Introduction
Primary brain lymphoma is a rare central nervous
system malignancy, and only accounts for 1.5% of all intracranial
tumors (1). However, with the
continuous development of medical technology in recent years, the
widespread use of immunological agents and the maturity of organ
transplantations have made patients prone to primary brain lymphoma
due to immunodeficiency (2,3). Ferreri et al (4) reported that the number of patients with
primary brain lymphoma increased by 80,000 in 2000–2005 compared
with that in 1990s. Nayak et al (5) also reported that the incidence of
primary brain lymphoma showed an increasing trend, and it will
become a type of malignant intracranial tumor with extremely high
incidence in 2025. Clinically, prevention of primary brain lymphoma
has become an extremely important issue (6). The universal treatment of intracranial
tumors is ‘early detection and early treatment’, and the main
clinical diagnosis methods are magnetic resonance imaging (MRI),
and computed tomography (CT). Primary brain lymphoma show no
obvious signs during the early stages, and specific imaging
features are also lacking. Thus, early diagnosis is difficult
(7,8).
Therefore, this study aimed to analyze the imaging diagnosis of MRI
and CT for patients with primary brain lymphoma with an expectation
of providing reference and guidance for the early diagnosis of
patients with primary brain lymphoma.
Patients and methods
General information
A total of 230 patients with primary brain lymphoma
admitted to People's Hospital of Rizhao (Rizhao, China) were
selected from July, 2005 to December, 2016 into the study and their
clinical data were analyzed retrospectively. There were 147 males
and 83 females, with a mean age of 48.12±10.57 years. Among those
patients, 87 patients were examined by CT, 74 patients by MRI, and
69 patients by both MRI and CT. Inclusion criteria: Patients with
primary brain lymphoma confirmed by biopsy; patients with complete
clinical record; patients willing to cooperate with researchers.
Exclusion criteria: Patients combined with upper respiratory tract
diseases; patients combined with lower gastrointestinal diseases;
patients combined with cardiovascular diseases; patients
transferred to other hospitals during treatment; patients with
severe physical disability; patients treated with drugs prescribed
by other hospitals. All patients signed written informed consent.
The study was approved by the Ethics Committee of People's Hospital
of Rizhao. Signed written informed consents were obtained from the
patients and/or guardians.
Instruments and methods
CT detector was a LightSpeed 16-slice spiral CT (GE
Healthcare Life Sciences, Waukesha, WI, USA), and MRI detector was
a Vision Plus 1.5T superconducting scanner (Siemens, Munich,
Germany). All reagents used are original equipment supporting
reagents. All patients who underwent CT were subjected to head
plain scanning and enhanced CT scanning. Both T1W1 and T2W1
scanning were performed in MRI by using both selective echo (SE)
and fast spin echo (FSE) imaging (Table
I for parameter settings).
 | Table I.Parameter settings for CT and MRI. |
Table I.
Parameter settings for CT and MRI.
| Methods | Thickness (mm) | Layer interval
(mm) |
|---|
| CT | 10 | 10 |
| MRI | 5 | 1 |
Imaging analysis
Clinical data and pathological test results were
used as gold standard to evaluate the accuracies of three methods.
Imaging features of lesions in MRI and CT scanning were observed
with a focus on the density, number and margins of lesions. All MRI
and CT images were analyzed by four experienced imaging physicians
through double-blind method, and clinical values were analyzed.
Statistical analysis
SPSS 22.0 statistical software (IBM Corp., Armonk,
NY, USA) was used for all statistical analyses. Enumeration data
were expressed as rate, and comparisons among multiple groups were
performed by Chi-square test. Sensitivity and specificity of
diagnosis were analyzed by ROC curve.
Results
Clinical patient data
Comparison of clinical data showed that there were
no significant differences in age, sex, ethnicity, marital status,
living area, smoking index, alcohol consumption, exercise status,
pathological stages and clinical symptoms among three groups (CT,
MRI and CT combined with MRI; p>0.05) (Table II).
 | Table II.Clinical patient data. |
Table II.
Clinical patient data.
| Variables | CT group (n=87) | MRI group (n=74) | MRI+CT group
(n=69) | F-value | P-value |
|---|
| Age (years) |
|
|
| 2.351 | 0.294 |
|
<45 | 51 (58.6) | 48 (64.9) | 39 (56.5) |
|
|
| ≥45 | 36 (41.4) | 26 (35.1) | 30 (43.5) |
|
|
| Sex |
|
|
| 3.250 | 0.348 |
| Male | 57 (65.5) | 48 (64.9) | 42 (60.9) |
|
|
|
Female | 30 (34.5) | 26 (35.1) | 27 (39.1) |
|
|
| Ethnicity |
|
|
| 3.184 | 0.404 |
| Han | 81 (93.1) | 70 (94.6) | 62 (89.9) |
|
|
|
Others | 6 (6.9) | 4 (5.4) | 7 (10.1) |
|
|
| Marital status |
|
|
| 2.215 | 0.310 |
|
Married | 75 (86.2) | 61 (82.4) | 55 (79.7) |
|
|
|
Unmarried | 9 (10.3) | 10 (13.5) | 11 (15.9) |
|
|
|
Widowed | 3 (3.4) | 3 (4.1) | 3 (4.3) |
|
|
| Living area |
|
|
| 3.034 | 0.425 |
|
Countryside | 59 (67.8) | 47 (63.5) | 41 (59.4) |
|
|
| Urban
area | 28 (32.2) | 27 (36.5) | 28 (40.6) |
|
|
| Smoking index |
|
|
| 3.076 | 0.352 |
|
<400 | 45 (51.7) | 39 (52.7) | 33 (47.8) |
|
|
| ≥400 | 42 (48.3) | 35 (47.3) | 36 (52.2) |
|
|
| Drinking |
|
|
| 2.585 | 0.316 |
| Do not
drink or drink rarely | 48 (55.2) | 38 (51.4) | 35 (50.7) |
|
|
| Drink a
lot | 39 (44.8) | 36 (48.6) | 34 (49.3) |
|
|
| Exercise habits |
|
|
| 2.489 | 0.259 |
| Yes | 31 (35.6) | 30 (40.5) | 26 (37.7) |
|
|
| No | 56 (64.4) | 44 (59.5) | 43 (62.3) |
|
|
| Pathological
stages |
|
|
| 3.167 | 0.317 |
| I–II | 44 (50.6) | 39 (52.7) | 35 (50.7) |
|
|
|
III–IV | 43 (49.4) | 35 (47.3) | 34 (49.3) |
|
|
| Clinical
symptoms |
|
|
| 2.529 | 0.277 |
|
Headache | 71 (81.6) | 60 (81.1) | 55 (79.7) |
|
|
|
Vomit | 66 (75.9) | 52 (70.3) | 46 (66.7) |
|
|
|
Intracranial hypertension | 54 (62.1) | 41 (55.4) | 39 (56.5) |
|
|
|
Unresponsive | 71 (81.6) | 65 (87.8) | 61 (88.4) |
|
|
|
Abnormal behavior | 43 (49.4) | 30 (40.5) | 29 (42.0) |
|
|
|
Sleepiness | 24 (27.6) | 25 (33.8) | 41 (59.4) |
|
|
| Cranial
nerve paralysis | 39 (44.8) | 29 (39.2) | 29 (42.0) |
|
|
|
Aphasia | 56 (64.4) | 48 (64.9) | 48 (69.6) |
|
|
Imaging results
A total of 353 lesions were found in 230 primary
brain lymphoma patients, and 224 lesions were single lesions, and
129 lesions were multiple lesions. Most lesions were on the upper
curtain (81.3%, 187 cases) and 43 cases (18.7%) were on the lower
curtain. Among those lesions, 20.4% (72 lesions) were located in
the frontal lobes, 16.4% (58) in the temporal lobe, 25.5% (90) in
the parietal lobe, 18.1% (64) in the occipital lobe, 15.3% (54) in
the basal ganglia and 4.2% (15) in the cerebellum hemisphere. The
average size of lesions was 2.8×3.0×3.0 cm, and most lesions were
round or irregular shape.
CT and MRI imaging results
A total of 92 lesions were found from 87 patients
who underwent CT examination, and 27 lesions (29.3%) showed uniform
density and 65 lesions (70.7%) showed high density. Lesions showed
clear edges, with low-density edema around the tumor. All lesions
showed enhanced signals after enhanced scan. A total of 81 lesions
were found from 74 patients who underwent MRI examination. Results
of plain scan showed that all lesions were in uniform state, all
lesions showed low signal on T1WI, and 79.0% (64) lesions showed
high signal on T2WI, and 20.2% (17)
lesions showed no signal or equal signal. All lesions showed mild
mass effect. After enhanced scan, 86.9% (73) lesions showed
markedly uniform enhancement, 7.4% (6) showed uneven enhancement, and 2.5%
(2) showed ependymal dissemination.
No obvious cystic lesions, calcification or bleeding was found
within the lesions.
Diagnostic accuracy
Of the 87 patients who underwent CT examination, 72
cases of primary brain lymphoma were diagnosed, and the diagnostic
accuracy was 82.8%. Of 74 patients with MRI examination, 62 cases
were diagnosed, and the diagnostic accuracy was 83.8%. Of the 69
patients tested by MRI and CT, 62 cases were detected, and the
diagnostic accuracy was 89.9%. Therefore, combined diagnosis showed
highest accuracy (p<0.05) (Table
III).
 | Table III.Diagnostic accuracy of three
methods. |
Table III.
Diagnostic accuracy of three
methods.
| Methods | Diagnosis (n) | Misdiagnosis
(n) | Accuracy (%) |
|---|
| MRI (n=74) | 62 | 12 | 83.8 |
| CT (n=87) | 72 | 15 | 82.8 |
| MRI+CT (n=69) | 62 | 7 | 89.9 |
| F-value |
|
| 12.54 |
| P-value |
|
| 0.036 |
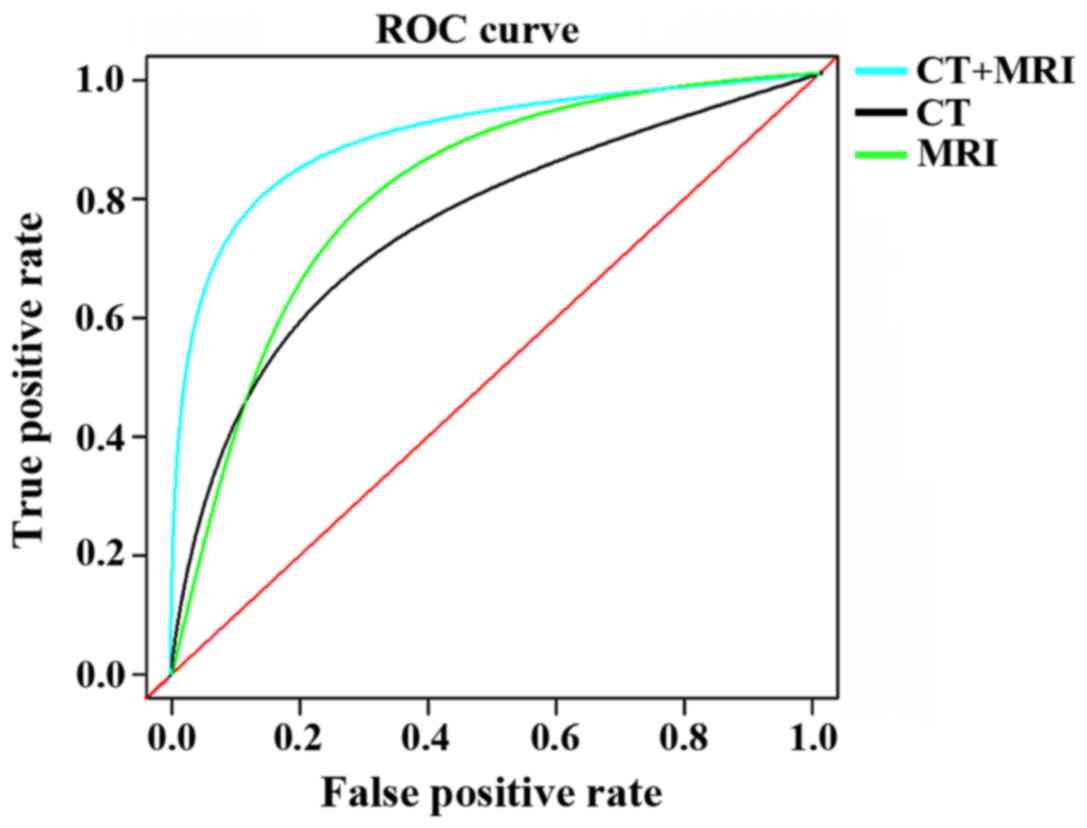
ROC curve analysis
ROC curve analysis showed that the AUC of MRI was
0.726 (95% CI, 0.215–2.337); the AUC of CT was 0.785 (95% CI,
0.616–1.242), and the AUC of MRI combined with CT was 0.845 (95%
CI, 0.145–4.632). Diagnostic sensitivity and specificity of MRI was
79.3 and 64.9%, respectively. Diagnostic sensitivity and
specificity of CT was 75.5 and 67.4%, respectively. Diagnostic
sensitivity and specificity of MRI combined with CT was 86.3 and
75.8%, respectively. The specificity and sensitivity of combined
detection were both higher than CT or MRI alone (p<0.05)
(Table IV; Fig. 1).
 | Table IV.ROC curve analysis results. |
Table IV.
ROC curve analysis results.
| Methods | AUC | 95% CI | Specificity
(%) | Sensitivity
(%) |
|---|
| MRI | 0.726 | 0.215–2.337 | 79.3 | 64.9 |
| CT | 0.785 | 0.616–1.242 | 75.5 | 67.4 |
| MRI+CT | 0.845 | 0.145–4.632 | 86.3 | 75.8 |
| F-value |
|
| 11.69 | 12.94 |
| P-value |
|
| 0.045 | 0.027 |
Discussion
Primary brain lymphoma is a lymphoma that occurs
only in the central nervous system (intracranial) and is not
commonly found in intracranial tumors due to its high requirement
of conditions of occurrence and development (2). With the development of medical
technology, all kinds of technologies that impair the function of
the patient's body have been applied and the deterioration of the
social environment has changed so that the immune function of the
modern human body has plummeted (9).
The development of primary brain lymphoma from mononuclear
phagocyte system in the perivascular space is due to the lack of
immune resistance in the body (10,11).
Therefore, in recent years, the incidence of primary brain lymphoma
showed an increasing trend. Studies (12–14) have
shown that the onset age of primary brain lymphoma is becoming
increasingly younger, which needs additional attention in the
clinic. Primary brain lymphoma at the early stages usually shows no
obvious signs, and error diagnosis and misdiagnosis are common
(15). Imaging is the most commonly
used method for the clinical diagnosis of primary brain lymphoma.
In this study, the imaging results of 230 patients with primary
brain lymphoma were analyzed with an expectation of providing
reference and guidance for the early diagnosis of patients with
primary brain lymphoma.
In this study, 87 of 230 patients with primary brain
lymphoma were examined by CT, 74 by MRI, and 69 by MRI and CT.
There was no significant difference in general information among
the three groups (p>0.05). MRI and CT imaging results showed
that primary brain lymphoma may occur in any part of the brain.
Disease usually develops in the perivascular space between the
mononuclear phagocyte system. So, more lesions were found in the
intracranial upper curtain (frontal lobe and basal ganglia) than in
lower curtain. In this study, the results of CT-examined lesions
were mostly isodense or high-density nodules, suggesting that the
arrangement of cells in primary brain lymphoma lesions usually
shows dense network structure with very little interstitial water
and high density of nuclear plasma, so X-ray absorption during the
CT scan is quite large, and this was reflected in the imaging
results. In MRI examination, imaging results were basically
consistent with the relevant studies (16–18); T1W1
showed low signal; T2W2 mostly showed high signal and equal signal,
which also proved that the primary brain lymphoma lesions usually
showed fibrous mesh arrangment. Patrick and Mohile (19) suggested that primary brain lymphoma is
a malignant tumor that is lesion-centered and destructive to the
surrounding area. Therefore, enhanced imaging of MRI is often
accompanied by significant enhancement. In this study, tumor
scanning by enhanced CT and MRI showed enhanced signal, which
supported the mass effects and invasive features of this disease.
Therefore, early diagnosis and treatment is needed, in order to
avoid the deterioration of primary brain lymphoma. For diagnosis
results of CT combined with MRI, diagnosis of primary brain
lymphoma is mainly based on meningioma-like melanoma signal. Mild
edema, obvious mass effect and big tumor body all meet the imaging
features of primary brain lymphoma. Therefore, mass effect may be
an indicator of primary brain lymphoma. CT, MRI and combine
diagnosis all achieved satisfactory diagnostic results, but are not
enough for the qualitative diagnosis of primary brain lymphoma.
Therefore, both clinical imaging results and pathological
examination results should be used in the diagnosis.
In this study, 230 patients with primary brain
lymphoma were studied, and the results of MRI and CT images were
analyzed, but there are still some shortcomings. The sample size
was small and experimental conditions were limited, and CT and MRI
detectors may have differences in image results. We will improve
those shortcomings in our future studies.
In conclusion, both CT and MRI can provide
satisfactory diagnosis for primary brain lymphoma, but pathological
examinations are always needed.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YQ and JZ conceived and designed the study. YQ, HL
and XW were responsible for the collection and analysis of the
data. AB, GZ and JZ interpreted the data and drafted the
manuscript. AB and JZ revised the manuscript critically for
important intellectual content. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
People's Hospital of Rizhao (Rizhao, China). Signed written
informed consents were obtained from the patients and/or
guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dolecek TA, Propp JM, Stroup NE and
Kruchko C: CBTRUS statistical report: Primary brain and central
nervous system tumors diagnosed in the United States in 2005–2009.
Neuro-oncol. 14 Suppl 5:v1–v49. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Korfel A, Thiel E, Martus P, Möhle R,
Griesinger F, Rauch M, Röth A, Hertenstein B, Fischer T,
Hundsberger T, et al: Randomized phase III study of whole-brain
radiotherapy for primary CNS lymphoma. Neurology. 84:1242–1248.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hoang-Xuan K, Bessell E, Bromberg J,
Hottinger AF, Preusser M, Rudà R, Schlegel U, Siegal T, Soussain C,
Abacioglu U, et al: European Association for Neuro-Oncology Task
Force on Primary CNS Lymphoma: Diagnosis and treatment of primary
CNS lymphoma in immunocompetent patients: Guidelines from the
European Association for Neuro-Oncology. Lancet Oncol.
16:e322–e332. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ferreri AJ, Cwynarski K, Pulczynski E,
Ponzoni M, Deckert M, Politi LS, Torri V, Fox CP, Rosée PL, Schorb
E, et al: International Extranodal Lymphoma Study Group (IELSG):
Chemoimmunotherapy with methotrexate, cytarabine, thiotepa, and
rituximab (MATRix regimen) in patients with primary CNS lymphoma:
Results of the first randomisation of the International Extranodal
Lymphoma Study Group-32 (IELSG32) phase 2 trial. Lancet Haematol.
3:e217–e227. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nayak L, Pentsova E and Batchelor TT:
Primary CNS lymphoma and neurologic complications of hematologic
malignancies. Continuum (Minneap Minn). 21:355–372. 2015.PubMed/NCBI
|
|
6
|
Omuro A, Correa DD, DeAngelis LM,
Moskowitz CH, Matasar MJ, Kaley TJ, Gavrilovic IT, Nolan C,
Pentsova E, Grommes CC, et al: R-MPV followed by high-dose
chemotherapy with TBC and autologous stem-cell transplant for newly
diagnosed primary CNS lymphoma. Blood. 125:1403–1410. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Touitou V, LeHoang P and Bodaghi B:
Primary CNS lymphoma. Curr Opin Ophthalmol. 26:526–533. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Houillier C, Choquet S, Touitou V,
Martin-Duverneuil N, Navarro S, Mokhtari K, Soussain C and
Hoang-Xuan K: Lenalidomide monotherapy as salvage treatment for
recurrent primary CNS lymphoma. Neurology. 84:325–326. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Omuro A, Chinot O, Taillandier L,
Ghesquieres H, Soussain C, Delwail V, Lamy T, Gressin R, Choquet S,
Soubeyran P, et al: Methotrexate and temozolomide versus
methotrexate, procarbazine, vincristine, and cytarabine for primary
CNS lymphoma in an elderly population: An intergroup ANOCEF-GOELAMS
randomised phase 2 trial. Lancet Haematol. 2:e251–e259. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Vater I, Montesinos-Rongen M, Schlesner M,
Haake A, Purschke F, Sprute R, Mettenmeyer N, Nazzal I, Nagel I,
Gutwein J, et al: The mutational pattern of primary lymphoma of the
central nervous system determined by whole-exome sequencing.
Leukemia. 29:677–685. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yahalom J, Illidge T, Specht L, Hoppe RT,
Li YX, Tsang R and Wirth A: International Lymphoma Radiation
Oncology Group: Modern radiation therapy for extranodal lymphomas:
Field and dose guidelines from the International Lymphoma Radiation
Oncology Group. Int J Radiat Oncol Biol Phys. 92:11–31. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jiang S, Yu H, Wang X, Lu S, Li Y, Feng L,
Zhang Y, Heo HY, Lee DH, Zhou J, et al: Molecular MRI
differentiation between primary central nervous system lymphomas
and high-grade gliomas using endogenous protein-based amide proton
transfer MR imaging at 3 Tesla. Eur Radiol. 26:64–71. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yamada S, Ishida Y, Matsuno A and Yamazaki
K: Primary diffuse large B-cell lymphomas of central nervous system
exhibit remarkably high prevalence of oncogenic MYD88 and CD79B
mutations. Leuk Lymphoma. 56:2141–2145. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kasenda B, Loeffler J, Illerhaus G,
Ferreri AJ, Rubenstein J and Batchelor TT: The role of whole brain
radiation in primary CNS lymphoma. Blood. 128:32–36. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Montesinos-Rongen M, Purschke FG, Brunn A,
May C, Nordhoff E, Marcus K and Deckert M: Primary central nervous
system (CNS) lymphoma B cell receptors recognize CNS proteins. J
Immunol. 195:1312–1319. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Mabray MC, Cohen BA, Villanueva-Meyer JE,
Valles FE, Barajas RF, Rubenstein JL and Cha S: Performance of
apparent diffusion coefficient values and conventional MRI features
in differentiating tumefactive demyelinating lesions from primary
brain neoplasms. AJR Am J Roentgenol. 205:1075–1085. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kasenda B, Ferreri AJ, Marturano E, Forst
D, Bromberg J, Ghesquieres H, Ferlay C, Blay JY, Hoang-Xuan K,
Pulczynski EJ, et al: First-line treatment and outcome of elderly
patients with primary central nervous system lymphoma (PCNSL) - a
systematic review and individual patient data meta-analysis. Ann
Oncol. 26:1305–1313. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Welch MR, Sauter CS, Matasar MJ, Faivre G,
Weaver SA, Moskowitz CH and Omuro AM: Autologous stem cell
transplant in recurrent or refractory primary or secondary central
nervous system lymphoma using thiotepa, busulfan and
cyclophosphamide. Leuk Lymphoma. 56:361–367. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Patrick LB and Mohile NA: Advances in
primary central nervous System lymphoma. Curr Oncol Rep. 17:602015.
View Article : Google Scholar : PubMed/NCBI
|