Introduction
Bladder cancer is the most common malignancy of the
urinary tract and the 14th leading cause of cancer-associated
mortality worldwide (1,2). In Western countries, bladder cancer
ranks the 4th most frequently diagnosed cancer (3). Multidisciplinary treatment approaches,
including surgery, chemotherapy and radiation are available for
bladder cancer. Despite advances in diagnosis and treatment, the
prognosis, particularly for muscle-invasive disease, remains poor,
with a 5-year overall survival of 30–50% (4,5).
Therefore, the development of novel effective therapeutic methods
for bladder cancer is of clinical significance.
The phosphoinositide-3 kinase/protein kinase B
(PI3K/Akt) pathway has a pivotal role in tumor growth and
development (6). Depletion of
ubiquitin-conjugating enzyme E2T was found to inhibit the
proliferation and invasion of osteosarcoma cells (7). It has been reported that activation of
PI3K/Akt signaling contributes to Derlin-1-mediated malignant
phenotype in muscle invasive bladder cancer cells (8). Inhibition of PI3K/Akt signaling accounts
for the induction of death in bladder cancer cells by combination
treatment with rapamycin and resveratrol (9). These studies suggest that the PI3K/Akt
pathway is an important target for anticancer treatment.
Genipin, a natural compound derived from the fruit
of Gardenia jasminoides, has demonstrated various biological
properties including anti-inflammatory (10), anti-oxidative (11), anti-diabetic (12), anti-thrombotic (13), and neuroprotective (14) activities. Previous studies indicate
that genipin also exhibits a broad range of anticancer activities
in different types of human cancer cells (15,16). For
instance, genipin has been suggested to suppress hepatocellular
carcinoma metastasis through the inhibition of matrix
metalloproteinase-2 activity (15).
However, few studies have explored the biological activity of
genipin in bladder cancer.
The present study aimed to investigate the effects
of genipin on cell growth, cell cycle progression and apoptosis in
human bladder cancer. Considering the importance of the PI3K/Akt
pathway in tumor progression (6,7), it was
also investigated whether this signaling pathway is involved in the
action of genipin.
Materials and methods
Antibodies
The primary antibodies used in western blot analysis
were as follows: Rabbit anti-cyclin D1 (catalog no. 2922), rabbit
anti-cyclin-dependent kinase (CDK)2 (catalog no. 2546), rabbit
anti-CDK4 (catalog no. 12790), mouse anti-cytochrome c
(catalog no. 12963), rabbit anti-phospho-PI3K (catalog no. 4228),
rabbit anti-PI3K (catalog no. 4257), mouse anti-phospho-Akt
(catalog no. 12694), and mouse anti-Akt (catalog no. 2920) (all
from Cell Signaling Technology, Inc., Danvers, MA, USA), mouse
anti-cyclin-dependent kinase inhibitor 1 (p21; catalog no.
sc-136020), rabbit anti-cyclin-dependent kinase inhibitor 1B (p27;
catalog no. sc-528), mouse anti-β-actin (catalog no. sc-81178),
mouse anti-B-cell lymphoma 2-like protein 4 (Bax; catalog no.
sc-20067) (all from Santa Cruz Biotechnology, Inc., Dallas, TX,
USA), and rabbit anti-Heat shock protein 60 (catalog no. ab46798;
Abcam, Cambridge, UK). Horseradish peroxidase (HRP)-conjugated
secondary antibodies were purchased from Santa Cruz Biotechnology,
Inc.
Cell culture and genipin
treatment
The human bladder cancer T24 and 5637 cell lines and
the immortalized normal human uroepithelial SV-HUC-1 cell line were
purchased from the Type Culture Collection of Chinese Academy of
Sciences (Shanghai, China). They were cultured in Dulbecco's
modified Eagle's medium (DMEM) supplemented with 10% fetal bovine
serum (FBS), penicillin (100 U/ml), and streptomycin (100 µg/ml)
(all from Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA,
USA) at 37°C in a humidified 5% CO2 atmosphere. Cells
were treated with genipin (Sigma-Aldrich; Merck KGaA, Darmstadt,
Germany), which was dissolved in 0.1% dimethyl sulfoxide (DMSO;
Sigma-Aldrich; Merck KGaA). DMSO-treated cells were used as a
vehicle control.
Cell transfection
A constitutively active Akt construct (Myr-Akt
plasmid) and empty vector were purchased from AddGene (Cambridge,
MA, USA). Cells were transfected with 0.3 µg Myr-Akt or vector
using Lipofectamine 2000® (Invitrogen; Thermo Fisher
Scientific, Inc.), according to the manufacturer's instructions. At
24 h post-transfection, cells were exposed to genipin for
additional 48 h prior to cell viability and apoptosis analysis. For
each condition, three replicates were performed.
Cell viability assay
Cells were plated in 96-well plates at a density of
2×104 cells/well and incubated with different
concentrations (10, 30, 60, 100, and 300 µM) of genipin for 48 h.
DMSO-treated cells were used as a control. Each assay was performed
in quadruplicate. Cell viability was measured using the MTT assay.
Briefly, cells were added with MTT (0.5 mg/ml; Sigma-Aldrich; Merck
KGaA) and allowed to incubate for 4 h at 37°C. Following removal of
MTT, the resulting formazan was dissolved in DMSO. Absorbance was
measured at 570 nm using a microplate reader (xMark; Bio-Rad
Laboratories, Inc., Hercules, CA, USA).
Clonogenic growth assay
T24 and 5637 cells (5×103 cells/well)
were seeded in triplicate onto 6-well plates and treated with 30 or
60 µM of genipin or DMSO (vehicle control) on the following day.
DMEM containing genipin was renewed every 3 days. Following 10 days
of culture, cells were stained with 0.5% crystal violet
(Sigma-Aldrich; Merck KGaA). Colonies (>50 cells) were counted
in 10 independent microscopic fields (magnification, ×40) using an
inverted microscope.
Animal experiments
A total of 12 athymic male BALB/c (nu/nu) mice, 4 to
6 weeks old and weighing 16–20 g, were obtained from the Animal
Center of the Chinese Academy of Medical Science (Beijing, China).
The mice were housed 4 per cage at 22°C and 80% humidity in a 12-h
light/dark cycle with access to food and water ad libitum.
Mice were injected subcutaneously in the left flank with
4×106 T24 cells. When xenograft tumors reached a
diameter of ~5 mm, the mice were divided into 3 groups (n=4 for
each group) and DMSO (vehicle control) or genipin (20 and 50 mg/kg)
was administered intraperitoneally three times/week for 4 weeks.
The tumors were measured every week with microcalipers. Tumor
volume was calculated using the following equation: Tumor volume
(mm3) = 1/2 × (tumor length) × (tumor
width)2. Mice were sacrificed 5 weeks after cell
injection and tumors were resected and weighted. Animal experiments
were approved by the Institutional Animal Care and Use Committee of
Chinese Academy of Medical Science. Animal care and treatment were
performed in accordance with the international guidelines for
laboratory animals use (https://www.apa.org/science/leadership/care/guidelines.aspx).
Cell cycle and apoptosis analysis
Cell cycle distribution was determined by flow
cytometry following staining with propidium iodide (PI). Briefly,
subsequent to 30 or 60 µg of genipin or DMSO (vehicle control) for
48 h at 37°C, T24 and 5637 cells were collected and fixed in 70%
ethanol overnight at 4°C. The cells were resuspended in staining
solution containing 0.05 mg/ml PI and 7 U/ml RNase A
(Sigma-Aldrich; Merck KGaA) for 30 min at 37°C. Stained cells were
analyzed by a flow cytometer (FACSCanto II; BD Biosciences, San
Jose, CA, USA) with FlowJo software version 7.6.1 (TreeStar, Inc.,
Ashland, OR, USA). Cell apoptosis was examined using the Annexin
V-fluorescein isothiocyanate (FITC) Apoptosis Detection kit
(Beyotime Institute of Biotechnology, Haimen, China), as per the
manufacturer's instructions. Following incubation with Annexin
V-FITC and PI, T24 and 5637 cells were analyzed by flow cytometry
using FlowJo software version 7.6.1. Each assay was performed in
triplicate.
Preparation of protein samples
For preparation of the whole cellular lysates, cells
were suspended in radioimmunoprecipitation assay buffer (Beyotime
Institute of Biotechnology, Inc.) containing protease inhibitors on
ice for 15 min. For extraction of mitochondrial and cytosolic
fractions, a commercial mitochondria/cytosol fractionation kit
(Beyotime Biotechnology, Inc.) was used. Briefly, cells were
suspended in ice-cold cytosolic separation buffer containing
protease inhibitors for 15 min and centrifuged at 800 × g for 5 min
at 4°C. The supernatant was centrifuged at 12,000 × g for 30 min at
4°C to obtain the cytosolic fraction. The pellet was resuspended in
mitochondrial separation buffer for 30 min and then centrifuged at
10,000 × g for 10 min at 4°C to obtain the mitochondrial fraction.
Total protein concentrations were determined using a Pierce
Bicinchoninic Acid Protein Assay kit (Thermo Fisher Scientific,
Inc.).
Western blot analysis
Whole and fractionated cell lysates (50 µg total
protein per lane) were mixed with loading buffer and subjected to
12% SDS-PAGE and transferred onto polyvinylidene fluoride
membranes. Membranes were blocked with 5% fat-free milk in TBS
containing 0.05% Tween-20 for 1 h at room temperature and incubated
with primary antibodies overnight at 4°C. All primary antibodies
were diluted to 1:500. Subsequent to washing three times (10 min
for each time), the membranes were incubated with HRP-conjugated
secondary antibodies (dilution at 1:3,000) for 1 h. Membranes were
developed with enhanced chemiluminescence reagents (Amersham
Biosciences; GE Healthcare, Chicago, IL, USA). Densitometric
analysis of protein signals was conducted with Quantity One
software version 4.6.2 (Bio-Rad Laboratories). Each assay was
performed in triplicate.
Assessment of mitochondrial membrane
potential (Δψm)
Measurement of Δψm was performed using the
fluorescent probe JC-1, as previously described (17). At low Δψm, JC-1 exists primarily in a
monomeric form and produces green fluorescence. At high Δψm, JC-1
aggregates in intact mitochondria and yields red fluorescence. In
brief, T24 and 5637 cells were incubated for 30 min at 37°C with 2
µM JC-1 (Molecular Probes, Inc.; Thermo Fisher Scientific, Inc.).
Cells were collected and analyzed by the FACSCanto II flow
cytometer using FlowJo software version 7.6.1. Results are
expressed as the red/green fluorescence intensity ratio; whose
reduction indicates loss of Δψm.
Statistical analysis
Data are presented as the mean ± standard deviation,
and were analyzed using one-way analysis of variance followed by
pair-wise comparisons with Tukey's post-hoc test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Genipin exerts growth suppressive
effects on bladder cancer cells
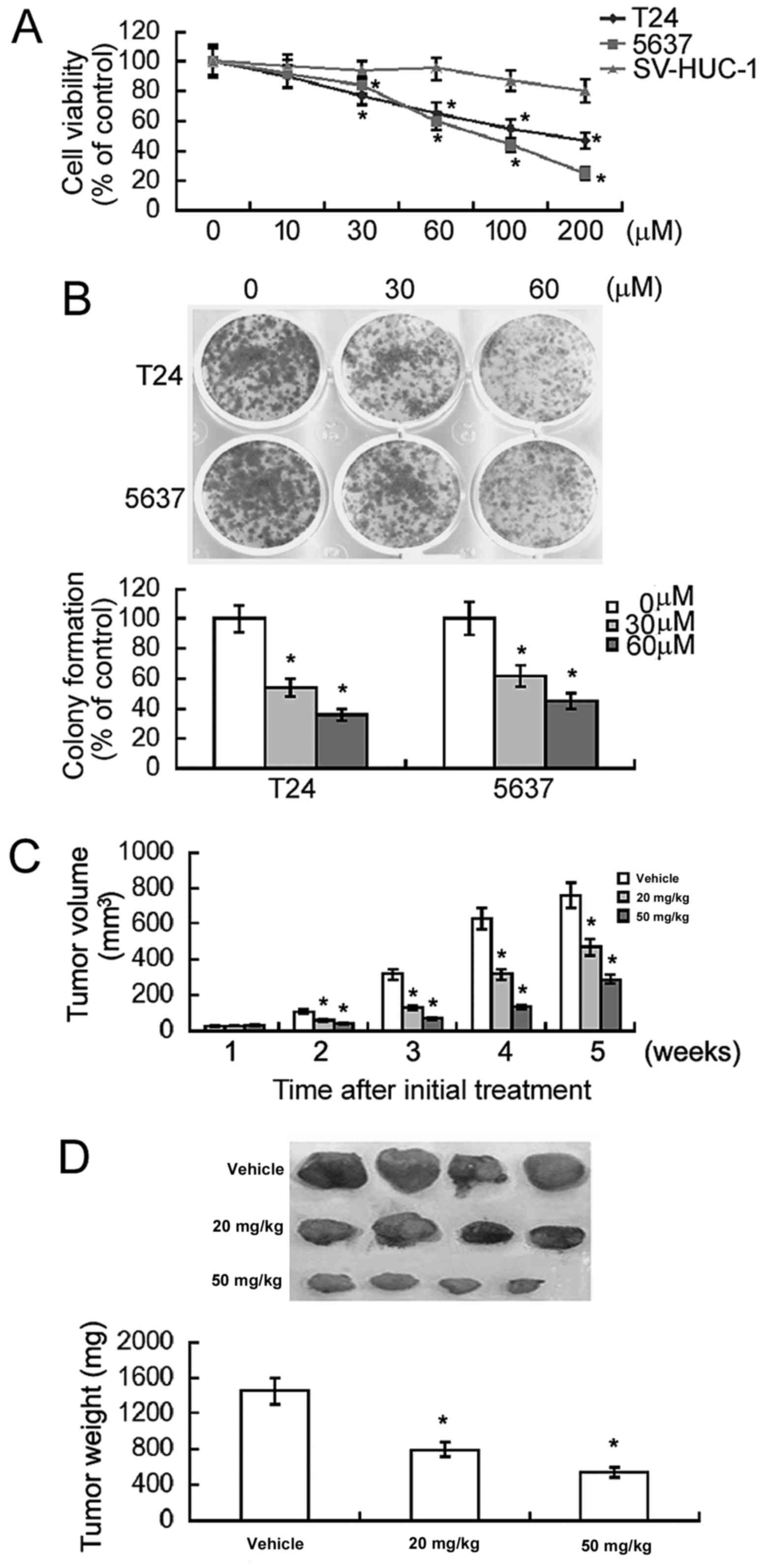
Genipin treatment for 48 h resulted in a
concentration-dependent inhibition of the viability of T24 and 5637
bladder cancer cells, compared with the vehicle control (Fig. 1A). In contrast, ≤60 µM genipin did not
exhibit a significant effect on the viability of non-malignant
uroepithelial SV-HUC-1 cells. These results suggested that a low
concentration of genipin was selectively cytotoxic to bladder
cancer cells. In the following experiments, genipin was used at a
final concentration of 30 or 60 µM unless indicated otherwise.
Next, the effect of genipin on clonogenic growth of
bladder cancer cells was determined. As demonstrated in Fig. 1B, exposure to genipin significantly
decreased the colony formation in T24 and 5637 cells by 2–3-fold.
The in vivo antitumor effect of genipin on the growth of T24
xenograft tumors was also examined in nude mice. Compared to the
DMSO-treated group, genipin treatment significantly inhibited the
growth of T24 xenograft tumors (P<0.05; Fig. 1C). Genipin at the dose of 50 mg/kg
caused significantly greater tumor suppression compared with 20
mg/kg genipin. At the end of the experiment, the tumor weight was
reduced by >60% in the genipin (50 mg/kg)-treated group
(Fig. 1D). These results confirmed
the growth suppressive effects of genipin in bladder cancer.
Genipin induces G0/G1 cell cycle
arrest in bladder cancer cells
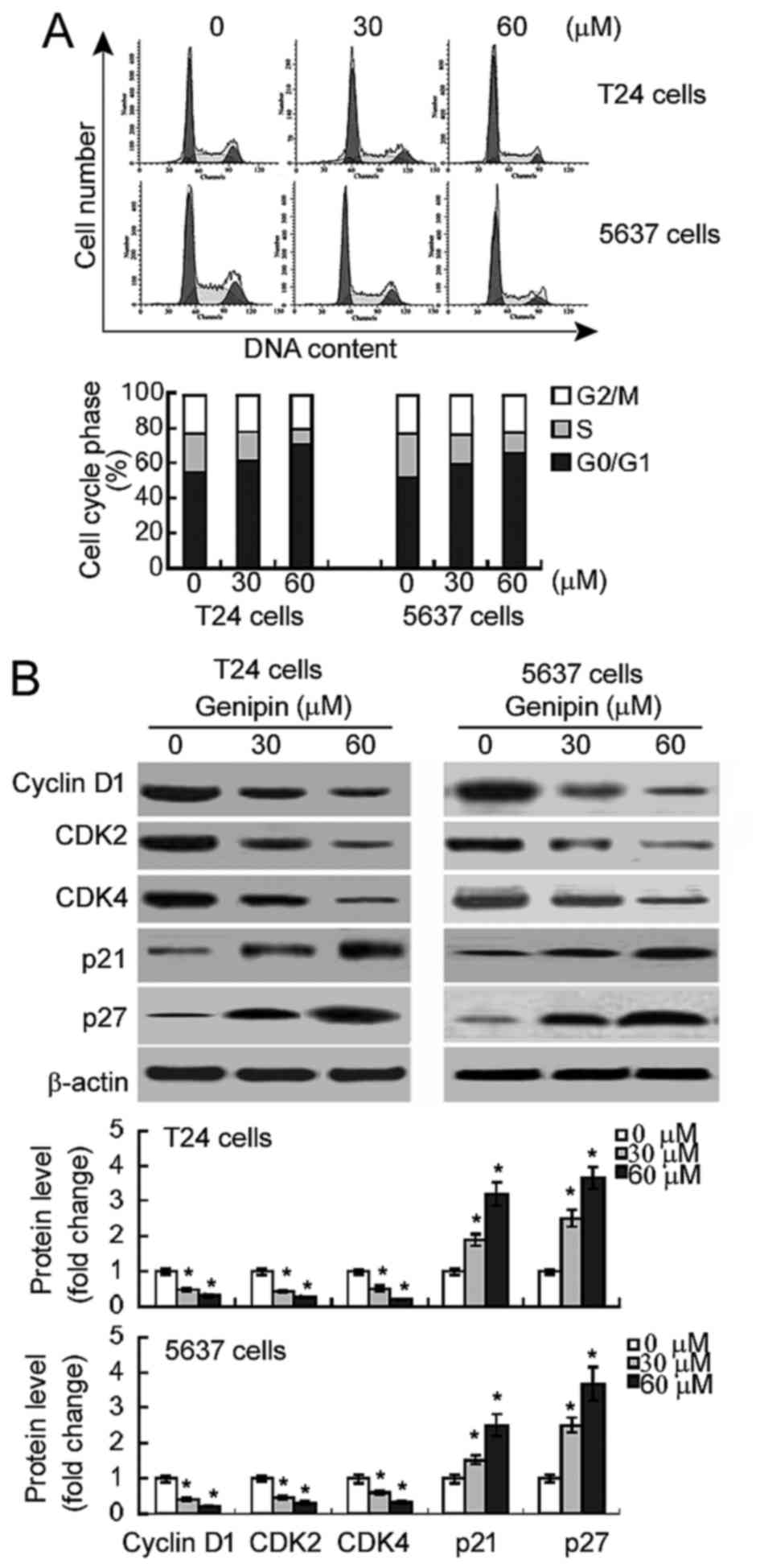
Flow cytometric analysis revealed that
genipin-treated T24 and 5,637 cells exhibited a marked increase in
the percentage of cells in the G0/G1 phase and a concomitant
reduction in the percentage of S phase cells (Fig. 2A). The percentage of cells in the G2/M
phase was comparable between genipin-treated and DMSO-treated
cells. Western blot analysis demonstrated that genipin treatment
significantly reduced the expression levels of cyclin D1, CDK2 and
CDK4 in T24 and 5,637 cells (Fig.
2B). By contrast, the levels of the CDK inhibitors (p21 and
p27) were significantly raised in response to genipin exposure.
Genipin promotes apoptosis in bladder
cancer cells via the mitochondrial pathway
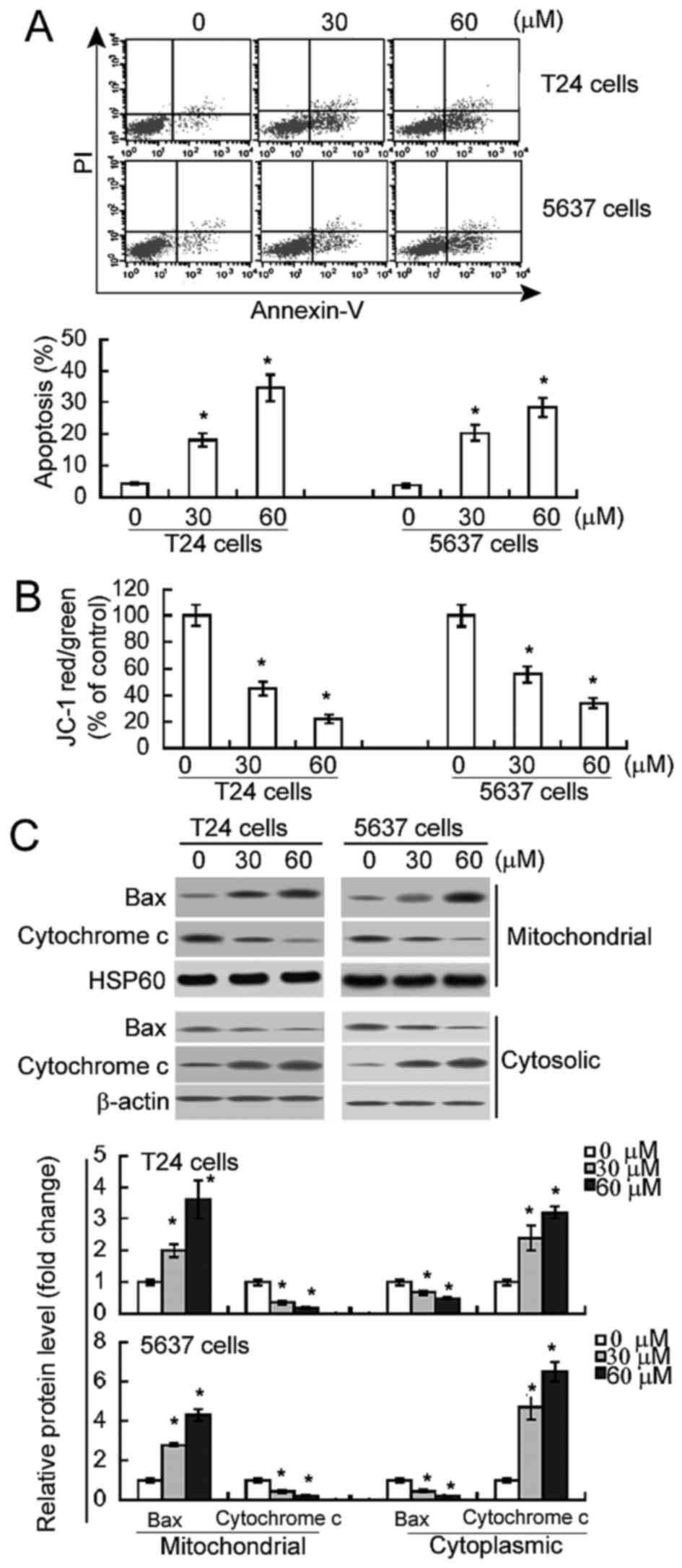
Annexin V/PI staining analysis demonstrated that
genipin treatment resulted in a significant increase in the
percentage of Annexin V-positive apoptotic cells, compared with
DMSO treatment (P<0.05; Fig. 3A).
Subsequent to treatment with 60 µM genipin, the percentage of
apoptotic cells increased from 4.5±0.9 to 34.6±2.1% in T24 cells
and from 3.9±0.8 to 28.5±2.4% in 5637 cells. To test the
involvement of the mitochondrial pathway in genipin-mediated
apoptosis, Δψm, Bax translocation into mitochondria and the release
of mitochondrial cytochrome c were measured. As demonstrated
in Fig. 3B, there was 70–80% loss in
Δψm in the cells treated with 60 µM genipin, compared with
DMSO-treated controls (P<0.05). Additionally, genipin-treated
cells exhibited increased Bax and decreased cytochrome c
expression in the mitochondrial fractions, compared with control
cells (P<0.05; Fig. 3C).
Additionally, there was decreased Bax and increased cytochrome
c expression in the cytoplasmic fractions of genipin-treated
cells (Fig. 3C). These results
suggest that genipin-induced apoptosis involves mitochondrial
damage and cytochrome c release.
Inactivation of PI3K/Akt signaling
mediates genipin-induced anticancer effects
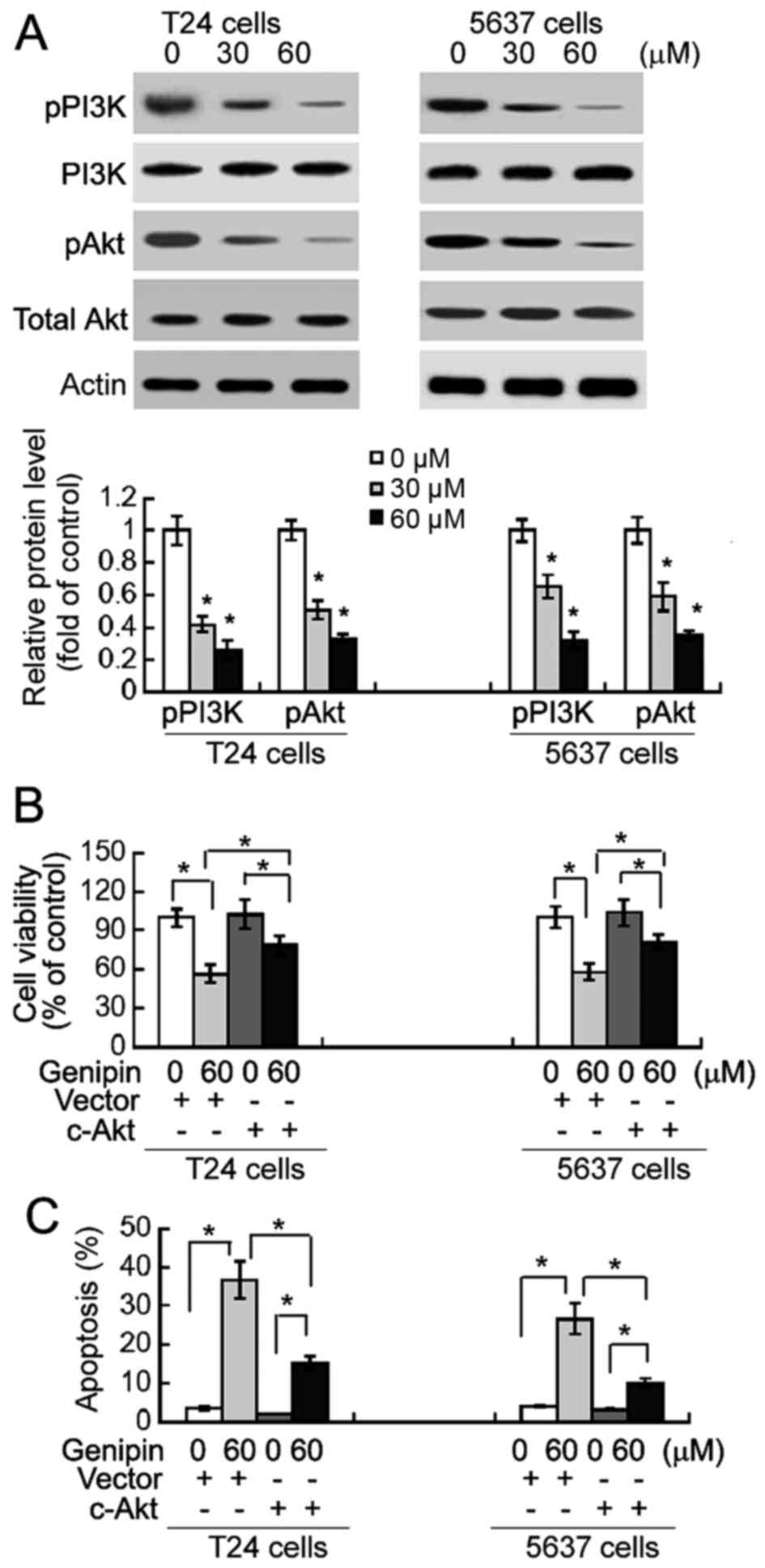
Finally, the potential involvement of PI3K/Akt
signaling in the anticancer activity of genipin was examined.
Western blot analysis suggested that genipin treatment
significantly (P<0.05) reduced the phosphorylation levels of
PI3K and Akt in T24 and 5637 cells, compared to DMSO-treated cells
(Fig. 4A). Of note, overexpression of
constitutively active Akt significantly (P<0.05) increased the
viability (Fig. 4B) and inhibited
apoptotic response (Fig. 4C) in
genipin-treated T24 and 5,637 cells.
Discussion
Natural phytochemicals have attracted increasing
attention in cancer therapy due to their broad anticancer activity
and low cytotoxicity in normal cells (14,18).
Genipin has demonstrated anticancer properties in different types
of cancers such as hepatocellular carcinoma (15) and colon cancer cells (16). The data of the present study indicated
that this natural compound also exerted anticancer effects against
bladder cancer cells. Genipin treatment significantly inhibited the
viability and clonogenic growth of bladder cancer cells in
vitro. Notably, a low concentration of genipin (≤60 µM) was
selectively cytotoxic to bladder cancer cells, but not
non-malignant uroepithelial cells. A previous study also indicates
the low cytotoxicity of genipin to normal cells (19). In vivo studies additionally
confirmed the inhibitory effect of genipin on the growth of bladder
cancer xenografts. Therefore, genipin may represent a promising
chemotherapeutic agent for bladder cancer.
As reduced cell growth often occurs as a result of
cell cycle arrest, the effect of genipin on cell cycle progression
of bladder cancer cells was next examined. It was identified that
genipin treatment induced a G0/G1 cell cycle arrest in T24 and
5,637 cells, as evidenced by an increase in the percentage of
G0/G1-phase cells and a reduction in the percentage of S-phase
cells. In agreement with these results, Cao et al (20) suggested that genipin induces cell
cycle arrest at the G1 phase in HeLa human cervical carcinoma
cells. Genipin has also been identified to induce G2/M-phase cell
cycle arrest in AGS human gastric cancer cells (21) and human leukemia K562 cells (22). These results suggest that the growth
suppressive activity of genipin is not cell cycle-specific. The
data of the present study also suggested that genipin-mediated cell
cycle arrest may be ascribed to a reduction of cyclin D1, CDK2 and
CDK4 expression, particularly the upregulation of p21 and p27.
Increased p21 and p27 levels have been identified to interfere with
the formation of CDKs/cyclin complexes and prevent the cell cycle
progression to S phase (23).
In addition to induction of cell cycle arrest,
genipin demonstrated the ability to cause apoptosis in bladder
cancer cells. In addition, genipin treatment resulted in
mitochondrial depolarization and the release of mitochondrial
cytochrome c into the cytosol. The pro-apoptotic protein Bax
has been documented to translocate from the cytosol to the
mitochondria in response to apoptotic stimuli, resulting in loss of
Δψm and release of cytochrome c (24). In the present study, it was observed
that genipin-treated bladder cancer cells exhibited increased Bax
levels in mitochondrial fractions and decreased Bax amounts in
cytoplasmic fractions. Overall, genipin induced apoptosis in
bladder cancer cells through Bax-mediated cytochrome c
release from the mitochondria. Similarly, induction of a
mitochondrial apoptotic cascade has been described in non-small
cell lung cancer H1299 cells following genipin treatment (25).
Inactivation of the PI3K/Akt pathway in
genipin-treated bladder cancer cells was also observed in the
present study, as evidenced by reduced phosphorylation levels of
PI3K and Akt. The PI3K/Akt pathway is involved in the regulation of
cancer cell growth and survival, and has been suggested as an
important anticancer target (6). Qin
et al (26) demonstrated that
(−)-epigallocatechin-3-gallate, a component of green tea, promotes
apoptosis in T24 bladder cancer cells through the inhibition of the
PI3K/Akt pathway. Kim et al (27) revealed that naproxen
[(S)-6-methoxy-α-methyl-2-naphthaleneacetic acid] induces
cell-cycle arrest and apoptosis in bladder cancer cells through the
inhibition of PI3K activity. To confirm the role of the PI3K/Akt
pathway in mediating the action of genipin, constitutively active
Akt was overexpressed in bladder cancer cells prior to genipin
exposure. Notably, it was observed that overexpression of
constitutively active Akt reversed the effects of genipin on
bladder cancer cell viability and apoptosis. Therefore, it may be
suggested that the genipin-induced anticancer effects against
bladder cancer cells are likely mediated through the inhibition of
PI3K/Akt signaling.
In summary, genipin exerts growth-suppressive
effects against bladder cancer cells via the induction of a G0/G1
cell cycle arrest and mitochondrial apoptosis. These anticancer
effects of genipin are largely ascribed to inhibition of the
PI3K/Akt pathway. Genipin may represent a potential anticancer
agent for bladder cancer.
References
|
1
|
Burger M, Catto JW, Dalbagni G, Grossman
HB, Herr H, Karakiewicz P, Kassouf W, Kiemeney LA, La Vecchia C,
Shariat S and Lotan Y: Epidemiology and risk factors of urothelial
bladder cancer. Eur Urol. 63:234–241. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mahdavifar N, Ghoncheh M, Pakzad R,
Momenimovahed Z and Salehiniya H: Epidemiology, incidence and
mortality of bladder cancer and their relationship with the
development index in the world. Asian Pac J Cancer Prev.
17:381–386. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ferlay J, Soerjomataram I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide: Sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Li S, Zeng XT, Ruan XL, Wang XH, Guo Y and
Yang ZH: Simultaneous transurethral resection of bladder cancer and
prostate may reduce recurrence rates: A systematic review and
meta-analysis. Exp Ther Med. 4:685–692. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Vinall RL, Tepper CG, Ripoll AA,
Gandour-Edwards RF, Durbin-Johnson BP, Yap SA, Ghosh PM and deVere
White RW: Decreased expression of let-7c is associated with
non-response of muscle-invasive bladder cancer patients to
neoadjuvant chemotherapy. Genes Cancer. 7:86–97. 2016.PubMed/NCBI
|
|
6
|
Cirone P, Andresen CJ, Eswaraka JR, Lappin
PB and Bagi CM: Patient-derived xenografts reveal limits to
PI3K/mTOR-and MEK-mediated inhibition of bladder cancer. Cancer
Chemother Pharmacol. 73:525–538. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang Y, Leng H, Chen H, Wang L, Jiang N,
Huo X and Yu B: Knockdown of UBE2T inhibits osteosarcoma cell
proliferation, migration, and invasion by suppressing the PI3K/Akt
signaling pathway. Oncol Res. 24:361–369. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dong Q, Fu L, Zhao Y, Tan S and Wang E:
Derlin-1 overexpression confers poor prognosis in muscle invasive
bladder cancer and contributes to chemoresistance and invasion
through PI3K/AKT and ERK/MMP signaling. Oncotarget. 8:17059–17069.
2017.PubMed/NCBI
|
|
9
|
Alayev A, Salamon RS, Schwartz NS, Berman
AY, Wiener SL and Holz MK: Combination of rapamycin and resveratrol
for treatment of bladder cancer. J Cell Physiol. 232:436–446. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nam KN, Choi YS, Jung HJ, Park GH, Park
JM, Moon SK, Cho KH, Kang C, Kang I, Oh MS and Lee EH: Genipin
inhibits the inflammatory response of rat brain microglial cells.
Int Immunopharmacol. 10:493–499. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang GF, Wu SY, Rao JJ, Lü L, Xu W, Pang
JX, Liu ZQ, Wu SG and Zhang JJ: Genipin inhibits endothelial
exocytosis via nitric oxide in cultured human umbilical vein
endothelial cells. Acta Pharmacol Sin. 30:589–596. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang CY, Parton LE, Ye CP, Krauss S, Shen
R, Lin CT, Porco JA Jr and Lowell BB: Genipin inhibits
UCP2-mediated proton leak and acutely reverses obesity- and high
glucose-induced beta cell dysfunction in isolated pancreatic
islets. Cell Metab. 3:417–427. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Suzuki Y, Kondo K, Ikeda Y and Umemura K:
Antithrombotic effect of geniposide and genipin in the mouse
thrombosis model. Planta Med. 67:807–810. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hughes RH, Silva VA, Ahmed I, Shreiber DI
and Morrison B III: Neuroprotection by genipin against reactive
oxygen and reactive nitrogen species-mediated injury in organotypic
hippocampal slice cultures. Brain Res. 1543:308–314. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang N, Zhu M, Tsao SW, Man K, Zhang Z and
Feng Y: Up-regulation of TIMP-1 by genipin inhibits MMP-2
activities and suppresses the metastatic potential of human
hepatocellular carcinoma. PLoS One. 7:e463182012. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wang R, MoYung KC, Zhao YJ and Poon K: A
mechanism for the temporal potentiation of genipin to the
cytotoxicity of cisplatin in colon cancer cells. Int J Med Sci.
13:507–516. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Perelman A, Wachtel C, Cohen M, Haupt S,
Shapiro H and Tzur A: JC-1: Alternative excitation wavelengths
facilitate mitochondrial membrane potential cytometry. Cell Death
Dis. 3:e4302012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Singh AN, Baruah MM and Sharma N:
Structure Based docking studies towards exploring potential
anti-androgen activity of selected phytochemicals against Prostate
Cancer. Sci Rep. 7:19552017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Koo HJ, Song YS, Kim HJ, Lee YH, Hong SM,
Kim SJ, Kim BC, Jin C, Lim CJ and Park EH: Antiinflammatory effects
of genipin, an active principle of gardenia. Eur J Pharmacol.
495:201–208. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Cao H, Feng Q, Xu W, Li X, Kang Z, Ren Y
and Du L: Genipin induced apoptosis associated with activation of
the c-Jun NH2-terminal kinase and p53 protein in HeLa cells. Biol
Pharm Bull. 33:1343–1348. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ko H, Kim JM, Kim SJ, Shim SH, Ha CH and
Chang HI: Induction of apoptosis by genipin inhibits cell
proliferation in AGS human gastric cancer cells via Egr1/p21
signaling pathway. Bioorg Med Chem Lett. 25:4191–4196. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Feng Q, Cao HL, Xu W, Li XR, Ren YQ and Du
LF: Apoptosis induced by genipin in human leukemia K562 cells:
Involvement of c-Jun N-terminal kinase in G2/M arrest. Acta
Pharmacol Sin. 32:519–527. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Coqueret O: New roles for p21 and p27
cell-cycle inhibitors: A function for each cell compartment? Trends
Cell Biol. 13:65–70. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pastorino JG, Chen ST, Tafani M, Snyder JW
and Farber JL: The overexpression of bax produces cell death upon
induction of the mitochondrial permeability transition. J Biol
Chem. 273:7770–7775. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yang X, Yao J, Luo Y, Han Y, Wang Z and Du
L: P38 MAP kinase mediates apoptosis after genipin treatment in
non-small-cell lung cancer H1299 cells via a mitochondrial
apoptotic cascade. J Pharmacol Sci. 121:272–281. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Qin J, Xie LP, Zheng XY, Wang YB, Bai Y,
Shen HF, Li LC and Dahiya R: A component of green tea,
(−)-epigallocatechin-3-gallate, promotes apoptosis in T24 human
bladder cancer cells via modulation of the PI3K/Akt pathway and
Bcl-2 family proteins. Biochem Biophys Res Commun. 354:852–857.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kim MS, Kim JE, Lim DY, Huang Z, Chen H,
Langfald A, Lubet RA, Grubbs CJ, Dong Z and Bode AM: Naproxen
induces cell-cycle arrest and apoptosis in human urinary bladder
cancer cell lines and chemically induced cancers by targeting PI3K.
Cancer Prev Res (Phila). 7:236–245. 2014. View Article : Google Scholar : PubMed/NCBI
|