Introduction
Colorectal cancer is the fourth leading cause of
cancer-associated mortality worldwide (1). Immunotherapy has become a focus of
research in association with colorectal cancer, and adoptive cell
therapy (ACT) has been widely applied in a clinical setting as a
treatment option (2,3). Previous studies have suggested that ACT,
which involves dendritic cell (DC) vaccines, cytotoxic T
lymphocytes (CTLs), DC-CTLs and tumor infiltrating lymphocytes, and
chimeric antigen receptor T-cell immunotherapy are safe and
effective forms of immunotherapy in preclinical and clinical trials
(3–5).
However, the efficacy of these treatments remains subject to
certain limitations due to tumor immune escape mechanisms,
including the interaction between programmed cell death-1 (PD-1)
and programmed death-ligand 1 (PD-L1) (6).
PD-L1 is a cell-surface protein that is selectively
expressed in many tumor types (7).
Through interacting with its corresponding receptor (PD-1 expressed
on T cells), PD-L1 may suppress CTL-mediated responses against the
tumor. As this suppression is detrimental to the anti-tumor
response, blocking this interaction may help enhance cancer
immunotherapy. In previous clinical trials, the therapeutic effect
of inhibiting PD-1-mediated suppression has been improved by
intravenously administering anti-PD-1 or anti-PD-L1 agents
(8–12). However, immune checkpoint blockers may
cause side effects, including the development of severe
inflammation, which may become life threatening if not managed
appropriately (13–15). Additional side effects may be caused
by an upregulated immune response. Therefore, further research is
required to identify an appropriate way of applying anti-PD-L1
agents within a clinical setting.
In addition to tumor cells, PD-L1 is also highly
expressed on DCs (16–18). DCs are potent antigen-presenting cells
and critical for the activation of T cells (19). Suppression of DC functions in patients
with cancer is thought to contribute to the inhibition of the
protective immune response and enhanced disease progression
(20). At present, there are few
studies that have compared the expression level of PD-L1 in DCs
between healthy donors and patients with cancer. To the best of our
knowledge, it is unknown whether PD-L1 expression on DCs that have
been sensitized by tumor antigens will have an effect on T cell
activation. Additionally, the effect of administering anti-PD-L1 to
block the interaction between PD-1 and PD-L1 on DCs and activated T
cells also remains unclear. Currently, the focus of the majority of
ACT research is to enhance the anti-tumor effect of immune cells
(21). In the present study,
anti-PD-L1 was applied to cultures of DCs and during T cell
activation to investigate whether it improved DC function and
DC-mediated T cell activation.
Materials and methods
DC preparation and phenotype
detection
Density gradient centrifugation was used for the
preparation of peripheral blood mononuclear cells (PBMCs). Between
May and July 2016, a volume of 20 ml peripheral blood was obtained
from 8 healthy donors and 11 patients with colorectal cancer in the
Chinese PLA General Hospital (Beijing, China). There were 10 male
patients and 9 female patients. The mean age of the patients was 53
years (range, 37–68 years). All participants in the present study
provided written informed consent prior to their inclusion and the
study was approved by the Ethics Committee of the Chinese PLA
General Hospital. The samples were collected in a 50 ml centrifuge
tube containing heparin for anticoagulation. Following
centrifugation of the samples at 1,600 × g for 30 min at 25°C, the
serum was removed using a pipette. A 50 ml centrifuge tube was
filled with normal saline (NS) and a 50 ml centrifuge tube
containing 20 ml lymphocyte separation medium (Tianjin Haoyang
Biological Products Technology Co., Ltd., Tianjin, China) was also
prepared. The blood was mixed with the NS using a pipette and added
to the surface of the lymphocyte separation medium along the tube
wall. Following centrifugation of the samples at 1,000 × g for 30
min at 25°C, the supernatant was removed. The PBMCs were collected
from the corresponding layer and placed into another 50 ml
centrifuge tube. Following centrifugation of the sample at 500 × g
for 10 min at 25°C, the serum was removed and normal saline (NS)
was added. Following centrifugation again at 500 × g for 10 min at
25°C, the serum was removed and the PBMCs were obtained. A 1 ml
volume of serum-free Cellix901 medium (Tianjin Haoyang Biological
Products Technology Co., Ltd.) was added to the PBMCs and they were
incubated for 3 h at 37°C in 5% CO2. The cell suspension
was removed and the adherent cells were scraped off the tube wall.
The immature DCs (iDCs) from the peripheral blood were subsequently
obtained. A total of 1,000 U/ml granulocyte-macrophage colony
stimulating factor (GM-CSF) and interleukin (IL)-4 were added and
the PBMCs were incubated at 37°C in 5% CO2. GM-CSF and
IL-4 were added daily to maintain a concentration of 1,000 U/ml.
Following 8 days of culture the mature DCs (mDCs) were harvested.
The surface markers of the iDCs and mDCs were analyzed using flow
cytometry (according to the method in the subsequent flow cytometry
paragraph).
Applying anti-PD-L1 and the detection
of DC phenotypes and cytokine production
The DCs were cultured as described above. On day 6,
5 µg/ml anti-PD-L1 monoclonal antibodies (cat. no. MPDL3280A;
Genentech, San Francisco, CA, USA) were added to the test group and
the same amount of NS was added to the control group. The DCs were
harvested on day 8, and a flow cytometry was performed to detect
the expression of markers on DCs. Cytokines [IL-10, IL-12, tumor
necrosis factor (TNF)-α and interferon (IFN)-γ] in the supernatants
were detected using a cytometric bead array (CBA) (22).
CTL preparation and phenotype
detection
The DCs were cultured and anti-PD-L1 was applied
according to the aforementioned protocol. Isolated PBMCs were
obtained and added to the mDCs in Serum-free Celix601 medium. The
cells were incubated at 37°C in 5% CO2. The following
day, 1,000 U/ml anti-CD3 and 1,000 U/ml IL-2 were added to the
cells. Following 3 days of culture at 37°C, 1,000 U/ml IL-2 was
added every day and the CTLs were harvested following 14 days of
culture. The expression of extracellular markers was measured using
flow cytometry (according to the method in the subsequent flow
cytometry paragraph).
Cytotoxicity of CTLs
A lactate dehydrogenase (LDH) release assay (CytoTox
96® Non-Radioactive Cytotoxicity assay; Promega
Corporation, Madison, WI, USA) was performed to test the
cytotoxicity of the harvested CTLs in vitro. On day 14 of
culture, the CTLs were resuspended to maintain a concentration of
1×106 cells/ml. The colorectal cancer cell line SW620
was purchased from the American Tissue Culture Collection
(Manassas, VA, USA). It was collected during the logarithmic phase
for use as the target cells. At 5:1 and 10:1 effector-target
ratios, the CTL cytotoxicity was examined using an LDH release
assay. The following formula was used to calculate cytotoxicity:
Cytotoxicity=[A(Experimental)-A(Effector Spontaneous)-A(Target
Spontaneous)×100/[A(Target maximum)-A(Target spontaneous)]
(23).
Flow cytometry
The blocking reagent: 5% bovine serum albumin (BSA;
Tianjin Haoyang Biological Products Technology Co., Ltd.) was added
to the tube with a total of 1×105 cells in suspension
for 15 min at 25°C. After blocking, the cells were washed with the
washing reagent (0.5 ml PBS). Then, the corresponding antibodies
were added to a test tube for 15 min at 25°C. And 2 ml PBS with 5%
BSA was added. Following centrifugation at 400 × g for 5 min at
25°C, supernatant was removed. Then, 0.5 ml PBS was added to the
tube and all samples were examined using a FACSCalibur instrument
(BD Biosciences, San Jose, CA, USA), and the data were analyzed
using FlowJo 7.6.1 software (FlowJo LLC, Ashland, OR, USA). The
phenotypic profiles of iDCs and mDCs were analyzed via staining
1×105 cells for 15 min at 25°C with: Fluorescein
isothiocyanate (FITC)-conjugated anti-CD86 (cat no. 555657),
phycoerythrin (PE)-conjugated anti-CD80 (cat no. 340294),
PE-PerCP-conjugated anti-HLA-DR (cat no. 347364), allophycocyanin
(APC)-conjugated anti-CD83 (cat no. 551073), PE-conjugated
anti-PD-L1 (cat no. 557924) and PE-conjugated anti-CD11c (cat no.
340544), APC-conjugated anti-CD123 (cat no. 340545). The phenotypic
profiles of CTLs, helper T cells, and NK cells were analyzed via
staining 1×105 cells for 15 min at 25°C with:
FITC-conjugated anti-CD4 (cat no. 340298), PE-conjugated anti-CD8
(cat no. 340298), PE-PerCP-conjugated anti-CD3 (cat no. 340298),
and APC-conjugated anti-CD56 (cat no. 341025). The phenotypic
profiles of Tregs were analyzed via staining 1×105 cells
for 15 min at 25°C with: FITC-conjugated anti-CD4 (cat no. 340133),
PE-conjugated anti-CD127 (cat no. 557938), PE-PerCP-conjugated
anti-CD3 (cat no. 347344) and APC-conjugated anti-CD25 (cat no.
340939). All the antibodies were purchased from BD Biosciences and
employed according to the manufacturer's protocols.
Statistical analysis
Data are expressed as the mean ± standard deviation
from at least three independent experiments. Statistical analyses,
including a Chi-square test, Student's t-tests and a Fisher's exact
test were performed as appropriate. One-way analysis of variance
and a Newman-Keuls post hoc test were used to compare differences
among multiple groups. For all tests, P<0.05 was considered to
indicate a statistically significant difference. SPSS version 23.0
(IBM Corp., Armonk, NY, USA) and GraphPad Prism 5.0 (GraphPad
Software, Inc., La Jolla, CA, USA) was used for data analysis.
Results
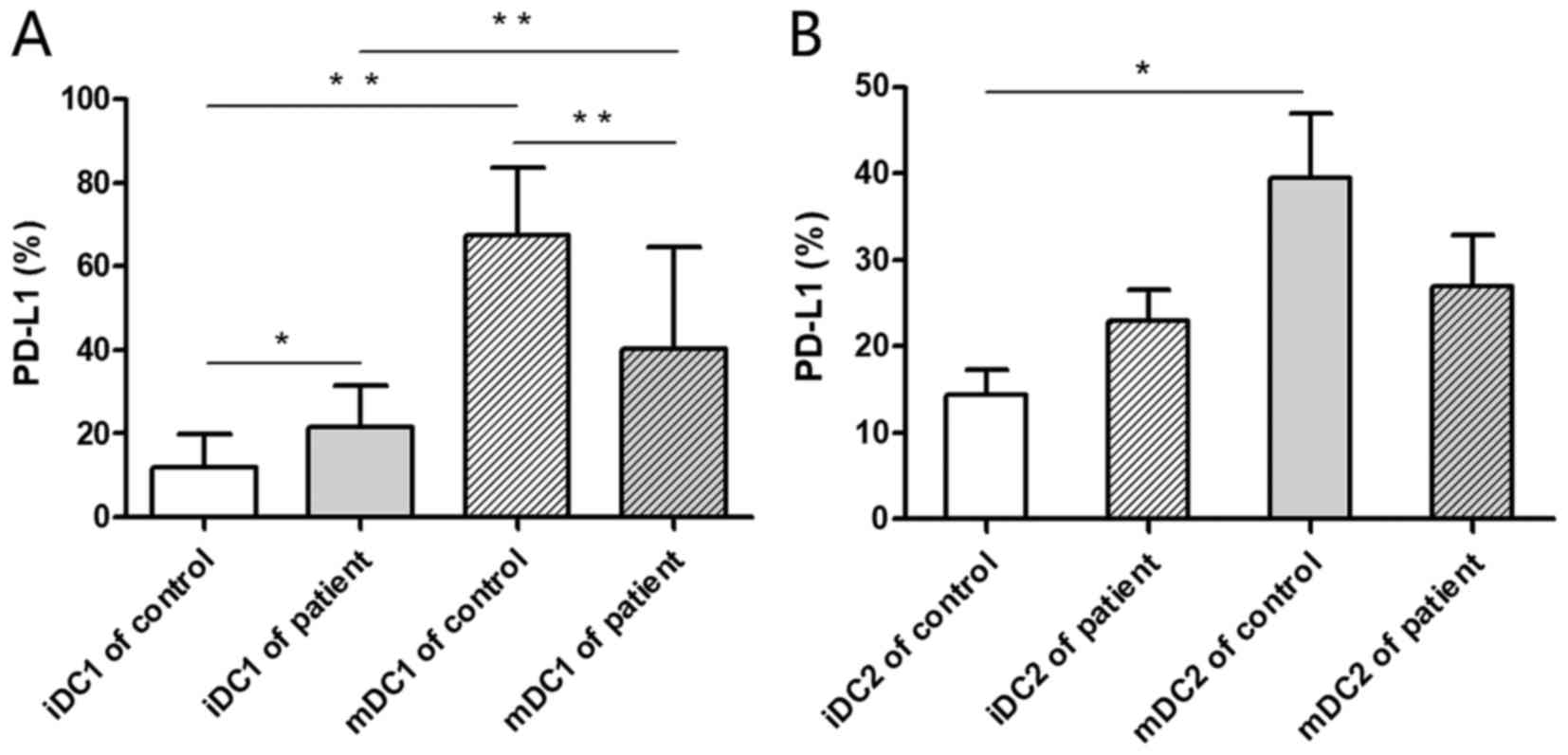
PD-L1 expression on DCs
Flow cytometry was performed for the detection of
PD-L1 expression on DC1 and DC2 subsets. The PD-L1 expression rate
on mDC1 cells was significantly higher compared with iDC1s in
healthy donors and patients with colorectal cancer (P<0.01;
Fig. 1A). This indicates that PD-L1
expression is upregulated during the formation and maturation of
DC1s. The PD-L1 expression rate on iDC1s was significantly higher
from the peripheral blood of patients with colorectal cancer
compared with healthy donors (P<0.05; Fig. 1A). This indicates that PD-L1
expression on iDC1 subsets may be significantly upregulated within
the tumor microenvironment. Additionally, the PD-L1 expression rate
of mDC2s was significantly higher compared with iDC2s in healthy
donors (P<0.05) while no significant difference was observed in
those derived from the patients with colorectal cancer (Fig. 1B).
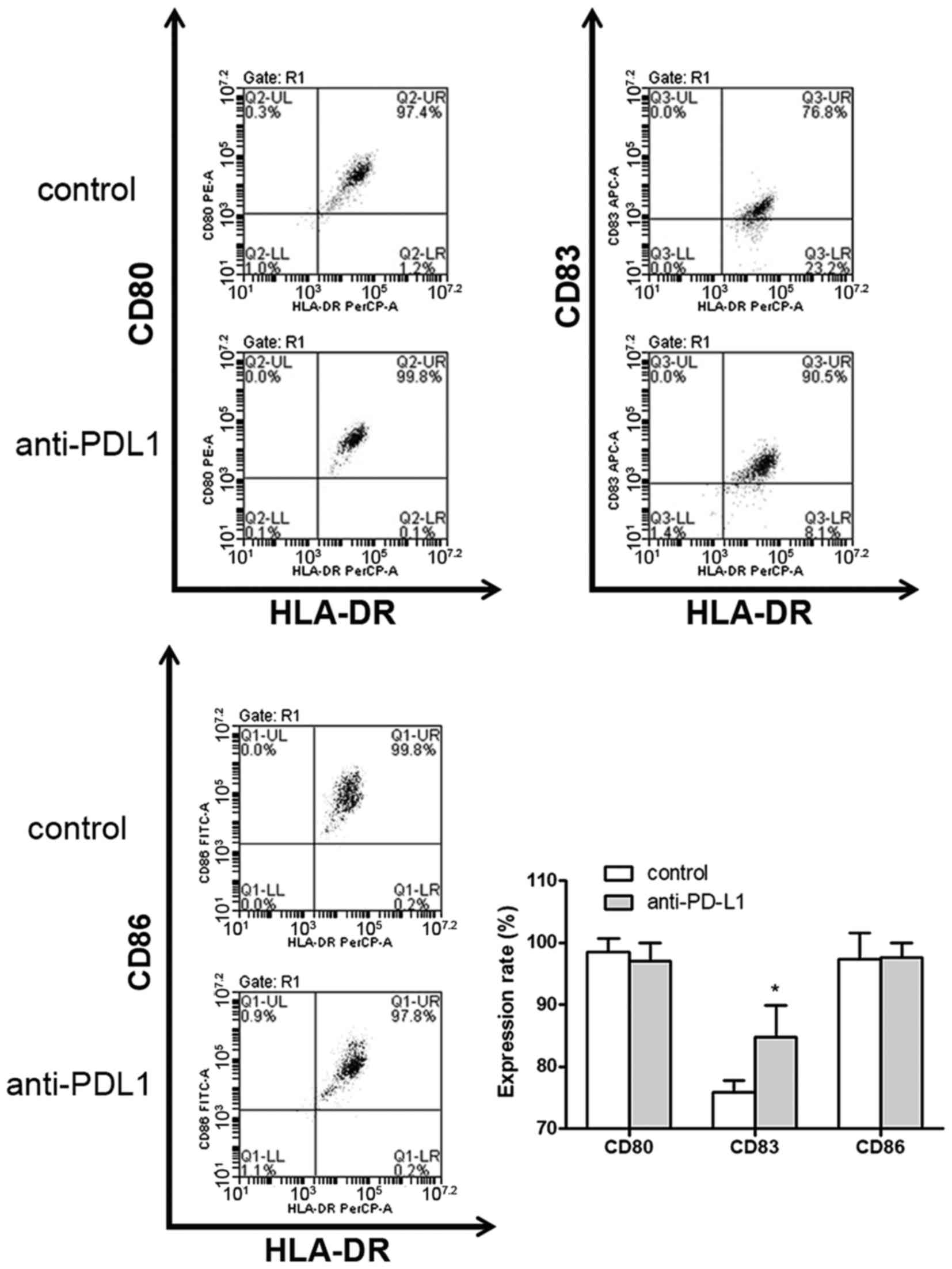
DC phenotype detection
Mature DC cell surface markers were detected by flow
cytometry (Fig. 2). In the anti-PD-L1
group DC surface markers, including CD80, CD83 and CD86 were
expressed at a frequency of 97.03±2.87, 84.80±5.12 and 97.57±2.46%,
respectively (data not shown). In the control group, the percentage
of CD80, CD83 and CD86 detected was 98.60±2.08, 75.83±1.94 and
97.30±4.33%, respectively (data not shown). CD83 expression on DCs
in the anti-PD-L1 group was significantly higher compared with the
control group (P<0.05; Fig. 2).
There was no statistically significant difference observed between
the two groups regarding the expression of CD80 and CD86 on
DCs.
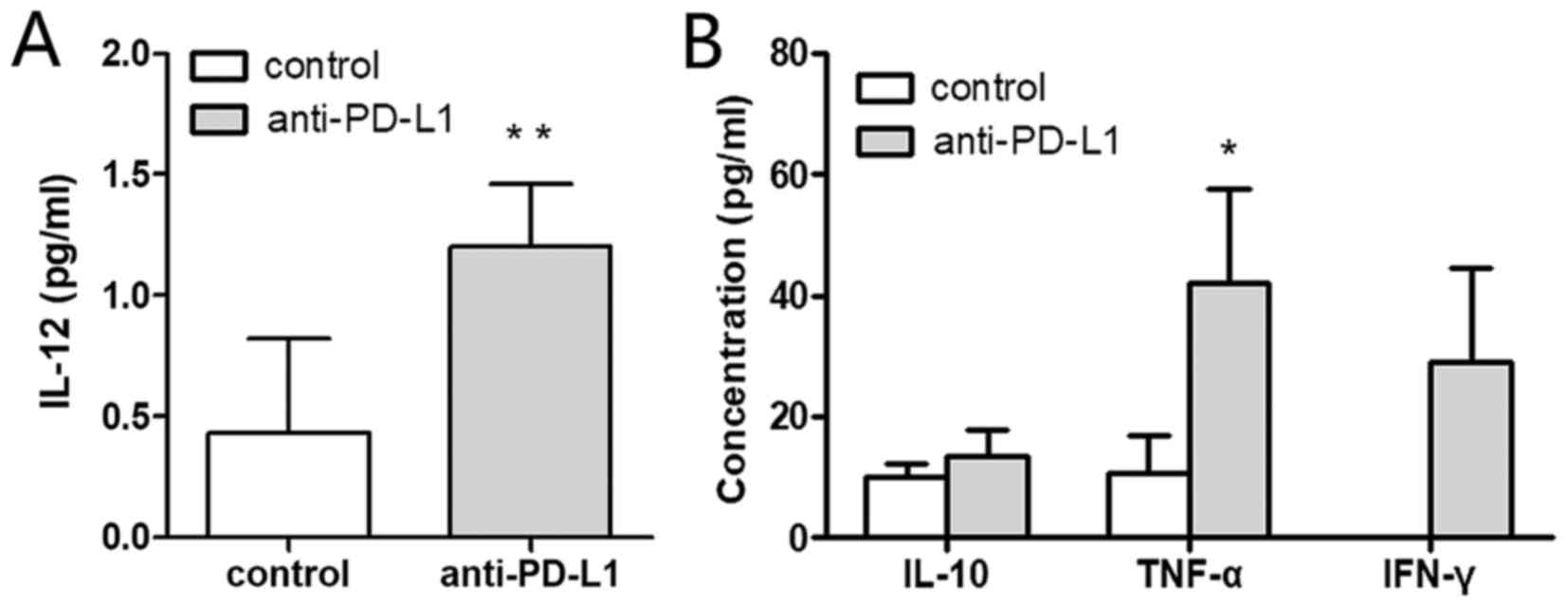
Cytokine assays
Cytokines within the supernatants were measured by
CBA. The IL-12 concentration was significantly higher in the
anti-PD-L1 group compared with the control group, 1.20±0.26 and
0.43±0.39 pg/ml, respectively (P<0.01; Fig. 3A). The level of TNF-α was also
significantly increased in the anti-PD-L1 group compared with the
control, 42.12±15.47 and 10.67±6.38 pg/ml, respectively (P<0.05;
Fig. 3B). The IFN-γ concentration in
the anti-PD-L1 group was 28.87±15.57 pg/ml, but it was undetectable
in the control group. IFN-γ was significantly higher in the
anti-PD-L1 group, compared with the control (P<0.05). The
concentration of IL-10 in the anti-PD-L1 and control groups was
13.52±4.19 and 9.92±2.47 pg/ml, respectively (P<0.05). However,
no statistically significant differences were observed regarding
the concentration of IL-10 secreted in each group.
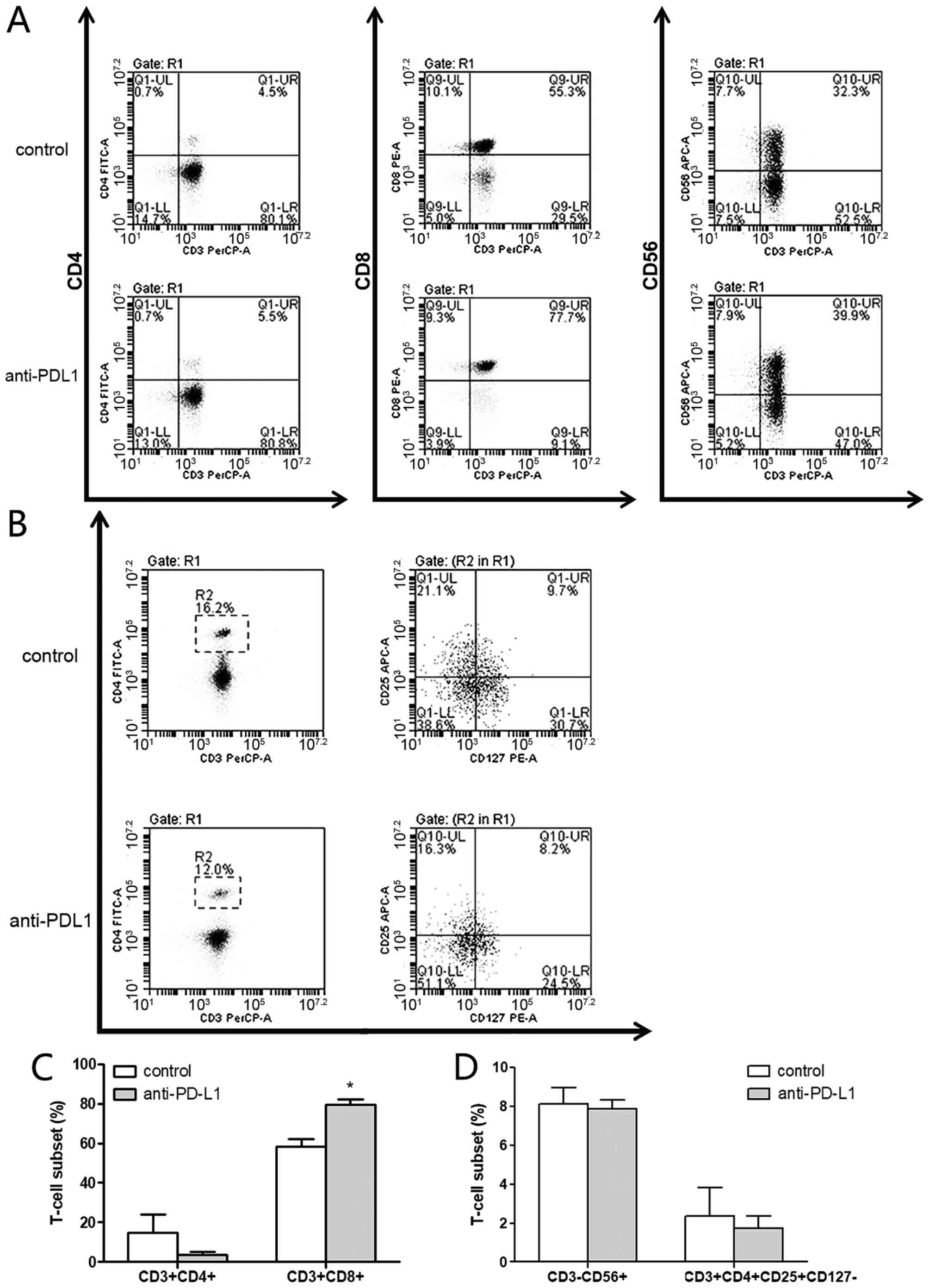
CTL phenotype detection
The CTL phenotype was measured by flow cytometry and
compared between the two groups (Fig. 4A
and B). In the anti-PD-L1 group, the percentage of helper T
cells (CD3+CD4+), cytotoxic T lymphocytes
(CD3+CD8+), NK cells
(CD3−CD56+) and regulatory T cells
(CD3+CD4+CD25+CD127−)
in the CTL cultures was 3.53±1.71, 79.57±2.81, 7.87±0.45 and
1.73±0.46%, respectively. In the control group the percentages were
14.97±9.07, 58.17±4.21, 8.13±0.84 and 2.37±1.46%, respectively.
These results indicated that there was a significantly higher
percentage of cytotoxic T lymphocytes
(CD3+CD8+) in the anti-PD-L1 group compared
with the control group (P<0.05; Fig.
4C). The percentage of helper T cells
(CD3+CD4+; Fig.
4C) was notably lower in the anti-PD-L1 group compared with the
control, however there were no significant differences, in
comparison of NK cells (CD3−CD56+; Fig. 4D) and regulatory T cells
(CD3+CD4+CD25+CD127−;
Fig. 4D) between the two groups.
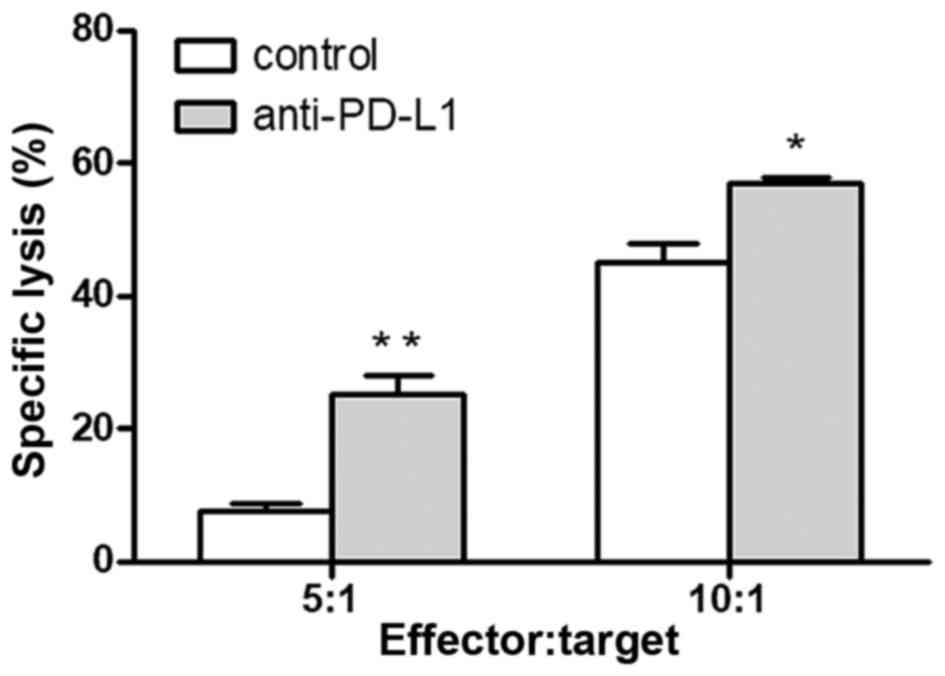
Cytotoxicity of CTLs
To confirm the anti-tumor effects of CTLs induced by
DCs treated with monoclonal antibodies against PD-L1, their
cytotoxicity was examined by an LDH release assay. In an in
vitro killing experiment at the 5:1 effector-target ratio, the
cytotoxicity in the anti-PD-L1 and control groups was 25.21±5.02
and 7.68±1.86%, respectively (P=0.005; Fig. 5). When the same experiment was
performed at the 10:1 effector-target ratio, the cytotoxicity in
the anti-PD-L1 and control groups was 56.88±1.82 and 44.96±5.23%
(P=0.02; Fig. 5). The CTLs induced by
DCs combined with anti-PD-L1 demonstrated a significantly higher
cytotoxicity towards the human colorectal cancer cell line SW620
in vitro compared with the CTLs without anti-PD-L1 in the
control group at each effector-target ratio. These results indicate
that PD-L1 expression on DCs restrains the DC function and
decreases CTL proliferation. Additionally, blocking the PD-1/PD-L1
interaction may rescue this impairment and improve the anti-tumor
effect of CTLs.
Discussion
PD-L1 is highly expressed on DCs and is one of the
immune checkpoints of the human immune system (24). The binding of PD-1 on the surface of
various immune cells, including T cells, induces an inhibitory
effect and regulates the immunological function of the human body
(25). Curiel et al (26) demonstrated that the expression rate of
PD-L1 on DCs may be significantly upregulated within the tumor
microenvironment. DCs have the ability to present antigens, as well
as suppress the immune response mediated by the interaction of
PD-L1 and PD-1 (25). Blocking the
PD-1/PD-L1 interaction may benefit certain patients with cancer
(10). However, it is unclear whether
using anti-PD-L1 combined with ACT will produce better curative
effects. Therefore, it is essential to improve the curative effect,
minimize side effects and seek an appropriate approach to using
anti-PD-L1 in the treatment of cancer within a clinical
setting.
DC subsets primarily consist of DC1
(HLA-DR+, CD11c+ and CD123−) and
DC2 subsets (HLA-DR+, CD11c− and
CD123+) (27). The DC1
subset serves a key role in anti-tumor cytotoxicity due to its
robust antigen-presentation capacity and T cell activating
abilities (28). In the present
study, the PD-L1 expression rate on mDC1s was higher than that
expressed on iDC1s in healthy donors and patients with colorectal
cancer. This indicates that the PD-L1 expression rate on the DC1
subset increases with DC maturation. Since the high expression of
PD-L1 in DC1 subsets will have negative effects on immune response,
applying anti-PD-L1 during the activation and differentiation of T
cells may reduce the negative suppressive effects of the DC1
subsets. Additionally, the PD-L1 expression rate of iDC1s in
patients with colorectal cancer was higher than that of healthy
donors, and the patients with colorectal cancer exhibited a lower
PD-L1 expression rate on mDC1s compared with the healthy donors.
These results indicate that there was no corresponding increase in
PD-L1 expression associated with DC maturation in colorectal cancer
patients. These findings may explain the poor functionality of DCs
in patients undergoing ACT, however further study is required to
confirm this suggestion.
DC cell-surface markers were also measured in the
present study. The DC maturation marker, CD83, co-stimulatory
molecules CD80 and CD86, and major histocompatibility complex (MHC)
class II molecule, HLA-DR were compared between the PD-L1 and
control groups. The expression level of these markers reflects the
degree of maturity and functional status of the DCs (29). In the present study, no statistically
significant differences were observed between the two groups for
the comparison of CD80, CD86 and MHC. However, the CD83 expression
rate in the anti-PD-L1 group was significantly higher compared with
the control group. A high expression level of CD83 suggests that
treatment with monoclonal antibodies against PD-L1 promotes DC
maturation and enhances its associated functionality.
IL-12 produced by DCs, B cells and macrophages is
one of the most potent type 1 T helper cytokines and may promote
the activation of CTL and NK cells (30). IL-12 has also been used as a cytokine
for improving DC-based immunotherapy (31). In the present study, cytokine
detection by CBA revealed that the concentration of IL-12 was
significantly higher in the anti-PD-L1 group. An increased
secretion of IL-12 by DCs may translate into enhanced anti-tumor
immunity (31). However, the
concentration of IL-10, which may impair the potent APC function of
DCs and produce negative effects on immunity (32), was not significantly different between
the two groups in the present study. This suggests that there is no
association between the administration of anti-PD-L1 and IL-10
secretion by DCs. TNF-α was reported to be able to induce the
necrosis and apoptosis of tumor cells directly (33,34). In
the present study, following treatment with anti-PD-L1 the
secretion of TNF-α was significantly increased compared with the
control. According to previous adoptive T-cell transfer studies,
IFN-γ was reported to be crucial for efficient tumor rejection by
the upregulation of MHC class I and Fas levels on tumor cells
(35). In the present study it was
revealed that only a small amount of IFN-γ was secreted when
anti-PD-L1 was added while the DCs were maturing, whereas IFN-γ
secretion in the control group was undetectable. As the increased
secretion of TNF-α and IFN-γ may enhance anti-tumor effects,
applying anti-PD-L1 to maturing DCs may produce DC vaccines with a
higher immune activating potential.
CTLs are regarded as ideal cells for immunotherapy,
as they possess strong tumor specificity and exhibit stable
antitumor effects in clinical trials (36). At present, the improvement of
DC-mediated activation and proliferation of CTLs is a challenge for
ACT. According to the results of the present study, applying
anti-PD-L1 during the induction and activation of T cells may
produce a higher percentage of CTLs (CD3+,
CD8+). One possible reason for this observation may be
the improved function of the DC1 subset. As PD-L1 was highly
expressed on the DC1 subset following the application of
anti-PD-L1, the function of the DC1 subset was enhanced.
Furthermore, as described above the DC1 subset was demonstrated to
serve a leading role in antigen presentation and CTL induction.
Therefore, the application of anti-PD-L1 may effectively increase
the percentage of CTLs. As key players in driving immune
suppression, regulatory T cells (Tregs) may inhibit anti-tumor
immunity within the tumor microenvironment. In the present study,
although the percentage of Tregs was lower in the anti-PD-L1 group,
there was no significant difference between the two groups. Further
studies are required to examine whether applying anti-PD-L1 is
associated with a lower percentage of Tregs. Additionally, the CTL
cytotoxicity against the human colorectal cancer cell line SW620
was examined in the present study using an LDH release assay. At
5:1 and 10:1 effector-target ratios the cytotoxicity of the
anti-PD-L1 group was significantly higher compared with the control
group. The authors hypothesize that the increase in CTLs was the
primary reason for the improved cytotoxicity, however cytokine
changes in IL-12, TNF-α and IFN-γ may also contribute to the
observed enhanced anti-tumor effect.
In summary, treatment with anti-PD-L1 may promote
the maturation of DCs and enhance the functionality of the DC1
subtype. It may also improve the ability of CTL activation and
produce CTL cells with more potent anti-tumor activity. As applying
anti-PD-L1 may also enhance DC vaccines and DC-based immunotherapy,
the creation of DC vaccines in conjunction with anti-PD-L1 may be a
future effective treatment strategy for patients with colorectal
cancer.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Brenner H, Kloor M and Pox CP: Colorectal
cancer. Lancet. 383:1490–1502. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Makkouk A and Weiner GJ: Cancer
immunotherapy and breaking immune tolerance: New approaches to an
old challenge. Cancer Res. 75:5–10. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chia WK, Teo M, Wang WW, Lee B, Ang SF,
Tai WM, Chee CL, Ng J, Kan R, Lim WT, et al: Adoptive T-cell
transfer and chemotherapy in the first-line treatment of metastatic
and/or locally recurrent nasopharyngeal carcinoma. Mol Ther.
22:132–139. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jin CG, Chen XQ, Li J, Wu ZP, Liu X and
Wang XC: Moderating effects and maintenance of lung cancer cellular
immune functions by CIK cell therapy. Asian Pac J Cancer Prev.
14:3587–3592. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mesiano G, Todorovic M, Gammaitoni L,
Leuci V, Giraudo Diego L, Carnevale-Schianca F, Fagioli F,
Piacibello W, Aglietta M and Sangiolo D: Cytokine-induced killer
(CIK) cells as feasible and effective adoptive immunotherapy for
the treatment of solid tumors. Expert Opin Biol Ther. 12:673–684.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kelly RJ: Immunotherapy for esophageal and
gastric cancer. Am Soc Clin Oncol Educ Book. 37:292–300. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zou WP and Chen LP: Inhibitory B7-family
molecules in the tumour microenvironment. Nat Rev Immunol.
8:467–477. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brahmer JR, Drake CG, Wollner I, Powderly
JD, Picus J, Sharfman WH, Stankevich E, Pons A, Salay TM, McMiller
TL, et al: Phase I study of single-agent anti-programmed death-1
(MDX-1106) in refractory solid tumors: Safety, clinical activity,
pharmacodynamics, and immunologic correlates. J Clin Oncol.
28:3167–3175. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chung HC, Arkenau HT, Wyrwicz L, Oh DY,
Lee KW, Infante JR, Chin KM, von Heydebreck A, Kang YK and Safran
H: Safety, PD-L1 expression, and clinical activity of avelumab
(MSB0010718C), an anti-PD-L1 antibody, in patients with advanced
gastric or gastroesophageal junction cancer. J Clin Oncol. 34 4
suppl:S1672016. View Article : Google Scholar
|
|
10
|
Hamid O, Robert C, Daud A, Hodi FS, Hwu
WJ, Kefford R, Wolchok JD, Hersey P, Joseph RW, Weber JS, et al:
Safety and tumor responses with lambrolizumab (anti-PD-1) in
melanoma. N Engl J Med. 369:134–144. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Topalian SL, Sznol M, McDermott DF, Kluger
HM, Carvajal RD, Sharfman WH, Brahmer JR, Lawrence DP, Atkins MB,
Powderly JD, et al: Survival, durable tumor remission, and
long-term safety in patients with advanced melanoma receiving
nivolumab. J Clin Oncol. 32:1020–1030. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wolchok JD, Kluger H, Callahan MK, Postow
MA, Rizvi NA, Lesokhin AM, Segal NH, Ariyan CE, Gordon RA, Reed K,
et al: Nivolumab plus ipilimumab in advanced melanoma. N Engl J
Med. 369:122–133. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hofmann L, Forschner A, Loquai C,
Goldinger SM, Zimmer L, Ugurel S, Schmidgen MI, Gutzmer R, Utikal
JS, Göppner D, et al: Cutaneous, gastrointestinal, hepatic,
endocrine, and renal side-effects of anti-PD-1 therapy. Eur J
Cancer. 60:190–209. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Helissey C, Vicier C and Champiat S: The
development of immunotherapy in older adults: New treatments, new
toxicities? J Geriatr Oncol. 7:325–333. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cousin S and Italiano A: Molecular
pathways: Immune checkpoint antibodies and their toxicities. Clin
Cancer Res. 22:4550–4555. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Selenko-Gebauer N, Majdic O, Szekeres A,
Höfler G, Guthann E, Korthäuer U, Zlabinger G, Steinberger P, Pickl
WF, Stockinger H, et al: B7-H1 (programmed death-1 ligand) on
dendritic cells is involved in the induction and maintenance of T
cell anergy. J Immunol. 170:3637–3644. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Atefi M, Avramis E, Lassen A, Wong DJ,
Robert L, Foulad D, Cerniglia M, Titz B, Chodon T, Graeber TG, et
al: Effects of MAPK and PI3K pathways on PD-L1 expression in
melanoma. Clin Cancer Res. 20:3446–3457. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Okazaki T and Honjo T: PD-1 and PD-1
ligands: From discovery to clinical application. Int Immunol.
19:813–824. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Palucka K and Banchereau J: Cancer
immunotherapy via dendritic cells. Nat Rev Cancer. 12:265–277.
2012. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hargadon KM: Strategies to improve the
efficacy of dendritic cell-based immunotherapy for melanoma. Front
Immunol. 8:15942017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tähtinen S, Grönberg-Vähä-Koskela S, Lumen
D, Merisalo-Soikkeli M, Siurala M, Airaksinen AJ, Vähä-Koskela M
and Hemminki A: Adenovirus improves the efficacy of adoptive T-cell
therapy by recruiting immune cells to and promoting their activity
at the tumor. Cancer Immunol Res. 3:915–925. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Cavalcanti A, Santos R, Mesquita Z, Duarte
AL and Lucena-Silva N: Cytokine profile in childhood-onset systemic
lupus erythematosus: A cross-sectional and longitudinal study. Braz
J Med Biol Res. 50:e57382017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yan Y, Li S, Jia T, Du X, Xu Y, Zhao Y, Li
L, Liang K, Liang W, Sun H and Li R: Combined therapy with CTL
cells and oncolytic adenovirus expressing IL-15-induced enhanced
antitumor activity. Tumour Biol. 36:4535–4543. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ray A, Das DS, Song Y, Richardson P,
Munshi NC, Chauhan D and Anderson KC: Targeting PD1-PDL1 immune
checkpoint in plasmacytoid dendritic cell interactions with T
cells, natural killer cells and multiple myeloma cells. Leukemia.
29:1441–1444. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Yang J, Riella LV, Chock S, Liu T, Zhao X,
Yuan X, Paterson AM, Watanabe T, Vanguri V, Yagita H, et al: The
novel costimulatory programmed death ligand 1/B7.1 pathway is
functional in inhibiting alloimmune responses in vivo. J Immunol.
187:1113–1119. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Curiel TJ, Wei S, Dong HD, Alvarez X,
Cheng P, Mottram P, Krzysiek R, Knutson KL, Daniel B, Zimmermann
MC, et al: Blockade of B7-H1 improves myeloid dendritic
cell-mediated antitumor immunity. Nat Med. 9:562–567. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ueno H, Schmitt N, Klechevsky E,
Pedroza-Gonzalez A, Matsui T, Zurawski G, Oh S, Fay J, Pascual V,
Banchereau J and Palucka K: Harnessing human dendritic cell subsets
for medicine. Immunol Rev. 234:199–212. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Volovitz I, Melzer S, Amar S, Bocsi J,
Bloch M, Efroni S, Ram Z and Tárnok A: Dendritic cells in the
context of human tumors: Biology and experimental tools. Int Rev
Immunol. 35:116–135. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
MacDonald KP, Munster DJ, Clark GJ,
Dzionek A, Schmitz J and Hart DN: Characterization of human blood
dendritic cell subsets. Blood. 100:4512–4520. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Trinchieri G: Interleukin-12 and the
regulation of innate resistance and adaptive immunity. Nat Rev
Immunol. 3:133–146. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Vogt A, Sievers E, Lukacs-Kornek V, Decker
G, Raskopf E, Meumann N, Büning H, Sauerbruch T, Strassburg CP,
Schmidt-Wolf IG and Gonzalez-Carmona MA: Improving immunotherapy of
hepatocellular carcinoma (HCC) using dendritic cells (DC)
engineered to express IL-12 in vivo. Liver Int. 34:447–461. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Legitimo A, Consolini R, Failli A, Orsini
G and Spisni R: Dendritic cell defects in the colorectal cancer.
Hum Vacc Immunother. 10:3224–3235. 2014. View Article : Google Scholar
|
|
33
|
Huang J, Tatsumi T, Pizzoferrato E,
Vujanovic N and Storkus WJ: Nitric oxide sensitizes tumor cells to
dendritic cell-mediated apoptosis, uptake, and cross-presentation.
Cancer Res. 65:8461–8470. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Liu S, Yu Y, Zhang M, Wang W and Cao X:
The involvement of TNF-alpha-related apoptosis-inducing ligand in
the enhanced cytotoxicity of IFN-beta-stimulated human dendritic
cells to tumor cells. J Immunol. 166:5407–5415. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Blankenstein T: The role of tumor stroma
in the interaction between tumor and immune system. Curr Opin
Immunol. 17:180–186. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Butler MO, Lee JS, Ansén S, Neuberg D,
Hodi FS, Murray AP, Drury L, Berezovskaya A, Mulligan RC, Nadler LM
and Hirano N: Long-lived antitumor CD8+ lymphocytes for adoptive
therapy generated using an artificial antigen-presenting cell. Clin
Cancer Res. 13:1857–1867. 2007. View Article : Google Scholar : PubMed/NCBI
|