Introduction
Primary hepatic carcinoma (PHC) is a common
gastrointestinal cancer in humans. There are approximately 600,000
new patients diagnosed with PHC each year worldwide. Its mortality
ranks third among human malignancies (1). Thyroid carcinoma (TC) is the most common
cancer of the endocrine system. It is a malignancy derived from the
thyroid epithelial cells. Annual new patients diagnosed with TC
accounts for 1% of all patients newly diagnosed with malignant
tumors (2). Along with the economic
and social development, the incidence of PHC and TC has risen year
by year in recent decades, and patient age tends to be younger. In
the past, the patients were often in the advanced stage of the
disease when diagnosed, as a result of fast progression of the
disease and lack of specific clinical symptoms for early diagnosis
(3,4).
Therefore, early accurate diagnosis of PHC and TC is particularly
important, which can directly facilitate timely development of the
patient treatment plan and promise a good prognosis and quality of
life. According to literature, the 5-year survival rates of PHC and
TC were approximately 70 and 80%, respectively, after early
surgical treatment (5,6). Diagnosis based on pathological tests is
the most common practice for cancer diagnosis. This approach has a
high diagnostic rate, but also has some disadvantages. The main
drawback is its invasiveness which is necessary for tissue
harvesting from the patient. Therefore, a pathological test cannot
be performed routinely as an early screening test due to the
invasiveness (7). As the imaging
technologies advance, two-dimensional and color Doppler
ultrasonography have been gradually adopted in the early screening
and diagnosis of malignant tumors. Using the ultrasonography, the
number and size of tumor foci, as well as their location and
relationship with adjacent tissues, can be observed clearly in the
tumor mass. Ultrasonic diagnosis is non-invasive, reproducible and
cost-efficient (8,9). Due to these favorable features,
ultrasonography has been playing an important role in the clinic.
However, combination of two-dimensional and color Doppler
ultrasonography has rarely been reported in the early screening and
diagnosis of PHC and TC. In this study, both two-dimensional and
color Doppler ultrasonography were performed on 426 patients with
liver space-occupying lesions and 367 patients with thyroid
nodules. The diagnostic results based on the sonographic features
were compared with the postoperative pathological test results,
aiming to explore the applicable value of simultaneous use of two
ultrasound techniques in the differential diagnosis of liver
space-occupying lesions and thyroid nodules.
Patients and methods
Patients
Four hundred and twenty six patients diagnosed with
liver space-occupying lesions (453 foci) by ultrasonic examination,
who were admitted to Liaocheng People's Hospital (Liaocheng, China)
from March 2014 to October 2017, were enrolled in this study. These
patients were divided into two groups: 226 patients with 237 foci
in the PHC group and 200 patients with 216 foci in the benign liver
lesion group. There were 141 males and 85 females, aged 23–69
years, in the PHC group. Of the 237 cancer foci in the PHC group,
197 were hepatocellular carcinoma of origin, and 40 were
cholangiocellular carcinoma of origin. There were 109 males and 91
females, aged 25–73 years, in the benign liver lesion group. During
the same period, 367 patients diagnosed with thyroid nodules (382
nodules) by ultrasonic examination in Liaocheng People's Hospital
were also enrolled in this study. These patients were divided into
further two groups: 193 patients with 203 nodules in the TC group
and 174 patients with 179 nodules in the benign thyroid nodule
group. There were 35 males and 158 females, aged 24–76 years, in
the TC group. Among the 203 cancer nodules, 3 were metastatic TC of
origin, 7 were anaplastic TC of origin, 15 were of medullary TC of
origin, 34 were follicular TC, and 144 were papillary TC of origin.
There were 21 males and 153 females, aged 21–69 years, in the
benign thyroid nodule group. Among the 179 benign nodules, 79 were
benign thyroid tumor of origin, and 100 were nodular goiter of
origin.
Inclusion and exclusion criteria
The following patients were included in this study:
Patients with clear primary lesions diagnosed by histopathological
and cytological tests, as well as imaging with MRI (10) and patients who had complete ultrasonic
examination record. Patients who had the following conditions were
excluded from this study: Severe heart failure, severe lung, kidney
or hematopoietic dysfunction; with a history of previous mental
disease and with a family history of mental disease. This study was
approved by Liaocheng People's Hospital's Ethics Committee. All the
patients or their families signed the informed consent.
Methods
Ultrasonic examination was performed using a GE
Logiq E9 color Doppler ultrasound system. The system was equipped
with a GE 3.5C convex array transducer probe, and the probe had a
frequency of 6–9 MHz.
Liver examination method
The patient fasted for 8 h prior to the examination.
At the time of examination, the patient was placed in the supine
position. After the ultrasound system was adjusted to the right
parameter settings, a 2D multi-sectional examination of the whole
liver was performed. If necessary, the patient's position was
changed so that the sonographic features of the lesions could be
clearly observed. First, the liver was carefully inspected for any
abnormality in size, shape, echo of liver parenchyma, liver
capsule, blood vessels, and internal echo. After lesions were
found, attention should be paid to the number, locations,
morphology, boundary, internal and posterior echoes of the lesion
foci. These sonographic features were recorded in detail. In
addition, the ultrasonic blood flow distribution and spectrum were
inspected as well. The images were saved.
Thyroid examination method
The patient was placed in the supine position with
the neck fully exposed. The thyroid gland was scanned for
transverse, longitudinal and oblique views. When a nodule was
found, its size, morphology, parenchymal echo pattern,
calcification, blood vessels and internal echo were carefully
inspected. The lymph node status, as well as the ultrasonic blood
flow distribution and spectrum, were inspected. The images of the
blood flow distribution and spectrum were saved.
Statistical analysis
The statistical software SPSS 17.0 (SPSS, Inc.,
Chicago, IL, USA) was used for statistical analysis. The
measurement data were expressed as mean ± standard deviation (SD).
The Chi-square test was used for comparison of the enumeration data
between two groups, and the t-test was used for comparison of the
measurement data between two groups. One way analysis of variance
was used for data comparison between multiple groups and the post
hoc test was Least Significant Difference. The difference was
statistically significant at p<0.05.
Results
Baseline data of patients in the PHC
and the benign liver lesion group
As shown in Table I,
the differences in baseline clinical data such as sex, age, status
of viral hepatitis, of cirrhosis, and of α-fetoprotein (AFP) were
not statistically significant between patients in the PHC and the
benign liver lesion group (p>0.05).
 | Table I.Baseline clinical data of patients in
the PHC and benign liver lesion group. |
Table I.
Baseline clinical data of patients in
the PHC and benign liver lesion group.
|
| Groups |
|
|
|---|
|
|
|
|
|
|---|
| Items | PHC | Benign liver
lesion | t value | P-value |
|---|
| Patient no. | 226 | 200 | |
|
| Sex, n (%) |
| Male | 141 (62.39) | 109 (54.50) | 2.724 | 0.115 |
|
Female | 85
(37.61) | 91
(45.50) |
|
|
| Age, years | 49.6±13.3 | 48.3±8.7 | 1.177 | 0.239 |
| Status of viral
hepatitis, n (%) |
| Yes | 143 (63.27) | 108 (54.00) | 3.771 | 0.061 |
| No | 83
(36.73) | 92
(46.00) |
|
|
| Status of cirrhosis,
n (%) |
| Yes | 33
(14.60) | 21
(10.50) | 1.613 | 0.243 |
| No | 193 (85.40) | 179 (89.50) |
|
|
| Status of AFP, n
(%) |
|
Positive | 53
(23.45) | 31
(15.50) | 4.238 | 0.051 |
|
Negative | 173 (76.55) | 169 (84.50) |
|
|
Baseline data of patients in the TC
and the benign thyroid nodule group
As shown in Table II,
the differences in baseline clinical data such as sex, age, serum
thyroid-stimulating hormone (TSH), serum free triiodothyronine
(FT3), serum free thyroxine (FT4), serum thyroid peroxidase
antibody (TPO-Ab) and serum thyroglobulin antibody (Tg-Ab) were not
statistically significant between patients in the TC and the benign
thyroid nodule group (p>0.05).
 | Table II.Baseline clinical data of patients in
the TC and benign thyroid nodule group. |
Table II.
Baseline clinical data of patients in
the TC and benign thyroid nodule group.
|
| Groups |
|
|
|---|
|
|
|
|
|
|---|
| Items | TC | Benign thyroid
nodule | t value | P-value |
|---|
| Patient no. | 193 | 174 |
|
|
| Sex, n (%) |
| Male | 35
(18.13) | 21
(12.07) | 2.604 | 0.112 |
|
Female | 158 (81.87) | 153 (87.93) |
|
|
| Age, years | 47.1±12.8 | 44.9±11.6 | 1.719 | 0.086 |
| TSH (mU/l) | 1.73±1.15 | 1.61±0.89 | 1.109 | 0.268 |
| FT3 (mU/l) | 4.78±1.21 | 4.63±0.73 | 1.419 | 0.156 |
| FT4 (mU/l) | 17.38±3.74 | 16.87±3.51 | 1.343 | 0.18 |
| TPO-Ab (mU/l) | 217.62±127.82 | 199.47±115.19 | 1.423 | 0.155 |
| Tg-Ab (mU/l) | 81.56±31.73 | 86.68±34.28 | 1.486 | 0.138 |
Diagnosis of PHC using
ultrasonography
Among the 453 foci found in patients with liver
space-occupying lesions, 237 were believed to be PHC of origin in
226 patients, and 216 were of benign liver lesion of origin in 200
patients, following confirmation by pathological tests. Of the 237
cancer foci, 197 were hepatocellular carcinoma of origin in 188
patients, and 40 were cholangiocellular carcinoma of origin in 38
patients. Of the 216 benign foci, 120 were hemangioma of origin in
114 patients, 62 were hyperplastic nodules of liver cirrhosis in 58
patients, 15 were hepatic abscess in 12 patients, and 19 were focal
nodular hyperplasia of origin in 16 patients. As shown in Table III, the sensitivity, specificity and
accuracy of the ultrasonic diagnosis of PHC were 78.32% (177/226),
71.00% (142/200) and 74.88% (319/426), respectively.
 | Table III.Diagnosis of PHC using ultrasonography
and pathological tests. |
Table III.
Diagnosis of PHC using ultrasonography
and pathological tests.
|
| Pathological
tests |
|
|---|
|
|
|
|
|---|
| Items | PHC | Benign liver
lesions | Total |
|---|
| Ultrasonic
diagnosis |
| PHC | 177 | 58 | 235 |
| Benign
liver lesions | 49 | 142 | 191 |
| Total | 226 | 200 | 426 |
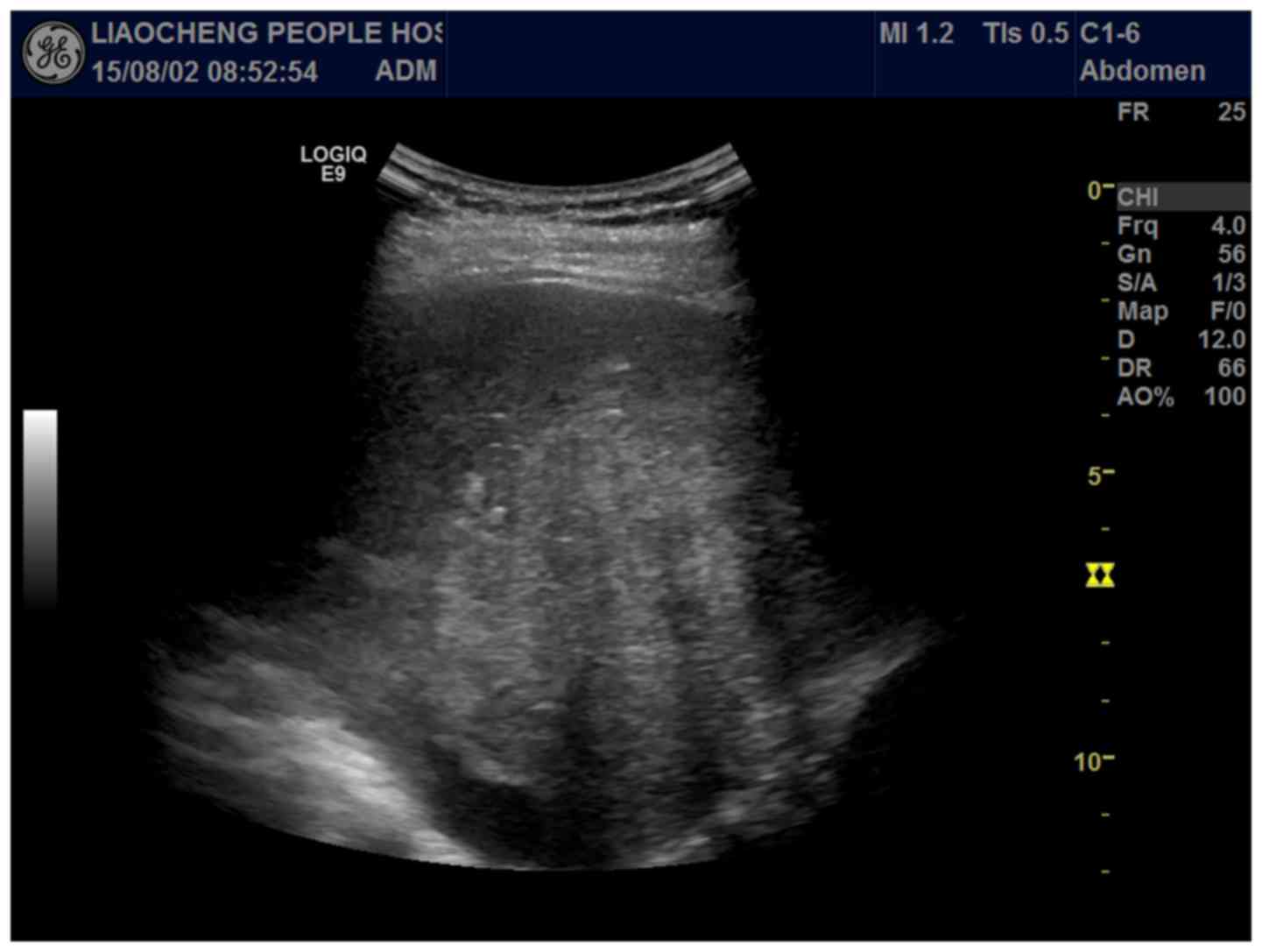
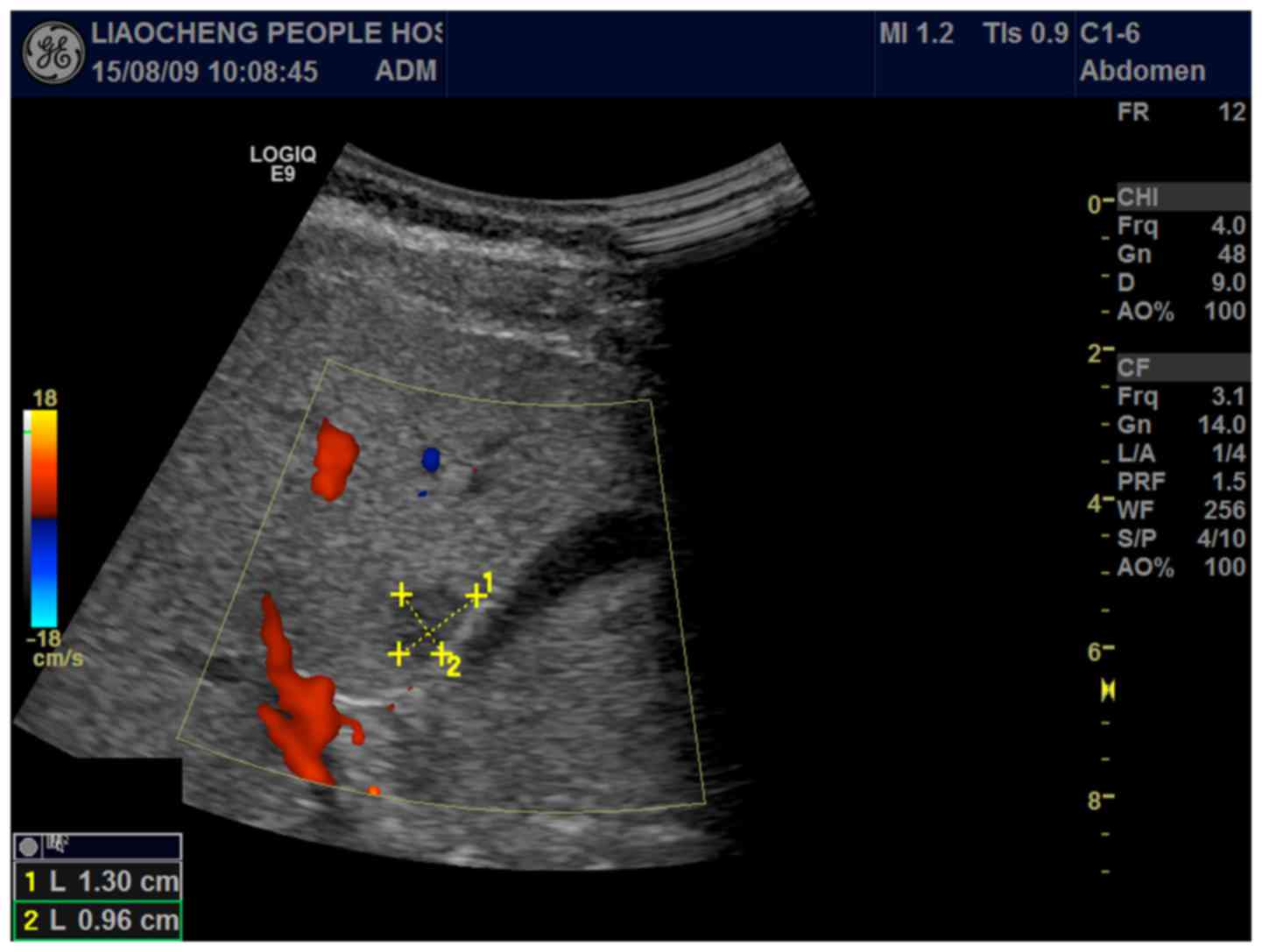
Sonographic features of PHC
As shown in Table IV,
the differences in the sonographic features such as focus
morphology, focus size, internal echo pattern, halo and blood flow
distribution were statistically significant between patients in the
PHC and the benign liver lesion group (p<0.001). The major
sonographic features of PHC included regular shape in focus
morphology, >3 cm in focus size, hypoechoic internal echo,
visible thin halo signs, and rich internal blood flow. Sonographic
features of PHC are shown in Figs. 1
and 2.
 | Table IV.Sonographic features of 453 foci in
patients with occupied liver space. |
Table IV.
Sonographic features of 453 foci in
patients with occupied liver space.
|
| Groups |
|
|
|---|
|
|
|
|
|
|---|
| Sonographic
features | PHC n (%) | Benign liver lesion
n (%) | χ2
value | P-value |
|---|
| Total foci | 237 | 216 |
|
|
| Focus
multiplicity |
|
Single | 226 (95.36) | 200 (92.59) | 1.543 | 0.238 |
|
Multiple | 11 (4.64) | 16 (7.41) |
|
|
| Focus
morphology |
|
Regular | 153 (64.56) | 94 (43.52) | 20.173 | <0.001 |
|
Irregular | 84 (35.44) | 122 (56.48) |
|
|
| Focus boundary |
|
Clear | 106 (44.73) | 93 (43.06) | 0.128 | 0.776 |
|
Vague | 131 (55.27) | 123 (56.94) |
|
|
| Focus size, cm |
| ≤3 | 34 (14.35) | 107 (49.54) | 65.282 | <0.001 |
|
>3 | 203 (85.65) | 109 (50.46) |
|
|
| Internal echo |
|
Hypoechoic | 145 (61.18) | 52 (24.07) | 63.407 | <0.001 |
|
Isoechoic | 40 (16.88) | 68 (31.48) |
|
|
|
Hyperechoic | 52 (21.94) | 96 (44.44) |
|
|
| Halo |
|
Yes | 153 (64.56) | 99 (45.83) | 16.050 | <0.001 |
| No | 84 (35.44) | 117 (54.17) |
|
|
| Lymph node
metastasis |
|
Yes | 23 (9.70) | 16 (7.41) | 0.758 | 0.407 |
| No | 214 (90.30) | 200 (92.59) |
|
|
| Blood flow
distribution lesions |
| Grade
I | 43 (19.91) | 78 (32.91) | 22.980 | <0.001 |
| Grade
II | 71 (32.87) | 97 (40.93) |
|
|
| Grade
III | 102 (47.22) | 62 (26.16) |
|
|
Diagnosis of TC using
ultrasonography
Among the 382 nodules found in patients with thyroid
nodules, 203 were believed to be TC origin in 193 patients, and 179
were believed to be benign thyroid nodules of origin in 174
patients, following confirmation by pathological tests. Of the 203
cancer nodules, 3 were metastatic TC of origin in 3 patients, 7
were anaplastic TC of origin in 7 patients, 15 were medullary TC in
15 patients, 34 were the follicular TC of origin in 30 patients,
and 144 were papillary TC in 138 patients. Of the 179 benign
nodules, 79 were the benign thyroid tumor of origin in 77 patients,
and 100 were nodular goiter of origin in 97 patients. As shown in
Table V, the sensitivity, specificity
and accuracy of the ultrasonic diagnosis of TC were 79.27%
(153/193), 75.86% (132/174) and 77.65% (285/367), respectively.
 | Table V.Diagnosis of TC using ultrasonography
and pathological tests. |
Table V.
Diagnosis of TC using ultrasonography
and pathological tests.
|
| Pathological
tests |
|
|---|
|
|
|
|
|---|
| Items | TC | Benign thyroid
nodules | Total |
|---|
| Ultrasonic
diagnosis |
| TC | 153 | 42 | 195 |
| Benign
thyroid nodules | 40 | 132 | 172 |
| Total | 193 | 174 | 367 |
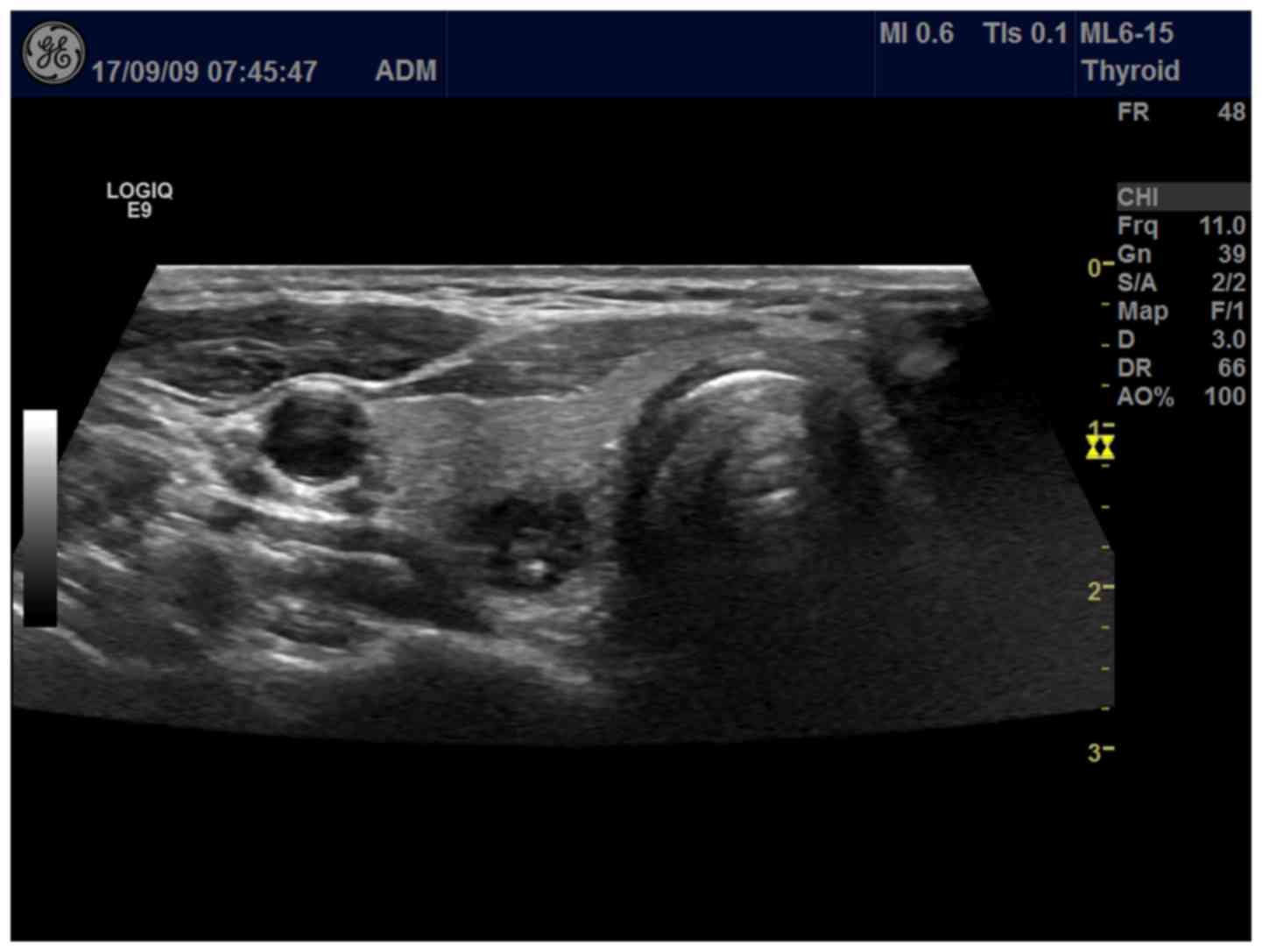
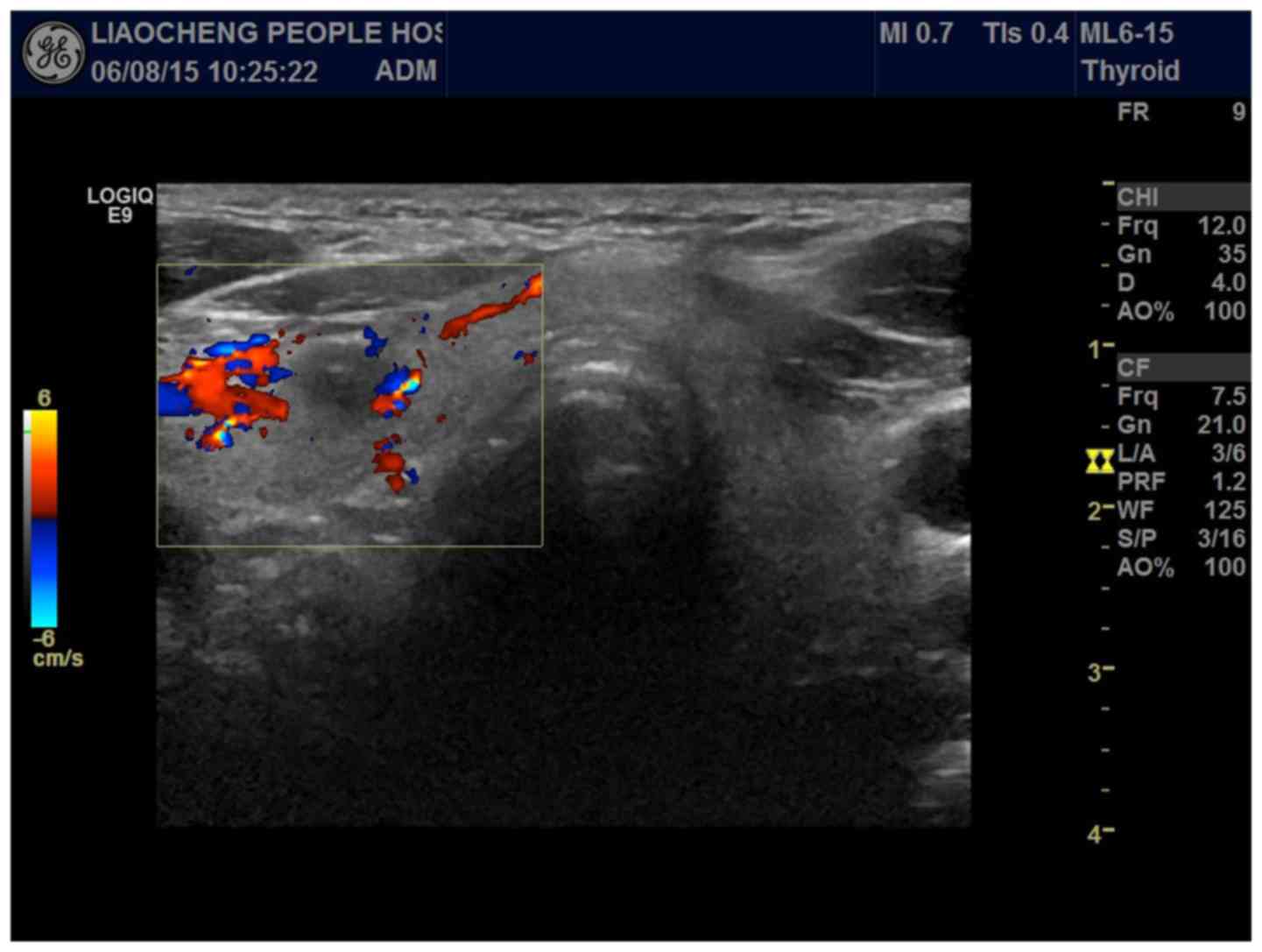
Sonographic features of TC
As shown in Table VI,
the differences in the sonographic features such as nodule
boundary, nodule size, internal echo, microcalcification, lymph
node status and blood flow distribution were statistically
significant between patients in the TC and the benign thyroid
nodule group (p<0.01). The major sonographic features of TC
included blurred nodule boundary, >1 cm in nodule size,
hypoechoic internal echo pattern, visible microcalcification,
enlarged lymph nodes, and rich internal blood flow. Sonographic
features of TC are shown in Figs. 3
and 4.
 | Table VI.Sonographic features of 382 nodules
in patients with thyroid nodules. |
Table VI.
Sonographic features of 382 nodules
in patients with thyroid nodules.
|
| Groups |
|
|
|---|
|
|
|
|
|
|---|
| Sonographic
features | TC n (%) | Benign thyroid
nodule n (%) | χ2
value | P-value |
|---|
| Total nodules | 203 | 179 |
|
|
| Nodule
multiplicity |
|
Single | 193 (95.07) | 174 (97.21) | 1.168 | 0.306 |
|
Multiple | 10 (4.93) | 5 (2.79) |
|
|
| Nodule
morphology |
|
Regular | 139 (68.47) | 116 (64.80) | 0.557 | 0.514 |
|
Irregular | 64 (31.53) | 63 (35.20) |
|
|
| Nodule
boundary |
|
Clear | 66 (32.51) | 26 (14.53) | 16.833 | <0.001 |
|
Vague | 137 (67.49) | 153 (85.47) |
|
|
| Nodule size,
cm |
| ≤1 | 79 (38.92) | 36 (20.11) | 16.775 | <0.001 |
|
>1 | 124 (61.08) | 143 (79.89) |
|
|
| Internal echo |
|
Hypoechoic | 160 (78.82) | 50 (27.93) | 99.518 | <0.001 |
|
Isoechoic | 5 (2.46) | 16 (8.94) |
|
|
|
Hyperechoic | 38 (18.72) | 113 (63.13) |
|
|
|
Microcalcification |
|
Yes | 77 (37.93) | 45 (25.14) | 7.160 | 0.008 |
| No | 126 (62.07) | 134 (74.86) |
|
|
| Enlarged lymph
nodes |
|
Yes | 84 (41.38) | 38 (21.23) | 17.768 | <0.001 |
| No | 119 (58.62) | 141 (78.77) |
|
|
| Blood flow
distribution |
| Grade
I | 53 (26.11) | 44 (24.58) | 6.464 | 0.039 |
| Grade
II | 38 (18.72) | 53 (29.61) |
|
|
| Grade
III | 112 (55.17) | 82 (45.81) |
|
|
Discussion
The incidence of PHC and TC has risen in recent
years. However, the pathogenesis of the diseases has not been
elucidated. PHC and TC are often in advanced stages when there are
clear symptoms and the patients seek medical assistance due to no
symptoms in the early stages, which increases the difficulty of
clinical intervention (11,12). Therefore, early diagnosis of PHC and
TC, as well as timely effective treatments, is of great
significance to patients' survival and prognosis. As medical
technologies are advancing, two-dimensional and color Doppler
ultrasonography have gradually been applied clinically to the early
screening of malignant tumors. The two ultrasound-based
technologies have high resolution, and can clearly show the
location, size, morphology, internal echo, and blood flow
distribution of lesions. In the clinic, ultrasonography has become
the preferred imaging method for malignant tumors, and is playing
an important role in severity assessment of malignant tumors and
decision making of treatment plan, as well as prediction of
prognosis (13,14).
Two-dimensional and color Doppler ultrasonography
have been playing an important role in the clinical screening and
diagnosis of malignant tumors. Two-dimensional ultrasonography can
clearly show the specific location, size and morphology of lesions.
Color Doppler ultrasonography has a high diagnostic value in
differentiating benign and malignant lesions in patients with rich
blood flow in the liver (15). In
this study, the sensitivity, specificity and accuracy of the
ultrasonic diagnosis of PHC were 78.32, 71.00 and 74.88%,
respectively. Through analysis of the sonograms, most of the PHC
foci were found to be in a regular shape and have a diameter of
>3 cm. Narrow halo signs were visible around the lesions. The
lesioned tissue was homogeneous in composition, consisting of
densely packed cancer cells. A high-velocity and low-impedance
blood flow spectrum was observed, indicating a rich blood flow
inside the lesioned tissue. Enlarged arterial branches and
increased blood flow were observed around the tumor. However, some
lesions of small hepatocellular carcinoma showed an isoechoic
internal echo texture, and appeared to have no halo sign and no
mosaic pattern. Missed diagnosis and misdiagnosis easily occur
under these circumstances. Therefore, precautions were taken in the
process to avoid diagnostic errors. In this study, the differences
in the sonographic features such as focus morphology, focus size,
internal echo, halo and blood flow distribution were statistically
significant between patients in the PHC and the benign liver lesion
group (p<0.001). This finding suggested that PHC can be
differentiated from benign liver lesions by evaluation of focus
morphology, focus size, internal echo, halo, and blood flow
distribution. The differential diagnosis had a good diagnostic
rate. In a similar study reported by Bhartia et al, lesions
of PHC in 316 patients showed irregular morphology, hypoechoic
internal echo texture, and homogeneity in composition (16). The reported differential diagnosis of
PHC also had a good diagnostic rate.
Two-dimensional and color Doppler ultrasonography
are the most commonly used techniques in diagnosis of TC. Al-Hilli
et al reported that sonographic features, such as irregular
morphology, unclear boundary, aspect ratio of ≥1, hypoechoic
internal echo, calcification and internal low blood supply, can be
used to differentiate malignant thyroid nodules from benign ones
(17). Especially, the three
sonographic features, i.e., unclear boundary, aspect ratio of ≥1
and calcification, were regarded as typical of thyroid malignancies
(17). In this study, the
sensitivity, specificity and accuracy of the ultrasonic diagnosis
of TC were 79.27, 75.86 and 77.65%, respectively. Through analysis
of the sonograms, most of the TC nodules were found to have an
unclear boundary, a size of >1 cm, and show a hypoechoic
internal echo texture, microcalcifications, rich internal blood
flow, abnormal blood vessels, and internal enlarged arteries. In
addition, tumor cells were large and overlapping, and had little
interstitial fluid. There were no interfaces allowing strong
reflection. Some thyroid follicular and medullary carcinomas showed
a hyperechoic internal echo texture, regular morphology and a clear
boundary. Cystic lesions or necrosis were found in large cancer
tissues. The calcification was deposition of calcium salts due to
proliferation of fibrous components and blood vessels while tumor
cells were rapidly growing. It may also be the calcified substances
formed in tumor cell metabolism (18). When calcification is found, much
attention should be paid to the possible thyroid malignancy.
Fukuoka et al reported that calcification was closely
associated with papillary TC and represented the major sonographic
feature in its ultrasonography (19).
Lymph node metastasis was commonly observed in papillary TC,
presenting typical sonographic features such as enlarged lymph
nodes, a heterogeneous internal echo texture, rich and disorderly
blood flow, and calcification. In this study, the differences in
the sonographic features such as nodule boundary, nodule size,
internal echo pattern, microcalcification, lymph node status and
blood flow distribution were statistically significant between
patients in the TC and the benign thyroid nodule group (p<0.01).
This finding suggested that TC can be differentiated from benign
thyroid nodules by evaluation of nodule boundary, nodule size,
internal echo pattern, microcalcification, lymph node status, and
blood flow distribution. This differential diagnosis had a good
diagnostic rate. Our results were different from those in a recent
report, in which the ultrasonic diagnosis using high frequency
color Doppler ultrasonography gave low sensitivity, specificity and
accuracy (52.4, 43.8 and 54.9%, respectively) in 415 patients with
thyroid nodules. In addition, the rate of missed diagnosis and
misdiagnosis was high (20). The
discrepancy might be due to differences in subjects enrolled in the
studies and in instruments used. Further studies may be needed to
validate the differential diagnosis.
To ensure reliability of the research results in
this study, a large number of subjects were recruited, following
the strict inclusion and exclusion criteria. As a diagnostic
technique, ultrasonography is convenient, fast, cost-efficient and
non-invasive, and has high diagnostic rate. Therefore, in the
clinic it is the preferred imaging diagnostic tool for malignant
tumors. However, there were still some cases of missed diagnosis
and misdiagnosis for PHC and TC in this study. The sonographic
features, as well as diagnostic decisions, were susceptible to
various factors such as obesity, internal gas, breathing, angles,
and body position. Thus, ultrasonography still had some limitations
in the diagnosis of liver and thyroid diseases. It is hoped that in
the near future a more effective, fast and non-invasive way could
be found in the screening and diagnosis of PHC and TC.
In conclusion, PHC can be differentiated from benign
liver lesions by evaluation of focus morphology, focus size,
internal echo pattern, halo, and blood flow distribution. TC can be
differentiated from benign thyroid nodules by evaluation of nodule
boundary, nodule size, internal echo pattern, microcalcification,
lymph node status, and blood flow distribution. Ultrasonic
diagnosis of PHC and TC is not only accurate, but also convenient,
fast, cost-efficient and non-invasive. Thus, application of
ultrasonography in the diagnosis of PHC and TC should be expanded
for the benefit of patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LW drafted this manuscript. LW and XP were mainly
devoted on liver ultrasonic examination. JQ helped with thyroid
ultrasonic examination. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Liaocheng People's Hospital, (Liaocheng, China). Signed written
informed consents were obtained from the patients or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bhaijee F, Krige JE, Locketz ML and Kew
MC: Liver resection for non-cirrhotic hepatocellular carcinoma in
South African patients. S Afr J Surg. 49:68–74. 2011.PubMed/NCBI
|
|
2
|
Schlumberger M, Elisei R, Müller S,
Schöffski P, Brose M, Shah M, Licitra L, Krajewska J, Kreissl MC,
Niederle B, et al: Overall survival analysis of EXAM, a phase III
trial of cabozantinib in patients with radiographically progressive
medullary thyroid carcinoma. Ann Oncol. 28:2813–2819. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Khalaf N, Ying J, Mittal S, Temple S,
Kanwal F, Davila J and El-Serag HB: Natural history of untreated
hepatocellular carcinoma in a US cohort and the role of cancer
surveillance. Clin Gastroenterol Hepatol. 15:273–281.e1. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu J, Marcaccio MJ, Young JE, Aziz T, Wat
J and Asa SL: Pancreatic struma with papillary thyroid carcinoma: A
diagnostic dilemma. Endocr Pathol. 28:91–94. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sia D, Villanueva A, Friedman SL and
Llovet JM: Liver cancer cell of origin, molecular class, and
effects on patient prognosis. Gastroenterology. 152:745–761. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Elisei R, Schlumberger MJ, Müller SP,
Schöffski P, Brose MS, Shah MH, Licitra L, Jarzab B, Medvedev V,
Kreissl MC, et al: Cabozantinib in progressive medullary thyroid
cancer. J Clin Oncol. 31:3639–3646. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhou J, Luo Y, Ma BY, Ling WW and Zhu XL:
Contrast-enhanced ultrasound diagnosis of hepatic metastasis of
concurrent medullary-papillary thyroid carcinoma: A case report.
Medicine (Baltimore). 96:e90652017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Li F, Han J, Han F, Wang JW, Luo RZ, Li AH
and Zhou JH: Combined hepatocellular cholangiocarcinoma
(biphenotypic) tumors: Potential role of contrast-enhanced
ultrasound in diagnosis. AJR Am J Roentgenol. 209:767–774. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hong YR, Luo ZY, Mo GQ, Wang P, Ye Q and
Huang PT: Role of contrast-enhanced ultrasound in the pre-operative
diagnosis of cervical lymph node metastasis in patients with
papillary thyroid carcinoma. Ultrasound Med Biol. 43:2567–2575.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xu B, Scognamiglio T, Cohen PR, Prasad ML,
Hasanovic A, Tuttle RM, Katabi N and Ghossein RA: Metastatic
thyroid carcinoma without identifiable primary tumor within the
thyroid gland: A retrospective study of a rare phenomenon. Hum
Pathol. 65:133–139. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kitahata S, Hiraoka A, Kudo M, Murakami T,
Ochi M, Izumoto H, Ueki H, Kaneto M, Aibiki T, Okudaira T, et al:
Abdominal ultrasound findings of tumor-forming hepatic malignant
lymphoma. Dig Dis. 35:498–505. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gannon AW, Langer JE, Bellah R, Ratcliffe
S, Pizza J, Mostoufi-Moab S, Cappola AR and Bauer AJ: Diagnostic
accuracy of ultrasound with color flow Doppler in children with
thyroid nodules. J Clin Endocrinol Metab. Mar 12–2018.(Epub ahead
of print). View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ling W, Qiu T, Ma L, Lei C and Luo Y:
Contrast-enhanced ultrasound in diagnosis of primary hepatic
angiosarcoma. J Med Ultrason (2001). 44:267–270. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shin JH, Baek JH, Chung J, Ha EJ, Kim JH,
Lee YH, Lim HK, Moon WJ, Na DG, Park JS, et al Korean Society of
Thyroid Radiology (KSThR), ; Korean Society of Radiology, :
Ultrasonography diagnosis and imaging-based management of thyroid
nodules: Revised Korean Society of thyroid radiology consensus
statement and recommendations. Korean J Radiol. 17:370–395. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Saitta C, Raffa G, Alibrandi A,
Brancatelli S, Lombardo D, Tripodi G, Raimondo G and Pollicino T:
PIVKA-II is a useful tool for diagnostic characterization of
ultrasound-detected liver nodules in cirrhotic patients. Medicine
(Baltimore). 96:e72662017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bhartia B, Ward J, Guthrie JA and Robinson
PJ: Hepatocellular carcinoma in cirrhotic livers: Double-contrast
thin-section MR imaging with pathologic correlation of explanted
tissue. AJR Am J Roentgenol. 180:577–584. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Al-Hilli Z, Strajina V, McKenzie TJ,
Thompson GB, Farley DR and Richards ML: The role of lateral neck
ultrasound in detecting single or multiple lymph nodes in papillary
thyroid cancer. Am J Surg. 212:1147–1153. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Haugen BR, Alexander EK, Bible KC, Doherty
GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM,
Schlumberger M, et al: 2015 American Thyroid Association management
guidelines for adult patients with thyroid nodules and
differentiated thyroid cancer: The American Thyroid Association
guidelines task force on thyroid nodules and differentiated thyroid
cancer. Thyroid. 26:1–133. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fukuoka O, Sugitani I, Ebina A, Toda K,
Kawabata K and Yamada K: Natural history of asymptomatic papillary
thyroid microcarcinoma: Time-dependent changes in calcification and
vascularity during active surveillance. World J Surg. 40:529–537.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gong B, Liu JD, Ying H, Wang T and Jia M:
The diagnostic analysis of high frequency color Doppler ultrasound
in thyroid cancer. Proceedings of the 2015 International Conference
on Medicine and Biopharmaceutical (China). Med Biopharmaceut.
245–250. 2016. View Article : Google Scholar
|