Introduction
Abdominal aortic aneurysm (AAA) refers to the local
permanent expansion of the aorta, and is defined as an aortic
diameter >1.5 times larger than the normal value (typically
>3 cm). Aortectasia refers to the local expansion of the aorta
with a diameter <1.5 times of the normal value (1). The morbidity of AAA for individuals
>65 years is up to 9% (2). The
majority of arterial aneurysms are asymptomatic; however, damage to
the vascular structure of the aorta subsequent to aneurysm will
lead to an increase in the aorta tube diameter (3). If the diameter is >5.5 cm, it is
likely to eventually rupture; the risk of aortoclasia is associated
with the diameter size (4). The
prognosis for AAA ruptures remains poor, with a mortality rate of
80–90% (4). The primary therapeutic
strategy for AAA with a diameter >5.5 cm includes surgery and
intracavitary interventional treatment (5). However, for AAA with a diameter <5.5
cm, no effective therapy option is available (5).
Inflammatory cell infiltration is a critical event
in the formation of AAA. Inflammatory cells may secrete a large
number of inflammatory cytokines, chemokines, chemotaxis cytokines,
leukotrienes, reactive oxygen species (ROS) and immunoglobulins
(6). The vasa vasorum of the aorta is
the channel for inflammatory cell intrusion into the aortic intima
and membrane (6). Mesolamella
neovascularization formation and vascular smooth muscle cell
reduction are characteristics of AAA (7). An intraluminal thrombus may induce
neovascularization and inflammation by inducing hypoxia in the
endometrium and membrane. Inflammatory cells in the thrombus may
release proteases, including matrix metalloproteinase 9 (MMP-9) and
urokinase-type fibrinolytic enzymes (8). Inflammation of AAA is primarily induced
by cytokines expressed by type 2 T helper cells (8); however, there may also be cytokines from
type 1 T helper cells (8). In
addition, ROS and reactive nitrogen species function in a number of
types of chronic disease. An increase in ROS is associated with a
local inflammatory reaction that may lead to cell and tissue
damage, i.e. oxidative stress (9). A
previous study demonstrated the effects of oxidative stress on the
pathogenesis of AAA (9).
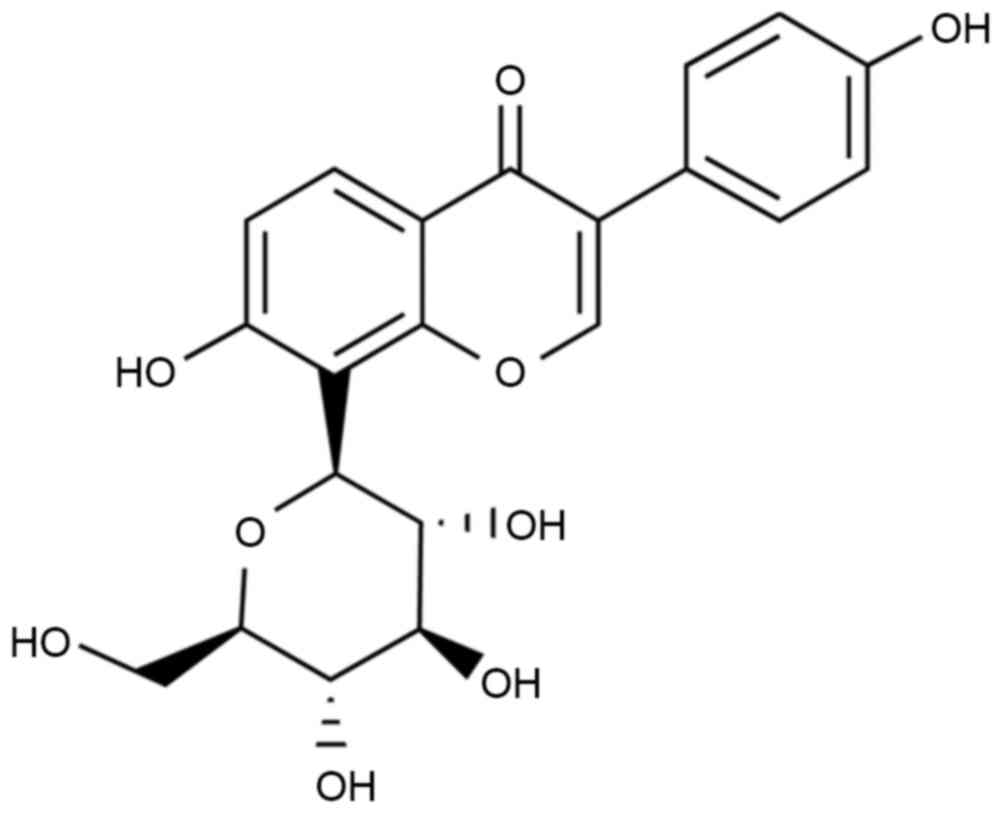
Puerarin (Fig. 1) is
an active ingredient abundant in Pueraria lobata (10). Puerarin demonstrates a variety of
pharmacological activities and specific pesticide effects; in
particular, puerarin has demonstrated efficacy in the treatment of
cardiovascular and cerebrovascular diseases (11). Puerarin is a promising medicine with
the potential for a variety of clinical applications, as is
effective despite low toxicity and few side effects (12). A previous study demonstrated that
puerarin exerts an endothelium-dependent dilation effect (12). Puerarin mediated ion channels in
smooth muscle cells have been demonstrated to improve its water
solubility and lipid solubility, enhance combination capacity
between drugs and hemoglobin, reduce drug polarity, improve oral
bioavailability and drug targeting effects (13,14).
In the present study, it was examined whether
puerarin exhibited an anti-inflammation effect. The results of the
present study demonstrated that puerarin significantly inhibited
cell growth in angiotensin II (angII)-induced aortic aneurysm
formation by activating reduced nicotinamide-adenine dinucleotide
phosphate (NADPH) oxidase and oxidative stress-induced activator
protein 1 (AP-1) signaling pathways.
Materials and methods
Ethical statement and animals
C57BL/6 background mice (n=24, male, 5–6 weeks,
20–22 g) were obtained from the Experiment Center of The First
Affiliated Hospital of Guangzhou Medical University (Guangzhou,
China) and housed at 22–24°C, 55–60% humidity, 12 h light/dark
cycle, and free access to food and water. All mice were randomly
divided into the following 4 experimental groups: Sham (n=6), angII
model (n=6), 100 mg/kg puerarin treatment (n=6) and 200 mg/kg
puerarin treatment (n=6) groups. Mice from the angII model, 100
mg/kg puerarin treatment and 200 mg/kg puerarin treatment groups
were continuously treated with angII (1,000 ng/kg/min) for 4 weeks,
as previously described (15). From
the third week onwards, mice from the 100 and 200 mg/kg puerarin
treatment groups were continuously administered with 100 or 200
mg/kg puerarin for 2 weeks, respectively. All protocols in the
present study were approved by the Ethics Committee of the Hainan
Provincial People's Hospital (Guangzhou, China). Following
treatment with puerarin, mice were anesthetizated using 35 mg/kg
pentobarbital sodium, and then sacrificed using decollation. The
tissue of aortic aneurysm was acquired and stored at −80°C.
Determination of the activity of NADPH
oxidase
Proteins were extracted from isolated abdominal
aortic tissues homogenized using PTN50 buffer (50 mM
Na3PO4, pH 7.4, 50 mM NaCl and 1% Triton
X-100) with protease inhibitors (cat. no. P8340; Sigma-Aldrich;
Merck KGaA, Darmstadt, Germany) at 4°C for 15 min. A bicinchoninic
acid (BCA) kit (Pierce; Thermo Fisher Scientific, Inc., Waltham,
MA, USA) was used to determine protein concentration. NADPH oxidase
activity was assessed using a NADPH oxidase activity kit (catalog
no. A127, Nanjing Jiancheng Biology Engineering Institute) in a
50-mmol/l phosphate buffer (pH 7.0) containing 100 µmol/l NADPH as
the substrate. Photoemissions were then detected using the Lumat
LB9507 luminometer (Berthold Technologies GmbH & Co. KG, Bad
Wildbad, Germany).
Detection of ROS production
Isolated abdominal aortic tissues were homogenized
with a homogenizer for 20 sec in 2 ml RIPA assay (Beyotime
Institute of Biotechnology, Nanjing, China). An aliquot of
2′7′-dichlorodihydroflurescein diacetate (25 µmol/l) was added to
the homogenates and ROS production was determined by absorbance at
530 nm using an ELISA plate reader (Bio-Rad Laboratories, Inc.,
Hercules, CA, USA).
Western blot analysis
Proteins were extracted from isolated abdominal
aortic tissues homogenized using PTN50 buffer with protease
inhibitors, as previously described. The BCA kit was used to
determine protein concentration. A total of 60 µg protein/lane was
separated using 12% SDS-PAGE and transferred to a polyvinylidene
difluoride membrane (Invitrogen; Thermo Fisher Scientific, Inc.).
The membrane was blocked using 5% skimmed milk in PBS-Tween-20
(0.05%) for 1 h at 37°C and immunoblotted using anti-MMP-2
(sc-10736; dilution, 1:3,000), anti-AP-1 (sc-52; dilution,
1:3,000), and anti-β-actin (dilution, 1:3,000; all Santa Cruz
Biotechnology, Inc., Dallas, TX, USA) and anti-phosphorylated-Jun
(p-Jun; 3270; dilution, 1:4,000; Cell Signaling Technology, Inc.,
Danvers, MA, USA) antibodies overnight at 4°C. Subsequently, the
membrane was incubated with horseradish peroxidase-conjugated
rabbit anti-goat secondary antibody (sc-2004 dilution, 1:5,000;
Santa Cruz Biotechnology, Inc.) at 37°C for 1 h, detected using an
enhanced chemiluminescence substrate (GE Healthcare, Chicago, IL,
USA) and analyzed using Image Lab version 3.0 (Bio-Rad
Laboratories, Inc., Hercules, CA, USA).
Cell culture and proliferation
Murine hemangioendothelioma (EOMA) cells were
obtained from the Shanghai Cell Bank (Shanghai, China) and cultured
with Dulbecco's modified Eagle's medium (Thermo Fisher Scientific,
Inc.) containing 10% fetal bovine serum (Thermo Fisher Scientific,
Inc.) at 37°C in an atmosphere containing 5% CO2. EOMA
cells were plated at 3,000 cells/well in 96-well plates and
cultured with dimethyl sulfoxide (DMSO; Thermo Fisher Scientific,
Inc.), 50, 100 or 200 µM puerarin for 0, 24 or 48 h. Subsequently,
150 µl MTT (Thermo Fisher Scientific, Inc.) was added to each well
and incubated at room temperature for 4 h. The medium was removed
and 200 µl of DMSO (Thermo Fisher Scientific, Inc.) was added into
each well for 20 min to dissolve formazan. The cell viability rate
was determined at 490 nm using an ELISA plate reader.
Apoptosis rate determination
EOMA cells were plated at 1×106
cells/well in 6-well plates and cultured with DMSO, or 50, 100 or
200 µM puerarin for 48 h. EOMA cells were stained with 10 µl
annexin V-allophycocyanin (eBioscience; Thermo Fisher Scientific,
Inc.) and 5 µl propidium iodide at room temperature in the dark for
30 min. The rate of apoptosis was determined using flow cytometry
(EPICS® ALTRA™; Beckman Coulter, Inc., Brea,
CA, USA) and analyzed using FlowJo version 7.6.1 (FlowJo LLC,
Ashland, OR, USA).
Detection of caspase-9/3 activity
EOMA cells were plated at 1×106
cells/well in 6-well plates and cultured with DMSO, or 50, 100 or
200 µM puerarin for 48 h. EOMA cells were stained with
Ac-LEHD-pNA (Beyotime Institute of Biotechnology) for
caspase-9 activity and Ac-DEVD-pNA (Beyotime Institute of
Biotechnology) for caspase-3 activity at 37°C for 1 h. The
caspase-9/3 activity was determined at the wavelength of 405 nm
using an ELISA plate reader.
Statistical analysis
The data are expressed as the mean ± standard error
of the mean using SPSS version 17.0 (SPSS, Inc., Chicago, IL, USA).
Statistical analysis was performed with an analysis of variance
followed by Tukey's post hoc test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Puerarin attenuates angII-induced AAA
in mice
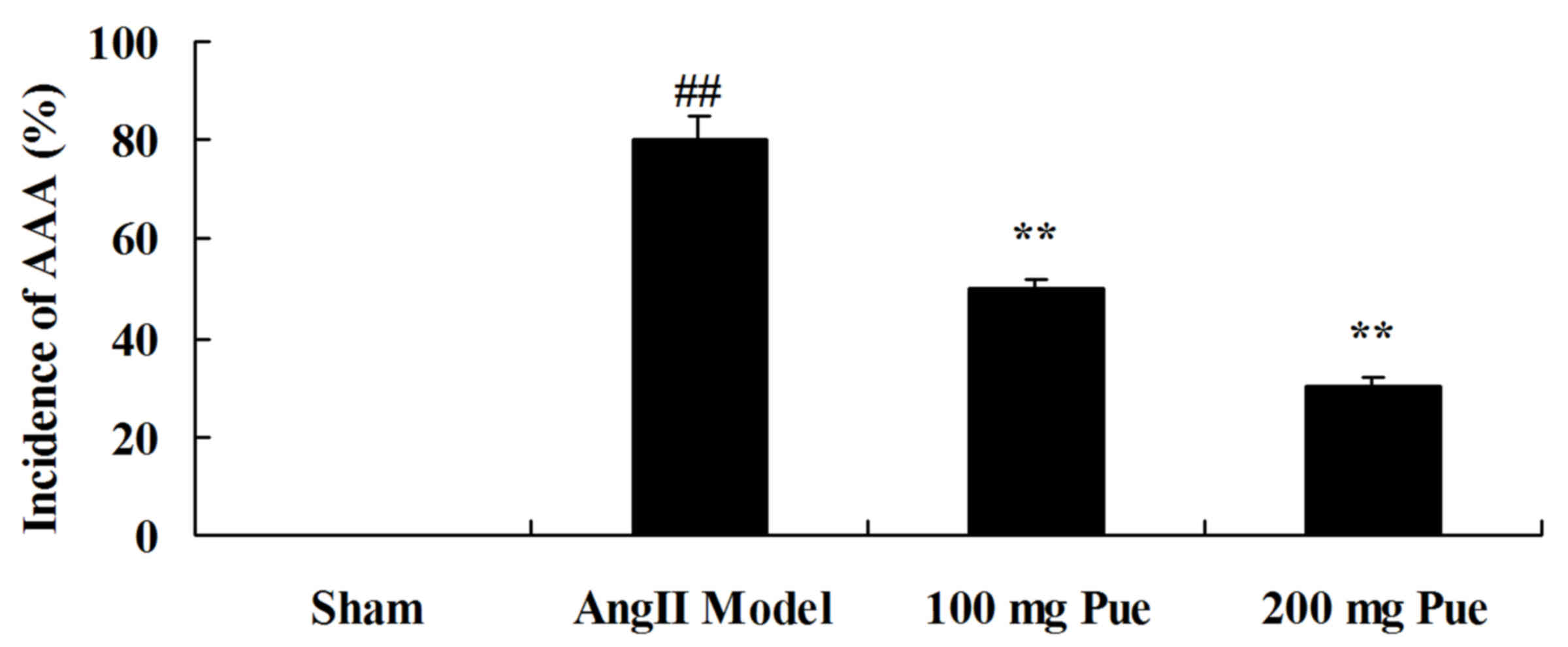
AngII-induced AAA was initially observed in the
different groups. As presented in Fig.
2, the angII-induced AAA rate of the AAA model was markedly
increased, compared with that of the sham control group. However,
puerarin decreased the angII-induced AAA rate in mice (Fig. 2).
Puerarin suppresses the NADPH oxidase
activity in angII-induced AAA in mice
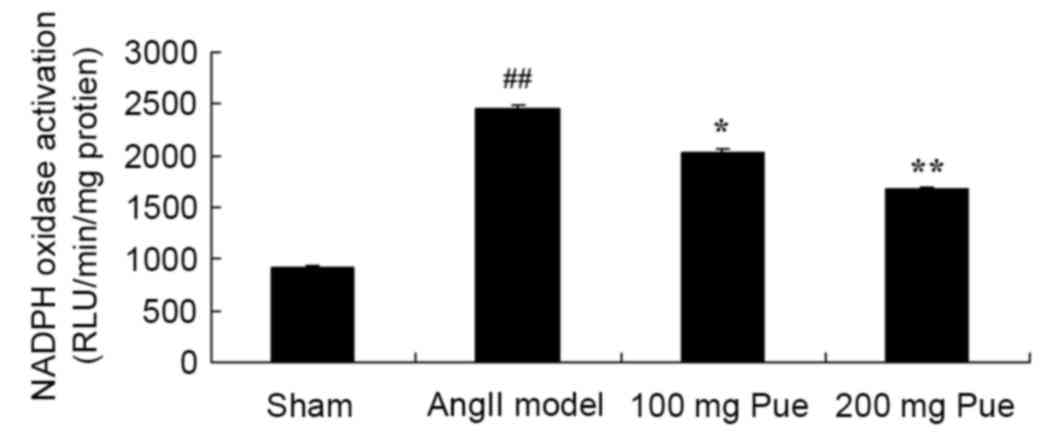
Subsequently, the NADPH oxidase activity from each
group was determined, to analyze the protective effect of puerarin
on the formation of angII-induced aortic aneurysms. Compared with
the sham group, NADPH oxidase activity was observably increased by
angII (Fig. 3). Treatment with
puerarin significantly decreased the angII-induced NADPH oxidase
activity in mice (Fig. 3).
Puerarin suppresses MMP-2 protein
expression in angII-induced AAA in mice
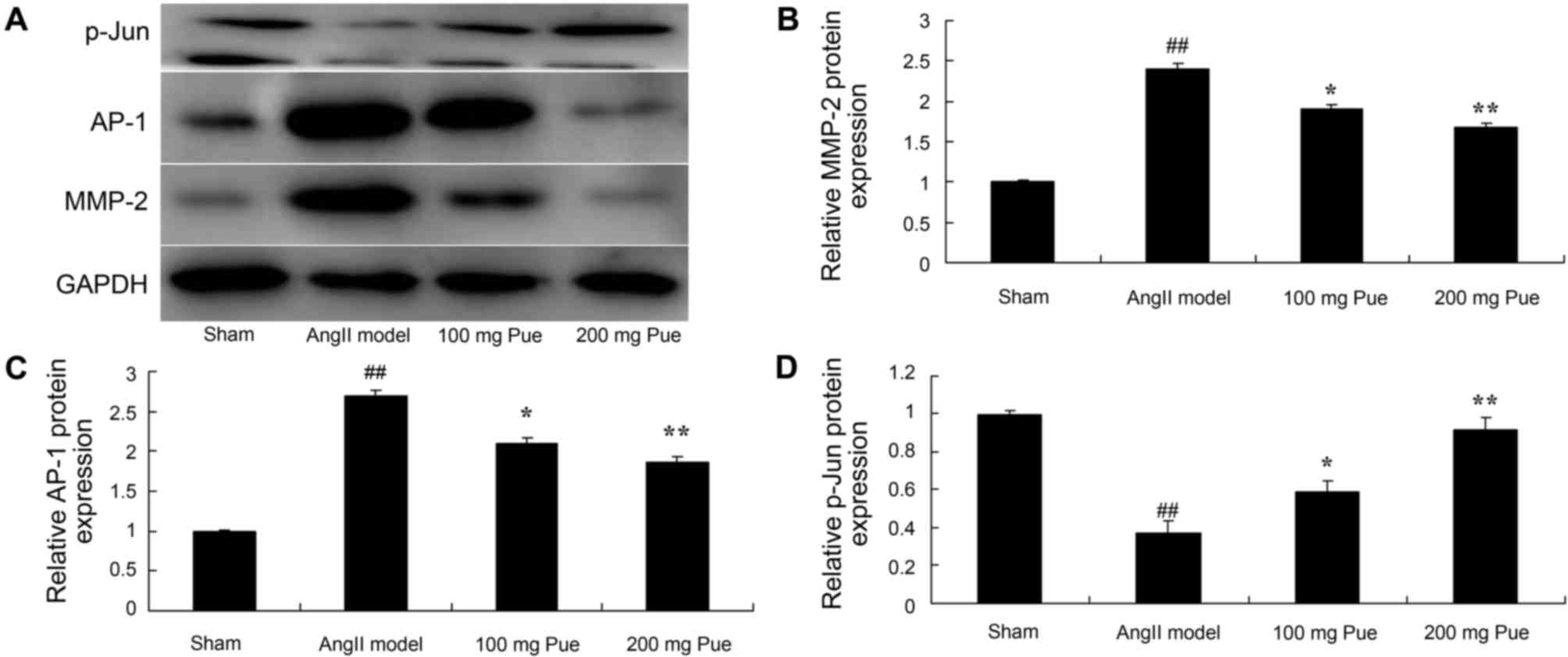
It was hypothesized that an effect on MMP-2 protein
expression was important in the protective effect of puerarin on
angII-induced aortic aneurysm formation. The results from western
blot analysis demonstrated that angII markedly induced MMP-2
protein expression in the AAA model group compared with the sham
group (Fig. 4). Puerarin treatment
significantly inhibited the expression of MMP-2 protein in
angII-induced AAA in mice (Fig.
4).
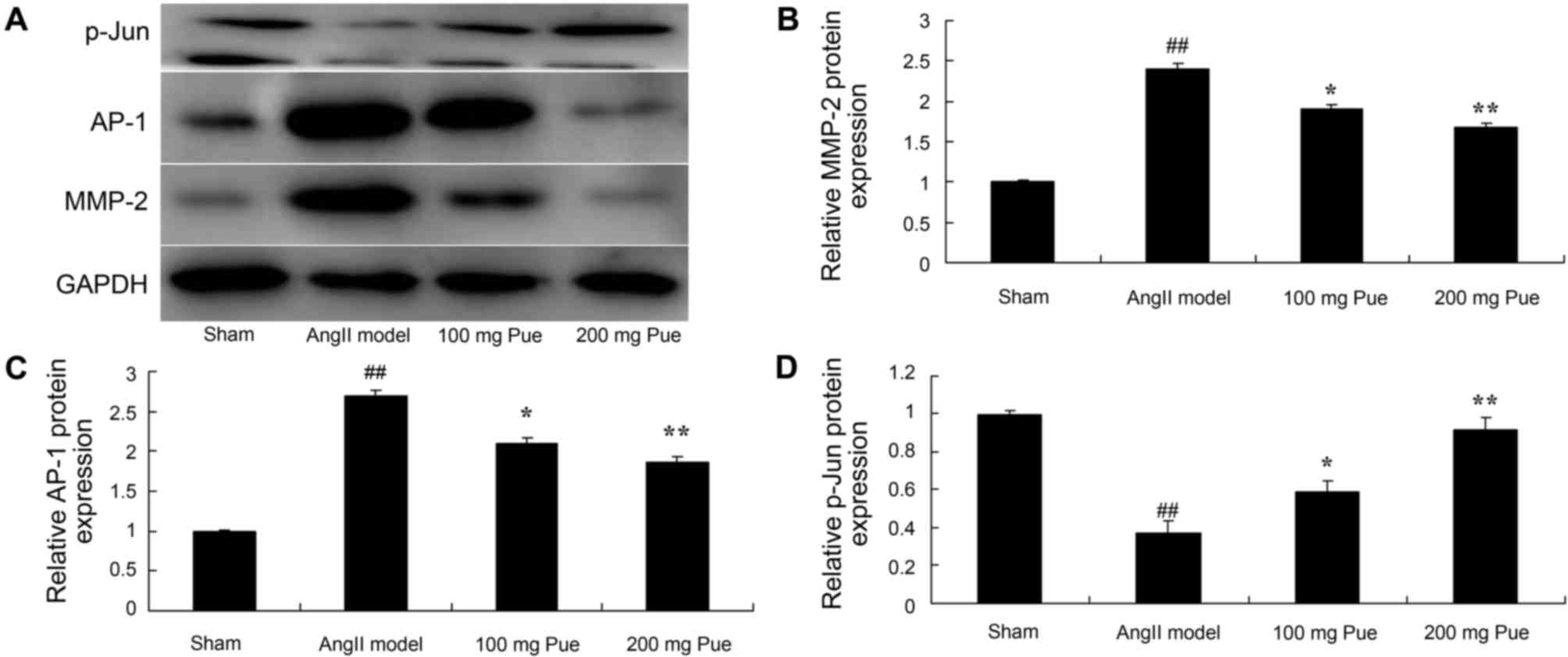 | Figure 4.Pue treatment suppressed MMP-2 and
AP-1 protein expression, and promoted p-Jun protein expression, in
angII-induced abdominal aortic aneurysm in mice. (A) Western
blotting was performed, and the results for (B) MMP-2, (C) AP-1 and
(D) p-Jun were quantified by normalization to GAPDH.
##P<0.01 vs. sham group; *P<0.05, **P<0.01 vs.
angII model group. Pue, puerarin; MMP-2, matrix metalloproteinase
2; AP-1, activator protein-1; p-Jun, phosphorylated Jun; angII,
angiotensin II. |
Puerarin inhibits the AP-1 protein
expression in angII-induced AAA in mice
The effect of puerarin on the AP-1 protein
expression of angII-induced AAA in mice was analyzed. As presented
in Fig. 4, angII significantly
induced AP-1 protein expression in AAA mice compared with the sham
group. Treatment with puerarin significantly inhibited the AP-1
protein expression of angII-induced AAA in mice (Fig. 4).
Puerarin induces the p-Jun protein
expression of angII-induced AAA in mice
Western blot analysis was used to determine the
effect of puerarin on p-Jun protein expression in angII-induced AAA
in mice. As presented in Fig. 4,
p-Jun protein expression of AAA in mice was significantly
suppressed by angII compared with the sham mice. Puerarin treatment
significantly increased the p-Jun protein expression of AAA in mice
(Fig. 4).
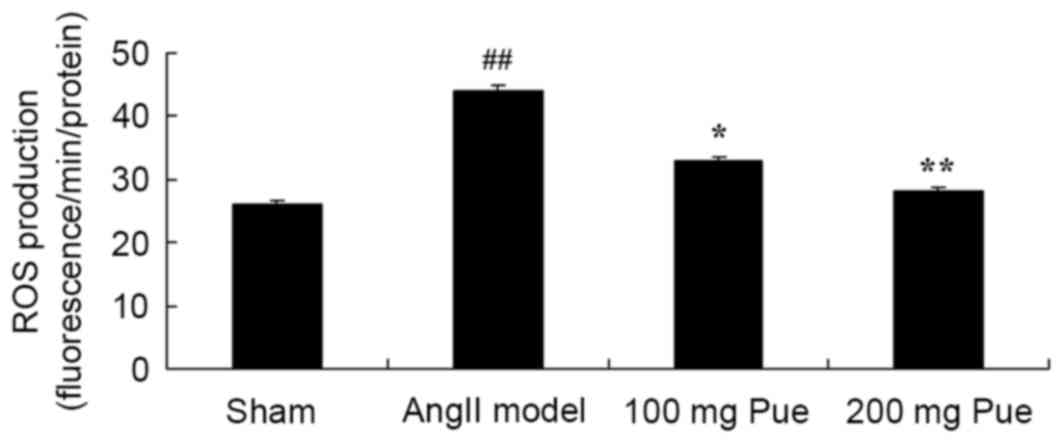
Puerarin suppresses the ROS production
in angII-induced AAA in mice
Subsequently, whether puerarin suppressed the ROS
production of angII-induced AAA in mice was investigated. As
presented in Fig. 5, there was a
marked increase in ROS production of angII-induced AAA model mice
compared with the sham group. Puerarin treatment significantly
decreased the extent of ROS production in angII-induced AAA mice
(Fig. 5).
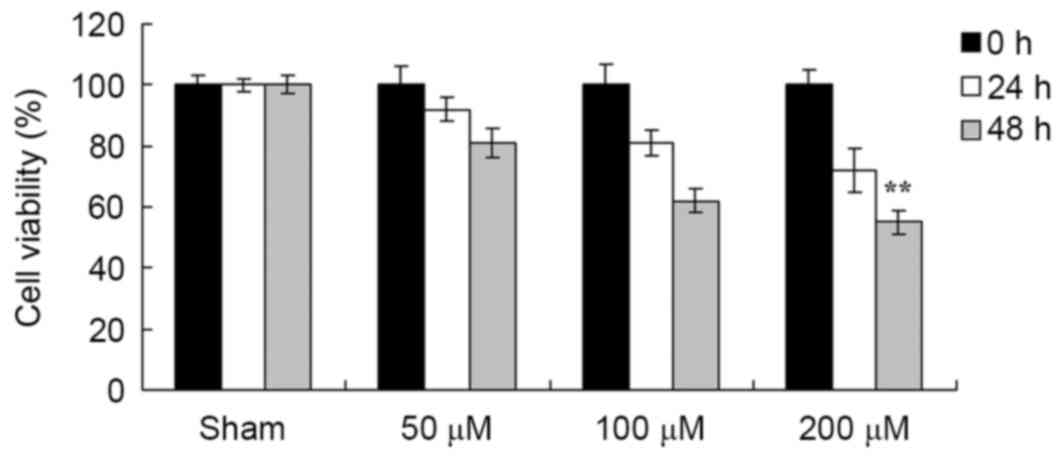
Puerarin attenuates the viability of
EOMA cells
A total of 50, 100 or 200 µM puerarin was added to
EOMA cells and viability was determined using an MTT assay. As
presented in Fig. 6, puerarin
significantly suppressed the viability of EOMA cells, compared with
the sham group (DMSO only).
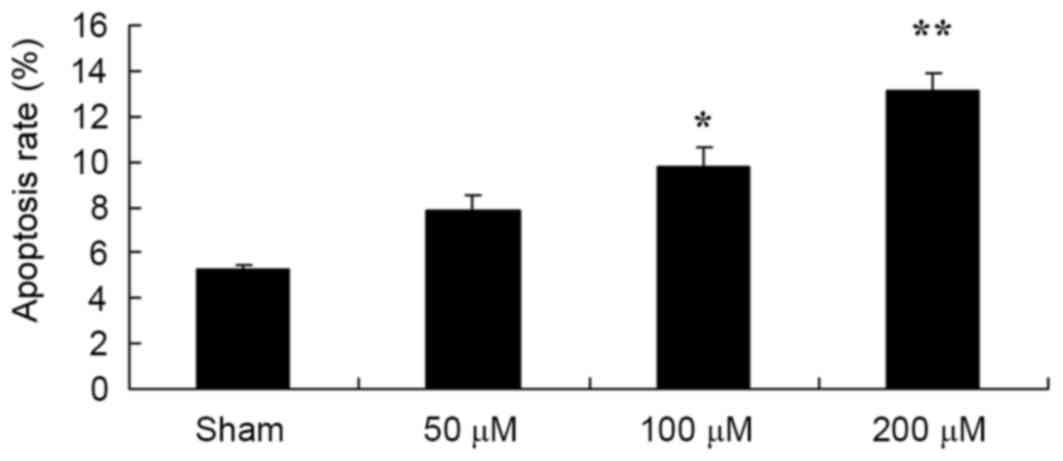
Puerarin induces the apoptosis of EOMA
cells
The effect of puerarin on the apoptosis of EOMA
cells was subsequently determined. As presented in Fig. 7, puerarin induced the apoptosis of
EOMA cells in a dose-dependent manner. In particular, 100 and 200
µM puerarin significantly induced the apoptosis of EOMA cells at 48
h (Fig. 7).
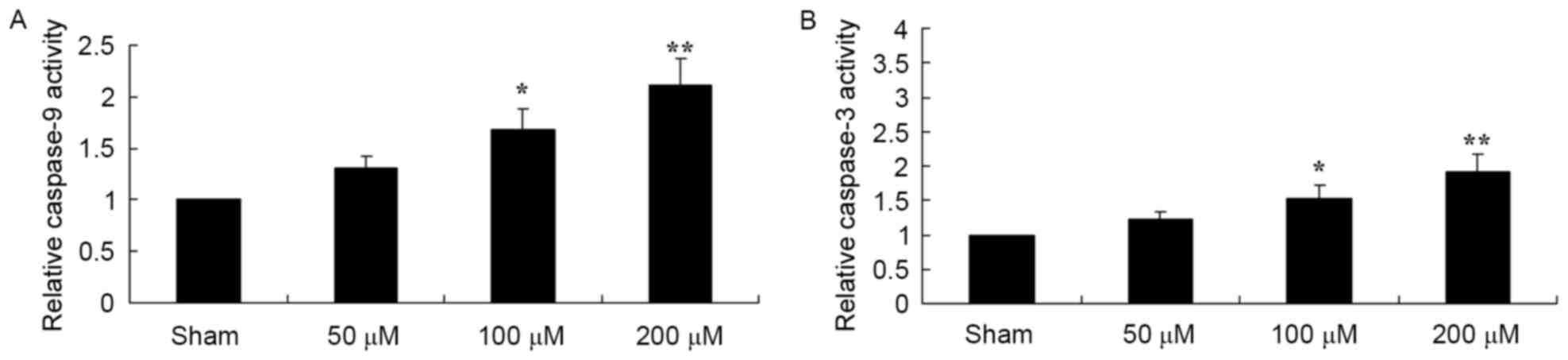
Puerarin induces increased caspase-9
and −3 activity in the EOMA cells
To determine the effect of puerarin on the caspase-9
and −3 activity of EOMA cells, caspase-9 and caspase-3 were
measured using a chromogenic assay. As presented in Fig. 8, 100 and 200 µM puerarin significantly
increased the activities of caspase-9 and caspase-3 in EOMA
cells.
Discussion
During the development of AAA, a large number of ROS
will be generated and inflammatory cells will release cytokines,
damaging the normal structure of the vascular wall (4). The expression level of ROS and reactive
nitrogen species (RNS) in human AAA specimens is significantly
increased (16). A previous study
demonstrated that the oxidative stress reaction in the aorta wall
is associated with the incidence of AAA; it can prevent the
formation of atherosclerosis (16).
Oxidative stress may promote the formation of AAA through the
regulation of p-Jun/AP-l (8). To the
best of our knowledge, the present study was the first to
demonstrate that puerarin significantly decreased the angII-induced
AAA rate in mice and suppressed viability, induced apoptosis and
increased the caspases 9 and 3 activity in EOMA cells. Zhang et
al (17) revealed that puerarin
inhibits growth and induces apoptosis of hepatocellular carcinoma
cells. In addition, Yu et al (13) indicated that puerarin induced
apoptosis and decreased the viability of colon cancer cells.
NADPH oxidase's substrates are O2 and
NADPH. The catalytic reaction process may generate a large amount
of O2−; NADPH oxidase is the principal source
of ROS in the vascular wall (18).
The specific inhibitor of NADPH oxidase, acetovanillone, was
determined to inhibit AAA in a mouse model (19). NADPH oxidase requires membrane
coupling and accessory proteins (including Rac, p47phox and
p67phox) to catalyze the generation of superoxide (20). It was previously identified that
quercetin downregulated the expression of p47phox in vitro
and in vivo, decreasing the generation of
O2− in the aorta (20). Following the gene knockout of p47phox,
oxidative stress levels are alleviated and the formation of AAA is
inhibited (19). Furthermore, the
results of the present study demonstrated that puerarin
significantly decreased the angII-induced NADPH oxidase activity in
AAA in mice. Kim et al (14)
demonstrated that puerarin inhibits the apoptosis of retinal
pericytes by inhibiting NADPH oxidase-related oxidative stress.
Oxidative stress is associated with the pathological
process of the inflammatory reaction. Oxidative stress is tissue
damage incurred subsequent to ROS increase and/or depletion
(21). There is a balance between the
generation of ROS (including NADPH oxidase) with antioxidants and
antioxidant enzymes (22). It is
hypothesized that ROS and oxidative stress may be associated with
human AAA pathogenesis; ROS and RNS are increased in AAA tissue
(22). The results of the present
study demonstrated that puerarin treatment significantly decreased
the production of ROS in angII-induced AAA mice. Zhang et al
(23) previously identified that
puerarin attenuates cognitive dysfunction and oxidative stress by
ROS generation in a rat model of vascular dementia.
The balance between MMPs and their inhibitors is
required to maintain the integrity of the arterial wall structure
(24). MMP-2 and −9 are predominantly
expressed in AAA tissue. A previous study has identified that MMP
regulation may serve a protective role in AAA; for example, mice
lacking MMP-2 or −9 did not form AAA (25). Oxidative stress is an important
regulator of MMPs; ROS may activate MMPs and induce the degradation
of the extracellular matrix. In thoracic aortic aneurysms, the MMP
activity is enhanced subsequent to NADPH oxidase overexpression
(26). In addition, in a mouse model
with thin arteries and veins, an increase in silicate increased the
activity of MMP-2 and −9, and induced vascular remodeling (27). In the present study, puerarin
treatment significantly inhibited the expression of MMP-2 protein
in angII-induced AAA mice. Yang et al (28) demonstrated that puerarin decreased
alveolar bone loss and collagen destruction by inhibiting the
production of MMP-2 and MMP-9 in rats.
The stress response in various cell types activates
c-Jun N-terminal kinases (JNKs). For this reason, JNKs are also
known as stress-activated protein kinases (29). It has been established that ROS and
RNS stimulate the production of NADPH. It has also been
demonstrated that JNKs are important in the incidence of AAA.
Through drug inhibition, it has been demonstrated that JNKs may
decrease the activity of MMPs and prevent the formation of AAA
(30). JNKs may regulate the
phosphorylation and nuclear translocation of transcription factors,
including AP-1, and other kinases (31). Gang et al (10) demonstrated that puerarin suppressed
angII-induced cardiac hypertrophy by the AP-1 and JNK1/2 signaling
pathways. In the present study, puerarin significantly inhibited
AP-1 protein expression and increased the p-Jun protein expression
in AAA in mice. Thus, puerarin treatment may reduce the oxidative
stress level and prevent the development of AAA via the regulation
of the JNK/AP-1 pathway and MMPs.
In conclusion, in the present study, it was
demonstrated that puerarin significantly decreased the
angII-induced AAA rate in a mouse model, suppressed viability,
induced apoptosis, and increased the activity of caspase-9 and −3
in EOMA cells. This may have been due to the inhibition of NADPH
oxidase activation and oxidative stress-triggered AP-1 signaling
pathways.
Acknowledgements
Not applicable.
Funding
No funding received.
Availability of data and materials
The analyzed data sets generated during the study
are available from the corresponding author on reasonable
request.
Authors' contributions
JH designed the experiment, JY, SC, ZX and YQ
performed the experiments, JH and JY analyzed the data and JH wrote
the manuscript.
Ethics approval and consent to
participate
All protocols in the present study were approved by
the Ethics Committee of the Hainan Provincial People's Hospital
(Guangzhou, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hansen Lyck M, Thomsen Dahl M, Rasmussen
LM and Lindholt JS: Abdominal aortic aneurysm, arterial stiffening
and the role of the intraluminal thrombus. Vasa. 44:349–353. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Barakat HM, Shahin Y, Barnes R, Gohil R,
Souroullas P, Khan J, McCollum PT and Chetter IC: Supervised
exercise program improves aerobic fitness in patients awaiting
abdominal aortic aneurysm repair. Ann Vasc Surg. 28:74–79. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Nienaber CA, Kische S, Rousseau H,
Eggebrecht H, Rehders TC, Kundt G, Glass A, Scheinert D, Czerny M,
Kleinfeldt T, et al: Endovascular repair of type B aortic
dissection: long-term results of the randomized investigation of
stent grafts in aortic dissection trial. Circ Cardiovasc Interv.
6:407–416. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
United Kingdom EVAR Trial Investigators, .
Greenhalgh RM, Brown LC, Powell JT, Thompson SG and Epstein D:
Endovascular repair of aortic aneurysm in patients physically
ineligible for open repair. N Engl J Med. 362:1872–1880. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wong YY, Flicker L, Yeap BB, McCaul KA,
Hankey GJ and Norman PE: Is hypovitaminosis D associated with
abdominal aortic aneurysm, and is there a dose-response
relationship? Eur J Vasc Endovasc Surg. 45:657–664. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cafueri G, Parodi F, Pistorio A,
Bertolotto M, Ventura F, Gambini C, Bianco P, Dallegri F, Pistoia
V, Pezzolo A and Palombo D: Endothelial and smooth muscle cells
from abdominal aortic aneurysm have increased oxidative stress and
telomere attrition. PLoS One. 7:e353122012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Guzik B, Sagan A, Ludew D, Mrowiecki W,
Chwała M, Bujak-Gizycka B, Filip G, Grudzien G, Kapelak B, Zmudka
K, et al: Mechanisms of oxidative stress in human aortic
aneurysms-association with clinical risk factors for
atherosclerosis and disease severity. Int J Cardiol. 168:2389–2396.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kaneko H, Anzai T, Horiuchi K, Kohno T,
Nagai T, Anzai A, Takahashi T, Sasaki A, Shimoda M, Maekawa Y, et
al: Tumor necrosis factor-α converting enzyme is a key mediator of
abdominal aortic aneurysm development. Atherosclerosis.
218:470–478. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sawada H, Hao H, Naito Y, Oboshi M,
Hirotani S, Mitsuno M, Miyamoto Y, Hirota S and Masuyama T: Aortic
iron overload with oxidative stress and inflammation in human and
murine abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol.
35:1507–1514. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gang C, Qiang C, Xiangli C, Shifen P,
Chong S and Lihong L: Puerarin suppresses angiotensin ii-induced
cardiac hypertrophy by inhibiting nadph oxidase activation and
oxidative stress-triggered ap-1 signaling pathways. J Pharm Pharm
Sci. 18:235–248. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu X, Mo Y, Gong J, Li Z, Peng H, Chen J,
Wang Q, Ke Z and Xie J: Puerarin ameliorates cognitive deficits in
streptozotocin-induced diabetic rats. Metab Brain Dis. 31:417–423.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gao Z, Wei B and Qian C: Puerarin
injection for treatment of unstable angina pectoris: A
meta-analysis and systematic review. Int J Clin Exp Med.
8:14577–14594. 2015.PubMed/NCBI
|
|
13
|
Yu Z and Li W: Induction of apoptosis by
puerarin in colon cancer HT-29 cells. Cancer Lett. 238:53–60. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim J, Kim KM, Kim CS, Sohn E, Lee YM, Jo
K and Kim JS: Puerarin inhibits the retinal pericyte apoptosis
induced by advanced glycation end products in vitro and in vivo by
inhibiting NADPH oxidase-related oxidative stress. Free Radic Biol
Med. 53:357–365. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ren H, Li F, Tian C, Nie H, Wang L, Li HH
and Zheng Y: Inhibition of proteasome activity by low-dose
bortezomib attenuates angiotensin ii-induced abdominal aortic
aneurysm in apoe(−/-) mice. Sci Rep. 5:157302015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Blogowski W, Dolegowska B, Pikula E,
Gutowski P and Starzynska T: The effect of PGE administration on
the activity of oxidative system in erythrocytes and platelets
during ischemia reperfusion injury and on postoperative renal
function in patients undergoing open abdominal aortic aneurysm
reconstruction. J Biol Regul Homeost Agents. 26:429–438.
2012.PubMed/NCBI
|
|
17
|
Zhang WG, Liu XF, Meng KW and Hu SY:
Puerarin inhibits growth and induces apoptosis in SMMC-7721
hepatocellular carcinoma cells. Mol Med Rep. 10:2752–2758. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Liu Z, Luo H, Zhang L, Huang Y, Liu B, Ma
K, Feng J, Xie J, Zheng J, Hu J, et al: Hyperhomocysteinemia
exaggerates adventitial inflammation and angiotensin II-induced
abdominal aortic aneurysm in mice. Circ Res. 111:1261–1273. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Thomas M, Gavrila D, McCormick ML, Miller
FJ Jr, Daugherty A, Cassis LA, Dellsperger KC and Weintraub NL:
Deletion of p47phox attenuates angiotensin II-induced abdominal
aortic aneurysm formation in apolipoprotein E-deficient mice.
Circulation. 114:404–413. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Miao XN, Siu KL and Cai H: Nifedipine
attenuation of abdominal aortic aneurysm in hypertensive and
non-hypertensive mice: Mechanisms and implications. J Mol Cell
Cardiol. 87:152–159. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang H, Wang ZW, Wu HB, Li Z, Li LC, Hu
XP, Ren ZL, Li BJ and Hu ZP: Transforming growth factor-β1 induces
matrix metalloproteinase-9 expression in rat vascular smooth muscle
cells via ROS-dependent ERK-NF-κB pathways. Mol Cell Biochem.
375:11–21. 2013.PubMed/NCBI
|
|
22
|
Yan H, Cui B, Zhang X, Fu X, Yan J, Wang
X, Lv X, Chen Z and Hu Z: Antagonism of toll-like receptor 2
attenuates the formation and progression of abdominal aortic
aneurysm. Acta Pharm Sin B. 5:176–187. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhang J, Guo W, Tian B, Sun M, Li H, Zhou
L and Liu X: Puerarin attenuates cognitive dysfunction and
oxidative stress in vascular dementia rats induced by chronic
ischemia. Int J Clin Exp Pathol. 8:4695–4704. 2015.PubMed/NCBI
|
|
24
|
Dale MA, Suh MK, Zhao S, Meisinger T, Gu
L, Swier VJ, Agrawal DK, Greiner TC, Carson JS, Baxter BT and Xiong
W: Background differences in baseline and stimulated MMP levels
influence abdominal aortic aneurysm susceptibility.
Atherosclerosis. 243:621–629. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rabkin SW: Differential expression of
MMP-2, MMP-9 and TIMP proteins in thoracic aortic aneurysm -
comparison with and without bicuspid aortic valve: a meta-analysis.
Vasa. 43:433–442. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zhang T, Xu J, Li D, Chen J, Shen X, Xu F,
Teng F, Deng Y, Ma H, Zhang L, et al: Salvianolic acid A, a matrix
metalloproteinase-9 inhibitor of Salvia miltiorrhiza, attenuates
aortic aneurysm formation in apolipoprotein E-deficient mice.
Phytomedicine. 21:1137–1145. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Deguchi JO, Huang H, Libby P, Aikawa E,
Whittaker P, Sylvan J, Lee RT and Aikawa M: Genetically engineered
resistance for MMP collagenases promotes abdominal aortic aneurysm
formation in mice infused with angiotensin II. Lab Invest.
89:315–326. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yang X, Zhang H, Wang J, Zhang Z and Li C:
Puerarin decreases bone loss and collagen destruction in rats with
ligature-induced periodontitis. J Periodontal Res. 50:748–757.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wang C, Chang Q, Qian X, Tian C and Sun X:
Angiotensin II induces an increase in MMP-2 expression in
idiopathic ascending aortic aneurysm via AT1 receptor and JNK
pathway. Acta Biochim Biophys Sin (Shanghai). 47:539–547. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
DiMusto PD, Lu G, Ghosh A, Roelofs KJ,
Sadiq O, McEvoy B, Su G, Laser A, Bhamidipati CM, Ailawadi G, et
al: Increased JNK in males compared with females in a rodent model
of abdominal aortic aneurysm. J Surg Res. 176:687–695. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang L, Cheng X, Li H, Qiu F, Yang N, Wang
B, Lu H, Wu H, Shen Y, Wang Y and Jing H: Quercetin reduces
oxidative stress and inhibits activation of cJun Nterminal
kinase/activator protein1 signaling in an experimental mouse model
of abdominal aortic aneurysm. Mol Med Rep. 9:435–442. 2014.
View Article : Google Scholar : PubMed/NCBI
|