Introduction
Yolk sac tumors (YSTs), also referred to as
endodermal sinus tumors, are a type of malignant germ cell tumor
that usually grow in the gonads (1).
In 1959, the tumor was identified in the ovaries and testes of
young patients, and defined as a specific form of malignant germ
cell neoplasm by Telium (2). YSTs are
difficult to identify in other sites outside the gonads. However,
between 10 and 15% of YST occur in the midline structures of the
mediastinum, retroperitoneum and sacrococcygeal areas (3). Certain cases have been reported in other
location such as in the pineal region and head and neck (4,5). No case
has been reported involving the upper lip. The present study
reports the case of a child with an isolated YST occurring in the
upper lip, and reviews 20 cases of primary YST of the head and neck
region, not including the intracranial and orbit regions, from the
literature since 1997.
Case report
A 13-month-old female damaged her upper lip upon
falling and the hematoma formed 2 months prior to admission to
hospital. The patient underwent a hematoma puncture drainage at
Juxian People's Hospital (Rizhao, Cina), but the mass recurred
quickly. Upon examination, an exogenous reddish mass measuring 4×5
cm in diameter was revealed at the midline of the upper lip. The
surface of the tumor was bleeding and scabby, as demonstrated in
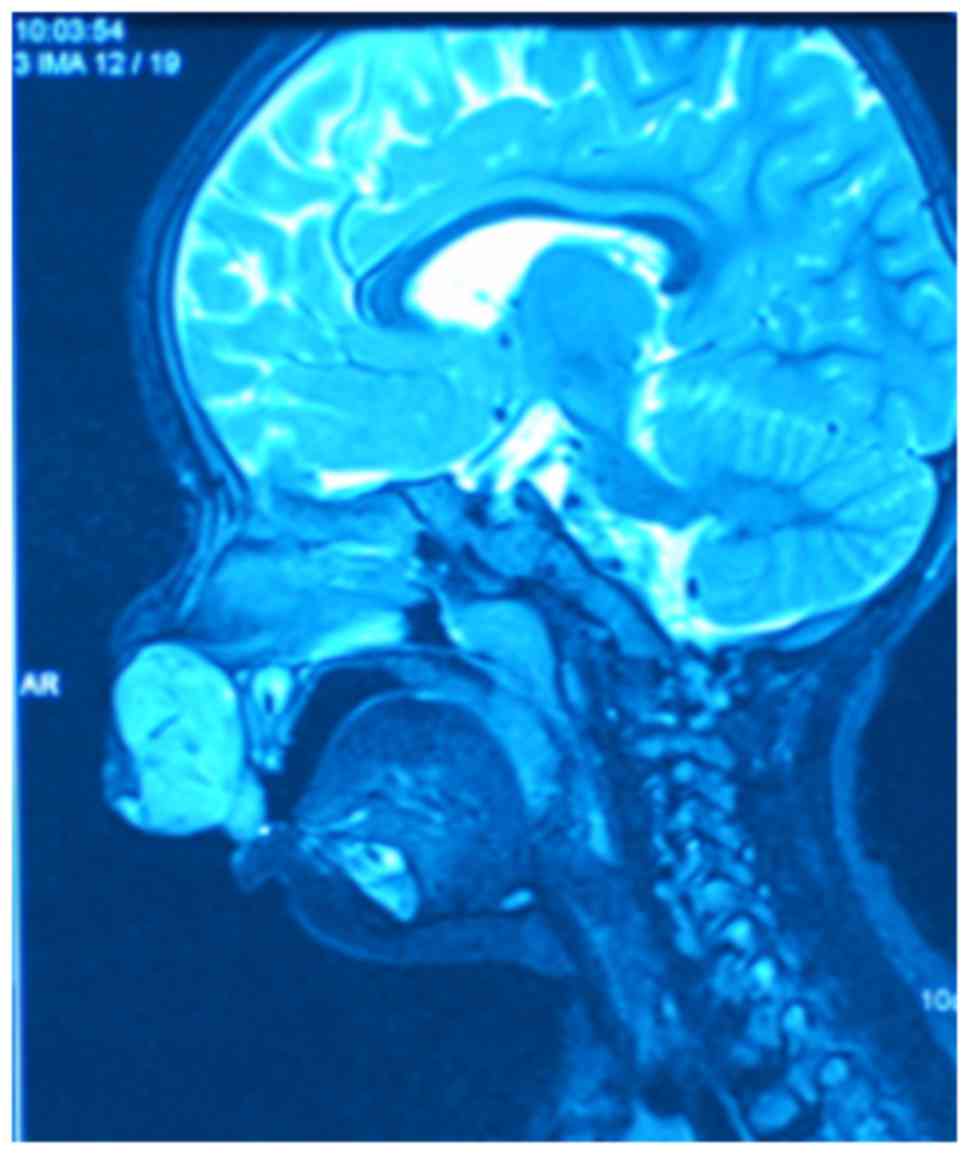
Fig. 1. Magnetic resonance imaging
demonstrated a strong signal mass on the fat suppression imaging T2
weighted image in the upper lip with a clear border, as illustrated
in Fig. 2. A biopsy sample was
obtained from the fleshy mass under general anesthesia and the
results confirmed the diagnosis of a YST. The biopsy sample was cut
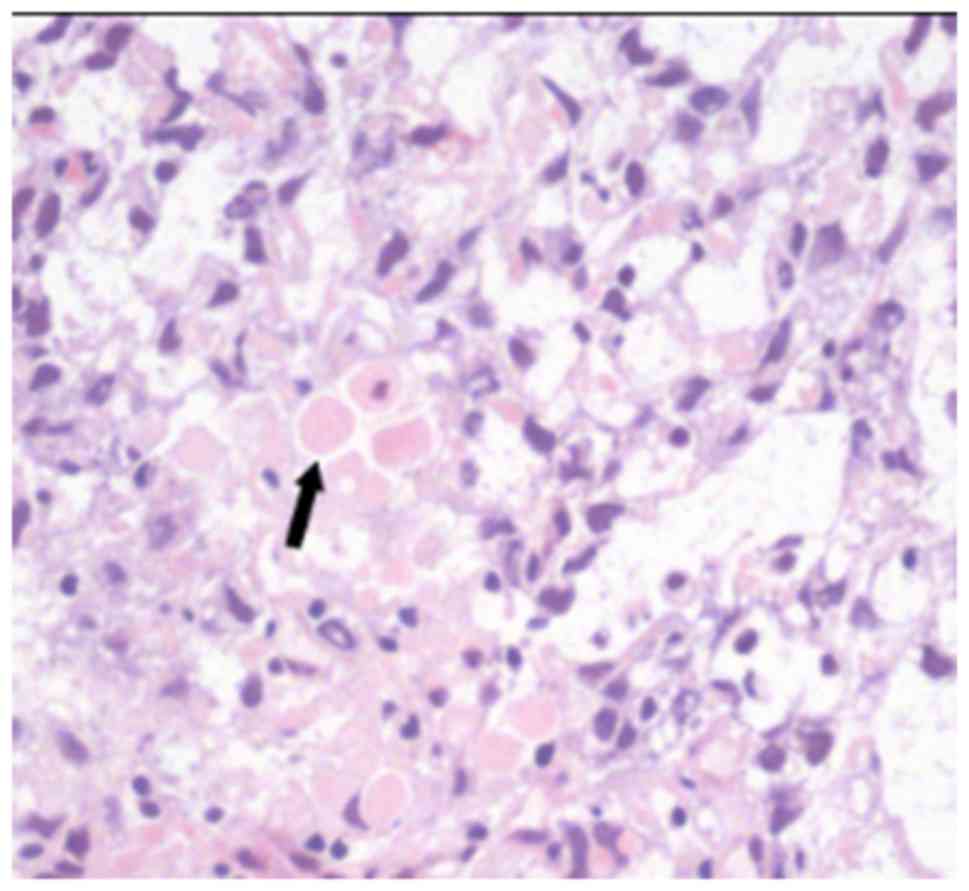
into pathological sections (4 µm thick). Certain pathological
sections underwent hematoxylin-eosin staining (stained with
hematoxylin-eosin at 60°C for 60 sec) and others underwent
immunohistochemical staining with α-fetoprotein (incubated with
anti-α-fetoprotein at 37°C for 2 h). Subsequently, the tissue
sections were observed using a biological microscope at a
magnification of ×400. Microscopic analysis revealed the
characteristic reticular pattern and eosinophilic ball, as
demonstrated in Fig. 3,
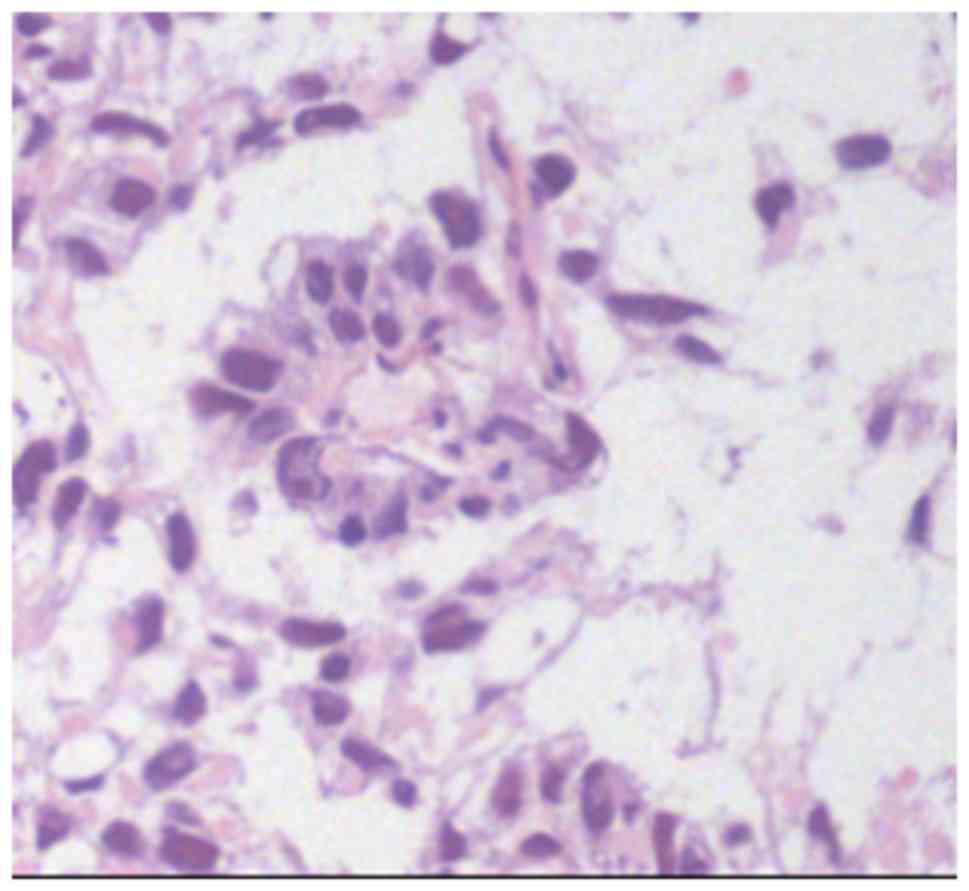
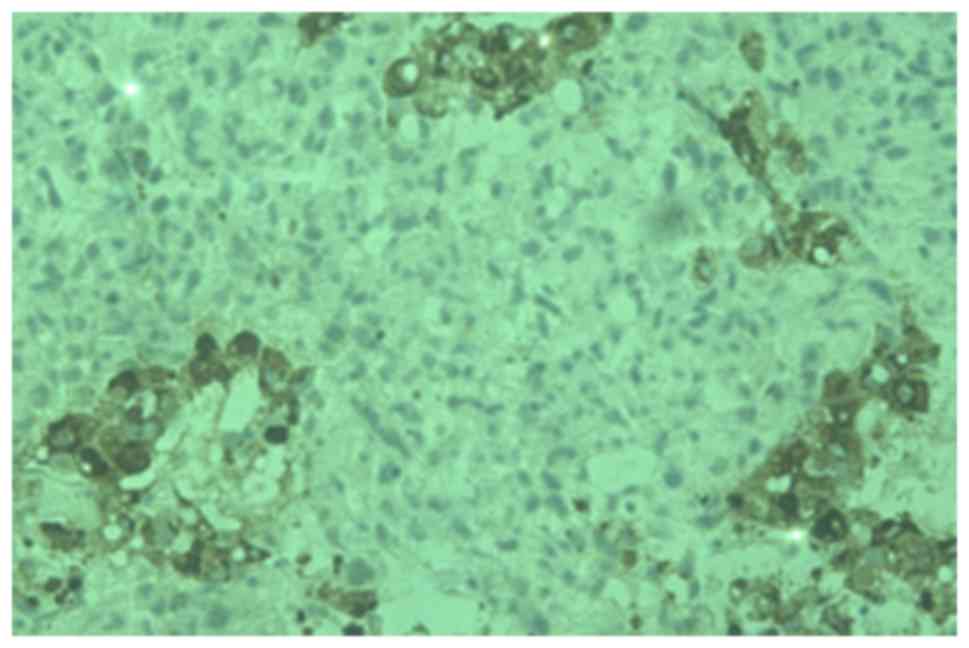
Schiller-Duval bodies, as illustrated in Fig. 4, and immunohistochemical staining
positive for α-fetoprotein (AFP), as demonstrated in Fig. 5. Laboratory screening revealed an AFP
level >1,308 µg/l, with 1–30 µg/l being the normal range.
Computerized tomography scans of the head, neck and thoracic
regions and ultrasonography of the abdominal and pelvic areas
demonstrated no signs of metastasis. Initial treatment comprised
two cycles of Adriamycin (30 mg/m2, day 2,9),
vincristine (1.5 mg/m2, day 1,8), cyclophosphamide (300
mg/m2, day 1–3) and cisplatin (90 mg/m2, day
1) (AVCP) chemotherapy and 1 cycle of ifosfamide (1.5
g/m2, day 1–5), etoposide (100 mg/m2, day
1–5) and vincristine (1.5 mg/m2, day 1,8) (IEV)
chemotherapy. Subsequent to this regimen, the mass in the upper lip
reduced to ~1×2 cm in diameter. The patient then underwent surgical
resection. The biopsies of the resected area revealed only
fibrosis, without any residual tumor tissue. The AFP level was
measured subsequent to chemotherapy and resection, and exhibited a
decline to within the normal range. After 36 months, there were no
signs of recurrence or metastasis at follow-up examination.
Discussion
YSTs are one of the most common types of malignant
germ cell tumor exhibited within the pediatric age group,
particularly in females (4,6). To the best of our knowledge, few cases
of YST in the head and neck have been reported, whilst no cases
have been reported involving the upper lip. Devaney and Ferlito
(5) reviewed 27 patients with primary
YSTs of the head and neck extracranial regions prior to 1997, and
Kamal et al (7) reviewed 16
patients with primary orbital YST, yet there has been no review of
those cases subsequent to 1997. Therefore, the present study
reviewed 20 patients with primary YST of the head and neck region,
not including intracranial and orbit region, occurring subsequent
to 1997, and discussed the clinical and pathological features of
YSTs, as summarized in Table I.
 | Table I.Clinical features of 20 patients with
head and neck yolk sac tumors. |
Table I.
Clinical features of 20 patients with
head and neck yolk sac tumors.
| Study/year
reported | Gender (M/F) | Age (y) | Primary site | Treatment | Follow-up
perioda | Outcome and
survival | (Refs.) |
|---|
| Kusamakumari, et
al 1997 | M | 1.5 | Palate | Surgical excision,
chemotherapy | Lost to
follow-up | Unknown | (13) |
| Kusamakumari, et
al 1997 | F | 1 | Neck | Incisional biopsy,
chemotherapy | Unknown | Died of
infection | (13) |
| Choufani, et
al 1998 | F | 26 mo | Ear | Surgical
excision | 3 months | Died of disease | (21) |
| Kutluhan, et
al 1998 | F | 7 mo | Gingival | Incisional
biopsy | 17 days | Died of disease | (14) |
| Gangopadhyay, et
al 1999 | M | 4 | Maxillary sinus | Incisional biopsy,
chemotherapy, radiotherapy | 15 years | Alive, no evidence of
disease | (22) |
| Frank, et al
2000 | M | 2.5 | Temporal bone | Recurrence after
surgical excision, chemotherapy | 6 months | Alive, no evidence of
disease | (23) |
| Gábris, et al
2001 | F | 3 y 9 mo | Nasal cavity | Incisional biopsy,
surgical excision, chemotherapy, radiotherapy | 7 years | Alive, no evidence of
disease | (24) |
| Westerveld, et
al 2001 | F | 3 | Maxillary sinus | Incisional biopsy,
surgical excision, chemotherapy | 10 months | Died of disease | (17) |
| Sredni, et al
2004 | F | 16 mo | Parotid gland | Surgical excision,
chemotherapy | 2 years | Alive, no evidence of
disease | (25) |
| Mishra, et al
2008 | M | 59 | Paranasal
sinuses | Incisional biopsy,
chemotherapy, surgical excision, radiotherapy | 1 year | Alive, no evidence of
disease | (26) |
| Filho, et al
2008 | M | 48 | Nasal cavity | Surgical excision,
radiotherapy | 7 years | Alive, no evidence of
disease | (27) |
| Steinbacher, et
al 2008 | F | 8 mo | Mandible | Incisional biopsy,
chemotherapy, surgical excision | 8 months | Alive, no evidence of
disease | (20) |
| Pasricha, et
al 2010 | F | 9 mo | Face | Incisional biopsy,
chemotherapy | Lost to
follow-up | Unknown | (28) |
| Furtado, et
al 2011 | F | 10 | Thyroid gland | Fine needle biopsy,
surgical excision, chemotherapy | 4 months | Alive, no evidence
of disease | (19) |
| Jin, et al
2011 | F | 6 | Floor of mouth | Surgical
excision | 2 months | Died of lung
metastasis | (9) |
| Mamoon, et
al 2011 | M | 4 | Parapharyngeal
space | Surgical excision,
chemotherapy | 1 year | Alive, no evidence
of disease | (29) |
| Rozbahany, et
al 2012 | F | 2 | Postauricular | Incisional biopsy,
surgical excision | 9 months | Alive, no evidence
of disease | (30) |
| Zhang, et al
2013 | F | 14 mo | Floor of mouth | Surgical
excision | 4 months | Died of
disease | (15) |
| Chuang, et
al 2014 | F | 1 y 3 mo | Sinonasal | Surgical excision,
chemotherapy | 13 months | Alive, no evidence
of disease | (31) |
| Mei, et al
2015 | F | 58 | Sinonasal | Incisional biopsy,
surgical excision, chemotherapy | 8 months | Alive, no evidence
of disease | (32) |
The mechanisms underlying primitive yolk sac cell
migration to the upper lip remain unknown. There are two principal
theories that have been put forward to explain the origin of
extragonadal germ cell tumors (EGCTs) (8). The first hypothesizes that during
embryonic development, those EGCTs arising from primordial germ
cells are caused by defects in the cell migration pathways. In the
4-week-old embryo, primordial germ cells first appear in the wall
of the yolk sac and migrate along the dorsal mesentery to the
genital ridge during embryogenesis (9). Certain germ cells may not complete this
migration, resulting in retention at several sites along the dorsal
wall of the embryo near the midline (9). This provides the basis for the midline
propensity of the case reported in the present study, but does not
explain the development of EGCTs in the out-of-midline regions. The
second theory suggests that EGCTs arise from totipotential cells,
which are scattered throughout numerous areas of the body during
embryonic development and normally remain dormant. However, these
cells possess the potential for additional growth and
differentiation when suitably stimulated, leading to the formation
of EGCTs (8).
In the rare case discussed in the present study the
diagnosis was established by histological and immunohistochemical
examinations. The major pathologic characteristics of YSTs include
a reticular pattern, a solid pattern, a hepatoid pattern with
hyaline globules, a festoon pattern, enteric differentiation,
Schiller-Duval bodies, the presence of a granulomatous tissue
reaction and a polyvesicular vitelline pattern (10,11).
Schiller-Duval bodies have been reported as a common feature to
extragonadal YSTs, as observed in large quantities in a previous
study (12). Typical Schiller-Duval
bodies comprise cuboidal or low columnar-shaped tumor cells
surrounding the capillaries of a thin-walled sinus (13,14).
Immunohistochemically, AFP is an important tumor biomarker for
diagnosis (15). Immunofluorescent
techniques have been developed to localize the site of AFP
synthesis in YST samples (16). The
serum level of AFP was elevated in the patient of the present
study, and reduced subsequent to excision of the tumor. The serum
levels of the protein may be used as a tumor biomarker during
diagnosis, and in the follow-up of patients with YST (14,17).
Similar to testicular tumors, YSTs generally exhibit
a poor prognosis as they tend to recur locally and demonstrate a
high incidence of metastasis (18).
Consequently, therapy includes extensive surgical resection, an
intensive combination of chemotherapies and occasionally radiation
therapy (19). Chemotherapy may
improve the prognosis between 20–50% for YSTs (18). The combination of cisplatin, bleomycin
and etoposide has been demonstrated to be effective, and is the
most common type of chemotherapeutic regimen (4). The patient of the present study was
administered AVCP chemotherapy. When the first cycle of AVCP
chemotherapy was completed, the patient exhibited bone marrow
suppression associated with an infection and high fever.
Consequently, treatment was altered temporarily to IEV
chemotherapy. Subsequent to 3 cycles of chemotherapy, the tumor
mass of our case almost entirely disappeared and the patient was
eligible for surgical resection All cases of YST should receive
adjuvant chemotherapy except primary testicular tumors, which
exhibit excellent responses to surgery alone (20).
The present study reported the first case of an
isolated YST in the upper lip. The histology and AFP elevation were
typical for this tumor. In the case of the present study, the YST
was cured through effective chemotherapy and surgical resection.
The patient remained asymptomatic after 36 months and exhibited no
sign of recurrence or metastasis. According to data of previous
studies, multimodal therapy including surgery, chemotherapy and
radiotherapy may achieve a good prognosis.
References
|
1
|
Brodeur GM, Howarth CB, Pratt CB, Caces J
and Hustu HO: Malignant germ cell tumors in 57 children and
adolescents. Cancer. 48:1890–1898. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Telium G: Endodermal sinus tumors of the
ovary and testes. Comparative morphogenesis of the so-called
mesonephroma ovarii (Schiller) and extraembryonic (yolk
sac-allantoic) structures of the rat's placenta. Cancer.
12:1092–1105. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shebib S, Sabbah RS, Sackey K, Akhtar M
and Aur RJ: Endodermal sinus (yolk sac) tumor in infants and
children. A clinical and pathological study: An 11 year review. Am
J Pediatr Hematol Oncol. 11:36–39. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Devaney KO, Perlito A and Rinaldo A:
Endodermal sinus tumor (yolk sac tumor) of the temporal bone: An
exotic disease for otorhinolaryngologists and head and neck
surgeons. Acta Otolaryngol. 123:747–748. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Devaney KO and Ferlito A: Yolk sac tumors
(endodermal sinus tumors) of the extracranial head and neck
regions. Ann Otol Rhinol Laryngol. 106:254–260. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Harms D and Jänig U: Germ cell tumours of
childhood. Report of 170 cases including 59 pure and partial
yolk-sac tumours. Virchows Arch A Pathol Anat Histopathol.
409:223–239. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kamal S, Kaliki S, Sreedhar A and Mishra
DK: Primary orbital yolk sac tumor: Report of a case and review of
literature. Int Ophthalmol. 36:435–444. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brown NJ: Teratomas and yolk-sac tumors. J
Clin Pathol. 29:1021–1025. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jin X, Han C and Sun H: Primary yolk sac
tumor in floor of mouth in a child. J Oral Maxillofac Surg.
69:1973–1977. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Narita T, Moriyama Y and Ito Y: Endodermal
sinus (yolk sac) tumor of the liver. A case report and review of
the literature. J Pathol. 155:41–47. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Robban JT and Zaloudek C: Ovarian yolk sac
tumors. Pathol Case Rev. 11:50–57. 2006. View Article : Google Scholar
|
|
12
|
Juckes AW, Fraser MM and Detxer D:
Endodermal sinus (yolk sac) tumors in infants and children. J
Pediatr Surg. 14:520–524. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kusumakumari P, Geetha N, Chellam VG and
Nair MK: Endodermal sinus tumors in the head and neck region. Med
Pediatr Oncol. 29:303–307. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kutluhan A, Uğraş S and Akman E:
Endodermal sinus (yolk sac) tumor of oral cavity originating from
gingiva. Auris Nasus Larynx. 25:459–462. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang Q, Huang Y, Bao CY and Li LJ: Yolk
sac tumour involving floor of mouth: Case report. Br J Oral
Maxillofac Surg. 51:e67–e69. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wold LE, Kramer SA and Farrow GM:
Testicular yolk sac and embryonal carcinomas in pediatric patients:
Comparative immunohistochemical and clinicopathologic study. Am J
Clin Pathol. 81:427–435. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Westerveld GJ, Quak JJ, Bresters D, Zwaan
CM, van der Valk P and Leemans CR: Endodermal sinus tumor of the
maxillary sinus. Otolaryngol Head Neck Surg. 124:691–692. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ablin AR, Krailo MD, Ramsay NK,
Malogolowkin MH, Isaacs H, Raney RB, Adkins J, Hays DM, Benjamin
DR, Grosfeld JL, et al: Results of treatment of malignant germ cell
tumors in 93 children: A report from the Children's Cancer Study
Group. J Clin Oncol. 9:1782–1792. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Furtado LV, Leventaki V, Layfield LJ,
Lowichik A, Muntz HR and Pysher TJ: Yolk sac tumor of the thyroid
gland: A case report. Pediatr Dev Pathol. 14:475–479. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Steinbacher DM, Upton J, Rahbar R and
Ferraro NF: Yolk sac tumor of the mandible. J Oral Maxillofac Surg.
66:151–153. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Choufani G, Saussez S, Detemmerman D,
Salmon I, Tainmont J, Louryan S, Remmelink M and Hassid S: Yolk sac
tumor of the ear in a child. Am J Otol. 19:298–300. 1998.PubMed/NCBI
|
|
22
|
Gangopadhyay K, McArthur PD, Martin JM and
Saleem M: Endodermal sinus tumor of the maxillary sinus: A case
report. Ear Nose Throat J. 78(376–377): 381–382. 1999.
|
|
23
|
Frank TC, Anand VK and Subramony C: Yolk
sac tumor of the temporal bone: Report of a case. Ear Nose Throat
J. 79(183): 187–188, 191–192. 2000.
|
|
24
|
Gábris K, Orosz M and Suba Z: The effects
on teeth of radiotherapy for nasal endodermal sinus tumor (yolk sac
tumor) in childhood. Int J Oral Maxillofac Surg. 30:356–358. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sredni ST, da Cunha IW, de Carvalho Filho
NP, Magrin J, Pinto CA and Lopes LF: Endodermal sinus tumor of the
parotid gland in a child. Pediatr Dev Pathol. 7:77–80. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mishra A, El-Naggar AK, DeMonte F and
Hanna EY: Endodermal sinus tumor of the paranasal sinuses. Head
Neck. 30:539–543. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Filho BC, McHugh JB, Carrau RL and Kassam
AB: Yolk sac tumor in the nasal cavity. Am J Otolaryngol.
29:250–254. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Pasricha S, Gupta A, Shah M and Vadodaria
H: Extragonadal yolk sac tumor of face in a female infant: A case
report. Indian J Pathol Microbiol. 53:592–593. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mamoon N, Jaffri SA, Ilahi F, Muzaffar K,
Iqbal Y, Akhter N, Nasir H and Ahmad IN: Yolk sac tumour arising in
mature teratoma in the parapharyngeal space. J Pak Med Assoc.
61:1025–1027. 2011.PubMed/NCBI
|
|
30
|
Rozbahany NA, Hasanzadazar M, Latifi H,
Mohammadi A, Ilkhanizadeh B and Ghasemi-Rad M: Yolk-sac tumor of
the postauricular region: Case report and review of the literature.
J Oral Maxillofac Surg. 70:1891–1895. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chuang HC, Kang CJ and Lee LY: Sinonasal
pure yolk sac tumor: A case report and literature review. Fetal
Pediatr Pathol. 33:127–134. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Mei X, Xia Y, Sasano H and Gao H:
Sinonasal yolk sac (Endodermal sinus) tumor in an adult female-A
case report and review of the literature. APMIS. 123:810–814. 2015.
View Article : Google Scholar : PubMed/NCBI
|