Introduction
Calcifying cystic odontogenic tumor (CCOT) is a
novel classification of calcifying odontogenic cyst (COC) that was
recommended by the 2005 classification of the World Health
Organization (WHO) (1). COC was first
described as a likely analogue of the calcifying epithelioma of
Malherbe (also termed pilomatricoma or pilomatrixoma) in a study by
Gorlin et al in 1962 (2);
therefore, the eponym of ‘Gorlin cyst’ is frequently used (3,4). The
histopathological features of this pathological entity are the most
notable, including a cyst lining demonstrating characteristic
‘ghost’ epithelial cells with a propensity to calcify, and the
occasional association of this observation with certain odontogenic
tumors, including odontoma and ameloblastoma (5). An association is often found between COC
and impacted or displaced adjacent teeth. By contrast, dentigerous
cysts (DC) are the second most common type of odontogenic cyst,
following radicular cysts (6). DCs
form at a frequency of 1.44/100 unerupted teeth, representing
~17.1% of all true jaw cysts (7).
According to the WHO classification of jaw cysts, DC is defined as
an epithelial developmental odontogenic cyst (8). As for CCOT and DC, certain studies have
observed recurrent cases with subsequent malignant transformation
(9,10). The present study describes the case of
a 13-year-old boy who exhibited CCOT and DC within the same cavity,
an occurrence that, to the best of our knowledge, has not been
previously identified in the literature. Although they may have
arisen coincidentally, the presence of two odontogenic lesions in
the same cavity in the same patient, one of which is categorized as
a neoplasm and the other as a cyst, raises the question regarding
their origin and growth process. These issues are investigated in
the present study, with a brief review of the literature.
Case report
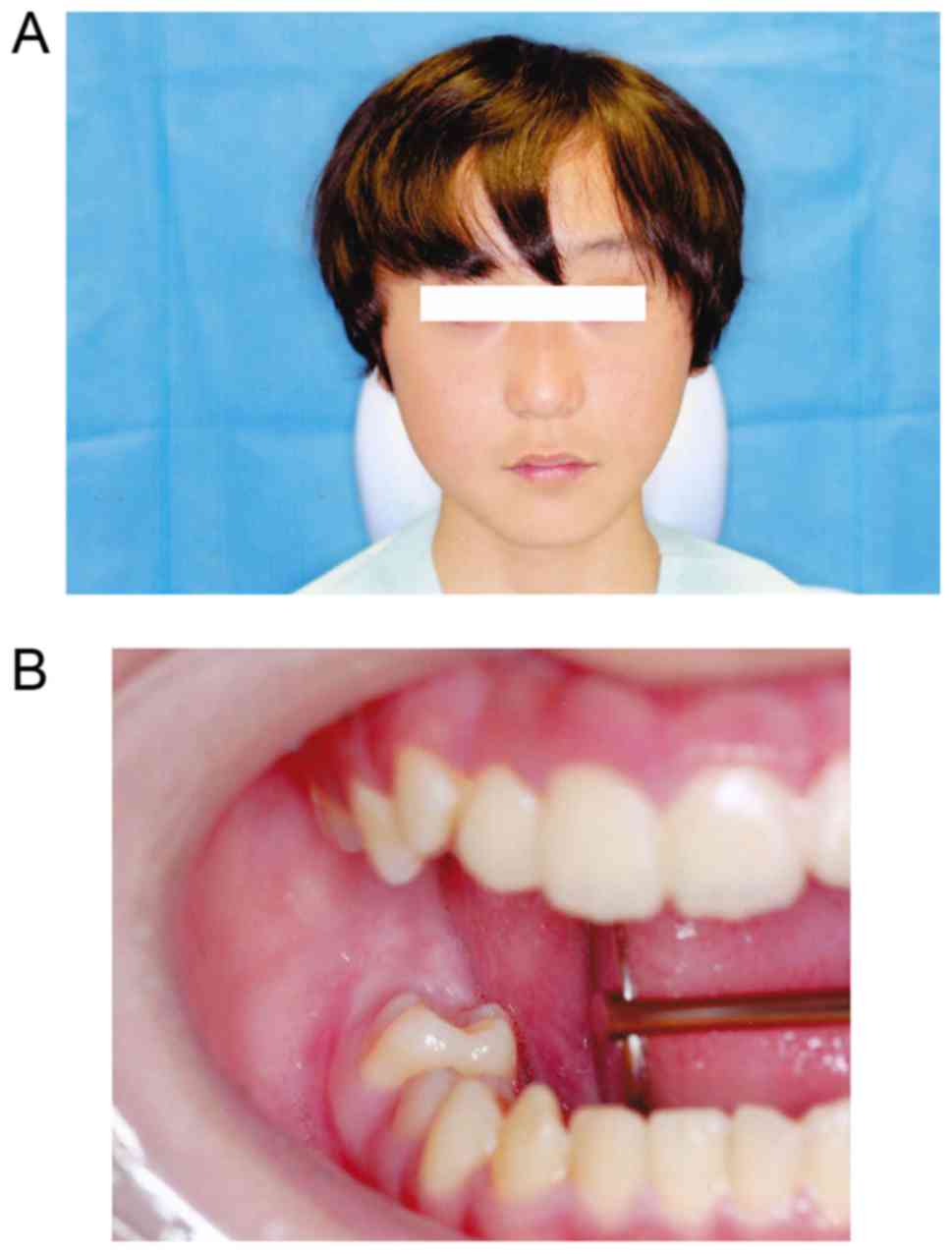
A 13-year-old asymptomatic Japanese boy was referred
to the outpatient clinic of the Osaka Dental University Hospital
(Osaka, Japan) on March 23rd, 2015 by a dentist for additional
investigation of an area of radiolucency in the lower right molar
area. The lesions were first detected on conventional radiographs
at a local dental clinic that the patient had visited for dental
checkups. Clinical examination revealed slight facial asymmetry and
no intra-oral swelling (Fig. 1). The
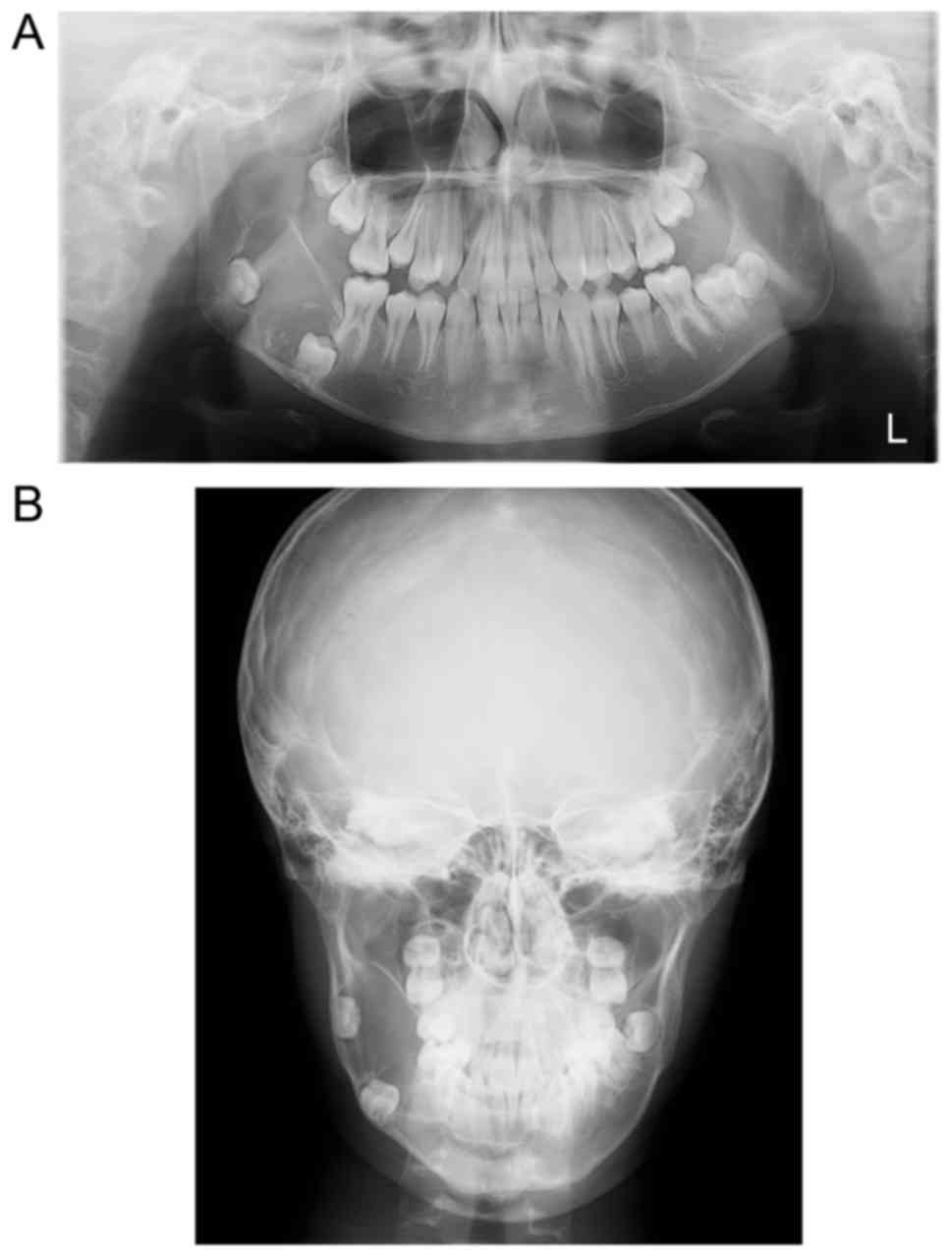
initial conventional radiograph was obtained using panoramic
equipment (Super Veraview X500 AE; J Morita Manufacturing Corp.,
Kyoto, Japan) at 78 kV, 9 mA, and conventional equipment
(UD150B-10; Shimadzu Corp., Kyoto, Japan) at 60 kV, 200 mA; this
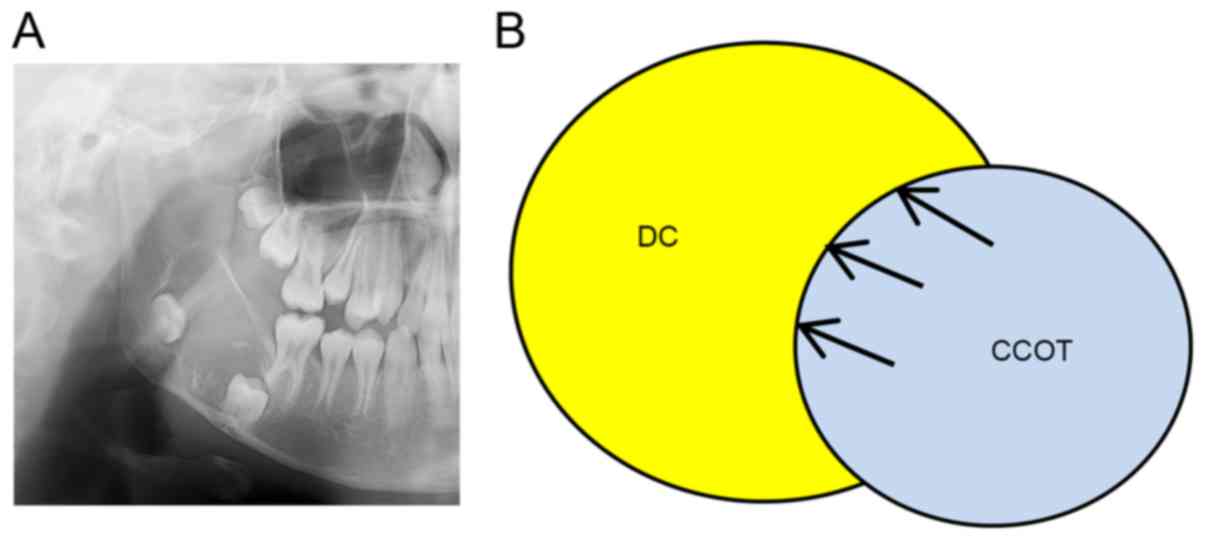
revealed the presence of a well-defined, unilocular, radiolucent
lesion with a smooth margin associated with impacted lower right
second and third molars. The outline of the whole lesion
encompassed an area of scalloping between the two impacted molars,
although none of the observations were indicative of the presence
of a septum inside the lesion. Large and small radio-opaque bodies
formed a perimeter in the lesion around the impacted lower right
second molar, which are characteristics specifically observed in
CCOT. Radio-opaque bodies were thinly spaced in the distal portion
of the lesion. Root resorption or displacement of the lower right
first molar was indistinct, although the lesion was located close
to the distal side of the first molar. The mandibular canal was
shifted downward due to pressure from the lesion (Fig. 2). The quality of the intraoral
radiograph was poor as the X-ray sensor induced the patient's gag
reflex.
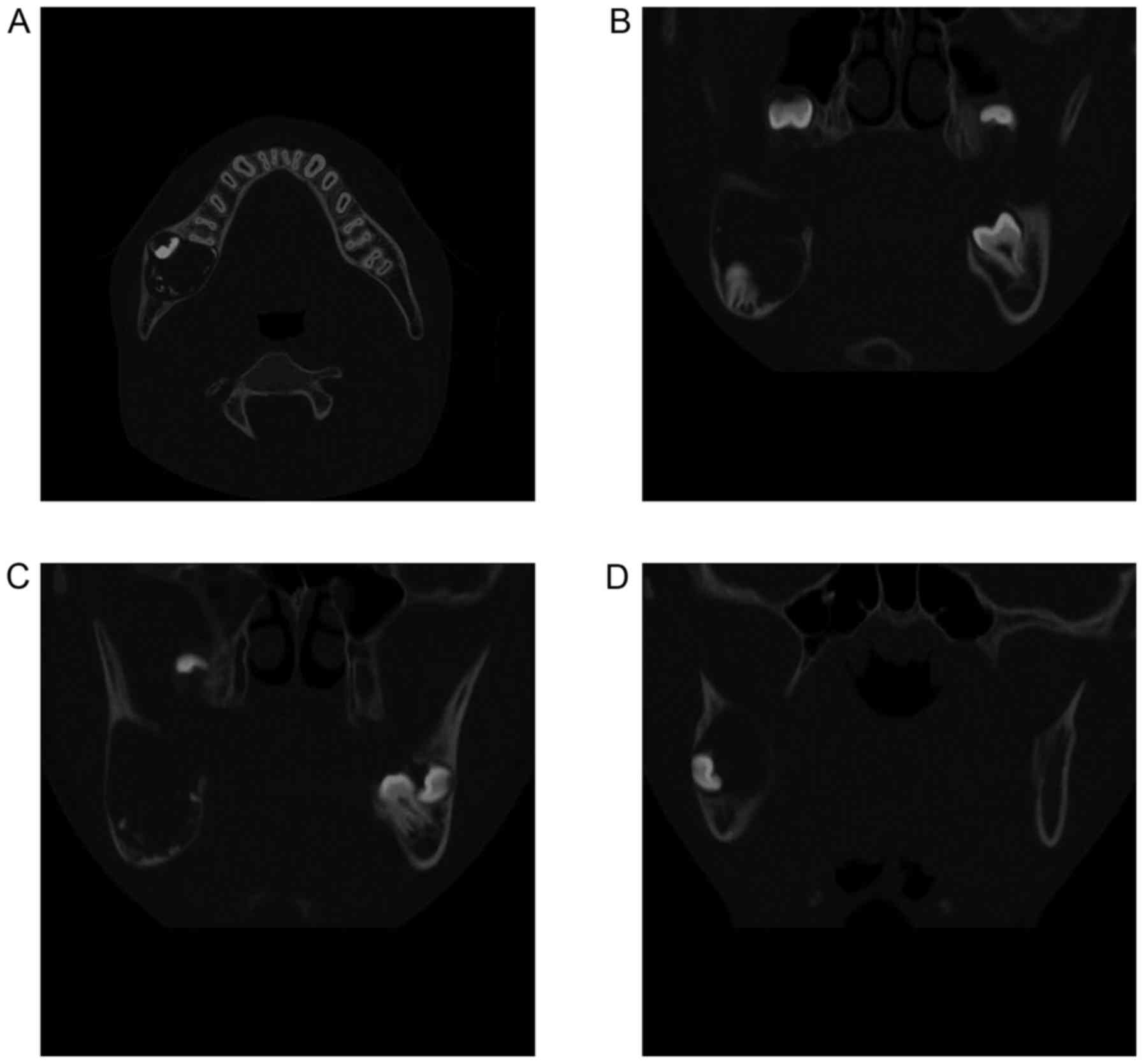
Computed tomography (CT) images were obtained using
a CT scanner (BrightSpeed Elite; GE Healthcare, Chicago, IL, USA)
at 120 kV. The electrical current was automatically optimized for
the object thickness (maximum, 120 mA). In addition, the CT was
performed according to the following parameters: Slice thickness,
0.65 mm; pitch and tube voltage, 0.625:1; and field of view, 16.8
cm2. CT images revealed a 20-mm sized, elliptical,
well-defined, unilocular expanding lesion with thinned buccolingual
cortical plates in the right mandible molar area (Fig. 3). Lower right second and third molars
were impacted underneath the bulk of the lesion, near the inferior
margin of the mandible. Large and small radio-opaque bodies lined
the margin of the mesial lesion around the impacted lower right
second molar. Radio-opaque bodies were poorly detected in the
distal portion around the impacted third molar. The mandibular
canal near the lesion was shifted downward. There were no
observations that indicated the existence of a septum. These
results were consistent with those of the panoramic radiograph,
providing additional information concerning buccolingual bony
expansion. The CT value of the radiolucency inside the lesion was
30 HU, representing fluid, and that of the radio-opaque bodies was
~1,200 Hounsfield units, suggesting that they were tooth-like
masses.
Overall, the imaging diagnosis was of a CCOT. The
lesion was judged to be a single mass due to the absence of a
septum. It was hypothesized that the CCOT had displaced or
prevented the eruption of molars, as the development of CCOT and
tooth eruptions occurred concurrently.
Following fenestration and incisional biopsy,
histopathological examinations were performed. The specimens were
fixed in 10% formalin solution and embedded in paraffin at room
temperature for 24 h. Samples were sliced into 2-µm-thick sections,
deparaffinized in l-limonene (Hemo-D, FALMA Co., Ltd., Tokyo,
Japan) and dehydrated through a graded ethanol series (80, 90, 95
and 100%). Antigen retrieval was performed by autoclaving at 121°C
for 15 min in retrieval buffer (pH 6.0; Mitsubisi Kagaku Yatoron,
Tokyo, Japan). Subsequent to autoclaving, slides were allowed to
cool down to room temperature. The endogenous peroxidase activity
was blocked with 3% hydrogen peroxidase, and non-specific reactions
were blocked with 2% normal horse serum (Vector Laboratories, Inc.,
Burlingame, CA, USA). The section was incubated with anti-human
B-cell lymphoma-2 (Bcl-2) oncoprotein mouse monoclonal antibody
(1:100, clone 124, cat. no. M0887, lot no. 00056477, Dako; Agilent
Technologies, Inc., Santa Clara, CA, USA). This antibody was
incubated for 60 min at room temperature. Subsequently, the section
was incubated with peroxidase conjugated anti-mouse antibody (1:1,
cat. no. 10037259, Dako; Agilent Technologies, Inc.) for 30 min at
room temperature. The section was visualized by
3,3′-diaminobenzidine-tetrahydrochloride and counterstained with 1%
hematoxylin at room temperature for 60 min. As a negative control,
a non-immunized antibody [mouse immunoglobulin G (cat. no. X0943,
lot no. 012C013; dilution, 1:1,000 Dako; Agilent Technologies,
Inc.)] was used instead of primary antibodies. The specimen was
independently interpreted by two pathologists without using any
software. If decisions between the pathologists differed, agreement
was reached by consensus decision-making.
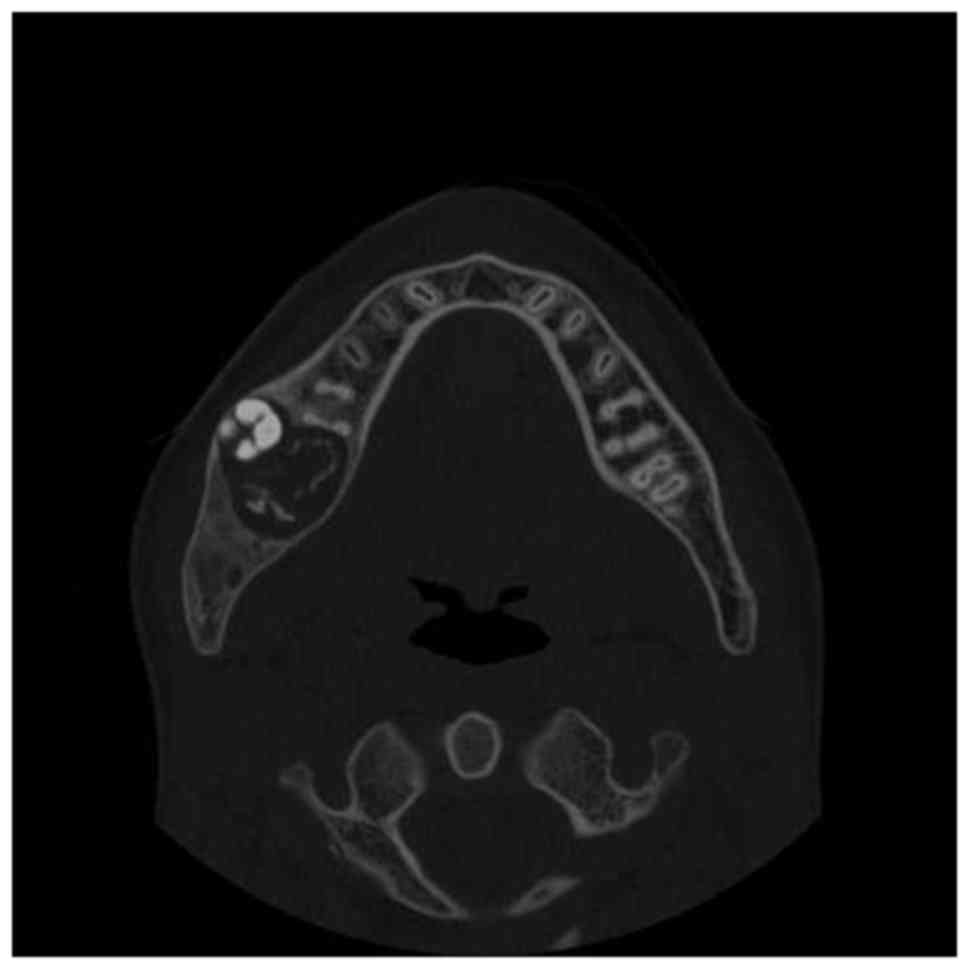
The histopathological results demonstrated that the
lesion may have been an odontogenic fibroma with odontogenic
epithelium. CT was performed 3.5 months after the initial CT and it
was observed that the calcification inside the lesion had increased
in the interval between the fenestration and the tumor excision
(Fig. 4).
With a tentative diagnosis of a benign odontogenic
tumor of the mandible, surgical enucleation under general
anesthesia was performed. The patient underwent surgical treatment
with extensive bone curettage and extraction of the lower right
second and third molars 4 months after the fenestration.
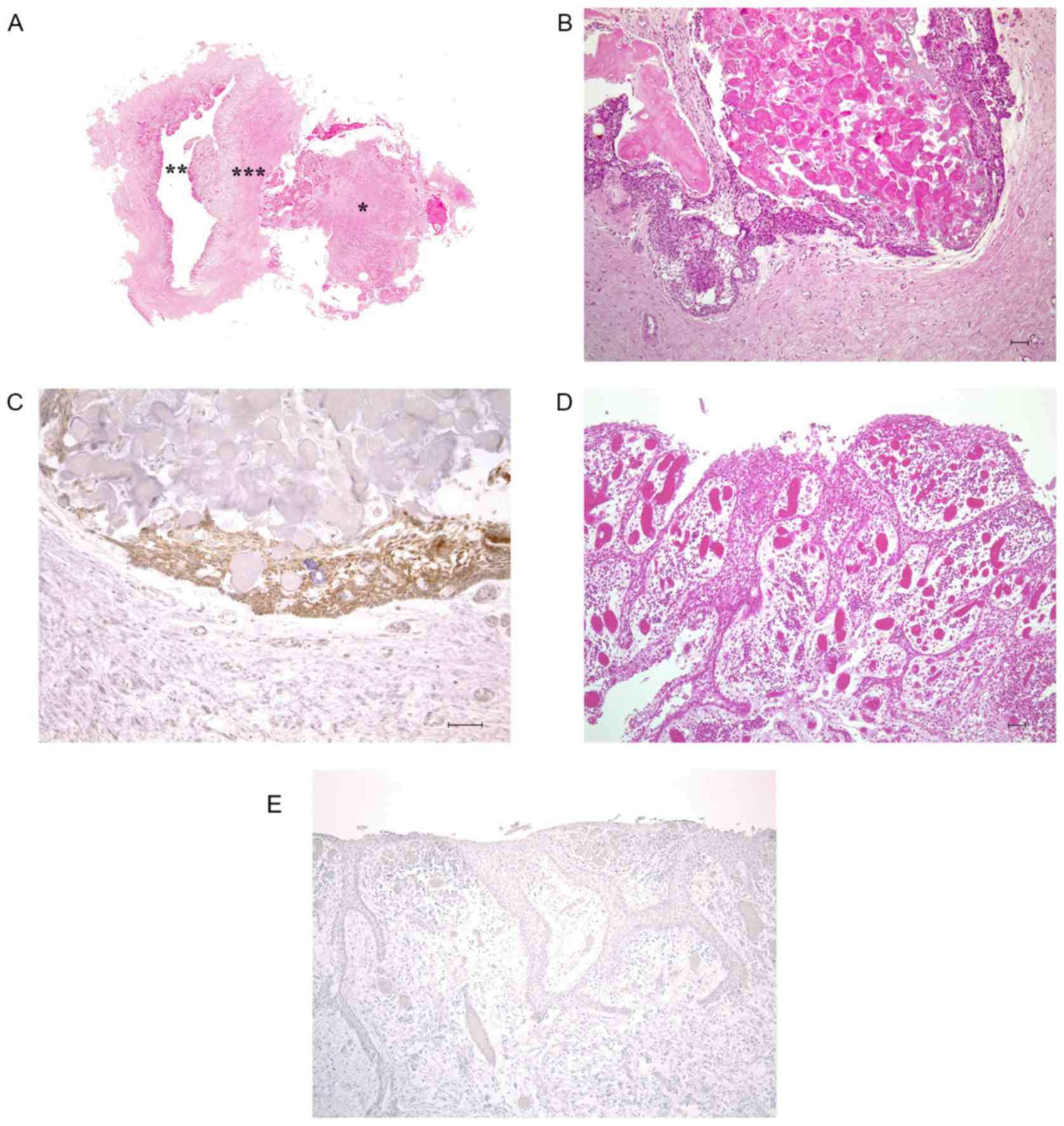
Histopathological examination of the whole-mount
section of the excisional biopsy specimens, sectioned in a
mesiodistal direction, demonstrated that the lesion exhibited two
distinctive features (Fig. 5A). In
the mesial portion around the lower right second molar, the cystic
wall was lined by an ameloblastomatous epithelium with dentin-like
structures, ‘ghost cells’ and numerous calcified particles
(Fig. 5B). Only this portion of the
specimen was stained by an antibody against Bcl-2 protein, the
presence of which distinguishes tumors from other pathologies and
is associated with the mechanism of apoptosis (11,12), which
confirmed the existence of tumor cells (Fig. 5C). Conversely, in the distal portion
around the third molar, the cystic lesion was lined by
unkeratinized stratified squamous epithelia that included an area
of proliferation due to inflammation caused by the fenestration
(Fig. 5D). This portion did not
demonstrate any expression of Bcl-2 protein (Fig. 5E). These histopathological results
supported the diagnoses of a CCOT and DC. A thick layer of collagen
fiber was also observed between the two different histopathological
entities.
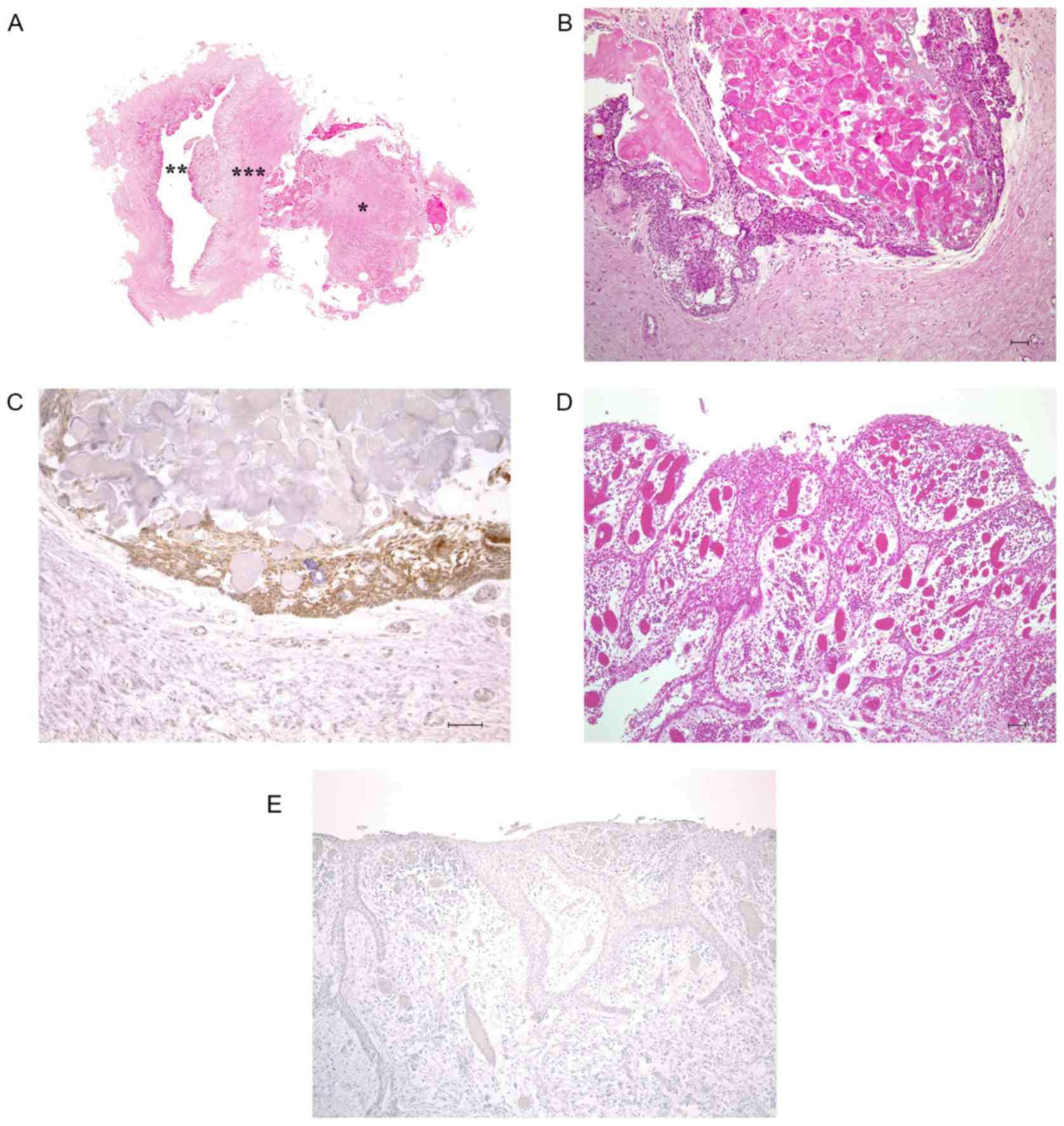 | Figure 5.Histopathological data. (A) Image
demonstrating the synchronism of the two aspects of the lesion.
Hematoxylin and eosin staining; *, the mesial portion indicating
calcifying cystic odontogenic tumor; **, the distal portion
indicating a dentigerous cyst; ***, a thick layer of collagen
fibers. Granulation tissue accompanied by cholesterol gap occupies
the ex-cystic space due to inflammation potentially caused by
fenestration. However, a remaining cyst cavity may be observed near
to the cyst wall surrounding the granulation tissue. (B) Image
obtained from the mesial portion of the specimen. The cystic wall
was lined by an ameloblastomatous epithelium with ‘ghost cells’ and
numerous calcified particles. The dentin-like hard tissue was
visible (scale bar, 50 µm; original magnification, ×100). (C) The
same tissue portion as (B) was stained by an antibody against Bcl-2
protein, which confirmed that this portion consisted of tumor cells
(scale bar, 50 µm; original magnification, ×100). (D) Image
obtained from the distal portion of the specimen. The cystic lesion
was lined by unkeratinized stratified squamous epithelia (scale
bar, 50 µm; original magnification, ×100). (E) The same portion as
(D) was stained by an antibody against Bcl-2 protein (original
magnification, ×100). Bcl-2, B-cell lymphoma-2. |
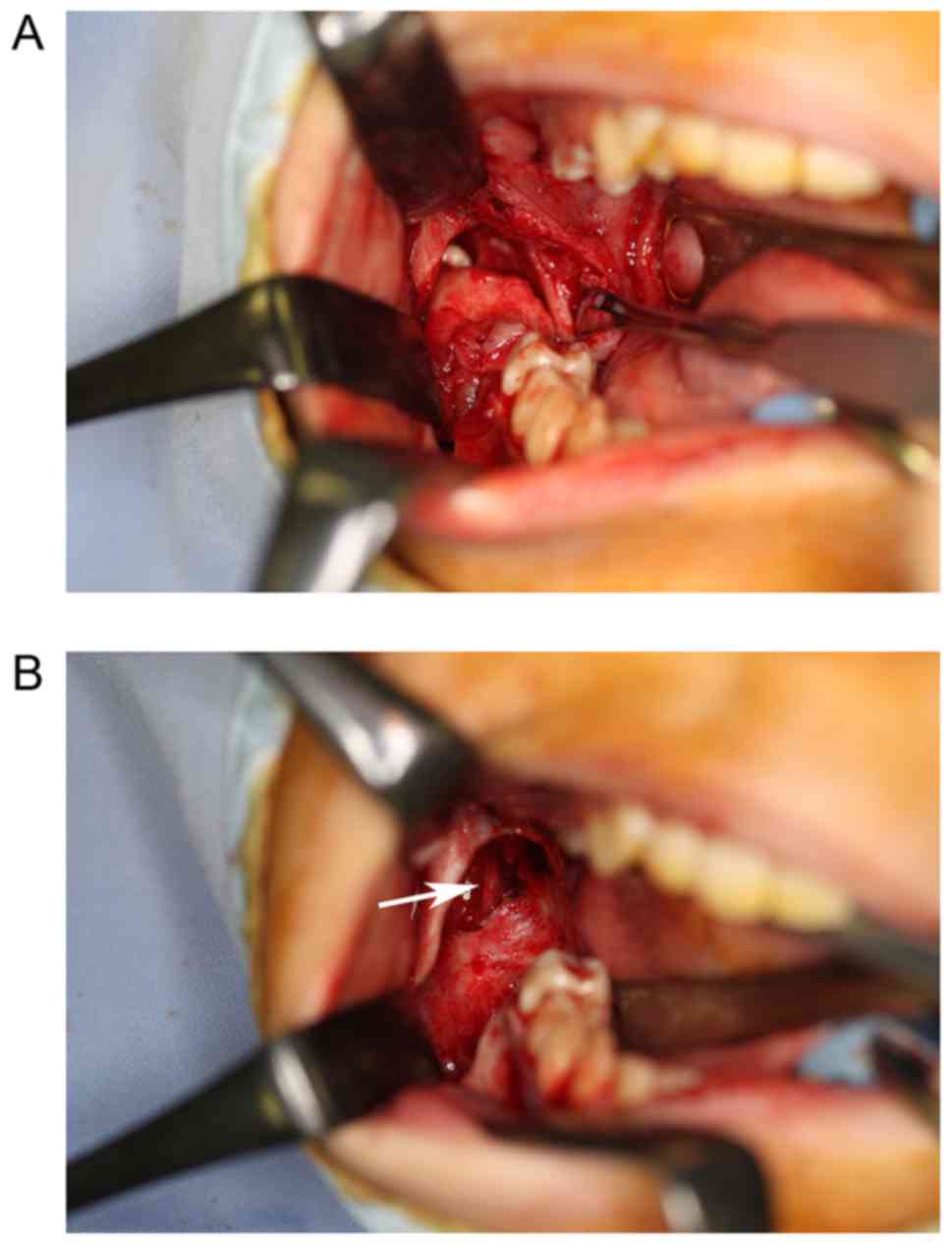
The results of the surgery were consistent with the
radiological data (Fig. 6A) and the
mandibular canal existed just underneath the impacted teeth
(Fig. 6B). The enucleated material
exhibited a solid structure with calcification in the thick wall.
No recurrence or postoperative complications were observed during a
2-year follow-up period. Written informed patient consent was
obtained for the publication of this study.
Discussion
The current case presents two important clinical
points, namely that CCOT and DC may occur simultaneously and
adjacently in a single cavity of the same jaw, and that CT is
useful in evaluating the result of the fenestration by visualizing
the change in the total size of the tumor.
The present study reports a case of the simultaneous
occurrence of CCOT and DC in the mandible of a patient. To the best
of our knowledge, the synchronous occurrence of CCOT and DC as
distinct lesions has not been previously identified. In the present
case, the diagnoses reached from the imaging and histopathological
studies were inconsistent. The presence of a single mandibular
radiolucent lesion led to the suspected diagnosis of a CCOT.
However, the definitive diagnosis of the two pathologically
distinct entities of CCOT and DC was made by pathologists based on
the excisional biopsies. CCOT may occasionally be an aggressive and
recurrent tumor (1,13), therefore close post-surgical follow-up
is preferable.
In general, odontogenic lesions containing
calcifications are particularly difficult to diagnose based only on
histopathological data. X-rays are occasionally crucial to reach
the definite diagnosis. However, regarding the present case, it was
important to consider potential explanations for the difficulty in
achieving the diagnosis based on X-ray images alone, which were not
able to detect the existence of DC. Considering the X-ray and
histopathological data, two different types of soft tissues were
estimated to be adjacent to each other in a single hard-tissue
cavity. Previous literature has described the simultaneous
occurrence of odontogenic lesions as hybrid or distinct lesions
(3,14–18). Among
these studies, Chindasombatjaroen et al (17) described the case of a patient with
CCOT associated with an odontoma, a supernumerary tooth, and DC
that simultaneously occurred at varying maxillary locations. By
contrast, the present study described the occurrence of two
independent lesions that existed concomitantly in a single cavity.
The characteristic feature of the case in the present study was
that the CT images did not demonstrate any indication of the
existence of a septum; only a bundle of collagen fibers separated
the two lesions.
It was also found that CT is useful not only for
diagnosing the disease, but for evaluating the issue of
fenestration. From a radiological viewpoint, the focus was directed
towards the internal structure of the lesion. The CT images
demonstrated that the calcification inside the lesion had increased
in the interval between fenestration and enucleation. The following
two assumptions about this observation could be made: The
development of the CCOT was accelerated by stimulation caused by
the fenestration, and the ossification as part of the healing
process occurred inside the lesion. Neither assumption was correct
in the present case. It was important to focus on the fact that the
whole lesion had decreased in size following the fenestration,
which indicated that sound healing was obtained subsequent to
surgical intervention. According to the surgeon, additional
development or ossification inside the CCOT may occur over the
years following initial downsizing, due to surgical decompression
or fenestration. This issue highlighted the unforeseen difference
of viewpoints between radiologists and surgeons.
CCOT generally appears as a unilocular lesion with a
well-defined margin (5,19). The tumor may resemble a calcifying
epithelial odontogenic tumor, odontoma, adenomatoid odontogenic
tumor, ossifying fibroma or fibrous dysplasia. The lining of COC
consists of ameloblastic epithelium and ‘ghost cells’, which
undergo dystrophic calcification (20). In the early developmental stages, COCs
will appear completely radiolucent. During maturation,
calcifications develop that produce a well-circumscribed, mixed
radiolucent-radiopaque appearance (4). In the case of the present study,
well-defined unilocular forms and regular margins were observed on
conventional radiographs and CT images. Unexpectedly, the CT images
did not demonstrate any indications of the slightly scalloped
outline and septum-like structure that was observed on the
panoramic radiograph. The reason for this may be associated with
the projection geometry peculiar to conventional radiographs,
termed the ‘eggshell effect’. Conventional radiographs that project
a three-dimensional volume onto a two-dimensional receptor may
produce an eggshell effect of corticated structures. The
septum-like structure that was present only on the panoramic
radiograph was a key result in the interpretation of the case, as
it was present in a single lesion. It suggested that there was a
difference in the potential doubling time between the two lesions.
Considering the nature of tumors and cysts, the growth of the CCOT
was potentially quicker compared with that of the DC, which could
result in pressure from the CCOT on the side of the DC. Fig. 7 demonstrates the schematic view of the
two lesions being exposed to an X-ray beam.
CCOT rarely presents in association with other
odontogenic tumors, including ameloblastic fibro-odontoma,
ameloblastic fibroma, odontoameloblastoma and odontogenic
myxofibroma (16,21,22). DC,
ameloblastic fibro-odontoma, adenomatoid odontogenic tumors and
calcifying epithelial odontogenic tumors are all included in the
differential diagnosis of a CCOT. A definitive diagnosis may be
reached histologically (16,23). In the X-ray investigation of the
present case, ameloblastic fibro-odontoma was ruled out, as
radiopacity was not observed in the central region of the tumor,
the density of which resembled that of dental hard tissue, as
observed in odontomas (24). A
calcifying epithelial odontogenic tumor was also ruled out, as the
radiolucent margin was clearly demarcated from the normal bone at
the periphery.
By definition, a DC encloses the crown of an
unerupted tooth as a result follicular expansion, and it is
attached to the cement-enamel tooth junction. The peak incidence
for DCs is within the second and third decades of life, with the
mandibular third molars being the most frequently involved teeth
(24). The histological appearance of
the lesion is of a thin myxoid-appearing fibrous tissue wall, lined
by non-keratinizing stratified squamous epithelium, which is
actually a derivative of reduced enamel epithelium (25). Radiologically, a well-circumscribed
cyst that contains the crown of the tooth is observed. As the cyst
grows, it pulls the unerupted tooth with it. A small DC is
unilocular. Large cysts may be multilocular, and the confined tooth
may be displaced from its normal location (20,26).
In the present case, achieving a diagnosis based on
radiology was challenging for the following reasons: The suspected
entities of CCOT and DC are occasionally associated with impacted
or unerupted teeth (20) and no
septum-like structure was observed on the CT images. In this
regard, it is possible that resorption of the septum occurred due
to the skeletal growth of the patient. However, the amount of
calcification was markedly different between the portions around
the second and third molars. The existence of considerable
differences between the two portions was confirmed by CT.
In conclusion, the present case demonstrated that
CCOT and DC may be present simultaneously in a single cavity.
Additionally, CT was important in evaluating the healing process in
detail. The present case may serve as a valuable warning that CCOT,
which may recur and transform into malignancy if improperly
treated, may be present in such lesions.
Acknowledgements
The authors would like to thank Dr Kaname Tsuji
(First Department of Oral and Maxillofacial Surgery, Osaka Dental
University, Osaka, Japan) for providing support to the study, and
ThinkSCIENCE Inc. (Tokyo, Japan) for providing language editing
services.
References
|
1
|
Utumi ER, Pedron IG, da Silva LP, Machado
GG and Rocha AC: Different manifestations of calcifying cystic
odontogenic tumor. Einstein (Sao Paulo). 10:366–370. 2012.(In
English, Portuguese). View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gorlin RJ, Pindborg JJ, Odont, Clausen FP
and Vickers RA: The calcifying odontogenic cyst-a possible analogue
of the cutaneous calcifying epithelioma of Malherbe. An analysis of
fifteen cases. Oral Surg Oral Med Oral Pathol. 15:1235–1243. 1962.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Basile JR, Klene C and Lin YL: Calcifying
odontogenic cyst with odontogenic keratocyst: A case report and
review of the literature. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 109:e40–e45. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Menat S, Md S, Attur K and Goyal K:
Ameloblastomatous CCOT: A case report of a rare variant of CCOT
with a review of the literature on its diverse histopathologic
presentation. Case Rep Dent. 2013:4076562013.PubMed/NCBI
|
|
5
|
Iida S, Fukuda Y, Ueda T, Aikawa T, Arizpe
JE and Okura M: Calcifying odontogenic cyst: Radiologic findings in
11 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
101:356–362. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Son HJ, Jeong YJ, Jeong JS and Kang DY: An
inflammatory dentigerous cyst shows rim uptake on bone scan: A case
report. Nucl Med Mol Imaging. 48:79–81. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Narang RS, Manchanda AS, Arora P and
Randhawa K: Dentigerous cyst of inflammatory origin-a diagnostic
dilemma. Ann Diagn Pathol. 16:119–123. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sumbh B, Sumbh SG, Jain P and Pagare J:
Classification of odontogenic cysts: A review. IOSR J Dental Med
Sci. 16:79–82. 2017. View Article : Google Scholar
|
|
9
|
Mokhtari S, Mohsenifar Z and Ghorbanpour
M: Predictive factors of potential malignant transformation in
recurrent calcifying cystic odontogenic tumor: Review of the
literature. Case Rep Pathol. 2013:8530952013.PubMed/NCBI
|
|
10
|
Zapała-Pośpiech A, Wyszyńska-Pawelec G,
Adamek D, Tomaszewska R, Zaleska M and Zapała J: Malignant
transformation in the course of a dentigerous cyst: A problem for a
clinician and a pathologist. Considerations based on a case report.
Pol J Pathol. 64:64–68. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cheung TH, Chung TK, Lo KW, Yu MY,
Krajewski S, Reed JC and Wong YF: Apotosis-related proteins in
cervical intraepithelial neoplasia and squamous cell carcinoma of
the cervix. Gynecol Oncol. 86:14–18. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Murakami M, Sakai H, Kodama A, Mori T,
Maruo K, Yanai T and Masegi T: Expression of the anti-apoptotic
factors Bcl-2 and survivin in canine vascular tumours. J Comp
Pathol. 139:1–7. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Daniels JS: Recurrent calcifying
odontogenic cyst involving the maxillary sinus. Oral Surg Oral Med
Oral Pathol Oral Radiol Endod. 98:660–664. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hisatomi M, Asaumi J, Konouchi H, Yanagi Y
and Kishi K: A case of glandular odontogenic cyst associated with
ameloblastoma: Correlation of diagnostic imaging with
histopathological features. Dentomaxillofac Radiol. 29:249–253.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shimamoto H, Kishino M, Okura M,
Chindasombatjaroen J, Kakimoto N, Murakami S and Furukawa S:
Radiographic features of a patient with both cemento-ossifying
fibroma and keratocystic odontogenic tumor in the mandible: A case
report and review of literature. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 112:798–802. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chindasombatjaroen J, Kakimoto N, Akiyama
H, Kubo K, Murakami S, Furukawa S and Kishino M: Computerized
tomography observation of a calcifying cystic odontogenic tumor
with an odontoma: Case report. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 104:e52–e57. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chindasombatjaroen J, Poomsawat S and
Klongnoi B: Calcifying cystic odontogenic tumor associated with
other lesions: Case report with cone-beam computed tomography
findings. Oral Surg Oral Med Oral Pathol Oral Radiol. 113:414–420.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Fregnani ER, da Cruz Perez DE, Soares FA
and Alves FA: Synchronous ameloblastoma and orthokeratinized
odontogenic cyst of the mandible. J Oral Pathol Med. 35:573–575.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Uchiyama Y, Akiyama H, Murakami S, Koseki
T, Kishino M, Fukuda Y, Shimizutani K and Furukawa S: Calcifying
cystic odontogenic tumour: CT imaging. Br J Radiol. 85:548–554.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Som PM and Brandwein MS: Tumors and
tumor-like conditionsHead and Neck Imaging. Som PM and Curtin HD:
4th. Mosby, St. Louis: pp. 345–346, p352, p9385. 2003
|
|
21
|
Yoon JH, Kim HJ, Yook JI, Cha IH, Ellis GL
and Kim J: Hybrid odontogenic tumor of calcifying odontogenic cyst
and ameloblastic fibroma. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 98:80–84. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lin CC, Chen CH, Lin LM, Chen YK, Wright
JM, Kessler HP, Cheng YS and Ellis E III: Calcifying odontogenic
cyst with ameloblastic fibroma: Report of three cases. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod. 98:451–460. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
McGowan RH and Browne RM: The calcifying
odontogenic cyst: A problem of preoperative diagnosis. Br J Oral
Surg. 20:203–212. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Koenig LJ: Mandible and maxillaDiagnostic
Imaging Oral and Maxillofacial. Koenig LJ, Tamimi D, Petrikowski
CG, Harnsberger HR, Ruprecht A, Benson BW, Van Dis ML, Hatcher D
and Perschbacher SE: Amirsys, Milwaukee, WI: pp. 50–53, pp100-1032.
2012
|
|
25
|
Shephard M and Coleman H: Simultaneous
adenomatoid odontogenic and keratocystic odontogenic tumours in a
patient with Gorlin-Goltz syndrome. Aust Dent J. 59:121–124. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Verbin RS and Barnes L: Cysts and cystlike
lesions of the oral cavity, jaws and neckSurgical Pathology of the
Head and Neck. 1st. Barns L: Marcel Dekker, Inc.; New York, NY: pp.
1233–1307. 1985
|