Introduction
As one of the most common gynecological diseases,
the incidence rate of ovarian cancer has exceeded both endometrial
and cervical cancer, becoming one of the gynecological diseases
with high mortality rate (1).
Although research on ovarian cancer has achieved some progress,
definite diagnosis of ovarian cancer typically occurs at advanced
stages. Reasons for the late diagnosis include the deep location in
the pelvic cavity of ovarian cancer (2) and the absence of obvious symptoms in
early stages, which hampers the subsequent treatment (3). Therefore, early detection and treatment
are critical goals for the recovery of ovarian cancer patients
(4). In recent years, the development
of molecular biological techniques found that the CD44 gene
in chromosome 11 plays an importance regulatory role in lymphocyte
homing, movement, activation (5,6), signal
transduction, and adhesion among cells (7,8). The
CD44 gene contains 20 highly conserved exons including
constitutive exons and alternatively spliced exons in the V-area.
The structural domain encoded by the alternative exons in the
V-area has a close correlation with the incidence and deterioration
of many malignant tumors (9). For
example, the positive expression of CD44V is closely associated
with the poor prognosis of colon and breast cancer (10). Moreover, the deficiency of
CD44V has a close relationship with the poor prognosis of
bladder cancer (10), whereas
CD44V6 is involved in peritoneal metastasis, and high
expression of CD44V6 can severely disturb postoperative
recovery.
In the present study, we studied the expression of
CD44V6 in normal ovarian tissue, benign ovarian tissue, and ovarian
cancer. The results provide new experimental findings to assist in
the diagnosis and treatment of ovarian cancer.
Patients and methods
Patient data
We recruited 38 patients, admitted to the Hubei
Cancer Hospital (Hubei, China), who received gynecological surgery
for ovarian cancer from February 2014 to February, 2015. This
experimental group had an average age of 45.4 years. We also
recruited 23 patients with benign ovarian tumor with an average age
of 43.4 years and 20 with normal ovarian tissue with an average age
of 44.3 years. The patients with ovarian cancer were diagnosed
according to the Ovarian Cancer International Federation of
Gynecology and Obstetrics. Exclusion criteria for the study were:
Patients with other related gynecological diseases such as cervical
and endometrial cancer. This study was approved by the Ethics
Committee of Hubei Cancer Hospital. Signed written informed
consents were obtained from all participants before the study.
RNA extraction from ovarian cancer
cells
Ovarian samples were kept in liquid nitrogen at °C
until needed, then 0.1 g, was placed on ice, to which 0.6 ml of RNA
Plus was added (Takara Bio, Dalian, China). Samples were ground
quickly in precooled mortar and homogenates were transferred to 1.5
ml tube, washed with 0.3 ml of RNA Plus, and transferred to a
centrifuge tube, after which 200 µl of chloroform was added,
agitated for 15 sec and incubated on ice for 15 min. We centrifuged
samples at 10,000 × g for 15 min at 4°C. The supernatant was
transferred to a tube without RNase, and equivalent isopropanol was
added, mixed, and incubated on ice for 10 min, then centrifuged
again at 1,000 × g for 15 min at 4°C. The supernatant was removed
and 750 µl of 75% ethanol was added, with gentle mixing and
centrifugation at 10,000 × g for 10 min at 4°C. The supernatant was
then removed. RNase-free water was added and the total RNA was
measured.
Fluorogenic quantitative PCR
The procedure was conducted according to Takara
fluorogenic quantitative PCR instructions, with some modifications
(11). The primers for fluorogenic
quantitative PCR were synthesized by Suzhou Jinweizhi Biotechnology
(Suzhou, China) and the sequences are shown in Table I.
 | Table I.Fluorogenic quantitative PCR
primers. |
Table I.
Fluorogenic quantitative PCR
primers.
| Primers | Sequences |
|---|
| CD44V6-F |
GTCGATGCTAGCTAGCCGTAGCATG |
| CD44V6-R |
CGAGCTAGTCGTAGTCGATCGATCG |
| GAPDH-F |
GTCGATGGCTAGTCGTAGCATCGAT |
| GAPDH-R |
TGCTAGCTGGCATGCCCGATCGATC |
ELISA
We conducted enzyme-linked immunosorbent assay
(ELISA) following the instructions of the ELISA kit (Takara
Company) with minor modifications (12). The standard protein sample for ELISA
was diluted with assay buffer at 1:50 to create standard curve.
After dilution with phosphate-buffered saline (PBS) (pH 7.2) at
1:100, the samples were mixed with 100 µl of sample solution and 50
µl of detection solution, and incubated for 2 h at room
temperature. Then, TMB chromogenic substrate was added and light
absorption was measured at 495 nm. CD44V6 concentration was
calculated according to the standard curve. The primary mouse
monoclonal CD44V6 antibody (dilution, 1:500; cat. no. ab78960) and
secondary goat anti-rabbit (HRP) IgG antibody (dilution, 1:2000;
cat. no. ab6721) were from Abcam (Cambridge, MA, USA).
Western blot analysis
Total protein in the sample was extracted with the
protein extraction kit from Roche according to the manufacturer's
recommendations. Then, we proceeded with standard western blot
analysis procedures.
Immunohistochemistry
Immunohistochemistry SP-linking method was applied
in this study. Normal ovarian tissue, benign ovarian tumor, and
ovarian cancer samples were fixed in 10% formaldehyde, embedded in
paraffin, and sectioned at 4 µm. The sections were fixed on a glass
slide and placed in an oven for 2 h at 60°C. Then, we
de-paraffinized with xylene, re-dehydrated in ethyl alcohol
gradients, and hydrated by washing in PBS 5 times, heated and
boiled for 2 min in a pressure cooker. After cooling, the sections
were placed in PBS for 30 min at room temperature. Then, we added
50 µl of peroxidase blocker, incubated at 37°C for 10 min, and
washed in PBS 5 times. PBS solution was removed, and 45 µl of
pre-immune serum was added and incubated for 10 min at room
temperature. Then, primary antibody was added and incubated at room
temperature for 2 h (or overnight at 4°C), and washed 5 times in
PBS; 50 µl of streptomycin-HRP was added and incubated for 2 h at
room temperature, and washed 5 times in PBS; and 100 µl of
coloration solution was added and observed under the microscope.
After 10 min, followed washing with distilled water and re-dyeing
by hematoxylin for 5 min, washing again, dehydration in ethyl
alcohol gradient, air drying, and then the slides were sealed.
Quantification of stained slides
Positive immunohistochemical staining is the
accumulation of yellow particles in membrane or cytoplasm, which
was judged as positive. The standards for immunohistochemistry
showed (9) that membrane stain
<10% or negative tumor cells after stained were determined as
negative. Only the stained membrane or tumor cell with membrane
stain >10% was identified as positive. The results were judged
through the KI index, which was the numbers of positive cells in
each field.
Statistical analysis
SPSS 20.0 software (Chicago, IL, USA) was used to
process and analyze the data. CD44V6 protein expression in
different tissue samples was detected by χ2. The result
of immunohistochemistry KI index was tested by t-test.
Results
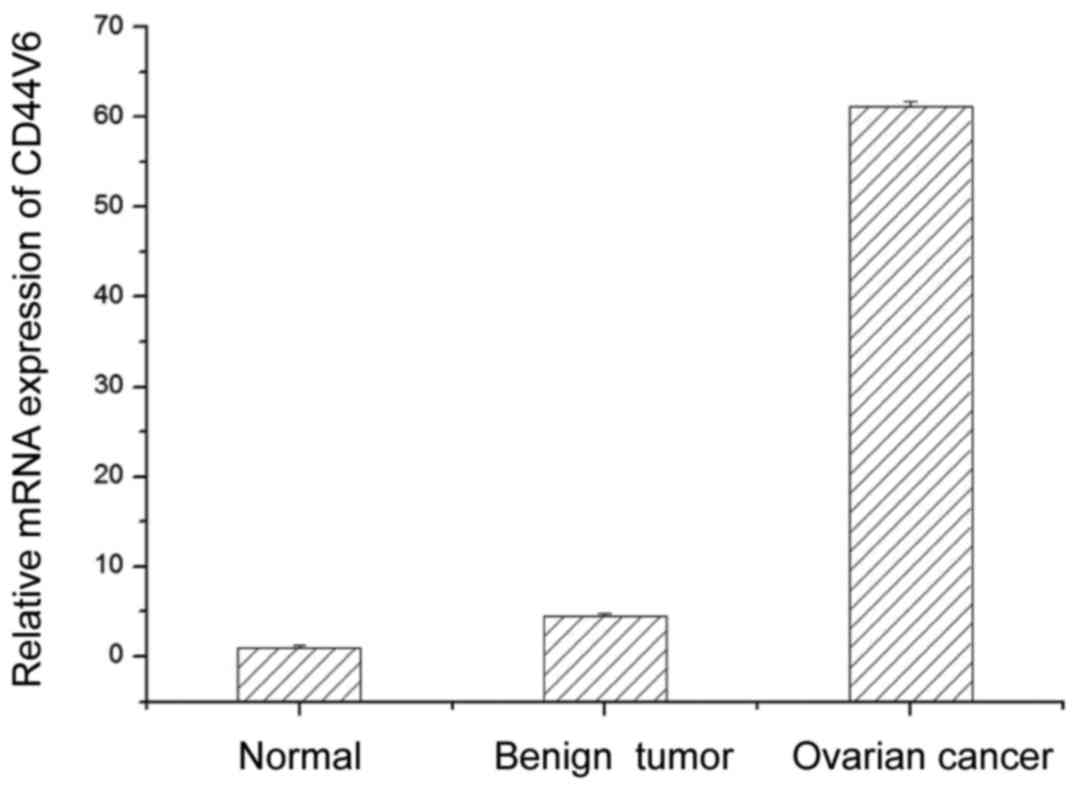
CD44V6 mRNA expression
To determine the role of CD44V6 in ovarian
cancer, we examined CD44V6 mRNA levels in ovarian cancer, and
benign and normal ovaries. Compared with normal ovaries, MEG-A3
mRNA content in benign ovarian tumor and ovarian cancer were
higher. CD44V6 mRNA expression in benign ovarian tumor was
4.5 times higher than in normal ovarian tissues. Moreover, the
expression of CD44V6 mRNA in ovarian cancer was 13.6-fold
higher than that in the benign ovarian tumor. These results
demonstrated that CD44V6 mRNA expression strongly associates
with ovarian tumors, with the highest values identifying ovarian
cancer (Fig. 1).
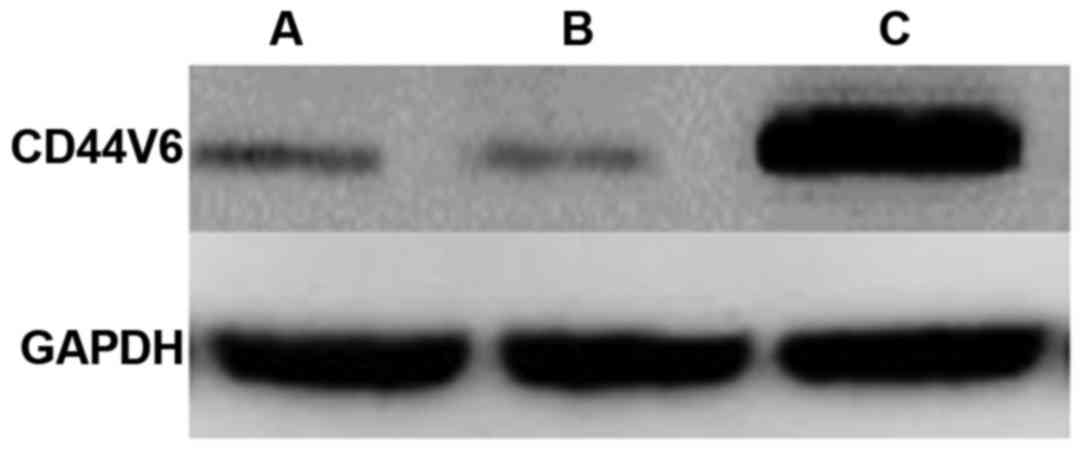
CD44V6 protein expression by western
blot analysis
After identifying strong upregulation of
CD44V6 at the mRNA level, we examined the expression of
CD44V6 protein by western blot analysis in normal ovarian tissue,
benign ovarian tumor, and ovarian cancer. We found no significant
difference in the expression of CD44V6 protein between normal
ovarian tissue and benign ovarian tumors (Fig. 2). However, CD44V6 protein content in
ovarian cancer tissue was significantly higher compared with normal
ovarian tissue and benign ovarian tumors (Fig. 2), which is consistent with the
upregulation of CD44V6 mRNA.
CD44V6 protein expression by
ELISA
After identifying strong upregulation of CD44V6
protein in ovarian cancer by western blot analysis, we verified
this result using a more quantitative technique. We found no
significant difference in CD44V6 protein expression between normal
ovarian tissue and benign ovarian tumors (Table II). However, CD44V6 expression was
significantly higher in ovarian cancer tissue than in normal
ovaries and in benign ovarian tumors (Table II). This further supports the
association of CD44V6 protein with ovarian cancer.
 | Table II.CD44V6 protein expression in normal
ovarian tissue, benign ovarian tumor and ovarian cancer. |
Table II.
CD44V6 protein expression in normal
ovarian tissue, benign ovarian tumor and ovarian cancer.
| Groups | CD44V6 protein
(µg) | P-value |
|---|
| Normal ovarian
tissue |
2.1±0.13 |
|
| Benign ovarian
tumor |
2.8±0.18 | >0.05 |
| Ovarian cancer | 16.2±0.21 | <0.05 |
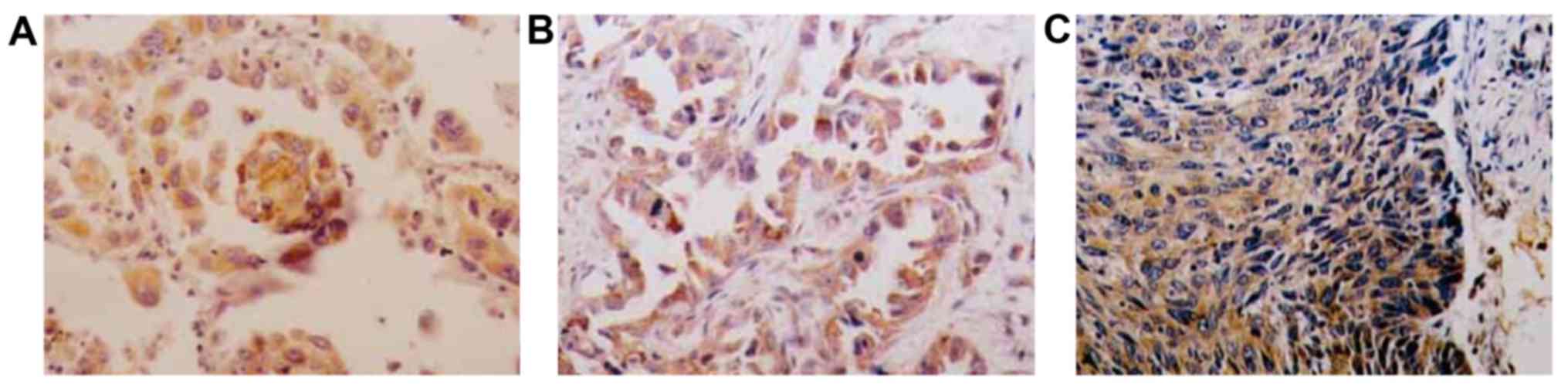
CD44V6 immunohistochemistry
To examine the accumulation and distribution of
CD44V6, we conducted immunohistochemistry on normal ovarian tissue,
benign ovarian tumor, and ovarian cancer (Table III). We found that CD44V6 was low in
normal ovarian tissue and slightly higher in benign ovarian tumor,
although the difference was not significant (Fig. 3 and Table
III). However, we found a large number of CD44V6-positive cells
in ovarian cancer (Fig. 3 and
Table III). These results are
consistent with the results with ELISA and western blot
analysis.
 | Table III.CD44V6-positive cells in normal
ovarian tissue, benign ovarian tumor, and ovarian cancer. |
Table III.
CD44V6-positive cells in normal
ovarian tissue, benign ovarian tumor, and ovarian cancer.
| Groups | Total no. of cells
(n) | CD44V6-positive
cells | CD44V6-positive
cells | KI value (%) | P-value |
|---|
| Normal ovarian
tissue | 400 | 35 | 365 | 8.75 |
|
| Benign ovarian
tumor | 400 | 51 | 349 | 12.75 | >0.05 |
| Ovarian cancer | 400 | 328 | 72 | 82.0 | <0.01 |
Discussion
CD44V6 is an adhesive molecule that plays an
important role in normal signal transduction and intercellular
material exchange (13–15). Overexpression of CD44V is associated
with malignant cell changes (16).
Overexpression of CD44V can promote the incidence and deterioration
of a malignant tumor to some extent (17). CD44V6 can be involved in the process
of cell invasion and the transformation of tumor cells (18). Further research showed that CD44V6 can
promote the fusion between capillary endothelial cells and tumor
cells, which enables tumor cells to avoid the immune system and
promote the transformation of tumor cells (19). In recent years, with research on
gynecological diseases such as endometrial cancer, it was proposed
that CD44V could be involved in the incidence and progression of
many gynecological diseases. For instance, CD44V expression in
cervical cancer tissue is significantly higher than that of normal
tissue (20).
The growing incidence of ovarian cancer has resulted
in more studies and relevant molecular and cellular discoveries. In
the present study, we found that CD44V6 is highly expressed in
ovarian cancer, suggesting that a high expression of CD44V6 can
promote the incidence and progression of ovarian cancer. Moreover,
we found that CD44V6 mRNA levels are significantly higher in
benign ovarian tumor compared to normal ovaries, but there was no
difference at the protein level. These results suggest a close
connection with the transformation of ovarian tissue, where
CD44V6 mRNA is first upregulated in benign tumor and higher
upregulation in malignant tumor results in elevated CD44V6. Thus,
CD44V6 expression is strongly associated with the tumorous
transformation of ovarian cells. Together with research in other
cancers, these results suggest that CD44V6 is directly responsible
for the transition from normal ovary to benign tumor to cancer.
Understanding the role of CD44V6 in ovarian cancer can help in
designing tests to improve early diagnosis and treatment of
advanced-stage ovarian cancer.
References
|
1
|
Zhang X, Ng WL, Wang P, Tian L, Werner E,
Wang H, Doetsch P and Wang Y: MicroRNA-21 modulates the levels of
reactive oxygen species by targeting SOD3 and TNFα. Cancer Res.
72:4707–4713. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ouyang YB, Lu Y, Yue S and Giffard RG:
miR-181 targets multiple Bcl-2 family members and influences
apoptosis and mitochondrial function in astrocytes. Mitochondrion.
12:213–219. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Webb PM, Purdie DM, Grover S, Jordan S,
Dick ML and Green AC: Symptoms and diagnosis of borderline, early
and advanced epithelial ovarian cancer. Gynecol Oncol. 92:232–239.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Singer CF, Tea MK, Pristauz G, Hubalek M,
Rappaport C, Riedl C and Helbich T: Guideline for the prevention
and early detection of breast and ovarian cancer in high risk
patients, particularly in women from HBOC (hereditary breast and
ovarian cancer) families. Wien Klin Wochenschr. 124:334–339.
2012.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yu P, Zhou L, Ke W and Li K: Clinical
significance of pAKT and CD44v6 overexpression with breast cancer.
J Cancer Res Clin Oncol. 136:1283–1292. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Afify A, Purnell P and Nguyen L: Role of
CD44s and CD44v6 on human breast cancer cell adhesion, migration,
and invasion. Exp Mol Pathol. 86:95–100. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Liang J, Jiang D, Griffith J, Yu S, Fan J,
Zhao X, Bucala R and Noble PW: CD44 is a negative regulator of
acute pulmonary inflammation and lipopolysaccharide-TLR signaling
in mouse macrophages. J Immunol. 178:2469–2475. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Matsumura Y, Hanbury D, Smith J and Tarin
D: Non-invasive detection of malignancy by identification of
unusual CD44 gene activity in exfoliated cancer cells. BMJ.
308:619–624. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Li J, Zha XM, Wang R, Li XD, Xu B, Xu YJ
and Yin YM: Regulation of CD44 expression by tumor necrosis
factor-α and its potential role in breast cancer cell migration.
Biomed Pharmacother. 66:144–150. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nagel S, Hirschmann P, Dirnhofer S,
Günthert U and Tzankov A: Coexpression of CD44 variant isoforms and
receptor for hyaluronic acid-mediated motility (RHAMM, CD168) is an
International Prognostic Index and C-MYC gene status-independent
predictor of poor outcome in diffuse large B-cell lymphomas. Exp
Hematol. 38:38–45. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shi J, Zhou Z, Di W and Li N: Correlation
of CD44v6 expression with ovarian cancer progression and
recurrence. BMC Cancer. 13:1822013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhao S, He JL, Qiu ZX, Chen NY, Luo Z,
Chen BJ and Li WM: Prognostic value of CD44 variant exon 6
expression in non-small cell lung cancer: a meta-analysis. Asian
Pac J Cancer Prev. 15:6761–6766. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jung T, Gross W and Zöller M: CD44v6
coordinates tumor matrix-triggered motility and apoptosis
resistance. J Biol Chem. 286:15862–15874. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang J, Xiao L, Luo CH, Zhou H, Zeng L,
Zhong J, Tang Y, Zhao XH, Zhao M and Zhang Y: CD44v6 promotes
β-catenin and TGF-β expression, inducing aggression in ovarian
cancer cells. Mol Med Rep. 11:3505–3510. 2015.PubMed/NCBI
|
|
15
|
Misra S, Heldin P, Hascall VC, Karamanos
NK, Skandalis SS, Markwald RR and Ghatak S: Hyaluronan-CD44
interactions as potential targets for cancer therapy. FEBS J.
278:1429–1443. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Heider KH, Kuthan H, Stehle G and Munzert
G: CD44v6: a target for antibody-based cancer therapy. Cancer
Immunol Immunother. 53:567–579. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Marhaba R and Zöller M: CD44 in cancer
progression: adhesion, migration and growth regulation. J Mol
Histol. 35:211–231. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Spiegelberg D, Kuku G, Selvaraju R and
Nestor M: Characterization of CD44 variant expression in head and
neck squamous cell carcinomas. Tumour Biol. 35:2053–2062. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ponta H, Sherman L and Herrlich PA: CD44:
from adhesion molecules to signalling regulators. Nat Rev Mol Cell
Biol. 4:33–45. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rassouli FB, Matin MM, Bahrami AR,
Ghaffarzadegan K, Cheshomi H, Lari S, Memar B and Kan MS:
Evaluating stem and cancerous biomarkers in CD15+CD44+ KYSE30
cells. Tumour Biol. 34:2909–2920. 2013. View Article : Google Scholar : PubMed/NCBI
|