Introduction
Carcinoid tumors occur in various types of organs,
the most frequent of which are identified in the digestive system
(64.2%). Primary carcinoid tumor of the middle ear is an extremely
rare form of carcinoid tumor (<0.7%) (1,2). Almost
all cases of the disease are diagnosed via biopsy analysis,
postoperative pathological examination, or transmission electron
microscopy in atypical histopathological cases (3,4). In
carcinoid tumors of other organs, such as those of the digestive
system and lungs, fine needle aspiration cytology (FNAC) is a
routine preoperative examination. However, in carcinoid tumors of
the middle ear, FNAC is not usually performed as a preoperative
examination as there is a risk of complications due to the complex
anatomical structure of the middle ear. To the best of our
knowledge, there have been no previous reports on preoperative
cytodiagnosis for carcinoid tumors of the middle ear.
The primary course of treatment is surgery in the
majority of localized cases (2,5); however,
treatment for patients with unresectable metastatic disease may
involve a combination of surgical resection and systemic therapy
(e.g., a course of chemotherapy) (5).
For patients with functional tumors, somatostatin analogues are the
primary treatment regime, which aims to control symptoms caused by
an excess of hormones including insulin gastrin, glucagon,
vasoactive intestinal peptide and somatostatin (5). A recent study provided evidence that the
choice of treatment options for patients with carcinoid tumors
should increased and be based upon the extent, tumor proliferation
rate, symptoms, histological grade and primary tumor site (5). Therefore, accurate clinical and/or
histological diagnosis is required for patients with carcinoid
tumor.
The present study discusses a primary middle ear
tumor, which was preoperatively diagnosed as neuroendocrine tumor
(NET) using cytology and was postoperatively diagnosed as a
carcinoid tumor using histological examination.
Case report
A 22-year old Japanese woman with no previous
history of disease complained of left-side otalgia and visited the
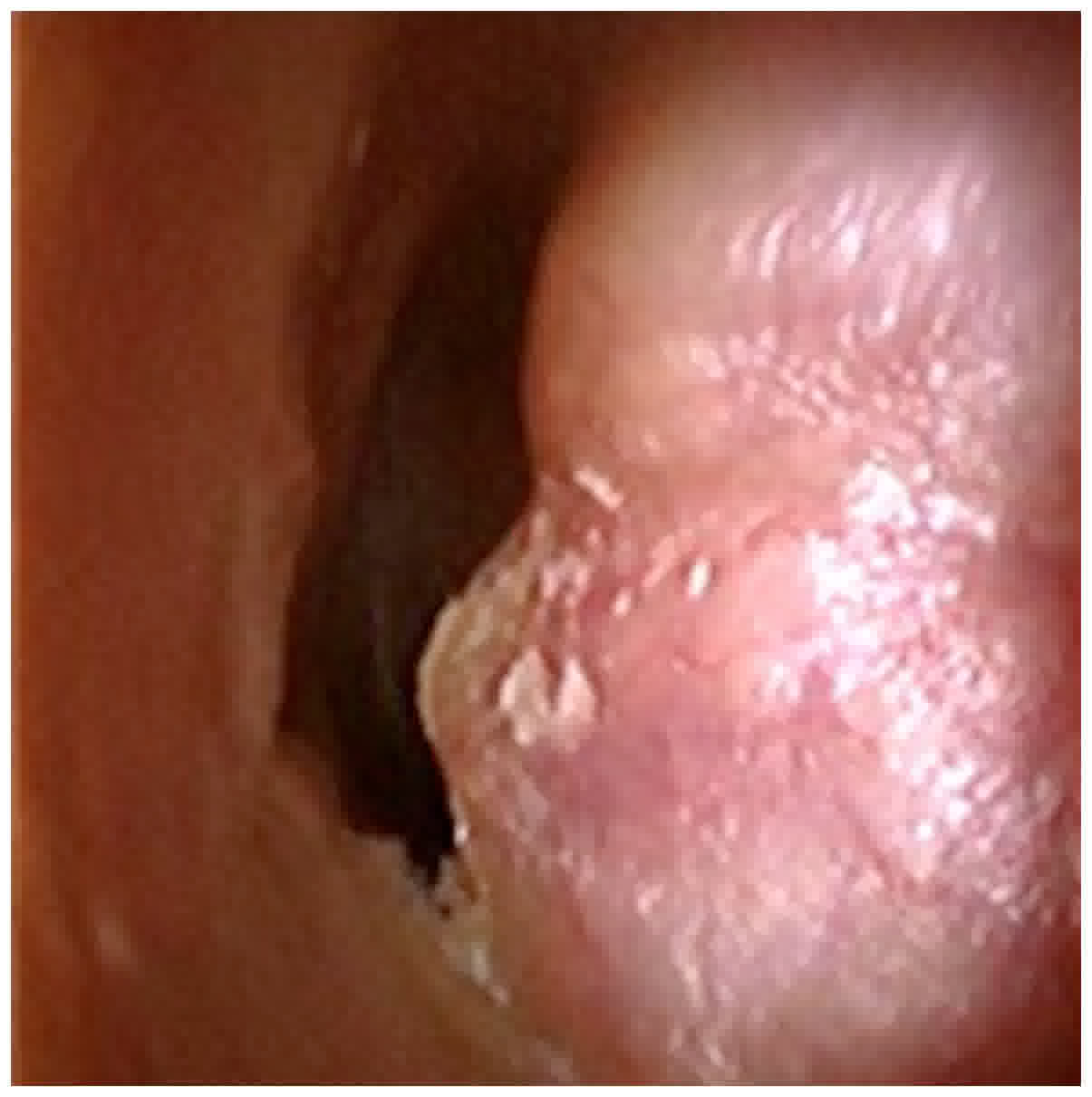
outpatient clinic of Kurume University Hospital (Kurume, Japan). A
physical examination revealed a subcutaneous tumor protruding into
the left external acoustic meatus (the external auditory canal)
(Fig. 1). An audiogram demonstrated
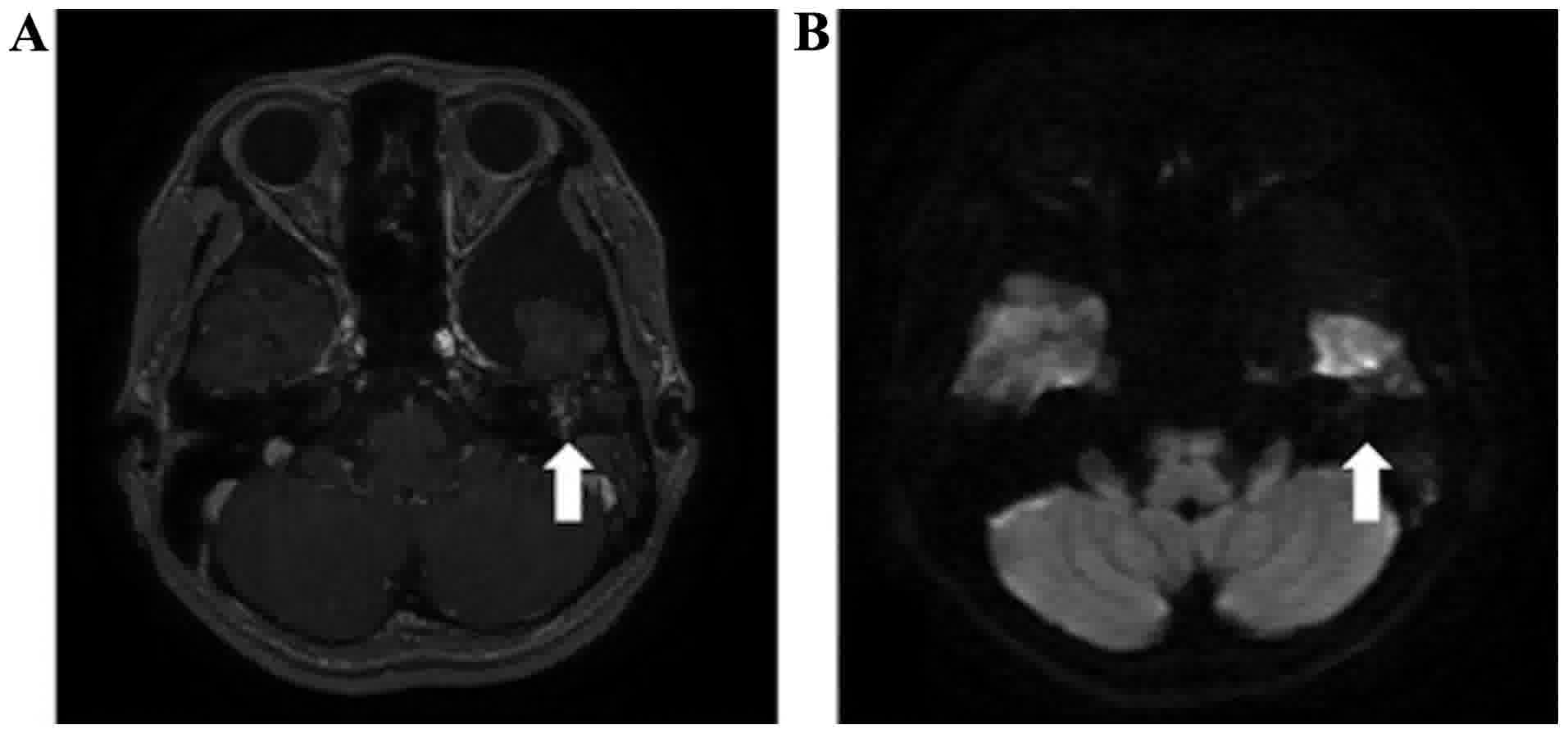
conductive hearing loss. Gadolinium-enhanced T1-weighted magnetic
resonance imaging (MRI) with low contrast enhancement (Fig. 2A) and diffusion weighted MRI with low
intensity (Fig. 2B) revealed a
tumor-like lesion occupied in the tympanic cavity of the middle
ear, extending to the mastoid antrum and mastoid cells of the
middle ear and to the external acoustic meatus. The lesion was
considered to be a primary middle ear tumor, as it would never have
extended to the mastoid antrum and mastoid cells if the tumor had
originated from the external acoustic meatus. These imaging results
were not able to lead to a definitive diagnosis, although they
excluded the possibility of glomus tumor or cholesteatoma.
Therefore, FNAC was performed.
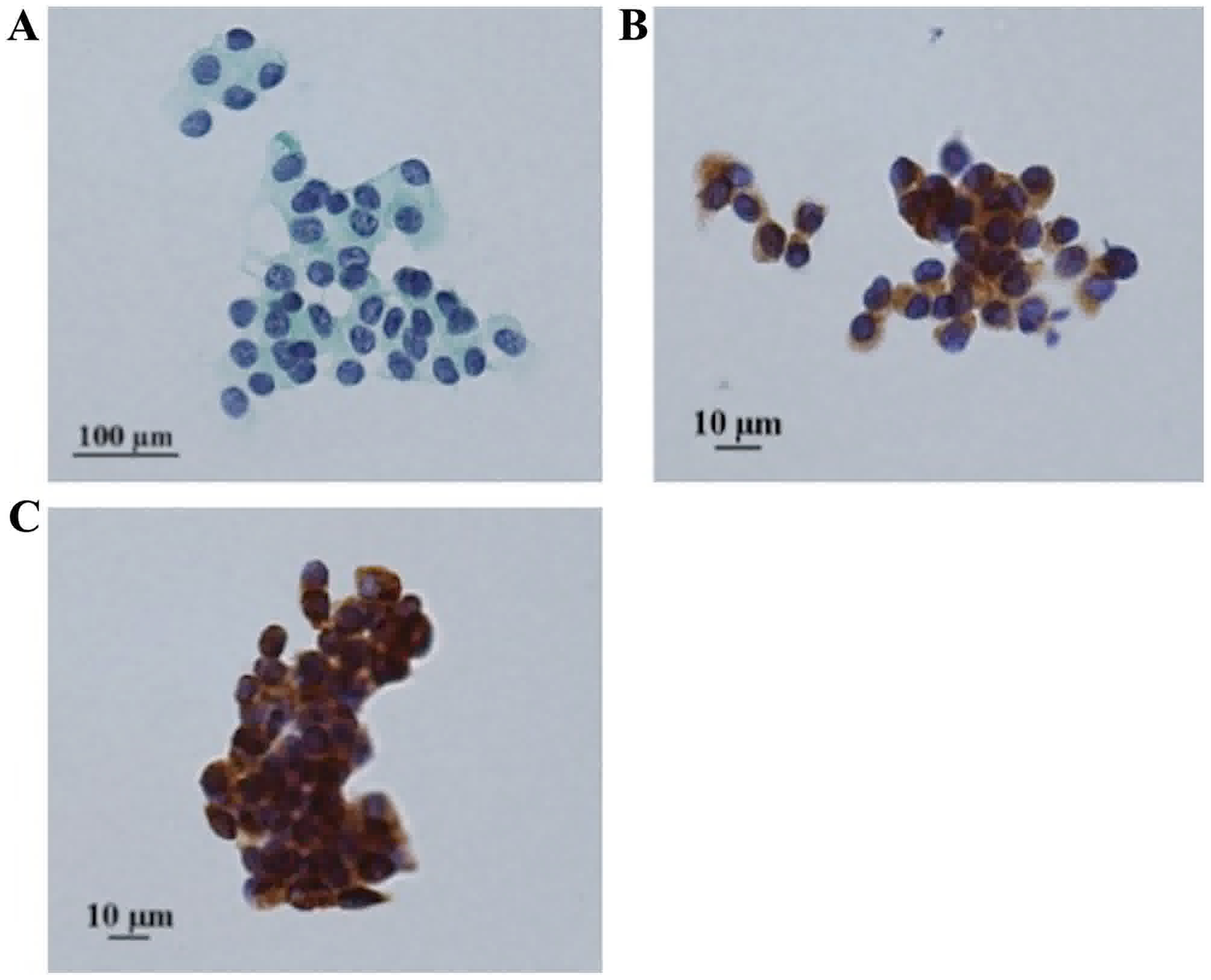
The cytological findings revealed that the tumor was
composed of cells, which exhibited small round nuclei with
dispersed chromatin and granular eosinophlic cytoplasm, arranged in
a nested pattern (Fig. 3A). These
tumor cells were positive for synaptophysin (Fig. 3B) and cytokeratin CAM5.2 (Fig. 3C) and negative for tumor protein p63
and Wilms tumor 1 immunocytochemically; Ki-67 immunoreactivity was
observed in <1% of the tumor cells. These results indicated that
the tumor may be NET, likely a carcinoid tumor. The smears were
fixed in 95% ethanol at room temperature for one day and analyzed
using Papanicolaou staining. Papanicolaou staining was performed as
below.
Briefly, slides were washed with 70% ethanol for 3
min and then washed with tap water for 2 min. Slides were stained
with Gill's hematoxylin (Muto Pure Chemicals Co., Ltd., Tokyo,
Japan) at room temperature for 5 min, rinsed with 1% hydrochloric
acid alcohol for 7 sec, washed with tap water for 7 min, and then
twice with 95% ethanol for 1 min each. Slides were then stained
using Orange G-6 (Ready to use dilution, Matsunami Glass Ind., Ltd.
Osaka, Japan) solution (Matsunami Glass Ind., Ltd., Kishiwada,
Japan) at room temperature for 3 min, and washed twice with 95%
ethanol for 1 min each. Slides were then stained using eosin A-50
solution (Matsunami Glass Ind., Ltd.) at room temperature for 4
min, and washed twice with 95% ethanol for 1 min each. Slides were
washed three times with 100% ethanol for 2 min each, immersed in
xylene three times for 2 min each and mounted in Marinol mounting
medium (Muto Pure Chemicals Co., Ltd.).
Laboratory examination revealed that serum
5-hydroxyindoleacetic acid (5-HIAA, normal range: 1.8–6.1 ng/ml)
and vanillylmandelic acid (3.3–8.6 ng/ml), urine total
catecholamine (normal range: 52.0–195.3 µg/day) and 5-HIAA (normal
range: 1.0–6.0 mg/day) were within the normal reference ranges.
Briefly, serum samples were dispensed, and deproteinised with 6%
perchloric acid. Following centrifugation (11,269 × g, 4°C, 17
min), the supernatant was extracted and used for analysis.
Wakosil-II 5C18HG (cat. no. N 235-51001; Wako Pure Chemical
Industries, Ltd., Osaka, Japan) and Wakosil-II 3C18HG (cat. no. N
238-50251, Wako Pure Chemical Industries, Ltd.) were used for
5-HIAA analysis. TSKgel ODS-80Ts (cat. no. N 0018151; Tosoh
Bioscience, Tokyo, Japan) and Pegasil ODS (cat. no. N
PG-ODS-1101-SPW; Senshu Scientific Co., Ltd, Tokyo, Japan) were
used for vanillylmandelic acid. Serum 5-HIAA and vanillylmandelic
acid samples were analyzed using a high liquid performance
chromatography (HPLC) system (Shimadzu Corporation, Kyoto, Japan).
Single voided urine samples were dispensed, and Wakosil-II 5C18HG
(cat. no. N 232-51011; Wako Pure Chemical Industries, Ltd.) was
used for urine 5-HIAA analysis, and Wakosil-II 5C18RS (cat. no. N
232-51371; Wako Pure Chemical Industries, Ltd.) and TSKgel CA-2
(cat. no. N 0018932; Tosoh Bioscience) were used for catecholamine
analysis. Urine catecholamine and 5-HIAA samples were analyzed
using an HPLC system, perfomed by Shimadzu Corporation.
There was no paraneoplasia, including diarrhea,
suffusion or edema. No other tumor lesions in other organs were
detected on computed tomography scans. Consequently, a diagnosis of
primary carcinoid tumor of the middle ear was considered.
Since the tumor involved the mastoid anturm, mastoid
cells and external auditory canal, two-staged tympanoplasty and
mastiodectomy was performed. Since the boundary of the tumor in the
tympanic cavity around the stapes was unclear, the incus was
removed to allow for complete resection of the tumor. A
second-stage operation was planned to prevent recurrence.
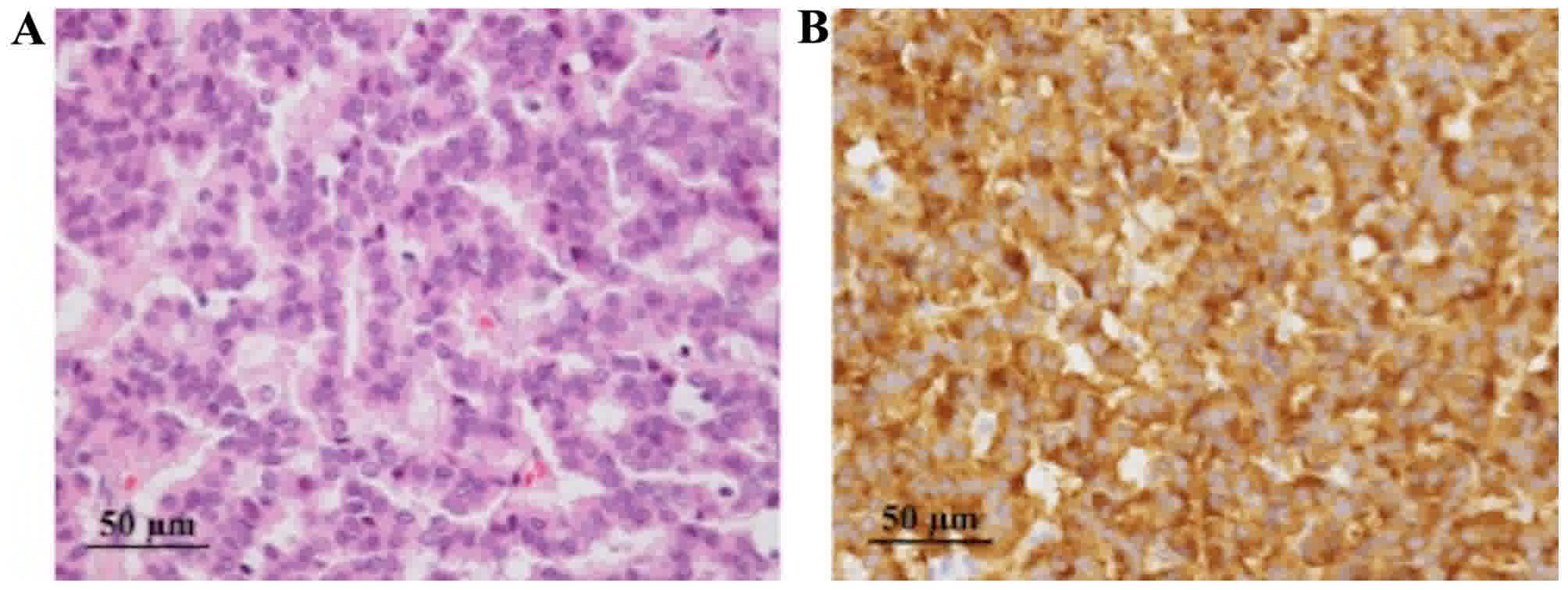
The tumor was histologically composed of small
uniform cells with small round nuclei and granular eosinophilic
cytoplasm, and was proliferating in trabecular and mosaic patterns
(Fig. 4A and B). Immunoreactivity
with synaptophysin was identified in tumor cells. On the other
hand, immunoreactivity with chromogranin A and cluster of
differentiation (CD)56 was not detected. Ki-67 index was identified
in <2% of the cells. The definitive diagnosis was carcinoid
tumor.
Briefly, paraffin-embedded tissue samples were cut
at 4 µm thick, examined on a coated slide glass and labeled with
the following antibodies: Mouse monoclonal anti-synaptophysin (cat.
no. N 413831; ready to use dilution, Nichirei, Tokyo, Japan), mouse
monoclonal anti-chromogranin A (cat. no. M0869; 1:400; Dako;
Agilent Technologies, Inc., Santa Clara, CA, USA), mouse monoclonal
anti-CD56 (cat. no. NCL-L-CD56-1B6; 1:200; Leica Microsystems,
Ltd., Milton Keynes, UK) and mouse monoclonal anti-Ki67 (cat. no.
M7240; 1:100; clone MIB1; Dako; Agilent Technologies, Inc.).
Two fully automated immunostainers, the BenchMark
ULTRA system (Ventana Medical Systems, Inc., Tucson, AZ, USA) and
the Bond-III system (Leica Microsystems, Ltd.), were used. The
BenchMark ULTRA system was used for Ki-67 immunostaining. Briefly,
each slide was heat-treated using the Ventana ULTRA cell
conditioning 1 retrieval solution (EDTA; pH 8.5; Ventana Medical
Systems, Inc. UAS) for 60 min at 95°C, and then incubated with the
Ki-67 antibody (as aforementioned) for 30 min at 37°C. The
automated system used the Ventana UltraVIEW 3,3′ diaminobenzidine
(DAB) detection kit with a horseradish peroxidase (HRP) multimer as
a secondary antibody, peroxidase inhibitor, DAB chromogen,
H2O2, and copper (cat. no. 760-500; Ventana
Medical Systems, Inc., USA). This detection kit is an indirect,
biotin-free system for detecting mouse immunoglobulin (Ig)G, mouse
IgM and rabbit primary antibodies. Each slide was incubated with
the secondary antibodies for 30 min at 37°C and visualized with DAB
and 0.04% hydrogen peroxide.
Immunostaining with synaptophysin, chromogranin A
and CD56 were performed on the automated Bond-III system (Leica
Microsystems, Ltd.) using onboard heat-induced antigen retrieval
with epitope retrieval solution 2 (EDTA-based buffer; pH 9.0; Leica
Microsystems, Ltd.) for 15 min at 99°C, and incubated with each
primary antibody for 30 min at room temperature. This automated
system used a refine polymer detection kit (cat. no. TA9145; Leica
Microsystems, Ltd.) with HRP-conjugated anti-mouse/rabbit IgG and
goat polyclonal antibody as a secondary antibody, and was incubated
for 30 min at room temperature. Slides were visualized using DAB
and 0.1% hydrogen peroxide.
Prior to hematoxylin and eosin staining, slides were
placed in xylene and hydrated by passing through alcohol (70, 80,
90 and 95% alcohol for 2 min each). Slides were stained in
hematoxylin (cat. no. 8650, Sakura Finetek Europe B.V., Flemingweg,
The Netherlands) for 5 min, washed with tap water for 5 min, and
then stained with eosin (cat. no. 8659, Sakura Finetek Europe B.V.)
for 10 min at room temperature.
At 8 months following the primary surgery, incus
interposition ossiculoplasty was performed as the second-stage
operation. The patient remained recurrence-free for 11 months
during follow-up examinations. The patient provided written
informed consent for inclusion in the present study.
Discussion
The middle ear is composed of the tympanic cavity,
mastoid antrum and mastoid cells. The tympanic cavity is a tiny
cavity containing auditory ossicles. FNAC of the middle ear is not
a routine examination owing to the risk of complications, including
ossicular disruption or bleeding. Krouse et al (6) reported that the tympanic membrane was
retained but was reddened, thickened or bulging in almost all cases
of carcinoid tumor of the middle ear. There are few reports of
tumors of the middle ear that have invaded into the subcutaneous
tissue of the external acoustic meatus (3,7). Biopsies
were attempted in these cases, although FNAC was not performed.
FNAC is a common examination for canal tumors of the
external acoustic meatus (8). Mohan
et al (9) reported a case of
adenoid cystic carcinoma of the external acoustic meatus diagnosed
by FNAC and discussed its utility. In subcutaneous tumor cases, an
incisional biopsy is required to obtain adequate specimens;
however, there is a risk of bleeding. As FNAC is relatively safe
compared with biopsy, cytology can be a complementary or
alternative examination for biopsy for tumors of the external
acoustic meatus and the middle ear. In the present case, FNAC may
be performed because the tumor protruded into the external auditory
canal.
Carcinoid tumors of the middle ear were first
described by Murphy et al (10) in 1980. Additional cases have been
reported and their clinical and histopathological characteristics
have also become clear. Carcinoid tumors of the middle ear exhibit
the same histopathological and morphological characteristics as
pulmonary and gastrointenstinal carcinoid tumors (11).
Morphological findings of carcinoid tumors are
described in which the nuclei are round-to-oval with dispersed
chromatin, and eosinophilic and granular cytoplasm (11). In Papanicolaou staining, aspirated
specimens exhibit monotonous groups of well-preserved round cells
or a mixture of round and spindle cells (12). Cytological features of NETs, including
carcinoid tumor, often mimic small cell carcinoma and/or malignant
lymphoma. It is important to distinguish carcinoid tumor from these
neoplasms, as the clinical treatment is completely different.
Immunohistochemical examination is useful for distinguishing these
tumors.
Immunohistochemistry of neuroendocrine markers,
including chromogranin A, synaptophysin and cluster of
differentiation 56, is useful for making a diagnosis of NETs. There
are several reports on the immunohistochemistry of carcinoid tumors
(11–13). Immunocytochemistry was not commonly
performed because the amount of cells is limited. However, with the
advances in liquid based cytology (such as the BD Diagnostics
SurePath test), performing immunocytochemistry has become easy.
Indeed, immunocytochemistry was performed using liquid-based
cytology material in the present case. Immunocytochemistry can be
performed when carcinoids occur in unusual sites, including the
middle ear or larynx (4,14). As primary carcinoid of the middle ear
is extremely rare, an entire body examination must be performed
preoperatively to exclude the possibility of metastasis.
In the present case, stained with Papanicoloau
stains, the nuclei of the tumor cells were round with dispersed
chromatin and exhibited low-grade atypia, and the cytoplasm of the
tumor cells were granular. On the basis of the morphological
features, NETs, including a carcinoid tumor, were suspected, with
immunocytochemical results supporting the cytological
diagnosis.
In previous cases of carcinoid tumors of the middle
ear, removal of the tumor by conventional tympanomastoidectomy
improved the surgical procedure as tympanomastoidectomy enabled
complete removal of the tumor within the middle ear (6,15,16). It is not necessary to perform
exploratory surgery in preoperatively diagnosed cases; therefore,
it is important to achieve a diagnosis prior to surgery to perform
radical surgery for the primary operation. Preoperative FNAC makes
a substantial contribution to determining the operative method in
cases of NETs, including carcinoid tumors of the middle ear.
In a previous cytological study, carcinoid and
neuroendocrine cancer were diagnosed based on morphology and
immunocytochemical analysis (17). In
examinations that involve a comparison of the intraoperative
cytologic diagnosis in small specimen with final histologic
diagnosis of the resected specimen, the cytodiagnostic sensitivity
and specificity are 86.7 and 98.7% respectively to diagnose
pulmonary neuroendocrine tumor (18).
As carcinoid tumors of the middle ear exhibit the same
histopathological and morphological characteristics exhibited in
pulmonary neuroendocrine tumors, FNAC with immunocytochemical
analysis is a reliable examination for patients with carcinoid
tumor of the middle ear.
To conclude, FNAC with immunocytochemistry is a
reliable preoperative examination for NETs, including carcinoid
tumors of the middle ear.
Acknowledgements
The authors would like to thank the members of SRL,
Inc. (Tokyo, Japan) for providing information about the laboratory
examination.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study, except those performed by an external organization, are
included in this published article.
Authors' contributions
KS, RM, JA, HU and HY designed the study. KS wrote
the initial draft of the manuscript. RM, TK, TY and AK contributed
to analysis and interpretation of data. All authors revised the
manuscript critically for important intellectual content and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
inclusion in the present study.
Consent for publication
The patient provided written informed consent for
publication of the present study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Soga J: Carcinoid and their variant
endocrinomas. An analysis of 11842 reported cases. J Exp Clin
Cancer Res. 22:517–530. 2003.PubMed/NCBI
|
|
2
|
Godwin JD II: Carcinoid tumors. An
analysis of 2,837 cases. Cancer. 36:560–569. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ramsey MJ, Nadol JB Jr, Pilch BZ and
Mckenna MJ: Carcinoid tumor of the middle ear: Clinical features,
recurrences, and metastases. Laryngoscope. 115:1660–1666. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tamai S, Iri H, Maruyama T, Kasahara M,
Akatsuka S, Sakurai S and Murakami Y: Laryngeal carcinoid tumor:
Light and electron microscopic studies. Cancer. 48:2256–2259. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kunz PL: Carcinoid and neuroendocrine
tumors: Building on success. J Clin Oncol. 33:1855–1863. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Krouse JH, Nadol JB Jr and Goodman ML:
Carcinoid tumors of the middle ear. Ann Otol Rhinol Laryngol.
99:547–552. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Inoue S, Tanaka K and Kannae S: Primary
carcinoid tumor of the ear. Virchows Arch A Pathol Anat Histol.
396:357–363. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ohta Y, Morihana T, Hanada Y, Imai T,
Iwamoto Y, Uno A, Kawashima T, Hasegawa T, Kitahara T, Morii E and
Inohara H: A clinical study of 61 cases of tumorous disease in
external ear canal: Diagnosis of tumor. Otol Jpn. 25:771–776.
2015.
|
|
9
|
Mohan H, Handa U, Amanjit, Kotwal SA and
Dass A: Adenoid cystic carcinoma of the external auditory canal. A
case report with diagnosis by fine needle aspiration. Acta Cytol.
47:792–794. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Murphy GF, Pilch BZ, Dickersin GR, Goodman
ML and Nadol JB Jr: Carcinoid tumor of the middle ear. Am J Clin
Pathol. 73:816–823. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Torske KR and Thompson LD: Adenoma versus
carcinoid tumor of the middle ear: A Study of 48 cases and review
of the literature. Mod Pathol. 15:543–555. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Renshaw AA, Haja J, Lozano RL and Wilbur
DC: Cytology Committee, College of American Pathologists:
Distinguishing carcinoid tumor from small cell carcinoma of the
lung: Correlating cytologic features and performance in the College
of American Pathologists Non-Gynecologic Cytology Program. Arch
Pathol Lab Med. 129:614–618. 2005.PubMed/NCBI
|
|
13
|
Burke AP, Thomas RM, Elsayed AM and Sobin
LH: Carcinoids of the jejunum and ileum: An immnohistochemical and
climicopathologic study of 167 cases. Cancer. 79:1086–1093. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sato K, Higaki Y, Sakaguchi S, Hirano M,
Tanimura A and Sasaguri Y: Carcinoid tumor of the larynx. Auris
Nasus Larynx. 18:39–53. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Manni JJ, Faverly DR and Van Haelst UJ:
Primary carcinoid tumors of the middle ear. Report on four cases
and review of the literature. Arch Otolaryngol Head Neck Surg.
118:1341–1347. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Knerer B, Matula C, Youssefzadeh S, Ulrich
W and Swoboda H: Treatment of a local recurrence of a carcinoid
tumor of the middle ear by extended subtotal petrosectomy. Eur Arch
Otorhinolaryngol. 255:57–61. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Inzani F, Petrone G, Fadda S and Rindi G:
Cyto-histology in NET: What is necessary today and what is the
future. Rev Endocr Metab Disore. 2017.Doi:
10.1007/s11154-017-9428-x. View Article : Google Scholar
|
|
18
|
Biancosino C, Krüger M, Vollmer E and
Welker L: Intraoperative fine needle apirations-dignosis and typing
of lung cancer in small biopsies: Challenges and limitations. Diagn
Pathol. 11:592016. View Article : Google Scholar : PubMed/NCBI
|