Introduction
Lung cancer is a leading cause of cancer-associated
mortality worldwide and 80% of all lung cancer cases are non-small
cell lung cancer (NSCLC) (1). Radical
surgery is the standard treatment for NSCLC. However, a large
number of patients experience disease progression, and therefore, a
poor prognosis, within a short time following resection (2). Although several studies have been
performed, the optimal prognostic factors for facilitating
individualized treatments and an improvement in the prognosis of
patients with NSCLC remain controversial (3). Therefore, it is of great importance to
identify reliable preoperative prognostic variables to perform
prognostic risk stratification and provide individualised
treatment.
Previously, significant attention has been paid to
the association between malignancies and coagulation (4). Among the coagulation factors, fibrinogen
and D-dimer have been widely studied and are regarded as important
prognostic factors in multiple types of solid tumour; including
colorectal (5), uterine (6), cervical (7) and breast carcinoma (8). However, data regarding the prognostic
significance of fibrinogen and D-dimer levels in NSCLC are
lacking.
It has been widely recognized that cancer-related
inflammatory variables, including the neutrophil-lymphocyte ratio
(NLR), platelet-lymphocyte ratio (PLR) and lymphocyte-monocyte
ratio (LMR), serve an important role in the promotion of cell
proliferation, angiogenesis and tumour metastasis, and in the
inhibition of apoptosis (9,10). Recently, an increasing number of
studies have evaluated the prognostic significance of the
combination of fibrinogen and NLR (COF-NLR) to predict
postoperative survival in patients with oesophageal squamous cell
and colon cancer (11–13). However, the prognostic significance of
these two variables in patients with NSCLC has not been fully
investigated.
Therefore, in the present study, a retrospective
analysis was conducted to assess the prognostic relevance of
preoperative coagulation factors and inflammatory indicators in a
cohort of patients with non-metastatic NSCLC. Furthermore, a novel
prognostic score was established by combining the optimal
coagulation and inflammatory indicator status to assess the
prognosis of patients with NSCLC that have undergone a complete
resection.
Patients and methods
Patient selection
A total of 456 histopathologically-confirmed
patients with NSCLC, who had undergone complete pulmonary resection
and systematic lymphadenectomy with curative intent at the
Department of Thoracic Surgery, the First Hospital of Qinhuangdao
between January 2007 and June 2011, were retrospectively analysed.
All patients provided written informed consent for the use of their
information from the hospital database in the present study.
The eligibility criteria for the present study were
as follows: Histopathologically-confirmed primary NSCLC without
distant metastasis, complete surgical resection and systematic node
dissection, no clinical evidence of infection or other inflammatory
conditions, no autoimmune or coagulation disorders, no preoperative
chemotherapy, radiotherapy or other treatment, complete
clinicopathological records, including preoperative coagulation
test, blood cell counts and complete follow-up as described
below.
The preoperative evaluation included a physical
examination, biochemical tests, coagulation tests, complete blood
cell counts, flexible bronchoscopy, chest radiography, computed
tomography (CT) scans, brain magnetic resonance imaging and
radionuclide bone scans. The clinical stage was evaluated on the
basis of the 7th edition of the Tumour-Node-Metastasis (TNM)
classification for NSCLC by the Union for International Cancer
Control (14).
Coagulation measurements and blood
cell count analysis
Fasting preoperative venous blood samples were
obtained within one week prior to surgery and were stored in a
blood collection tube containing EDTA. Preoperative plasma
fibrinogen concentrations were assayed based on the Clauss clotting
method using DADE Thrombin Reagent™ and a Sysmex CA-7000 analyser
(Sysmex Corporation, Kobe, Japan) (15). The plasma D-dimer level was measured
by Microparticle Enzyme-linked Immunoassay using AxSYM analyser
(Abbott Laboratories, Chicago, IL, USA), according to the
manufacturer's protocols.
Complete blood cell counts and differential white
blood cell count analysis of all patients were performed using the
Sysmex XE-5000 automated haematology analyser (cat. no., M349228;
Sysmex Corporation, Kobe, Japan). The NLR was defined as the
neutrophil count/the lymphocyte count. The PLR was defined as the
platelet count/the lymphocyte count. The LMR was defined as the
absolute lymphocyte count/the absolute monocyte count.
Definition of COF-NLR score
The preoperative COF-NLR score was calculated by
combining the fibrinogen and NLR, as previously described (11–13);
patients with elevated plasma fibrinogen and NLR levels were
assigned a score of 2, those that demonstrated elevated levels of
one or neither were assigned a score of 1 and 0, respectively.
Follow-up assessments
Following surgery, all patients received a follow-up
evaluation via verbal or written correspondence or hospital visits
every 3 months for the first year, every 6 months for the second
year and subsequently every year until mortality or the final
follow-up date (June 2016). Physical and laboratory examinations,
as well as imaging studies, were performed at each hospital visit.
Patient check-up included physical examination, tumor-marker
examination, chest radiography, CT scans, neck and abdominal
ultrasonography, and radionuclide bone scans when necessary to
detect recurrence and/or metastasis. Overall survival (OS) time was
calculated as the period from the date of surgery to the date of
the patient's mortality or the final follow-up. The follow-up rate
was 95.6% and the overall median follow-up time of the entire
cohort was 42 months (range, 3–108 months).
Statistical analysis
All statistical analyses were performed using SPSS
software version 18.0 (SPSS, Inc., Chicago, IL, USA). The most
appropriate cut-off values of the preoperative fibrinogen, NLR, PLR
and LMR for survival prediction were calculated using receiver
operating characteristic (ROC) curve analyses. The area under the
curve (AUC) was determined to estimate the diagnostic accuracy. The
χ2 test was used to analyse statistical associations
between categorical variables. The 5-year OS rate was calculated by
Kaplan-Meier analysis and compared using the log-rank test. Factors
identified as potentially significant by univariate analyses
(P<0.05) were entered into a multivariate analysis with Cox
regression model to identify the significant independent prognostic
factors. The foundation of a novel prognostic score was based on
the risk factors identified in the Cox proportional hazard model.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Clinicopathological variables of
patients
A total of 456 patients with NSCLC with complete
clinicopathological records were enrolled in the present study. The
enrolled cohort consisted of 318 (69.7%) males and 138 (30.3%)
females, with a median age of 61 years (range, 35–81 years). Of the
enrolled patients, 387 (84.9%) underwent lobectomy and 69 (15.1%)
underwent pneumonectomy. A total of 238 (52.2%) patients exhibited
squamous cell carcinoma, 157 (34.4%) patients exhibited
adenocarcinoma and 61 (13.4%) patients exhibited an unspecified
type of post-operative pathological subtype. A total of 170
patients presented with stage I TNM, 101 with stage II and 185 with
stage IIIA.
Determination of the appropriate
cut-off values for fibrinogen, NLR, PLR, LMR and D-dimer
levels
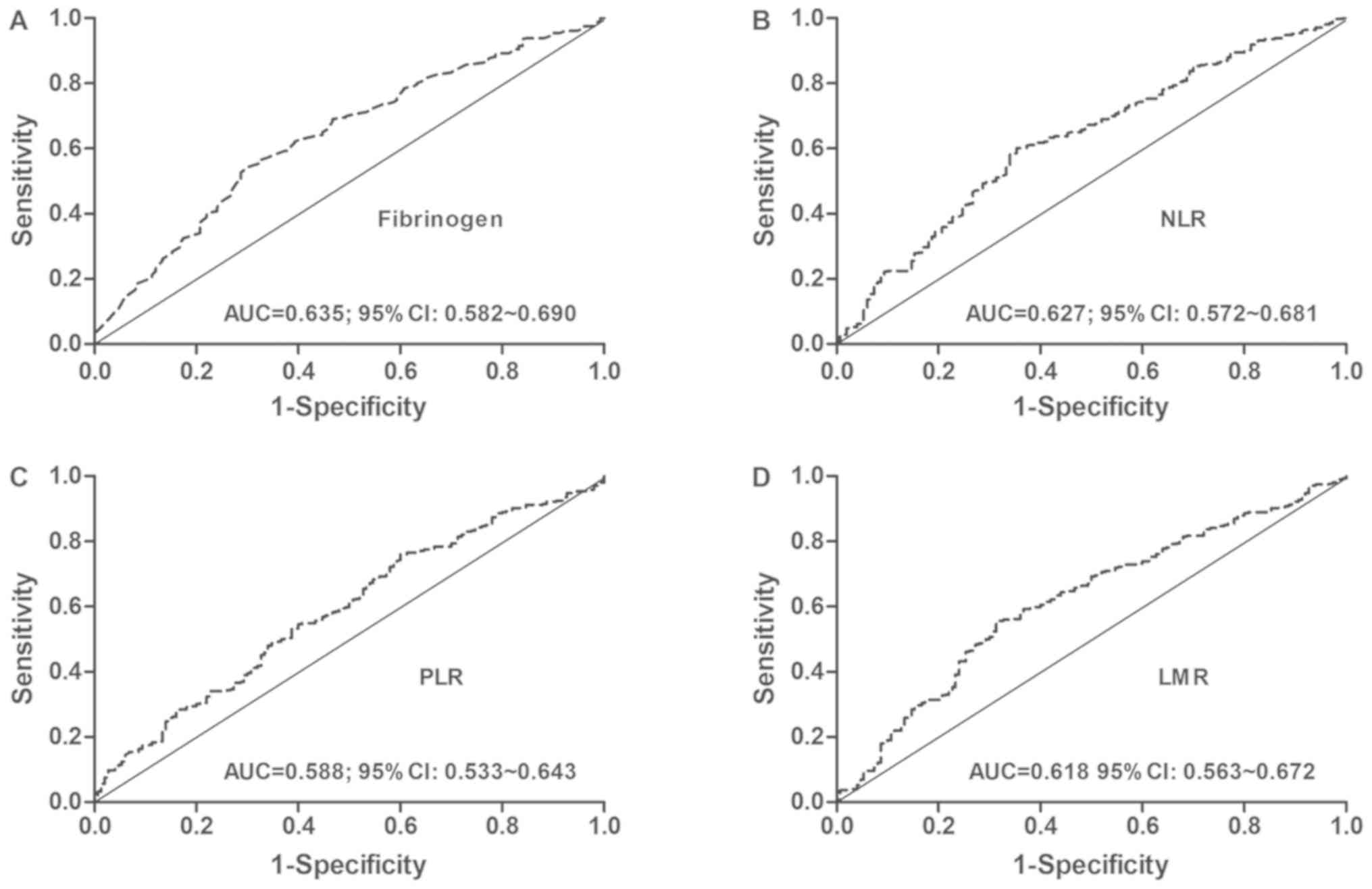
The median value of plasma fibrinogen concentrations
was 3.61 g/l. The optimal fibrinogen cut-off point was 3.77 g/l,
according to the ROC analysis, with an AUC of 0.635 (P<0.001;
Fig. 1A). The median value of NLR was
2.21. The optimal cut-off value was 2.28, according to the ROC
analysis, with an AUC of 0.627 (P<0.001; Fig. 1B). The median value of PLR was 125.45.
The optimal cut-off point was 106.24, according to the ROC
analysis, with an AUC of 0.588 (P<0.001; Fig. 1C). The median value of LMR was 3.62.
The optimal cut-point was 3.70, according to the ROC analysis, with
an AUC of 0.618 (P<0.001; Fig.
1D).
Based on these cut-off point values, patients were
divided into two groups for each measured variable: Fibrinogen [low
(≤3.77 g/l, n=246) and high (>3.77 g/l, n=210)], NLR [low
(≤2.28, n=242) and high (>2.28, n=214)], PLR [low (≤106.24,
n=145) and high (>106.24, n=311)], and LMR [low (≤3.7, n=240)
and high (>3.7, n=216)].
Furthermore, the reference value for D-dimer was
≤500 ng/ml. Among the enrolled patients, 325 (71.3%) demonstrated
low plasma D-dimer levels (D-dimer ≤500 ng/ml) and 131 (28.7%)
demonstrated high plasma D-dimer levels (D-dimer >500 ng/ml).
Patients were therefore categorized into two groups according to
plasma D-dimer levels: Low (D-dimer ≤500 ng/ml) and high (D-dimer
>500 ng/ml).
Association between preoperative
fibrinogen or D-dimer levels and clinicopathological variables
The associations between preoperative plasma
fibrinogen or D-dimer levels and the clinicopathological variables
of patients with NSCLC are presented in Table I. These results revealed that high
preoperative plasma fibrinogen levels were significantly associated
with sex (P<0.001), age (P=0.018), smoking history (P<0.001),
lesion type (P=0.001), T stage (P<0.001), pathological stage
(P=0.002), NLR (P<0.001), PLR (P<0.001) and LMR (P<0.001).
However, no statistically significant associations were identified
between preoperative plasma fibrinogen level and tumour location or
lymph node metastasis (P>0.05).
 | Table I.The association of preoperative plasma
fibrinogen and D-dimer levels with clinicopathological variables in
patients with NSCLC. |
Table I.
The association of preoperative plasma
fibrinogen and D-dimer levels with clinicopathological variables in
patients with NSCLC.
|
|
| Fibrinogen |
|
| D-dimer |
|
|
|---|
|
|
|
|
|
|
|
|
|
|---|
| Clinicopathological
variable | n | Low (%) | High (%) | χ2 | P-value | Low (%) | High (%) | χ2 | P-value |
|---|
| Sex |
|
|
| 21.273 | <0.001 |
|
| 0.355 | 0.551 |
|
Male | 318 | 149 (46.9) | 169 (53.1) |
|
| 224 (70.4) | 94 (29.6) |
|
|
|
Female | 138 | 97 (70.3) | 41 (29.7) |
|
| 101 (73.2) | 37 (26.8) |
|
|
| Age (years) |
|
|
| 5.552 | 0.018 |
|
| 4.468 | 0.035 |
|
<61 | 227 | 135 (59.5) | 92 (40.5) |
|
| 172 (75.8) | 55 (24.2) |
|
|
|
≥61 | 229 | 111 (48.5) | 118 (51.5) |
|
| 153 (66.8) | 76 (33.2) |
|
|
| Smoking
history |
|
|
| 23.999 | <0.001 |
|
| 0.552 | 0.457 |
|
None | 151 | 106 (70.2) | 45 (29.8) |
|
| 111 (73.5) | 40 (26.5) |
|
|
|
Yes | 305 | 140 (45.9) | 165 (54.1) |
|
| 214 (70.2) | 91 (29.8) |
|
|
| Tumor location |
|
|
| 0.241 | 0.624 |
|
| 0.355 | 0.551 |
|
Left | 192 | 101 (52.6) | 91 (47.4) |
|
| 134 (69.8) | 58 (30.2) |
|
|
|
Right | 264 | 145 (54.9) | 119 (45.1) |
|
| 191 (72.3) | 73 (27.7) |
|
|
| Lesion type |
|
|
| 10.666 | 0.001 |
|
| 2.816 | 0.093 |
|
Peripheral | 315 | 186 (59.0) | 129 (41.0) |
|
| 232 (73.7) | 83 (26.3) |
|
|
|
Central | 141 | 60 (42.6) | 81 (57.4) |
|
| 93 (66.0) | 48 (34.0) |
|
|
| T stage |
|
|
| 41.301 | <0.001 |
|
| 8.992 | 0.011 |
| T1 | 150 | 111 (74.0) | 39 (26.0) |
|
| 115 (76.7) | 35 (23.3) |
|
|
| T2 | 258 | 121 (46.9) | 137 (53.1) |
|
| 184 (71.3) | 74 (28.7) |
|
|
|
T3-4 | 48 | 14 (29.2) | 34 (70.8) |
|
| 26 (54.2) | 22 (45.8) |
|
|
| Lymph node
metastasis |
|
|
| 0.120 | 0.729 |
|
| 2.507 | 0.113 |
| No | 232 | 127 (54.7) | 105 (45.3) |
|
| 173 (74.6) | 59 (25.4) |
|
|
|
Yes | 224 | 119 (53.1) | 105 (46.9) |
|
| 152 (67.9) | 72 (32.1) |
|
|
| Pathological
stage |
|
|
| 12.467 | 0.002 |
|
| 13.297 | 0.001 |
| I | 170 | 109 (64.1) | 61 (35.9) |
|
| 138 (81.2) | 32 (18.8) |
|
|
| II | 101 | 44 (43.6) | 57 (56.4) |
|
| 64 (63.4) | 37 (36.6) |
|
|
|
IIIA | 185 | 93 (50.3) | 92 (49.7) |
|
| 123 (66.5) | 62 (33.5) |
|
|
| NLR |
|
|
| 49.700 | <0.001 |
|
| 7.863 | 0.005 |
|
Low | 242 | 168 (69.4) | 74 (30.6) |
|
| 186 (76.9) | 56 (23.1) |
|
|
|
High | 214 | 78 (36.4) | 136 (63.6) |
|
| 139 (65.0) | 75 (35.0) |
|
|
| PLR |
|
|
| 19.301 | <0.001 |
|
| 2.895 | 0.089 |
|
Low | 145 | 100 (69.0) | 45 (31.0) |
|
| 111 (76.6) | 34 (23.4) |
|
|
|
High | 311 | 146 (46.9) | 165 (53.1) |
|
| 214 (68.8) | 97 (31.2) |
|
|
| LMR |
|
|
| 30.757 | <0.001 |
|
| 0.706 | 0.401 |
|
Low | 240 | 100 (41.7) | 140 (58.3) |
|
| 167 (69.6) | 73 (30.4) |
|
|
|
High | 216 | 146 (67.6) | 70 (32.4) |
|
| 158 (73.1) | 58 (26.9) |
|
|
There were also significant associations between
D-dimer level and age (P=0.035), T stage (P=0.011), pathological
stage (P=0.001) and NLR (P=0.005). However, no significant
associations were identified between D-dimer level and sex, smoking
history, tumour location, lesion type, lymph node metastasis, PLR
or LMR (all P>0.05; Table I).
Prognostic significance of
preoperative coagulation and inflammatory indicators
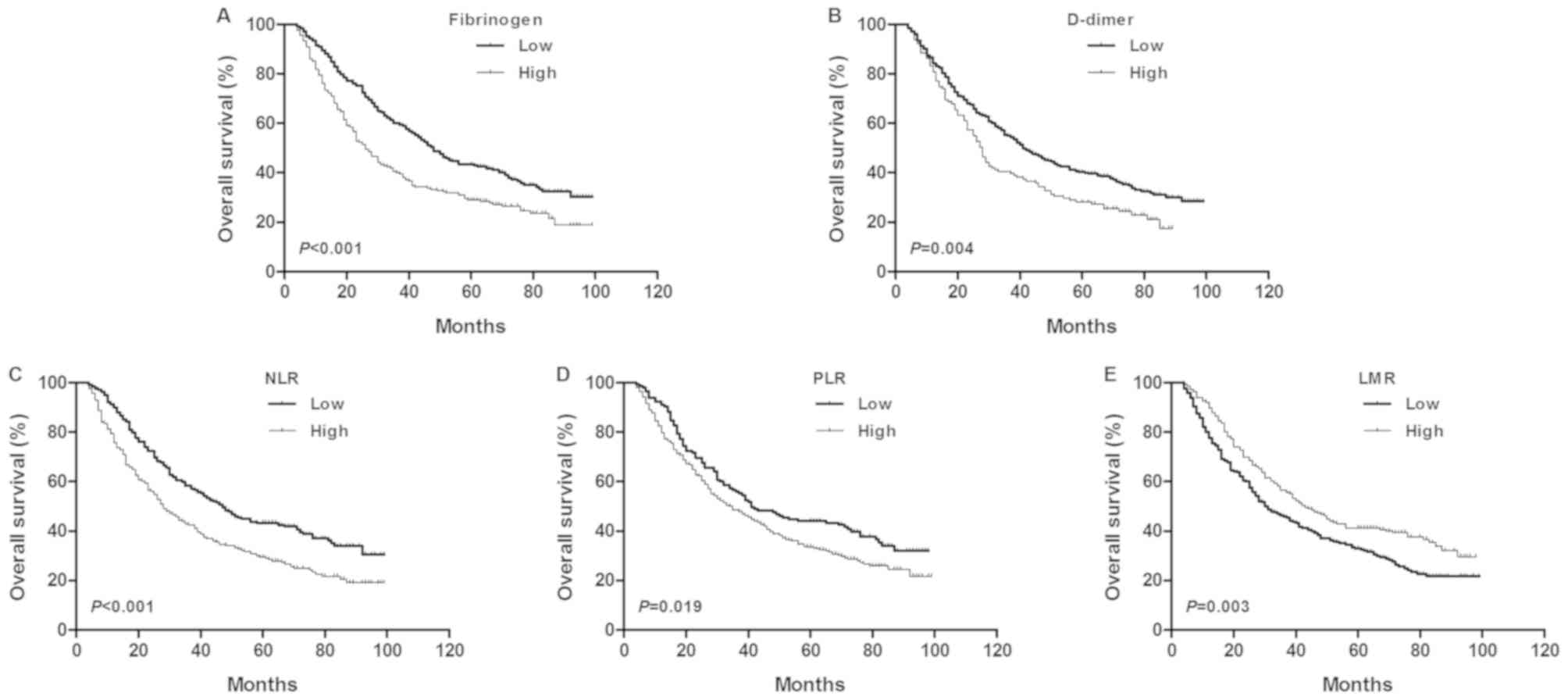
Kaplan-Meier analyses and log-rank tests were
performed to determine the prognostic value of coagulation factors
and inflammatory indicators in predicting patient 5-year OS rates.
The data demonstrated that the 5-year OS rate and median OS time of
the fibrinogen-low group were significantly higher than those of
the fibrinogen-high group [43.5 vs. 29.0% (48.0 vs. 26.0 months),
P<0.001; Fig. 2A]. The 5-year OS
rate and median OS time of the D-dimer-low group was significantly
higher than those of the D-dimer-high group [40.3 vs. 28.2% (41.0
vs. 28.0 months), P=0.004; Fig. 2B].
The 5-year OS rate and median OS time of the NLR-low group were
significantly higher than those of the NLR-high group [43.4 vs.
29.4% (47.0 vs 28.0 months), P<0.001; Fig. 2C]. The 5-year OS rate and median OS
time of the PLR-low group were significantly higher than those of
the PLR-high group [44.1 vs. 33.4% (41.0 vs. 35.0 months), P=0.019;
Fig. 2D]. In addition, the 5-year OS
probability and median OS time of the LMR-high group were also
significantly higher than those of the LMR-low group [41.2 vs.
32.9% (43.0 vs. 30.0 months), P=0.003; Fig. 2E].
Univariate and multivariate survival
analyses of independent prognostic variables in patients with
NSCLC
To further identify predictors of postoperative OS,
clinicopathological variables, including coagulation and
inflammatory indicators, were evaluated using univariate and
multivariate analyses. Univariate analyses for OS with a log-rank
test demonstrated that smoking history (P=0.023), lesion type
(P=0.030), resection type (P=0.018), T stage (P=0.025), lymph node
metastasis (P<0.001), plasma fibrinogen (P<0.001), D-dimer
(P=0.004), NLR (P<0.001), PLR (P=0.019) and LMR (P=0.003) were
significantly associated with patient prognosis (Table II).
 | Table II.Univariate survival analysis of
prognostic factors by the Kaplan-Meier method in patients with
NSCLC. |
Table II.
Univariate survival analysis of
prognostic factors by the Kaplan-Meier method in patients with
NSCLC.
| Clinicopathological
variable | n | 5-year OS rate,
% | MST | χ2
value | P-value |
|---|
| Sex |
|
|
| 0.782 | 0.377 |
|
Male | 318 | 36.5 | 36.0 |
|
|
|
Female | 138 | 37.7 | 39.0 |
|
|
| Age, years |
|
|
| 1.404 | 0.236 |
|
<61 | 227 | 37.4 | 40.0 |
|
|
|
≥61 | 229 | 36.2 | 33.0 |
|
|
| Smoking
history |
|
|
| 5.155 | 0.023 |
|
None | 151 | 43.0 | 44.0 |
|
|
|
Yes | 305 | 33.8 | 33.0 |
|
|
| Histological
type |
|
|
| 0.528 | 0.768 |
|
Squamous | 238 | 35.7 | 35.0 |
|
|
|
Adenocarcinoma | 157 | 37.6 | 39.0 |
|
|
|
Others | 61 | 39.3 | 32.0 |
|
|
| Tumor location |
|
|
| 1.418 | 0.234 |
|
Left | 192 | 34.4 | 34.0 |
|
|
|
Right | 264 | 38.6 | 39.0 |
|
|
| Lesion type |
|
|
| 4.735 | 0.030 |
|
Peripheral | 315 | 39.7 | 41.0 |
|
|
|
Central | 141 | 30.5 | 32.0 |
|
|
| Resection type |
|
|
| 5.592 | 0.018 |
|
Lobectomy | 387 | 38.8 | 39.0 |
|
|
|
Pneumonectomy | 69 | 26.1 | 30.0 |
|
|
| T stage |
|
|
| 7.374 | 0.025 |
| T1 | 150 | 39.3 | 41.0 |
|
|
| T2 | 258 | 38.5 | 38.0 |
|
|
|
T3-4 | 48 | 20.8 | 25.0 |
|
|
| Lymph node
metastasis |
|
|
| 46.357 | <0.001 |
| No | 232 | 50.0 | 58.0 |
|
|
|
Yes | 224 | 23.2 | 27.0 |
|
|
| Fibrinogen
level |
|
|
| 15.413 | <0.001 |
|
Low | 246 | 43.5 | 48.0 |
|
|
|
High | 210 | 29.0 | 26.0 |
|
|
| D-dimer |
|
|
| 8.072 | 0.004 |
|
Low | 325 | 40.3 | 41.0 |
|
|
|
High | 131 | 28.2 | 28.0 |
|
|
| NLR |
|
|
| 15.979 | <0.001 |
|
Low | 242 | 43.4 | 47.0 |
|
|
|
High | 214 | 29.4 | 28.0 |
|
|
| PLR |
|
|
| 5.503 | 0.019 |
|
Low | 145 | 44.1 | 41.0 |
|
|
|
High | 311 | 33.4 | 35.0 |
|
|
| LMR |
|
|
| 8.967 | 0.003 |
|
Low | 240 | 32.9 | 30.0 |
|
|
|
High | 216 | 41.2 | 43.0 |
|
|
All 10 factors indicated as significant by
univariate analyses were further subjected to multivariate analyses
with a Cox proportional hazards model to determine the independent
prognostic factors associated with OS. The results indicated that
lymph node metastasis (P<0.001), plasma fibrinogen level
(P=0.024) and NLR (P=0.028) were significant independent prognostic
variables associated for a poor OS rate (Table III).
 | Table III.Multivariate survival analysis of
independent prognostic factors by the Cox proportional hazard model
in patients with NSCLC. |
Table III.
Multivariate survival analysis of
independent prognostic factors by the Cox proportional hazard model
in patients with NSCLC.
| Clinicopathological
variable | B | SE | Wald | P-value | HR | 95% CI |
|---|
| Smoking
history | −0.066 | 0.132 | 0.249 | 0.618 | 0.936 | 0.722~1.214 |
| Lesion type | −0.087 | 0.135 | 0.412 | 0.521 | 0.917 | 0.703~1.195 |
| Resection type | 0.138 | 0.163 | 0.717 | 0.397 | 1.148 | 0.834~1.579 |
| T stage | 0.033 | 0.095 | 0.119 | 0.730 | 1.033 | 0.858~1.244 |
| Lymph node
metastasis | 0.754 | 0.118 | 41.020 | <0.001 | 2.125 | 1.687~2.676 |
| Fibrinogen
level | 0.299 | 0.132 | 5.119 | 0.024 | 1.348 | 1.041~1.746 |
| D-dimer | 0.238 | 0.123 | 3.775 | 0.058 | 1.269 | 0.998~1.614 |
| NLR | 0.295 | 0.134 | 4.858 | 0.028 | 1.344 | 1.033~1.747 |
| PLR | 0.044 | 0.132 | 0.112 | 0.738 | 1.045 | 0.806~1.355 |
| LMR | −0.085 | 0.128 | 0.437 | 0.509 | 0.919 | 0.715~1.181 |
Prognostic analysis based on COF-NLR
score for NSCLC patients
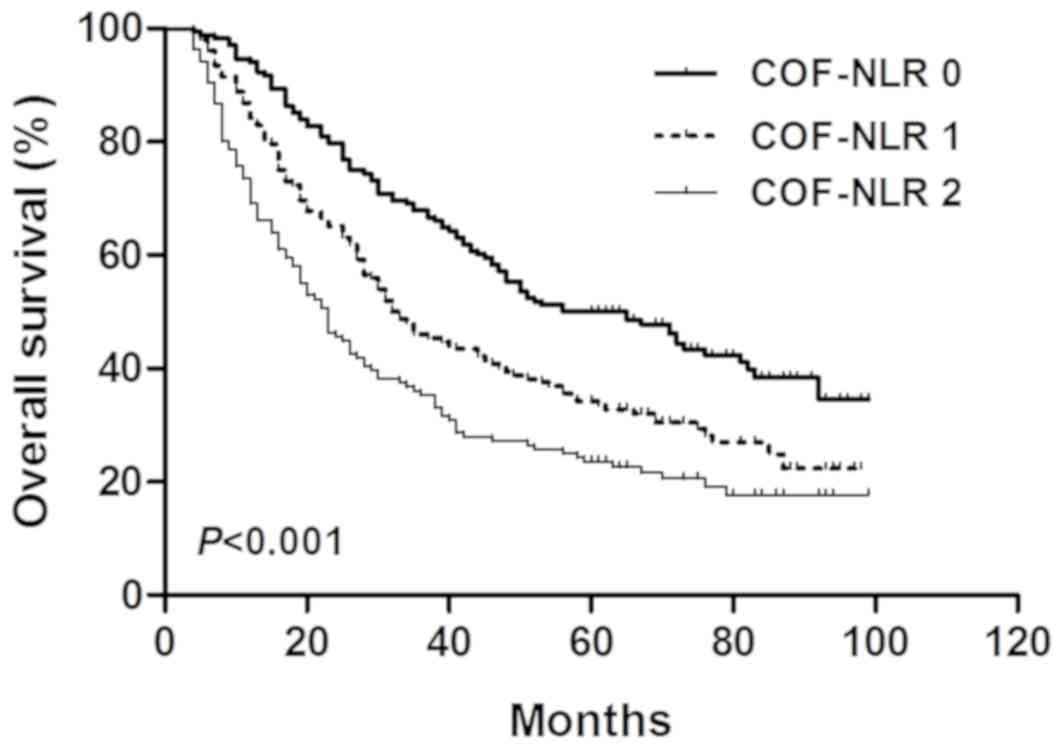
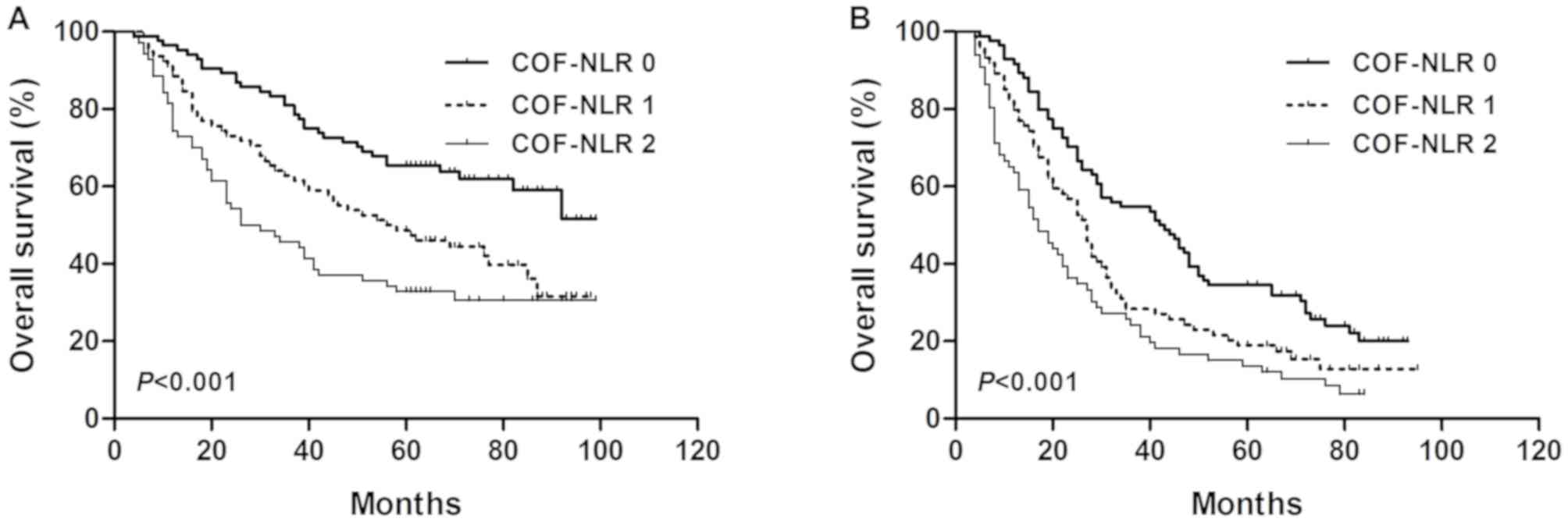
According to the grading system of the COF-NLR
score, 168 (36.8%) patients had a COF-NLR score of 0, 152 (33.3%)
patients had a COF-NLR score of 1 and 136 (29.8%) patients had a
COF-NLR score of 2. The 5-year OS rates for patients with COF-NLR
scores of 0, 1 and 2 were 50.0, 34.2 and 23.5%, respectively
(P<0.001; Fig. 3). Therefore, it
was possible to classify the patients into three distinct
prognostic groups using the preoperative COF-NLR score.
Prognostic significance of
preoperative COF-NLR in subgroups of patients
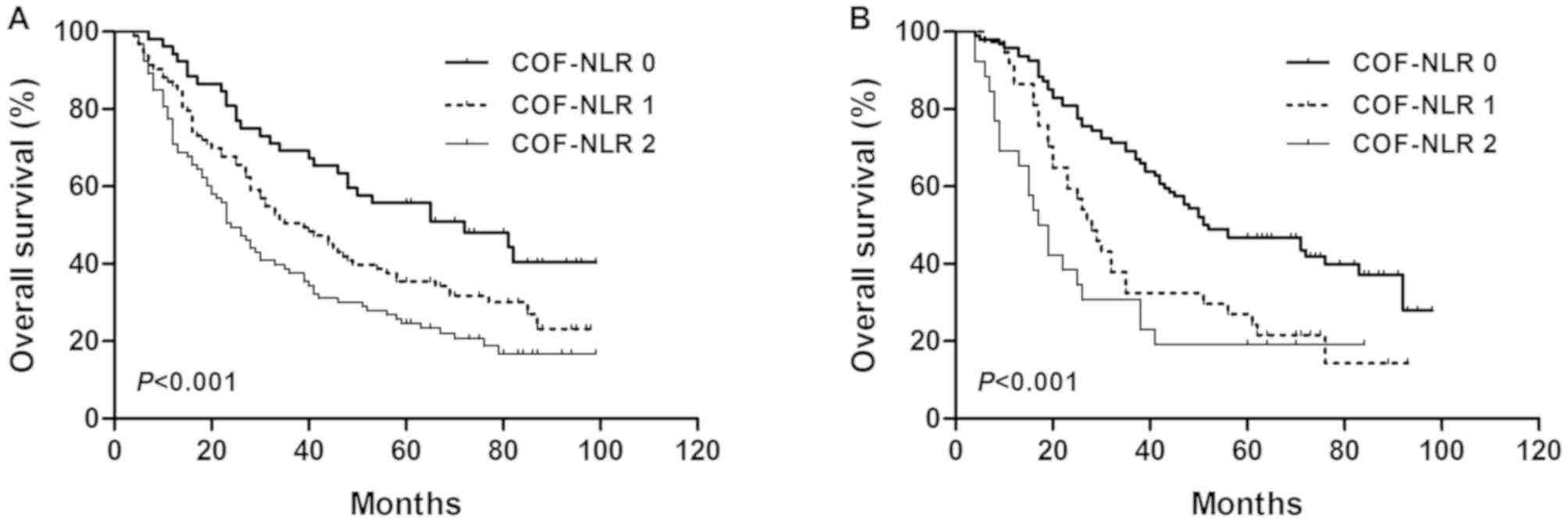
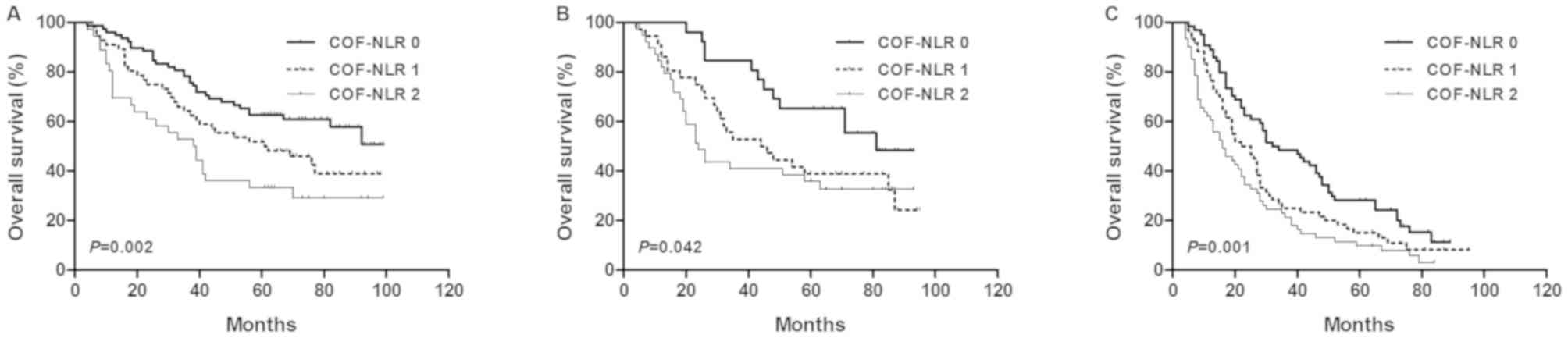
The results of the present study demonstrated that
preoperative COF-NLR was significantly associated with OS. To
further evaluate the prognostic value of COF-NLR in subgroups of
patients with NSCLC, the patients were further classified according
to histopathological subtype, lymph node status and pathological
stage. The results revealed that, in the squamous cell cancer
subgroup, COF-NLR exhibited notable prognostic value in predicting
poorer OS rates (Fig. 4A) and was
also effective in patients with adenocarcinoma (Fig. 4B). In addition, COF-NLR was a
prognostic indicator for OS in patients with or without lymph node
metastasis (Fig. 5). Furthermore,
when stratifying the patients based on clinical stage, COF-NLR also
retained its predictive value for patients with pathological stage
I, II or IIIA tumours (Fig. 6).
Therefore, it appears that COF-NLR may serve as a powerful
prognostic factor for categorising patients with NSCLC into
different risk subgroups.
Discussion
Establishing one optimal preoperative prognostic
factor for facilitating individual risk stratification and
management is critical for improving outcomes for patients with
NSCLC. Although numerous studies have been conducted to search for
predictors, there is a continuing debate regarding the optimal
preoperative prognostic factor for NSCLC (16–18). The
activated coagulation system and systematic inflammatory response
serve important functions in tumour invasion, angiogenesis
promotion, metastasis and poor prognosis in several types of
malignant disease (3,19,20).
Therefore, the present study evaluated the clinical and prognostic
value of preoperative coagulation factor levels (fibrinogen and
D-dimer) and inflammatory variables (NLR, PLR and LMR), and
assessed the prognostic value of combining fibrinogen with NLR in
NSCLC as a novel, single prognostic model.
Tumour-mediated activation of the coagulation
pathway is associated with tumour growth, angiogenesis promotion
and metastasis (21). Fibrinogen and
D-dimer are key components of the coagulation system. Fibrinogen,
an acute-phase reactant glycoprotein, is involved in the thrombin
transformation of the coagulation cascade and clot formation
(22). D-dimer, a stable end product
of fibrin degradation, is associated with the presence of venous
thromboembolism in cancer patients (23). The present study analysed the
association between preoperative fibrinogen, D-dimer and
clinicopathological variables. It identified that elevated
fibrinogen was associated with the tumour size (T) and TNM stages,
which is consistent with the findings of Zeng et al
(3). Furthermore, the association
between preoperative elevated D-dimer levels and
clinicopathological variables in NSCLC was reported for the first
time, and the results demonstrated that elevated D-dimer levels
were also associated with the T and TNM stages. In addition, the
results of multivariate prognostic analyses revealed that
preoperative elevated fibrinogen levels, not D-dimer levels, was an
independent prognostic factor for patients with NSCLC. However, the
mechanism for this effect remains to be elucidated. A previous
study demonstrated that interleukin-6 produced by cancer cells
could stimulate the secretion of fibrinogen in lung cancer
(24). Furthermore, elevated
fibrinogen can promote angiogenesis and facilitate tumour cell
metastasis by serving as an extracellular matrix for migration
(25,26).
Imbalance in the host systematic inflammatory system
serves an important role in tumour progression, proliferation and
metastasis (27). A systematic
inflammatory response causes variations in the number of
circulating white blood cells, including neutrophils, lymphocytes
and monocytes, during cancer progression (11). Previous studies have reported that
three haematological indices, as the ratio of absolute counts of
these three white cell constituents (NLR, PLR and LMR) were
independent prognostic factors in NSCLC (28), gastric cancer (29) and oesophageal cancer (30). The present study examined the
prognostic value of preoperative NLR, PLR and LMR in patients with
NSCLC. The results demonstrated that a decreased 5-year OS rate in
patients with NSCLC was associated with a higher NLR and PLR, and a
lower LMR. In multivariate survival analysis, a higher preoperative
NLR was demonstrated to be an independent prognostic factor for
patients with NSCLC. Neutrophils promote tumour angiogenesis by
releasing angiogenic factors, including vascular endothelial growth
factor, angiopoietin-1 and fibroblast growth factor-2 (31). Lymphocytes can induce the suppression
of antitumor immunity by releasing inhibitory immunological
mediators, including interleukin-10 and transforming growth
factor-β (32). This may explain why
an elevated NLR was associated with poorer survival rates in
patients with NSCLC.
The present study also investigated the association
between the three inflammatory indictors and coagulation factors,
and demonstrated that higher fibrinogen levels were associated with
NLR, PLR and LMR, whereas elevated D-dimer levels were only
associated with higher NLR. Host inflammatory (monocyte/macrophage)
cell-mediated triggering of clotting activation may be one possible
mechanism in NSCLC (33). However,
the mechanism behind activation of coagulation due to an increase
in host inflammatory response requires further study.
As fibrinogen and NLR were demonstrated to be
independent prognostic factors for patients with NSCLC in the
present study, COF-NLR may aid the identification of patients with
a poor prognosis following surgery and the provision of
individualised treatment. In previous studies, the combined
prognostic value of fibrinogen with inflammatory indicators has
been discussed for gastric (11),
bladder (34), hepatocellular
(13) and oesophageal squamous cell
carcinoma (35). However, the
prognostic significance of COF-NLR has not been reported in NSCLC
and this was investigated in the present study. Based on the
preoperative COF-NLR score proposed in the current study, patients
with NSCLC were divided into three distinct risk groups. The
prognostic value of COF-NLR for histological subtype, lymph node
metastasis and pathological stage subgroups was also investigated.
The COF-NLR maintained its prognostic value in OS prediction for
all subgroups of patients with NSCLC, indicating the reliable
prognostic value of COF-NLR. To the best of our knowledge, the
present study was the first to investigate the prognostic value of
COF-NLR in patients with NSCLC. Considering that fibrinogen and NLR
are markers that can be readily evaluated in conventional blood
analyses (11), the preoperative
assessment of COF-NLR may be suitable as a reliable prognostic tool
for patients with NSCLC; the lower-scoring COF-NLR groups are
associated with an improved prognosis compared with the
higher-scoring COF-NLR groups.
However, there are certain limitations to the
present study. To begin with, this retrospective study was
conducted by a single institution. Secondly, all data were selected
from one relatively small sample of patients, and a control arm was
not set for validation. Therefore, the preoperative prognostic
significance of COF-NLR in patients with NSCLC should be further
strengthened in a larger, multicentre prospective study.
In conclusion, in the present study it was
identified that, of the coagulation and inflammatory indicators,
preoperative fibrinogen and NLR were independent prognostic
predictors for NSCLC. A novel prognostic factor was further
proposed, based on the combination of fibrinogen with the NLR from
blood specimen analysis (COF-NLR), and was demonstrated to have
prognostic predictive potential for patients with NSCLC. In the
future, by adding this prognostic factor to clinical work, it may
be possible to make insightful preoperative prognostic predictions
and customise individual treatment plans for patients with
NSCLC.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Science
Foundation of Qinhuangdao (grant no. 201502A093).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
HL and KG performed the experiment and wrote the
manuscript. HL was responsible for the design of the experiment. RJ
and JL analyzed the experiment data. CW helped with the statitical
analysis. JL and CW helped to revise the manuscript. All authors
read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of the First Hospital of Qinhuangdao and written informed
consent was obtained from each patient prior to enrolment.
Patient consent for publication
Each patient provided written informed consent for
the publication of this study.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
OS
|
overall survival
|
|
NSCLC
|
non-small cell lung cancer
|
|
NLR
|
neutrophil-lymphocyte ratio
|
|
PLR
|
platelet-lymphocyte ratio
|
|
LMR
|
lymphocyte-monocyte ratio
|
|
TNM
|
Tumour-Node-Metastasis
|
|
COF-NLR
|
combination of fibrinogen and NLR
|
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2015. CA Cancer J Clin. 65:5–29. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kamangar F, Dores GM and Anderson WF:
Patterns of cancer incidence, mortality, and prevalence across five
continents: Defining priorities to reduce cancer disparities in
different geographic regions of the world. J Clin Oncol.
24:2137–2150. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zeng Q, Xue N, Dai D, Xing S, He X, Li S,
Du Y, Huang C, Li L and Liu W: A nomogram based on inflammatory
factors C-reactive protein and fibrinogen to predict the prognostic
value in patients with resected non-small cell lung cancer. J
Cancer. 8:744–753. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Murray JC: Coagulation and cancer. Br J
Cancer. 64:422–424. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Son HJ, Park JW, Chang HJ, Kim DY, Kim BC,
Kim SY, Park SC, Choi HS and Oh JH: Preoperative plasma
hyperfibrinogenemia is predictive of poor prognosis in patients
with nonmetastatic colon cancer. Ann Surg Oncol. 20:2908–2913.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vahid DM, Ahmari S, Alipour S and
Tehranian A: The comparison of plasma D-dimer levels in benign and
malignant tumors of cervix, ovary and uterus. Int J Hematol Oncol
Stem Cell Res. 9:107–111. 2015.PubMed/NCBI
|
|
7
|
Nakamura K, Nakayama K, Ishikawa M,
Katagiri H, Minamoto T, Ishibashi T, Ishikawa N, Sato E, Sanuki K,
Yamashita H, et al: High pre-treatment plasma D-Dimer level as a
potential prognostic biomarker for cervical carcinoma. Anticancer
Res. 36:2933–2938. 2016.PubMed/NCBI
|
|
8
|
Dirix LY, Salgado R, Weytjens R, Colpaert
C, Benoy I, Huget P, van Dam P, Prové A, Lemmens J and Vermeulen P:
Plasma fibrin D-dimer levels correlate with tumour volume,
progression rate and survival in patients with metastatic breast
cancer. Br J Cancer. 86:389–395. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dunn GP, Old LJ and Schreiber RD: The
immunobiology of cancer immunosurveillance and immunoediting.
Immunity. 21:137–148. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
McMillan DC: Systemic inflammation,
nutritional status and survival in patients with cancer. Curr Opin
Clin Nutr Metab Care. 12:223–226. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Arigami T, Uenosono Y, Matsushita D,
Yanagita S, Uchikado Y, Kita Y, Mori S, Kijima Y, Okumura H,
Maemura K, et al: Combined fibrinogen concentration and
neutrophil-lymphocyte ratio as a prognostic marker of gastric
cancer. Oncol Lett. 11:1537–1544. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Arigami T, Okumura H, Matsumoto M,
Uchikado Y, Uenosono Y, Kita Y, Owaki T, Mori S, Kurahara H, Kijima
Y, et al: Analysis of the fibrinogen and neutrophil-lymphocyte
ratio in esophageal squamous cell carcinoma: A promising blood
marker of tumor progression and prognosis. Medicine (Baltimore).
94:e17022015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fu SJ, Ji F, Han M, Chen MG, Wang XP, Ju
WQ, Zhao Q, Wu LW, Ren QQ, Guo ZY, et al: Prognostic value of
combined preoperative fibrinogen and neutrophil-lymphocyte ratio in
patients with hepatocellular carcinoma after liver transplantation.
Oncotarget. 8:4301–4312. 2017.PubMed/NCBI
|
|
14
|
Xia H, Sun Z, Deng L, Zhu D and Wang D:
Prognostic significance of the preoperative lymphocyte to monocyte
ratio in patients with stage I non-small cell lung cancer
undergoing complete resection. Cancer Invest. 34:378–384. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Dorn-Beineke A, Dempfle CE, Bertsch T and
Wisser H: Evaluation of the automated coagulation analyzer Sysmex
CA-7000. Thromb Res. 116:171–179. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tian S: Classification and survival
prediction for early-stage lung adenocarcinoma and squamous cell
carcinoma patients. Oncol Lett. 14:5464–5470. 2017.PubMed/NCBI
|
|
17
|
Fang L, Sheng H, Wan D, Zhu C, Jiang R,
Sun X and Feng J: Prognostic role of multidrug
resistance-associated protein 1 expression and platelet count in
operable non-small cell lung cancer. Oncol Lett. 16:1123–1132.
2018.PubMed/NCBI
|
|
18
|
Zou Q, Wang T, Li B, Li G, Zhang L, Wang B
and Sun S: Overexpression of circ-0067934 is associated with
increased cellular proliferation and the prognosis of non-small
cell lung cancer. Oncol Lett. 16:5551–5556. 2018.PubMed/NCBI
|
|
19
|
Yamashita H, Kitayama J, Kanno N, Yatomi Y
and Nagawa H: Hyperfibrinogenemia is associated with lymphatic as
well as hematogenous metastasis and worse clinical outcome in T2
gastric cancer. BMC Cancer. 6:1472006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Palumbo JS: Mechanisms linking tumor
cell-associated procoagulant function to tumor dissemination. Semin
Thromb Hemost. 34:154–160. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Lal I, Dittus K and Holmes CE: Platelets,
coagulation and fibrinolysis in breast cancer progression. Breast
Cancer Res. 15:2072013. View
Article : Google Scholar : PubMed/NCBI
|
|
22
|
Weisel JW: Fibrinogen and fibrin. Adv
Protein Chem. 70:247–299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Arpaia G, Carpenedo M, Verga M,
Mastrogiacomo O, Fagnani D, Lanfredini M, Milani M and Cimminiello
C: D-dimer before chemotherapy might predict venous
thromboembolism. Blood Coagul Fibrinolysis. 20:170–175. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yamaguchi T, Yamamoto Y, Yokota S,
Nakagawa M, Ito M and Ogura T: Involvement of interleukin-6 in the
elevation of plasma fibrinogen levels in lung cancer patients. Jpn
J Clin Oncol. 28:740–744. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Garcia MG, Bayo J, Bolontrade MF, Sganga
L, Malvicini M, Alaniz L, Aquino JB, Fiore E, Rizzo MM, Rodriguez
A, et al: Hepatocellular carcinoma cells and their fibrotic
microenvironment modulate bone marrow-derived mesenchymal stromal
cell migration in vitro and in vivo. Mol Pharm. 8:1538–1548. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zheng S, Shen J, Jiao Y, Liu Y, Zhang C,
Wei M, Hao S and Zeng X: Platelets and fibrinogen facilitate each
other in protecting tumor cells from natural killer cytotoxicity.
Cancer Sci. 100:859–865. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Vesely MD and Schreiber RD: Cancer
immunoediting: Antigens, mechanisms, and implications to cancer
immunotherapy. Ann N Y Acad Sci. 1284:1–5. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu G, Yao Y, Bai C, Zeng J, Shi D, Gu X,
Shi X and Song Y: Combination of platelet to lymphocyte ratio and
neutrophil to lymphocyte ratio is a useful prognostic factor in
advanced non-small cell lung cancer patients. Thorac Cancer.
6:275–287. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Lee S, Oh SY, Kim SH, Lee JH, Kim MC, Kim
KH and Kim HJ: Prognostic significance of neutrophil lymphocyte
ratio and platelet lymphocyte ratio in advanced gastric cancer
patients treated with FOLFOX chemotherapy. BMC Cancer. 13:3502013.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hirahara N, Matsubara T, Mizota Y,
Ishibashi S and Tajima Y: Prognostic value of preoperative
inflammatory response biomarkers in patients with esophageal cancer
who undergo a curative thoracoscopic esophagectomy. BMC Surg.
16:662016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Neagoe PE, Brkovic A, Hajjar F and Sirois
MG: Expression and release of angiopoietin-1 from human
neutrophils: Intracellular mechanisms. Growth Factors. 27:335–344.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hoffmann TK, Dworacki G, Tsukihiro T,
Meidenbauer N, Gooding W, Johnson JT and Whiteside TL: Spontaneous
apoptosis of circulating T lymphocytes in patients with head and
neck cancer and its clinical importance. Clin Cancer Res.
8:2553–2562. 2002.PubMed/NCBI
|
|
33
|
Gabazza E, Taguchi O, Yamakami T, Machishi
M, Ibata H and Suzuki S: Correlation between increased granulocyte
elastase release and activation of blood coagulation in patients
with lung cancer. Cancer. 72:2134–2140. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ma C, Lu B, Diao C, Zhao K, Wang X, Ma B,
Lu B and Sun E: Preoperative neutrophil-lymphocyte ratio and
fibrinogen level in patients distinguish between muscle-invasive
bladder cancer and non-muscle-invasive bladder cancer. Onco Targets
Ther. 9:4917–4922. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Kijima T, Arigami T, Uchikado Y, Uenosono
Y, Kita Y, Owaki T, Mori S, Kurahara H, Kijima Y, Okumura H, et al:
Combined fibrinogen and neutrophil-lymphocyte ratio as a prognostic
marker of advanced esophageal squamous cell carcinoma. Cancer Sci.
108:193–199. 2017. View Article : Google Scholar : PubMed/NCBI
|