Introduction
Desmoid-type fibromatosis, previously described as
aggressive fibromatosis, is a rare soft tissue tumor with the
typical clinical behavior of frequent local recurrence without
distant spread (1). It usually occurs
in the abdominal wall and in the superficial muscular-aponeurotic
tissues of the extremities (1–3). Mammary
desmoid-type fibromatosis is a rare and locally aggressive
intermediate tumor of the breast; it originates from fibroblasts
and myofibroblasts within the breast parenchyma and does not
metastasize (1–5). The condition is locally aggressive and
has a high rate of recurrence. Extra-abdominal desmoid tumors
account for 3% of all soft-tissue tumors, with an incidence of
2.4–4.3 per million each year (1).
Fibromatosis of the chest wall represents 8–10% of all cases
(2). Fibromatosis arising from within
the breast itself is very rare, accounting for 0.2% of all breast
tumors (5–12). The etiology of mammary fibromatosis is
unknown, and breast imaging examinations are not specific for
fibromatosis; to distinguish mammary fibromatosis from malignant
breast tumors through physical examination and imaging techniques
can be difficult. There appears to be general agreement that a
complete wide excision is the treatment of choice of fibromatosis
involving only the breast (1–4). The current study presents 2 cases of
women with breast fibromatosis, including one with a locally
advanced aggressive form of the disease.
Case reports
Case 1
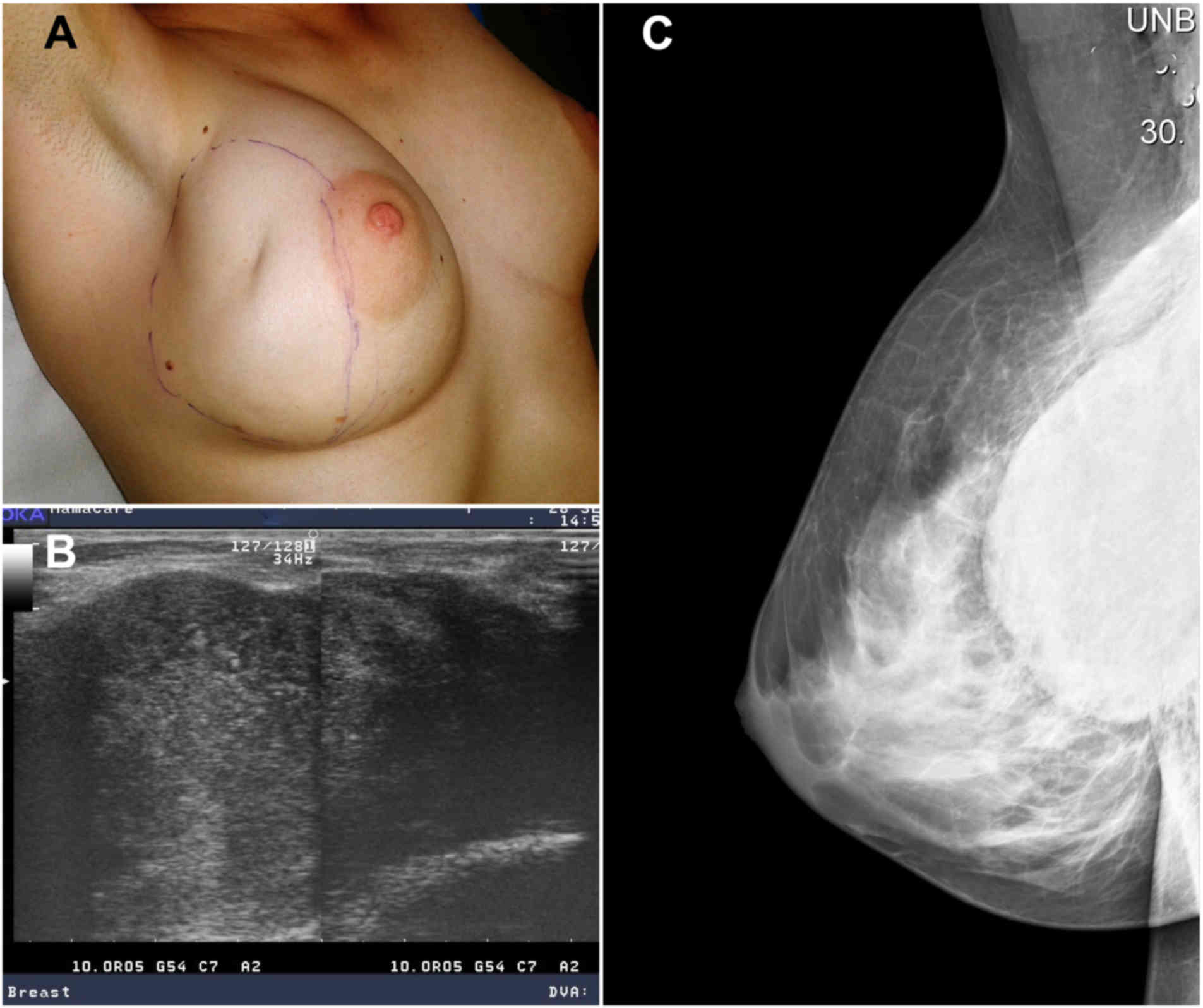
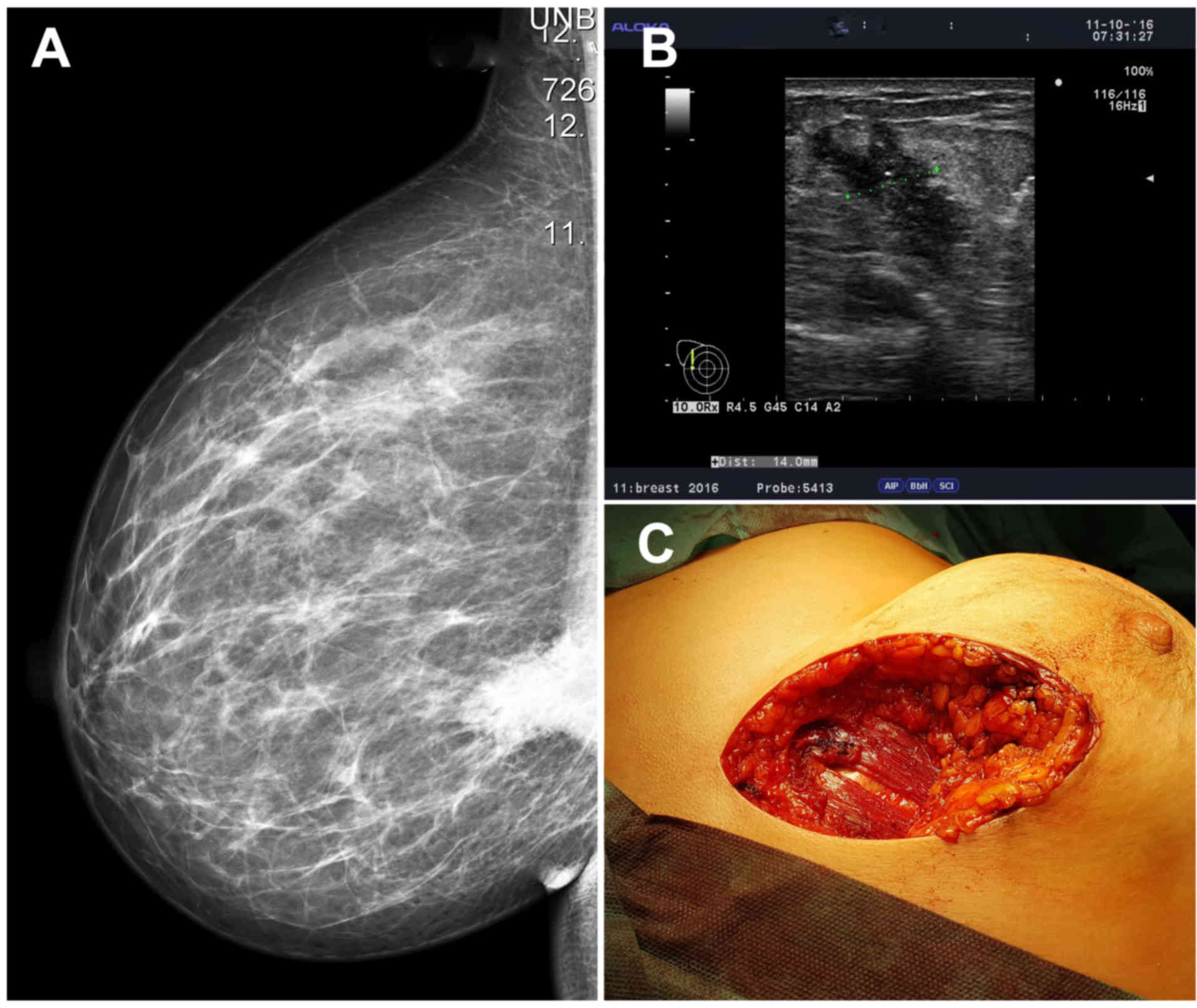
A 36-year-old Caucasian woman with no previous
medical history was referred in September 2016 to the Breast Unit
of the Second Department of Gynecology and Obstetrics, University
Hospital of Bratislava (Slovakia), for a rapidly growing lump in
the right breast following a small trauma. Physical examination
revealed a large, breast- and skin-infiltrating, prominent tumor
located predominantly in the lateral quadrants of the right breast
(Fig. 1A). The tumor mass was fixed
to the chest wall. A well circumscribed hypoechoic area with a
rather homogenous echotexture and lateral acoustic shadowing could
be observed on breast ultrasound (Fig.
1B). Mammography suggested a circumscribed, round, radiopaque
lesion with mostly sharp contours, with the dorsal region of the
lesion being impossible to define (Fig.
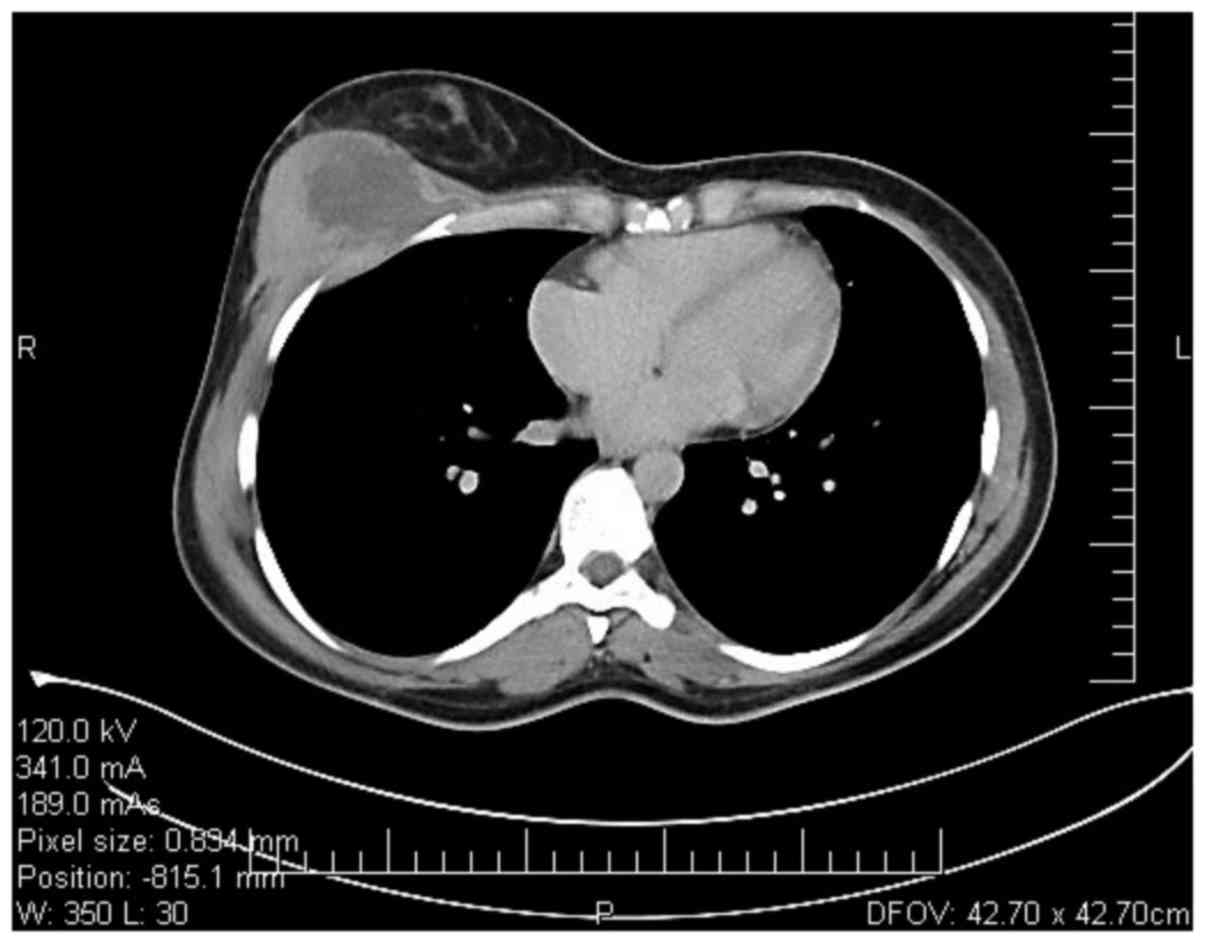
1C). As the tumor was fixed to the chest wall, a
thoracoabdominal computed tomography scan was made; it showed a
large (8.4×7.5×5.4 cm), inhomogeneous mass in the right breast that
appeared to be in continuity with the right pectoralis major muscle
and the right serratus anterior muscle (Fig. 2). Findings on the intra-thoracic and
intra-abdominal organs were physiological. A core needle biopsy was
performed on the palpable right breast mass, which supposed the
diagnosis of fibromatosis. Once a diagnosis was established,
surgery was scheduled. The patient was taken to the operating room
at the Department of Thoracic Surgery (University Hospital of
Bratislava) for the breast surgery and possible en bloc resection
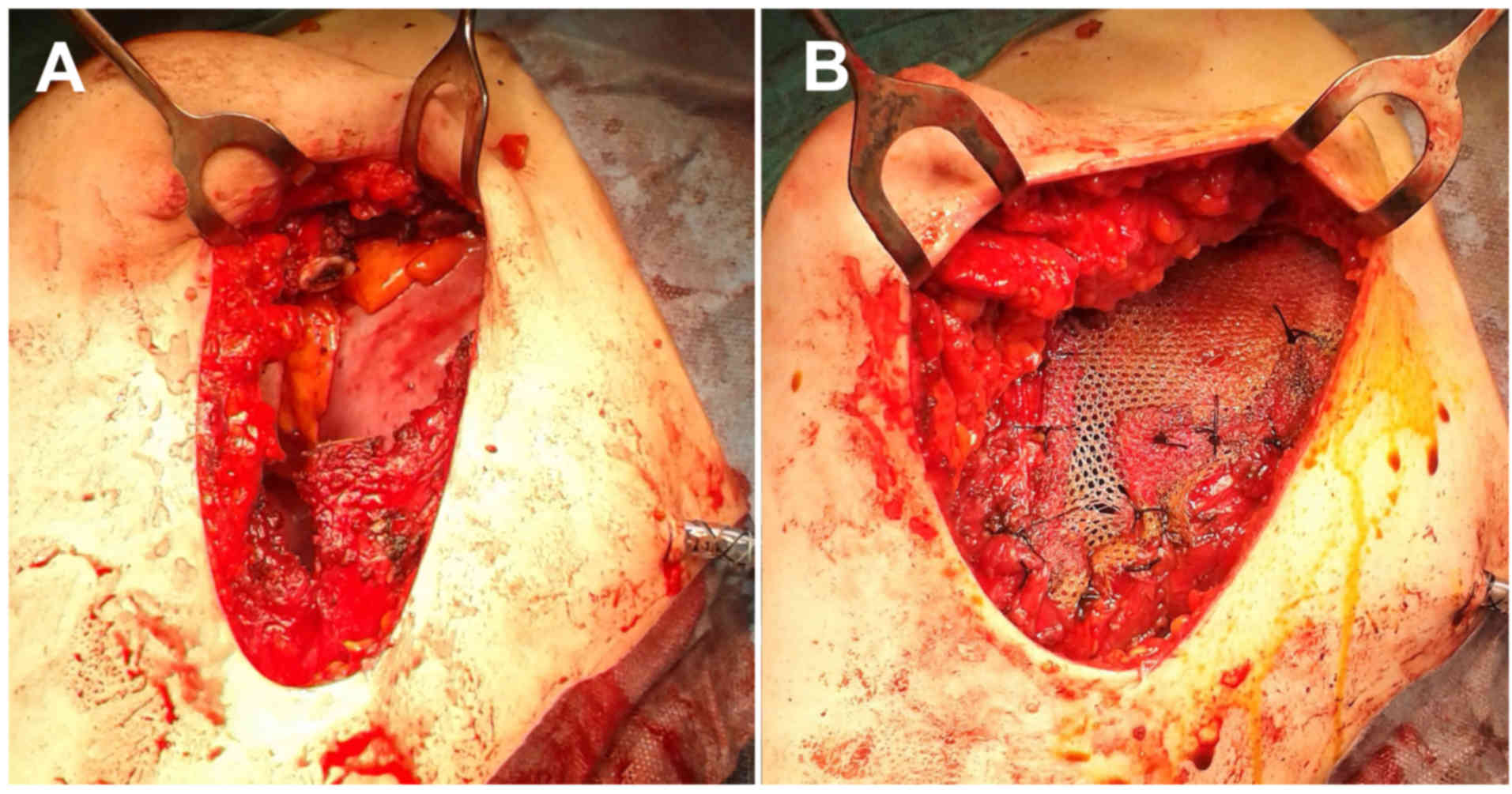
of the underlying regions of the thoracic wall. Surgery was
performed under general anesthesia with selective intubation. The
patient underwent a right partial mastectomy with en bloc resection
of the underlying musculature (inferior lateral portion of the
right pectoralis major muscle and the anterior portion of the right
serratus anterior muscle) and en bloc resection of the underlying
chest wall structures (fourth and fifth ribs, intercostal muscles
and parietal pleura; Fig. 3A).
Repeated frozen section examinations during surgery were required
for confirmation or exclusion of chest wall infiltration. The right
chest wall defect was then closed with a 15.0×15.0-cm polypropylene
flat sheet mesh (Parietene™; Medtronic, Minneapolis, MN, USA;
Fig. 3B). The right partial
mastectomy site was then closed in a standard manner. No attempts
at cosmetic breast reconstruction with autologous tissue transfer
or expander/implant placement were considered at that time.
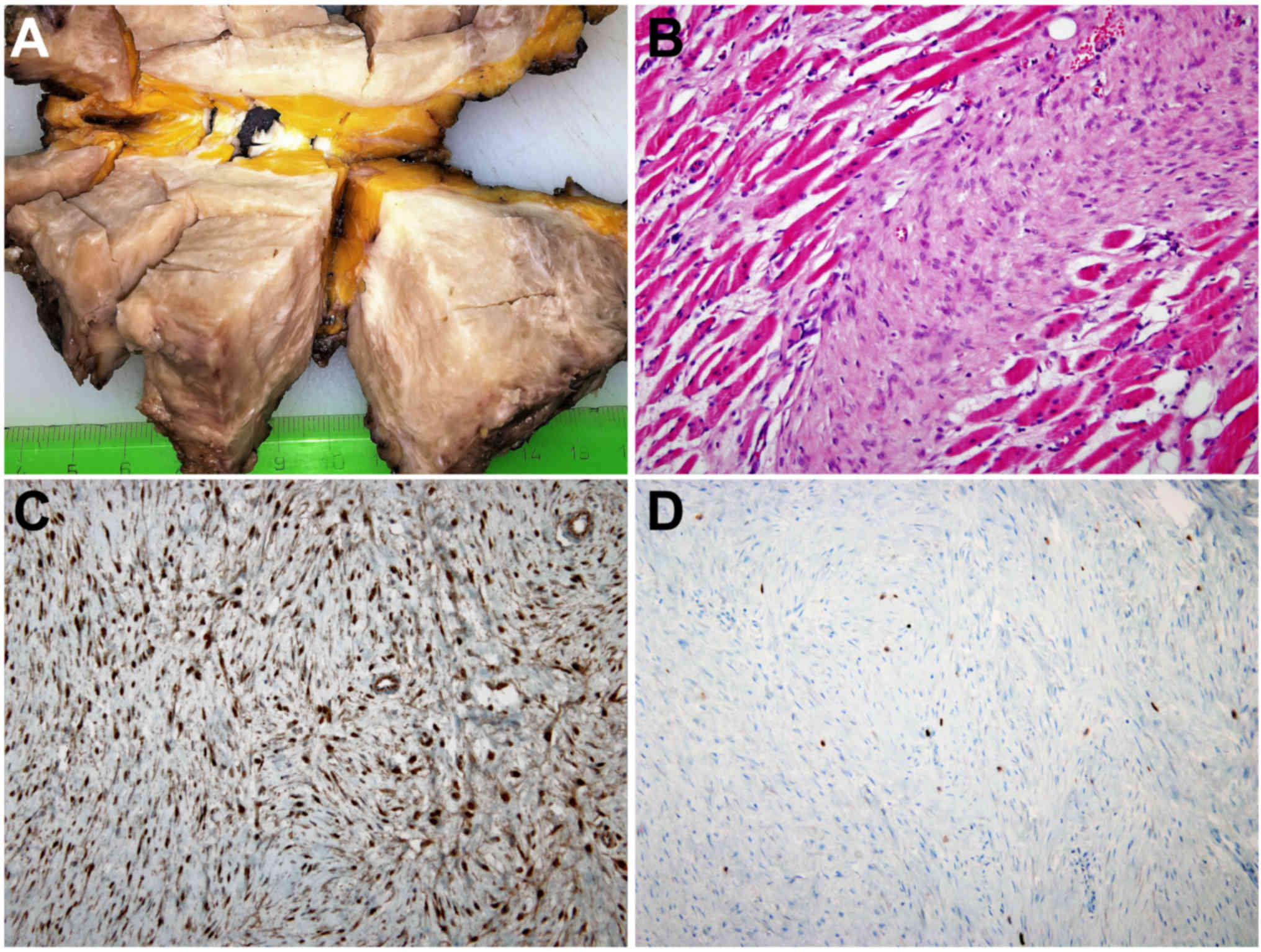
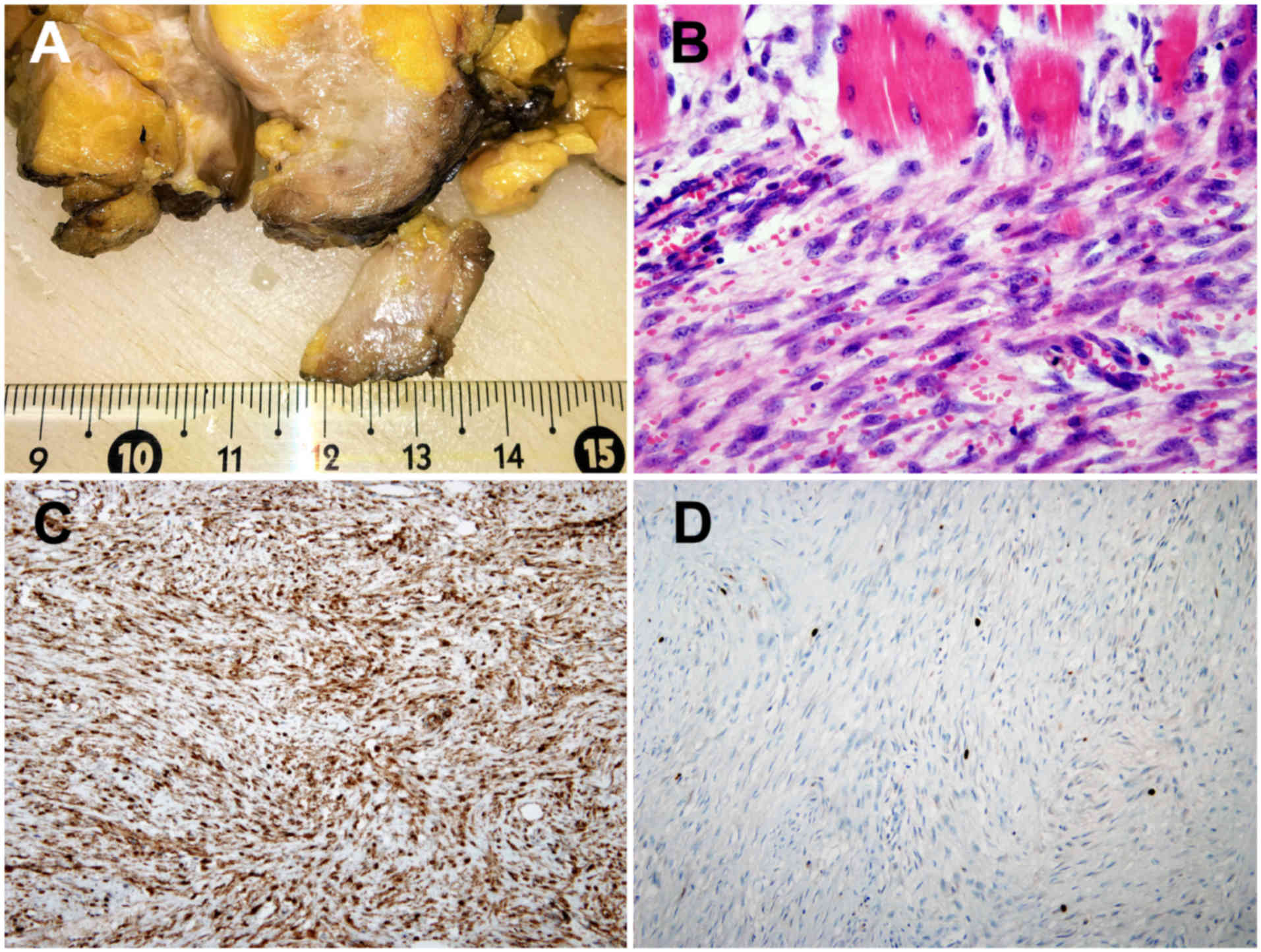
The surgically removed specimen was 12.0×10.5×7.2 cm
in size, containing a grossly circumscribed firm tumor with
off-white, whorled patterns, without necrosis (Fig. 4A). The specimen was fixed in 10%
neutral buffered formalin for 24 h. The fixed specimen was trimmed
with a scalpel to enable it to fit into a tissue cassette. It was
processed in an automated tissue processing machine (BenchMark XT;
Ventana Medical Systems, Inc., Tucson, AZ, USA). The processing
included dehydration, clearing and embedding, in which the
specimens were infiltrated with paraffin wax to create paraffin
blocks. These blocks were cut with a rotary microtome (Leica
RM2235, Leica Biosystems GmbH, Nussloch, Germany) to produce 5-µm
sections. The sections were then stained with hematoxylin and
eosin.
Histological evaluation of the surgical specimens
revealed a proliferation of more or less evenly spaced uniform
spindle cells arranged in intersecting fascicles and associated
with mild to moderate amounts of collagen and occasional mitotic
figures (Fig. 4B). The tumor invasion
of the underlying tissue involved resected muscles and
inter-/pericostal soft tissue. There was no evidence of invasion
into the bony ribs or underlying parietal pleura. A definitive
diagnosis of breast desmoid-type fibromatosis was established from
serial paraffin sectioning (as previously described) and
immunohistochemistry (IHC). IHC analysis of the tumor with
anti-β-catenin antibody (rabbit primary monoclonal antibody; clone
E247; catalog no. AB32572; dilution, 1:200; incubation for 60 min
at 25°C; Abcam, Cambridge, UK) revealed diffuse nuclear positivity
(Fig. 4C). The Ki-67 proliferation
index (defined as the percentage of the total number of tumor cells
with nuclear staining) measured on paraffin sections using the
MIB-1 antibody (rabbit monoclonal antibody; clone MIB-1; catalog
no. M7240; dilution, 1:100; incubation for 30 min at 25°C; Dako;
Agilent Technologies, Inc., Santa Clara, CA, USA) was <5%
(Fig. 4D). The post-operative course
was uneventful and the patient was discharged home on
post-operative day 7. The patient is now 10 months post-surgery and
remains disease-free.
Case 2
A 43-year-old, premenopausal Caucasian woman with no
previous medical history was referred in October 2016 to the Breast
Unit of the Second Department of Gynecology and Obstetrics,
University Hospital of Bratislava, for a palpable lump in the
inner, lower side of the right breast, which was fixed to the chest
wall. Breast imaging examinations suggested an invasive breast
tumor, likely carcinoma, infiltrating the muscles of the chest wall
(Fig. 5A and B). Therefore, the
patient underwent a thoracic computed tomography scan, which showed
an obscured chest wall infiltration. An ultrasound-guided core
needle biopsy revealed a low-grade myofibroblastic proliferation
consistent with breast fibromatosis. As in case 1, the patient was
transferred to an operating room in the Department of Thoracic
Surgery (University Hospital of Bratislava) for breast saving
surgery and possible en bloc resection of the underlying regions of
the thoracic wall. Surgery was performed under general anesthesia
with selective intubation. The patient underwent a right
quadrantectomy, with a partial resection of the underlying
musculature (Fig. 5C). A definitive
diagnosis of breast fibromatosis was established from serial
paraffin sectioning and immunohistochemistry (using the
aforementioned IHC procedures from case 1; Fig. 6). The spindle cell proliferations
invaded only into the adjacent skeletal muscle. The patient is now
8 months post-surgery and remains disease-free.
Discussion
The World Health Organization defines desmoid-type
fibromatosis as an intermediate soft-tissue tumor that is
characterized by clonal fibroblastic proliferation arising in the
deep soft tissues, with a tendency for infiltration of the local
tissues and local recurrence, but an inability to metastasize
(1). Cases of desmoid-type
fibromatosis are often broadly categorized into one of two groups.
The largest group contains sporadic cases, with an incidence of
3.42 per million person-years, forming 84–93% of all cases
(1,6).
In this group, somatic β-catenin-activating mutations are
considered to be the cause of the disease (13). The second, smaller group of cases
consists of those associated with familial adenomatous polyposis
(14). The etiology of mammary
fibromatosis is unknown; it has no predilection for age, family
history or exposure factors, although certain cases occur after
trauma (4,6). The disease is usually painless and the
presenting symptom is always a palpable, firm breast mass (2,6,7). Breast imaging examinations are not
specific for fibromatosis and often imitate breast cancer (8,11)
(Fig. 5A and B). Computed tomography
and/or magnetic resonance imaging assists in defining the
infiltration into adjacent tissue, particularly in patients in whom
there was a preoperative suspicion of chest wall musculature
involvement (1,2,11; Fig. 2). Large
core-needle biopsies are not always successful in the differential
diagnosis of tumors of mesenchymal origin (15). A diagnosis can be made from
microscopic findings on routine hematoxylin and eosin-stained
sections. In general, the lesion does not have malignant features
such as a high mitotic rate, cellular atypia, necrosis or vascular
invasion (15,16). Immunohistochemical staining for
β-catenin with nuclear positivity is also useful in establishing a
diagnosis (Figs. 4C and 6C), but there are no specific immunomarkers
for breast fibromatosis (1,15).
Standard treatment of this recurrent tumor involves
a wide surgical resection with safe margins (1–5). The
reasons for such an aggressive surgical approach include the
potential for the fibromatosis to undergo aggressive, local growth
and for invasion into the surrounding structures, plus a high local
recurrence rate when incompletely excised with positive surgical
margins. Povoski et al (2)
described the requirement for repeated surgical intervention in a
patient with multiple recurrences of fibromatosis due to positive
resection margins in specimens from the primary surgery. The
surgical management throughout the final surgical treatment of the
disease, which involved infiltration of the chest wall, was very
similar to the procedure in case 1 of the present study (Fig. 3A and B). In the present study, a wide
en bloc resection was chosen to avoid future recurrence, based on
negative surgical margins on the frozen section as an alternative
to mastectomy. Mastectomy should be avoided in cases where it is
possible, particularly in young women (1,16,17). Ha et al (8) presented the case of a 30-year-old
Caucasian woman with a palpable mass within the medial portion of
the right breast. The mammographic presentation of breast
fibromatosis mimicking breast carcinoma was almost identical to
that of case 2 in the present study (Fig.
5A). The lesion was surgically resected via a wide local
excision. Follow-up mammograms that were performed at 1 and 2 years
post-resection showed no evidence of recurrence on radiography
(8). Notably, 24 cases of breast
desmoid tumors that developed following augmentation mammoplasty
have been described in the literature (12). In total, 16 of the patients developed
fibromatosis in association with silicone implants. The natural
progression of fibromatosis remains unpredictable and enigmatic.
While this disease has been described as progressing rapidly and
aggressively in certain cases, in other cases, desmoid tumors have
demonstrated slow and locally invasive growth (1,7,15). Several potential characteristics
(including tumor size, location and patient age) have been
investigated as predictors of tumor behavior, but the specific
parameters of these predictors are yet to be determined (1,17).
A reassessment of the overall management of
fibromatosis has taken place over the last few years, and
preservation of function has become a priority (17–22). A
biopsy confirming diagnosis is mandatory and should be confirmed by
an expert pathologist. Immunostaining for β-catenin with nuclear
positivity is useful in establishing a diagnosis (15). Active surveillance has only been shown
to lead to spontaneous regression of 28–50% of cases of
extra-abdominal fibromatosis (18,22).
Surgery remains a valid option, however, preservation of function
and quality of life are essential (16,17,21). The
role of adjuvant radiotherapy also remains unclear, and the optimal
regimes, doses and durations of other systemic therapies (including
chemotherapy, hormonal therapy and tyrosine kinase inhibitors)
require elucidation (1,16,22).
Patients should be followed closely for at least 3 years to monitor
regression or recurrence (16).
Magnetic resonance scans are best suited to accurately reflect
disease progression or regression, or to assess treatment
response.
In conclusion, desmoid-like fibromatosis is a rare
breast neoplasm. Despite its classification as an intermediate
soft-tissue tumor, breast fibromatosis does possess the potential
for aggressive local behavior. Breast imaging examinations are not
specific for fibromatosis and often imitate breast cancer. Surgery
remains a valid option, however, preservation of function and
quality of life are essential. The role of adjuvant therapy is also
not entirely clear, and the optimal regimes, doses and durations of
systemic treatment of the disease require elucidation. Due to the
rare involvement of the breast in patients with desmoid-like
fibromatosis, the present study reports 2 cases with their clinical
features and histological findings in order to improve and add to
our knowledge of the disease.
References
|
1
|
Eastley N, McCulloch T, Esler C, Hennig I,
Fairbairn J, Gronchi A and Ashford R: Extra-abdominal desmoid
fibromatosis: A review of management, current guidance and
unanswered questions. Eur J Surg Oncol. 42:1071–1083. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Povoski SP, Marsh WL Jr, Spigos DG, Abbas
EA and Buchele BA: Management of a patient with multiple
recurrences of fibromatosis (desmoid tumor) of the breast involving
the chest wall musculature. World J Surg Oncol. 4:322006.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shen C, Zhou Y and Che G: Management of a
female with recurrence of fibromatosis of the chest wall adjacent
to the breast: A case report. J Cardiothorac Surg. 8:412013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Abbas AE, Deschamps C, Cassivi SD, Nichols
FC III, Allen MS, Schleck CD and Pairolero PC: Chest-wall desmoid
tumors: Results of surgical intervention. Ann Thorac Surg.
78:1219–1223. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Croce S, Letourneux C, Dale G and Mathelin
C: Breast fibromatosis: An uncommon benign breast disease. Gynecol
Obstet Fertil. 37:442–446. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Taylor TV and Sosa J: Bilateral breast
fibromatosis: Case report and review of the literature. J Surg
Educ. 68:320–325. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yamaguchi H, Sakakibara T, Hino M, Ryu M,
Senuma K, Nakai K, Tomiki Y, Sakamoto K, Kamano T, Tsurumaru M and
Matsumoto T: A case of fibromatosis of the breast. Breast Cancer.
9:175–178. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ha KY, Deleon P and Hamilton R: Breast
fibromatosis mimicking breast carcinoma. Proc (Bayl Univ Med Cent).
26:pp. 22–24. 2013; PubMed/NCBI
|
|
9
|
He P, Cui LG, Lei YT, Liu JY and Wang JR:
Ultrasound elastographic findings of mammary fibromatosis. Case Rep
Radiol. 2015:8294682015.PubMed/NCBI
|
|
10
|
Plaza MJ and Yepes M: Breast fibromatosis
response to tamoxifen: Dynamic MRI findings and review of the
current treatment options. J Radiol Case Rep. 6:16–23.
2012.PubMed/NCBI
|
|
11
|
Matherne TH, Green A Jr, Tucker JA and
Dyess DL: Fibromatosis: The breast cancer imitator. South Med J.
97:1100–1103. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jeong WS, Oh TS, Sim HB and Eom JS:
Desmoid tumor following augmentation mammoplasty with silicone
implants. Arch Plast Surg. 40:470–472. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hamada S, Futamura N, Ikuta K, Urakawa H,
Kozawa E, Ishiguro N and Nishida Y: CTNNB1 S45F mutation predicts
poor efficacy of meloxicam treatment for desmoid tumors: A pilot
study. PLoS One. 9:e963912014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nieuwenhuis MH, Casparie M, Mathus-Vliegen
LM, Dekkers OM, Hogendoorn PCW and Vasen HF: A nation-wide study
comparing sporadicand familial adenomatous polyposis-related
desmoid-type fibromatoses. Int J Cancer. 129:256–261. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rakha EA, Badve S, Eusebi V, Reis-Filho
JS, Fox SB, Dabbs DJ, Decker T, Hodi Z, Ichihara S, Lee AH, et al:
Breast lesions of uncertain malignant nature and limited metastatic
potential: Proposals to improve their recognition and clinical
management. Histopathology. 68:45–56. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kasper B, Baumgarten C, Bonvalot S, Haas
R, Haller F, Hohenberger P, Moreau G, van der Graaf WT and Gronchi
A; Desmoid Working Group, : Management of sporadic desmoid-type
fibromatosis: a European consensus approach based on patients' and
professionals' expertise-a sarcoma patients EuroNet and European
Organisation for Research and Treatment of Cancer/Soft Tissue and
Bone Sarcoma Group initiative. Eur J Cancer. 51:127–136. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fiore M, Rimareix F, Mariani L, Domont J,
Collini P, Le Péchoux C, Casali PG, Le Cesne A, Gronchi A and
Bonvalot S: Desmoid-type fibromatosis: A front-line conservative
approach to select patients for surgical treatment. Ann Surg Oncol.
16:2587–2593. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bonvalot S, Ternès N, Fiore M, Bitsakou G,
Colombo C, Honoré C, Marrari A, Le Cesne A, Perrone F, Dunant A and
Gronchi A: Spontaneous regression of primary abdominal wall desmoid
tumors: More common than previously thought. Ann Surg Oncol.
20:4096–4102. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Crago AM, Denton B, Salas S, Dufresne A,
Mezhir JJ, Hameed M, Gonen M, Singer S and Brennan MF: A prognostic
nomogram for prediction of recurrence in desmoid fibromatosis. Ann
Surg. 258:347–353. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Keus RB, Nout RA, Blay JY, de Jong JM,
Hennig I, Saran F, Hartmann JT, Sunyach MP, Gwyther SJ, Ouali M, et
al: Results of a phase II pilot study of moderate dose radiotherapy
for inoperable desmoid-type fibromatosis-an EORTC STBSG and ROG
study (EORTC 62991–22998). Ann Oncol. 24:2672–2676. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Colombo C, Miceli R, Le Péchoux C,
Palassini E, Honoré C, Stacchiotti S, Mir O, Casali PG, Dômont J,
Fiore M, et al: Sporadic extra abdominal wall desmoid-type
fibromatosis: Surgical resection can be safely limited to a
minority of patients. Eur J Cancer. 51:186–192. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Al-Jazrawe M, Au M and Alman B: Optimal
therapy for desmoid tumors: Current options and challenges for the
future. Expert Rev Anticancer Ther. 15:1443–1458. 2015. View Article : Google Scholar : PubMed/NCBI
|