Introduction
Exposure to tobacco, dietary habits, occupational
carcinogens, environmental pollutions and the characteristics of
host are factors that have played an increasingly important role in
the high lung cancer incidence in at least the last 50 years,
making this disease the most common cause for cancer-related
mortality (1). In China, the
mortality rate of lung cancer ranks first in various types of
malignant tumors (2). Nevertheless,
the early detection rate of lung cancer is gradually on the
increase with the development of early screening techniques of lung
cancer and the enhancement in the consciousness of physical
examination of residents.
According to the survey of US medical care insurance
surveillance systems, no distant metastasis of tumor was identified
in the first diagnosis of over 40% of lung cancer patients
(3). Surgery is considered the main
method for the treatment of non-small cell lung cancer at the early
stage, but the application of conventional thoracotomy is limited
by long surgery incision, severe injuries to the thoracic muscle,
heavy damage to postoperative pulmonary functions, a variety of
complications, which have become the major causes for patients
succumbing to the disease during the perioperative period (4). Ever since the application of the
thoracoscope for thoracic surgery in the late 20th century, the
minimally invasive technique, with the advantages, including small
incision, slight injury and rapid postoperative recovery, has been
employed in many research domains of thoracic surgery (5). Furthermore, after the concept of
‘Precision Medicine’ was suggested, this technique has been widely
applied in the treatment of lung cancer at early stage (6).
In the present study, we performed minimally
invasive segmentectomy for the treatment of lung cancer at early
stage to investigate the clinical safety and efficacy of this
technique, thereby providing more appropriate procedures for lung
cancer patients at early stage. The results corroborate the
efficacy and safety of this technique.
Materials and methods
General material
We selected 86 lung cancer patients at early stage
who were admitted to the Affiliated Central Hospital of Qingdao
University (Qingdao, China) for treatment between May 2010 and
December 2010. Based on the random number table, the patients were
randomly divided into the control (n=43) and observation (n=43)
groups. Inclusion criteria for the study were: i) Patients who were
diagnosed as having lung cancer at early stage via computed
tomography and pathological examination; ii) patients who had not
received any prior surgery, chemotherapy or radiotherapy; and iii)
patients who provided written informed consent. Exclusion criteria
for the study were: i) Patients with abnormal coagulation function
or with a clinical stage above stage IIIa; and ii) patients with a
history of thoracotomy or metastasis in hilar or mediastinal lymph
nodes, or distant metastasis. No statistically significant
difference was identified in comparison of the general material of
patients between the two groups (P>0.05; Table I). This study was approved by the
Ethics Committee of The Affiliated Central Hospital of Qingdao
University and informed consents were signed by the patients and/or
guardians.
 | Table I.Comparison of the general material of
patients between the two groups. |
Table I.
Comparison of the general material of
patients between the two groups.
| Items | Control group
(n=43) | Observation group
(n=43) | t/χ2 | P-value |
|---|
| Sex
(male/female) | 26/17 | 25/18 | 0.048 | 0.826 |
| Age (years) | 40–70 | 40–75 |
|
|
| Average age
(years) | 56.69±7.49 | 55.59±7.58 | 0.677 | 0.500 |
| Smoking (n, %) |
|
|
|
|
|
Cigarettes ≥5 | 21 (48.84) | 19 (44.19) | 0.193 | 0.908 |
|
Cigarettes <5 | 8 (18.60) | 9 (20.93) |
|
|
| Non-smoker | 14 (32.56) | 15 (34.88) |
|
|
Preoperative preparation
In the two groups, patients received regular
examinations prior to surgery to eliminate any surgical
contradictions. Two weeks prior to operation, the patients were
required to discontinue smoking, fasting was required for patients
at 6 h before operation, and at 4 h before operation, the patients
were required to take 300–400 ml 10% glucose injection via drinking
or injection.
Treatment
Patients in the two groups received endotracheal
intubation for intravenous anesthesia, during which the arterial
blood gases, arterial blood pressure, pulse and electrocardiogram
were monitored. For patients in the control group, conventional
thoracotomy was performed as treatment. With patients in the
lateral position, an incision was made on the posterolateral site
to expose the thoracic cavity layer by layer. After dissection of
the mediastinal lymph nodes, the patients underwent regular
lobectomy, during which unnecessary squeeze or pull of normal lung
tissues was avoided during surgery. After the operation, the
thoracic cavity was rinsed using warm saline, the residual ends of
lung and bronchus were examined to identify air leakage, and the
drainage tube was left in the cavity followed by suturing the
incisions.
In the observation group, patients in the lateral
position underwent video-assisted thoracoscopic segmentectomy as
treatment. After regular disinfection, the patients were required
to lie on the operating drape, and an incision of approximately 1
cm long was made between the 7th and 8th ribs along the midaxillary
line on the affected side as the observation hole, the main
operation hole was prepared through the incision (approximately 3
cm in length) between the 4th and 5th ribs along the anterior
axillary line, and the auxiliary operation hole was prepared
through the incision (approximately 1 cm in length) in the 8th rib
along the scapular line. After the thoracoscope was placed, we
observed the thoracic cavity, and performed the segmentectomy for
different pulmonary segments, such as left superior pulmonary
segment, lingual segment, anterior segment of right superior lung,
apex and dorsal and posterior segments of right superior lung.
Subsequently, mediastinal lymph nodes were dissected and the
procedures conducted during the operation were guided via video.
Following surgery, we examined the dilation of residual lung, and
air leakages in the residual ends of lung and bronchus. The
drainage tube was then placed through the observation hole, and the
incision was sutured.
Detection of CRP, IL-6 and −10 levels
in serum
In the two groups, we extracted 3–5 ml fasting
peripheral venous blood in the morning before operation and on the
3rd, 5th and 7th days after operation. Samples were centrifuged for
15 min at 1,000 × g, and the supernatant was placed in an Eppendorf
tube for preservation in a refrigerator at −20°C. C-reaction
protein (CRP), interleukin (IL) −6 and −10 levels in serum were
detected via enzyme-linked immunosorbent assay (ELISA), in which
the relevant kits were purchased from Shanghai Haoben Biotechnology
Co., Ltd., (Shanghai, China) and all the procedures were in
accordance with the manufacturer's instructions. Optical density
was read by a microplate reader (Thermo Fisher Scientific, Waltham,
MA, USA), with which the corresponding levels of CRP, IL-6 and
IL-10 in samples were calculated.
Postoperative treatment and
follow-up
Following surgery, patients in the two groups
received regular treatment, such as antibiotics and aerosol
inhalation. After the drainage tubes were removed, re-examinations
were carried out through the chest X-ray images. After being
discharged, the patients received 5-year follow-up as follows: i)
Once every 3 months in the first two years; ii) once every 6 months
in the 2nd and 3rd years; and iii) once every year in the 4th and
5th years. During follow-up, we observed the recurrence and
survival rate of patients.
Evaluation indexes
The intraoperative bleeding amount, quantity of
dissected lymph nodes, postoperative intubation time and length of
stay (LOS) were recorded, and the incidence of postoperative
complications, including the recordings of incidence rate of
intraoperative bleeding amount, persistent air leakage (>1
week), and postoperative arrhythmia and atelectasis were
compared.
The visual analogue scale was used for evaluating
the pain of patients within a range of 0–10 points (0 point for no
pain, and 10 points for intolerable acute pain), and the evaluation
criteria were set as: i) Grade I: score between 0 and 2 points for
no or imperceptible pain; ii) grade II: score between 3 and 5
points for tolerable pain; iii) grade III: score between 6 and 8
points for obvious pain that affected regular activities; and iv)
grade IV: score ≥8 points for intolerable pain.
Prior to operation and on the 3rd, 5th and 7th days
after operation, 5 ml fasting venous blood was collected from the
patients for isolation and extraction of serum, and the levels of
CRP, IL-6 and −10 in serum were detected via ELISA. Three months
after operation, we examined the pulmonary functions of patients,
including the indexes: forced vital capacity (FVC), forced
expiratory volume in one second (FEV1), FEV1/FVC and maximal
expiratory flow rate.
During the 5-year follow-up, we carried out
statistics on the recurrence rate, disease-free survival (DFS), and
5-year survival rate, in which the DFS started from the 1st day
after the operation and ended at the time of initial recurrence or
metastasis. In addition, for patients with no recurrence or
metastasis during the 5-year follow-up, this period was considered
as 5 years.
Statistical analysis
SPSS 19.0 (IBM Corp., Armonk, NY, USA) was employed
for data processing. Measurement data were presented as mean ±
standard deviation (false), and the Kaplan-Meier test was carried
out for intergroup comparison. Countable data were presented as
rate, and χ2 test was performed. P<0.05 was
considered to indicate a statistically significant difference.
Results
Comparison of surgical condition of
patients between the two groups
A comparison of surgical conditions of patients
between the two groups showed that the surgery duration,
postoperative intubation time and LOS were shorter than those in
the control group, and the intraoperative bleeding amount of
patients were significantly lower than that in the control group
(P<0.05). However, no significant difference was detected in a
comparison of the number of dissected lymph nodes of patients
between the two groups (P>0.05; Table
II).
 | Table II.Comparison of surgery condition of
patients between the two groups. |
Table II.
Comparison of surgery condition of
patients between the two groups.
| Groups | Observation group
(n=43) | Control group
(n=43) | t-test | P-value |
|---|
| Surgery duration
(min) | 123.24±8.65 |
163.56±9.72 | 20.320 | <0.001 |
| Intraoperative
bleeding amount (ml) | 226.48±108.35 | 349.58±107.47 | 5.289 | <0.001 |
| Intubation time
(days) | 3.47±1.15 | 6.64±1.26 | 12.185 | <0.001 |
| Quantity of dissected
lymph nodes (n) | 7.35±1.28 | 7.68±1.36 | 1.159 | 0.250 |
| LOS (days) | 9.35±3.28 | 16.68±3.36 | 10.237 | <0.001 |
Comparison of postoperative pain rate
between the two groups
A comparison of the postoperative pain degree of
patients between the two groups showed that in the observation
group, patients suffered less pain following surgery than those in
the control group, with a statistically significant difference
(P<0.05; Table III).
 | Table III.Comparison of postoperative pain rate
of patients between the two groups. |
Table III.
Comparison of postoperative pain rate
of patients between the two groups.
| Groups | Cases | Grade I | Grade II | Grade III | Grade IV |
|---|
| Observation | 43 | 31 (72.09) | 9 (20.93) | 3 (6.98) | 0 (0.00) |
| Control | 43 | 16 (37.21) | 12 (27.91) | 11 (25.58) | 4 (9.30) |
| χ2 |
| 13.787 |
|
|
|
| P-value |
| 0.003 |
|
|
|
Comparison of CRP, IL-6 and −10 level
in patients between the two groups
We compared the CRP level of patients between the
two groups, and found that before operation, there were no
significant differences (P>0.05). By contrast, on the 3rd, 5th
and 7th days after operation, the CRP levels in the observation
group were significantly lower than those in the control group
(P<0.05; Table IV).
 | Table IV.Comparison of CRP level in patients
between the two groups (mg/l). |
Table IV.
Comparison of CRP level in patients
between the two groups (mg/l).
| Groups | Cases | Before operation | On the 3rd day after
operation | On the 5th day after
operation | On the 7th day after
operation |
|---|
| Observation | 43 | 3.43±1.24 | 39.67±3.23 | 25.35±3.28 | 18.68±3.24 |
| Control | 43 | 3.62±1.58 | 57.27±3.64 | 46.47±3.36 | 32.83±3.78 |
| t-test |
| 0.620 | 23.716 | 29.495 | 18.637 |
| P-value |
| 0.537 | <0.001 | <0.001 | <0.001 |
We compared the IL-6 levels of patients between the
two groups, and found that before operation, there were no
significant differences (P>0.05). By contrast, on the 3rd, 5th
and 7th days after operation, the IL-6 levels in the observation
group were significantly lower than those in the control group
(P<0.05; Table V).
 | Table V.Comparison of IL-6 level in patients
between the two groups (ng/l). |
Table V.
Comparison of IL-6 level in patients
between the two groups (ng/l).
| Groups | Cases | Before operation | On the 3rd day after
operation | On the 5th day after
operation | On the 7th day after
operation |
|---|
| Observation | 43 | 46.43±3.24 | 121.67±7.23 | 106.35±5.25 | 78.67±3.23 |
| Control | 43 | 47.62±3.58 | 137.27±7.64 | 126.45±5.32 | 96.82±3.79 |
| t-test |
| 1.616 | 9.725 | 17.634 | 23.901 |
| P-value |
| 0.110 | <0.001 | <0.001 | <0.001 |
We compared the IL-10 levels of patients between the
two groups, and found that before surgery, there was no significant
difference (P>0.05). By contrast, on the 3rd, 5th and 7th days
after operation, the level of IL-10 in the observation group was
significantly lower than those in the control group (P<0.05;
Table VI).
 | Table VI.Comparison of IL-10 level in patients
between the two groups (ng/l). |
Table VI.
Comparison of IL-10 level in patients
between the two groups (ng/l).
| Groups | Cases | Before
operation | On the 3rd day
after operation | On the 5th day
after operation | On the 7th day
after operation |
|---|
| Observation | 43 | 45.75±3.25 | 122.64±6.28 | 106.36±4.27 | 73.52±3.16 |
| Control | 43 | 46.82±3.57 | 138.56±6.63 | 125.47±5.36 | 97.56±3.74 |
| t-test |
| 1.453 | 11.432 | 18.286 | 32.196 |
| P-value |
| 0.150 | <0.001 | <0.001 | <0.001 |
Comparison of adverse reactions,
postoperative pulmonary functions, and the recurrence and survival
rates of patients between the two groups
A comparison of the incidence rate of postoperative
complications of patients in the two groups showed that following
surgery, the incidence rate of complications [postoperative
bleeding amount, persistent air leakage (>1 week), postoperative
arrhythmia and atelectasis] in the observation group was 6.98%,
which was significantly lower than that in the control group
(30.23%) (P<0.05; Table
VII).
 | Table VII.Comparison of adverse reactions of
patients between the two groups (n,%). |
Table VII.
Comparison of adverse reactions of
patients between the two groups (n,%).
| Groups | Cases | Intraoperative
bleeding amount | Persistent air
leakage | Postoperative
arrhythmia | Atelectasis | Total |
|---|
| Observation | 43 | 1 (2.33) | 0 (0) | 1 (2.33) | 1 (2.33) | 3 (6.98) |
| Control | 43 | 4 (9.30) | 3 (6.98) | 2 (4.65) | 4 (9.30) | 13 (30.23) |
| χ2 |
| 6.202 |
|
|
|
|
| P-value |
| 0.012 | <0.001 |
|
|
|
Comparison on postoperative pulmonary functions of
patients between the two groups revealed that the FVC, FEV1,
FEV1/FVC and PEER in the observation group were all significantly
higher than those in the control group (P<0.05; Table VIII).
 | Table VIII.Comparison of pulmonary function
indexes of patients between the two groups. |
Table VIII.
Comparison of pulmonary function
indexes of patients between the two groups.
| Groups | Cases (n) | FEV 1 (%) | PEER (l/sec) | FEV1/FVC (%) | FVC (l) |
|---|
| Control | 43 | 66.23±4.02 | 3.41±1.24 | 2.15±0.33 | 1.75±0.64 |
| Observation | 43 | 71.75±4.56 | 4.26±1.36 | 2.56±0.35 | 2.19±0.73 |
| t-test |
| 5.954 | 3.029 | 5.589 | 2.972 |
| P-value |
| <0.001 | 0.003 | <0.001 | 0.004 |
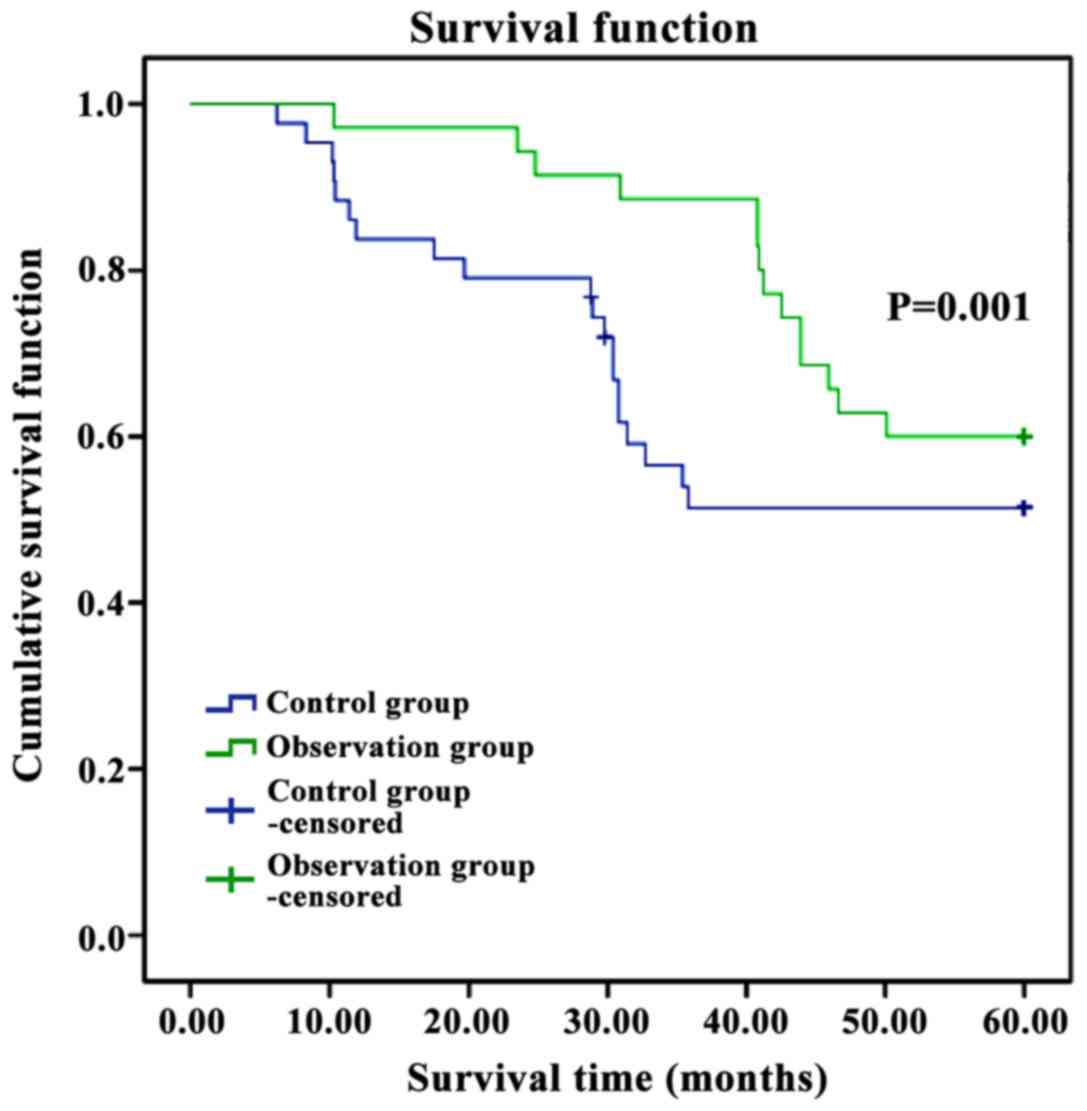
We compared the recurrence and survival rates of
patients between the two groups, and found that the average
survival period in the observation group was significantly longer
than that in the control group, the recurrence rate was
significantly lower than that in the control group, and the
postoperative 5-year survival rate was significantly higher than
that in the control group (P<0.05; Table IX and Fig.
1).
 | Table IX.Comparison of 5-year follow-up of
patients between the two groups. |
Table IX.
Comparison of 5-year follow-up of
patients between the two groups.
| Groups | Cases | 5-year survival (n,
%) | Recurrence rate (n,
%) | Average survival
period (months) |
|---|
| Observation | 43 | 31 (72.09) | 2 (4.65) | 48.56±7.48 |
| Control | 43 | 21 (48.83) | 8 (18.60) | 41.64±7.53 |
|
t/χ2 |
| 4.864 | 4.074 | 4.152 |
| P-value |
| 0.027 | 0.044 | 0.001 |
Discussion
The incidence and mortality rates of lung cancer are
on the increase worldwide. In many countries, lung cancer has
become the primary malignant tumor and poses a threat to the health
of human beings (7). The clinical
manifestations of lung cancer are not obvious at early stage, but
when it comes to advanced stage, symptoms, generally including
fever, weight loss, coughing, chest pains, blood-stained sputum,
hemoptysis, chest distress and short of breath, emerges at the
advanced stage, which are relatively acute in elderly patients
(8). At the middle and advanced
stages, patients with lung cancer may suffer from direct, lymphatic
or hematogenous metastasis, and poor prognosis, leading to a
significant decrease in the patient survival rate (9). However, with the enhancement in the
consciousness on healthcare and the development in imaging
techniques, the detection rate of lung cancer at an early stage is
also on the increase. The present and previous findings (10) have shown that the 5-year survival rate
of lung cancer patients in stages IA, IB, IIA and IIB who underwent
surgery as treatment may be increased from 50 to 80%. Thus, early
diagnosis and treatment are of great significance for lung
cancer.
Conventional thoracotomy is generally applied in the
treatment of lung cancer, but its application has been limited by
larger surgical incision, more significant postoperative pain and
additional complications (11). In
previous years, continuous improvement and updates have been
observed in surgical and anesthetic techniques and the equipment in
thoracic surgeries, and an increasing number of surgical methods
have been applied in the treatment of lung cancer, especially the
increasingly mature minimally invasive technique (12). At the same time, adverse effects on
patients are markedly reduced (12).
The results of the present study showed that
duration of surgery, intubation time and LOS of patients in the
observation group were significantly shorter than those in the
control group, the intraoperative bleeding amount was also
significantly lower than that in the control group, and the pain
rate of patients in the observation group was significantly reduced
when compared with the control group, suggesting that the degree of
pain in patients was significantly ameliorated (P<0.05).
Additionally, there was no significant difference in a comparison
of the quantity of lymph nodes that were dissected in the operation
for the two groups (P>0.05). This was because in the operation
conducted using conventional thoracotomy the major muscular tissues
of patients (e.g., the musculus serratus anterior and the
latissimus dorsi) were excised, thus enlarging surgical incision,
further increasing the intraoperative bleeding amount. By contrast,
the rib cage was distracted using a rib retractor, which would
generate larger trauma and stimulation to patients, thus
significantly aggravating the degree of pain of patients following
surgery. However, compared with the conventional thoracotomy,
surgeries guided via video provide surgeons with an amplified
surgery image through a smaller incision. Consequently, through
utilization of video imaging, surgeons were better able to identify
the lymph nodes and tiny veins allowing for more efficient
isolation and ligation of the microstructures via a smaller
incision without any unnecessary damage, and dissect the lymph
nodes in deep sites thoroughly, thus reaching similar dissection
efficiency with the conventional thoracotomy. Additionally,
minimally invasive surgery could save the time for opening and
closing the thoracic cavity, allowing for surgery time to be
significantly shortened (13).
Surgical treatment may induce stress responses of
lung cancer patients, sequentially resulting in the changes in
catechol, and the immunosuppression may be induced to activate the
large section of cytokines, thus causing inflammatory responses
(14). CRP is a kind of acute phase
reactive protein, and usually serves as an index for inflammatory
responses in clinical practice. By binding chromatin, it can
activate the complement system to enhance the leukocyte phagocytic
function, and exert a regulatory effect by activating the cells
(15). Under normal circumstances,
the content of CRP is usually very low, but when it comes to
injuries, its concentration is markedly increased. Thus, it can be
frequently detected in patients after operation (16). As a member of hte interleukin family,
IL-6 is a kind of reactive lymphocyte factor in the acute phase and
plays diversified roles in immune responses (17). Stress responses in the surgeries of
lung cancer affect the activities of macrophages and T cells, thus
promoting the secretion and generation of IL-6, which can suppress
the immune functions and initiate the defensive reactions, thus
exerting bi-directional effects (18). IL-10, as another member in the
interleukin family, suppresses the activity of natural killer
cells, which aids the tumor cells to escape from the surveillance
of immune system. Under normal circumstances, IL-10 is at a low
level, but after lobectomy, its concentration is elevated to a high
level (19). The results of the
present study showed that there were no statistically significant
differences in a comparison of CRP, IL-6 and −10 levels before
operation, but on the 3rd, 5th and 7th days after operation, we
found that the levels of CRP, IL-6 and −10 in patients in the
observation group were significantly higher than those before the
operation, but the levels in the observation were significantly
lower than those in the control group, and the incidence rate of
postoperative complications of patients in the observation was
significantly lower than that in the control group (P<0.05).
Compared with conventional thoracotomy, the minimally invasive
segmentectomy generates fewer traumas and induces slighter stress
responses in surgery, which may result in relatively slight
reactions in the activated immune system. Thus, a release of
cytokines, such as CRP, IL-6 and −10, may sustain a low level.
Minimally invasive surgeries generate less postoperative pain, and
scarcely hinder the recovery of patients, leading to a decrease in
the incidence rate of complications.
The results of the present study showed that FVC,
FEV1, FEV1/FVC and PEER of patients in the observation group after
operation were significantly higher than those in the control group
(P<0.05). This is because conventional thoracotomy may generate
extensive injuries to muscles on the chest wall, severely affecting
the activity of chest muscles. In addition, oppressions on lung can
hardly be avoided in the operation, thus resulting in the contusion
and edema in respiratory membrane. Moreover, postoperative cough
and breath of patients may cause pain in incisions, while the
practice of breath functions may decrease the compliance of
patients. These factors contribute to a slow recovery in pulmonary
function. With the assistance of video, microstructures in the
thoracoscopic segmentectomy can be amplified. Thus, surgeons can
avoid injuries to the lung, which can effectively protect the
pulmonary function and promote the postoperative recovery of
patients (20). With smaller
incisions, slighter inflammatory responses and immunosuppression,
and less effect on the immune functions, minimally invasive
surgeries can significantly increase the survival rate and survival
period of patients after operation.
In conclusion, compared with conventional
thoracotomy, minimally invasive segmentectomy, with the advantages
such as smaller incisions, rapid recovery of patient after
operation, and less effect on the pulmonary function, is superior
in safety and effectiveness. Thus, it is of important value in the
surgical treatment of lung cancer at early stage.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors contributions
CS contributed significantly to writing the
manuscript and preoperative preparation. CZ detected and analyzed
CRP, IL-6 and IL-10 levels in serum. WY and YS helped postoperative
treatment and follow-up. ZZ contributed significantly to manuscript
preparation, the conception of the study and statistical analysis.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
The Affiliated Central Hospital of Qingdao University (Qingdao,
China) and informed consents were signed by the patients and/or
guardians.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Travis WD, Travis LB and Devesa SS: Lung
cancer. Cancer. 75:191–202. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Del Vescovo V and Denti MA: microRNA and
lung cancer. Adv Exp Med Biol. 889:153–177. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Howlader N, Noone AM, Krapcho M, Miller D,
Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, et al:
SEER Cancer Statistics Review, 1975–2014National Cancer Institute;
Bethesda, Md: http://seer.cancer.gov/csr/1975_2014based on
November 2016 SEER data submission posted to the SEER web site.
April. 2017
|
|
4
|
Puri V, Patel A, Majumder K, Bell JM,
Crabtree TD, Krupnick AS, Kreisel D, Broderick SR, Patterson GA and
Meyers BF: Intraoperative conversion from video-assisted
thoracoscopic surgery lobectomy to open thoracotomy: A study of
causes and implications. J Thorac Cardiovasc Surg. 149:55–61. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yu PS, Capili F and Ng CS: Single port
VATS: Recent developments in Asia. J Thorac Dis. 8:302–307.
2016.
|
|
6
|
Klapper J and D'Amico TA: VATS versus open
surgery for lung cancer resection: Moving toward a minimally
invasive approach. J Natl Compr Canc Netw. 13:162–164. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Cooper WA: Preface-molecular genetics of
lung cancer. Transl Lung Cancer Res. 4:1092015.PubMed/NCBI
|
|
8
|
Mohamed SAA, Mousa EM, Hamed AM, Amin SE
and Abdel Aziz NMA: Utility of multidetector row computed
tomography and virtual bronchoscopy in evaluation of hemoptysis due
to lung cancer. Egypt J Chest Dis Tuberc. 65:279–287. 2016.
View Article : Google Scholar
|
|
9
|
Lin L, Gu ZT, Chen WH and Cao KJ:
Increased expression of the long non-coding RNA ANRIL promotes lung
cancer cell metastasis and correlates with poor prognosis. Diagn
Pathol. 10:14–21. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yu JB, Soulos PR, Cramer LD, Decker RH,
Kim AW and Gross CP: Comparative effectiveness of surgery and
radiosurgery for stage I non-small cell lung cancer. Cancer.
121:2341–2349. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pan TW, Wu B, Xu ZF, Zhao XW and Zhong L:
Video-assisted thoracic surgery versus thoracotomy for
non-small-cell lung cancer. Asian Pac J Cancer Prev. 13:447–450.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Laursen LØ, Petersen RH, Hansen HJ, Jensen
TK, Ravn J and Kongea L: Video-assisted thoracoscopic surgery
lobectomy for lung cancer is associated with a lower 30-day
morbidity compared with lobectomy by thoracotomy. Eur J
Cardiothorac Surg. 49:870–875. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu C, Li Z, Bai C, Wang L, Shi X and Song
Y: Video-assisted thoracoscopic surgery and thoracotomy during
lobectomy for clinical stage I non-small-cell lung cancer have
equivalent oncological outcomes: A single-center experience of 212
consecutive resections. Oncol Lett. 9:1364–1372. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gelalis ID, Arnaoutoglou CM, Politis AN,
Batzaleksis NA, Katonis PG and Xenakis TA: Bacterial wound
contamination during simple and complex spinal procedures. A
prospective clinical study. Spine J. 11:1042–1048. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li SF, Hu YW, Zhao JY, Ma X, Wu SG, Lu JB,
Hu YR, Wang YC, Gao JJ, Sha YH, et al: Ox-LDL upregulates CRP
expression through the IGF2 pathway in THP-1 macrophages.
Inflammation. 38:576–583. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Waterland P, Ng J, Jones A, Broadley G,
Nicol D, Patel H and Pandey S: Using CRP to predict anastomotic
leakage after open and laparoscopic colorectal surgery: Is there a
difference? Int J Colorectal Dis. 31:861–868. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hunter CA and Jones SA: IL-6 as a keystone
cytokine in health and disease. Nat Immunol. 16:448–457. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gomes M, Coelho A, Araújo A, Azevedo A,
Teixeira ALO, Catarino R and Medeiros R: IL-6 polymorphism in
non-small cell lung cancer: A prognostic value? Tumour Biol.
36:3679–3684. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang YM, Mao YM and Sun YX: Genetic
polymorphisms of IL-6 and IL-10 genes correlate with lung cancer in
never-smoking Han population in China. Int J Clin Exp Med.
8:1051–1058. 2015.PubMed/NCBI
|
|
20
|
Goto T, Kadota Y, Mori T, Yamashita S,
Horio H, Nagayasu T and Iwasaki A: Video-assisted thoracic surgery
for pneumothorax: Republication of a systematic review and a
proposal by the guideline committee of the Japanese association for
chest surgery 2014. Gen Thorac Cardiovasc Surg. 63:8–13. 2015.
View Article : Google Scholar : PubMed/NCBI
|