Introduction
After surgical resection of localized colorectal
cancer, the tumor stage is determined by the extent of wall
invasion and lymph node (LN) involvement (1). When regional LN metastasis is
pathologically confirmed, the tumor is classified as Stage III
cancer of the colon and rectum. In such cases, postoperative
adjuvant chemotherapy is recommended to suppress tumor recurrence,
which improves overall survival (2).
When the tumor invades more than the muscular layer without LN
metastasis, the tumor is classified as Stage II. Although adjuvant
chemotherapy for Stage II colon cancer is not a general practice
due to the lack of survival benefit, a patient with a Stage II
tumor showing high risk features might benefit from adjuvant
chemotherapy. According to the European Society for Medical
Oncology and American Society of Clinical Oncology guidelines, in
addition to the pathological tumor type and more advanced wall
invasion, less than 12 pathologically evaluated LNs is also
considered as a risk factor for tumor recurrence (3,4).
The clear reason for the relationship between a
smaller number of retrieved LNs and poorer prognosis is not fully
understood, although several studies point out their connection
(5,6).
A diminished immunological response or weakened immune system may
contribute to the identification of fewer LNs and tumor progression
(5). Others speculate that inadequate
evaluation of LNs may result in stage migration, where stage III
disease is understated as Stage II. In addition to the need for
elucidating the underlying cause of this relationship, studies
clearly suggest that LNs need to be adequately examined in a
qualitative and quantitative manner.
The method of searching for LNs in Japan is unique
from other countries, where LN retrieval is performed by
pathologists or pathological assistants on formaldehyde-fixed
specimens (7,8). In most cases in Japan, surgeons search
for the LNs immediately after surgery (before fixation). The
mesentery is dissected from the large intestine, and the LNs within
the adipose tissue are inspected and palpated one-by-one after
cutting the peritoneum and connective tissues. A nationwide survey
held in Japan reported that this method yielded a mean LN number of
20.3 in the teaching hospitals. However, the number of LNs
identified may not be sufficient when performed in non-teaching
hospitals (9). We consider that this
method of LN retrieval requires a certain level of experience and
motivation. In addition, obesity [high body mass index (BMI)] might
hamper the identification of very small LNs within the abundant
adipose tissue (Y. Fujieda, unpublished data, 2017).
In this context, a simple and assured method of
identifying LNs after colorectal surgery needs to be established.
Thus, the present study aimed to evaluate the efficacy of a fat
dissolution liquid for aiding the search for LNs in the mesentery
of the colon and rectum. A fat dissolution method was originally
described by Fujino et al in 2014 using the enzymes,
collagenase and trypsin (10), while
the present study utilizes a commercially available fat dissolution
liquid composed of collagenase and lipase. As fat dissolution
liquid has been rarely used in the clinical setting, we planned to
evaluate whether additional LNs (which were initially overlooked)
could be identified by using the fat dissolution liquid on the
remnant mesentery, after LN retrieval by the conventional
inspection and palpation method.
Materials and methods
Patients
A target sample size of 20 patients was chosen for
the present study. Patients were included in the study if the
following inclusion criteria were met: i) a diagnosis of colorectal
cancer via endoscopic and/or pathological examination, requiring
surgical resection with LN dissection; ii) ≥20 years old; iii) the
ability to fully understand the present study; and iv) provided
written informed consent. Besides failing to meet the inclusion
criteria, the patients were excluded when investigators considered
it unsuitable to include the patient into this study. The study was
approved by the institutional review board of Kochi Medical School
(ID: 28–59), and conducted after written informed consent was
provided. The trial registration number is UMIN000023892.
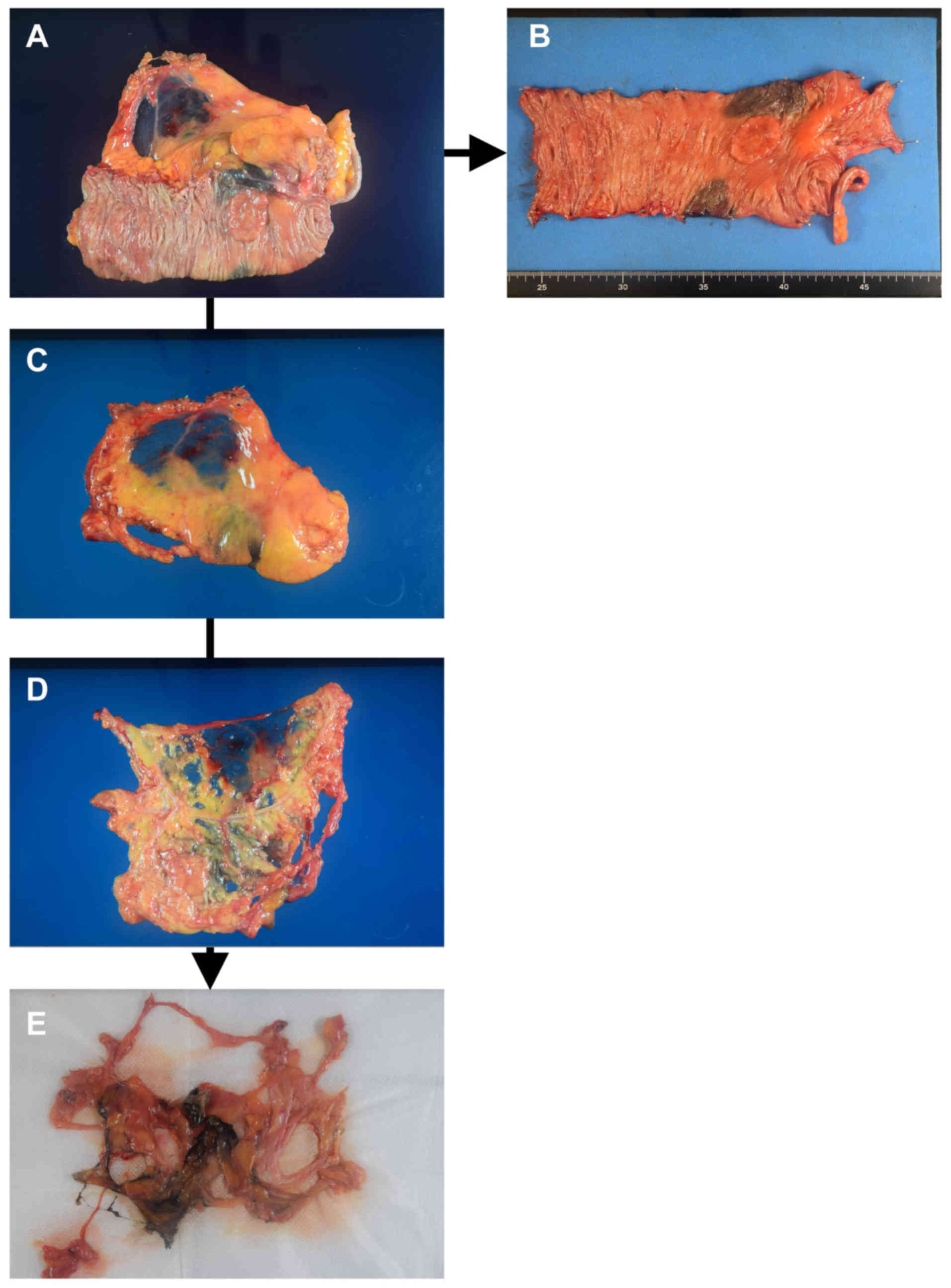
First LN search using the conventional
method
A regional LN search was performed immediately after
the operation using a manual technique, which is common practice in
our institute. First, the mesentery was dissected from the large
bowel (Fig. 1). The large bowel with
the primary tumor was pinned on a board to facilitate the
pathological diagnosis of wall invasion (T factor). For the
mesentery, the serous membrane was cut with scissors and the
tumor-feeding arteries were exposed to classify the LNs according
to the definition issued by the Japanese Society for Cancer of the
Colon and Rectum (11). The
connective tissue was gently cut and the LNs within the mesentery
were located by inspection and palpation. Identified LNs were fixed
in 10% formaldehyde and sent to the pathologist as LNs from the
first search.
Second LN search after fat
dissolution
A commercially available fat dissolution liquid was
provided by Sysmex (Kobe, Japan) according to the study contract.
The fat dissolution liquid was prepared by adding 50 ml of water
into crystallized collagenase and lipase, and then gently dissolved
immediately before use (the final concentration of collagenase and
lipase was not disclosed).
The liquid was injected into the remnant adipose
tissue using an 18G needle. The adipose tissue and liquid that
leaked out of the mesentery were incubated in a water bath at 37°C
for 40–60 min. The tissue was then transferred onto 5–10 sheets of
gauze to drain the liquid. The tissue was pressed with gauze
several times in order to further push out the remaining liquid
(Fig. 1E). Then, the tissue was
searched again for LNs for pathological examination.
Statistical analysis
The patient sample size was calculated based on the
hypothesis that the fat dissolution liquid could detect an
additional 20% of LNs from the number identified at the first
assessment. If the mean number of additional LNs was 3.0 (standard
deviation: 4.0), the required sample size was calculated as 16,
using two-sided α=0.05 and power=0.8. Finally, a target sample size
of 20 patients was chosen, allowing for some ineligible cases.
In this study, the LNs identified near the colon or
rectum during the microscopic examination for tumor wall invasion
were excluded from the analysis. The number of LNs obtained after
the first search was compared to the total number of LNs (defined
as the sum of the LNs identified at the first and second
assessments), using a paired t test. The maximum diameters of the
LNs obtained at the first and second assessments were compared
using the Wilcoxon signed-rank test. A P-value of less than 0.05
was considered significant. For statistical analysis and graph
depiction, Microsoft Office Excel 2007 (Microsoft Corporation,,
Redmond, WA) and JMP 12.2 (SAS Institute Inc., Cary, NC, USA) were
used.
Results
A total of 20 patients participated in this study
between September 2016 and January 2017. The clinical features of
the participating patients are presented in Table I. One patient was excluded from the
analysis because LN dissection was not performed due to an
oncological reason (Table I). Of the
remaining 19 patients, 7 were male, 6 had rectal cancer, and 17
underwent laparoscopic surgery. The mean age of the patients was
69.1 years and their mean BMI was 22.1 kg/m2 (Table I).
 | Table I.Patient and clinical
characteristics. |
Table I.
Patient and clinical
characteristics.
| Characteristics | Value |
|---|
| Patient
characteristics |
|
| Age, mean
(SD), years | 69.1 (10.1) |
| Sex
(male/female) | 7/12 |
| Body mass
index, mean (SD), kg/m2 | 22.1 (4.2) |
| Tumor
site (right side/left side/rectum) | 9/6/4 |
| Tumor and operative
characteristics |
|
| T factor
(T1/T2/T3/T4) | 2/5/9/3 |
| N factor
(node-negative/node-positive) | 16/3 |
| Distant
metastasis (No/yes) | 17/2 |
| Tumor
size, mean (SD), cm | 44.4 (21.6) |
|
Pathological type
(well/mod/muc/poor) | 6/10/1/2 |
| Surgical
approach (open/laparoscopic) | 2/17 |
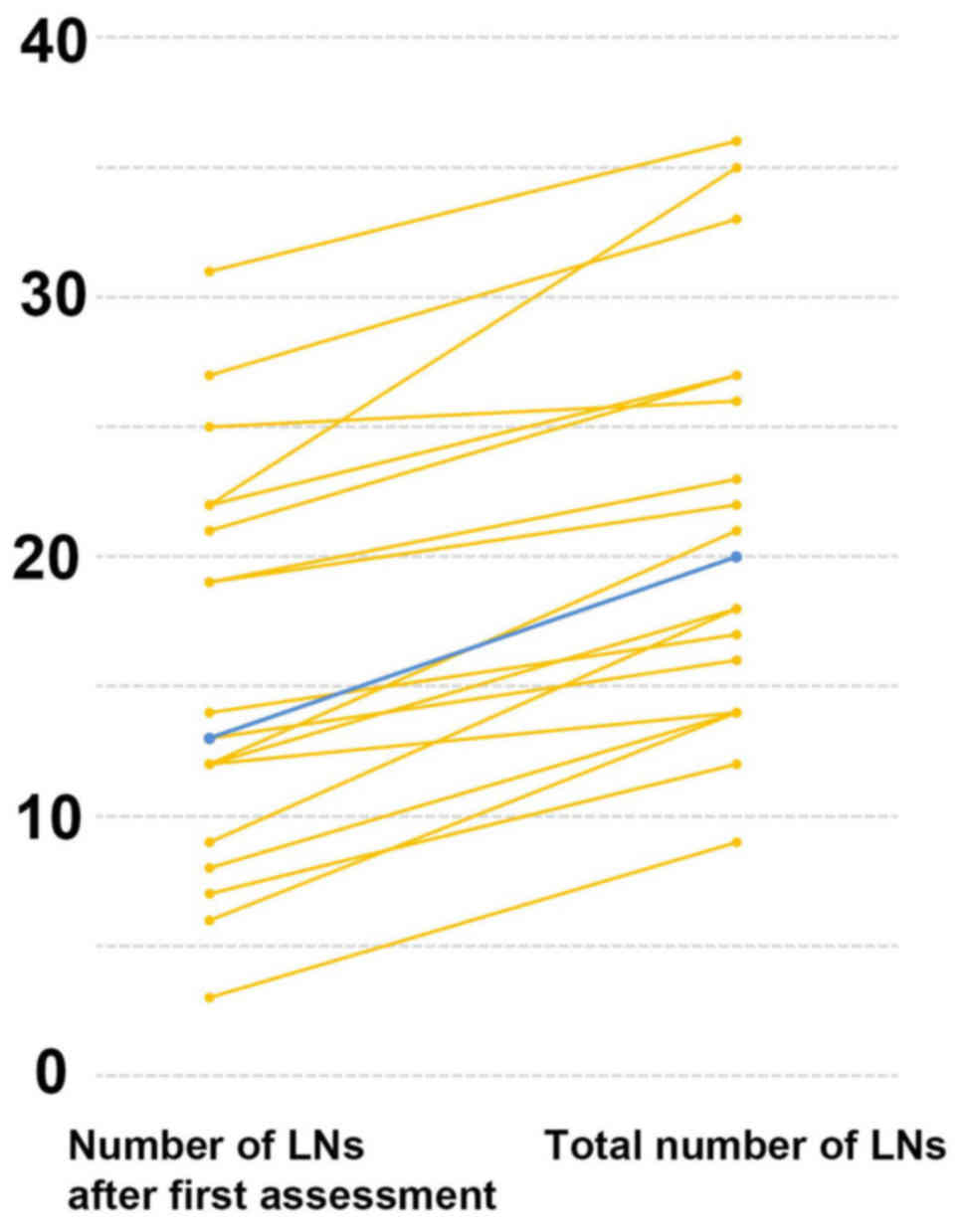
Primary endpoint
Number of LNs identified at first and
second assessments
The median number of LNs identified at the first
search was 13 (range, 3–31), while the second search identified a
median of 6 additional LNs (range, 1–13; Table II). Consequently, a paired t test
found a significant difference between the number of LNs found at
the first search and the total number of LNs found in the mesentery
(13 vs. 20, respectively; P<0.01; Fig.
2).
 | Table II.Number of LNs obtained from first and
second assessments and the number of LN metastases. |
Table II.
Number of LNs obtained from first and
second assessments and the number of LN metastases.
|
|
| First assessment | Second
assessment |
|
|---|
|
|
|
|
|
|
|---|
| Patient | Stage | LNs | Positive nodes | LNs | Positive nodes | Total LNs |
|---|
| 1a | I | 6 | 0 | 8 | 0 | 14 |
| 2a | I | 8 | 0 | 6 | 0 | 14 |
| 3 | I | 13 | 0 | 3 | 0 | 16 |
| 4 | I | 19 | 0 | 3 | 0 | 22 |
| 5 | I | 19 | 0 | 4 | 0 | 23 |
| 6 | I | 22 | 0 | 5 | 0 | 27 |
| 7 | I | 22 | 0 | 13 | 0 | 35 |
| 8a | II | 7 | 0 | 5 | 0 | 12 |
| 9a | II | 9 | 0 | 9 | 0 | 18 |
| 10 | II | 12 | 0 | 2 | 0 | 14 |
| 11 | II | 12 | 0 | 6 | 0 | 18 |
| 12 | II | 12 | 0 | 9 | 0 | 21 |
| 13 | II | 14 | 0 | 3 | 0 | 17 |
| 14 | II | 25 | 0 | 1 | 0 | 26 |
| 15 | II | 27 | 0 | 6 | 0 | 33 |
| 16 | II | 31 | 0 | 5 | 0 | 36 |
| 17 | III | 13 | 1 | 7 | 1 | 20 |
| 18 | IV | 3 | 2 | 6 | 0 | 9 |
| 19 | IV | 21 | 1 | 6 | 0 | 27 |
| Median | – | 13 | – | 6 | – | 20 |
| (range) |
| (3–31) |
| (1–13) |
| (9–36) |
| Mean | – | 15.5 | – | 5.6 | – | 21.2 |
| (SD) |
| (7.7) |
| (2.8) |
| (7.8) |
Secondary endpoints
Rate of positive LNs
Only one positive node was identified among the
additionally identified LNs. Therefore the rate of positive nodes
among the additional LNs was 0.9% (1/107), while that of the first
assessment was 1.4% (4/295).
Influence on treatment
Tumor staging was not altered by the additional
search for LNs. However, in four patients without distant
metastasis, the second search using the fat dissolution technique
had an impact on the adequacy of identified LNs, in terms of the
minimum number required for pathological examination (minimum of
12). In two patients with Stage I cancer and two with Stage II
cancer, less than 12 LNs were identified at the first search
(patient numbers 1, 2, 8 and 9 in Table
II). In the two patients with Stage I cancer, their subsequent
treatment would not have been influenced by the lack of an
additional LN search. However, in the two patients with Stage II
colorectal cancer, the tumor could have been diagnosed as high-risk
Stage II, and it would have been possible that adjuvant
chemotherapy was started in these two patients if the second LN
search had not been performed.
Maximum diameter of the additional
LNs
The median maximum diameter of the LNs obtained
after the second search was significantly smaller than the maximum
diameter of the LNs obtained at the first search (4 vs. 7.7 mm,
respectively; P<0.01, Wilcoxon signed-rank test; Table III). Meanwhile, the minimum diameter
of the LNs identified in the first and second assessments did not
differ significantly (1.9 vs. 1.1 mm, respectively; P=0.35;
Table III).
 | Table III.Diameter of LNs obtained at the first
and second assessments. |
Table III.
Diameter of LNs obtained at the first
and second assessments.
|
| First
assessment | Second
assessment |
|---|
|
|
|
|
|---|
| Patient | Maximum diameter
(mm) | Maximum diameter
(mm) | Maximum diameter
(mm) | Maximum diameter
(mm) |
|---|
| 1 |
5.1 | 1.5 | 4.0 | 1.0 |
| 2 |
6.9 | 1.2 | 4.0 | 1.1 |
| 3 |
8.2 | 1.0 | 4.2 | 1.3 |
| 4 | 12.6 | 2.5 | 5.0 | 2.0 |
| 5 |
7.7 | 1.3 | 4.0 | 2.1 |
| 6 |
7.1 | 0.9 | 6.7 | 2.2 |
| 7 |
4.4 | 0.5 | 2.1 | 0.9 |
| 8 |
9.0 | 1.8 | 4.2 | 2.1 |
| 9 |
4.7 | 1.0 | 4.0 | 1.2 |
| 10 |
4.0 | 0.9 | 2.6 | 2.3 |
| 11 |
6.4 | 1.0 | 4.0 | 2.0 |
| 12 | 14.3 | 4.0 | 9.0 | 3.6 |
| 13 |
5.9 | 1.5 | 2.7 | 1.8 |
| 14 | 11.0 | 1.0 | 2.4 | – |
| 15 |
7.3 | 1.1 | 4.0 | 0.9 |
| 16 | 11.7 | 0.9 | 7.2 | 1.8 |
| 17 | 11.7 | 1.0 | 4.9 | 2.0 |
| 18 | 14.0 | 4.1 | 2.8 | 1.5 |
| 19 |
8.5 | 1.5 | 5.0 | 2.1 |
| Median (range) | 7.7 (4–14.3) | 1.1 (0.5–4.1) | 4.0 (2.1–9) | 1.9 (0.9–3.6) |
| Mean (SD) | 8.4 (3.2) | 1.5 (1.0) | 4.4 (1.7) | 1.8 (0.7) |
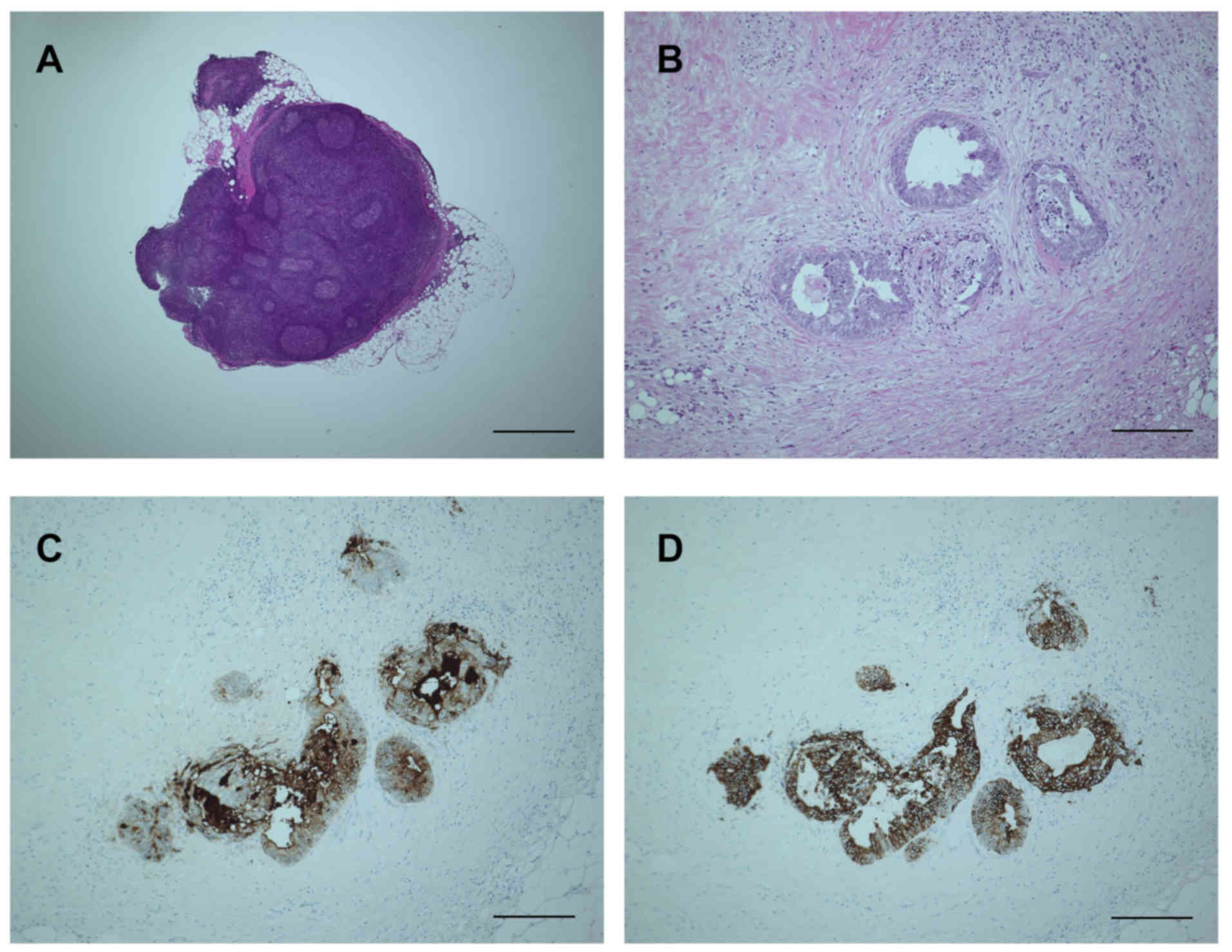
Staining for tumor-specific
antigens
Because only one patient had a tumor nodule among
the additionally obtained LNs, only one nodule was evaluated. As
there was no clear histological evidence of a residual LN in the
nodule, the node was diagnosed as a tumor nodule according to the
definition of the Japanese Classification of Cancer in the Colon
and Rectum (1,12), and the Union for International Cancer
Control-TNM classification. Immunohistochemistry clearly revealed
that the tumor cells were positive for carcinoembryonic antigen,
cytokeratin-20 and pankeratin (Fig.
3). These results suggest that the fat dissolution method does
not alter the stainability of tumor-specific antigens.
Discussion
This study clearly demonstrates that the fat
dissolution technique increases the total number of examined LNs
when applied to the remnant adipose tissue of the mesentery. In the
present study, the median and mean number of LNs obtained at the
first assessment was 13 and 15.6, respectively. A statistical
comparison between our previous data (12) and the results of this study was not
performed because the background characteristics significantly
influenced the number of LNs retrieved (5). However, we note that the median LN
number of 13 was quite similar to our previous data. Moreover, 13
of 17 patients (76.5%) with localized colorectal cancer received
adequate LN examination, which surpasses the rate reported from
non-teaching hospitals in the US, and is similar to that reported
from specialized institutes (13). We
consider that these two points suggest that the quality of the
first LN search was adequate. Nevertheless, the fat dissolution
technique applied to the remnant mesentery yielded additional LNs,
and as a result of the whole procedure, LN examination was
sufficiently performed in all but one patient with Stage IV
disease.
The comparison of the maximum diameters of LNs
obtained from the first and second assessments showed that the
residual LNs were smaller than those obtained with the conventional
method. However, searching for smaller LNs can still have a
significant clinical impact. Rodriguez-Bigas et al
retrospectively studied the size of LNs in patients with Stage III
colorectal cancer, identifying 253 positive nodes out of 3087 LNs.
Among the positive nodes, they reported that 69% were 5 mm or less
in diameter (14). Similarly, Rollvén
et al reported that 66% of positive nodes were less than 4
mm (15). Although tumor staging was
not influenced by the fat dissolution technique in the present
study, these reports highlight the importance of the examination of
an adequate number of LNs, irrespective of the size of the LNs.
The most significant drawback of the fat dissolution
technique introduced in the present study is the incubation time.
The incubation time could be reduced by modifying the
concentrations of collagenase and lipase (10), which is hampered by the increased cost
so far. The conventional method itself requires approximately 30–60
min to be performed (10), followed
by 40–60 min of incubation time for fat dissolution, and then the
second assessment. Therefore, this time-consuming procedure would
be quite difficult to perform in all cases as a routine practice.
Alternatively, it could be applied only to cases where a low number
of LNs have been retrieved by the conventional method, or in
patients where LN retrieval is expected to be difficult due to high
a BMI (Y. Fujieda, unpublished data, 2017). Another disadvantage is
that this method can only be used in specimens before formaldehyde
fixation.
Besides the small number of recruited patients, one
limitation of the present study was that the fat dissolution
technique was applied only to the remnant mesentery after the
initial conventional assessment. Although this technique could be
directly applied to the mesentery without a conventional LN search,
the efficacy of the technique under this setting has yet to be
determined. Another limitation is that only one metastatic node was
obtained after using the fat dissolution technique. While
hematoxylin and eosin staining and immunohistochemistry staining
demonstrated that fat dissolution does not hamper microscopic
examination, further study would be necessary to confirm this
finding. To address these points, another clinical study is
currently underway (UMIN ID: UMIN000029448).
In conclusion, the present study demonstrates that
our fat dissolution technique yields additional LNs for examination
when used on the remnant mesentery of the colon and rectum.
Specifically, this method should be considered when the number of
identified LNs is insufficient after conventional LN retrieval.
Acknowledgements
The authors would like to thank Ms. Nishimori and
Ms. Yamaguchi for their assistance with data management.
References
|
1
|
Union for International Cancer Control:
TNM Classification of Malignant Tumours. Sobin LH, Gospodarowicz MK
and Wittekind C: 7th edition. Wiley-Blackwell; Hoboken, NJ:
2010
|
|
2
|
Sargent DJ, Patiyil S, Yothers G, Haller
DG, Gray R, Benedetti J, Buyse M, Labianca R, Seitz JF, O'Callaghan
CJ, et al: End points for colon cancer adjuvant trials:
Observations and recommendations based on individual patient data
from 20,898 patients enrolled onto 18 randomized trials from the
ACCENT Group. J Clin Oncol. 25:4569–4574. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Benson AB III, Schrag D, Somerfield MR,
Cohen AM, Figueredo AT, Flynn PJ, Krzyzanowska MK, Maroun J,
McAllister P, Van Cutsem E, et al: American society of clinical
oncology recommendations on adjuvant chemotherapy for stage II
colon cancer. J Clin Oncol. 22:3408–3419. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Schmoll HJ, Van Cutsem E, Stein A,
Valentini V, Glimelius B, Haustermans K, Nordlinger B, van de Velde
CJ, Balmana J, Regula J, et al: ESMO consensus guidelines for
management of patients with colon and rectal cancer. A personalized
approach to clinical decision making. Ann Oncol. 23:2479–2516.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Märkl B: Stage migration vs. immunology:
The lymph node count story in colon cancer. World J Gastroenterol.
21:12218–12233. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Parsons HM, Tuttle TM, Kuntz KM, Begun JW,
McGovern PM and Virnig BA: Association between lymph node
evaluation for colon cancer and node positivity over the past 20
years. JAMA. 306:1089–1097. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kuo YH, Lee KF, Chin CC, Huang WS, Yeh CH
and Wang JY: Does body mass index impact the number of LNs
harvested and influence long-term survival rate in patients with
stage III colon cancer? Int J Colorectal Dis. 27:1625–1635. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Linebarger JH, Mathiason MA, Kallies KJ
and Shapiro SB: Does obesity impact lymph node retrieval in colon
cancer surgery? Am J Surg. 200:478–482. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ueno H, Hase K, Hashiguchi Y, Shinto E,
Shimazaki H, Yamamoto J, Nakamura T and Sugihara K: Potential
causes of stage migration and their prognostic implications in
colon cancer: A nationwide survey of specialist institutions in
Japan. Jpn J Clin Oncol. 44:547–555. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fujino S, Miyoshi N, Ohue M, Noura S,
Tomita Y, Yano M and Sakon M: New enhanced and effective method for
staging cancer to detect lymph nodes after fat-dissociation. Oncol
Rep. 32:922–926. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Japanese Society for Cancer of the Colon
and Rectum: Japanese Classification of Colorectal Carcinoma. 8th
edition. Kanehira-Syuppan; Tokyo: 2013, (In Japanese).
|
|
12
|
Shiga M, Maeda H, Oba K, Okamoto K,
Namikawa T, Fujisawa K, Yokota K, Kobayashi M and Hanazaki K:
Safety of laparoscopic surgery for colorectal cancer in patients
over 80 years old: A propensity score matching study. Surg Today.
47:951–958. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Baxter NN, Virnig DJ, Rothenberger DA,
Morris AM, Jessurun J and Virnig BA: Lymph node evaluation in
colorectal cancer patients: A population-based study. J Natl Cancer
Inst. 97:219–225. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rodriguez-Bigas MA, Maamoun S, Weber TK,
Penetrante RB, Blumenson LE and Petrelli NJ: Clinical significance
of colorectal cancer: Metastases in lymph nodes <5 mm in size.
Ann Surg Oncol. 3:124–130. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rollvén E, Abraham-Nordling M, Holm T and
Blomqvist L: Assessment and diagnostic accuracy of lymph node
status to predict stage III colon cancer using computed tomography.
Cancer Imaging. 17:32017. View Article : Google Scholar : PubMed/NCBI
|