Introduction
Pancreatic cancer is one of the most lethal causes
of cancer-associated mortality worldwide (1). The survival outcomes of patients with
pancreatic cancer have been gradually improved using effective
adjuvant chemotherapies (2), and
previous studies have demonstrated that the administration of
gemcitabine or 5-fluorouracil (5-FU) plus folinic acid improves the
progression-free and overall survival (OS) rates following surgical
resection in patients with pancreatic cancer compared with surgery
alone (3–7). Previously, the Japan Adjuvant Study
Group of Pancreatic Cancer (JASPAC-01) trial demonstrated that S-1,
which is the oral 5-FU prodrug tegafur combined with oteracil and
gimeracil (CDHP), is effective as adjuvant chemotherapy for
Japanese patients undergoing curative resection for stage II
disease or lower or stage III disease with combined resection of
the celiac artery (8). According to
these results, adjuvant chemotherapy with S-1 is now considered to
be the standard treatment following curative resection for
pancreatic cancer in Japan. However, ~60% of the patients still
develop recurrence following curative resection followed by
adjuvant S-1 therapy. To improve the clinical outcomes, it is
important to identify the characteristics of patients with improved
prognoses and the expression of enzymes and tumor-specific
activity.
A number of enzymes serve key roles in the
fluoropyrimidine metabolism. Among them, dihydropyrimidine
dehydrogenase (DPD) is a rate-limiting enzyme in 5-FU catabolism.
Increased DPD expression in tumors has been hypothesized to result
in relatively low sensitivity to fluoropyrimidine-based
chemotherapy (9). However, the number
of published studies evaluating the clinical value of the
expression of DPD in resected pancreatic cancer followed by
adjuvant chemotherapy with S-1 is limited and therefore no
definitive conclusions have yet been made (10–13). In
order to develop individualized adjuvant chemotherapy treatment,
the characterization of genes associated with tumor sensitivity or
resistance to antitumor agents using cancer tissues from the
patients is required for the selection of preferable
treatments.
In the present study, DPD expression was
investigated in consecutive patients with pancreatic cancer who
underwent curative resection followed by adjuvant chemotherapy with
S-1, and the association among the DPD expression results, the
clinicopathological parameters and the survival rate was
evaluated.
Patients and methods
Patients
The patients were selected from the medical records
of 201 consecutive patients with pancreatic cancer who underwent
pancreatic surgery at Kanagawa Cancer Center (Yokohama City, Japan)
from April 2005 to March 2014. The following inclusion criteria
were applied: i) A pathologically diagnosed pancreatic ductal
adenocarcinoma according to the definitions of the 7th edition of
the International Union Against Cancer (UICC) tumor-node-metastasis
(TNM) classification (14); ii)
patients who initially underwent R0 or R1 resection; and iii)
patients who received adjuvant chemotherapy with S-1. The resected
specimens were examined histopathologically and staged according to
the 7th edition of the UICC TNM classification. Patients with other
types of pancreatic cancer, including intraductal papillary
mucinous neoplasm, cystadenocarcinoma or neuroendocrine tumors, or
patients who underwent R2 resection were excluded from the present
study. Of the 201 patients initially considered, 66 were eligible
for inclusion in the present study. The median age was 70 years
(range, 46–81 years); 36 patients were male and 30 were female. A
total of 40 patients underwent pancreaticoduodenectomy, 19
underwent distal pancreatectomy (DP) and 7 underwent total
pancreatectomy. The median follow-up period was 29.2 months (range,
14.6–102.8 months). The present study was approved by the
Institutional Review Board Committee of the Kanagawa Cancer
Center.
Surgical procedure
All pancreatic surgeries were performed in
accordance with standard procedures that have been described
previously (15). In cases of
pancreaticoduodenectomy, lymph node dissection along the
hepatoduodenal ligament, common hepatic artery, vena cava, superior
mesenteric vein and the right side of the superior mesenteric
artery was a standard part of the procedure. Multiple
intraperitoneal drains were placed: The first was posterior to
choledochojejunostomy, and the second was on the anterior surface
of pancreaticojejunostomy or the closed remnant of the pancreas. In
cases of DP, lymph node dissection was performed in the region of
the celiac trunk and the superior mesenteric artery and vein, as
well as behind the pancreas along the left side of the renal vein
and the left adrenal gland. Intraperitoneal drains were placed
close to the pancreatic stump.
Adjuvant chemotherapy
S-1 treatment was initiated within 10 weeks of
surgery. The patients received S-1 at between 80 and 120 mg/day for
4 weeks followed by 2 weeks of rest, and treatment was continued
for 6 months. The doses were modified in accordance with the
JASPAC-01 trial (8); when adverse
reactions appeared, the dose was decreased from 120 to 100 mg/day
or from 100 to 80 mg/day, or administration was temporarily
discontinued. Treatment was discontinued when the patient exhibited
disease recurrence or adverse reactions that were uncontrollable
even by dose modification or the temporary withdrawal of drug
administration.
Follow-up
Patients were followed up at outpatient clinics.
Hematological tests and physical examinations were performed at
least every 2 weeks during adjuvant chemotherapy, and at least
every 3 months for 5 years following the end of the course of
adjuvant chemotherapy. The carcinoembryonic antigen and cancer
antigen 19–9 tumor marker levels were evaluated at least every 3
months for 5 years. Patients underwent a computed tomography
examination every 3 months during the first 3 years following
surgery, and then every 6 months for 5 years following surgery.
Peritoneal recurrence was defined as positive when imaging studies
identified at least one of the following characteristics: Massive
ascites, ascites confirmed by cytology, enhanced abdominal nodules,
abnormal intestinal wall thickness, increased fat density of the
intestinal mesentery, diffuse hydronephrosis or an intra-abdominal
mass. When liver metastasis was suspected according to imaging
studies, magnetic resonance imaging or contrast-enhanced
ultrasonography was performed to confirm the diagnosis.
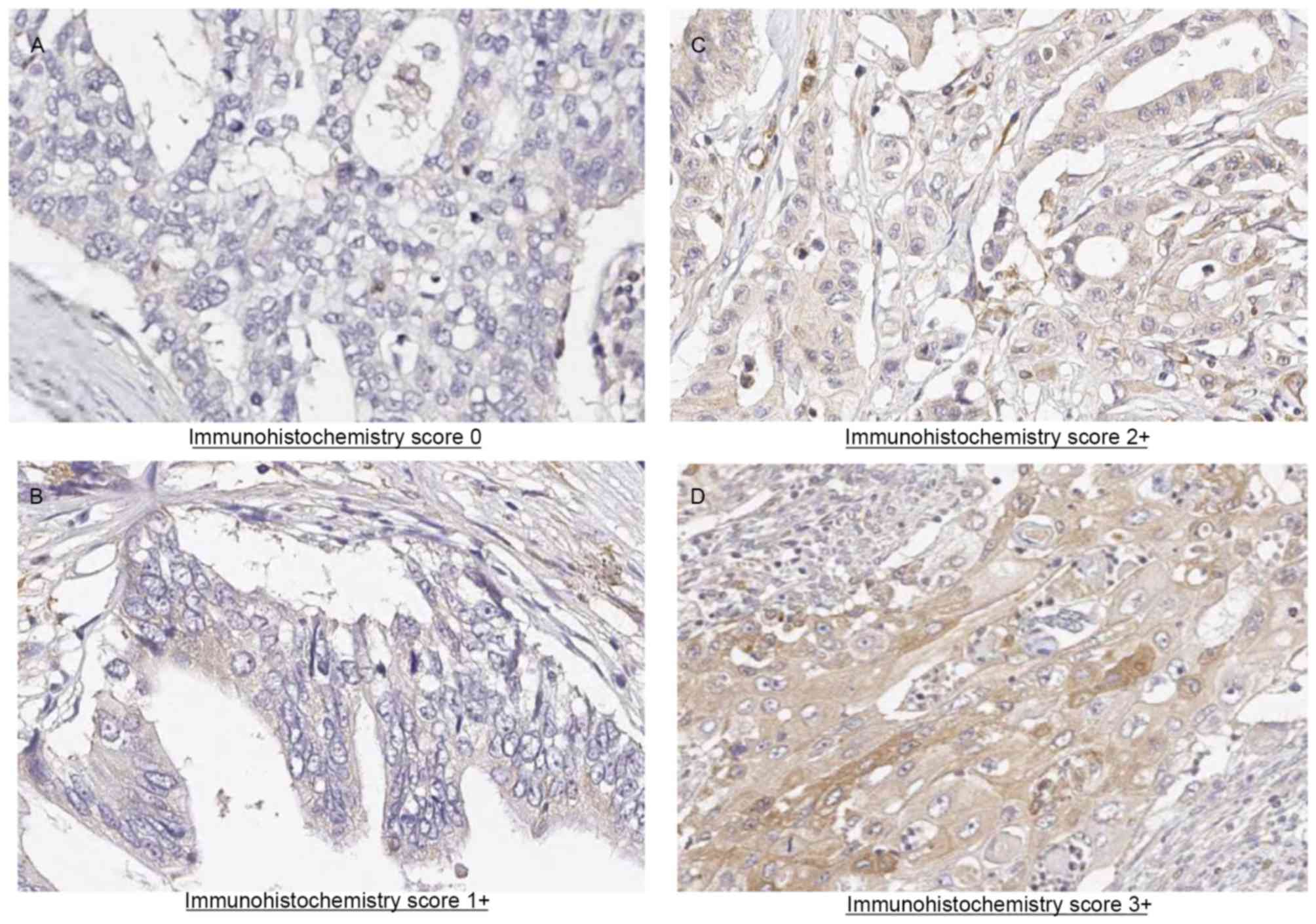
Immunohistochemical analysis of the
DPD expression
Hematoxylin and eosin-stained slides containing
specimens from each pancreatic ductal adenocarcinoma were reviewed,
and a representative tumor region and the corresponding
formalin-fixed paraffin-embedded tissue block was selected for use
in a tissue microarray. Slides of 4-µm thickness were used for
immunohistochemical staining. Slides were deparaffinized in xylene
for 30 min, rehydrated using a gradient of ethanol and steamed for
5 min. Antigen retrieval was performed with 121°C in a buffer with
(10 mM sodium citrate, pH 6.0) in a pressure boiler. Slides
remained in the pressure boiler to cool down to 90°C and then
incubated for 20 min at room temperature. Endogenous peroxidase
activity was blocked by immersion in 3% hydrogen peroxide at room
temperature for 10 min, with 3 TBST washes both before and after.
The slices were incubated with anti-dihydropyrimidine
dehydrogenase/DPYD anti rabbit polyclonal antibody (1:50; #ABC451;
EMD Millipore, Billerica, MA, USA) at room temperature for 60 min
with 3 washes in TBST both before and after. The detection was
performed according to the manufacturers protocol of Histofine
Simple Stain MAX-PO Polymer (#424141; Nichirei Bioscience, Inc.,
Tokyo, Japan) at room temperature for 30 min with 3 washes in TBST
both before and after. Visualization was performed ‘DAB Substrate
Kit’ (425011, NICHIREI BIOSCIENCES INC, Japan) used as a chromogen.
Finally, slices were counterstained with hematoxylin.
The intensity of DPD staining was scored using a
light microscope (CH30; Olympus Corporation, Tokyo, Japan) as
follows: Grade 0, not stained; grade 1, faintly stained; grade 2,
weakly stained in comparison with plasma and stroma cells; and
grade 3, stained as strongly as plasma and stroma cells. For the
evaluation of the cytoplasmic DPD expression, if grade 2 or 3
staining was observed in >50% of the neoplasms, the sample was
considered to exhibit positive DPD expression, whereas if grade 0
or 1 staining was observed in >50% of tumor cells, the sample
was considered to exhibit negative DPD expression. Furthermore, if
grade 3 staining was observed in >50% of the neoplasms, the
sample was considered exhibit high DPD expression. The
immunohistochemical evaluation of DPD expression was independently
confirmed by two observers (M.M. and Y.M.) and a consensus was
reached by joint review.
Evaluation and statistical
analyses
The significance of the association between DPD
expression and clinicopathological parameters was determined using
Fisher's exact test or a χ2 test. The OS rate was
defined as the period between surgery and mortality. The data of
the patients who had not experienced an event were censored at the
date of the final observation. The OS rate was evaluated using
univariate and multivariate analyses. OS curves were calculated
using the Kaplan-Meier estimator method and compared using the
log-rank test. The univariate and multivariate survival analyses
were performed using Cox's proportional hazards model. P<0.05
was considered to indicate a statistically significant difference.
The survival data were obtained from hospital records or from the
city registry system. SPSS software (version 11.0J for Windows;
SPSS Inc., Chicago, IL, USA) was used for all statistical
analyses.
Results
Immunohistochemical analyses and the
association between clinicopathological factors
Representative results of immunohistochemical
staining for DPD in pancreatic adenocarcinoma tissue sections are
presented in Fig. 1. Immunoreactivity
was observed in the cytoplasm of cancer cells. Of the 66 tumor
samples analyzed, 10 (14.5%) exhibited negative staining, 22
samples (31.9%) exhibited weak staining, 16 samples (23.2%)
exhibited moderate staining and 18 (26.1%) exhibited strong
staining. A total of 32 patients were assigned to the DPD-negative
expression group and 34 patients were assigned to the DPD-positive
expression group (Table I). In total,
9 clinicopathological factors were evaluated. Although a
significant increase in DPD expression in male patients was
observed, no significant difference for the other
clinicopathological parameters, including T factor or N factor, was
identified between the DPD-positive and DPD-negative expression
groups. In an exploratory analysis according to DPD status, 18
patients were assigned to the DPD-high expression group and 48
patients were assigned to the DPD-low expression group (Table II). The clinicopathological factors
were compared between the patients exhibiting high and low DPD
expression. A total of 9 clinicopathological factors were
evaluated. Although a significant increase in DPD expression was
observed in male patients, no significant difference for the other
clinicopathological parameters, including T factor or N factor, was
identified between the DPD-high and DPD-low expression groups.
 | Table I.Comparison of the patient background
between the DPD-positive and DPD-negative groups. |
Table I.
Comparison of the patient background
between the DPD-positive and DPD-negative groups.
| Characteristic | Patients exhibiting
positive DPD expression (n=34) | Patients exhibiting
negative DPD expression (n=32) | P-value |
|---|
| Median age, years
(range) | 71 (50–80) | 66 (51–81) | 0.266 |
| Sex |
|
| 0.025 |
| Male | 23 (67.6%) | 13 (40.6%) |
|
|
Female | 11 (32.4%) | 19 (59.4%) |
|
| Surgical
procedure |
|
| 0.235 |
| PD | 24 (70.6%) | 16 (50.0%) |
|
| DP | 8 (23.5%) | 11 (34.4%) |
|
| TP | 2 (5.9%) | 5 (15.6%) |
|
| Median
size of tumor, mm (range) | 34.5 (18–105) | 40 (15–80) | 0.718 |
| Pathological
type |
|
| 0.708 |
| tub1 | 20 (58.8%) | 19 (59.4%) |
|
| tub2 | 10 (29.4%) | 8 (25.0%) |
|
| por | 3 (8.8%) | 2 (6.3%) |
|
|
Others | 1 (2.9%) | 3 (9.4%) |
|
| Pathological T
factor |
|
| 0.163 |
| T2 | 1 (2.9%) | 0 (0.0%) |
|
| T3 | 32 (94.1%) | 32 (100.0%) |
|
| T4 | 1 (2.9%) | 0 (0.0%) |
|
| Pathological N
factor |
|
| 0.351 |
| N0 | 11 (32.4%) | 6 (18.8%) |
|
| N1 | 23 (67.6%) | 26 (81.3%) |
|
| Stage (7th UICC
classification) |
|
| 0.351 |
| IIA | 11 (32.4) | 6 (18.8) |
|
| IIB | 22 (64.7%) | 26 (81.3%) |
|
| III | 1 (2.9%) | 0 (0.0%) |
|
 | Table II.Comparison of the patient background
between the DPD-high and DPD-low expression groups. |
Table II.
Comparison of the patient background
between the DPD-high and DPD-low expression groups.
| Characteristic | Patients exhibiting
high DPD expression (n=18) | Patients exhibiting
low DPD expression (n=48) | P-value |
|---|
| Median age, years
(range) | 71.5 (56–79) | 68.5 (46–81) | 0.527 |
| Sex |
|
| 0.001 |
|
Male | 16 (88.9%) | 20 (41.7%) |
|
|
Female | 2 (11.1%) | 28 (58.3%) |
|
| Surgical
procedure |
|
| 0.686 |
| PD | 12 (66.7%) | 28 (58.3%) |
|
| DP | 5 (27.8%) | 14 (29.2%) |
|
| TP | 1 (5.6%) | 6 (12.5%) |
|
| Median size of
tumor, mm (range) | 33.5 (15–90) | 38 (15–105) | 0.319 |
| Pathological
type |
|
| 0.323 |
|
tub1 | 9 (50.0%) | 30 (62.5%) |
|
|
tub2 | 7 (38.9%) | 11 (22.9%) |
|
|
por | 2 (11.1%) | 3 (6.3%) |
|
|
Others | 0 (0.0%) | 4 (8.3%) |
|
| Pathological T
factor |
|
| 0.727 |
| T3 | 18 (100.0%) | 47 (97.9%) |
|
| T4 | 0 (0.0%) | 1 (2.1%) |
|
| Pathological N
factor |
|
| 0.038 |
| N0 | 8 (44.4%) | 9 (18.8%) |
|
| N1 | 10 (55.6%) | 39 (81.3%) |
|
| Stage (7th UICC
classification) |
|
| 0.101 |
|
IIA | 8 (44.4%) | 9 (18.8%) |
|
|
IIB | 10 (55.6%) | 38 (79.2%) |
|
|
III | 0 (0.0%) | 1 (2.1%) |
|
Survival analysis
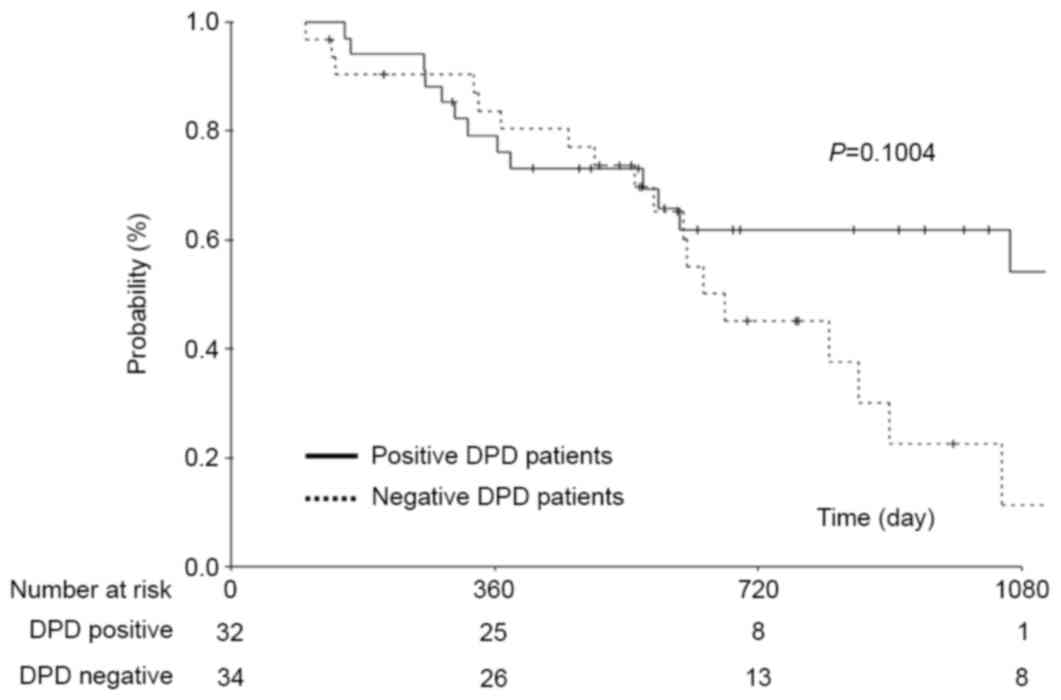
No significant difference in the 3-year OS rates in
patients exhibiting positive and negative DPD expression (12.6 and
14.5%, respectively) was identified (P=0.1004; Fig. 2).
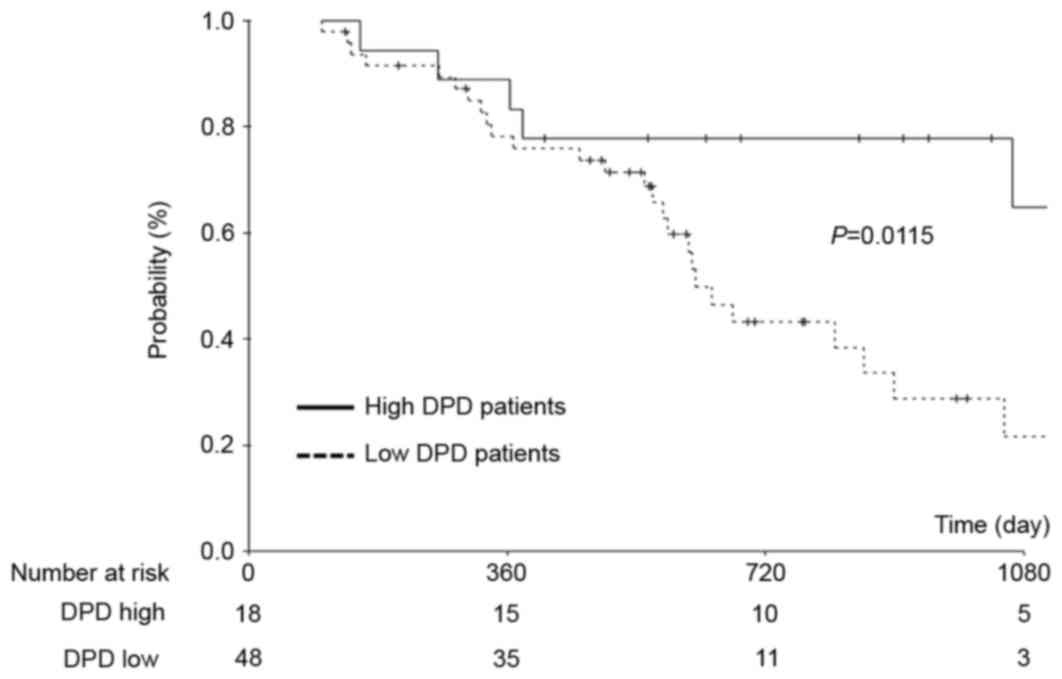
An exploratory analysis according to the DPD status
suggested that the OS time was longer in patients exhibiting high
DPD expression than in patients exhibiting low DPD expression. To
explore this result, a subgroup analysis was performed, with
patients stratified according to high (DPD staining grade 3) or low
(DPD staining grades 0–2) levels of DPD protein in their tumors. A
significantly increased 3-year OS rate was identified in patients
exhibiting high DPD expression compared with those exhibiting low
DPD expression (58.9 and 14.5%, respectively; P=0.0115; Fig. 3). Furthermore, univariate and
multivariate analysis demonstrated that high DPD expression was an
independent risk factor for the OS rate (P=0.02; Table III).
 | Table III.Univariate and multivariate analyses
of risk factors for the overall survival rates of patients
exhibiting high DPD expression compared with those exhibiting low
DPD expression. |
Table III.
Univariate and multivariate analyses
of risk factors for the overall survival rates of patients
exhibiting high DPD expression compared with those exhibiting low
DPD expression.
|
|
| Univariate
analysis | Multivariate
analysis |
|---|
|
|
|
|
|
|---|
| Factor | n | OR | 95% CI | P-value | OR | 95% CI | P-value |
|---|
| Sex |
|
|
| 0.662 |
|
|
|
|
Female | 30 | 1 |
|
|
|
|
|
|
Male | 36 | 1.177 | 0.567–2.441 |
|
|
|
|
| Age, years |
|
|
| 0.532 |
|
|
|
|
<70 | 29 | 1 |
|
|
|
|
|
|
≥70 | 37 | 1.259 | 0.612–2.587 |
|
|
|
|
| Size of tumor,
mm |
|
|
| 0.352 |
|
|
|
|
<38 | 33 | 1 |
|
|
|
|
|
|
≥38 | 33 | 1.42 | 0.678–2.974 |
|
|
|
|
| Tumor location |
|
|
| 0.239 |
|
|
|
| Body or
tail | 19 | 1 |
|
|
|
|
|
|
Head | 47 | 1.709 | 0.700–4.169 |
|
|
|
|
| Pathological N
factor |
|
|
| 0.034 |
|
|
|
| N0 | 17 | 1 |
|
|
|
|
|
| N1 | 49 | 3.627 | 1.099–11.971 |
|
|
|
|
| DPD status |
|
|
| 0.023 |
|
| 0.02 |
|
Low | 48 | 1 |
|
| 1 |
|
|
|
High | 18 | 3.078 | 1.164–8.135 |
| 3.183 | 1.197–8.467 |
|
Discussion
In the present study, DPD status was evaluated in
pancreatic adenocarcinoma patients who underwent curative resection
followed by adjuvant chemotherapy with S-1, and no significant
difference in the OS rate was identified between patients
exhibiting positive DPD expression and patients exhibiting negative
DPD expression. By contrast, a significant increase was identified
in the OS rate of the patients exhibiting high DPD expression
compared with patients exhibiting low DPD expression. These results
suggested that DPD status is a potential predictive marker in
patients with pancreatic cancer who undergo curative resection with
S-1 adjuvant chemotherapy.
Previous studies have investigated the presence and
effect of DPD protein overexpression or gene amplification in
patients. These studies have identified that DPD expression is
increased in between 30 and 50% of patients. Kondo et al
(16) evaluated the intratumoral DPD
expression in pancreatic carcinoma using immunohistochemical
methods in 86 Japanese patients with pancreatic carcinoma who were
treated with adjuvant S-1-based chemotherapy. This study identified
that high DPD expression was observed in 35 (41%) patients. In
addition, Shimoda et al (13)
determined DPD expression in 57 Japanese patients with pancreatic
carcinoma who were treated with adjuvant S-1 or gemcitabine
chemotherapy. This study identified that high DPD expression was
observed in 52% of the patients in the S-1 group. These results
were similar to those of the present study. Therefore, the
incidence of high DPD expression may be between 40 and 50% in
patients with resectable pancreatic cancer.
With regard to the association between the DPD
expression and clinicopathological factors, a study by Kondo et
al (11) identified that there
were no significant differences in clinicopathological factors,
including UICC pathological T factor and lymph node status, between
the patients exhibiting high and low DPD expression. A study by
Nakahara et al (17) also
identified similar results in 18 patients. In the present study, no
significant differences in the clinicopathological factors between
the patients exhibiting high and low DPD expression were
identified. Therefore, DPD expression appears to be independent of
clinicopathological factors.
In the present study, DPD expression was not
identified to be a predictive marker in patients with pancreatic
cancer who underwent curative resection with S-1 adjuvant
chemotherapy. However, DPD status is a potential predictive marker
in patients with pancreatic cancer who undergo curative resection
with S-1 adjuvant chemotherapy. Indeed, multivariate OS analysis in
the study by Kondo et al (16)
identified that high DPD expression is one of the predictive
markers (hazard ratio, 1.98; 95% confidence interval, 1.06–3.71;
P=0.03).
It is hypothesized that tumor cells which exhibit
high DPD expression are resistant to fluoropyrimidine-based therapy
(18). In the present study, survival
analysis results indicated that the antitumor effect of S-1 for
pancreatic cancer was not influenced by intratumoral DPD gene
expression; furthermore, improved survival was observed in patients
exhibiting high DPD expression. There are potential explanations
for these conflicting results. First, similar results were observed
in previous studies. In a study by Sasako et al (19) an association between thymidylate
synthase (TS), which is the rate-limiting enzyme in the de novo
synthesis of 2′-deoxy-thymidine-5′-monophosphate, and DPD
expression in tumors and the clinical outcomes in stage II/III
gastric cancer was identified. This study identified that high TS
and DPD gene expression in tumors was associated with an enhanced
benefit from postoperative adjuvant S-1 treatment in gastric
cancer. This study demonstrated that S-1 caused certain effects not
exerted by other fluoropyrimidines. Ichikawa et al (20) described “some effect” that was
explained by the inhibition of intratumoral DPD by CDHP, which is
contained in S-1 therapy. Secondly, the intratumoral DPD mRNA
expression level in pancreatic cancer was significantly increased
compared with in colorectal cancer and gastric cancer (21). In addition, Takechi et al
(22) demonstrated that the in
vitro antitumor activity of 5-FU against tumor cells with low
DPD expression levels was not appreciably affected by the addition
of CDHP (22). Therefore, in
pancreatic cancer, it is considered that high DPD expression
influences S-1 treatment and this discrepancy is dependent on the
difference between S-1 and other 5-FU agents.
Careful attention is required when interpreting the
results of the present study owing to a number of potential
limitations. First, the present study was a retrospective analysis
which was performed at a single institution. There is the
possibility that the results were incidental. Secondly, there was a
subjective bias in the immunohistochemical evaluation of the DPD
expression. The methods of evaluating DPD expression were not
standardized. Furthermore, the appropriate DPD threshold value is
unclear. Considering these limitations, the results of the present
study require confirmation in another cohort or in a prospective
multicenter study.
DPD status is considered to be a potentially useful
predictive marker in pancreatic cancer patients who undergo
curative resection with S-1 adjuvant chemotherapy. However, the
results of the present study require confirmation in another cohort
or in a prospective multicenter study.
Acknowledgements
The present study was supported by the Kanagawa
Prefectural Hospitals Cancer Fund.
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Vincent A, Herman J, Schulick R, Hruban RH
and Goggins M: Pancreatic cancer. Lancet. 378:607–620. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Burris HA III, Moore MJ, Andersen J, Green
MR, Rothenberg ML, Modiano MR, Cripps MC, Portenoy RK, Storniolo
AM, Tarassoff P, et al: Improvements in survival and clinical
benefit with gemcitabine as first-line therapy for patients with
advanced pancreas cancer: A randomized trial. J Clin Oncol.
15:2403–2413. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Neoptolemos JP, Stocken DD, Friess H,
Bassi C, Dunn JA, Hickey H, Beger H, Fernandez-Cruz L, Dervenis C,
Lacaine F, et al: A randomized trial of chemoradiotherapy and
chemotherapy after resection of pancreatic cancer. N Engl J Med.
350:1200–1210. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Oettle H, Post S, Neuhaus P, Gellert K,
Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C,
et al: Adjuvant chemotherapy with gemcitabine vs observation in
patients undergoing curative-intent resection of pancreatic cancer:
A randomized controlled trial. JAMA. 297:267–277. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Neoptolemos JP, Stocken DD, Smith C Tudur,
Bassi C, Ghaneh P, Owen E, Moore M, Padbury R, Doi R, Smith D and
Büchler MW: Adjuvant 5-fluorouracil and folinic acid vs observation
for pancreatic cancer: Composite data from the ESPAC-1 and −3(v1)
trials. Br J Cancer. 100:246–250. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Neoptolemos JP, Stocken DD, Bassi C,
Ghaneh P, Cunningham D, Goldstein D, Padbury R, Moore MJ, Gallinger
S, Mariette C, et al: Adjuvant chemotherapy with fluorouracil plus
folinic acid vs gemcitabine following pancreatic cancer resection:
A randomized controlled trial. JAMA. 304:1073–1081. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Maeda A, Boku N, Fukutomi A, Kondo S,
Kinoshita T, Nagino M and Uesaka K: Randomized phase III trial of
adjuvant chemotherapy with gemcitabine versus S-1 in patients with
resected pancreatic cancer: Japan Adjuvant Study Group of
Pancreatic Cancer (JASPAC-01). Jpn J Clin Oncol. 38:227–229. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Salonga D, Danenberg KD, Johnson M,
Metzger R, Groshen S, Tsao-Wei DD, Lenz HJ, Leichman CG, Leichman
L, Diasio RB and Danenberg PV: Colorectal tumors responding to
5-fluorouracil have low gene expression levels of dihydropyrimidine
dehydrogenase, thymidylate synthase, and thymidine phosphorylase.
Clin Cancer Res. 6:1322–1327. 2000.PubMed/NCBI
|
|
10
|
Saif MW, Hashmi S, Bell D and Diasio RB:
Prognostication of pancreatic adenocarcinoma by expression of
thymidine phosphorylase/dihydropyrimidine dehydrogenase ratio and
its correlation with survival. Expert Opin Drug Saf. 8:507–514.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kondo N, Murakami Y, Uemura K, Sudo T,
Hashimoto Y, Nakashima A, Ohge H and Sueda T: Prognostic impact of
dihydropyrimidine dehydrogenase expression on pancreatic
adenocarcinoma patients treated with S-1-based adjuvant
chemotherapy after surgical resection. J Surg Oncol. 104:146–154.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nakamura A, Hayashi K, Nakajima G,
Kamikozuru H, Okuyama R, Kuramochi H, Hatori T and Yamamoto M:
Impact of dihydropyrimidine dehydrogenase and γ-glutamyl hydrolase
on the outcomes of patients treated with gemcitabine or S-1 as
adjuvant chemotherapy for advanced pancreatic cancer. Exp Ther Med.
2:1097–1103. 2011.PubMed/NCBI
|
|
13
|
Shimoda M, Kubota K, Shimizu T and Katoh
M: Randomized clinical trial of adjuvant chemotherapy with S-1
versus gemcitabine after pancreatic cancer resection. Br J Surg.
102:746–754. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Scoazec JY and Sabourin JC: 2010: The
seventh edition of the TNM classification. Ann Pathol. 30:2–6.
2010.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aoyama T, Murakawa M, Katayama Y, Yamaoku
K, Kanazawa A, Higuchi A, Shiozawa M, Morimoto M, Yoshikawa T,
Yamamoto N, et al: Impact of postoperative complications on
survival and recurrence in pancreatic cancer. Anticancer Res.
35:2401–2409. 2015.PubMed/NCBI
|
|
16
|
Kondo N, Murakami Y, Uemura K, Sudo T,
Hashimoto Y, Nakashima A and Sueda T: Combined analysis of
dihydropyrimidine dehydrogenase and human equilibrative nucleoside
transporter 1 expression predicts survival of pancreatic carcinoma
patients treated with adjuvant gemcitabine plus S-1 chemotherapy
after surgical resection. Ann Surg Oncol. 19 Suppl 3:S646–S655.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nakahara O, Takamori H, Tanaka H, Sakamoto
Y, Ikuta Y, Furuhashi S, Watanabe M, Beppu T, Hirota M, Kanemitsu K
and Baba H: Clinical significance of dihydropyrimidine
dehydrogenase and thymidylate synthase expression in patients with
pancreatic cancer. Int J Clin Oncol. 15:39–45. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang WB, Yang Y, Zhao YP, Zhang TP, Liao Q
and Shu H: Recent studies of 5-fluorouracil resistance in
pancreatic cancer. World J Gastroenterol. 20:15682–15690. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sasako M, Terashima M, Ichikawa W, Ochiai
A, Kitada K, Kurahashi I, Sakuramoto S, Katai H, Sano T and Imamura
H: Impact of the expression of thymidylate synthase and
dihydropyrimidine dehydrogenase genes on survival in stage II/III
gastric cancer. Gastric Cancer. 18:538–548. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ichikawa W, Takahashi T, Suto K, Yamashita
T, Nihei Z, Shirota Y, Shimizu M, Sasaki Y and Hirayama R:
Thymidylate synthase predictive power is overcome by irinotecan
combination therapy with S-1 for gastric cancer. Br J Cancer.
91:1245–1250. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kuramochi H, Hayashi K, Uchida K, Nakajima
G, Hatori T, Danenberg KD, Danenberg PV and Yamamoto M: High
intratumoral dihydropyrimidine dehydrogenase mRNA levels in
pancreatic cancer associated with a high rate of response to S-1.
Cancer Chemother Pharmacol. 63:85–89. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Takechi T, Fujioka A, Matsushima E and
Fukushima M: Enhancement of the antitumour activity of
5-fluorouracil (5-FU) by inhibiting dihydropyrimidine dehydrogenase
activity (DPD) using 5-chloro-2,4-dihydroxypyridine (CDHP) in human
tumour cells. Eur J Cancer. 38:1271–1277. 2002. View Article : Google Scholar : PubMed/NCBI
|