Introduction
Carcinoma of the uterine cervix is the fourth most
common female malignancy globally, following breast, colorectal and
lung cancers (1). In developed
countries, including the USA, ~12,900 women are diagnosed with
cervical cancer and ~4,100 mortalities per year are attributed to
this disease (2). The 5-year overall
survival rate is 68% for all stages of cervical cancer; however,
the survival rate is 91% when the disease is diagnosed in an early
phase. Patients with metastases in regional lymph nodes only have a
57% 5-year survival rate, and those with distant metastases only
have a 16% 5-year survival rate. The overall 5-year survival rate
is relatively high in Korea (80–81.2% over the last 15-year period)
(3). Increased cancer screening and
updated treatment strategies are key factors that have produced
improved results (4). Specifically,
the survival of women with recurrent cervical cancer or para-aortic
lymph node (PAN) metastasis remains poor. More effective treatment
methods and regimens are therefore needed. Cisplatin is an
effective single therapeutic regimen for first-line therapy, but
single-agent regimens for recurrent cervical cancer have a poor
response rate (only 13%) (5). The
recurrence rate is lower for patients with a pelvic recurrence
within previously irradiated areas than for those with extra-pelvic
sites of disease. In addition, the responsiveness of pelvic
recurrences is partial at best and has a brief (median 4–6 months)
duration (6). To enhance the
therapeutic response, chemotherapy was combined with hyperthermia
(cisplatin + hyperthermia for previously radiated cases), which has
been demonstrated to be feasible (7)
when used in tri-modal applications for the cervix (8–11). By
using local hyperthermia and systemic administration of
chemotherapy, it is possible to achieve maximum synergism without
increasing the systemic side effects, which primarily affect the
bone marrow and kidneys (12).
Modulated electro-hyperthermia, which was used in the present
study, is a type of hyperthermia used in oncological treatments
that avoids the drawbacks of conventional electromagnetic heating
(13,14). This treatment device is designed to
selectively heat malignant tumors and tumor cells by modularly
delivering 13.56 MHz RF (15–18). This method works by heating the
malignant cells, selectively and effectively acting on the cell
membrane (19), and inducing
apoptotic cell death (20). This
advanced treatment produces damage-associated cellular patterns and
promotes immunogenic cell death (21). The heat-induced increase in the tumor
response to radiotherapy is due, at least in part, to an increase
in the oxygen supply via increased blood circulation in tumors. The
enhanced response of tumors to chemotherapy may be due to three
factors. First, mild heating increases the delivery of chemotherapy
drugs to the tumors by increasing blood flow to and within the
tumor. Second, mild heating increases the cellular uptake of drugs
by increasing cell membrane permeability. Third, heating
facilitates the reaction rate of drugs, which potentiates their
cytotoxicity (21,22).
This method uses modulated radiofrequency for energy
delivery and achieves selective thermal action in non-homogeneous
tissue (23). It is also notably
gentle, and its use on brain malignancies has been successful
(24–26), even at increased doses for advanced
cases (16). Modulated
electro-hyperthermia does not cause pain and has fewer side
effects, which results in improved patient satisfaction and quality
of life (18). Patients treated with
modulate electro-hyperthermia have reported pain relief (23) and, as a result, a decreased dose of
analgesic is required (22). The aim
of the present study was to evaluate the effect of modulated
electro-hyperthermia combined with conventional chemotherapy
compared with chemotherapy alone on recurrent cervical cancer
previously treated with irradiation, by analyzing the outcomes of
patients subjected to each treatment. The objectives of the present
study were to determine the local control, treatment outcome and
side effects.
Materials and methods
Ethics statement
The present study was approved by the Institutional
Review Board of Chonbuk National University Hospital (Jeonju,
Republic of Korea) and was conducted according to the Declaration
of Helsinki regarding biomedical research involving human subjects
and the Guidelines for Good Clinical Practice. Written, informed
consent was obtained from all patients.
Patients
A total of 20 subjects were included in the
chemotherapy only group, and 18 subjects were included in the
chemotherapy combined with modulated electro-hyperthermia group and
all patients underwent treatment at the Chonbuk National University
Hospital (Table I). Patients were
included in the present study if they had histologically confirmed
cervical cancer (histological diagnosis of squamous cell carcinoma
or adenocarcinoma) and if complete remission (CR) was achieved
following first-line treatment. In addition, a patient who
experienced recurrence following surgery and chemo-radiotherapy was
included in the present study. A patient who received
chemo-radiotherapy as primary treatment suffered a relapse; the
tumor was inoperable and radio-refractory following recurrence.
Local metastases were included, for example metastasis of the PANs
or the adjacent pelvic lymph nodes (PLNs), but distant metastases
were excluded. The selected patients were required to have an ECOG
status of ≤3. Patients underwent 36 modulated electro-hyperthermia
sessions and at least 6 months of follow-up. Patients in the
chemotherapy only group had the following indications: 1,
recurrence in a PAN alone or in a PLN and/or the bed of the cervix;
2, no distant metastasis (excluding PANs); 3, radiotherapy was not
possible due to recurrence in a previous radiotherapy field; and 4,
at least 6 months of follow-up.
 | Table I.Characteristics of patients with
recurrent cervical cancer who had previously undergone
chemo-radiotherapy, who were subsequently subjected to chemotherapy
alone or chemotherapy combined with modulated
electro-hyperthermia. |
Table I.
Characteristics of patients with
recurrent cervical cancer who had previously undergone
chemo-radiotherapy, who were subsequently subjected to chemotherapy
alone or chemotherapy combined with modulated
electro-hyperthermia.
| Parameter | Chemotherapy alone
(n=20) | Chemotherapy and
modulated electro-hyperthermia (n=18) |
|---|
| Age, years |
|
|
Range | 36–71 | 36–71 |
| Mean | 53 | 50.8 |
| FIGO stage |
|
|
| Ib | 2 | 3 |
| IIa | 3 | 3 |
| IIb | 3 | 3 |
| IIIa | 5 | 2 |
| IIIb | 4 | 4 |
| IVa | 3 | 3 |
| Pathology |
|
|
| Squamous
cell carcinoma | 15 | 15 |
|
Adenocarcinoma | 5 | 3 |
| Recurrent
lesions |
|
|
| Cervix
bed alone | 4 | 6 |
| PAN
alone | 4 | 4 |
| Iliac LN
alone | 4 | 5 |
| Iliac
LN+cervix bed | 8 | 3 |
Patients in the chemotherapy combined with modulated
electro-hyperthermia group had the following indications: i)
Recurrence in a PAN or PLN and the bed of the cervix (specifically,
in the 30 cm probe treatment area); ii) no distant metastasis
(excluding PANs); iii) 36 sessions of hyperthermia therapy (3
sessions per week); iv) radiotherapy was not possible due to
recurrence in a previous radiotherapy field; and v) at least 6
months of follow-up.
Chemotherapy
All patients received platinum-based chemotherapy
for recurrence according to local hospital policy. The treatment
characteristics are summarized in Table
II. Depending on local hospital policy, the goal of combined
chemotherapy with modulated electro-hyperthermia was to administer
36 sessions of modulated electro-hyperthermia during chemotherapy.
All patients were evaluated for toxicity each week.
 | Table II.Treatment characteristics of the
chemotherapy alone and chemotherapy combined with modulated
electro-hyperthermia groups. |
Table II.
Treatment characteristics of the
chemotherapy alone and chemotherapy combined with modulated
electro-hyperthermia groups.
| Group | TP (cycle) | TC (cycle) | FP (cycle) | Cisplatin
(cycle) |
|---|
| Chemotherapy alone
(n=20) | 8 (5–7) | 6 (6–9) | 6 (4–6) |
0 |
| Chemotherapy and
modulated electro-hyperthermia (n=18) | 6 (5–6) | 4 (6) | 6 (4–6) | 2 (5–6) |
Modulated electro-hyperthermia
Modulated electro-hyperthermia treatment was applied
using an EHY2000 clinical heating device (Oncotherm GmbH,
Troisdorf, Germany) set at a 13.56 MHz carrier frequency, and the
amplitude was modulated according to a time fractal pattern.
Modulated electro-hyperthermia was performed for 60 min. The
patients were placed in a supine position on a water mattress
electrode. A circular upper electrode (30 cm in diameter) was
coupled over the recurrent cervical mass or PAN mass. Prior to
modulated-electro hyperthermia, all patients underwent a
two-dimensional simulation. The treatment field encompassed the
mass with a 3 cm margin in the X, Y, and Z directions. Modulated
electro-hyperthermia was performed three times each week beginning
at the initiation of chemotherapy, and patients underwent a total
of 36 sessions.
The power output was 80 W for the first 10 min, 120
W for the next 10 min and 150 W for the remaining treatment time.
Self-calibration of the device was performed prior to each
treatment (11). The body
temperature, blood pressure and pulse rate of each patient were
measured prior to, during and following treatment. Body temperature
was measured using an infrared ear thermometer (Infrared
Thermometer IRT 4020; Braun GmbH, Kronberg, Germany) and the
temperature of the abdominal skin surface below the circular upper
electrode probe was measured using a non-contact infrared
thermometer transmitter (Thermo Checker DT-060; Easytem Co., Ltd.,
Siheung, Korea). Adverse events (AEs) of the
associated-hyperthermia and chemotherapy were monitored throughout
the present study. Hyperthermia-associated adverse events were hot
sensation, skin burn and gastric discomfort.
Chemotherapy-associated adverse events were pancytopenia, nausea,
vomiting, anorexia and gastric discomfort. AEs were determined by
investigator inquiry and by spontaneous patient reports. The AEs
were recorded with regard to the symptoms, signs, duration and
severity (mild, moderate, and severe). Clinical safety parameters,
including blood glucose levels, vital signs, 12-lead ECG results
and clinical laboratory tests, were observed during the regular
chemotherapy cycles (3–4 weeks intervals).
Statistics
The end points of the present study were tumor
response [CR, partial remission (PR), stable disease (SD) and
progressive disease (PD)], overall survival, final follow-up status
and toxicity. Student's t-test was used for treatment response
analysis.
The time to an event variable was estimated using
Kaplan-Meier analysis. The statistical analysis was performed using
SAS software (version 9.3; SAS Institute, Inc., Cary, NC, USA).
P<0.05 was considered to indicate statistically significant
difference.
Results
The 38 included patients were
evaluated for treatment response
The response rates for the chemotherapy alone group
(n=20) and the chemotherapy combined with modulated
electro-hyperthermia (n=18) are summarized in Table III. For patients diagnosed with
cervical cancer, the time to relapse following curative treatment
was 8.95 months following the first treatment for the chemotherapy
only group and 9.16 months for the combined chemotherapy with
modulated electro-hyperthermia group. The overall response rate
(CR+PR+SD/PD) to treatment was significantly greater in the group
that underwent chemotherapy combined with modulated
electro-hyperthermia (P=0.0461; Table
III).
 | Table III.Clinical response of the
chemotherapy-alone and the chemotherapy-combined with modulated
electro-hyperthermia groups following completion of treatment. |
Table III.
Clinical response of the
chemotherapy-alone and the chemotherapy-combined with modulated
electro-hyperthermia groups following completion of treatment.
| Group | Complete
remission | Partial
response | Stable disease | Progressive
disease | P-value |
|---|
| Chemotherapy alone
(n=20) | 4 | 3 | 1 | 12 | 0.0461 |
| Chemotherapy and
modulated electro-hyperthermia (n=18) | 9 | 2 | 2 | 5 |
|
At the evaluation conducted at the final follow-up
visit, the reaction was significantly greater (P=0.0218; Table IV) in the group that underwent
chemotherapy combined with modulated electro-hyperthermia compared
with the group that underwent chemotherapy alone.
 | Table IV.Analysis of the last follow-up
treatment response to chemotherapy alone or chemotherapy combined
with modulated electro-hyperthermia. |
Table IV.
Analysis of the last follow-up
treatment response to chemotherapy alone or chemotherapy combined
with modulated electro-hyperthermia.
| Group | Complete
remission | Partial
response | Stable disease | Progressive
disease | P-value |
|---|
| Chemotherapy alone
(n=20) | 3 | 3 | 1 | 13 | 0.0218 |
| Chemotherapy and
modulated electro-hyperthermia (n=18) | 9 | 2 | 2 | 5 |
|
In the case of chemotherapy alone, statistically
significant recurrence was only observed when the cervix was the
target of the therapeutic response (P=0.0456), but in the
chemotherapy combined with modulated electro-hyperthermia, no
significant differences between abdominal lymph node and cervical
recurrences were observed (P=0.6199). The follow-up period was 7–21
months (mean 11 months) for the chemotherapy only group and the
follow-up period was 7–28 months (mean 13.5 months) for the
chemotherapy combined with modulated electro-hyperthermia group.
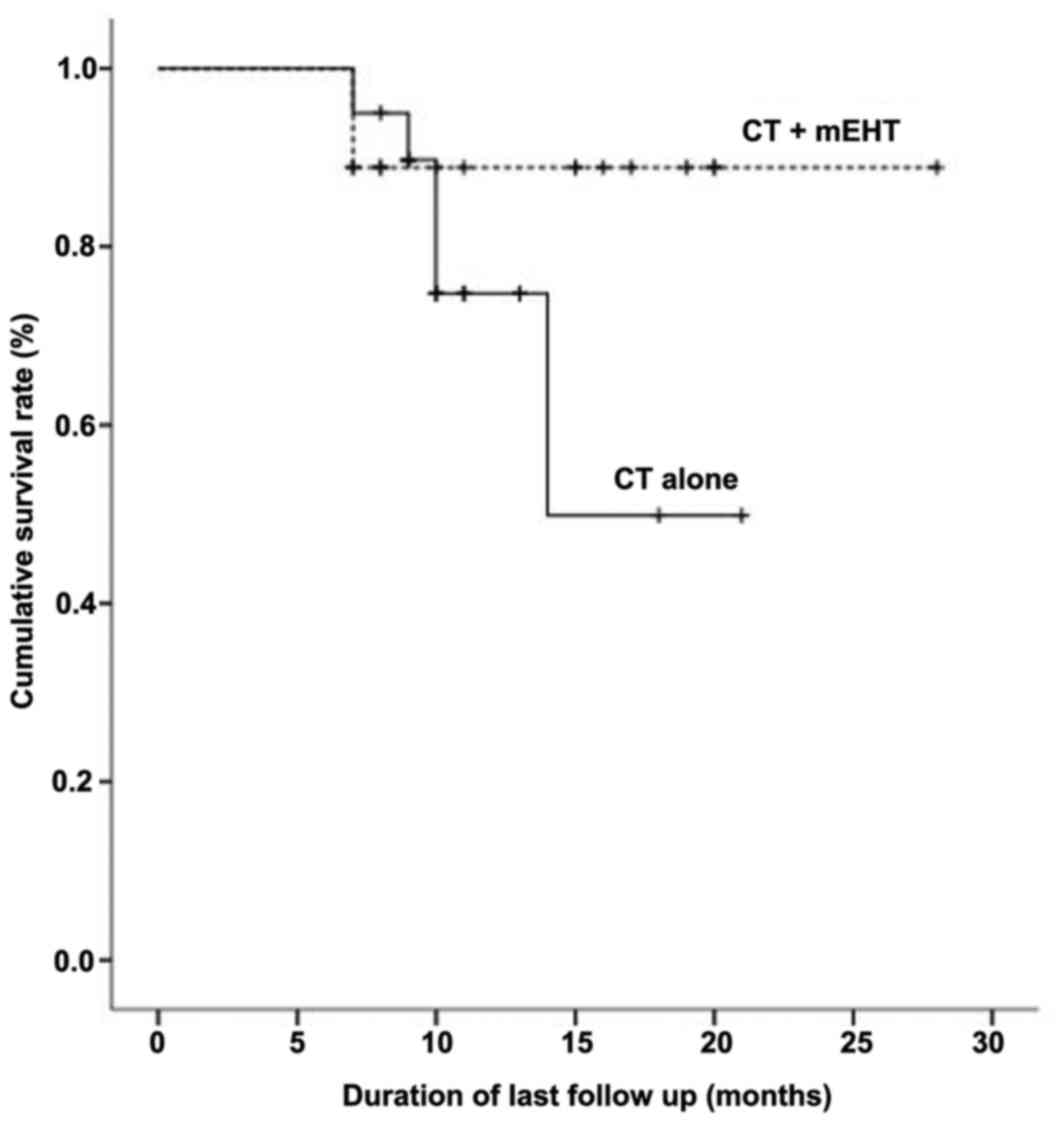
The Kaplan-Meier plot of overall survival is presented in Fig. 1. Based on the overall survival rates
of the two groups, chemotherapy combined with modulated
electro-hyperthermia did not significantly increase disease-free
survival compared with chemotherapy alone (P=0.235).
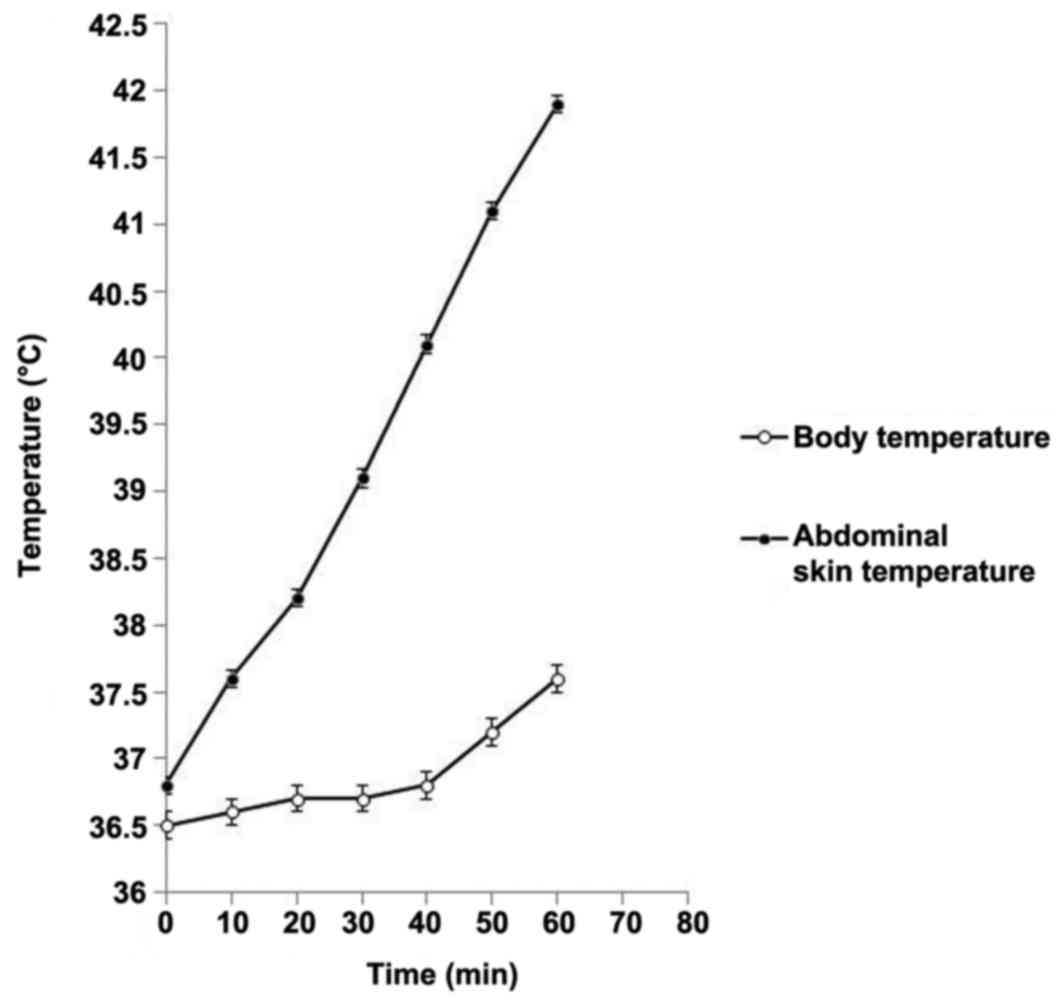
The body temperature ranged from 36.4–36.9°C (mean,
36.5°C) prior to treatment and 36.9–38.2°C (mean, 37.6°C) following
modulated electro-hyperthermia indicating an average increase of
1.1°C. The temperature of the abdominal skin surface below the
upper electrode ranged from 36.4–37.3°C (mean, 36.8°C) prior to
heating, and increased to 39.8–41.9°C (mean, 40.8°C), for an
average surface temperature increase of ~4°C (Fig. 2).
The majority of patients suffered the following
chemotherapy complications: Nausea, vomiting, pancytopenia and
peripheral neuropathy. However, severe chemotherapy-related
complications did not occur. The side effects included hot
sensations and abdominal discomfort for 8/18 (44%) patients, and no
other side effects (burns or blisters) were reported. No late
toxicity associated with modulated electro-hyperthermia was
observed.
The pathological characteristics, chemotherapeutic
regimens, cycles, dosages and ages were not significantly different
with respect to treatment response.
Discussion
Surgery, chemotherapy, radiotherapy, or a
combination of these modalities continues to be the primary
treatment option for invasive cervical cancer. However, following
surgery and postoperative radiotherapy, primary definitive
concurrent chemo-radiation therapy or radiotherapy alone results in
the development of recurrent pelvic disease in up to 40% of
patients. With the exception of salvage surgery as a treatment
option for certain individuals among these patients, the use of
systemic chemotherapy is the only remaining treatment modality
(27). Cisplatin has emerged as the
most active single agent for treating patients with metastatic
disease, and no other standard cytotoxic drug has been consistently
associated with objective response rates of ≥25%. However, for
patients who experience relapse following definitive radiation
therapy, cisplatin has only a minor effect (6,28).
In a study by Potter et al (29), the complete response rate to cisplatin
in patients with distant metastases was 53% with an overall
response rate of 73%, whereas no complete responses and only 7
partial responses (21%) were observed among 33 patients with
localized pelvic recurrence or persistent disease. Thus, the
application of deep local hyperthermia along with the systemic
administration of cisplatin appears to be an attractive option in
patients with recurrent pelvic cervical cancer. Once initial
feasibility data regarding the clinical use of cisplatin and local
hyperthermia combination treatment were reported (29), Rietbroek et al (7) published a phase II study of combined
weekly locoregional hyperthermia and systemic cisplatin
administration in patients with previously irradiated recurrent
cervical carcinoma (30). Using a
regimen of 50 mg of cisplatin per week with a one-week interruption
following four cycles for a total of 12 cycles, corresponding to a
projected dose intensity of 40 mg per week, these authors observed
an overall response in 12/23 patients (52%; 95% confidence
interval, 31–73%) (7).
The expectation is that a hyperthermia-induced
increase in temperature may increase blood flow in the targeted
region as a homeostatic response (31,32). An
elevated local temperature (≤40°C) has been demonstrated to
initiate various physical and chemical processes and to ease pain
in patients with cancer (27). Drug
potentiation in target tissues increases the treatment response.
The temperature increase induced by hyperthermia enhances the
reaction rate of a given drug independent of an increase in drug
delivery due to enhanced blood flow, and increases the reaction
rate in target tumor cells, thereby escalating tumor cell death
(18,23). The thermally increased metabolism (the
so-called enhanced chemo-metabolism) associated with hyperthermia
also increases the absorption of cytotoxins (27) and is expected to enhance drug
absorption.
It is well known that heating tumors to mild
temperatures, for example 40–43°C, kills tumor cells and increases
the tumor response of radiotherapy and chemotherapy with various
anti-cancer drugs (33,34). The heat-induced increase in the tumor
response to radiotherapy is due, at least in part, to an increase
in oxygen supply via the heat-induced enhancement of intratumoral
blood circulation. The heat-induced increase in the tumor response
to chemotherapy may be due to the following three factors. First,
mild heating increases the delivery of chemotherapy drugs to tumors
by increasing tumor blood flow. Second, mild heating elevates the
cellular uptake of drugs by increasing cell membrane permeability.
Third, heating facilitates the reaction rate of drugs, which
potentiates their cytotoxicity (27).
It must be noted that the systemic body temperature may increase
when tumors are treated with regional or local hyperthermia
(22). It is therefore likely that
such an increase in body temperature may alter the pharmacokinetics
of chemotherapy drugs when chemotherapy and regional hyperthermia
are concomitantly applied (35).
In the present study, concerning cervical cancer
recurrence in patients previously treated with irradiation,
chemotherapy combined with modulated electro-hyperthermia
significantly increased the treatment response. The overall
response rate (CR+PR+SD/PD) to treatment was significantly improved
among the patients who underwent chemotherapy combined with
modulated electro-hyperthermia compared with those that underwent
chemotherapy alone (P=0.0461). At the evaluation conducted at the
last follow-up visit, the results were significantly improved in
the group that underwent chemotherapy combined with modulated
electro-hyperthermia compared with chemotherapy alone (P=0.0218).
According to the present study, anti-cancer treatment and
hyperthermia may have a synergistic effect.
Specifically, in the case of chemotherapy alone,
significant recurrence was observed only when the cervix was the
target of the therapeutic response (P=0.0456), but in the
chemotherapy combined with modulated electro-hyperthermia group, no
significant differences in abdominal lymph node and cervical
recurrence were observed (P=0.6199). Hyperthermia may therefore be
slightly more effective for the treatment of abdominal lymph node
metastasis.
The present study demonstrated the feasibility and
advantages of chemotherapy combined with hyperthermia, concurrent
with the application of platinum derivatives, for patients with
recurrent cervical cancer who have regional lymph node metastasis.
A longer-term follow-up study is required to compare the
disease-free survival rates of patients.
Acknowledgements
The present study was supported by funds from the
Institute of Clinical Medicine of Chonbuk National
University-Biomedical Research Institute, Chonbuk National
University Hospital.
References
|
1
|
International Agency for Research on
Cancer, . World Health OrganizationLatest world cancer statistics.
IARC; Lyon: 2013
|
|
2
|
American Society of Clinical Oncology
(ASCO), . Cervical cancer: Statistics. http://www.cancer.net/cancer-types/cervical-cancer/statistics
|
|
3
|
Korean statistical information service, .
Statistics Korea. Statistics Korea, Daejeon. 2012, http://kosis.kr
|
|
4
|
Seol HJ, Ki KD and Lee JM: Epidemiologic
characteristics of cervical cancer in Korean women. J Gynecol
Oncol. 25:70–74. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kuo DY, Blank SV, Christos PJ, Kim M,
Caputo TA, Pothuri B, Hershman D, Goldman N, Ivy PS, Runowicz CD,
et al: Paclitaxel plus oxaliplatin for recurrent or metastatic
cervical cancer: A New York cancer consortium study. Gynecol Oncol.
116:442–446. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
de Wit R, van der Zee J, van der Burg ME,
Kruit WH, Logmans A, van Rhoon GC and Verweij J: A phase I/II study
of combined weekly systemic cisplatin and locoregional hyperthermia
in patients with previously irradiated recurrent carcinoma of the
uterine cervix. Br J Cancer. 80:1387–1391. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rietbroek RC, Schilthuis MS, Bakker PJ,
van Dijk JD, Postma AJ, González González D, Bakker AJ, van der
Velden J, Helmerhorst TJ and Veenhof CH: Phase II trial of weekly
locoregional hyperthermia and cisplatin in patients with a
previously irradiated recurrent carcinoma of the uterine cervix.
Cancer. 79:935–943. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jones EL, Samulski TV, Dewhirst MW,
Alvarez-Secord A, Berchuck A, Clarke-Pearson D, Havrilesky LJ,
Soper J and Prosnitz LR: A pilot phase II trial of concurrent
radiotherapy, chemotherapy, and hyperthermia for locally advanced
cervical carcinoma. Cancer. 98:277–282. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tsuda H, Tanaka M, Manabe T, Ikeda H,
Negoro S, Ishiko O and Yamamoto K: Phase I study of combined
radiation, hyperthermia and intra-arterial carboplatin for local
recurrence of cervical cancer. Ann Oncol. 14:298–303. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Westermann AM, Jones EL, Schem BC, van der
Steen-Banasik EM, Koper P, Mella O, Uitterhoeve AL, de Wit R, van
der Velden J, Burger C, et al: First results of triple-modality
treatment combining radiotherapy, chemotherapy, and hyperthermia
for the treatment of patients with stage IIB III, and IVA cervical
carcinoma. Cancer. 104:763–770. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Franckena M, de Wit R, Ansink AC,
Notenboom A, Canters RA, Fatehi D, Van Rhoon GC and Van Der Zee J:
Weekly systemic cisplatin plus locoregional hyperthermia: An
effective treatment for patients with recurrent cervical carcinoma
in a previously irradiated area. Int J Hyperthermia. 23:443–450.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Dahl O: Interaction of heat and drugs in
vitro and in vivoThermoradiotherapy and Thermochemotherapy.
Seegenschmiedt MH, Fessenden P and Vernon CC: 1. Springer Verlag;
Berlin: pp. 103–121. 1995, View Article : Google Scholar
|
|
13
|
Hegyi G, Szigeti GP and Szász A:
Hyperthermia versus oncothermia: Cellular effects in complementary
cancer therapy. Evid Based Complement Alternat Med.
2013:6728732013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Andocs G, Okamoto Y, Kawamoto K, Osaki T,
Tsuka T, Imagawa T, Minami S, Balogh L, Meggyeshazi N and Szasz O:
Oncothermia basic research at in vivo level: The first results in
Japan. Conference Papers Med. 2013:pp. 1973282013;
|
|
15
|
Szasz A, Vincze G, Szasz O and Szasz N: An
energy analysis of extracellular hyperthermia. Electromagn Biol
Med. 22:103–115. 2003. View Article : Google Scholar
|
|
16
|
Meggyeshazi N, Andocs G, Balogh L, Balla
P, Kiszner G, Teleki I, Jeney A and Krenacs T: DNA fragmentation
and caspase-independent programmed cell death by modulated
electrohyperthermia. Strahlenther Onkol. 190:815–822. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Andocs G, Meggyeshazi N, Balogh L, Spisak
S, Maros ME, Balla P, Kiszner G, Teleki I, Kovago C and Krenacs T:
Upregulation of heat shock proteins and the promotion of damage
associated molecular pattern signals in a colorectal cancer model
by modulated electro-hyperthermia. Cell Stress Chaperones.
20:37–46. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Szasz A: Challenges and solutions in
oncological hyperthermia. Med. 29:1–23. 2013.
|
|
19
|
Fiorentini G, Giovanis P, Rossi S, Dentico
P, Paola R, Turrisi G and Bernardeschi P: A phase II clinical study
on relapsed malignant gliomas treated with electro-hyperthermia. In
Vivo. 20:721–724. 2006.PubMed/NCBI
|
|
20
|
Hager ED, Sahinbas H, Groenemeyer DH and
Migeod F: Prospective phase II trial for recurrent high-grade
malignant gliomas with capacitive coupled low radiofrequency (LRF)
deep hyperthermia. J Clin Oncol. 26:20472008. View Article : Google Scholar
|
|
21
|
Sahinbas H, Grönemeyer DH, Böcher E and
Szasz A: Retrospective clinical study of adjuvant
electro-hyperthermia treatment for advanced brain-gliomas. Dtsch Z
Onkol. 39:154–160. 2007. View Article : Google Scholar
|
|
22
|
Wismeth C, Dudel C, Pascher C, Ramm P,
Pietsch T, Hirschmann B, Reinert C, Proescholdt M, Rümmele P,
Schuierer G, et al: Transcranial electro-hyperthermia combined with
alkylating chemotherapy in patients with relapsed high-grade
gliomas: Phase I clinical results. J Neurooncol. 98:395–405. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Andocs G, Szasz O and Szasz A: Oncothermia
treatment of cancer: From the laboratory to clinic. Electromagn
Biol Med. 28:148–165. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Szasz A: Current status of oncothermia
therapy for Lung cancer. Korean J Thorac Cardiovasc Surg. 47:77–93.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jeung TS, Ma SY, Yu J and Lim S: Cases
that respond to Oncothermia Monotherapy. Conference Papers Med.
2013:pp. 3924802013;
|
|
26
|
Szasz A, Iluri N and Szasz O: Local
hyperthermia in oncology-to choose or not to choose?Hyperthermia.
Huilgol N: InTech; Croatia: pp. 1–82. 2013
|
|
27
|
Gonzalez-Gonzalez D: Thermo-radiotherapy
for tumors of the lower gastro-instenstinal tractThermoradiotherapy
and thermochemiotherapy: Biology, physiology, physics.
Seegenschmiedt MH, Fessenden P and Vernon CC: Springer Verlag;
Berlin: pp. 105–109. 1996, View Article : Google Scholar
|
|
28
|
Brader KR, Morris M, Levenback C, Levy L,
Lucas KR and Gershenson DM: Chemotherapy for cervical carcinoma:
Factors determining response and implications for clinical trial
design. J Clin Oncol. 16:1879–1884. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Potter ME, Hatch KD, Potter MY, Shingleton
HM and Baker VV: Factors affecting the response of recurrent
squamous cell carcinoma of the cervix to cisplatin. Cancer.
63:1283–1286. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Green DM, Burton GV, Cox EB, Hanson D,
Moore J and Oleson JR: A phase I/II study of combined cisplatin and
hyperthermia treatment for refractory malignancy. Int J
Hyperthermia. 5:13–21. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Song CW: Effect of local hyperthermia on
blood flow and microenvironment: A review. Cancer Res. 44 10
Suppl:4721s–4730s. 1984.PubMed/NCBI
|
|
32
|
Hegyi G, Vincze G and Szasz A: On the
dynamic equilibrium in homeostasis. Open J Biophys. 2:64–71. 2012.
View Article : Google Scholar
|
|
33
|
Urano M, Kuroda M and Nishimura Y: For the
clinical application of thermochemotherapy given at mild
temperatures. Int J Hyperthermia. 15:79–107. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Urano M, Wong KH, Reynolds R and Begley J:
The advantageous use of hypoxic tumour cells in cancer therapy:
Identical chemosensitization by metronidazole and misonidazole at
moderately elevated temperatures. Int J Hyperthermia. 11:379–388.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Heijkoop ST, van Doorn HC, Stalpers LJ,
Boere IA, van der Velden J, Franckena M and Westermann AM: Results
of concurrent chemotherapy and hyperthermia in patients with
recurrent cervical cancer after previous chemoradiation. Int J
Hyperthermia. 30:6–10. 2014. View Article : Google Scholar : PubMed/NCBI
|