
| Control | 36 | 3 | 4 | 1 | 1 | 9 (25.0) |
| Observation | 44 | 5 | 5 | 1 | 2 | 13 (29.5) |
| t
(χ2) |
|
|
|
|
| 0.205 |
| P-value |
|
|
|
|
| 0.651 |
Comparison of the judgement of
lymphatic metastases by preoperative high-frequency color
ultrasonography with results of definite diagnoses during surgery
in the observation group
A total of 44 patients were included in the
observation group, 38 of whom were diagnosed with lymph node
metastasis during surgery. The 34 cases of metastasis occurred in
area VI (77.3%), the number of metastasis was 1–4 with an average
of 2.3±0.6. The 2 cases of metastasis occurred in area III, 1 case
occurred in area IV, and 1 case occurred in area II. Of the 41
cases of suspicious lymph node removal found in preoperative
ultrasound, 37 cases were true-positive, 4 cases were
fasle-positive and 1 case was false-negative, 2 cases were true
negative, the sensitivity was 97.4%, specificity was 33.3%,
positive predictive value was 90.2% and negative predictive value
was 66.7% (Table II).
Discussion
The basic principle of surgical treatment for cancer
is that patients with lymph node metastasis need to undergo neck
lymph node removal. However, the specificity of DTC biological
behavior and complexity of neck dissection make the surgery highly
risky, during which accidental injury and complications are likely
to happen (6). There is no agreement
on DTC neck lymph node removal, either at home or abroad. Studies
have suggested that the enlarged neck lymph node removal range is
much more likely to increase the risk of recurrent nerve and
parathyroid injury rather than to have tumor recurrence, and the
former leads to severe clinical complications and greatly lower
patients' life quality (7).
Nevertheless, it is undeniable that neck lymph node removal has
become an important factor affecting the prognosis of thyroid
cancer, the prognosis of patients is closely connected with primary
surgical approach and surgical resection. The reasonable surgical
approach can effectively reduce recurrence rate and reoperation
rate (8).
Papillary thyroid carcinoma is the most typical
tumor that mainly spreads to lymph node. Unilateral or bilateral
carcinoma spreads to regional lymph nodes (9), and 20–90% patients with papillary
carcinoma are detected with regional lymph node metastasis during
diagnosis and the distant hematogenous metastasis only occurs in
the later period (10). However,
tumor of follicular thyroid mainly spreads through hematogenous
metastasis. The rules and treating principle of neck lymph node
metastasis are similar to that of papillary thyroid carcinoma
(11). Central area (area VI) is the
first station of lymph node metastasis manifested by paratracheal
and pretracheal lymph node metastasis in ipsilateral neck central
region (12). It is rare to have
cases in which no metastasis occurs in the central area while
saltatory metastasis to the lateral neck can be found under a
microscope (13). However, when tumor
spreads to lymph gland of lateral neck, lymph nodes in area II–V
are considered to be infringed. Tumor generally spreads to multiple
human regions rather than single region (14). With continuous application of
high-frequency color ultrasonography and drawing on exprience, the
accuracy of preoperative judgment of whether tumor metastasis
occurs and the scope of metastasis is continuously improving
(15). In the observation group, by
comparing the judgement of lymphatic metastases by preoperative
high-frequency color ultrasonic results of definite diagnoses
during surgery, we found that the sensitivity was 97.4%,
specificity was 33.3%, positive predictive value was 90.2% and
negative predictive value was 66.7%. To determine the criteria of
neck lymph metastasis and neck lymph areas by color
ultrasonography, there was a high degree of sensitivity and
positive predictive value. Furthermore, ultrasonography is worthy
of wide use due to its simple operations and reasonable price
(16). The reason for insignificant
specificity was connected to multiple factors, namely, the diameter
of the primary tumor, the location of lymph node, patient's
somatotype and the examiners' level of experience (17).
The study indicated that the tumor recurrence rate
of the observation group was significantly lower than that of the
control group and the survival rate of the observation group was
significantly higher than that of the control group. The DTC
spreads to lymph gland at a later time with low degree of
malignancy and high excision rate and its prognosis is excellent.
However, DTC is silent which leads to tumor recurrence and
pro-metastasis of lymph node occurs in latter period after surgery.
Moreover, surgical stimulation and disseminated lesions are risk
factors for tumor recurrence (18).
The study is not only concerned with papillary carcinoma but also
follicular carcinoma, increasing the postive rate of results.
In comparison to previous studies, which only
focused on papillary carcinoma with lower malignancy, the study has
greater realistic significance. Some studies supported that
follicular carcinoma and differentiated carcinoma with diameter
more than 1 cm should undergo prophylactic lymphadenectomy
(19). The comparison of surgery
complications rate of two patient groups has no statistical
significance. Currently, the application of tracers (e.g.,
methylene blue and nano carbon) and microtechniques can identify
the parathyroid and lymph nodes, and retain the parathyroid tissue
and blood supply provided complete excision in surgery, thus
reducing the possibility of postoperative hypocalcemia symptoms
(20).
In summary, to decide on removal and removal range
of the lymph node for DTC patients having undergone thyroid tissue
excision with preoperative high-frequency color ultrasonography can
be highly accurate and beneficial to improving effects and reducing
the recurrence rate, thus it is of great clinical significance.
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Carty SE, Cooper DS, Doherty GM, Duh QY,
Kloos RT, Mandel SJ, Randolph GW, Stack BC Jr, Steward DL, Terris
DJ, et al: American Thyroid Association Surgery Working Group;
American Association of Endocrine Surgeons; American Academy of
Otolaryngology-Head and Neck Surgery; American Head and Neck
Society: Consensus statement on the terminology and classification
of central neck dissection for thyroid cancer. Thyroid.
19:1153–1158. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cooper DS, Doherty GM, Haugen BR, Kloos
RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F,
Schlumberger M, et al: American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer: Revised American Thyroid Association management guidelines
for patients with thyroid nodules and differentiated thyroid
cancer. Thyroid. 19:1167–1214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rotstein L: The role of lymphadenectomy in
the management of papillary carcinoma of the thyroid. J Surg Oncol.
99:186–188. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yüce I, Cağli S, Bayram A, Karasu F and
Güney E: Regional metastatic pattern of papillary thyroid
carcinoma. Eur Arch Otorhinolaryngol. 267:437–441. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pisello F, Geraci G, Lo Nigro C, Li Volsi
F, Modica G and Sciumè C: Neck node dissection in thyroid cancer. A
review. G Chir. 31:112–118. 2010.PubMed/NCBI
|
|
7
|
Vergez S, Sarini J, Percodani J, Serrano E
and Caron P: Lymph node management in clinically node-negative
patients with papillary thyroid carcinoma. Eur J Surg Oncol.
36:777–782. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ferlito A, Robbins KT, Silver CE, Hasegawa
Y and Rinaldo A: Classification of neck dissections: An evolving
system. Auris Nasus Larynx. 36:127–134. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hughes DT and Doherty GM: Central neck
dissection for papillary thyroid cancer. Cancer Control. 18:83–88.
2011.PubMed/NCBI
|
|
10
|
Moo TA and Fahey TJ III: Lymph node
dissection in papillary thyroid carcinoma. Semin Nucl Med.
41:84–88. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Clark OH: Thyroid cancer and lymph node
metastases. J Surg Oncol. 103:615–618. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang B, Niu HM, Wu Q, Zhou J, Jiang YX,
Yang X, Li JC, Zhao RN, Wang M, Li KN, et al: Comparison of
clinical and ultrasonographic features of poorly differentiated
thyroid carcinoma and papillary thyroid carcinoma. Chin Med J
(Engl). 129:169–173. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Barbu CG, Florin A, Neamţu MC, Avramescu
ET, Terzea D, Miron A, Dănciulescu Miulescu R, Poiană C and Fica S:
Papillary thyroid carcinoma with anaplastic dedifferentiation in
the lymph node metastasis - a rare form of presentation even for a
tall cell variant. Rom J Morphol Embryol. 56:527–531.
2015.PubMed/NCBI
|
|
14
|
Wang Q, Zhu X and Tan Z: The clinical
significance of the Delphian lymph node metastasis in papillary
thyroid carcinoma. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi.
29:378–381. 2015.(In Chinese). PubMed/NCBI
|
|
15
|
Liang XN, Guo RJ, Li S, Zheng ZM and Liang
HD: Binary logistic regression analysis of solid thyroid nodules
imaged by high-frequency ultrasonography, acoustic radiation force
impulse, and contrast-enhanced ultrasonography. Eur Rev Med
Pharmacol Sci. 18:3601–3610. 2014.PubMed/NCBI
|
|
16
|
Ying M, Bhatia KS, Lee YP, Yuen HY and
Ahuja AT: Review of ultrasonography of malignant neck nodes:
Greyscale, Doppler, contrast enhancement and elastography. Cancer
Imaging. 13:658–669. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Isik S, Akbaba G, Berker D, Tutuncu YA,
Ozuguz U, Aydin Y, Peksoy I and Guler S: Thyroid-related factors
that influence preoperative localization of parathyroid adenomas.
Endocr Pract. 18:26–33. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lee CW, Gong G and Roh JL: Intraoperative
diagnosis of central compartment lymph node metastasis predicts
recurrence of patients with papillary thyroid carcinoma and
clinically node-negative lateral neck and may guide extent of
initial surgery. World J Surg. 39:194–202. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li ZJ, An CM, Yan DG, Zhang XW, Zhang ZM,
Xu ZG and Tang PZ: Significance of selective neck dissection in
patients with cN0 thyroid carcinoma. Zhonghua Zhong Liu Za Zhi.
35:783–786. 2013.(In Chinese). PubMed/NCBI
|
|
20
|
Chaojie Z, Shanshan L, Zhigong Z, Jie H,
Shuwen X, Peizhi F, Jing X, Xiaowen G, Yang L and Wei Z: Evaluation
of the clinical value of carbon nanoparticles as lymph node tracer
in differentiated thyroid carcinoma requiring reoperation. Int J
Clin Oncol. 17:32–34. 2015.
|