Introduction
Uniportal video-assisted thoracic surgery has become
one of the most important development directions of minimally
invasive thoracic surgery since the first case of uniportal
video-assisted thoracic lobectomy was performed in 2011 by Gonzalez
et al (1). In recent years,
an increasing number of thoracic surgeons have tried pulmonary
lobectomy or segmentectomy in uniportal video-assisted thoracic
surgery, thoracic experts have attempted sleeve lobectomy, tracheal
and carinal resection and other difficult surgery.
In 2003, Migliore (2)
first reported the application of uniportal video-assisted thoracic
surgery in the diagnosis and treatment of non-complex pleural
diseases. Rocco (3) reported
uniportal video-assisted thoracic surgical resections in 2004.
Miyajima et al (4) and Okada
(5) reported uniportal
video-assisted thoracic lobectomy and segmentectomy in 2011 and
2012, respectively. Uniportal video-assisted thoracic surgery is a
trend of endoscopic surgery. Compared with the conventional
thoracoscopic surgery, the incision is slightly forward, where the
intercostal space is relatively wide. The impact of the operation
on the intercostal nerve will be minimized, and the postoperative
pain of the patient will be alleviated with minor trauma (6). Consequently, it is more acceptable to
patients. Moreover, due to the smaller incision, the limited
viewing field and operating space require surgeons with excellent
skills. Different from conventional thoracoscopic surgery in the
operation ideas, it requires a long learning curve to change from
three-portal video-assisted thoracoscopic surgery to uniportal
video-assisted thoracic surgery. As a result, only a handful of top
specialists from major hospitals are performing the procedure.
However, due to only 2 surgeons in uniportal video-assisted
thoracic surgery, only one incision and lack of assistant, it
enhances the difficulty of surgical exposure, so that it becomes a
major problem of beginners to expose the surgical field in
uniportal video-assisted thoracic surgery. How to get a surgical
field without increasing extra distinct wound is the aim of this
study. We adopted the self-made thoracic needled suspending device
with a snare to help expose a surgical field in uniportal
video-assisted thoracic surgery and obtained an excellent
results.
Patients and methods
Patients
Eighty patients who received uniportal
video-assisted thoracic surgery in Mount Qianfuo Attatched Hospital
of Shandong University (Jinan, China) between July 2016 and July
2018 were enrolled. Among them, there were 52 males and 28 females,
aged from 28 to 76 years. Two patients had mild cough, and other
patients had no obvious clinical symptoms such as cough, fever,
bloody sputum and chest pain. These patients were randomly divided
into observation group and control group. Forty patients in the
observation group received the operation using the self-made
thoracic needled suspending device with a snare which hang affected
lungs, left and right vagus nerve at the level of tracheal
bifurcation, the arch of azygos vein, left phrenic nerve and left
and right bronchus on the chest wall to expose surgical field in
order to perform fluent operation. Another 40 patients in the
control group received the conventional uniportal video-assisted
thoracic surgery without using the self-made device. Systematic
mediastinal lymphadenectomy was performed in both groups. Operation
time, intraoperative blood loss, postoperative extubation time,
hospital stay and perioperative complications in the early stage of
patients in both groups were compared.
Retrospectively 80 cases of pulmonary lobectomy or
segmentectomy were analyzed with systematic mediastinal
lymphadenectomy in uniportal video-assisted thoracic surgery for
lung cancer. In the obervation group, the device was used to hang
affected lungs, left and right vagus nerve at the level of tracheal
bifurcation, the arch of azygos vein, left phrenic nerve and left
and right bronchus on the chest wall to offer a better exposure of
the operation field. In the control group, the self-made device was
not used. The assistant helped to expose the surgical field or the
surgeon used an elbow aspirator to expose the surgical field. The
rest of the surgical operations were the same in both groups.
This study was approved by the Ethics Committee of
Mount Qianfuo Attatched Hospital of Shandong University. Signed
informed consents were obtained from the patients and/or
guardians.
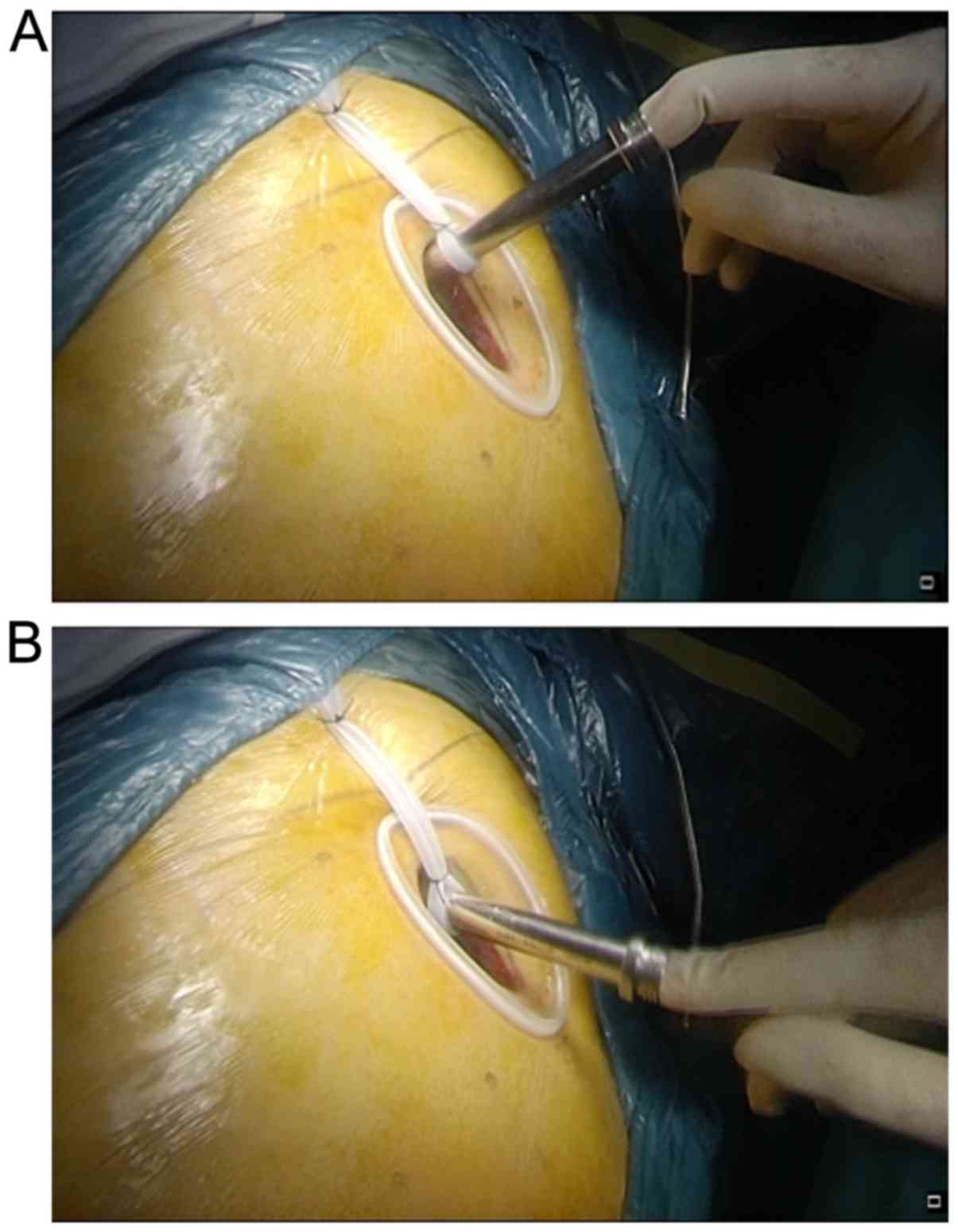
Preparation of the self-made thoracic needled
suspending device with a snare
Materials
Puncture needle (a transfusion puncture hollowed
needle), snare thread (a strip of 3-0 prolene), overhanging thread
(a strip of 7# silk thread), and 8# folded silicon ureter. The
materials were easily obtained in the operation room. The self-made
thoracic needled suspending device with a snare was made before
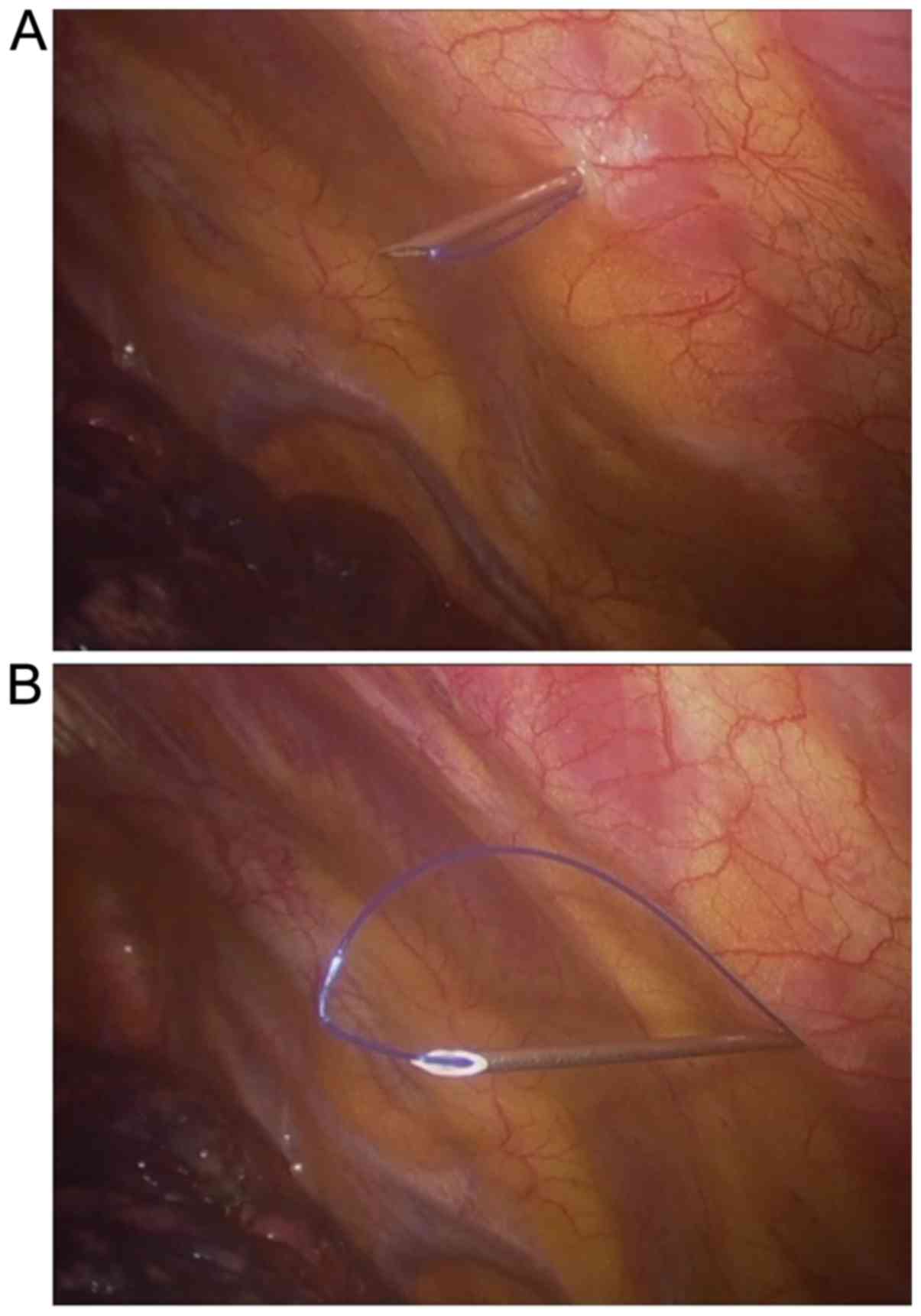
surgery. Firstly using a strip of 3-0 prolene passed the
transfusion puncture hollowed needle, and ligated the two ends of
the 3-0 prolene, so that a prolene loop was gained. Secondly, using
the transfusion puncture hollowed needle the suited point of the
chest wall was prodded, then the whole needle head was made in the
patient thoracic cavity. The needle was withdrawn about 1–2 cm, so
the prolene formed a snare, like a ring, at the pinhead of the
hollowed needle in thoracic cavity (Fig.
1). Lastly the prolene ring was passed using a strip of 7# silk
thread which pulled tissues needed, the hollowed needle was
dropped, and the prolene pulled out of the chest wall. At the same
time, the 7# silk thread was fixed and pulled out of the chest
wall. When a long time was needed at some part in the surgery, this
device was used to obtain favorable surgical field by overhanging
tissue to a suitable point of the chest wall. The tissues which
were often overhung were left and right vagus nerve at the level of
tracheal bifurcation, the arch of azygos vein, left and right
bronchus, left phrenic nerve, and diseased lungs.
Anesthesia and operative position
All patients were under general anesthesia, with
double-lumen intubition and single-lung ventilation, and in full
lateral decubitus position with flexion of the rotatable operation
table at the level of the mid-chest, allowing slight widening of
the intercostal space that improved exposure and facilitated access
to the pleural cavity. In the surgery, the rotatable operation
table can be rotated depending on operative need, so that
satisfactory operative field can be obtained because the lung can
be kept away from the surgical field due to the gravity of the
lung.
Surgical technique
Using uniportal video-assisted right upper lobectomy
through posterior approach with systematic mediastinal
lymphadenectomy as an example, we explain how the self-made needled
suspending device with snare play is used in exposing the surgical
field in uniportal video-assisted surgery.
i) Making incision: A 3–5 cm incision was made in
the fifth intercostal space posterior to the anterior axillary line
and a wound protector was commonly placed. One end of a strip of 8#
folded silicon ureter on the posterior side of the incision 5 cm
away from the wound protector was sutured and fixed, and the other
end was fixed on a camera cannula to facilitate the camera in and
out of the chest cavity. The operation was performed 2–4 cm ahead.
When rotated in different direction, the thoracoscope was kept on
the back edge of the incision in camera cannula by the traction of
elasticity of the 8# folded silicon ureter from beginning to end
(Fig. 2). Consequently, there is a
supporting point for camera holder, and the assistant could use one
hand to handle the camera and the other hand to help exposure or
sucking.
ii) Round oval forceps were used to lift part of the
lung tissue, with pointed curved forceps clamp. 7# silk thread was
used to ligate part of the lung tissue, and the hollow puncture
needle of the prefabricated needle snare device was used to
puncture through the chest wall, so that the whole hollow needle
head enters the chest cavity, and then the needle was withdrawn
about 1–2 cm, the slip line forms a circle at the tip of the needle
in the chest cavity. Finally, the 7# thread of the suspension
tissue was inserted into the sliding coil in the chest cavity, and
the hollow needle was removed. The slip line was pulled out of the
chest wall, and the 7# thread was pulled out of the body and
suspended, and the tattoo clamp was fixed. As a result, the
affected lung is suspended in the appropriate direction of the
chest wall, thereby exposing the operating field opposite to the
suspension direction. It expanded the field of surgery. Then the
conventional uniportal video-assisted thoracic lobectomy and
segmentectomy were performed. Due to increased suspension-assisted
exposure during the operation, the assistance through a single hole
is reduced, thus reducing the interference of the instruments
during the operation.
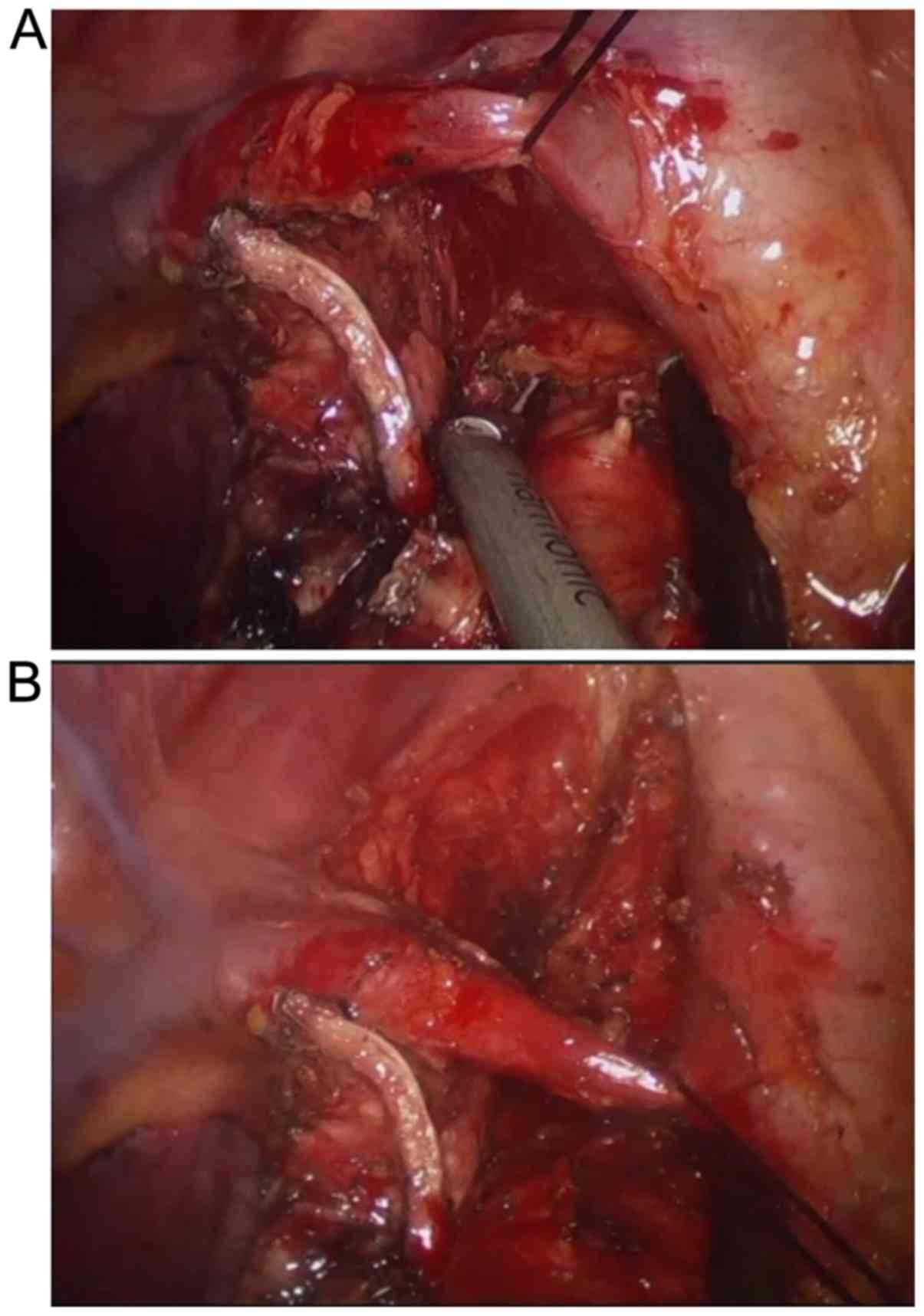
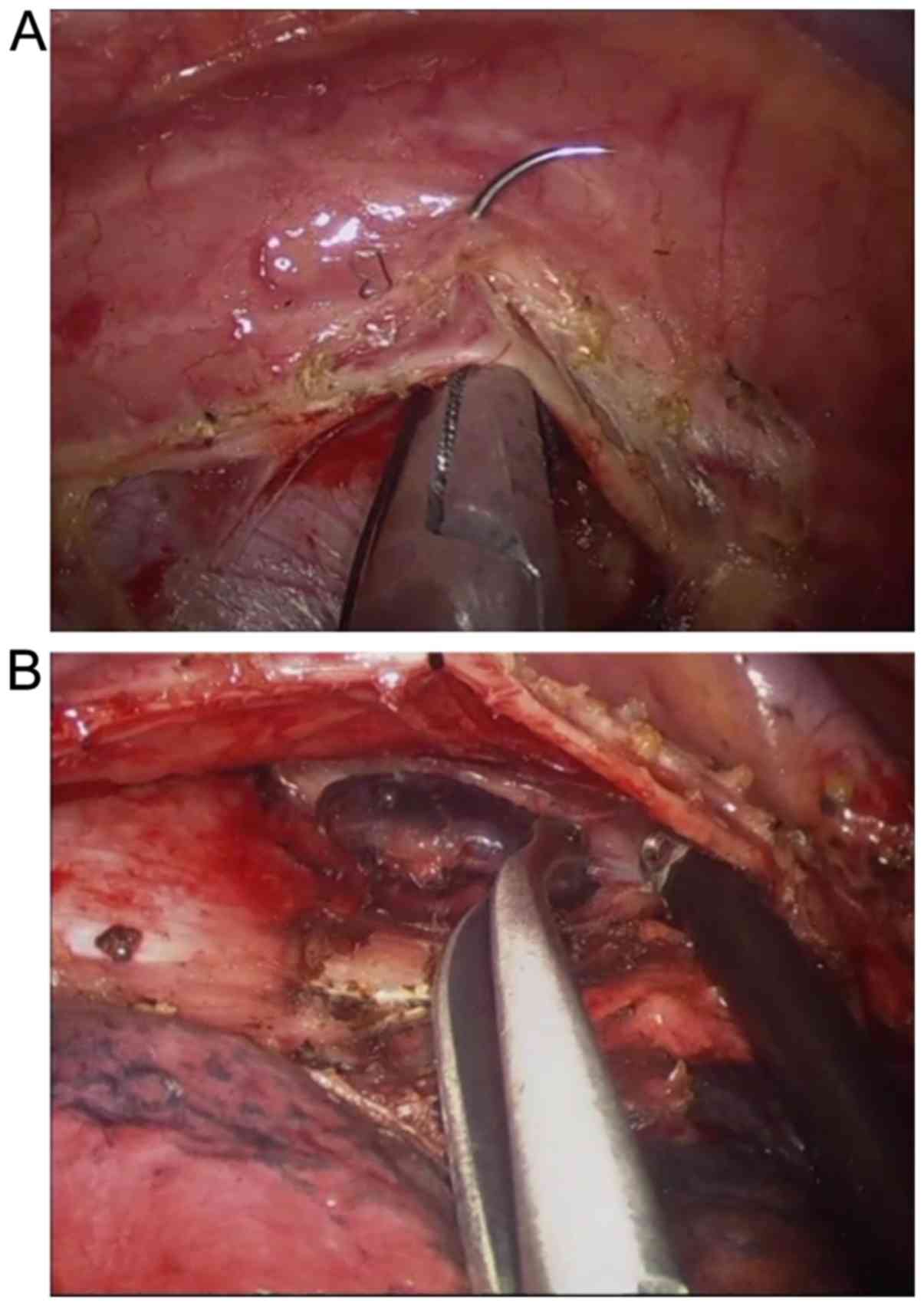
iii) By using the method of ligation or suture belt
mentioned above, nerve, blood vessel, bronchus were suspended in
the appropriate position of the chest wall to help the exposure of
surgical field. The right vagus nerve and pleura under the carina
were suspended in the posterior chest wall to expose the
supraspinatus surgery field, so as to facilitate the dissection of
7 groups of lymph nodes (Fig. 3).
The azygos arch was suspended in the forward, upper and lower
directions to facilitate the exposure of the surgical field for the
dissection of lymph nodes in groups 2 and 4 on the right (Fig. 4). The left phrenic nerve was
suspended in 2 directions forward and back to facilitate the
exposure of the surgical field, facilitating the dissection of the
left 5 and 6 groups of lymph nodes. The left main bronchus was
suspended forward and exposed to the left subcarina suture field to
facilitate dissection of the left 7 groups of lymph nodes. The left
main bronchus was suspended forward to facilitate dissection of the
left 4 groups of lymph nodes. It is suspended at the appropriate
position of the chest wall to assist the exposure of the surgical
field.
iv) At the end of the procedure, a strip of 20#
silicon tube was tunneled to thoracic apex through the
subcutaneous, serratus anterior and the upper border of the upper
lib of the incision. In addition, a central venous catheter was
used to puncture chest wall into the posterior costo-phrenic angle
for drainage.
Statistical analysis
SPSS 16.0 (SPSS, Inc., Chicago, IL, USA) statistical
software was used to analyze the data. The measurement data were
represented as mean ± SD, and t-test was used for comparison. The
comparison of count data was performed using χ2 test.
Difference at P<0.05 was considered to be statistically
significant.
Results
Of the 80 patients, 52 were males and 28 females, 50
patients underwent pulmonary lobectomy, and 30 patients underwent
pulmonary segmentectomy. There were 76 patients with
adenocarcinoma, 3 with squamous cell carcinoma, and 1 with small
cell carcinoma. Two patients converted to three port video-assisted
thoracic surgery because of extensive adhesion. One patient
converted to thoracotomy on account of middle lobar venous
hemorrhage, and the conversion rate was 2.5%. The rest received
successful uniportal video-assisted thoracic lobectomy and
segmentectomy as well as systematic mediastinal lymphadenectomy,
without serious complications or surgical death. The operation time
120.2±40.32 min, intraoperative blood loss 100.51±50.23 ml, and
postoperative suction drainage volume 208±97.56 ml/day in the
observation group were significantly different from those in the
control group (P<0.05), and there were no significant
differences in postoperative extubation time, hospital stay and
perioperative complications between the two groups (P>0.05)
(Table I).
 | Table I.Comparison of uniportal video-assisted
thoracic lobectomy and segmentectomy for lung cancer between two
groups. |
Table I.
Comparison of uniportal video-assisted
thoracic lobectomy and segmentectomy for lung cancer between two
groups.
| Items | Control (without the
self-made thoracic needled suspending device with a snare) | Observation (with the
self-made thoracic needled suspending device with a snare) | P-value |
|---|
| Case (n) | 40 | 40 | – |
| Operation time
(min) |
140.5±60.45 |
120.2±40.32a | 0.006 |
| Intraoperative blood
loss (ml) | 130.87±52.63 |
100.51±50.23a | 0.001 |
| Postoperative suction
drainage volume (ml/days) | 230.62±100.57 |
208±97.56a | 0.008 |
| Postoperative
extubation time (days) |
2.8±2.14 |
2.1±1.24a | 0.005 |
| Hospital stay after
operation (days) |
7.1±3.21 |
7.3±2.17 | 0.07 |
| Convert to three port
video-assisted thoracic surgery | 4 | 2 | 0.09 |
| Convert to
thoracotomy (n) | 0 | 1 | – |
| Serious
complications | 0 | 0 | – |
Discussion
Compared with three portal video-assisted thoracic
surgery, the vice operation hole of posterior axillary line and the
observation hole of axillary midline are not needed in the
uniportal video-assisted thoracic surgery. The incision was between
4th and 5th ribs of anterior axillary line with wide rib clearance,
few chest wall muscle layers and high elasticity, so the bleeding
is easy to be stopped, which leads to smaller damage to the body,
less postoperative pain and less impact on the patients' sensation
and movement (7). Chen et al
(8) compared the clinical effects of
20 cases of three portal video-assisted thoracic surgery and 10
cases of uniportal video-assisted thoracic surgery in the treatment
of pulmonary interstitial diseases, and found that the VAS score of
pain in the uniportal video-assisted thoracic surgery group on the
first day after surgery was 4.5±0.7 points significantly lower than
that of the three portal video-assisted thoracic surgery group
4.95±0.39 points with a statistically significant difference
(P=0.03. Bertolaccini et al (9) considered that unlike the three portal
video-assisted thoracic surgery, the uniportal video-assisted
thoracic surgery was closer to traditional open surgery.
Gonzalez-Rivas (10) reviewed the
evolution of thoracic surgery from open surgery, assisted
thoracoscopic surgery, total thoracoscopic surgery, the uniporta
thoracic surgery to the uniportal video-assisted thoracic surgery,
and believed that the perspectives of uniportal video-assisted
thoracic surgery and open surgery were basically similar.
Although it has more advantages in contrast with
three port surgery, it has its own disadvantages - the problem of
surgical exposure and the problem of instrumental mutual
interference. A retrospective analysis was performed on 40 patients
who underwent pulmonary lobectomy or segmentectomy with systematic
mediastinal lymphadenectomy in uniportal video-assisted thoracic
surgery for lung cancer. Self-made thoracic needled suspending
device with a snare was detailed in making and the method with
respect to this device, and right upper lobectomy and right
mediastinal lymphadenectomy in uniportal video-assisted thoracic
surgery were exampled for specific use of this device. Compared
with the conventional uniportal video-assisted thoracic surgery, it
has distinct advantages on blood loss and operation time.
Uniportal video-assisted thoracic surgery was
performed with the self-made thoracic needled suspending device
with a snare and was referred to as suspending uniportal
video-assisted thoracic surgery in this report. During the
operation, the self-made thoracic needled suspending device with a
snare was used to hang affected lungs, left and right vagus nerve
at the level of tracheal bifurcation, the arch of azygos vein, left
phrenic nerve and left and right bronchus on the chest wall in
uniportal video-assisted thoracic surgery to expose surgical field
in order to perform fluent operation. It was like a hand added in
the conventional uniportal video-assisted thoracic surgery to
facilitate the operation. The hand could help in different
directions in different locations on the chest wall to help the
fluent operation in various ways. This hand is invisible, and does
not pass through the chest wall incision. It only leaves a pinprick
on the chest wall which will not leave a scar after surgery. This
method can effectively offset the disadvantages of the uniportal
video-assisted thoracic surgery, including the mutual interference
of surgical instruments and the poor vision of the conventional
surgery. Since ligation and suture belt are used to fix target
tissue, it takes a certain time. To reduce the time of operation,
pulmonary forceps of the thoracoscope with a line will be used in
the future. Robotic surgery is a development direction of the
minimally invasive thoracic surgery and this method can be regarded
as low cost uniportal video-assisted thoracic robotic surgery,
because the mechanical hand can work in multiple directions. Like
the uniportal video-assisted thoracic robotic surgery, this method
could be an option for the thoracic surgery. Since this study
focuses on the feasibility of the surgical method, it has some
limitations. Long-term efficacy was not examined. Besides, this
study is a single center study, and multi-center study is still
required.
In conclusion, the self-made thoracic needled
suspending device with a snare is an excellent helper for uniportal
video-assisted thoracic surgery, because it helps to expose
surgical field and has no postoperative cicatrisation at puncture
point on the wall of the chest. The device and its use are worthy
of promotion.
Acknowledgements
Dr Shanlei Wang is grateful to Professor Diego
Gonzalez-Rivas for uniportal video-assisted thoracic surgery
training and wish to express his gratitude to Professor Song Zhao,
Professor Ge-Ning Jiang and Professor Zhong-Min Jiang for
mentoring.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SW, ZJ and DGR conceived the study and drafted the
manuscript. JR, WX, CM and CL acquired the data. LZ, GG and GY
analyzed the data. HT and JJ revised the manuscript and were
responsible for statistical analysis. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
Mount Qianfuo Attatched Hospital of Shandong University (Jinan,
China). Patients who participated in this research had complete
clinical data. The signed informed consents were obtained from the
patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gonzalez D, Paradela M, Garcia J and Dela
Torre M: Single-port video-assisted thoracoscopic lobectomy.
Interact Cardiovasc Thorac Surg. 12:514–515. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Migliore M: Efficacy and safety of
single-trocar technique for minimally invasive surgery of the chest
in the treatment of noncomplex pleural disease. J Thorac Cardiovasc
Surg. 126:1618–1623. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rocco G: One-port (uniportal)
video-assisted thoracic surgical resections - a clear advance. J
Thorac Cardiovasc Surg. 144:S27–S31. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Miyajima M, Watanabe A, Uehara M, Obama T,
Nakazawa J, Nakajiima T, Ogura K and Higami T: Total thoracoscopic
lung segmentectomy of anterior basal segment of the right lower
lobe (RS8) for NSCLC stage IA (case report). J Cardiothorac Surg.
6:1152011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Okada M: Identification of intersegmental
border in radical segmentectomy. Kyobu Geka. 63 (Suppl):697–701.
2010.(In Japanese). PubMed/NCBI
|
|
6
|
Ren M, Meng Q, Zhou W, Kong F, Yang B,
Yuan J, Wu D, Zhang J, Li Q, Lin Y, et al: Comparison of short-term
effect of thoracoscopic segmentectomy and thoracoscopic lobectomy
for the solitary pulmonary nodule and early-stage lung cancer. Onco
Targets Ther. 7:1343–1347. 2014.PubMed/NCBI
|
|
7
|
Shapiro M, Weiser TS, Wisnivesky JP, Chin
C, Arustamyan M and Swanson SJ: Thoracoscopic segmentectomy
compares favorably with thoracoscopic lobectomy for patients with
small stage I lung cancer. J Thorac Cardiovasc Surg. 137:1388–1393.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen PR, Chen CK, Lin YS, Huang HC, Tsai
JS, Chen CY and Fang HY: Single-incision thoracoscopic surgery for
primary spontaneous pneumothorax. J Cardiothorac Surg. 6:58. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bertolaccini L, Rocco G, Viti A and Terzi
A: Geometrical characteristics of uniportal VATS. J Thorac Dis. 5
(Suppl 3):S214–S216. 2013.PubMed/NCBI
|
|
10
|
Gonzalez-Rivas D: Evolving thoracic
surgery: From open surgery to single port thoracoscopic surgery and
future robotic. Chin J Cancer Res. 25:4–6. 2013.PubMed/NCBI
|