Introduction
With changes in people's dietary habits and living
environment, the incidence of malignant tumors has been on the
increase. Surgery, chemoradiotherapy and other therapies are
currently used to treat malignant tumors, but through these
treatments, patient quality of life decreases, and prognosis
remains poor (1,2). Since the pathological features of early
stage digestive tract malignant tumors are not obvious, diagnosis
can be challenging, and frequently a diagnosis is only made once
the tumor has reached middle or late stage, and after the
opportunity for curative surgery is no longer available, resulting
in poor 5-year survival rates (3). A
precancerous lesion is an intermediate link between normal tissue
and canceration and, although it is not a malignant tumor, it may
have the potential to progress to malignancy (4). Colitis and colon polyps are common
precancerous lesions associated with colon adenocarcinoma. Early
identification and diagnosis of precancerous lesions is presently a
research hotspot, and is likely to play a key role in the treatment
of digestive tract malignant tumors in the future.
Abnormal sugar-chain glycoprotein is also known as
tumor abnormal protein (TAP), and TAP expression can indirectly
reflect the extent and degree of cell canceration (5,6). There
have been data suggesting that a relatively high expression of TAP
exists in a variety of tumors, such as stomach, colorectal, thyroid
and bladder cancers (7–11). However, few reports are available
regarding the clinical significance of TAP in the screening of
colon pre-adenocarcinoma lesions. In the present study, TAP
expression was investigated in patients with colitis, colon polyps,
and colon adenocarcinoma to clarify the significance of TAP in
common digestive tract precancerous lesions.
Materials and methods
Study population
A total of 50 colitis patients admitted to the
Dezhou People's Hospital (Shandong, China) from March, 2012 to May,
2014 were selected as the colitis group, which comprised 27 males
and 23 females, aged 42–65 years (mean, 57.2 ± 2.6). The colon
polyp group included 50 patients with, of whom 26 were males and 24
females, aged 41–66 years (mean 57.6 ± 2.8). The colon
adenocarcinoma group comprised 50 patients, of whom 28 were males
and 22 females, aged 42–64 years (57.3 ± 2.1).
Inclusion criteria for the study were: i) Patients
who were definitely diagnosed by gastroscope, colonoscopy and
pathological examination, ii) patients who agreed to follow-up for
dynamic TAP monitoring for 2 years, and iii) who had signed
informed consent and agreed to participate in this study. Exclusion
criteria for the study were: i) Patients whose digestive tract
tumors had transferred and (or) invaded organs outside the
digestive tract when they were selected or before surgery, ii) who
had other concurrent tumors, iii) patients who had autoimmune
disease, iv) with tumors that approached or had reached late stage,
and v) with organ incompetence who could not tolerate endoscopy
examination. Study approval was obtained from the Medical Ethics
Committee of Dezhou People's Hospital.
TAP detection methods
Whole blood from the first and second drops of blood
from patient's fingertips was collected, prepared on glass slides,
and after being dried naturally, used for detection of TAP. TAP
detection reagent (Biosharp Biotech, Hefei, China) was added onto
the detection specimen and the condensation staining reaction was
performed, followed by microscopic examination to observe results
after the reaction was complete and the stain was dried.
Determination of TAP detection results: When TAP
exists in blood, it reacts with the reagent and produces a
crystal-like condensation product. For TAP-positive, the
condensation particle area was ≥225 µm2; for the TAP
weakly positive or critical type, the condensation product area was
between 121 and 225 µm2; and for TAP-negative, the
crystal-like condensation product was not observed.
H&E staining of pathological
specimens
Pathological tissue specimens of patients in the 3
groups were obtained from specimens of large volume excised by
surgery or diseased mucosal tissues obtained by gastrointestinal
endoscopy biopsy. Pathological sections were made and diagnosed
with the assistance of pathology doctors of high seniority.
After pathological sections were frozen and pasted
onto slides, the fixative of 95% 95 ml alcohol mixed with 5 ml
glacial acetic acid was used to fix them for 1 min, and then
hematoxylin was used for staining. To determine the results, the
cell nucleus was stained blue and cytoplasm was stained pink by
hematoxylin.
TAP follow-up monitoring
TAP expression levels were measured at
hospitalization and at 15 days after surgery; for patients who were
TAP-negative 1–2 years after treatment, detection was performed
once every 3 months; for TAP-negative 3–4 years after treatment,
detection was performed once or twice a year; for TAP-negative 5
years after treatment, detection was performed once a year; for
suspected cases of tumor recurrence and metastasis, or changes in
clinical treatment regimen, TAP detection was performed at that
time. This study presents data up to 2 years of follow-up.
Statistical analysis
Statistical software SPSS 20.0 (IBM, New York, NY,
USA) was used for analysis. Variance analysis was used for
comparisons between the 3 groups and a t-test was used for
comparison of pairs. Numerical data were presented as percentage
(%), and the Chi-square (χ2) test or exact probability
test was used for comparison in the 3 groups. A linear trend
χ2 test was used to reflect the specimen-positive
expression trend. P<0.05 was considered to indicate a
statistically significant diference.
Results
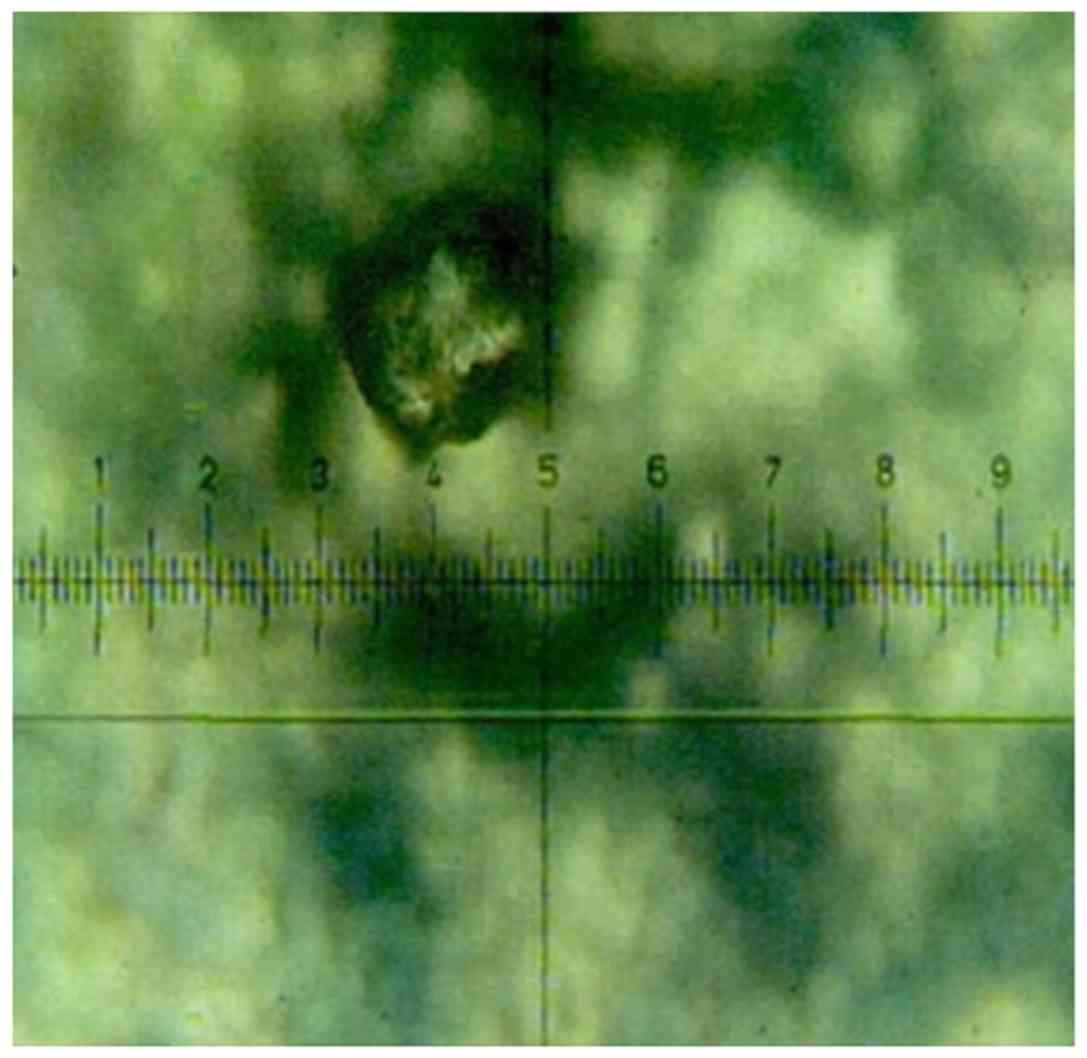
Contrast figures of colon polyp
endoscope, pathology and TAP-positive
Results of contrast figures of colon polyp
endoscope, pathology and TAP-positive are shown in Figs. 1–3.
TAP-positive expression in colitis,
colon polyp and colon adenocarcinoma patients before treatment
TAP-positive expression in colitis, colon polyp and
colon adenocarcinoma patients prior to treatment was 6,76 and 92%,
respectively, and the positive expression rate comparison between
the three groups was statistically significant (P<0.05)
(Table I).
 | Table I.TAP-positive expression in colitis,
colon polyp and colon adenocarcinoma patients before treatment. |
Table I.
TAP-positive expression in colitis,
colon polyp and colon adenocarcinoma patients before treatment.
|
|
| TAP expression |
|
|
|---|
|
|
|
|
|
|
|---|
| Groups | No. | Positive (%) | Negative (%) | χ2 | P-value |
|---|
| Colitis | 50 | 3 (6) | 47 (94) | 7.426 | <0.05 |
| Colon polyp | 50 | 38 (76) | 12 (24) |
|
|
| Colon
adenocarcinoma | 50 | 46 (92) | 4 (8) |
|
|
| Total | 150 | 87 | 63 |
|
|
TAP-positive expression in colitis, colon polyp and
colon adenocarcinoma patients before treatment showed an increasing
trend (Table II). This suggested
that TAP participated in the process from intestinal mucosal
inflammation to colon polyp formation to tissue canceration, and it
was correlated with them.
 | Table II.TAP expression trend in colitis, colon
polyp and colon adenocarcinoma patients before treatment. |
Table II.
TAP expression trend in colitis, colon
polyp and colon adenocarcinoma patients before treatment.
| Groups | No. | Positive cases | Positive (%) | Score | χ2 | P-value |
|---|
| Colitis | 50 | 3 | 6 | 1 | 6.335 | <0.05 |
| Colon polyp | 50 | 38 | 76 | 2 |
|
|
| Colon
adenocarcinoma | 50 | 46 | 92 | 3 |
|
|
| Total | 150 | 87 |
|
|
|
|
Relationship between TAP expression
and clinicopathological parameters of colitis, colon polyp and
colon adenocarcinoma
TAP-positive expression in all three groups had no
significant correlation with sex, age or ethnic group (P>0.05)
(Table III).
 | Table III.Relationship between TAP expression
and clinicopathological parameters of colitis, colon polyp and
colon adenocarcinoma. |
Table III.
Relationship between TAP expression
and clinicopathological parameters of colitis, colon polyp and
colon adenocarcinoma.
|
|
| Colitis group |
|
| Colon polyp
group |
|
| Colon adeno-carcinoma
group |
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|---|
| Clinicopa-thological
parameters | No. | Positive | Negative | χ2 | P-value | Positive | Negative | χ2 | P-value | Positive | Negative | χ2 | P-value |
|---|
| Sex |
|
|
|
|
|
|
|
|
|
|
|
|
|
| Male | 81 | 2 | 25 |
|
| 20 | 6 |
|
| 25 | 3 |
|
|
|
Female | 69 | 1 | 22 | 0.663 | >0.05 | 18 | 6 | 0.402 | >0.05 | 21 | 1 | 0.518 | >0.05 |
| Age (years) |
|
|
|
|
|
|
|
|
|
|
|
|
|
| ≤50 | 65 | 1 | 23 |
|
| 19 | 7 |
|
| 23 | 2 |
|
|
|
>50 | 85 | 2 | 24 | 0.007 | >0.05 | 18 | 6 | 0.072 | >0.05 | 23 | 2 | 0.114 | >0.05 |
| Ethnic group |
|
|
|
|
|
|
|
|
|
|
|
|
|
| Ethnic
Han | 102 | 2 | 34 |
|
| 28 | 8 |
|
| 33 | 3 |
|
|
| Other
ethnic groups | 48 | 1 | 13 | 0.116 | >0.05 | 10 | 4 | 0.105 | >0.05 | 13 | 1 | 0.158 | >0.05 |
TAP follow-up monitoring
TAP follow-up monitoring indicated that, the three
TAP-positive patients screened out from the colitis group were
examined by gastroscope or colonoscopy, CT, and B ultrasound before
treatment, and tumors were not detected. After 2 years of
follow-up, one case of colon adenocarcinoma was found. No cases of
colon adenocarcinoma were detected in the 47 TAP-negative patients
in this group.
The 38 TAP-positive patients screened out from the
colon polyp group were examined by gastroscope or colonoscopy, CT,
and B ultrasound before treatment, and no tumors were detected.
After the 2-year follow-up, 15 cases of colon adenocarcinoma were
identified. Only one case of colon adenocarcinoma was detected
among the 12 TAP-negative patients in this group. Therefore, the
tumor incidence rate in TAP-positive patients was significantly
higher than in TAP-negative patients (P<0.05) (Table IV).
 | Table IV.Comparison of tumor incidence or
recurrence between TAP-positive and TAP-negative patients n
(%). |
Table IV.
Comparison of tumor incidence or
recurrence between TAP-positive and TAP-negative patients n
(%).
|
|
| TAP-positive | TAP-negative |
|
|
|---|
|
|
|
|
|
|
|
|---|
| Groups | No. | Case | Tumor incidence or
recurrence | Case | Tumor incidence or
recurrence | χ2 | P-value |
|---|
| Colitis | 50 | 3 | 1
(33.3)a | 47 | 0 (0) | 9.832 | <0.05 |
| Colon polyp | 50 | 38 | 14
(36.8)a | 12 | 1 (8.3) | 10.561 | <0.05 |
| Colon
adenocarcinoma | 50 | 20 | 9 (45)a | 30 | 3 (10) | 11.085 | <0.05 |
TAP expression was measured in patients in the colon
adenocarcinoma group after surgery, of which there were 20
TAP-positive cases, and after 2 years, there were 9 cases of tumor
recurrence and metastasis. However, after 2 years, there were only
3 cases of tumor recurrence and metastasis among the 30
TAP-negative patients after surgery. Therefore, the tumor
recurrence rate after surgery was significantly higher in TAP
positive patients in the colon adenocarcinoma than in TAP negative
(P<0.05) (Table IV).
Discussion
As common digestive tract cancers are difficult to
detect in the early stages, they cause great harm to health. Since
the number of cancer cells is relatively small in malignant
digestive tract tumors of subclinical stage and nutrient vessels
are not yet present, early intervention at this stage can reverse
the condition, and 5-year survival rate can surpass 80% (12,13). Once
malignant digestive tract tumors reach middle and late stages,
there are no effective treatments, and 5-year survival rate is less
than 20% (14,15). Effective early diagnosis and treatment
for malignant digestive tract tumors is currently a major
challenge. Research has shown that serum tumor markers, such as
CEA, CA19-9 and CA125, are closely associated with tumor occurrence
and development. However, the detection of a single tumor marker,
such as CEA, CA19-9 or CA125 or traditional tumor marker detection
for early diagnosis has poor sensitivity and specificity. For this
reason, the above mentioned tumor markers have limited clinical
application for malignant tumor screening. The fundamental method
to prevent malignant tumors depends on early detection and
diagnosis. In previous years, a breakthrough in early diagnosis for
malignant digestive tract tumors has been elusive (16,17).
TAP is a type of tumor marker featuring an abnormal
sugar-chain (18). When the TAP
quantity released by malignant cells reaches a certain level, TAP
can be detected in peripheral blood. When TAP shows a positive
expression, specific condensation products in peripheral blood can
be found, which are different from sundries generated by normal
blood (19,20). Thus, we can conveniently determine
whether TAP exists in a subject's blood or not and can also
evaluate the TAP expression level. As a marker for malignant
digestive tract tumors, TAP has the following advantages (21–23): i) As
most glycoprotein is distributed on the cell surface and
extracellular matrix, when cells become cancerous, the change of
sugar chain is detectable; ii) because the O- and N-sugar chain can
be specifically recognized by agglutinin, condensation and sediment
phenomena can occur, and the specific shape of condensation
products can be observed though a microscope; iii) TAP detection
can sensitively identify abnormal sugar chains associated with
malignant digestive tract tumors, thus many tumor-related signals
can be gathered; and iv) TAP can be detected in malignant tumors of
subclinical stage. Previous studies have demonstrated that, TAP
expression can be detected up to 2 years earlier than clinical
signs, symptoms and malignant lumps (24).
Our investigations have shown that TAP-positive
expression rates in patients with colitis, colon polyps and colon
adenocarcinoma were 6,76 and 92%, respectively, and that a
comparison of the positive expression rate between groups was
statistically significant, with TAP-positive expression showing an
increasing trend. The TAP-positive expression was not significantly
correlated with sex, age or ethnicity in any of the three groups.
This result suggests that TAP can effectively distinguish colon
adenocarcinoma patients from the large number of patients with
colitis and colon polyps. TAP seems to have good specificity for
malignant digestive tract tumors, and it may be useful for the
early or supplementary diagnosis of this type of malignant
tumor.
TAP-negative expression indicates malignant tumors
may have been eliminated completely. However, after TAP-negative
expression, if TAP weak-positive expression occurs, followed by
TAP-positive expression in a short period of time, for example,
approximately 1 month, this indicates malignant tumors remain in
the body or have started being transferred. If TAP-negative
expression occurs, later followed by TAP-positive expression after
approximately 1 year, recurrence or metastasis of malignant tumors
can be determined (25,26). TAP follow-up monitoring showed that
the tumor incidence rates in TAP-positive patients in the colitis
colon polyp groups were significantly higher than those in the
TAP-negative patients. After surgery, the tumor recurrence rate in
TAP-positive patients in colon adenocarcinoma was significantly
higher than that in TAP-negative patients. This shows that TAP
expression is an important index with a high sensitivity to
evaluate postoperative recurrence and metastasis of digestive tract
tumors belonging to the colon adenocarcinoma type, and through TAP
detection, prognosis can be evaluated.
In conclusion, TAP expression is relatively high in
colon pre-adenocarcinoma lesions, and TAP actively participates in
the process from intestinal mucosal inflammation to colon polyp
development to tissue canceration, and is correlated with them. TAP
expression can be used for screening of this type of digestive
tract precancerous lesion, and has important clinical
significance.
References
|
1
|
Zhang H, Hou Y, Xu L, Zeng Z, Wen S, Du
YE, Sun K, Yin J, Lang L, Tang X and Liu M: Cytoplasmic drosha is
aberrant in precancerous lesions of gastric carcinoma and its loss
predicts worse outcome for gastric cancer patients. Dig Dis Sci.
61:1080–1090. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Abangah G, Rahmani A, Hafezi-Ahmadi MR,
Emami T, Asadollahi K, Jaafari-Haidarlo A and Moradkhani A:
Precancerous histopathologic lesions of upper gastrointestinal
tract among dyspeptic patients upon endoscopic evaluations. J
Gastrointest Cancer. 47:1–7. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Harmsen S, Meijerman I, Febus CL,
Maas-Bakker RF, Beijnen JH and Schellens JHM: PXR-mediated
induction of P-glycoprotein by anticancer drugs in a human colon
adenocarcinoma-derived cell line. Cancer Chemother Pharmacol.
66:765–771. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bukowska D: Expression and distribution of
zona pellucida proteins 3 and 4 in morphologically abnormal canine
oocytes: A confocal microscopic observation-based study. Med Weter.
72:68–74. 2016.
|
|
5
|
Albino-Sanchez ME, Vazquez-Hernandez J,
Ocadiz-Delgado R, Serafin-Higuera N, León-Galicia I, Garcia-Villa
E, Hernandez-Pando R and Gariglio P: Decreased RARβ expression
induces abundant inflammation and cervical precancerous lesions.
Exp Cell Res. 346:40–52. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Go H, Hwang HJ and Nam TJ: A glycoprotein
from Laminaria japonica induces apoptosis in HT-29 colon cancer
cells. Toxicol In Vitro. 24:1546–1553. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Carta F, Sionis S, Cocco D, Gerosa C,
Ferreli C and Puxeddu R: Enhanced contact endoscopy for the
assessment of the neoangiogenetic changes in precancerous and
cancerous lesions of the oral cavity and oropharynx. Eur Arch
Otorhinolaryngol. 273:1895–1903. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu Z, Cai J, Yu Y, Fang H, Si Y, Jankee
JJ and Shen M: Tumor abnormal protein as a novel biomarker in
papillary thyroid carcinoma. Clin Lab. 63:479–485. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lan F, Zhu M, Qi Q, Zhang Y and Liu Y:
Prognostic value of serum tumor abnormal protein in gastric cancer
patients. Mol Clin Oncol. 5:216–220. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zhang L, Guo X, Min Y and Xu J: Tumor
abnormal protein (TAP) examination contributes to primary diagnosis
of bladder cancer. Int J Clin Exp Med. 8:18528–18532.
2015.PubMed/NCBI
|
|
11
|
Wu XY and Huang XE: Clinical application
of serum tumor abnormal protein (TAP) in colorectal cancer
patients. Asian Pac J Cancer Prev. 16:3425–3428. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jin M, Roth R, Rock JB, Washington MK,
Lehman A and Frankel WL: The impact of tumor deposits on colonic
adenocarcinoma AJCC TNM staging and outcome. Am J Surg Pathol.
39:109–115. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mroz A and Kiedrowski M: An unusual case
of colonic adenocarcinoma development in the region of
disseminating lobular breast carcinoma infiltration: Diagnostic
approach and review of the literature. Int J Clin Exp Pathol.
8:7470–7474. 2015.PubMed/NCBI
|
|
14
|
Jafferbhoy S, Paterson H and Fineron P:
Synchronous gist, colon and breast adenocarcinoma with double
colonic polyp metastases. Int J Surg Case Rep. 5:523–526. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Grozdanov P, Hadjidekova S, Dimova I,
Nikolova I, Toncheva D, Ganchev G, Zlatkov V and Galabov AS:
Characterization of genomic changes in the cervical pre-cancerous
lesions and tumors induced by different types of human
papillomaviruses. Virusdisease. 27:271–276. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Musiienko AM, Alzahrani S, Simpson JA,
Heriot A and Warrier S: Colonic adenocarcinoma encasing the femoral
nerve: Complete surgical excision with preservation of function.
ANZ J Surg. 60:539–543. 2016.
|
|
17
|
Tatarian T, Arkonac D, Phillips B,
Isenberg GA and Goldstein SD: Colonic adenocarcinoma presenting as
sigmoidorectal intussusception: A consideration for intussusception
reduction. Am Surg. 82:181–182. 2016.PubMed/NCBI
|
|
18
|
Chen J, Ding Z, Peng Y, Pan F, Li J, Zou
L, Zhang Y and Liang H: HIF-1α inhibition reverses multidrug
resistance in colon cancer cells via downregulation of
MDR1/P-glycoprotein. PLoS One. 9:e988822014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jass JR: Colorectal cancer: A multipathway
disease. Crit Rev Oncog. 12:273–287. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Herrera-Covarrubias D,
Tecamachaltzi-Silvaran MB, Barradas-Moctezuma M, Rosales-Raya JB,
Manzo J, García LI, Aranda-Abreu GE, Ismail N, Coria-Avila GA and
Hernández ME: Effect of copulation on potentially precancerous
prostate lesions, serum testosterone and prolactin levels in rats.
Exp Oncol. 38:73–79. 2016.PubMed/NCBI
|
|
21
|
Kamalapuram SK, Kanwar RK and Kanwar JR:
Nanotheranostic based iron oxide (Fe3O4) saturated lactoferrin
nanocapsules for colonic adenocarcinoma. J Biomed Nanotechnol.
12:1758–1773. 2016. View Article : Google Scholar
|
|
22
|
Sun L, Xu S, Liang L, Zhao L and Zhang L:
Analysis of ROC: The value of HPV16 E6 protein in the diagnosis of
early stage cervical carcinoma and precancerous lesions. Oncol
Lett. 12:1769–1772. 2016.PubMed/NCBI
|
|
23
|
Halkias C, Sloane J, Ben-Gashir M and
Bashir G: Synchronous metastatic omental melanoma and colonic
adenocarcinoma: A case report. BMC Res Notes. 8:1252015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Jia AI, Lv Y, Guo X, Ren LI and Qin J:
Ectopic expression of p33(ING1b) suppresses proliferation and
induces apoptosis in colonic adenocarcinoma cells. Oncol Lett.
10:1517–1522. 2015.PubMed/NCBI
|
|
25
|
Almadi MA, Alharbi O, Azzam N, Wadera J,
Sadaf N and Aljebreen AM: Prevalence and characteristics of colonic
polyps and adenomas in 2654 colonoscopies in Saudi Arabia. Saudi J
Gastroenterol. 20:154–161. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Mersakova S, Nachajova M, Szepe P,
Kasajova PS and Halasova E: DNA methylation and detection of
cervical cancer and precancerous lesions using molecular methods.
Tumour Biol. 37:23–27. 2016. View Article : Google Scholar : PubMed/NCBI
|