Introduction
Biliary tract cancers (BTC) are rare malignancies,
representing <1% of all human cancers (1). Incidence is low in Western countries
with ~0.3–3.5/100.000 cases/year, while in Asia and particularly in
China, Thailand, and both North and South Korea, it is higher due
to an increased frequency of liver flukes (2,3). BTC arise
from biliary epithelium and almost 90% of cases are
adenocarcinomas. BTC are classified as: Intrahepatic
cholangiocarcinomas (CCs), extrahepatic CC, and gallbladder
carcinoma (GC).
Complete resection (R0) is the only potentially
curative treatment option. However, due to the advanced disease at
diagnosis, more than half of the patients are not surgical
candidates (4).
Radiotherapy (RT) generally combined with concurrent
and/or sequential chemotherapy is considered as a treatment option
for locally advanced BTC by international guidelines (4,5). In fact,
several studies on these tumors demonstrated the efficacy of
chemoradiation, sometimes followed by a brachytherapy (BT) boost
for symptoms palliation, local control (LC) and overall survival
(OS) improvement (6–9).
However, although RT is considered a treatment
option for locally advanced BTC, there is no consensus on clinical
target volume (CTV) definition. Recently, Marinelli et al
(10) published a review on the
incidence of metastases in the different regional nodal stations of
patients with BTC. Based on that analysis, we proposed guidelines
for the definition of the nodal CTV (CTV-N) in intrahepatic CC,
extrahepatic CC, and GC (10).
The aim of the presest study was to provide
supplementary literature data concerning the microscopic spread of
the primary lesion and to suggest a proper CTV definition of the
primary tumor (CTV-T). Furthermore, our objective was to define a
general CTV by merging these evidence-based CTV-T and CTV-N.
Finally, we aimed to present an atlas for locally advanced BTC
delineation.
Materials and methods
Nodal clinical target volume
(CTV-N)
The definition of the CTV-N was described in our
previous analysis (10) and is only
briefly summarized in the present study in Tables I–III.
 | Table I.CTV for intrahepatic
cholangiocarcinoma. |
Table I.
CTV for intrahepatic
cholangiocarcinoma.
| Delineation type | JSHBPS
classification | Recommended
margins |
|---|
| Tumor
delineation |
|
Intrahepatic
cholangiocarcinoma | – | GTV + 10 mm
radially |
| Lymph node group,
nodes delineation |
|
Hepatoduodenal ligament lymph
nodes | 12 | 10 mm margin around
the segment of portal vein from the confluence between the right
and left hepatic ducts and the upper border of the pancreas |
| Common
hepatic artery lymph nodes | 8 | 10 mm margin around
the common hepatic artery |
|
Para-aortic lymph nodes | 16 | 10 mm margin around
the abdominal aorta, from the diaphragmatic aortic hiatus to the
upper border of the origin of the inferior mesenteric artery |
| Posterior
pancreaticoduodenal lymph nodes | 13 | 10 mm around the
posterior pancreaticoduodenal artery |
| Left
gastric artery lymph nodes | 7 | 10 mm around the
trunk of the left gastric artery |
| Lesser
gastric curvature lymph nodes | 3 | The area around the
lesser curvature of the stomach |
| Right
paracardial lymph nodes | 1 | The narrowed
anatomic space identified between gastric cardia and the liver,
extending posteriorly to the aorta and inferiorly to the lesser
curvature LNs |
| Left
paracardial lymph nodes | 2 | The anatomic space
defined medially by the gastric fundus, anteromedially by the
visceral peritoneum, posteriorly by the spleen, superiorly by the
hemi diaphragm, and inferiorly by the great curvature LNs |
 | Table III.CTV for gallbladder carcinoma. |
Table III.
CTV for gallbladder carcinoma.
| Delineation
type | JSHBPS
classification | Recommended
margins |
|---|
| Tumor
delineation |
|
Gallbladder carcinoma | – | GTV + 25 mm
radially in hepatic direction + gallbladder residual volume |
| Lymph node group,
nodes delineation |
|
Hepatoduodenal ligament lymph
nodes | 12 | 10 mm margin around
the segment of portal vein from the confluence between the right
and left hepatic ducts and the upper border of the pancreas |
| Common
hepatic artery lymph nodes | 8 | 10 mm margin around
the common hepatic artery |
|
Para-aortic lymph nodes | 16 | 10 mm margin around
the abdominal aorta, from the diaphragmatic aortic hiatus to the
upper border of the origin of the inferior mesenteric artery |
|
Posterior pancreaticoduodenal
lymph nodes | 13 | 10 mm around the
posterior pancreaticoduodenal artery |
|
Anterior pancreaticoduodenal
lymph nodes | 17 | 10 mm margin around
the anterior pancreaticoduodenal artery |
|
Peri-choledochal nodes | 12b2 | 10 mm margin around
the choledochal duct |
| Cystic
duct lymph nodes | 12c | 10 mm around the
cystic duct |
All lymph nodes nomenclature was based on the 3rd
English Edition of the Classification of BTC established by the
Japanese Society of Hepato-Biliary-Pancreatic Surgery (11). We included in the hepatoduodenal lymph
nodes (LN), also those around both portal vein and hepatic artery
(groups 12a1, 12a2, 12p1 and 12p2), for anatomic contiguity of the
structures in the hepatic hilum. Furthermore, we assumed the
posterior pancreaticoduodenal LN (group 13) being similar to
retropancreatic LN. Finally, we respected the definition of left
and right paracardial LNs based on the gastric LNs contouring
Atlas, from Wo et al (12).
In this CTV-N delineation, a 10 mm margin of soft
tissue around vessels, ligament and ducts was suggested, based on
several literature data (12–15), without overlap with radiosensitive
structures (duodenum, liver, small bowel, stomach). Only for
para-cardials nodes and lesser gastric curvature nodes, the
suggested target was defined without any further expansion to
preserve the surrounding OARs.
Primary tumor CTV
Literature review
To define the CTV-T we studied the microscopic
extension of different sub sites of biliary cancers based on
available literature data.
Intrahepatic CC
Intrahepatic CC usually appears as a homogenous mass
with irregular but well-defined margins (mass-forming type).
Rarely, they present as small lesions with diffuse bile duct
thickening (periductal infiltrating type) or can grow
intraductally, showing only a duct ectasia with variable visible
mass (intraductal type) (16). Based
on the study of Bi et al (17), the microscopic extension from the
macroscopic disease ranged from 0.4 to 8.0 mm. From the comparison
between pathological evaluation of the surgical specimens and
radiological images, they concluded that the imaging-based gross
tumor volume (GTV) should be expanded by 9.8 mm to include any
microscopic disease with 100% accuracy.
Extrahepatic CCs
Extrahepatic CC show different behavior based on the
histological type. They can be described as papillary, nodular, and
sclerosing type. Papillary types often show an intraluminal growth,
whereas nodular and sclerosing types appear to spread
longitudinally along the submucosal layer. Chang et al
(18) reported a microscopic spread
of papillary, nodular, and sclerosing types of 15.6, 10.0, and 15.6
mm in 90% of cases, respectively. For the latter two histological
types, the length of microscopic tumor spread negatively correlates
with macroscopic tumor size. Ebata et al (19) reported 10 mm intramural extension
spread in all directions but observed that considering the
superficial involvement, surgical margins of 20 mm could be assured
to be negative proximally in 89.0% of cases and distally in
93.8%.
Gallbladder carcinoma (GC)
GC presents an early invasion through the subserosal
layer, due to the thin wall and lack of a muscolaris mucosae
(20). Depending on the type of
growth, Kondo et al (21)
classified GC as: i) Hepatic bed type, where the mass penetrates
through the gallbladder bed; ii) hepatic hilum type, with
infiltration of the hepatic hilum from the neck of the gallbladder;
iii) bed and hilum type, with massive invasion; iv) lymph node
type, with only lymphatic involvement; v) cystic duct type and vi)
localized type. There is lack of analyses in literature on
microscopic extension evaluation. Only Ogura et al (20) demonstrated an average microscopic
extension in most aggressive cases of advanced stage GC of 15.2 mm
(range: 2 to 25 mm).
Primary tumor CTV definition
Based on previously reported literature data, we
defined the CTV-T for the three different sub sites.
Intrahepatic CC
Based on the study of Bi et al (17), for intrahepatic CC we added 10 mm
radially to the GTV for CTV-T delineation (Table I).
Extrahepatic CC
Based on Chang et al (18) and Ebata et al data (19), our suggested CTV-T includes the GTV
plus 25 mm proximally and 20 mm distally through the bile duct, and
15 mm radially in all other directions (Table II).
 | Table II.CTV for extrahepatic
cholangiocarcinoma. |
Table II.
CTV for extrahepatic
cholangiocarcinoma.
| Delineation
type | JSHBPS
classification | Recommended
margins |
|---|
| Tumor
delineation |
|
Extrahepatic
cholangiocarcinoma | – | GTV + 25 mm on the
proximal direction of the bile duct + 20 mm on the distal direction
+ 15 mm radially in all directions |
| Lymph node group,
nodes delineation |
|
Hepatoduodenal ligament lymph
nodes | 12 | 10 mm margin around
the segment of portal vein from the confluence between the right
and left hepatic ducts and the upper border of the pancreas |
| Left
gastric artery lymph nodes | 7 | 10 mm around the
trunk of the left gastric artery |
| Common
hepatic artery lymph nodes | 8 | 10 mm margin around
the common hepatic artery |
|
Para-aortic lymph nodes | 16 | 10 mm margin around
the abdominal aorta, from the diaphragmatic aortic hiatus to the
upper border of the origin of the inferior mesenteric artery |
| Posterior
pancreaticoduodenal lymph nodes | 13 | 10 mm around the
posterior pancreaticoduodenal artery |
| Anterior
pancreaticoduodenal lymph nodes | 17 | 10 mm margin around
the anterior pancreaticoduo denal artery |
|
Peri-choledochal nodes | 12b2 | 10 mm margin around
the choledochal duct |
GC
Based on Ogura et al (20), for optimal control of microscopic
disease we suggest including in the CTV-T the GTV plus 25 mm
radially in the hepatic direction and any gallbladder residual
volume (Table III).
Overall CTV definition
The definition of the overall CTV was achieved by
merging the CTV-N as defined in our previous analysis (10), and the CTV-T as described in the
previous paragraph. The CTV-N definition was performed by including
for every sub site, all lymph node stations with an incidence of 5%
of metastasis (10).
Atlas design
Three patients with locally advanced unresectable
intrahepatic CC, extrahepatic CC, and GC were enrolled in this
study. Three different CTVs were defined according to the method
described above. Patients were immobilized in a customized Alpha
Cradle. GTV was delineated using contrast enhanced planning
computer tomography (CT) scans. Contouring of each anatomical
structure close to the tumor was performed by experienced
radiologists (MR, LC, GS, SG, RG) and radiation oncologists (GM,
FD, GCM, FC, AG).
Results
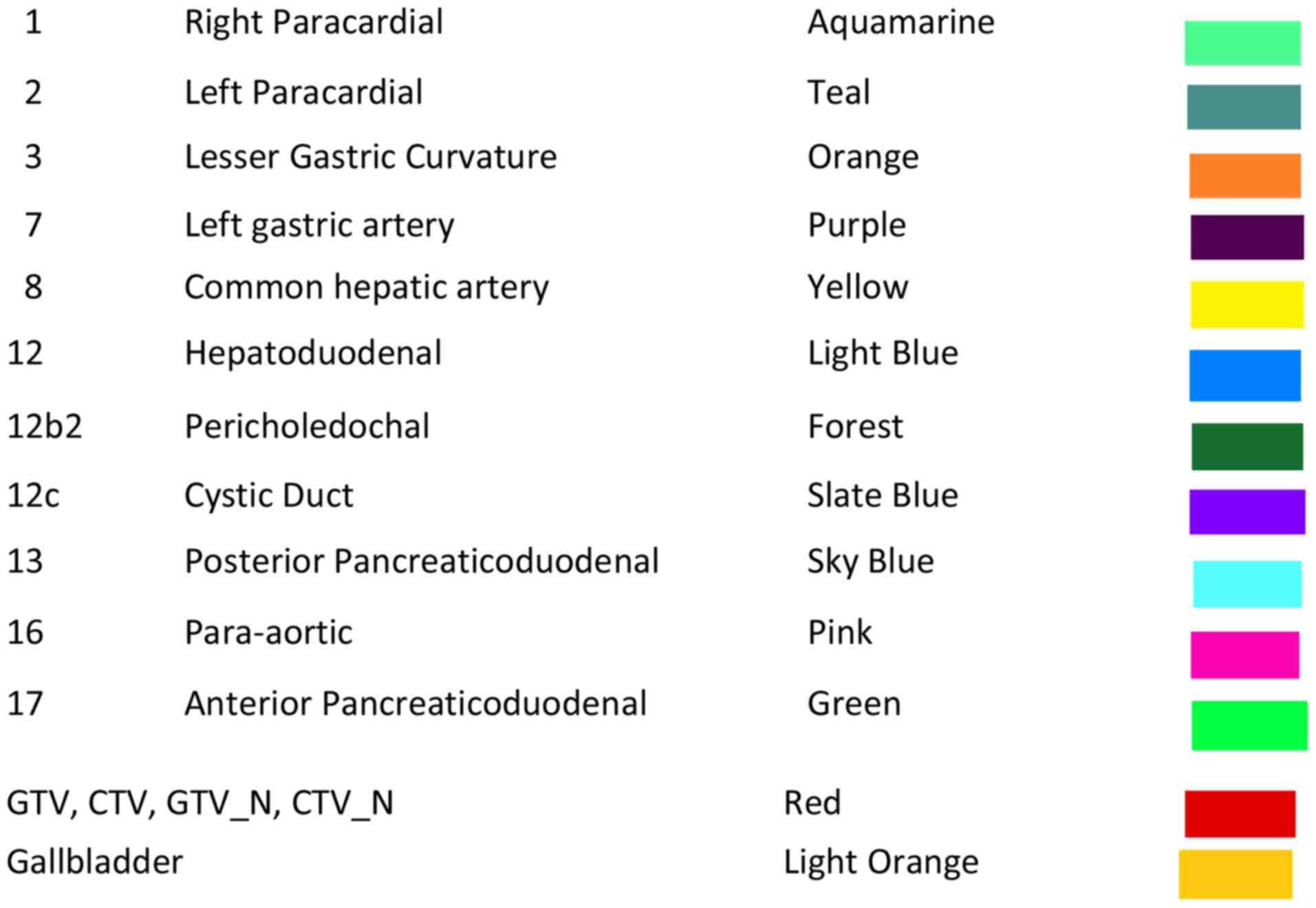
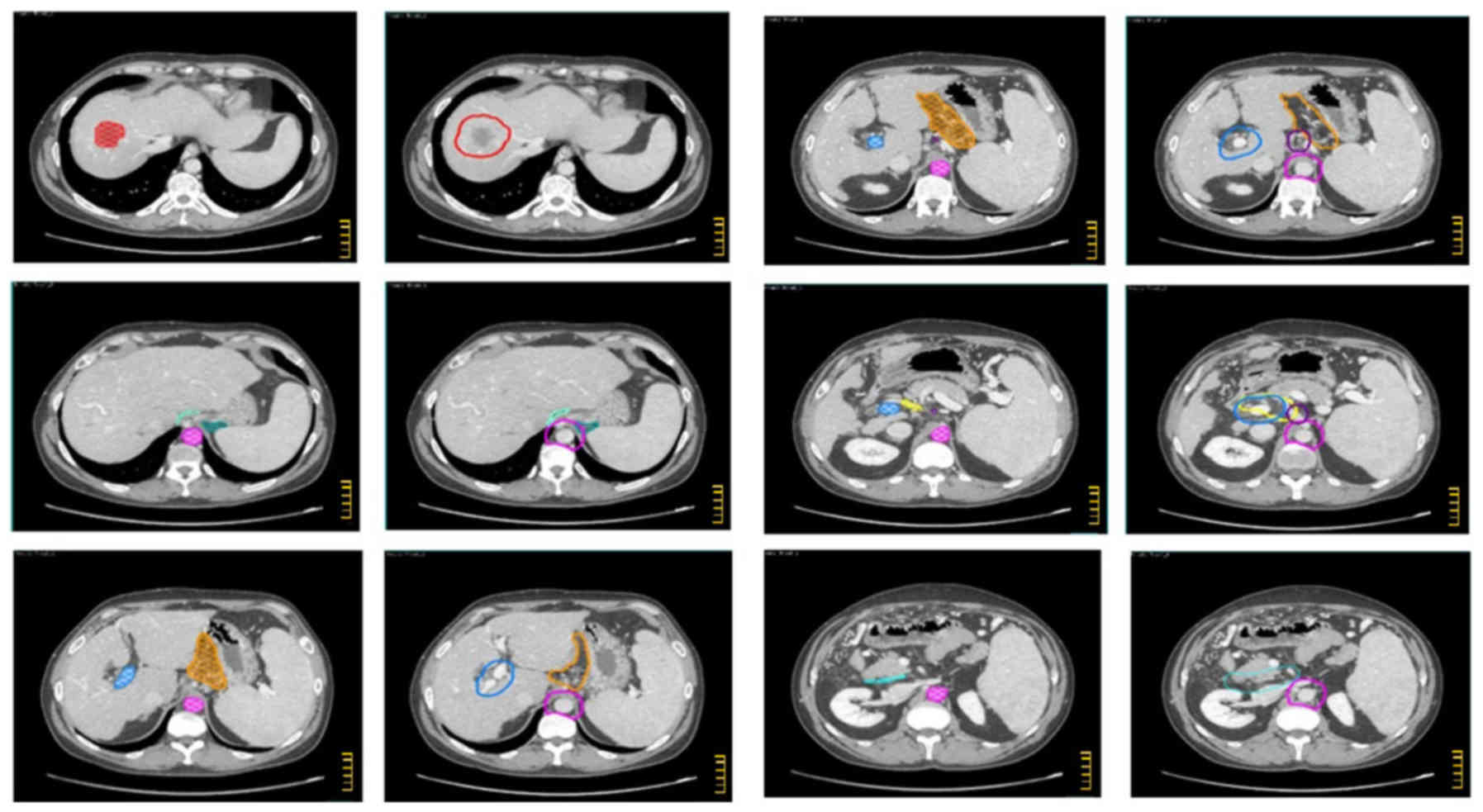
The CTV-N, CTV-T and overall CTV are described in
Tables I–III and shown in the atlas (Figs. 1–3)
regarding intrahepatic CC, extrahepatic CC, and GC, respectively.
In the atlas, the GTV and the main anatomical structures used as
land marks are indicated with different colors. Furthermore, on the
same figures, the different nodal sub sites and CTVs are also
delineated with different colors. The legend of used colors and
corresponding structures are shown in Fig. 4.
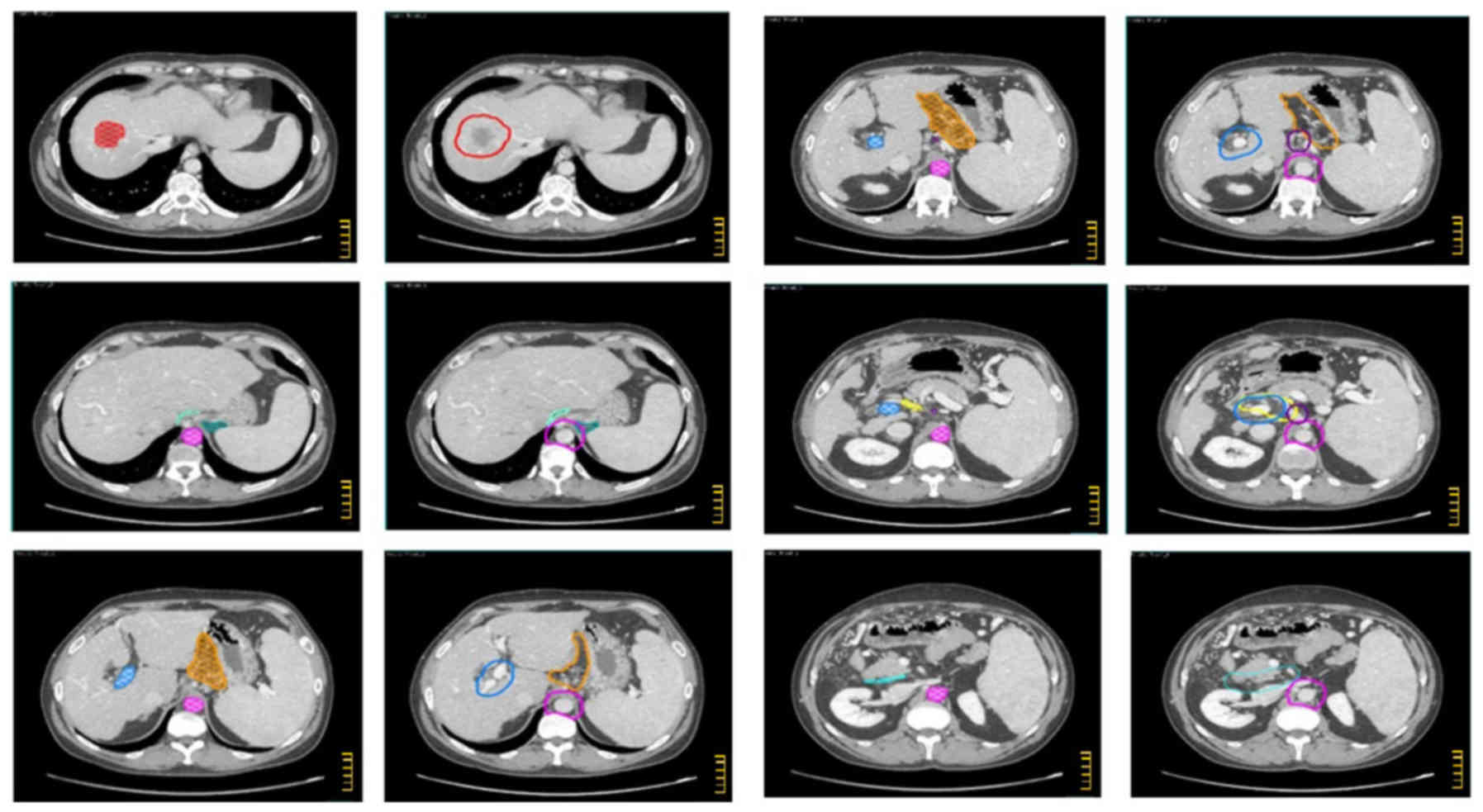
 | Figure 1.CTV definition for intrahepatic
cholangiocarcinoma. Color wash structures: GTV (red), aorta (pink),
left cardias (teal), right cardias (acquamarine), left gastric
artery (purple), portal vein (light blue), common hepatic artery
(yellow), lesser gastric curvature (orange), posterior
pancreatico-duodenal artery (sky blue). Contoured structures: CTV
(red), para-aortic LNs (purple), left para-cardial LNs (teal),
right para-cardial LNs (acquamarine), left gastric artery LNs
(purple), hepatoduodenal ligament (light blue), common hepatic
artery LNs (yellow), lesser gastric curvature LNs (orange),
posterior pancreatico-duodenal LNs (sky blue). The scale bar on the
figures is at 1 cm interval. |
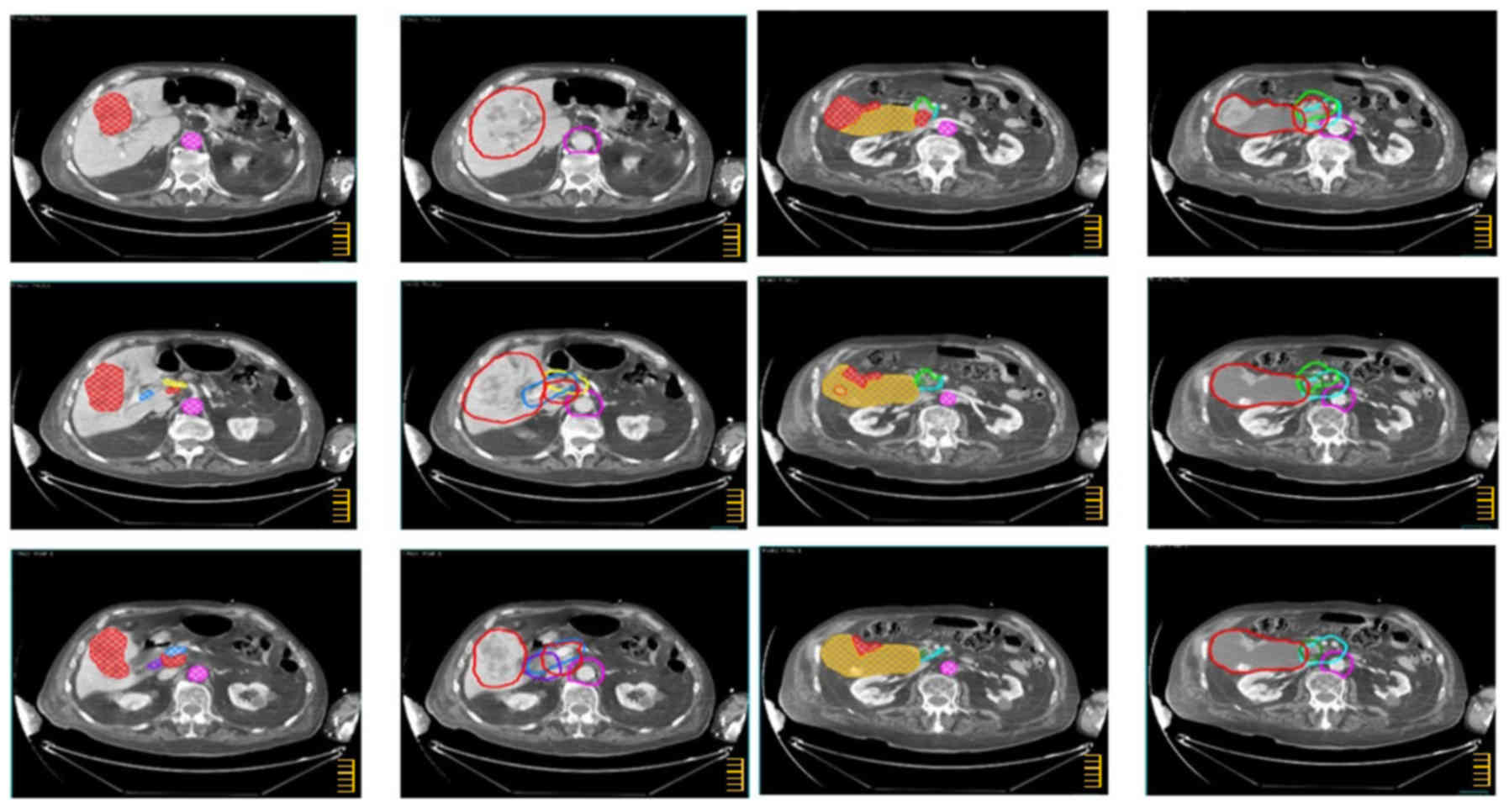
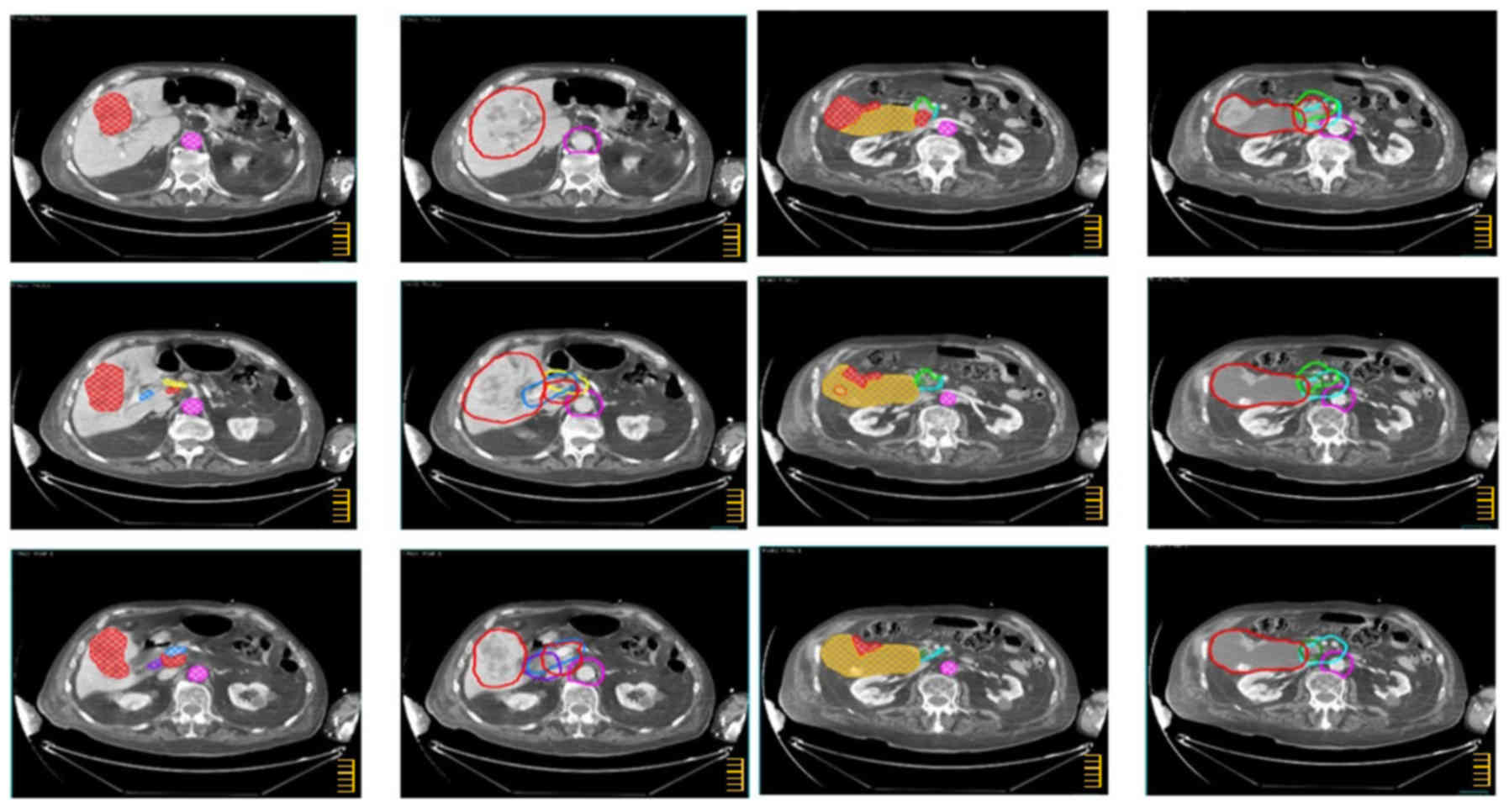 | Figure 3.CTV definition for gallbladder
carcinoma. Color wash structures: GTV (red), aorta (pink), portal
vein (light blue), common hepatic artery (yellow), posterior
pancreatico-duodenal artery (sky blue), anterior
pancreatico-duodenal artery (green), choledochal duct (forest),
cystic duct (slate blue), gallbladder (light orange), GTV_N (red).
Contoured structures: CTV (red), para-aortic LNs (purple),
hepatoduodenal ligament (light blue), common hepatic artery LNs
(yellow), posterior pancreatico-duodenal LNs (sky blue), anterior
pancreatico-duodenal LNs (green), pericholedochal LNs (forest),
cystic duct LNs (slate blue), gallbladder (light orange), CTV_N
(red). The scale bar on the figures is at 1 cm interval. |
Discussion
Locally advanced unresectable disease is the most
common presentation of BTC. Some studies demonstrated that
combined-modality therapy based on chemoradiation +/-BT boost could
reduce pain and improve LC, biliary decompression, and OS (6–9). In a
recent retrospective study on 37 patients with unresectable
extrahepatic CC treated with chemoradiation, 1-year LC and OS rates
were 90 and 59%, respectively (8).
Unfortunately, the results recorded in recent years
(22–27) did not show a significant improvement
of patients' outcome, which remain similar to those recorded in
previous decades (6–9). An improvement in the clinical results
could derive from innovative combinations with systemic therapies
and/or from a more intensive use of most advanced RT techniques
(IMRT, VMAT, IGRT). These could allow the delivery of higher RT
doses without worsening radio-induced toxicity. However, these
increasingly precise and conformed techniques require clearer
guidelines for the contouring of the target and our atlas can
represent a first proposal in this direction.
Our study presents some limitations mainly due to
the paucity of data cancerning BTC microscopic and nodal spread. In
fact, the information found in the analyzed studies were mainly
generic, without differentiation based on tumor stage and
sub-sites, nodal stage, and site of positive nodes. Therefore, we
were unable to give specific indications about CTV definition based
on the different stages and sub-sites of the three main BTCs. It
represents a limitation of our results and an area for future work
in this issue.
Obviously, the guidelines illustrated in this atlas
should be adapted to individual patients. Particularly, careful
attention must be given to inclusion in the target of any suspected
or positive node, even if outside the proposed CTV.
Further pathological studies and sentinel node
analysis would be useful to better understand the microscopic and
lymphatic spread of these tumors based on tumor stage and nodal
involvement.
The recommendations summarized in our atlas could be
supplemented in future by pattern of failure studies where patients
undergoing concurrent chemoradiation are closely followed using
modern imaging techniques to define the most frequent sites of
disease relapse. Studies of this type could lead to a more advanced
version of the atlas.
We should underline that our study has been
performed according to scientific literature where an atlas for
target delineation is presented using the images of a single
patient or as in this case, a few exemplary patients with different
tumor sites. Clearly, this modality cannot give us information on
the feasibility of large-scale application of the atlas. In
particular, we cannot estimate the impact of this type of target
contouring on OaRs irradiation. Therefore, further prospective
studies testing feasibility and efficacy of this CTV delineation
modality are justified.
In the last decade, there were no significant
improvements in the outcome of patients with biliary tumors treated
with chemoradiation. Therefore, innovative prospective trials are
needed to improve clinical outcomes. This atlas, while providing
practical guidelines for CTV delineation, could represent the basis
to design these new studies.
Acknowledgements
The abstract has previously been presented as an
oral communication at XXVII Congresso Nazionale Associazione
Italiana Radioterapia Oncologia, Rimini, Italy, November 11–13,
2017 and at the 37th Annual meeting of the European Society for
Radiotherapy & Oncology, Barcelona, Spain, April 20–24, 2018 as
an electronic poster.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
AGM and AG contributed to the conception and design
of the study. SB, MB and AGM conducted the literature review. SB,
AG, LF, MB and AGM wrote the manuscript. MR, LC, GS, SG and RG
designed the atlas. AG, GCM, FD and GM defined the targets. SCa,
AA, SCi and FD evaluated the images delineation. SCi, MB, AA, LG,
LF, FC, GM and GB analyzed and interpreted the data. SCa, AA, LG,
FC, GB and SCi critically revised the article for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
All patients provided written informed consent for
the use of their images. The study protocol was approved by the
Ethics Committee of ‘Giovanni Paolo II’ Foundation, Catholic
University of the Sacred Heart, Campobasso, Italy.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Shaib T and El-Serag HB: The epidemiology
of cholangiocarcinoma. Semin Liver Dis. 24:115–125. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bragazzi MC, Cardinale V, Carpino G,
Venere R, Semeraro R, Gentile R, Gaudio E and Alvaro D:
Cholangiocarcinoma: Epidemiology and risk factors. Tranls
Gastrointest Cancer. 1:21–32. 2012.
|
|
3
|
Siegel R, Ma J, Zou Z and Jemal A: Cancer
statistics, 2014. CA Cancer J Clin. 64:9–29. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
NCCN guideline version 2018, Hepatobiliary
Cancers. http://www.nccn.org/professionals/physician_gls/default.aspxMarch
17–2018
|
|
5
|
Valle JW, Borbath I, Khan SA, Huguet F,
Gruenberger T and Arnold D: ESMO Guidelines Committee: Biliary
cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment
and follow-up. Ann Oncol. 27 Suppl 5:v28–v37. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mattiucci GC, Autorino R, D'Agostino GR,
Deodato F, Macchia G, Perri V, Tringali A, Morganti AG, Mutignani M
and Valentini V: Chemoradiation and brachytherapy in extrahepatic
bile duct carcinoma. Crit Rev Oncol Hematol. 90:58–67. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Deodato F, Clemente G, Mattiucci GC,
Macchia G, Costamagna G, Giuliante F, Smaniotto D, Luzi S,
Valentini V, Mutignani M, et al: Chemoradiation and brachytherapy
in biliary tract carcinoma: Long-term results. Int J Radiat Oncol
Biol Phys. 64:483–488. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ghafoori AP, Nelson JW, Willett CG, Chino
J, Tyler DS, Hurwitz HI, Uronis HE, Morse MA, Clough RW and Czito
BG: Radiotherapy in the treatment of patients with unresectable
extrahepatic cholangiocarcinoma. Int J Radiat Oncol Biol Phys.
81:654–659. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chopra S, Mathew AS, Engineer R and
Shrivastava SK: Positioning high-dose radiation in
multidisciplinary management of unresectable cholangiocarcinomas:
Review of current evidence. Indian J Gastroenterol. 33:401–407.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Marinelli I, Guido A, Fuccio L, Farioli A,
Panni V, Giaccherini L, Arcelli A, Ercolani G, Brandi G, Cammelli
S, et al: Clinical target volume in biliary carcinoma: A systematic
review of pathological studies. Ant Res. 37:955–961. 2017.
|
|
11
|
Miyazaki M, Ohtsuka M, Miyakawa S, Nagino
M, Yamamoto M, Kokudo N, Sano K, Endo I, Unno M, Chijiiwa K, et al:
Classification of biliary tract cancers established by the Japanese
Society of Hepato-Biliary-Pancreatic Surgery: 3(rd) English
edition. J Hepatobiliary Pancreat Sci. 22:181–196. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wo JY, Yoon SS, Guimaraes AR, Wolfgang J,
Mamon HJ and Hong TS: Gastric lymph node contouring atlas: A tool
to aid in clinical target volume definition in 3-dimensional
treatment planning for gastric cancer. Pract Radiat Oncol.
3:e11–e19. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Caravatta L, Sallustio G, Pacelli F,
Padula GD, Deodato F, Macchia G, Massaccesi M, Picardi V, Cilla S,
Marinelli A, et al: Clinical target volume delineation including
elective nodal irradiation in preoperative and definitive
radiotherapy of pancreatic cancer. Radiat Oncol. 7:862012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Taylor A, Rockall AG, Reznek RH and Powell
ME: Mapping pelvic lymph nodes: Guidelines for delineation in
intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys.
63:1604–1612. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Haijun Y, Qiuji W, Zhenming F, Yong H,
Zhengkai L, Conghua X, Yunfeng Z and Yahua Z: A new approach to
delineating lymph node target volumes for post-operative
radiotherapy in gastric cancer: A phase II trial. Radiother Oncol.
116:245–251. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chung YE, Kim MJ, Park YN, Choi JY, Pyo
JY, Kim YC, Cho HJ, Kim KA and Choi SY: Varying appearances of
cholangiocarcinoma: Radiologic-pathologic correlation.
Radiographics. 29:683–700. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Bi AH, Zeng ZC, Ji Y, Zeng HY, Xu C, Tang
ZY, Fan J, Zhou J, Zeng MS and Tan YS: Impact factors for
microinvasion in intrahepatic cholangiocarcinoma: A possible system
for defining clinical target volume. Int J Radiat Oncol Biol Phys.
78:1427–1436. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chang YR, Lee KB, Jang JY, Lim CS, Kang
MJ, Kwon W, Jung WH and Kim SW: Analysis of microscopic tumor
spread patterns according to gross morphologies and suggestions for
optimal resection margins in bile duct cancer. J Gastrointest Surg.
18:1146–1154. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ebata T, Watanabe H, Ajioka Y, Oda K and
Nimura Y: Pathological appraisal of lines of resection for bile
duct carcinoma. Br J Surg. 89:1260–1267. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ogura Y, Tabata M, Kawarada Y and Mizumoto
R: Effect of hepatic invasion on the choice of hepatic resection
for advanced carcinoma of the gallbladder: Histologic analysis of
32 surgical cases. World J Surg. 22:262–267. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kondo S, Nimura Y, Kamiya J, Nagino M,
Kanai M, Uesaka K and Hayakawa N: Mode of tumor spread and surgical
strategy in gallbladder carcinoma. Langenbecks Arch Surg.
387:222–228. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Baisden JM, Kahaleh M, Weiss GR, Sanfey H,
Moskaluk CA, Yeaton P, de Lange EE and Rich TA: Multimodality
treatment with helical tomotherapy intensity modulated
radiotherapy, capecitabine, and photodynamic therapy is feasible
and well tolerated in patients with hilar cholangiocarcinoma.
Gastrintest cancer Res. 2:219–224. 2008.
|
|
23
|
Phelip JM, Vendrely V, Rostain F, Subtil
F, Jouve JL, Gasmi M, Michel P, Le Malicot K, Smith D, Seitz JF, et
al: Gemcitabine plus cisplatin versus chemoradiotherapy in locally
advanced biliary tract cancer: Fédération francophone de
cancérologie digestive 9902 phase II randomized study. Eur J
Cancer. 50:2975–2982. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Autorino R, Mattiucci GC, Ardito F,
Balducci M, Deodato F, Macchia G, Mantini G, Perri V, Tringali A,
Gambacorta MA, et al: Radiochemotherapy with gemcitabine in
unresectable extrahepatic cholangiocarcinoma: Long-term result of a
phase II study. Anticancer Res. 36:737–740. 2016.PubMed/NCBI
|
|
25
|
Lee KJ, Yi SW, Cha J, Seong J, Bang S,
Song SY, Kim HM and Park SW: A pilot study of concurrent
chemoradiotherapy with gemcitabine and cisplatin in patients with
locally advanced biliary tract cancer. Cancer Chemother Pharmacol.
78:841–846. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yi SW, Kang DR, Kim KS, Park MS, Seong J,
Park JY, Bang SM, Song SY, Chung JB and Park SW: Efficacy of
concurrent chemoradiotherapy with 5-fluorouracil or gemcitabine in
locally advanced biliary tract cancer. Cancer Chemother Pharmacol.
73:191–198. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen SC, Chen MH, Li CP, Chen MH, Chang
PM, Liu CY, Tzeng CH, Liu YM, Yen SH, Chao Y and Huang PI: External
bean radiation therapy with or without concurrent chemotherapy for
patients with unresectable locally advanced hilar
cholangiocarcinoma. Hepatogastroenterology. 62:102–107.
2015.PubMed/NCBI
|