Introduction
Colorectal cancer is considered thethird highest
malignancy in the United States, causing >55,000
mortalities/year (1). Environmental
and genetic factors influence the progression of colorectal cancer,
which is characterized by inflammation arising from various causes
(2). The most common type of chronic
intestinal inflammation associated with colorectal cancer is
inflammatory bowel disease, which includes ulcerative colitis (UC)
and Crohn's disease (CD). Colorectal cancer caused by inflammatory
bowel disease is referred to as colitis-associated cancer
(CAC).
CAC in patients with UC is caused by unifocal or
multifocal dysplastic mucosa in chronic inflammatory regions
(3). UC has been reported to increase
the risk of CAC by approximately eight-fold in comparison to the
general population (4). The degree
and duration of the disease, and the number of flares have been
recognized as risk factors, suggesting that uncontrolled
inflammation may drive tumorigenesis (5). Chronic inflammation has been proposed to
increase epithelial cell turnover in the colonic mucosa, resulting
in accelerated aging of colonic mucosa, and enhanced vulnerability
for acquiring genetic and epigenetic alternations (2). These results suggest that age-associated
inflammation may be used for the identification of patients with UC
with an increased risk of manifesting CAC later in life (6).
The molecular mechanisms underlying
inflammation-mediated cancer development are not fully understood,
and may differ between CAC and other forms of colorectal cancer.
The involvement of cytokines and immune mediators is well
understood in virtually all stages of colonic tumorigeneses,
including tumor initiation, promotion, progression and metastasis
(7). The pathogenesis of CAC is
affected by several cytokines. Interleukin (IL)-9 forms part of the
c-chain family of cytokines. Several types of cells receptive to
IL-9 exist, including mast, T, antigen-presenting and epithelial
cells, all of which are found in the human lung and gut (8). IL-9 also exhibits downstream regulatory
activities on epithelial cells in the airway and intestinal mucosa
barrier, where overexpression of IL-9 induces airway
hyper-responsiveness and increases intestinal permeability
(9). Previous research has recognized
that IL-9 serves an important role in the pathogenesis of several
chronic inflammatory and autoimmune diseases, including
inflammatory bowel disease, multiple sclerosis, lupus erythematous,
food allergies and asthma (10). For
instance, Gerlach et al confirmed that IL-9 expression is
associated with UC, whereby IL-9 expression is markedly increased
in patients diagnosed with UC compared with healthy control
participants and generally highest in patients with the more severe
form of the disease (11). Based on
these findings, we hypothesized that IL-9 inhibits the mucosal
healing process, the subsequent exacerbation of inflammation and
the formation of chronic lesions. In addition, IL-9 may mediate
cell proliferation and serve catalytic role in CAC
pathogenesis.
Inflammation is considered a cellular stressor that
initiates DNA damage or genetic instability. Chronic inflammation
may induce genetic abnormalities and epigenetic mechanisms, which
can subsequently mediate malignant cell alteration. The nuclear
transcription factor MYC proto-oncogene bHLH transcription factor
(c-Myc) is part of the Myc gene family and has been
reported to have multiple functionsas an important oncogene
(12). Given that it is an essential
transcription regulator, the activation of c-Myc may
accelerate cell cycle progression and induce cell apoptosis
(13). c-Myc is upregulated in
various types of malignant tumor, including colorectal cancer, and
is considered compulsory for the uncontrolled proliferation of
cancer cells (14). According to
whole-exome sequencing analysis, the c-Myc genomic locus has
been reported to be frequently expressed in CAC compared with
sporadic colorectal cancer (15).
Cyclins were named following their periodic cell cycle-dependent
pattern of expression. Notably, cyclin D1 is considered the
most popular given its widespread role in human cancer with a
larger depth of functional characterization. Cyclin D1 is
recognized as a proto-oncogene, whose overexpression is able to
cause cell proliferation to become malignant and uncontrolled
(16). Studies have reported the
overexpression of cyclin D1 gene in a variety of cancer
types, including breast cancer, bladder cancer, parathyroid
neoplasms, lymphoma, melanoma andlung cancer (17–22).
The present study aimed to examine the expression of
IL-9 in CAC colorectal tissue specimens and the determine effect of
IL-9 on cell proliferation. The results demonstrated that IL-9 was
overexpressed in CAC tissues compared with adjacent tissues, and
IL-9 overexpression promoted the growth of colonic epithelial cells
by upregulating the expression of c-Myc and
cyclinD1.
Materials and methods
Patients and tissue specimens
The present study was approved by the Research
Ethics Committee of the First Hospital of Shanxi Medical University
(Taiyuan, China). All patients agreed to participate and signed
informed consent forms. The study used 12 (8 male and 4 female)
colorectal tissue specimens from patients with CAC and
tumor-adjacent tissues as a control. The median age of patients was
72.5 years (72.5±17.3 years) at the time of surgery. The specimens
were collected from Department of Pathology at the First Hospital
of Shanxi Medical University between June 2010 and December 2017.
The diagnosis of CAC was founded on medical history, endoscopic
findings, histological examination, laboratory tests and clinical
disease presentation.
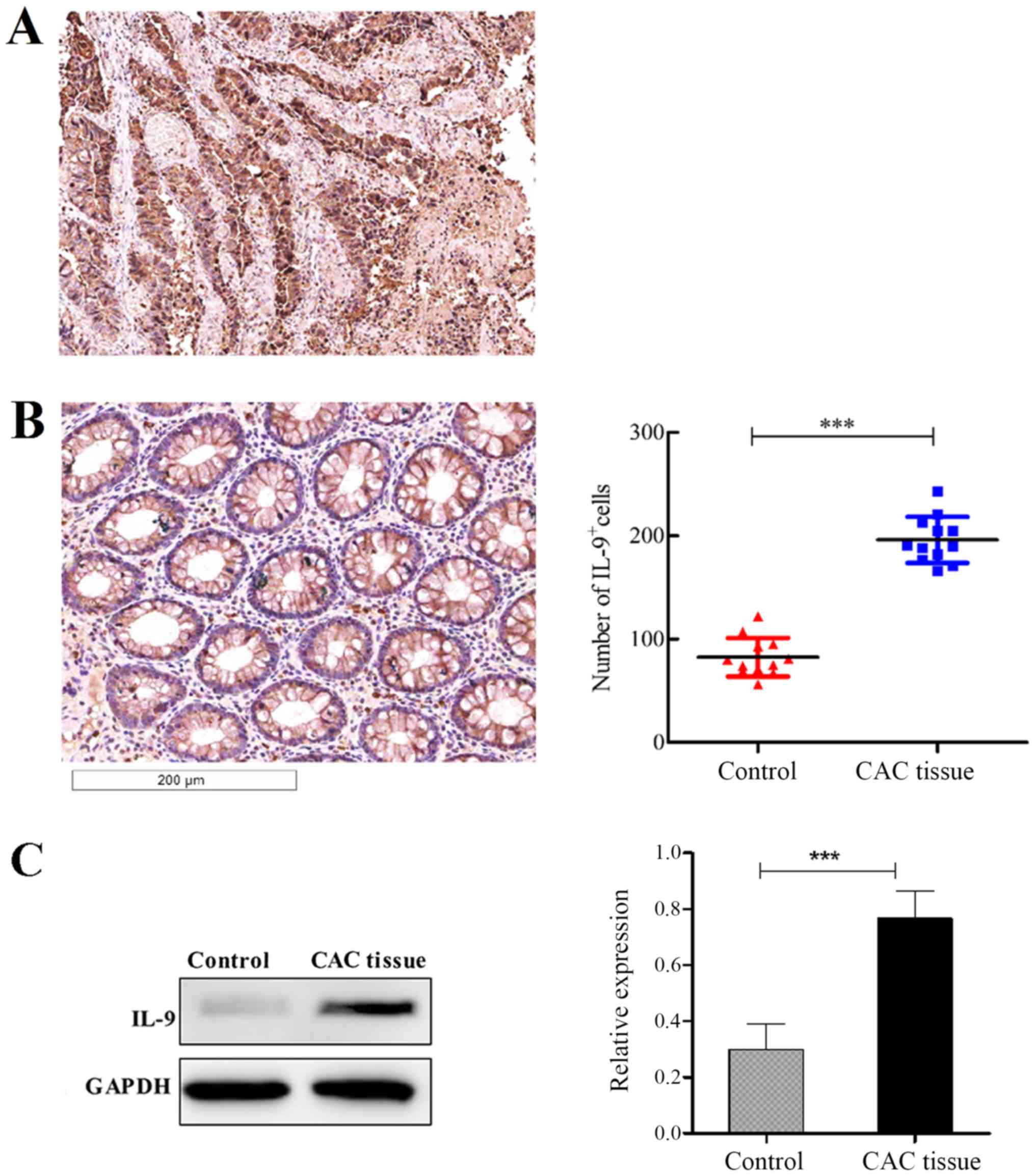
Immunohistochemistry
A total of 12 paired formalin-fixed,
paraffin-embedded samples were subjected to immunohistochemistry
staining for IL-9. Briefly, the cancer tissues were fixed in 4%
paraformaldehyde at 4°C for 48 h. Following dehydration, the
tissues were sliced at 4 µm thickness and blocked in 10% bovine
serum albumin (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at
room temperature for 30 min, followed by incubating with rabbit
anti-human IL-9 monoclonal antibody (cat. no. A1894; 1:50-1:200;
ABclonal Biotech Co., Ltd., Woburn, MA, USA) at 4°C overnight. The
slices were incubated with goat anti-rabbit IgG horseradish
peroxidase (HRP)-conjugated secondary antibody (cat. no. SPN-9001;
1:100; OriGene Technologies, Inc., Rockville, MD, USA) at room
temperature for 2 h. The SCANSCOP Digital Pathology Scanning system
(Aperio Technologies, Inc., Vista, CA, USA) was used forscanning of
pathological slices. Under alight microscope, five representative
high magnification fields of vision were selected for each slice,
and the number of IL-9-positive immunization cells was counted. The
mean value represents the IL-9 positive degree of the case.
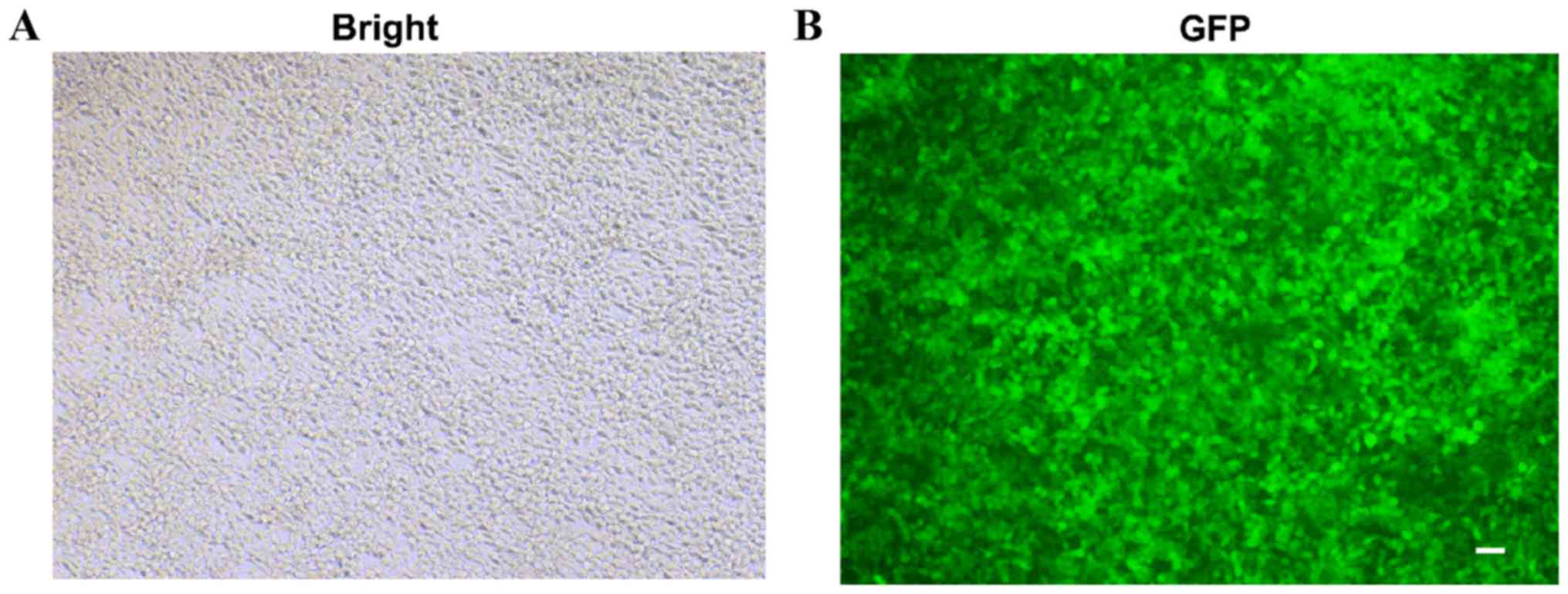
Construction of lentivirus
overexpressing IL-9
The gene sequence of IL-9 was based on National
Centre for Biotechnology Information (NM_000590.1, http://www.ncbi.nlm.nih.gov/nuccore/NM_000590.1),
and the Basic Local Alignment Search Tool (BLAST) sequence was
produced using DNAMAN software (version 6.0; Lynnon LLC, San Ramon,
CA, USA). Overexpression lentiviral vector pGV367 and
AgeI/NheI Restriction endonuclease were purchased
from Shanghai GenechemCo., Ltd. (Shangahi, China). Human IL-9 was
cloned from the human genome with the following primers: IL-9
forward, 5′-GAGGATCCCCGGGTACCGGTCGCCACCATGCTTCTGGCCATGGTCCTTAC-3′
and reverse, 5′-CACACATTCCACAGGCTAGTCATATCTTGCCTCTCATCCCTCTCATC-3′.
The lentivirus vector plasmid pGV367 and the IL-9 gene sequence
were digested by AgeI and NheI restriction enzymes.
Recombinant lentiviral vector was detected by DNA sequencing.
Following exact matching of the sequencing, pGV367-IL-9 was
cotransfected with two assistant plasmids pHelp 1.0 and pHelp 2.0
into 293 cells (purchased from the Type Culture Collection of the
Chinese Academy of Sciences, Shanghai, China) to establish the
recombinant lentivirus expressing IL-9 (LV-IL-9). LV-negative
control (NC) contains empty gene sequence was used as lentivirus
control group. All the vectors were purchased from Shanghai
GeneChem Co., Ltd.
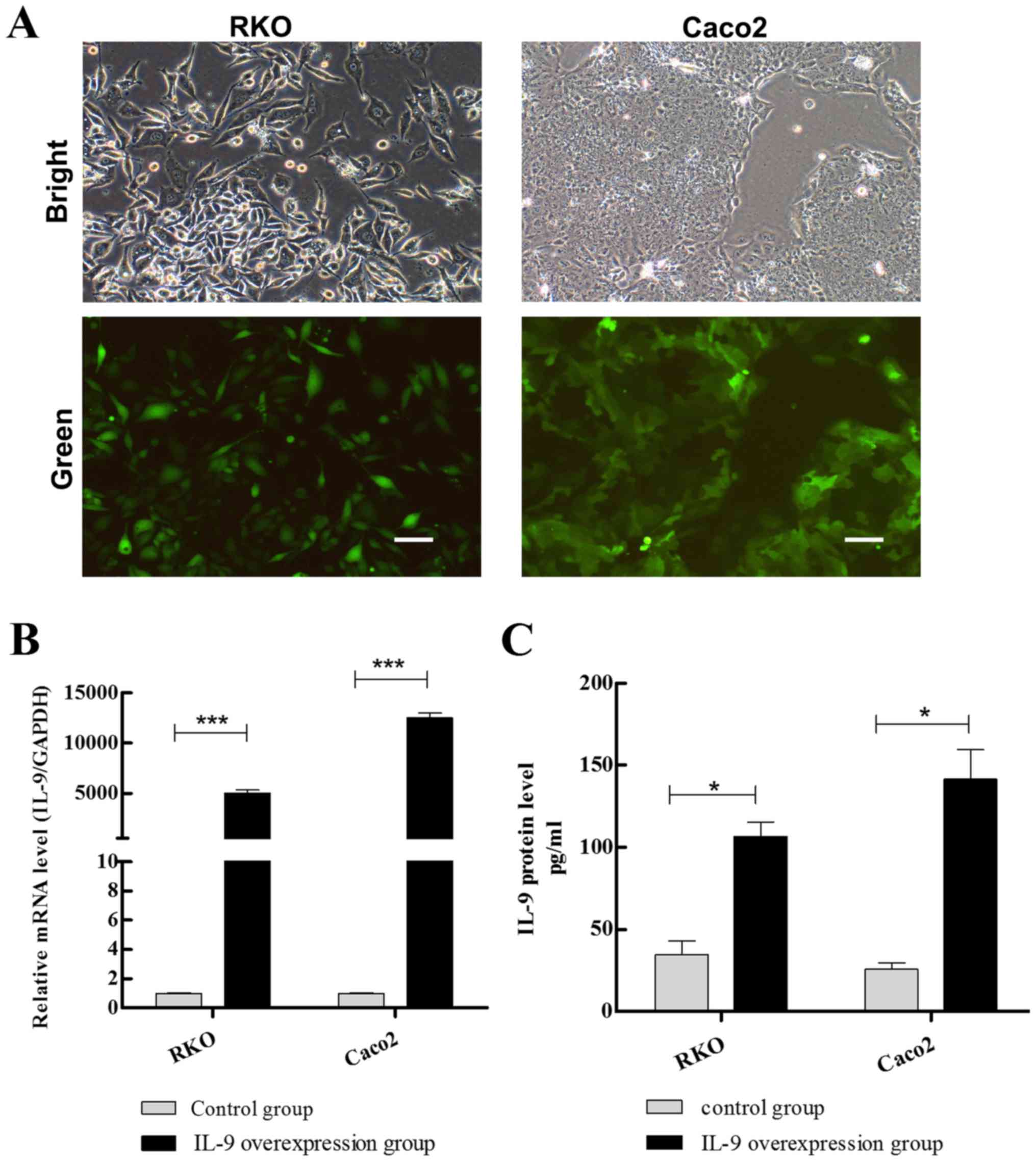
Cell culture and LV-IL-9
transfection
Colorectal cancer cell RKO and Caco2 cells are
adherent cells, and purchased from the Type Culture Collection of
the Chinese Academy of Sciences (Shanghai, China). Caco2 cells were
cultured in Dulbecco's modified Eagle medium (Gibco; Thermo Fisher
Scientific, Inc., Waltham, MA, USA) supplemented with 10% fetal
bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.),
L-glutamine (2 mM), penicillin (100 U/ml) and streptomycin (100
mg/ml) at 37°C with 5% CO2. RKO cells were cultured in
RPMI-1640 (Gibco; Thermo Fisher Scientific, Inc.) supplemented with
10% FBS (Gibco; Thermo Fisher Scientific, Inc.), 1%
penicillin/streptomycin (Life Technologies; Thermo Fisher
Scientific, Inc.) at 37°C with 5% CO2. RKO and Caco2
cells were infected with LV-IL-9 with amultiplicity of infection
(MOI) of 10 and 20 respectively at 80% confluence. Subsequently,
the expression of enhanced green fluorescent protein (GFP) was
observed by fluorescence microscope at a ×200 magnification (IX71;
Olympus Corporation, Tokyo, Japan).
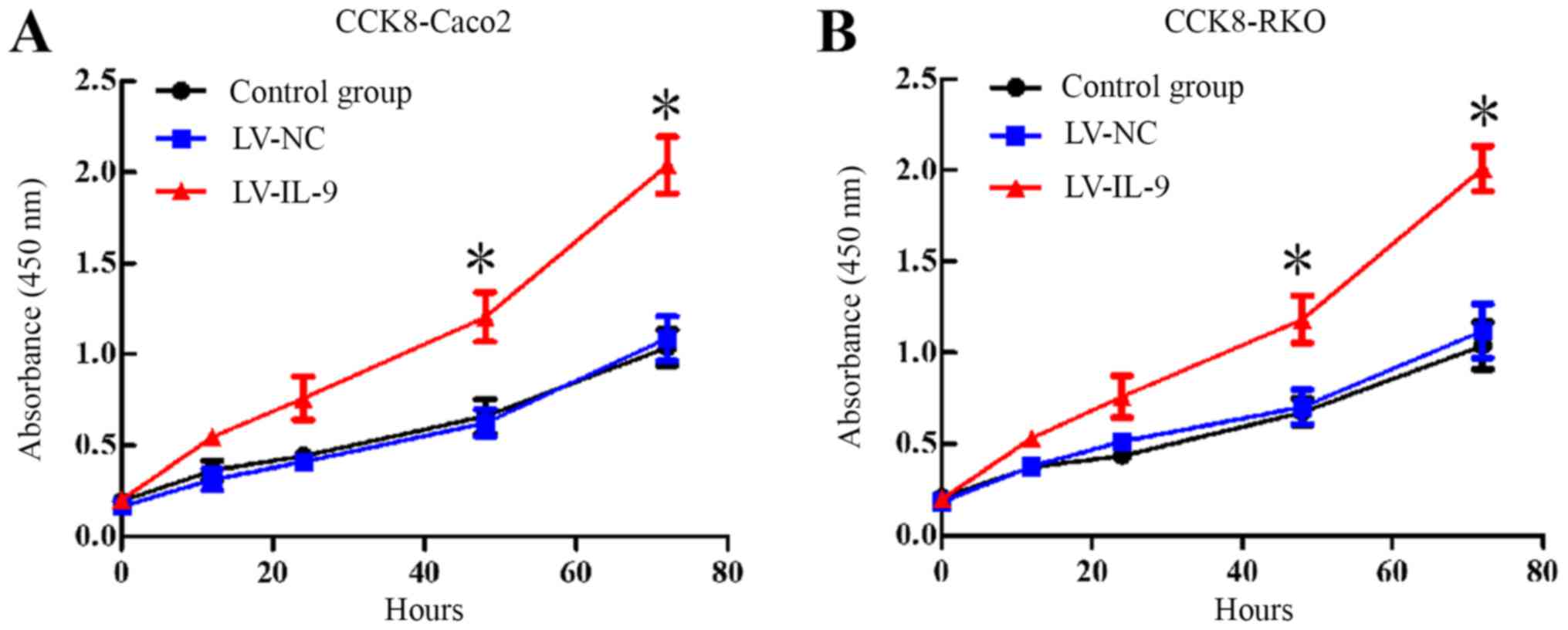
Cell proliferation assay
Cell proliferation was investigated and determined
using Cell Counting Kit 8 (CCK8; cat. no. AR1160-500; Wuhan Boster
Biological Technology, Ltd., Wuhan, China). RKO and Caco2 cells
were seeded into 96-well plates at a density of 2×103
cells/well in 100 µl of culture medium, and infected with LV-IL-9
at a MOI of 20 or with LV-NC (2 µl) (n=6) for 0, 12, 24, 48 and 72
h in a 5% CO2 humidified incubator at 37°C.
Subsequently, the cells were then incubated with 10 µl of CCK8/well
for 30 min at 37°C. The optical density of each well was assessed
at 450 nm using a microplate reader.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was isolated from RKO and Caco2 cells
using TRIzol (Invitrogen; Thermo Fisher Scientific, Inc.) according
to the manufacturer's protocol. RNA was reverse transcribed the
using Advantage® RT-for-PCR kit (cat. no. 639505; Takara
Biotechnology Co., Ltd., Dalian, China) according to the
manufacturer's protocol. Subsequently, the cDNA was subjected to
RT-qPCR analysis. Amplification was performed as follows: Initial
incubation at 95°C for 10 sec; followed by 40 cycles at 95°C for 5
sec and at 62°C for 45 sec; and extension at 72°C for 3 min. The 25
µl PCR reaction system included 1 µl cDNA temple, 2 µl primers, 2
µl dNTP, 0.5 µl RT/Platinum™ Taqmix (Invitrogen; Thermo
Fisher Scientific, Inc.) and distilled water. RT-qPCR was performed
using the T100-Thermal Cycler Real-Time PCR system (Bio-Rad
Laboratories, Inc., Hercules, CA, USA). Gene expression was
normalized to the levels of the internal reference GAPDH using the
2−ΔΔCq method (23). Each
sample was assessed in triplicate and the mean expression level was
determined. The following primers were used: c-Myc forward,
5′-TTCGGGTAGTGGAAAACCAG-3′ and reverse, 5′-AGCAGATCGAATTTCTTCCA-3′;
cyclinD1 forward, 5′-GAGGAAGAGGAGGAGGAGGA-3′ and reverse,
5′-GAGATGGAAGGGGGAAAGAG-3′; B cell lymphoma-2 (Bcl-2)
forward, GGATGCCTTTGTGGAACTGT-3′ and reverse,
5′-AGCCTGCAGCTTTGTTTCAT-3′; Bcl-2 associated X protein
(Bcl-xL) forward, 5′-TCTGGTCCCTTGCAGCTAGT-3′ and reverse,
5′-ATTCTGAGGCCAAGGGAACT-3′; surviving forward,
5′-ACCTGAAAGCTTCCTCGAGA-3′ and reverse, 5′-AACCCTTCCCAGACTCCACT-3′;
induced myeloid leukemia cell differentiation protein Mcl-1 homolog
(Mcl-1) forward, 5′-TGCTGGAGTAGGAGCTGGTT-3′ and reverse,
5′-CCTCTTGCCACTTGCTTTTC-3′; GAPDH forward,
5′-CCACCTTCGATGCCGGGGCT-3′ and reverse,
5′-GGGGCCGAGTTGGGATAGGG-3′.
Western blot analysis
The colorectal tissue specimens from patients with
CAC and tumor-adjacent tissues were pulverized and lysed with RIPA
buffer (Beyotime Institute of Biotechnology, Beijing, China)
containing proteinase inhibitor cocktail (cat. no. P8340;
Sigma-Aldrich; Merck KGaA). Protein concentration was measured
using a bicinchoninic acid protein assay kit. A total of 60 µg
protein were subjected to 12% SDS-PAGE and transferred onto
polyvinylidene difluoride membranes. Subsequently, the membranes
were blocked in 5% fat-free milk for 2 h at room temperature and
incubated with the following primary antibodies overnight at 4°C:
Rabbit polyclonal anti-IL9 (1:500; cat. no. ab111915; Abcam,
Cambridge, UK) and rabbit monoclonal anti-GAPDH (1:500; cat. no.
AF1186; Beyotime Institute of Biotechnology). Following incubation
with the HRP-conjugated secondary antibodies from Santa Cruz
Biotechnology, Inc. (1:2,000; cat. no. sc-2004, goat anti-rabbit
IgG-HRP; cat. no. sc-2005) for 2 h at room temperature, the
membranes were visualized using the ECLPlus kit (GE Healthcare,
Chicago, IL, USA).
Enzyme-linked immunosorbent assay
(ELISA)
Concentrations of IL-9 were detected in the culture
medium of RKO cells and Caco-2 cells using solid phase sandwich
ELISA according to the manufacturer's protocols of ELISA kit (cat.
no. BMS208196T, eBioscience; Thermo Fisher Scientific, Inc.). The
hormone assay sensitivity was set at 0.1 pg/ml and the assay range
was 3.1–200 pg/ml. For statistical analysis, the culture medium was
independently collected three times. The ELISA kit for IL-9 was
purchased from eBioscience (Thermo Fisher Scientific, Inc.).
Statistical analysis
All group data are presented as the mean ± standard
deviation. Comparisons among the three groups were performed using
one-way analysis of variance, using the Fisher's least significant
difference test for multiple comparisons. The Student's t-test was
applied to analyze the differences between two groups. P<0.05
was considered to indicate a statistically significant difference.
All statisticalanalys is was performed using GraphPad Prism 5.0
software (GraphPadSoftware, Inc., La Jolla, CA, USA).
Results
IL-9 expression is upregulated in CAC
tissues
A total of 12 patients with CAC were enrolled for
the present study, including eight males (66.7%) and four females
(33.3%), with a mean age of 72.5±17.3 years, and a history of
ulcerative colitis (lasting 25.8±3.8 years). The basic clinical
information of the patients was obtained by consulting their
disease history.
While IL-9 involvement in atopic diseases has been
previously established (24), its
expression in patients with CAC remains to be elucidated. To
investigate the potential role of IL-9 in CAC, IL-9 expression
levels were determined. Among the 12 cases of CAC, all had IL-9
expression in the intestinal mucosal epithelial cells and
inflammatory cell cytoplasm (Fig.
1A). It was demonstrated that the number of IL-9-positive cells
in the intestinal mucosa was significantly increased compared with
that in paracancerous tissues (Fig.
1B; P<0.001). Furthermore, the western blot analysis results
demonstrated that IL-9 protein expression was significantly
increased in CAC tissues (Fig. 1C;
P<0.001).
Identification of IL-9 gene
overexpression usinglentivirus vector
The BLAST results for the IL-9 cDNA sequence
determined that the expected IL-9 gene sequence was completely
consistent. It was confirmed that the IL-9 was correctly inserted
into the vector and that the IL-9 overexpression lentivirus vector
was successfully constructed. LV-IL-9-infected 293 cells were
detected by fluorescence microscopy through examining the level of
GFP-positive cells (Fig. 2A and
B).
LV-IL-9 effectively infected colonic
epithelial cells
GFP was observed in RKO and Caco2 cells under a
fluorescence microscope indicating that the lentivirus has been
successfully transfected (Fig. 3A).
The RT-qPCR results demonstrated that IL-9 gene expression in the
Caco-2 overexpression (OE) group was 12,508.689 times that of the
NCgroup (Fig. 3B; P<0.001).
Furthermore, IL-9 gene expression in the RKO OE group was 5,037.700
times that of the NC group (Fig. 3B;
P<0.001). IL-9 protein expression was 141.61±12.28 pg/ml in the
transfected Caco-2 cell medium as determined by ELISA, whereas IL-9
expression was 25.79±5.22 pg/ml in the untransfected group
(Fig. 3C). IL-9 protein level was
106.65±17.45 pg/ml in the transfected RKO medium and 35.23±4.45
pg/ml in untransfected RKO cells (Fig.
3C). The IL-9 protein expression levels were significant
increased in the two OE groups compared with their untransfected
counterparts (P<0.05).
IL-9 overexpression promotes cell
proliferation
The CCK8 assay demonstrated that IL-9 overexpression
induced a significant increase in the proliferation rates of Caco-2
and RKO cells compared with that of the corresponding NC groups
(Fig. 4A and B).
IL-9 overexpression upregulates c-Myc
and cyclinD1 mRNA expression
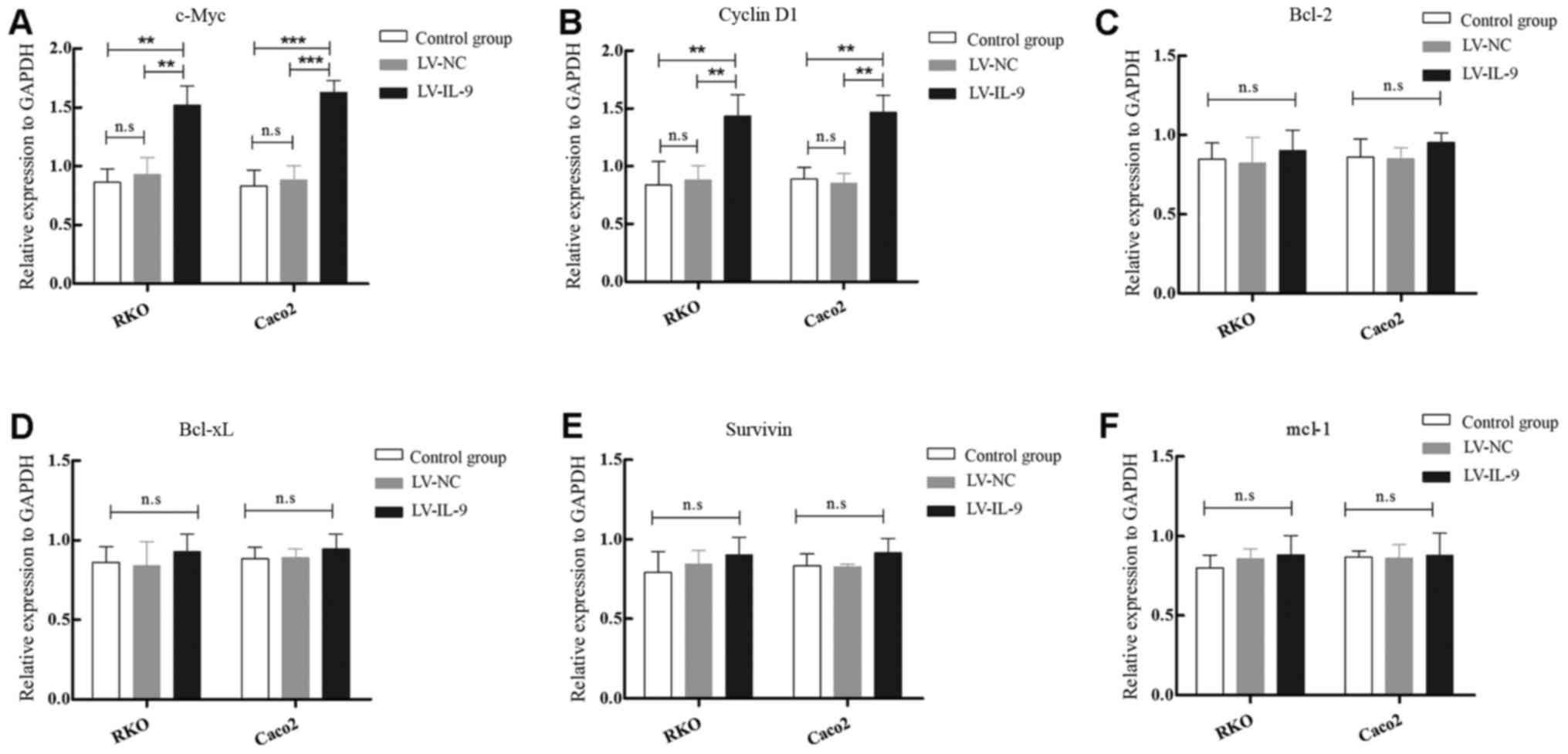
As presented in Fig. 5A
and B, compared with the control and LV-NC groups, the relative
levels of c-Myc and cyclinD1 mRNA were demonstrated
to be significantly increased in Caco-2 and RKO cells infected with
LV-IL-9. However, no significant differences in the expression
levels of Bcl-2, Bcl-xL protein, surviving or Mcl-1 were observed
following IL-9 OE (Fig. 5C-F).
Discussion
IL-9 is considered as a pleiotropic cytokine that
mediates the growth of several types of cells. The role of IL-9 in
tumor immunity is controversial, and its involvement in disease
remains unclear. Research has confirmed that the OE of IL-9 is
associated with the progression of various forms of lymphoma and
leukemia (25,26). However, the expression of IL-9 in CAC
and its clinical importance remain unclear.
In the current study, the expression of IL-9 in
cancer and adjacent colonic mucosa specimens were collected from
patients with CAC between 2010 and 2017, and was analyzed using
immunohistochemistry. The results confirmed that IL-9 is mainly
expressed in intestinal mucosal epithelial cells and inflammatory
cell cytoplasm. The expression of IL-9 in cancer tissues was
markedly higher than that in adjacent tissues, which suggests that
IL-9 may play an important role in the pathogenesis of CAC. Based
on these results, we presume that the expression level of IL-9
fluctuates between cancer types. The objective of our study was to
analyze the colonic biopsy specimens from patients with CAC and
examine how the expression of IL-9 may relate to the
proinflammatory effect of IL-9 in the pathogenesis of UC (27).
To investigate the mechanism of IL-9 function in the
pathogenesis of CAC, we constructed lentivirus expressing IL-9 and
infected RKO and Caco2 cells to study its role on cell
proliferation. The lentiviral vector overexpressing IL-9 gene was
successfully constructed and the lentivirus successfully infected
RKO and Caco2 cells. IL-9 overexpression could promote the
proliferation of colonic epithelial cells by upregulating of the
expression of c-Myc and cyclinD1. In alung cancer
study, Ye et al (28)
demonstrated that the proliferation rate of tumor cells increases
with the IL-9 intervention, suggesting that IL-9 promotes the
growth of lung cancer cells. The present study also showed that the
proliferation of tumor cells increased with the intervention of
IL-9, suggesting that IL-9 promotes the growth of colon cancer
cells, similar to the findings in lung cancer.
The c-Myc gene is typically downregulated in
inflammation, and overexpressed in sporadic and colitis-associated
colon adenocarcinomas. It regulates cell proliferation or
differentiation, and its overexpression is able to induce cell
transformation and tumor formation (29). CyclinD1, as one of the cell
cycle regulatory proteins, is overexpressed in several human tumor
types, including non-small cell lung cancer (30),esophageal cancer (31) and head and neck cancer (32). The observations in the present study
provided evidence that IL-9 overexpression may upregulate the
expression of c-Myc and cyclinD1 in RKO and Caco2
cells as described above. This evidence is in accordance with the
results of a previous study (13).
In conclusion, the results of the present study
demonstrated that IL-9 promoted the proliferation of RKO and Caco2
colonic epithelial cells, partially via the upregulation of
c-Myc and cyclinD1 expression. The results of this
study provide an important experimental basis for further study of
the role of IL-9 in CAC.
Acknowledgements
Not applicable.
Funding
The present study was supported by research grants
from the National Clinical Research Center for Digestive Diseases
(Xi an, China; grant no. 2015BAI13B07).
Availability of data and materials
The datasets generated/analyzed in the present study
are available on reasonable request from the corresponding
author.
Authors' contributions
LH conceived the study, performed the experimental
design and data interpretation, and prepared and revised the
manuscript. LT performed the majority of the experiments. YL and RC
performed the immunohistochemical assay. PZ and JZ performed the
quantitative polymerase chain reaction assay.
Ethics approval and consent to
participate
The present study was approved by the Research
Ethics Committee of the First Hospital of Shanxi Medical University
(Taiyuan, China). All patients agreed to participate and signed
informed consent forms.
Patient consent for publication
The study participants provided consent for the
publication of any associated data/images.
Competing interests
All authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
IL-9
|
interleukin-9
|
|
CAC
|
colitis-associated cancer
|
|
UC
|
ulcerative colitis
|
|
MOI
|
multiple of infection
|
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. doi: 10.3322/caac.21492.
|
|
2
|
Grivennikov SI: Insflammation and
colorectal cancer: Colitis-associated neoplasia. Semin
Immunopathol. 35:229–244. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ordas I, Eckmann L, Talamini M, Baumgart
DC and Sandborn WJ: Ulcerative colitis. Lancet. 380:1606–1619.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Francescone R, Hou V and Grivennikov SI:
Cytokines, IBD, and colitis-associated cancer. Inflamm Bowel Dis.
21:409–418. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Neurath MF: Cytokines in inflammatory
bowel disease. Nat Rev Immunol. 14:329–342. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Toiyama Y, Okugawa Y, Tanaka K, Araki T,
Uchida K, Hishida A, Uchino M, Ikeuchi H, Hirota S, Kusunoki M, et
al: A panel of methylated microRNA biomarkers for identifying
high-risk patients with ulcerative Colitis-associated colorectal
cancer. Gastroenterology. 153:1634–1646. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Antoniou E, Margonis GA, Angelou A,
Zografos GC and Pikoulis E: Cytokine networks in animal models of
colitis-associated cancer. Anticancer Res. 35:19–24.
2015.PubMed/NCBI
|
|
8
|
Neurath MF and Finotto S: IL-9 signaling
as key driver of chronic inflammation in mucosal immunity. Cytokine
Growth Factor Rev. 29:93–99. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Roy DN and Goswami R: IL-9 signaling
Pathway: An update. Methods Mol Biol. 1585:37–50. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Goswami R and Kaplan MH: A brief history
of IL-9. J Immunol. 186:3283–3288. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gerlach K, Hwang Y, Nikolaev A, Atreya R,
Dornhoff H, Steiner S, Lehr HA, Wirtz S, Vieth M, Waisman A, et al:
TH9 cells that express the transcription factor PU.1 drive T
cell-mediated colitis via IL-9 receptor signaling in intestinal
epithelial cells. Nat Immunol. 15:676–686. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kuttler F and Mai S: c-Myc, genomic
instability and disease. Genome Dyn. 1:171–190. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sipos F, Firneisz G and Muzes G:
Therapeutic aspects of c-MYC signaling in inflammatory and
cancerous colonic diseases. World J Gastroenterol. 22:7938–7950.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Farrell AS and Sears RC: MYC degradation.
Cold Spring Harb Perspect Med. 4:doi: 10.1101/cshperspect.a014365.
PubMed/NCBI
|
|
15
|
Robles AI, Traverso G, Zhang M, Roberts
NJ, Khan MA, Joseph C, Lauwers GY, Selaru FM, Popoli M, Pittman ME,
et al: Whole-exome sequencing analyses of inflammatory bowel
disease-associated colorectal cancers. Gastroenterology.
150:931–943. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Qie S and Diehl JA: Cyclin D1, cancer
progression, and opportunities in cancer treatment. J Mol Med
(Berl). 94:1313–1326. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kopparapu PK, Boorjian SA, Robinson BD,
Downes M, Gudas LJ, Mongan NP and Persson JL: Expression of cyclin
d1 and its association with disease characteristics in bladder
cancer. Anticancer Res. 33:5235–5242. 2013.PubMed/NCBI
|
|
18
|
Mudaliar K, Tetzlaff MT, Duvic M, Ciurea
A, Hymes S, Milton DR, Tsai KY, Prieto VG, Torres-Cabala CA and
Curry JL: BRAF inhibitor therapy-associated melanocytic lesions
lack the BRAF V600E mutation and show increased levels of cyclin D1
expression. Hum Pathol. 50:79–89. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ok CY, Xu-Monette ZY, Tzankov A, O'Malley
DP, Montes-Moreno S, Visco C, Møller MB, Dybkaer K, Orazi A, Zu Y,
et al: Prevalence and clinical implications of cyclin D1 expression
in diffuse large B-cell lymphoma (DLBCL) treated with
immunochemotherapy: A report from the International DLBCL
Rituximab-CHOP Consortium Program. Cancer. 120:1818–1829. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Peurala E, Koivunen P, Haapasaari KM,
Bloigu R and Jukkola-Vuorinen A: The prognostic significance and
value of cyclin D1, CDK4 and p16 in human breast cancer. Breast
Cancer Res. 15:R52013. View
Article : Google Scholar : PubMed/NCBI
|
|
21
|
Truran PP, Johnson SJ, Bliss RD, Lennard
TW and Aspinall SR: Parafibromin, galectin-3, PGP9.5, Ki67, and
cyclin D1: Using an immunohistochemical panel to aid in the
diagnosis of parathyroid cancer. World J Surg. 38:2845–2854. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhao W, Hu JX, Hao RM, Zhang Q, Guo JQ, Li
YJ, Xie N, Liu LY, Wang PY, Zhang C and Xie SY: Induction of
microRNAlet7a inhibits lung adenocarcinoma cell growth by
regulating cyclin D1. Oncol Rep. 40:1843–1854. 2018.PubMed/NCBI
|
|
23
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Koch S, Sopel N and Finotto S: Th9 and
other IL-9-producing cells in allergic asthma. Semin Immunopathol.
39:55–68. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Fischer M, Bijman M, Molin D, Cormont F,
Uyttenhove C, van Snick J, Sundström C, Enblad G and Nilsson G:
Increased serum levels of interleukin-9 correlate to negative
prognostic factors in Hodgkin's lymphoma. Leukemia. 17:2513–2516.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lemoli RM, Fortuna A, Tafuri A, Fogli M,
Amabile M, Grande A, Ricciardi MR, Petrucci MT, Bonsi L, Bagnara G,
et al: Interleukin-9 stimulates the proliferation of human myeloid
leukemic cells. Blood. 87:3852–3859. 1996.PubMed/NCBI
|
|
27
|
Weigmann B and Neurath MF: Th9 cells in
inflammatory bowel diseases. Semin Immunopathol. 39:89–95. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ye ZJ, Zhou Q, Yin W, Yuan ML, Yang WB,
Xiong XZ, Zhang JC and Shi HZ: Differentiation and immune
regulation of IL-9-producing CD4+ T cells in malignant pleural
effusion. Am J Respir Crit Care Med. 186:1168–1179. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Casey SC, Baylot V and Felsher DW: The MYC
oncogene is a global regulator of the immune response. Blood.
131:2007–2015. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Jin M, Inoue S, Umemura T, Moriya J,
Arakawa M, Nagashima K and Kato H: Cyclin D1, p16 and
retinoblastoma gene product expression as a predictor for prognosis
in non-small cell lung cancer at stages I and II. Lung cancer.
34:207–218. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Shamma A, Doki Y, Shiozaki H, Tsujinaka T,
Yamamoto M, Inoue M, Yano M and Monden M: Cyclin D1 overexpression
in esophageal dysplasia: A possible biomarker for carcinogenesis of
esophageal squamous cell carcinoma. Int J Oncol. 16:261–266.
2000.PubMed/NCBI
|
|
32
|
Bartkova J, Lukas J, Muller H, Strauss M,
Gusterson B and Bartek J: Abnormal patterns of D-type cyclin
expression and G1 regulation in human head and neck cancer. Cancer
Res. 55:949–956. 1995.PubMed/NCBI
|