Introduction
Extranodal NK/T-cell lymphoma (NKTL) is a highly
aggressive neoplasm that commonly involves the nasal cavity, which
accounts for 1–10% of all non-Hodgkin's lymphoma (1). The estimated 5-year overall survival
rate is 40–50% (2). This type of
tumor has distinct clinicopathological features and no standard
treatment options. In the early stages, the disease often presents
as a destructive lesion within the centrofacial region. However, in
advanced cases, the disease may involve distant extranodal organs,
frequently including the skin, liver, lung, testis or central
nervous system (1,3). Penile involvement, whether primary or
secondary, is extremely rare and seldom reported in the literature
(4,5).
Early diagnosis of lymphoma can aid in avoidance unnecessary penile
amputation and allow for optimal management (6). The first English-language case report of
extranodal NKTL with involvement of the penis was reported in 2008,
and is the only study in English to describe this entity (7).
The present study reports the comprehensive clinical
data of one case of extranodal NKTL with recurrence in the penis,
and reviews the previously reported cases of non-B-cell penile
lymphoma. Written informed consent for the publication of this
report was obtained from the patient.
Case report
Ethical approval was obtained from the Scientific
Research and Clinical Trial Ethics Committee of The First
Affiliated Hospital of Zhengzhou University (Zhengzhou, China) and
written informed consent was obtained from the patient. A
39-year-old Chinese male presented to The First Affiliated Hospital
of Zhengzhou University (Zhengzhou, China) in February 2013
complaining of nasal congestion and purulent rhinorrhea that had
lasted for 6 months. Upon physical examination, a mass was observed
in the right nasal cavity, and an enlarged palpable lymph node was
detected in the ipsilateral neck. A subsequent nasopharyngeal
computed tomography (CT) scan revealed a right nasal tumor.
Subsequently, an incisional biopsy of the right mass was performed.
Tissue was fixed in 10% buffered formalin for 6 h at 37°C,
dehydrated, embedded in paraffin and cut into 4-µm-thick sections.
The sections were blocked in 3% hydrogen peroxide for 4 min at 37°C
before incubation with antibodies. The primary antibodies used were
CD56 (cat no. 56C04; Thermo Fisher Scientific, Inc., Waltham, MA,
USA) in 1:200 dilution, CD3 (cat no. Kit-0003; MXB Biotechnologies,
Inc., Fuzhou, China) in undiluted solution, granzyme B (cat no.
ZA-0149; OriGene Technologies, Inc., Beijing, China) in undiluted
solution, T-cell-restricted intracellular antigen-1 (TIA-1; cat no.
MAB-0576; MXB Biotechnologies, Inc.) in undiluted solution, CD43
(cat no. MAB-0032; MXB Biotechnologies, Inc.) in undiluted
solution, CD20 (cat no. ZM-0039; OriGene Technologies, Inc.) in
1:200 dilution and Ki-67 (cat no. Kit-0005; MXB Biotechnologies,
Inc.) in undiluted solution. The section specimens were incubated
with primary antibodies against CD56, CD3, TIA-1, CD43, CD20 or
Ki67 for 36, 72, 64, 36, 36 or 64 min at 37°C respectively, then
incubated with ultraView Universal DAB Detection kit (cat no.
760-500; Roche Diagnostics, Shanghai, China) that included
anti-mouse and -rabbit secondary antibodies conjugated with
horseradish peroxidase and DAB in undiluted solutions at 37°C for
16 min. Images were taken with a Leica DM4 B microscope (×400
magnification; Leica Microsystems GmbH, Wetzlar, Germany). The
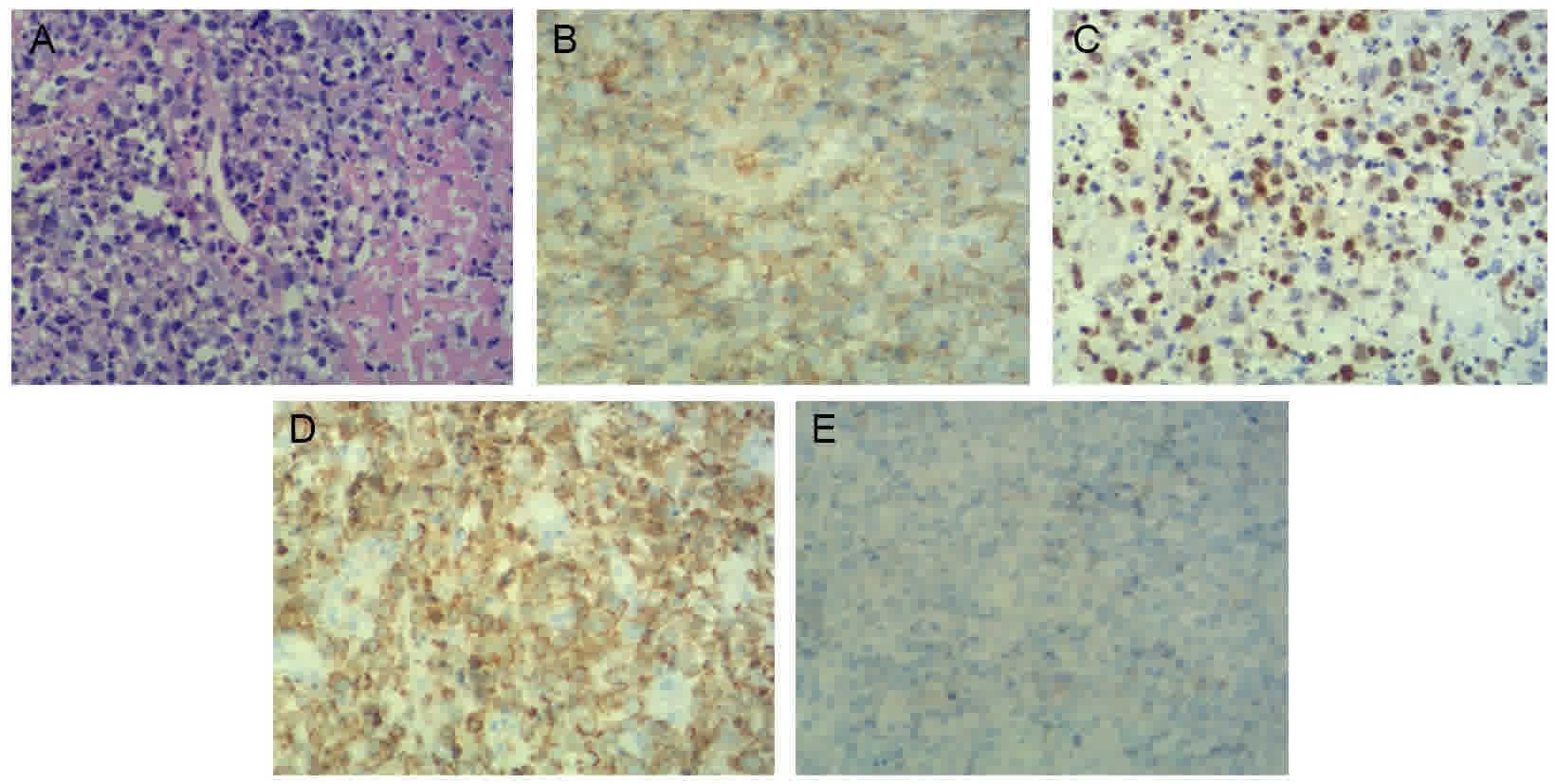
biopsy revealed atypical lymphocytes that were positive for CD56,
CD3, granzyme B, TIA-1and CD43, and negative for CD20. Positive
Ki-67 antigen staining, representing the proliferative activity,
was identified in 70% of the cells. A routine ultrasound scan
showed an enlarged lymph node, measuring 16×6 mm, in the right
neck. Abdominal and pelvic ultrasound examinations were negative,
and bone marrow smear and blood tests were unremarkable. These
findings led to a diagnosis of NKTL stage IIE (involvement of nasal
cavity and ipsilateral lymph nodes) according to the Ann Arbor
classification (8), and the
International Prognostic Index (IPI) (9) score was 1.
The patient received radiotherapy by radioisotope
60Co (200 cGy, 25 times; total, 5,000 cGy) followed by
seven cycles of chemotherapy, consisting of cyclophosphamide (750
mg/m2; day 1), doxorubicin (25 mg/m2; days 1
and 2) and vincristine (2 mg; day 1), with fotemustine (100
mg/m2; day 3) for the first 5 cycles. Each cycle lasted
21 days. A complete remission was achieved, and the patient was
disease-free for 16 months.
Subsequently, the patient presented with a painless
indurated mass in the glans penis that had been present for 1 week.
No fever, weight loss or night sweats were reported. The patient
denied having had unprotected sexual intercourse, previous sexually
transmitted diseases or recent trauma. The physical examination
revealed a firm mass affecting the glans penis, without ulceration
or swelling, and multiple enlarged palpable lymph nodes in the
bilateral inguinal regions. The results of a blood test and
biochemical analyses, including an analysis of Epstein-Barr virus
(EBV) DNA copies, were in the normal ranges. Enhanced CT showed a
soft tissue mass with obscure boundaries and moderate enhancement
on the arterial phase, and enlarged inguinal lymph nodes with
ring-like enhancement (Fig. 1). An
incisional biopsy of the penis was performed as described
previously, which led to a diagnosis of penile metastasis secondary
to NKTL. Immunohistochemical staining revealed that the biopsy
tissue was positive for CD3, CD56, CD43, TIA-1, granzyme B and
CD-30 (cat no. ZM-0043; OriGene Technologies, Inc.; Fig. 2). Additionally, in situ
hybridization analysis revealed positive expression of EBV-encoded
RNA (EBER; cat no. ISH-5021; OriGene Technologies, Inc.), the CD20
(Fig. 2) andanaplastic lymphoma
kinase staining results were negative, and staining for Ki-67 was
positive in 90% of cells. Enhanced CT scans of the nasopharynx,
chest and abdomen, an ultrasound scan of the superficial lymph
node-bearing region, and bone marrow aspiration were performed, and
no other lesions were detected. A diagnosis of recurrent extranodal
NKTL was determined. The patient's clinical stage was IIE, and the
IPI score was 1.
The patient then received three cycles of DDGP
chemotherapy, consisting of cisplatin (20 mg/m2; days
1–4), dexamethasone (15 mg/m2; days 1–5), gemcitabine
(0.8 g/m2; days 1 and 8) and pegaspargase (2,500
IU/m2; day 1). The penile mass decreased in size
following the first cycle and a partial remission was achieved.
After two cycles of chemotherapy, the mass in the glans penis and
the inguinal lymph nodes had regressed (Fig. 1). Following a further cycle of
chemotherapy, the patient remained in a stable condition. Follow-up
with the patient was not possible as contact was lost following the
last chemotherapy treatment.
Discussion
Extranodal NKTL, nasal type is a type of lymphoma
that associated with EBV, and is more commonly observed in Asian
populations than in people of European descent (1,3). This type
of tumor has distinct clinicopathological features and no standard
treatment options. In the early stages, the disease often presents
as a destructive lesion within the centrofacial region. However, in
advanced cases, the disease may involve distant extranodal organs,
frequently the skin, liver, lung, testis, or CNS (1,3). The
present study reports a rare case of primary nasal extranodal NKTL
with metastasis to the penis. In this patient, the tissue biopsy
obtained from the penile mass exhibited atypical lymph cells
infiltrating and damaging blood vessels, with considerable
necrosis, and cells positive for CD56, EBER, granzyme B and TIA-1,
and negative for CD20. The morphological characteristics and
immunohistochemical findings of these cells were similar to those
of primary nasal extranodal NKTL, and were thus consistent with a
diagnosis of penile metastasis from nasal extranodal NKTL.
Penile malignancy is extremely rare, despite the
rich blood supply to this region, with a reported incidence ranging
from 0.58 to 1.3 cases/100,000 individuals (4,5). Squamous
cell carcinoma is the most common histological type (91.7%)
(4,5).
Involvement of the penis by lymphoma is an even more rare
occurrence. Diffuse large B-cell lymphoma is the most common
histological subtype among cases of penile lymphoma (10). Sun et al (10) reported 33 cases of penile lymphoma,
only 9 of which had originated from T-cells. In the current study,
a search of PubMed with the terms ‘lymphoma’ combined with ‘penis’
or ‘penile’ identified only 12 cases of non-B-cell penile lymphoma
that have been reported since 1995, of which two cases were
ultimately diagnosed as NKTL. Four of these reports were in
published in Chinese. The clinical characteristics of these cases
are summarized in Table I (6,7,11–20).
 | Table I.Summary of reports of non-B-cell
lymphoma cases involving the penis published since 1995. |
Table I.
Summary of reports of non-B-cell
lymphoma cases involving the penis published since 1995.
| Authors, year | Patient age
(years) | Presentation | TPD/TPR | Lymphadenopathy | Pathology | Treatment | Follow-up | Outcome | (Refs.) |
|---|
| Present
casea | 39 | Mass | 1 month/16
months | Yes | NK/T | Chemotherapy | 2 months | PR | – |
| Lan et al,
2008a | 48 | Mass | NR/5 years | NR | NK/T | Chemotherapy | NR | CR | (7) |
| Yao et al,
2006 | 46 | Nodule, ulcer | 18 months (TPD) | Yes | NK/T | Surgery,
chemotherapy | 1 year | NR | (11) |
| Lin et al,
1999 | 76 | Ulcer | 6 months (TPD) | No | LCEL
(CD30+) | CO2 laser
excision | 18 months | CR | (6) |
| Terada et al,
2012 | 55 | Mass | NR | No | CTCL | Chemotherapy and
SCT | NR | NR | (12) |
| Li et al,
2011 | 76 | Swelling, mass,
ulcer | 2 months (TPD) | No | TCEL | Surgery, chemotherapy
and RT | 10 months | DOD | (13) |
| Zhou et al,
2008a | 49 | Erythema, ulcer,
swelling | 2 months/10
years | No | CTCL | Surgery | 2 months | DOD | (14) |
| Shi et al,
2008 | 65 | Enlargement of the
penis, ulcer | NR | Yes | PTCL | Chemotherapy | NR | NR | (15) |
| Wang et al,
2003 | 70 | Mass | 6 months (TPD) | No | TCEL | Chemotherapy | 20 months | CR | (16) |
| Tomb et al,
2003a | 29 | Ulcer | 2 weeks/2
years | No | TCEL
(CD30+) | Chemotherapy | 4 years | CR | (17) |
| Thorns et
al, 2003 | 59 | Dysuria, oliguria,
ulcer, phimosis | NR | No | CTCL | Circumcision | NR | NR | (18) |
| Pomara et
al, 2003 | 67 | Ulcerative
swelling | NR | Yes | T-rich B | Chemotherapy | 19 months | CR | (19) |
| Allen and Walsh,
1996 | 77 | Ulcer | NR | No | TCEL | Chemotherapy,
RT | 14 months | Died | (20) |
The ages of the 13 patients (including the patient
in the present case report) ranged from 29 to 77 years (median, 59
years). Of the 13 cases, 3 were extranodal NKTL, with 2 of these
cases being metastatic tumors. In these 2 cases of metastatic NKTL,
the time intervals between primary malignancy and recurrent penile
lymphoma were 16 months and 5 years (7), and the primary lymphomas were located in
nasal cavity in both cases. Following systemic chemotherapy,
remissions were achieved in these 2 cases. While the majority of
non-B-cell penile lymphoma cases respond to chemotherapy, 2 of the
13 patients reportedly succumbed to the disease.
The clinical presentations of penile lymphomas are
often non-specific and subtle, and include nodules (11), masses (7,12,13,16),
ulceration (6,11,13–15,17–20)
and diffuse penile swelling (13,14,19); more
rare symptoms include dysuria and phimosis (18). Among the reviewed cases, 69% (9/13
cases) exhibited ulceration during the course of the disease, which
may be a sign that indicates a possible diagnosis of penile
lymphoma. Lymph node involvement was reported in 31% of cases (4/13
patients).
The diagnosis of metastatic penile NKTL can be
challenging, and the time between presentation and a final
diagnosis can be as long as 18 months (11). A major differential diagnostic
challenge is the distinction between this entity and non-malignant
necrosis; necrosis is common in diagnostic biopsies, and may
significantly delay diagnosis. Biopsies must include the edges of
lesions in order to increase the chance of having viable tissue.
The differential diagnosis also includes vasculitis, trauma, and
sexually transmitted diseases (11,21).
Therefore, a full personal history, physical examination and an
incisional biopsy are essential to determine the correct diagnosis.
Systemic radiological investigation, including CT, magnetic
resonance imaging or positron emission tomography scans, as well as
bone marrow aspiration or biopsy, should be undertaken.
Since metastases of nasal extranodal NKTL to the
penis are rare, optimal treatment is not well established. Previous
cases of lymphoma of the penis have been treated with chemotherapy
(7,15–17,19),
chemotherapy combined with radiotherapy (20), surgery (14,18) or a
combination of these treatment modalities (6,11–13). Chemotherapy with or without
radiotherapy is the optimal initial treatment to eradicate this
type of tumor while preserving the physiology and function of the
penis. Surgery should be reserved only for failures (17–20). In
the present case, we opted to treat the patient aggressively with
chemotherapy for the disseminated lesions. Furthermore, considering
the patient's age, surgery or radiotherapy were not recommended due
to possible disfigurement and loss of function. Selection of the
optimal chemotherapeutic regimen is challenging due to the lack of
published research, with no standard chemotherapy treatment
established for NKTL, much less penile metastasis. Recent clinical
studies have suggested that pegaspargase-based chemotherapy is a
potential therapeutic option with a good remission rate for
advanced NKTL (22,23). In the current case, the patient
received three cycles chemotherapy of DDGP (including cisplatin,
dexamethasone, gemcitabine, pegaspargase), and the penile mass was
decreased after the first cycle. After two cycles of chemotherapy,
a partial remission was achieved. The patient subsequently received
another cycle of chemotherapy and remained in stable condition.
In conclusion, penile metastasis secondary to
extranodal NKTL without recurrence at the primary site, although
rare, should be considered in the differential diagnosis of a
penile mass. Pegaspargase-based chemotherapy may produce a positive
outcome in such cases, at least in the short-term.
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant no. 81570203).
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
YL and XF wrote the manuscript. JW, CY, ZL, ZS and
JY performed the literature review. FN, XZ, LL, XL and LZ organized
the figures and tables. WL and GW performed the pathologic
diagnosis. MZ directed the diagnosis and management procedure of
the patient and revised the manuscript.
Ethics approval and consent to
participate
Ethical approval was obtained from the Scientific
Research and Clinical Trial Ethics Committee of The First
Affiliated Hospital of Zhengzhou University (Zhengzhou, China) and
written informed consent was obtained from the patient.
Consent for publication
Written informed consent was obtained from the
patient for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Haverkos BM, Pan Z, Gru AA, Freud AG,
Rabinovitch R, Xu-Welliver M, Otto B, Barrionuevo C, Baiocchi RA,
Rochford R and Porcu P: Extranodal NK/T cell lymphoma, nasal type
(ENKTL-NT): An update on epidemiology, clinical presentation and
natural history in North American and European cases. Curr Hematol
Malig Rep. 11:514–527. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Suzuki R: Pathogenesis and treatment of
extranodal natural killer/T-cell lymphoma. Semin Hematol. 51:42–51.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Au WY, Weisenburger DD, Intragumtornchai
T, Nakamura S, Kim WS, Sng I, Vose J, Armitage JO and Liang R:
International Peripheral T-Cell Lymphoma Project: Clinical
differences between nasal and extranasal natural killer/T-cell
lymphoma: A study of 136 cases from the international peripheral
t-cell lymphoma project. Blood. 113:3931–3937. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Baldur-Felskov B, Hannibal CG, Munk C and
Kjaer SK: Increased incidence of penile cancer and high-grade
penile intraepithelial neoplasia in denmark 1978–2008: A nationwide
population-based study. Cancer Causes Control. 23:273–280. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Barnholtz-Sloan JS, Maldonado JL, Pow-sang
J, Giuliano AR and Guiliano AR: Incidence trends in primary
malignant penile cancer. Urol Oncol. 25:361–367. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lin DW, Thorning DR and Krieger JN:
Primary penile lymphoma: Diagnostic difficulties and management
options. Urology. 54:3661999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lan SK, Lin CW, Ho HC, Lee MS, Tzeng JE
and Su YC: Penile metastasis secondary to nasal NK/T-cell lymphoma.
Urology. 72:1014–1015. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lister TA, Crowther D, Sutcliffe SB,
Glatstein E, Canellos GP, Young RC, Rosenberg SA, Coltman CA and
Tubiana M: Report of a committee convened to discuss the evaluation
and staging of patients with Hodgkin's disease: Cotswolds meeting.
J Clin Oncol. 7:1630–1636. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lee J, Suh C, Park YH, Ko YH, Bang SM, Lee
JH, Lee DH, Huh J, Oh SY, Kwon HC, et al: Extranodal natural killer
T-cell lymphoma, nasal-type: A prognostic model from a
retrospective multicenter study. J Clin Oncol. 24:612–618. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sun J, Medeiros LJ, Lin P, Lu G,
Bueso-Ramos CE and You MJ: Plasmablastic lymphoma involving the
penis: A previously unreported location of a case with aberrant CD3
expression. Pathology. 43:54–57. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yao HJ, Ying J, Wang Z, Yao DH, Ren XM and
Bao YY: One case report of primary penile malignant lymphoma (with
a review of 24 case reports). Zhonghua Nan Ke Xue. 12:520–524.
2006.PubMed/NCBI
|
|
12
|
Terada T, Shirakashi Y and Sugiura M:
T-cell lymphoma of the penis as the first manifestation of adult
T-cell lymphoma/leukemia. Int J Dermatol. 51:973–975. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li YL, Wang QZ, Ding GF, Li LX, Ni Z and
Wang XM: Primary non-Hodgkin's lymphoma of the testis and penis:
Clinical analysis of 5 cases. Zhonghua Nan Ke Xue. 17:254–256.
2011.(In Chinese). PubMed/NCBI
|
|
14
|
Zhou ZL, Wang CY, Xu ZS and Zheng BZ:
Primary cutaneous T-cell lymphoma of the penis complicated by
Fournier gangrene: A case report. Zhonghua Nan Ke Xue. 14:542–544.
2008.PubMed/NCBI
|
|
15
|
Shi YL, Yin HL, Zhou XJ, Zhou HB and Lu
ZF: Primary peripheral T-cell lymphoma of the penis: A case report
and review of the literature. Zhonghua Nan Ke Xue. 14:1003–1006.
2008.(In Chinese). PubMed/NCBI
|
|
16
|
Wang HT, Lo YS and Huang JK: Primary
lymphoma of the penis. J Chin Med Assoc. 66:379–381.
2003.PubMed/NCBI
|
|
17
|
Tomb RR, Stephan F, Klein-Tomb L, Chahine
G and Grosshans E: Recurrent primary CD30+ lymphoma of the penis.
Br J Dermatol. 149:903–905. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Thorns C, Urban H, Remmler K, Dietel A,
Lange K and Merz H: Primary cutaneous T-cell lymphoma of the penis.
Histopathology. 42:513–514. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pomara G, Cuttano MG, Tripodo C, Carlino F
and Selli C: Primary T-cell rich B-cell lymphoma of the penis: A
first case. BJU Int. 91:8892003. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Allen DC and Walsh MY: Malignant lymphoma
of the scrotum and Wegener's granulomatosis of the penis-genital
presentation of systemic disease. Ulster Med J. 65:169–172.
1996.PubMed/NCBI
|
|
21
|
Yanagi H, Nakamura Y, Takagi D and Kubota
K: Extranodal natural killer/T-cell lymphoma: A diagnostic dilemma.
Rhinology. 50:325–331. 2012.PubMed/NCBI
|
|
22
|
Zhou Z, Li X, Chen C, Li X, Zhang L, Li L,
Wang X, Ma W, Fu X, Wu J, et al: Effectiveness of gemcitabine,
pegaspargase, cisplatin and dexamethasone (DDGP) combination
chemotherapy in the treatment of relapsed/refractory extranodal
NK/T cell lymphoma: A retrospective study of 17 patients. Ann
Hematol. 93:1889–1894. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wen JY, Li M, Li X, Chen J, Lin Q, Ma XK,
Dong M, Wei L, Chen ZH and Wu XY: Efficacy and tolerance of
pegaspargase-based chemotherapy in patients with nasal-type
extranodal NK/T-cell lymphoma: A pilot study. Asian Pac J Cancer
Prev. 15:6275–6281. 2014. View Article : Google Scholar : PubMed/NCBI
|