Introduction
Renal cell carcinoma (renal carcinoma for short) is
a kind of tumor with a high malignancy in the urinary system, and
it is one of the most common tumors. Also known as renal
adenocarcinoma, it is a malignant tumor originated in the tubule
epithelium in the renal parenchyma, accounting for 80–90% in renal
malignant tumor (1). Its incidence
and mortality rate are currently on the increase. Tumor metastasis
has been identified in approximately half of the patients when they
are examined, and a postoperative relapse rate as high as 90% is
evident in more than half of the patients (2). Renal carcinoma exhibits special genetic
and biological characteristics, heterogeneity and easy metastasis.
Conventional chemoradiotherapy has no ideal effect on renal
carcinoma with metastasis. Studies have found that satisfactory
therapeutic effects have been obtained by applying molecular
immunology, gene therapy and molecular-targeted therapy for tumor
vascularization for advanced or metastatic renal carcinoma
(3). The emergence of
tumor-associated factors has a good application prospect for the
diagnosis and treatment of renal carcinoma.
T-box (TBX) genes have the function of
regulating transcription factors related to development, and
TBX3 gene plays its role mainly by means of its expression
product TBX3 protein, which is involved in each process of
embryonic development in order to guarantee the normal
differentiation and development of tissues and organs in the
embryonic period (4). Previous
findings showed that the expression of TBX3 mRNA in some tumor
tissues is markedly higher than that in adjacent tissues (5). It has been concluded from statistical
analyses that several clinical features, including lymph node
metastasis and tumor-node-metastasis (TNM) staging, have a
significant correlation with the abnormal expression of TBX3
gene (6). Some studies also indicate
that TBX3 gene is an oncogene (7),
and TBX3 protein is a major product of its function. Furthermore,
TBX3 protein is a kind of inhibitory factor associated with
transcription, and the normal differentiation and development of
organs and tissues are dependent on its expression to some extent
(8,9).
Therefore, this study was conducted to investigate the correlation
of TBX3 gene with the occurrence and metastasis of renal
carcinoma by analyzing the expression level of TBX3 gene in
renal carcinoma tissues of patients with the disease.
Materials and methods
Research objects and materials
In total, 210 patients with renal carcinoma who were
admitted and treated in The Central Hospital of Wuhan, Tongji
Medical College (Wuhan, China) from March, 2006 to March, 2012 were
selected, and their carcinoma, adjacent and normal renal tissues
(renal tissues more than 3 cm away from the tumor) were collected.
Of the 210 patients, 86 patients were aged <60 years and 124
were aged ≥60 years, and 140 cases were males and 70 cases were
females. Concerning TNM staging, 146 patients were in stage I–II
and 64 were in stage III–IV. Regarding pathological typing, there
were 165 cases of clear cell carcinoma and 45 cases of non-clear
cell carcinoma, of which 95 cases were at low grade, and 115 were
at middle and high grade.
Inclusion criteria for the study were: Patients who
were histopathologically confirmed as renal carcinoma; patients who
did not undergo chemoradiotherapy; and patients who voluntarily
accepted this research and signed the informed consent. Exclusion
criteria for the study were: Patients complicated with other
malignant tumors; patients with congenital malformation or a long
history of nephritis; patients with severe hepatic or renal
dysfunction and coagulation disorders; and patients unable to
cooperate with the research due to various reasons. All the
patients received a long-term follow-up of >5 years. The study
was approved by the Ethics Committee of The Central Hospital of
Wuhan.
Major reagents
The quantitative polymerase chain reaction (qPCR)
reagent used was, EvaGreen fluorescence quantitative PCR reagent
(Biotium, Inc., Hayward, CA, USA). RNA extraction reagent TRIzol,
and reverse transcription kit (Invitrogen, Carlsbad, CA, USA) as
well as DNA Marker (100 bp ladder) (Beijing Dingguo Center for
Biotechnology Development, Beijing, China) were also used.
Reverse transcription-polymerase chain
reaction (RT-PCR)
Premier 6.0 software (Premier Biosoft International,
Palo Alto, USA) was used as a reference for the primer sequences of
TBX3 (primers were produced by Shanghai Yingjun Biological
Technology Co., Ltd., Shanghai, China). The upstream and downstream
sequences of TBX3 were: 5′-CCCGAAGAAGACGTAGAAGATGAC-3′, and
5′-CCCGAAGAAGAGGTGGAGGACGAC-3′. β-actin was used as an internal
reference primer, and the upstream and downstream sequences were
5′-CCTCCATCGTCCACCGCAAATG-3′ and 5′-TGCTGTCACCTTCACCGTTCCA-3′.
Methods
SYBR-Green I Real-Time PCR kit was utilized to
amplify target genes, of which the primers are listed above. The
2−∆∆Cq method was applied to detect the relative
expression levels of relevant genes. The RNAs of samples were
extracted in accordance with the methods and principles of qPCR.
Ultraviolet adsorption was used to measure the concentration and
purity of the RNA solution. Complementary DNA (cDNA) was produced
according to the conventional methods. The cDNA of renal carcinoma
tissue was marked as group A, adjacent tissues as group B, and
normal renal tissues as group C.
Statistical analysis
In the present study, Statistical Product and
Service Solutions (SPSS) 18.0 software (Chicago, IL, USA) was used
for statistical analyses on the data of this research. The
χ2 test was used for comparison between groups.
Measurement data were presented as mean ± standard deviation. The
t-test was used for comparison between groups. Cox regression model
was used for multivariate analyses on factors influencing the
prognosis of patients with renal carcinoma which were obtained from
the univariate analyses. The Kaplan-Meier survival analysis was
used to show the median survival time of patients in the two
groups. P<0.05 was considered to indicate a statistically
significant difference.
Results
Expression levels of TBX3 gene in
renal carcinoma tissues, adjacent tissues and normal renal
tissues
The comparison of the renal carcinoma tissues with
the adjacent tissues showed that TBX3 gene was obviously
highly expressed in renal carcinoma tissues (P<0.05). Compared
with that in normal renal tissues, TBX3 gene was obviously
highly expressed in renal carcinoma tissues (P<0.05). There was
no significant difference in the expression levels of TBX3
gene in normal renal tissues and adjacent tissues (P=0.15)
(Table I).
 | Table I.Expression levels of TBX3 gene
in renal carcinoma tissues, adjacent tissues and normal renal
tissues. |
Table I.
Expression levels of TBX3 gene
in renal carcinoma tissues, adjacent tissues and normal renal
tissues.
| Group | Renal carcinoma
tissues | Adjacent tissues | Normal renal
tissues |
|---|
| Expression level | 1.139±0.453 | 0.495±0.336 | 0.412±0.298 |
| P-value | P<0.05 | P=0.15 |
Relationship between the expression
level of TBX3 gene in renal carcinoma tissues and clinical
features
According to the median expression level (0.769) of
TBX3 gene in renal carcinoma tissues, the patients were
divided into the positive TBX3 gene expression group (105
patients in total, of which the TBX3 gene expression level
was >0.769) and the negative TBX3 gene expression group
(105 patients in total, of which the TBX3 gene expression
level was <0.769). The TBX3 gene expression level in the
carcinoma tissues with lymph node metastasis was obviously elevated
compared with that in carcinoma tissues without lymph node
metastasis (P<0.05). The expression of TBX3 gene in renal
carcinoma tissues was not related to the patients' age, sex and
depth of tumor invasion (P>0.05), but it was associated with TNM
staging and lymph node metastasis (P<0.05) (Table II).
 | Table II.Relationship between expression level
of TBX3 gene in renal carcinoma tissues and
clinicopathologic characteristics. |
Table II.
Relationship between expression level
of TBX3 gene in renal carcinoma tissues and
clinicopathologic characteristics.
|
| TBX3 gene
expression |
|
|---|
|
|
|
|
|---|
| Clinicopathologic
characteristics | Positive (n) | Negative (n) | P-value |
|---|
| Age (years old) |
|
| 0.198 |
|
<60 | 41 | 45 |
|
|
≥60 | 64 | 60 |
|
| Sex |
|
| 0.121 |
|
Male | 69 | 71 |
|
|
Female | 36 | 34 |
|
| TNM staging |
|
| 0.008a |
|
I+II | 56 | 90 |
|
|
III+IV | 49 | 15 |
|
| Lymph node
metastasis |
|
| 0.012a |
|
Yes | 74 | 11 |
|
| No | 31 | 94 |
|
| Pathological
grading |
|
| 0.097 |
| Middle
and high | 53 | 57 |
|
|
Low | 52 | 48 |
|
| Tumor size |
|
| 0.061 |
|
<7 | 45 | 66 |
|
| ≥7 | 60 | 39 |
|
| Pathological
typing |
|
| 0.135 |
| Clear
cell carcinoma | 79 | 86 |
|
|
Non-clear cell carcinoma | 26 | 19 |
|
Univariate analyses on factors
influencing prognosis of renal carcinoma
The results showed that TNM staging, lymph node
metastasis and 5-year survival rate of TBX3 gene had
statistical significance (P<0.05), indicating that the factors
affecting the prognosis of renal carcinoma. However, sex, age,
degree of differentiation and tumor size had no significant
differences on the 5-year survival rate of patients (P>0.05)
(Table III).
 | Table III.Clinicopathologic data of renal
carcinoma and 5-year survival rate. |
Table III.
Clinicopathologic data of renal
carcinoma and 5-year survival rate.
| Clinicopathologic
characteristics | Case | 5-year survival
rate (%) | χ2
test | P-value |
|---|
| Age (years
old) |
|
|
3.68 | 0.126 |
|
<60 | 86 | 50.1 |
|
|
|
≥60 | 124 | 48.3 |
|
|
| Sex |
|
|
4.14 | 0.121 |
|
Male | 140 | 49.8 |
|
|
|
Female | 70 | 51.2 |
|
|
| TNM staging |
|
| 12.35 | 0.000a |
|
I+II | 146 | 80.5 |
|
|
|
III+IV | 64 | 40.7 |
|
|
| Lymph node
metastasis |
|
| 10.17 | 0.002a |
|
Yes | 85 | 41.1 |
|
|
| No | 125 | 84.2 |
|
|
| Pathological
grading |
|
|
7.56 | 0.189 |
| Middle
and high | 110 | 52.9 |
|
|
|
Low | 100 | 43.7 |
|
|
| Tumor size |
|
|
6.47 | 0.076 |
|
<7 | 111 | 78.6 |
|
|
| ≥7 | 99 | 51.4 |
|
|
| Pathological
typing |
|
|
7.13 | 0.147 |
| Clear
cell carcinoma | 165 | 61.2 |
|
|
|
Non-clear cell carcinoma | 45 | 49.8 |
|
|
| TBX3 gene
expression |
|
| 10.21 | 0.006a |
|
Positive | 105 | 62.0 |
|
|
|
Negative | 105 | 32.0 |
|
|
Multivariate analyses on factors
influencing the prognosis of renal carcinoma
Cox regression model was used for multivariate
analyses on factors influencing the prognosis of patients with
renal carcinoma which were obtained from the univariate analyses
(P<0.05). It was found that TNM staging, lymph node metastasis
and TBX3 gene expression level were the independent risk
factors for renal carcinoma (P<0.05) (Table IV).
 | Table IV.Multivariate analyses on prognosis of
renal carcinoma. |
Table IV.
Multivariate analyses on prognosis of
renal carcinoma.
| Variables | Odds ratio
(OR) | 95% confidence
interval (95% CI) | P-value |
|---|
| TBX3 gene
expression | 4.24 | 1.87–5.35 | 0.016a |
| Lymph node
metastasis | 3.19 | 2.18–8.56 | 0.023a |
| TNM staging | 3.67 | 2.47–7.62 | 0.004a |
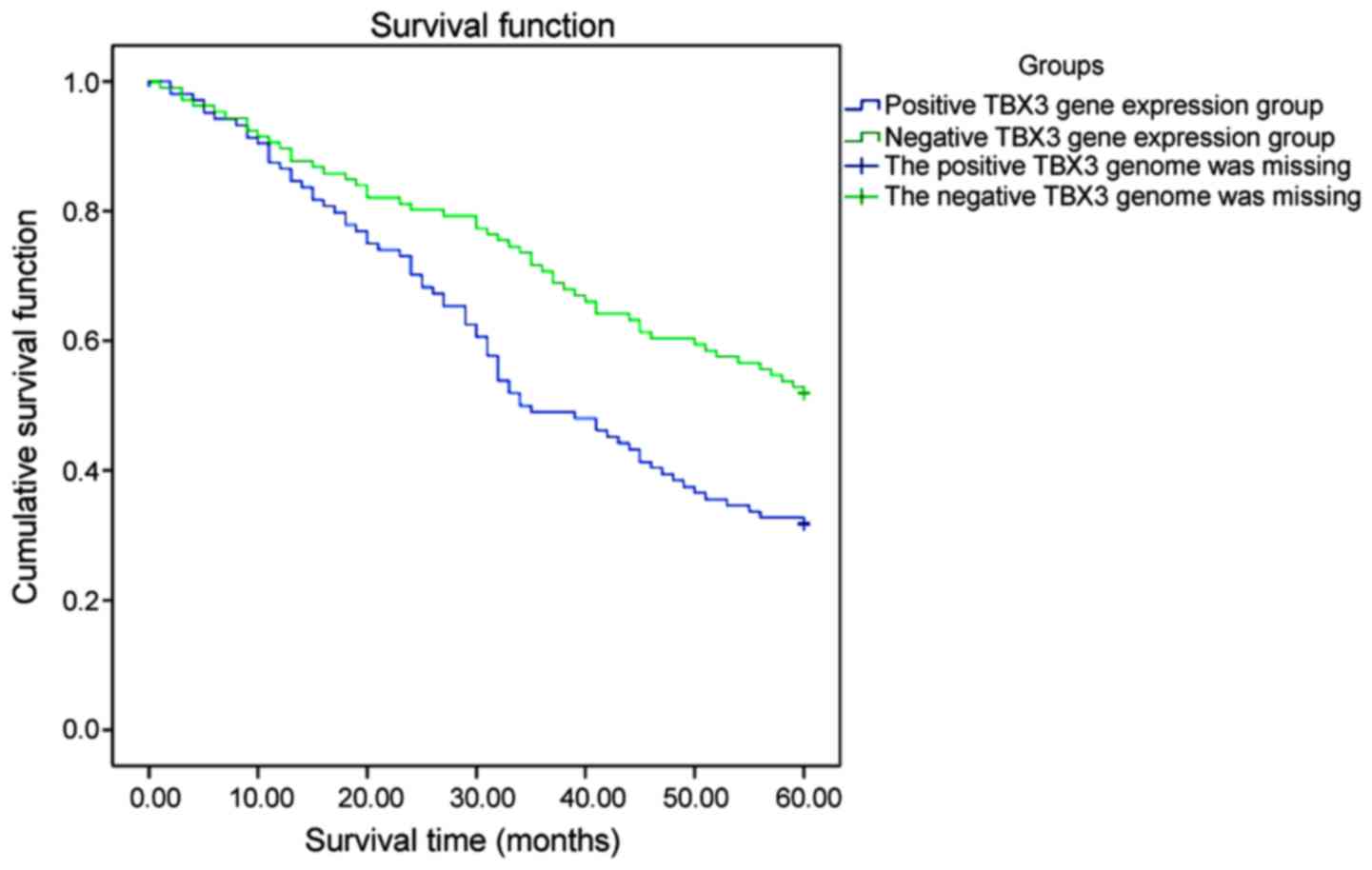
Relationship between the expression of
TBX3 gene in renal carcinoma and prognosis
The Kaplan-Meier survival analysis revealed that the
median survival time of patients in the positive TBX3 gene
expression group (37.5 months) was lower than that in the negative
TBX3 gene expression group (66 months), and there was a
statistical difference (P<0.05). The 3- and 5-year survival
rates in the negative TBX3 gene expression group were 74 and
62%, respectively. The 3- and 5-year survival rates in the positive
TBX3 gene expression group were 52 and 32%, respectively,
and the differences were significant (P<0.05) (Fig. 1).
Discussion
Studies in recent years have indicated that
TBX3 gene is highly expressed in multiple tumors, and
studies have been conducted with regard to breast cancer,
pancreatic cancer, colorectal cancer, lung cancer and melanoma
(10–14). However, to the best of our knowledge,
there is no detailed research on TBX3 gene in renal
carcinoma. Currently, the cause of renal carcinoma has yet to be
elucidated, and most of the clinical manifestations of early renal
carcinoma are not obvious. Most renal carcinomas are in advanced
stage once they are identified, and the staging of the disease is
closely associated with the 5-year survival rate (15,16). This
experiment provided an important reference for early diagnosis,
metastasis and other aspects of renal carcinoma by studying the
expression level of TBX3 gene in renal carcinoma tissues. It
also offered a better basis for assisting clinicians to treat the
disease. In the age of precision medicine (17), TBX3 gene is to become a
potentially effective therapeutic target and prognostic indicator
in patients with renal carcinoma.
Current studies have revealed that TBX3 gene
is closely associated with the occurrence and development of many
kinds of malignant tumors. TBX3 gene has multiple oncogenic
mechanisms, and studies have found that this gene can inhibit the
expression of cancer suppressive factor p19ARF (human p19ARF) of
inhibitor of CDK4/alternative reading frame (INK4α/ARF), in order
to suppress cell growth (18). As a
result, there is a small amount of TBX3 gene expression in
normal cells, which is consistent with Smith et al (18). Some scholars have found that
TBX3 gene can directly inhibit the cells by suppressing the
promoters of cyclin p21 (Cip1/WAF1) (19). In addition, TBX3 gene can act
on the transcriptional activation of p21 by attenuating p53
(20). In breast cancer, for example,
it can also be observed that TBX3 gene is upregulated.
Previous findings have revealed that TBX3 gene is associated
with the Wnt/β-catenin signaling pathway for tumor formation, and
the overexpression of TBX3 gene can inhibit the expression
levels of suppressor genes in normal cells, thus accelerating the
formation and development of malignant tumors (19,20). Other
studies have found that TBX3 gene can strengthen the
invasiveness of tumors by suppressing E-cadherin on the surface of
cell membrane and upregulating β-catenin (21,22), thus
leading to the invasion and metastasis of malignant tumors. In the
present study, the TBX3 gene expression level in tumor
tissues with lymph node metastasis of patients with renal carcinoma
was obviously elevated, which may be associated with the fact that
TBX3 gene can trigger tumor metastasis. Scholars have found
that TBX3 gene can exert its carcinogenic effect by virtue
of transforming growth factor-β1 (TGF-β1) (23–25).
Therefore, TBX3 gene can promote migration and invasion,
playing a vital role in the migration of malignant tumors (26).
In this study, the expression levels of TBX3
gene in renal carcinoma, adjacent and normal tissues were
investigated using a large sample size. The specimens were
collected in our hospital and the samples were strictly controlled
in accordance with the inclusion and exclusion methods, to
guarantee the reliability of the samples. The limitation of this
study was that it was a single-center study, which had a certain
sampling bias in terms of population and region. qPCR was applied
in this experiment to reverse transcribe cDNA, in order to
reversely infer the expression level of TBX3 gene. As a
result, it had decided that this experiment has shortcomings such
as money and time consumption. However, it was fully demonstrated
in this research that compared with that in the adjacent tissues,
TBX3 gene was obviously highly expressed in renal carcinoma
tissues (P<0.05). There was no significant difference in the
expression levels of TBX3 gene in normal renal and adjacent
tissues (P=0.15). Findings of the present study were consistent
with results of the studies conducted by Wang et al
(27) and Shan et al (28), which revealed that TBX3 gene
was highly expressed in tumors. It was shown in the present study
that the expression of TBX3 gene in renal carcinoma tissues
was not related to the patients' age, sex and tumor size
(P>0.05), but it was associated with TNM staging and lymph node
metastasis (P<0.05). The high expression of TBX3 gene may
be associated with tumor metastasis, results obtained by Li and
Varelas (20,21). The results of the presents study
showed that the median survival time of patients in the positive
TBX3 gene expression group (37.5 months) was lower than that
in the negative TBX3 gene expression group (66 months), and
there was a statistical difference (P<0.05). The 3- and 5-year
survival rates in the negative TBX3 gene expression group
were 74 and 62%, respectively. The 3- and 5-year survival rates in
the positive TBX3 gene expression group were 52 and 32%,
respectively, and the differences were significant (P<0.05).
In conclusion, TBX3 gene is highly expressed
in renal carcinoma tissues, and is associated with TNM staging,
lymph node metastasis and distant metastasis, and may be involved
in the occurrence and metastasis of renal carcinoma.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors’ contributions
YW researched the literature, designed the study,
analyzed and interpreted the patient data.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
The Central Hospital of Wuhan. Patients voluntarily accepted this
research and signed the informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fang Y, Bao W, Rao Q, Wang X, Xia Q, Shen
Q, Zhou X and Yao B: TFE3 regulates renal adenocarcinoma cell
proliferation via activation of the mTOR pathway. Mol Med Rep.
16:2721–2725. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wu X, Weng L, Li X, Guo C, Pal SK, Jin JM,
Li Y, Nelson RA, Mu B, Onami SH, et al: Identification of a
4-microRNA signature for clear cell renal cell carcinoma metastasis
and prognosis. PLoS One. 7:e356612012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Russo P: Renal cell carcinoma:
Presentation, staging, and surgical treatment. Semin Oncol.
27:160–176. 2000.PubMed/NCBI
|
|
4
|
Papaioannou VE: The T-box gene family:
Emerging roles in development, stem cells and cancer. Development.
141:3819–3833. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ito A, Asamoto M, Hokaiwado N, Takahashi S
and Shirai T: Tbx3 expression is related to apoptosis and cell
proliferation in rat bladder both hyperplastic epithelial cells and
carcinoma cells. Cancer Lett. 219:105–112. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ansari D, Rosendahl A, Elebro J and
Andersson R: Systematic review of immunohistochemical biomarkers to
identify prognostic subgroups of patients with pancreatic cancer.
Br J Surg. 98:1041–1055. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Boyd SC, Mijatov B, Pupo GM, Tran SL,
Gowrishankar K, Shaw HM, Goding CR, Scolyer RA, Mann GJ, Kefford
RF, et al: Oncogenic B-RAF(V600E) signaling induces the T-Box3
transcriptional repressor to repress E-cadherin and enhance
melanoma cell invasion. J Invest Dermatol. 133:1269–1277. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu J, Esmailpour T, Shang X, Gulsen G,
Liu A and Huang T: TBX3 over-expression causes mammary gland
hyperplasia and increases mammary stem-like cells in an inducible
transgenic mouse model. BMC Dev Biol. 11:652011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lu R, Yang A and Jin Y: Dual functions of
T-box 3 (Tbx3) in the control of self-renewal and extra embryonic
endoderm differentiation in mouse embryonic stem cells. J Biol
Chem. 286:8425–8436. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Dhawan P, Singh AB, Ellis DL and Richmond
A: Constitutive activation of Akt/protein kinase B in melanoma
leads to up-regulation of nuclear factor-kappaB and tumor
progression. Cancer Res. 62:7335–7342. 2002.PubMed/NCBI
|
|
11
|
Renard CA, Labalette C, Armengol C, Cougot
D, Wei Y, Cairo S, Pineau P, Neuveut C, de Reynies A, Dejean A, et
al: Tbx3 is a downstream target of the Wnt/beta-catenin pathway and
a critical mediator of beta-catenin survival functions in liver
cancer. Cancer Res. 67:901–910. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yarosh W, Barrientos T, Esmailpour T, Lin
L, Carpenter PM, Osann K, Anton-Culver H and Huang T: TBX3 is
overexpressed in breast cancer and represses p14 ARF by interacting
with histone deacetylases. Cancer Res. 68:693–699. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang HC, Meng QC, Shan ZZ, Yuan Z and
Huang XY: Overexpression of Tbx3 predicts poor prognosis of
patients with resectable pancreatic carcinoma. Asian Pac J Cancer
Prev. 16:1397–1401. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shan ZZ, Yan XB, Yan LL, Tian Y, Meng QC,
Qiu WW, Zhang Z and Jin ZM: Overexpression of Tbx3 is correlated
with epithelial-mesenchymal transition phenotype and predicts poor
prognosis of colorectal cancer. Am J Cancer Res. 5:344–353.
2015.PubMed/NCBI
|
|
15
|
Redmond KL, Crawford NT, Farmer H, D'Costa
ZC, O'Brien GJ, Buckley NE, Kennedy RD, Johnston PG, Harkin DP and
Mullan PB: T-box 2 represses NDRG1 through an EGR1-dependent
mechanism to drive the proliferation of breast cancer cells.
Oncogene. 29:3252–3262. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shen J, Lu J, Sui L, Wang D, Yin M,
Hoffmann I, Legler A and Pflugfelder GO: The orthologous Tbx
transcription factors Omb and TBX2 induce epithelial cell migration
and extrusion in vivo without involvement of matrix
metalloproteinases. Oncotarget. 5:11998–12015. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fischer K and Pflugfelder GO: Putative
breast cancer driver mutations in TBX3 cause impaired
transcriptional repression. Front Oncol. 5:2442015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Smith J, Mowla S and Prince S: Basal
transcription of the human TBX3 gene, a key developmental regulator
which is overexpressed in several cancers, requires functional NF-Y
and Sp1 sites. Gene. 486:41–46. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Capparelli C, Chiavarina B,
Whitaker-Menezes D, Pestell TG, Pestell RG, Hulit J, Andò S, Howell
A, Martinez-Outschoorn UE, Sotgia F, et al: CDK inhibitors
(p16/p19/p21) induce senescence and autophagy in cancer-associated
fibroblasts, ‘fueling’ tumor growth via paracrine interactions,
without an increase in neo-angiogenesis. Cell Cycle. 11:3599–3610.
2012. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li Y, Li B, Xu B, Han B, Xia H, Chen QM
and Li LJ: Expression of p53, p21(CIP1/WAF1) and eIF4E in the
adjacent tissues of oral squamous cell carcinoma: Establishing the
molecular boundary and a cancer progression model. Int J Oral Sci.
7:161–168. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Varelas X, Bouchie MP and Kukuruzinska MA:
Protein N-glycosylation in oral cancer: Dysregulated cellular
networks among DPAGT1, E-cadherin adhesion and canonical Wnt
signaling. Glycobiology. 24:579–591. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Li J, Weinberg MS, Zerbini L and Prince S:
The oncogenic TBX3 is a downstream target and mediator of the
TGF-β1 signaling pathway. Mol Biol Cell. 24:3569–3576. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Peters U, Jiao S, Schumacher FR, Hutter
CM, Aragaki AK, Baron JA, Berndt SI, Bézieau S, Brenner H,
Butterbach K, et al: Colon Cancer Family Registry and the Genetics
and Epidemiology of Colorectal Cancer Consortium: Identification of
genetic susceptibility loci for colorectal tumors in a Genome-Wide
meta-analysis. Gastroenterology. 144:799–807.e24. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Peres J, Davis E, Mowla S, Bennett DC, Li
JA, Wansleben S and Prince S: The highly homologous T-Box
transcription factors, TBX2 and TBX3, have distinct roles in the
oncogenic process. Genes Cancer. 1:272–282. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li J, Ballim D, Rodriguez M, Cui R, Goding
CR, Teng H and Prince S: The anti-proliferative function of the
TGF-β1 signaling pathway involves the repression of the oncogenic
TBX2 by its homologue TBX3. J Biol Chem. 289:35633–35643. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Walker AS, Johnson EK, Maykel JA,
Stojadinovic A, Nissan A, Brucher B, Champagne BJ and Steele SR:
Future directions for the early detection of colorectal cancer
recurrence. J Cancer. 5:272–280. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang HC, Meng QC, Shan ZZ, Yuan Z and
Huang XY: Overexpression of Tbx3 predicts poor prognosis of
patients with resectable pancreatic carcinoma. Asian Pac J Cancer
Prev. 16:1397–1401. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shan ZZ, Yan XB, Yan LL, Tian Y, Meng QC,
Qiu WW, Zhang Z and Jin ZM: Overexpression of Tbx3 is correlated
with Epithelial-Mesenchymal Transition phenotype and predicts poor
prognosis of colorectal cancer. Am J Cancer Res. 5:344–353.
2014.PubMed/NCBI
|