Introduction
Renal cell carcinoma (RCC) accounts for 2–3% of
cancer cases worldwide (1). The
majority of patients with RCC are aged >60 years, and the known
risk factors for the disease include cigarette smoking, obesity,
high blood pressure, advanced renal disease that requires dialysis,
male gender and certain germ line mutations; however, hormonal
changes, analgesic abuse, viral hepatitis or exposure to
trichloroethylene, cadmium and other potential carcinogens are
controversial with respect to their role in RCC risk (2–5). The
majority of cases of RCC are sporadic, whereas hereditary forms
comprise only 2–3% of all cases (6).
The most common subtypes of RCC are clear cell RCC (70–75% of
cases), papillary RCC (10–16%) and chromophobe RCC (5%), which
primarily metastasize to the lung, liver, bones and brain (7). Patients with RCC are usually
asymptomatic and are often coincidentally diagnosed during an
imaging procedure; as a result, 25–30% of patients already have
metastatic RCC (mRCC) at the time of diagnosis (8). Although the number of available
treatment options has increased, the survival of patients with mRCC
remains poor. As RCCs rarely respond to chemotherapy or radiation,
the therapeutic options predominantly include surgical
interventions and immunomodulatory approaches. These include
treatment with cytokines, such as interferon (IFN)-α and
interleukin-2(IL-2). Novel treatments, referred to as targeted
therapies, include various tyrosine kinase inhibitors (TKIs), such
as sunitinib, sorafenib, pazopanib and axitinib, as well as the
monoclonal antibody bevacizumab, which each act on different
pathways that inhibit tumor angiogenesis (9). Alternatively, drugs that inhibit
mammalian target of rapamycin, such as temsirolimus or everolimus,
may be used as targeted therapies in patients with mRCC.
In their treatment guidelines for RCC, the European
Association of Urology concluded that metastasectomy remains the
most adequate local treatment for mRCC, with the exception of cases
of brain and bone metastases, which are more likely to benefit from
radiotherapy in terms of symptomatic relief (2). In cases in which systemic treatment is
necessary, the TKI sunitinib is one of the first-line treatments
(10–15).
Little is known about the specific effects of
sunitinib on the immune system in different individuals. However,
the interaction of sunitinib with the natural killer (NK) cells in
the patient is of particular interest (16). NK cells are able to mediate antitumor
effects and have thus been used for NK cell adoptive therapy in
recent clinical trials (17). NK
cells have further been reported as key players in TKI-mediated
off-target effects on the immune system (18–20).
In the current study, blood samples from three
patients with mRCC who underwent treatment with sunitinib were
analyzed. In addition, blood samples from age-matched, healthy
controls were analyzed, and a comparison of leukocyte counts and
immune statuses of T, B and NK cells was conducted. Furthermore,
functional in vitro analyses were performed to investigate
whether NK cells may be affected by sunitinib treatment.
Materials and methods
Patients and sample preparation
The current immunomonitoring study was approved by
the ethics committee of the Friedrich-Alexander University
Erlangen-Nuremberg (Erlangen, Germany), according to the
Declaration of Helsinki (approval no. 4146). All patients provided
written informed consent.
Samples (10–20 ml heparinized peripheral blood) were
collected from 3 patients between June 2010 and June 2011. The
inclusion criteria for patients included a minimum age of 18 years
and a confirmed mRCC diagnosis. The samples were collected prior to
TKI administration (day 0) and then at 3–5, 8–10, 17–23 and 48 (1
patient only) weeks after the start of TKI treatment. Of the 3
patients, 2 were followed-up subsequent to the termination of TKI
therapy. Peripheral blood mononuclear cells (PBMCs) were isolated
from the samples by density gradient centrifugation (Pancoll human;
Pan-Biotech GmbH, Aidenbach, Germany).
Control group characteristics
The control group consisted of four healthy
individuals with an age range of 44–60 years. These individuals
were monitored over 91 days. Blood samples were obtained on days 0,
60 and 91.
Flow cytometry
The following mouse anti-human monoclonal antibodies
and antibody conjugates were used in different panels: Anti-T-cell
receptor α/β-allophycocyanin (APC; dilution, 1:100; cat. no.,
130-091-237) and anti-cluster of differentiation (CD) 335-APC
(dilution, 1:30; cat. no., 130-092-609; Miltenyi Biotec GmbH,
Bergisch Gladbach, Germany); anti-CD4-phycoerythrin (PE) -Cy7
(dilution, 1:100; cat. no., 557852), streptavidin-APC-Cy7
(dilution, 1:500; cat. no., 554063), anti-CD314-biotin (dilution,
1:50;cat. no., 552866) andanti-CD127-PE (dilution, 1:300;cat. no.,
557938; BD Pharmingen, San Diego, CA, USA);anti-CD25-PE (dilution,
1:60; cat. no., 341,011), anti-CD336-PE (dilution, 1:50; cat. no.,
558563), anti-CD8-peridinin chlorophyll (PerCP; dilution, 1:100;
cat. no., 345774), anti-CD117-PerCP-Cy5.5 (dilution, 1:50; cat.
no., 333950), anti-CD19-V450 (dilution, 1:300; cat. no., 560353)
and anti-CD3-V450 (dilution, 1:200;cat. no., 560366;BD Biosciences,
Franklin Lakes, NJ, USA), anti-CD3-APC-Cy7 (dilution, 1:300; cat.
no., 300318), anti-CD16-PE-Cy7 (dilution, 1:300; cat. no., 302016),
anti-CD19-PerCP (dilution, 1:50; cat. no., 302228), anti-CD107a-PE
(dilution, 1:10; cat. no., 328608), anti-CD56-fluorescein
isothiocyanate (FITC; dilution, 1:50; cat. no., 318304)
andanti-CD19-PE-Cy7 (dilution, 1:100; cat. no., 302216; Biolegend,
Inc., San Diego, CA, USA); anti-CD27-FITC (dilution, 1:70; cat. no.
MHCD2701) and anti-CD45-PE (dilution, 1:200; cat no., MHCD4504;
Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA)
andanti-CD159a-biotin (dilution, 1:30; cat. no., PNIM2750; Beckman
Coulter, Inc., Brea, CA, USA).
A total of 2×106 PBMCs with antibodies
were incubated for 10 min at 4°C in the dark for each staining
procedure. The PBMCs were then washed with phosphate-buffered
saline (PBS) for 4 min and then suspended in PBS. Staining with
DAPI was performed directly prior to cytometric analysis (dilution,
1:6,000, 4°C, 2 min) to identify dead cells and isotype controls
(IgG1-PE, IgG2a-FITC, IgG1-PerCP) were performed prior to analyzing
the samples with fluorescence-activated cell sorting (FACS). The
samples were examined using a BDFACSCanto II™ (BD Biosciences) with
three lasers (488, 633 and 405 nm). The experiment was repeated at
least five times before the start of analyzing patients' data, and
then performed once with each patient sample. Data were analyzed by
FlowJo 7.6.5 software (FlowJo, LLC, Ashland, OR, USA).
Functional in vitro assays
To determine the activity of NK cells, the extent of
degranulation was evaluated by CD107a staining following the
incubation of whole blood samples with target cells. Cells from the
human MHC-I deficient erythroleukaemic cell line K562 (American
Type Culture Collection, Manassas, VA, USA) were used as the target
cells. The cells were maintained in Iscove's modified Dulbecco's
medium (Invitrogen; Thermo Fisher Scientific, Inc.) containing 10%
FCS (Invitrogen; Thermo Fisher Scientific, Inc.) and 1%
penicillin/streptomycin.
A total of 200 µl from the heparinized whole blood
samples was incubated with 2×105 K562 target cells for 3
h at 37°C, as previously described by Claus et al (21). Erythrocyte lysis was then performed in
an ammonium-chloride-potassium buffer for 10 min at 4°C; the lysis
procedure was repeated 2–3 times for each sample. In order to stain
the cells for FACS, PBMC were incubated with anti-CD107a-PE,
anti-CD3-APC-Cy7, anti-CD19-PerCP, anti-CD56-FITC, anti-CD16-PE-Cy7
or anti-CD335-APC (as described in the Flow Cytometry section) for
10 min at 4°C. Staining with DAPI was performed, as previously
described, to identify dead cells. For each patient at each time
point, the extent of CD107a degranulation was measured in
triplicate. To serve as a control for spontaneous degranulation,
PBMCs from the samples were incubated without target cells. The
FACS data were analyzed using FlowJo 7.6.5 software; the NK cell
population was characterized as CD56+, CD3−
and CD19−, once dead cells and doublets had been
excluded. The mean CD56+ and CD107a+values of
three repetitions of the experiment and the control were then
presented in the figures.
To measure IFN-γ production, 2×105
freshly isolated PBMC were treated with 100 U/ml or 1,000 U/ml IL-2
(Novartis International AG, Basel, Switzerland) for 24 h in a
96-well round bottom microplate (BD Biosciences) with 200 µl cell
culture medium. Supernatants were removed to determine IFN-γ
concentration with an ELISA kit (BD OptEIA™ Set; BD Biosciences).
Control samples were incubated without IL-2. For each condition
(control, 100 U/ml IL2 and 1,000 U/ml IL2) triplicates were
performed.
Statistical methods
All analyses were performed using Prism software
(GraphPad Software, Inc., La Jolla, CA, USA). Statistical
significance was calculated with the Mann-Whitney U-test. P<0.05
was considered to indicate a statistically significant
difference.
Results
Patient characteristics
Three patients with advanced mRCC were selected for
a case study; these patients were patients A, B and C (Table I). Patient A, a 60-year-old male,
presented with clear cell RCC of stage T3b-N2-M1, with peritoneal
carcinomatosis and pulmonary, osseous and muscular metastases.
Patient B, a 63-year-old male, experienced multiple osseous,
pulmonary, and chest wall metastases from a clear cell RCC. Patient
C, a 68-year-old female, presented with a stage pT3a-pNx-cM1 clear
cell RCC with sarcomatoid features, as well as multiple pulmonary
and mediastinal lymph node metastases.
 | Table I.Characteristics of three selected
patients with metastatic RCC. |
Table I.
Characteristics of three selected
patients with metastatic RCC.
| Patient | Gender | Age, years | Diagnosis | TNM stage | Metastasis | First-line TKI |
|---|
| A | Male | 60 | RCC, clear
cell | T3b-N2-M1 | Osseous,
peritoneal, pulmonary, muscular | Sunitinib |
| B | Male | 63 | RCC, clear
cell | No primary tumor
detectable | Osseous, pulmonary,
chest wall | Sunitinib |
| C |
Female | 68 | RCC, clear cell,
sarcomatoid | pT3a-pNx-cM1 | Pulmonary,
mediastinal lymph nodes | Sunitinib |
All three patients were treated orally with 50 mg of
sunitinib (Sutent®; Pfizer, Inc., New York, NY, USA)
once daily for 4 weeks, followed by a 2-week break, in accordance
with prescribing information. Patient B underwent a dosage
reduction to 37.5 mg daily after 8 weeks due to adverse effects.
Patients B and C experienced disease progression, which led to a
change from sunitinib to sorafenib for patient C on day 98 and to
everolimus for patient B on day 126.
Patients A and B received sunitinib as a first-line
therapy prior to surgery, whereas patient C received sunitinib as a
first-line therapy immediately subsequent to nephrectomy.
Immunomonitoring during treatment with
sunitinib
To evaluate the effects of sunitinib treatment on
the immune system of patients with mRCC, blood samples were
collected at various time points prior to, during and subsequent to
TKI treatment. These samples were analyzed and the following
parameters were compared with those of the control group: Leukocyte
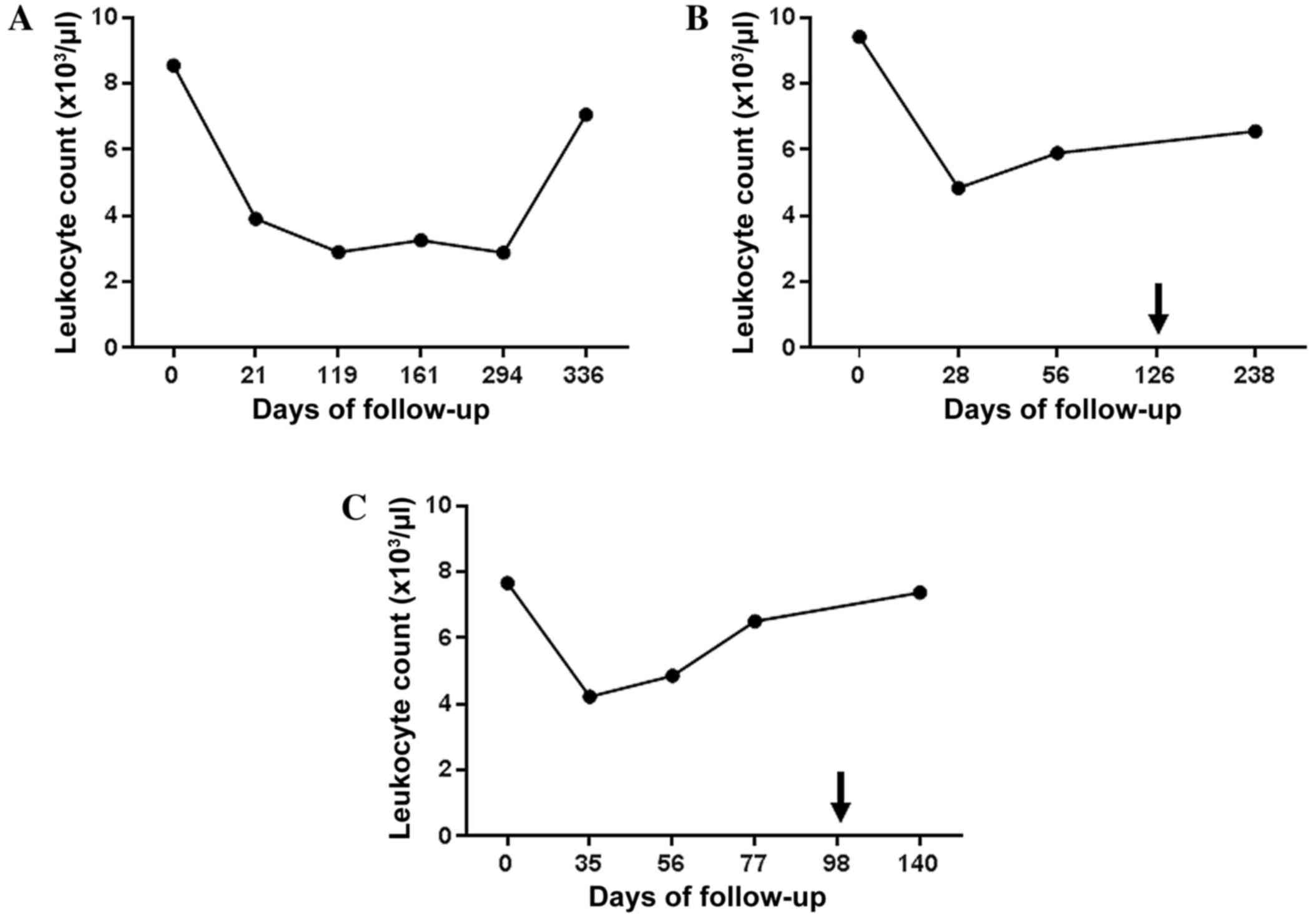
count (Fig. 1); immunomonitoring of
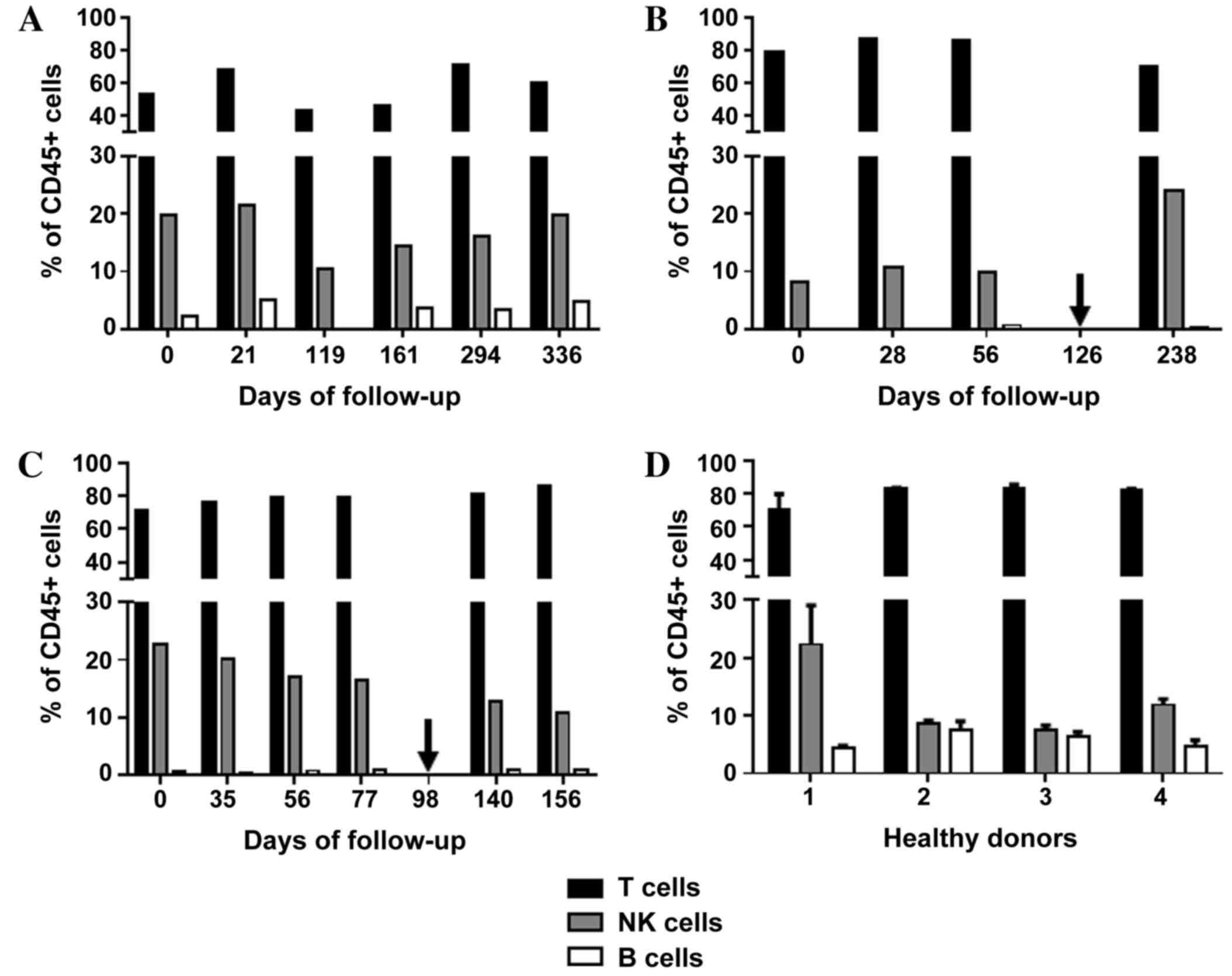
T, B, and NK cells (Fig. 2); ratio of
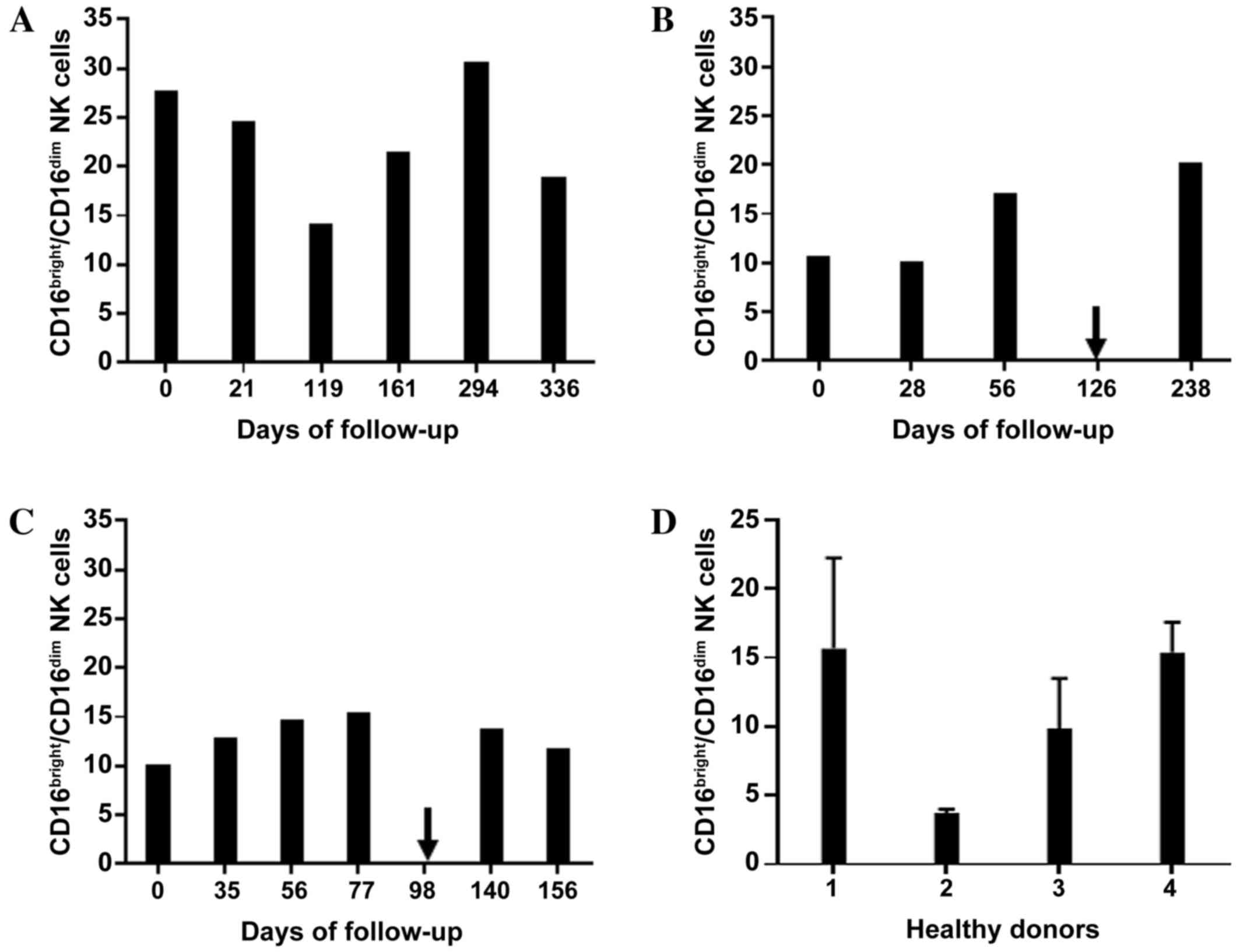
NK cell subsets (CD16bright:CD16dim; Fig. 3); NK cell function, as measured by
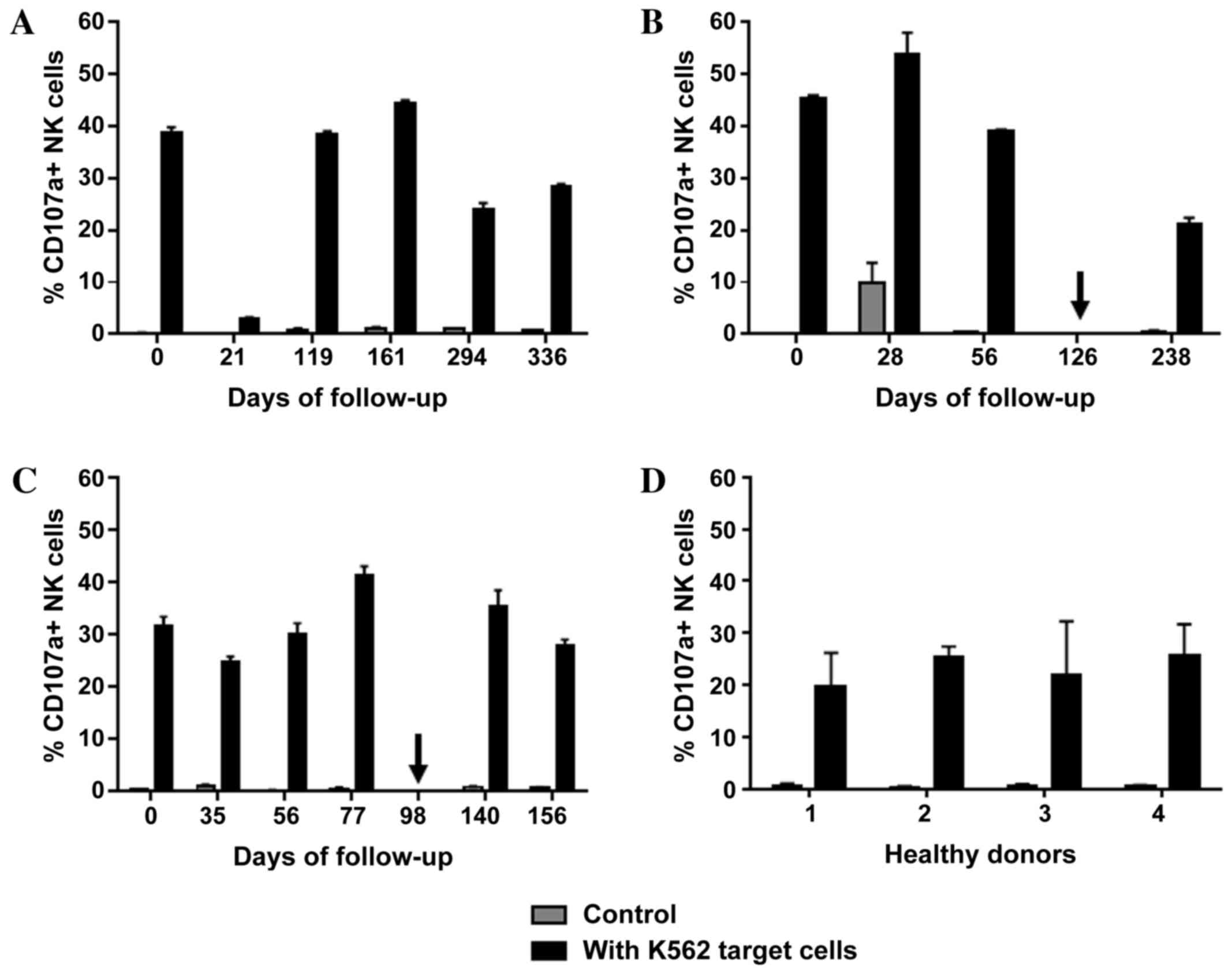
degranulation capacity (Fig. 4) and
IFN-γ production by PBMCs (Fig.
5).
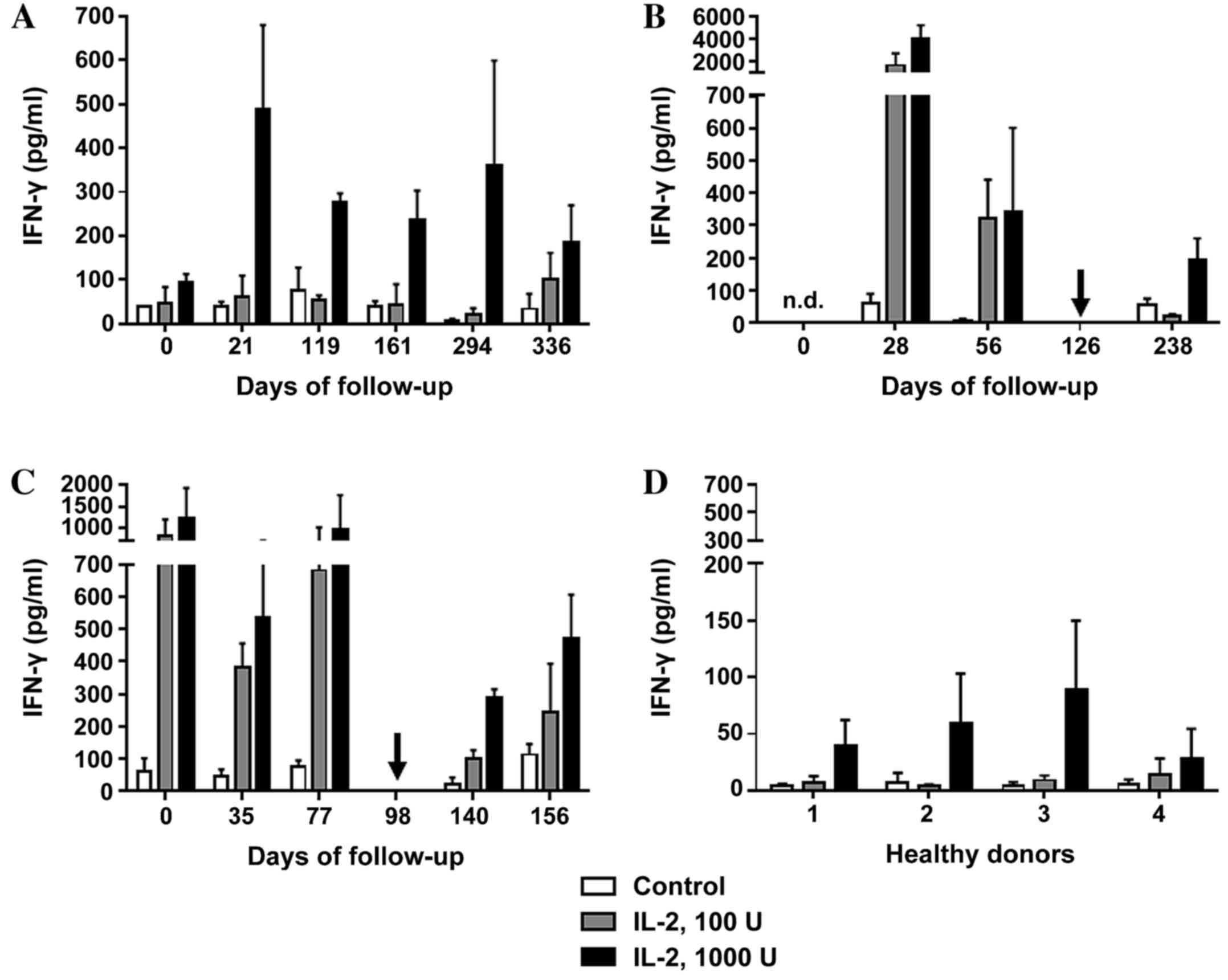
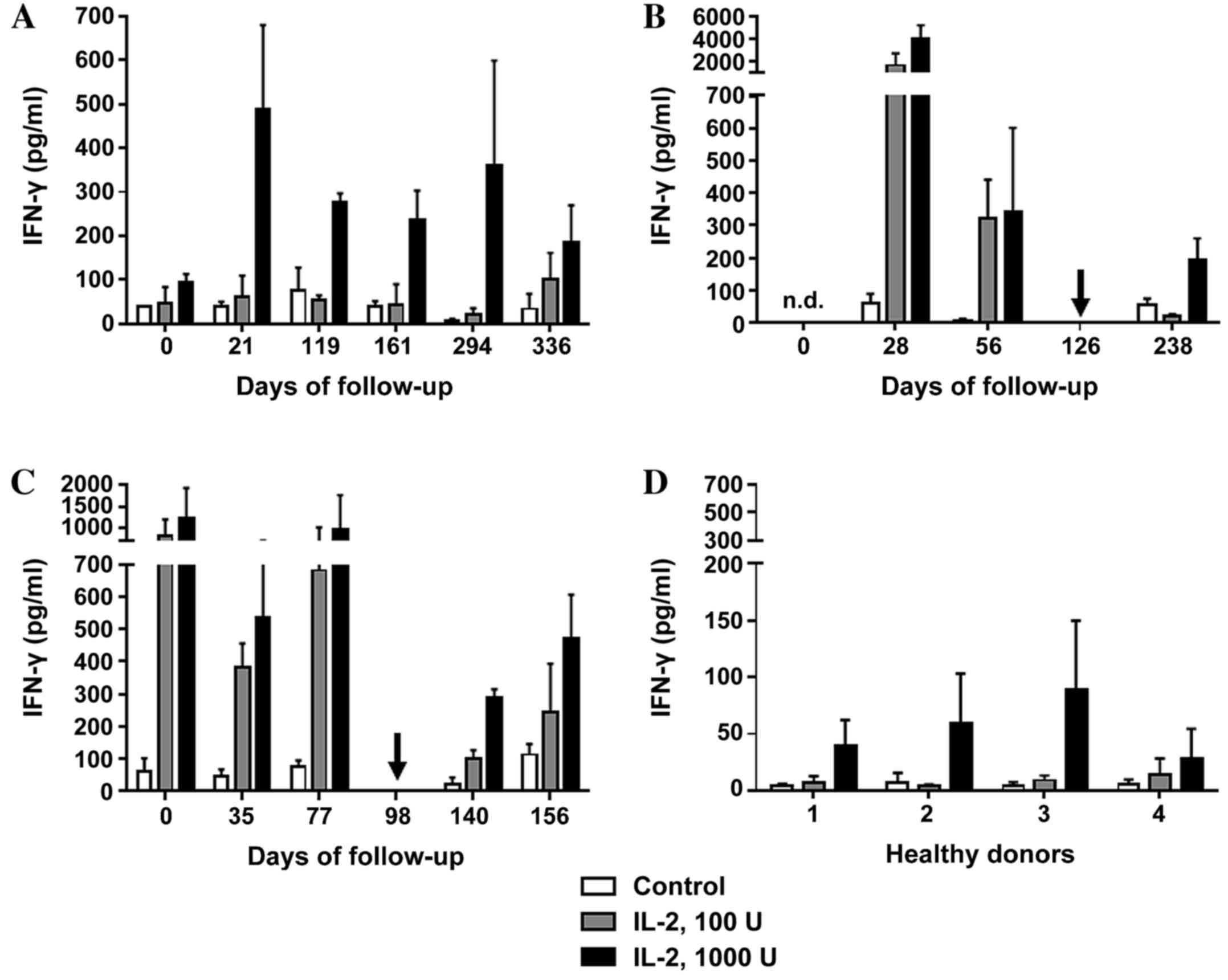 | Figure 5.IFN-γ production by peripheral blood
mononuclear cells. Cells were incubated with 0 U (control), 100 U
or 1,000 U of IL-2, and the concentration of IFN-γ produced was
measured in (A) patient A, (B) patient B and (C) patient C prior
to, during and subsequent to therapy with the tyrosine kinase
inhibitor sunitinib. All data are presented as the mean + standard
deviation from triplicate experiments. Arrows indicate the time
points when the treatment regimen was changed (from sunitinib to
everolimus in patient B, and from sunitinib to sorafenib in patient
C). (D) Measurements of IFN-γ concentration on day 0, 60 and 91 are
included for each of the healthy donor controls (nos. 1–4). IFN-γ,
interferon γ; IL-2, interleukin 2; n.d., no data. |
Patient A
A significant decrease in total leukocyte count from
8.5×103/µl to 3.9×103/µl was observed in
patient A within the first four months of sunitinib therapy, which
then stabilized and began to rise marginally between days 294 and
336 (Fig. 1A). Out of the total
number of lymphocytes, the percentage of T cells fluctuated between
43 and 71% during follow-up. The percentage of B cells marginally
increased between days 0 and 21, and then stabilized slightly
higher than the baseline level from day 161 until the end of the
study. The percentage of NK cells decreased by 50% (from 21.5 to
10.4%) between days 21 and 119 and then recovered to baseline
(Fig. 2A). As shown in Fig. 3A, the ratio of
CD16bright:CD16dim NK cell subsets decreased
between days 0 and 119; however, by day 294, it increased again to
a level higher than that on day 0. NK cell degranulation, which
serves as an indication of NK cell activity, appeared to fluctuate,
although the percentage of CD107a+ cells of the total NK
cell count remained at a higher level than that in the healthy
donor group, with the exception of the values at day 21 (Fig. 4A). The production of IFN-γ by PBMCs
following in vitro stimulation with 1,000 U/ml IL-2
exhibited a significant increase at all time points compared with
the starting point (Fig. 5A).
Patient B
Patient B exhibited a decrease in the total
leukocyte count from 9.4×103/µl to 4.8×103/µl
within the first month of sunitinib treatment. Subsequently, the
total leukocyte count increased during continued sunitinib
treatment; however, it did not reach the initial level measured at
day 0 (Fig. 1B). Out of the total
number of lymphocytes, the percentages of T and NK cells during
sunitinib treatment remained relatively stable at 79–87 and 8–10%,
respectively. However, the percentage of NK cells increased to 24%
when sunitinib treatment ended. The percentage of B cells in this
patient remained low (~0.5%) at all time points (Fig. 2B) compared with the percentages of B
cells in individuals from the healthy donor group (Fig. 2D). The ratio of
CD16bright:CD16dim NK cell subsets increased
from 10.4 on day 0 to 16.9 on day 56, and continued to increase
following the discontinuation of sunitinib treatment (Fig. 3B). NK cell degranulation, as shown in
Fig. 4B, marginally decreased from
45% of CD107a+of the total NK cell count on day 0 to 39%
on day 56, and further decreased to 21% following the
discontinuation of sunitinib treatment and the commencement of
everolimus treatment on day 126. No data are available regarding
IFN-γ production on day 0 as an insufficient number of cells were
obtained to allow for the isolation of PBMCs; however, on day 28,
the production of IFN-γ following in vitro stimulation with
1,000 U/ml IL-2 reached an extremely high level of 3,980 pg/ml.
This value decreased under continued sunitinib treatment and
further decreased following the change in TKI therapy (Fig. 5B).
Patient C
In patient C, a decrease in the total leukocyte
count from 7.6×103/µl to 4.2×103/µl on day 35
of sunitinib treatment was observed. Subsequently, the number
increased, reaching 6.5×103/µl on day 77, which was the
last follow-up time point prior to the end of sunitinib treatment
and the initiation of sorafenib treatment on day 98 (Fig. 1C). Out of the total number of
lymphocytes, the percentage of T cells during and following
sunitinib treatment remained stable at 71–79%, while the percentage
of B cells also remained stable at a low level during the entire
observation period. The percentage of NK cells during treatment
decreased marginally from 22% on day 0 to 16% on day 77. At 5
months after the change in treatment from sunitinib to sorafenib,
the percentage of NK cells had further decreased to 10% (Fig. 2C). The ratio of
CD16bright:CD16dim NK cell subsets increased
continuously from 9.9 on day 0 to 15.3 on day 77, and marginally
decreased again following the change in TKI treatment (Fig. 3C). NK cell degranulation in this
patient, measured as the percentage of CD107a+ NK cells,
reached various values, ranging from 24% (day 35) to 40% (day 77);
this value decreased marginally, compared with that on day 77,
following the change in TKI treatment (Fig. 4C). PBMC-associated IFN-γ production
following in vitro stimulation with 1,000 U/ml IL-2 led to
high IFN-γ values (>200 pg/ml) at baseline and throughout the
sunitinib treatment period (Fig.
5C).
Comparison of patients A, B, and C
with the healthy control group
There was a decrease in the total leukocyte count
from 8.5±0.87×103/µl on day 0 to
4.3±0.48×103/µl after the first month of treatment
within the patient population. Thereafter, leukocyte counts
stabilized and increased again, but did not return to the initial
levels by the end of the observation period (Fig. 1).
In order to assess the relative abundance of
different lymphocyte populations, the means ± SD of all data
throughout the whole observation period were evaluated. The
proportion of T cells in the total number of lymphocytes remained
relatively stable in all patients (patient A, 57.1%±11.5; patient
B, 80.7%±7.6; patient C, 78.9%±5.1) and in the control group
(79.5%±7.4). The proportion of B cells was also relatively stable
in the patient group (patient A, 3.83%±1.1; patient B, 0.5%±0.3;
patient C, 0.8%±0.2). Compared with the control group (5.6%±1.5),
the proportion of B cells was observed to be lower in patient
samples at all time points, including prior to the initiation of
sunitinib treatment. The relative abundance of NK cells was
12.9%±6.9 in the control group and 7–21% in the mRCC group (patient
A, 16.9%±4.1; patient B, 13.2%±7.2; patient C, 16.7%±4.4). There
was a wide range of NK proportions in patients and controls, but no
significant alteration in NK proportion was observed following
sunitinib treatment (Fig. 2).
The ratio of
CD16bright:CD16dim NK cell subsets varied
within the mRCC and the control groups. No trend was identified in
terms of alterations in the NK cell subset ratio during sunitinib
treatment (Fig. 3).
NK cell degranulation, as measured by the percentage
of CD107a-expressing NK cells, was efficiently stimulated by the
incubation with K562 target cells in the mRCC and healthy donor
groups. There was a significant increase of CD107a surface
expression in the mRCC patient and healthy donor samples compared
with the control specimens of the same source incubated without
target cells (co-culture with K562 target cells vs. control without
K562 target cells; P<0.0001; Fig.
4). Within the mRCC group, no significant trend was observed
with regard to NK cell degranulation during sunitinib treatment.
The expression of CD107a after stimulation with K562 cells was
significantly higher at all time points in patients compared with
the healthy donor group (P=0.011). The mean ± SD of all time points
were as follows: Patient A, 34.8%±8.4; patient B, 39.9%±13.8;
patient C, 31.9%±5.8 compared with the healthy donor group
23.2%±2.8 (P=0.011).
PBMC-associated IFN-γ production was efficiently
induced by 24 h of incubation following in vitro stimulation
with 1,000 U/ml IL-2 in the patient and healthy donor groups.
Notably, higher mean values were measured in the patient group
(mean ± SD of all data measured at different time points, as
follows: Patient A, 273±137 pg/ml; patient B, 506±2,144 pg/ml;
patient C, 699±385 pg/ml) compared with the control group (54±27
pg/ml; P<0.001, patients vs. healthy donors treated with 1000
U/ml IL-2; Fig. 5).
Discussion
Within the last two decades, numerous new strategies
have been developed to improve overall survival, quality of life
and disease regression in patients with advanced RCC (1,4–6,16,19), and TKI therapy has been shown to be an
important treatment modality in addressing these objectives
(10,12,13).
Nevertheless, data are limited on how TKIs may interact with the
immune system of an individual patient (16,19). The
present study analyzed the influence of the TKI sunitinib on the
cellular immunity of three patients with mRCC, focusing
specifically on NK cell phenotype and functionality as potential
targets for novel immunomodulatory treatment options.
A decrease in the total leukocyte count was observed
in all patients within the first month of sunitinib therapy;
however, this stabilized and increased again during continuous TKI
treatment. Although patients with mRCC, as compared with healthy
controls, appeared to have a lower percentage of B cells even prior
to treatment, the percentages of T and B cells out of the total
number of lymphocytes remained relatively stable over the
observation period. A decline in the total number of T cells, as
previously demonstrated by Powles et al (22), could not be confirmed in the present
study. The percentages of NK cells were variable within the patient
and control groups. These variations maybe the result of several
factors that inhibit or activate NK cells, such as different
pre-treatment regimens, states of disease or concomitant diseases.
Notably, no elevated infection rate was observed in the
sunitinib-treated patients.
Importantly, in all three patients, NK cell number,
subset distribution, and extent of degranulation did not exhibit
any significant changes that could be associated with sunitinib
treatment. The present study has confirmed in vivo what was
previously demonstrated by Krusch et al (16) in vitro; specifically, there is
no negative influence to NK cells CD107a expression and no decline
in cytokine production, including of IFN-γ, by PBMC when treated
with sunitinib. The enhanced activity rate of PBMC and NK cells
during and prior to therapy with sunitinib may be associated with
the underlying disease mechanics of mRCC. Notably, an increased
activity of the immune system such as elevated secretion of IFN-γ,
IL-2 and IL4, by CD4+ cells in patients with renal
cancer has been described (23–26).
In conclusion, the current case series revealed no
negative impact on NK cell number or function under sunitinib
treatment. B cell percentages appeared to be reduced in the mRCC
patients independently of the sunitinib therapy. B and T cell
counts were not observed to be negatively affected by continued
sunitinib treatment. The limitations of the current study include
the small numbers of mRCC patients and controls. Nevertheless, the
results suggest that treatment strategies involving NK cells, such
as adoptive NK cell transfer (17,19), may
potentially be used in combination with sunitinib and may offer a
feasible treatment option for patients with mRCC in the future.
Further trials are required to evaluate the effects of TKIs in
larger cohorts.
Acknowledgements
The authors would like to thank Dr Irena Kroeger, Dr
Stephanie Gerstner and Ms. Julia Schneider (Department of Internal
Medicine 5, Hematology and Oncology, University Hospital Erlangen,
Friedrich-Alexander University Erlangen-Nuremberg, D-91054
Erlangen, Germany) for their experimental and technical support.
They are also grateful to Dr Sara Tognarelli (LOEWE Center for Cell
and Gene Therapy, Goethe University Frankfurt, Germany) for proof
reading and discussing the manuscript. The authors were supported
by German Cancer Aid (Max Eder Nachwuchsgruppe, Deutsche
Krebshilfe) and by the LOEWE Center for Cell and Gene Therapy
(Frankfurt, Germany), funded by the Hessian Ministry of Higher
Education, Research and the Arts, Germany (grant no. III L
4-518/17.004).
Glossary
Abbreviations
Abbreviations:
|
APC
|
allophycocyanin
|
|
CD
|
cluster of differentiation
|
|
FACS
|
fluorescence-activated cell
sorting
|
|
FITC
|
fluorescein isothiocyanate
|
|
IFN
|
interferon
|
|
IL-2
|
interleukin 2
|
|
NK cells
|
natural killer cells
|
|
mRCC
|
metastatic renal cell carcinoma
|
|
PBMC
|
peripheral blood mononuclear cell
|
|
PE
|
phycoerythrin
|
|
PerCP
|
peridinin chlorophyll
|
|
RCC
|
renal cell carcinoma
|
|
SD
|
standard deviation
|
|
TKI
|
tyrosine kinase inhibitor
|
References
|
1
|
Lyon: Eurocim version 4.0. European
incidence database V2.3, 730 entity dictionary. European Network of
Cancer Registries. 2001.
|
|
2
|
Ljungberg B, Bensalah K, Bex A, Canfield
S, Dabestani S, Hofmann F, Hora M, Kuczyk MA, Lam T, Marconi L, et
al: Guidelines on Renal Cell Carcinoma. Eur Assoc Urol. 2014.
|
|
3
|
Ljungberg B, Campbell SC, Choi HY, Jacqmin
D, Lee JE, Weikert S and Kiemeney LA: The epidemiology of renal
cell carcinoma. Eur Urol. 60:615–621. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rini BI, Campbell SC and Escudier B: Renal
cell carcinoma. Lancet. 373:1119–1132. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Macleod LC, Hotaling JM, Wright JL,
Davenport MT, Gore JL, Harper J and White E: Risk factors for renal
cell carcinoma in the VITAL study. J Urol. 190:1657–1661. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Znaor A, Lortet-Tieulent J, Laversanne M,
Jemal A and Bray F: International variations and trends in renal
cell carcinoma incidence and mortality. Eur Urol. 67:519–530. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shuch B, Amin A, Armstrong AJ, Eble JN,
Ficarra V, Lopez-Beltran A, Martignoni G, Rini BI and Kutikov A:
Understanding pathologic variants of renal cell carcinoma:
Distilling therapeutic opportunities from biologic complexity. Eur
Urol. 67:85–97. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gupta K, Miller JD, Li JZ, Russell MW and
Charbonneau C: Epidemiologic and socioeconomic burden of metastatic
renal cell carcinoma (mRCC): A literature review. Cancer Treat Rev.
34:193–205. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schmidinger M: Improving outcomes in
metastatic clear cell renal cell carcinoma by sequencing therapy.
American Society of Clinical Oncology educational book/ASCO.
American Society of Clinical Oncology. Meeting. pp. e228–e238.
2014;
|
|
10
|
Dranitsaris G, Schmitz S and Broom RJ:
Small molecule targeted therapies for the second-line treatment for
metastatic renal cell carcinoma: A systematic review and indirect
comparison of safety and efficacy. J Cancer Res Clin Oncol.
139:1917–1926. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Escudier B, Albiges L and Sonpavde G:
Optimal management of metastatic renal cell carcinoma: Current
status. Drugs. 73:427–438. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Schnadig ID, Hutson TE, Chung H, Dhanda R,
Halm M, Forsyth M and Vogelzang NJ: Dosing patterns, toxicity, and
outcomes in patients treated with first-line sunitinib for advanced
renal cell carcinoma in community-based practices. Clin Genitourin
Cancer. 12:413–421. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim S, Ding W, Zhang L, Tian W and Chen S:
Clinical response to sunitinib as a multitargeted tyrosine-kinase
inhibitor (TKI) in solid cancers: A review of clinical trials. Onco
Targets Ther. 7:719–728. 2014.PubMed/NCBI
|
|
14
|
Poprach A, Pavlik T, Melichar B, Kubackova
K, Bortlicek Z, Svoboda M, Lakomy R, Vyzula R, Kiss I, Dusek L, et
al: Clinical and laboratory prognostic factors in patients with
metastatic renal cell carcinoma treated with sunitinib and
sorafenib after progression on cytokines. Urol Oncol. 32:488–495.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dudek AZ, Zolnierek J, Dham A, Lindgren BR
and Szczylik C: Sequential therapy with sorafenib and sunitinib in
renal cell carcinoma. Cancer. 115:61–67. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Krusch M, Salih J, Schlicke M, Baessler T,
Kampa KM, Mayer F and Salih HR: The kinase inhibitors sunitinib and
sorafenib differentially affect NK cell antitumor reactivity in
vitro. J Immunol. 183:8286–8294. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Terme M, Ullrich E, Delahaye NF, Chaput N
and Zitvogel L: Natural killer cell-directed therapies: Moving from
unexpected results to successful strategies. Nat Immunol.
9:486–494. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Geisler K, Reischer A, Kroeger I, Jacobs
B, Meinhardt K, Bauer R, Ryffel B, Mackensen A and Ullrich E:
Nilotinib combined with interleukin-2 mediates antitumor and
immunological effects in a B16 melanoma model. Oncol Rep.
31:2015–2020. 2014.PubMed/NCBI
|
|
19
|
Krieg S and Ullrich E: Novel immune
modulators used in hematology: Impact on NK cells. Front Immunol.
3:3882013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mignot G, Ullrich E, Bonmort M, Ménard C,
Apetoh L, Taieb J, Bosisio D, Sozzani S, Ferrantini M, Schmitz J,
et al: The critical role of IL-15 in the antitumor effects mediated
by the combination therapy imatinib and IL-2. J Immunol.
180:6477–6483. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Claus M, Greil J and Watzl C:
Comprehensive analysis of NK cell function in whole blood samples.
J Immunol Methods. 341:154–164. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Powles T, Chowdhury S, Bower M, Saunders
N, Lim L, Shamash J, Sarwar N, Sadev A, Peters J and Green J: The
effect of sunitinib on immune subsets in metastatic clear cell
renal cancer. Urol Int. 86:53–59. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kondo T, Nakazawa H, Ito F, Hashimoto Y,
Osaka Y, Futatsuyama K, Toma H and Tanabe K: Favorable prognosis of
renal cell carcinoma with increased expression of chemokines
associated with a Th1-type immune response. Cancer Sci. 97:780–786.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Olive C, Cheung C, Nicol D and Falk MC:
Expression of cytokine mRNA transcripts in renal cell carcinoma.
Immunol Cell Biol. 76:357–362. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Onishi T, Ohishi Y, Goto H, Tomita M and
Abe K: An assessment of the immunological status of patients with
renal cell carcinoma based on the relative abundance of T-helper 1-
and -2 cytokine-producing CD4+ cells in peripheral blood. BJU Int.
87:755–759. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Fehniger TA, Cooper MA, Nuovo GJ, Cella M,
Facchetti F, Colonna M and Caligiuri MA: CD56bright natural killer
cells are present in human lymph nodes and are activated by T
cell-derived IL-2: A potential new link between adaptive and innate
immunity. Blood. 101:3052–3057. 2003. View Article : Google Scholar : PubMed/NCBI
|