Introduction
Prostate cancer (PCA) is the second most common
malignant tumor following lung cancer and the fifth leading cause
of cancer-associated mortality in men worldwide (1). Prostate-specific antigen (PSA) is the
most widely used tumor marker for PCA in early diagnosis and
treatment evaluation (2). However,
PSA is not cancer specific; instead it is an organ-specific marker.
Benign prostatic hyperplasia (BPH), prostatic intraepithelial
neoplasia, acute and chronic prostatitis, and other non-malignant
prostate diseases may additionally lead to elevated plasma PSA
expression levels (3,4). Such a relatively low specificity may
lead to a false positive diagnosis in ≤65% of patients, if only the
plasma expression level of PSA was used to distinguish PCA from
benign diseases (4). In addition,
there is a weak correlation between PSA expression levels and PCA
severity, which undermines the use of PSA in disease grading
(5). At present, prostate biopsies
are necessary; however, it is an invasive method for precise
diagnosis in clinical practice. Therefore, more specific and
reliable biomarkers are required for the detection, diagnosis and
prognosis of PCA.
Interleukin (IL)-35 is a member of the IL-12
cytokine family, which possesses a unique immune regulatory
function. IL-35 is composed of an Epstein-barr virus-induced gene 3
(EBI3) subunit and IL-12A (p35) subunit (6). Previous studies demonstrated that IL-35
expression was increased in a variety of tumor tissues, including
pancreatic ductal adenocarcinoma (PDAC), colorectal cancer, renal
cell carcinoma and laryngeal squamous cell cancer (7–10).
Furthermore, IL-35 was demonstrated to promote tumor angiogenesis
and inhibit the anti-tumor cytotoxic lymphocyte response (11). Additionally, IL-35 protein expression
levels in the plasma are associated with tumor stages, tumor size
and the presence of adjacent lymph node metastasis in various types
of cancer, including PDAC and breast cancer (12,13),
suggesting that IL-35 may be associated with tumor progression.
Increased expression of IL-35 in tumor tissues and increased
expression levels in the plasma were associated with a poor
prognosis in a number of malignancies, including acute myeloid
leukemia, lung cancer, hepatocellular carcinoma and gastric cancer
(14–17).
At present, the expression patterns and functions of
IL-35 in PCA have not been studied extensively, to the best of the
authors' knowledge. Therefore, in the present study, plasma IL-35
protein expression levels in the peripheral blood and tumor tissues
of patients with PCA were examined, and the association between the
expression of IL-35 and the clinicopathological characteristics of
PCA was analyzed, to examine the potential involvement of IL-35 in
the progression of PCA.
Patients and methods
Patients and specimens
A total of 66 men with PCA [mean age ± standard
deviation (SD), 65.07±7.78 years], and 66 age-matched men with BPH
who were referred to The Tianjin Medical University Cancer Hospital
(Tianjin, China), between January 2013 and June 2014 were
recruited. The patients with PCA were enrolled in the present study
prior to receiving radiotherapy, chemotherapy or immunotherapy. In
addition, 56 healthy men, who visited The Tianjin Medical
University Cancer Hospital, were involved in the present study. The
healthy men were without acute or chronic diseases or any evidence
of malignancies. Individuals who smoked, were taking prescribed
medication, had a history of recurrent infections, asthma,
allergies or atopic diseases, or any other suspected immunological
diseases, were all excluded from the present study.
According to the medical records and pathological
reports, the existence of PCA was confirmed by surgery or needle
biopsy. The Tumor-Node-Metastasis (TNM) stage and clinical stage of
PCA were based on the principles for the Eighth Edition of the
American Joint Committee on Cancer TNM Staging Manual (18). The Gleason score was based on An
Update with Discussion on Practical Issues to Implement the 2014
International Society of Urological Pathology Consensus Conference
on Gleason Grading of Prostatic Carcinoma (19). Levels of PSA expression were obtained
from the patient medical records. The present study was approved by
The Ethics Committee of the Tianjin Medical University Cancer
Institute and Hospital. All participants were recruited subsequent
to providing written informed consent. A 5 ml specimen of
peripheral blood was obtained from all the individuals, and the
plasma was separated and stored at −80°C for analysis.
Measurement of the IL-35
concentration
The IL-35 concentration in the plasma was measured
using a human IL-35 ELISA kit (catalog no. SEC008Hu; Cloud-Clone
Corp., Katy, TX, USA) according to the manufacturer's protocol.
Each sample was assayed three times. The minimum detectable dose of
this kit is typically <5.8 pg/ml.
Human tumor specimens and
immunohistochemical staining
Human paraffin embedded tissue microarrays
(ProA180PG04; 90 cases/180 points) were ordered from Shanghai Outdo
Biotech Co. Ltd. (Shanghai, China). For the tissue microarray
1.5-mm core samples were used, and the thickness of the sections
was 4 µm. The major regents used were as follows: i) 10X PBS buffer
(formula: 80 g NaCl, 2 g KCl, 15.35 g
Na2HPO4, 2 g KH2PO4,
dissolved with deionized water up to 1 liter, pH 7.2). For 1X PBS
buffer, the 10X PBS buffer was diluted and the Tween reagents
(0.05% of total volume) were added; ii) citric acid solution: 0.1
mol/l sodium citrate solution (82 ml), 0.1 mol/l citric acid
solution (18 ml), deionized water (900 ml) (pH 6.0); and iii)
peroxidase-blocking reagent: 38.4 ml anhydrous methanol, 12 ml 30%
H2O2 and 9.6 ml ddH2O. The tissue
microarray was incubated in a dry oven at 63°C for 1 h. The
de-paraffinization and rehydration processes were performed at room
temperature. The slides were washed twice for 15 min each time with
Xylene and subsequently washed twice for 7 min with absolute
ethanol. Finally, the slides were washed for 5 min with 90, 80 and
70% ethanol, respectively. Subsequently, the slides were rinsed 3
times, for 1 min each time, with deionized water. Citric acid
high-pressure repair was used for antigen retrieval and the slides
were bathed in peroxidase-blocking reagent for 15 min at room
temperature. The sections were blocked with 3% BSA (Beijing
Solarbio Science and Technology Co., Ltd., Beijing, China; cat. no.
A8020), incubated with mouse anti-human p35 antibody (Abcam,
Cambridge, UK; cat. no. ab66064; 1:100) and rabbit anti-EBI3
antibody (Abcam; cat. no. ab83896; 1:100) overnight at 4°C in a
humidified chamber, and subsequently incubated with horseradish
peroxidase-conjugated secondary antibodies (Abcam; cat. nos.
ab97046 and ab6721; 1:800) at room temperature for 30 min. Finally,
expression was visualized with 3,3-diaminobenzidine (DAB) and
Mayer's hematoxylin staining. The slides were incubated with DAB
solution for 5 min and bathed for 40 sec in Mayer's hematoxylin
solution, both at room temperature. The Leica scanscope XT (Leica
Microsystems, Wetzlar, Germany) was used to capture the images
(magnification ×40 and ×200). The intensity score was evaluated
blindly by 3 independent observers using the following scoring
system: i) Negative, 0; ii) weak, 1; moderate, 2; and iii) strong,
3. The extent score was defined as: i) Negative, 0; ii) <25%
positive, 1; iii) 25–50% positive, 2; iv) 51–75% positive, 3; and
v) >75% positive, 4. The final score was calculated by
multiplying the scores of the intensity by the extent and dividing
the samples into four grades: i) Negative, 0, (−); ii) low
staining, 1–3, (+); iii) medium staining, 4–7, (++); and iv) high
staining, 8–12, (+++).
Statistical analysis
Statistical analyses were performed using SPSS 23.0
(IBM Corp., Armonk, NY, USA) or GraphPad Prism 7 (GraphPad
Software, Inc., La Jolla, CA, USA). Data are presented as the mean
± SD. A one-way analysis of variance was used, followed by the
least significant difference post hoc test, to determine the
statistical significance of differences between the
clinicopathological characteristics of the PCA, BPH and healthy
control groups. Continuous variables were measured using a
Kolmogorov-Smirnov test and a Student's t-test was used to test
parametric data. P<0.05 was considered to indicate a
statistically significant difference. A receiver operating
characteristic (ROC) curve was plotted and the area under the curve
(AUC) was calculated to compare the predictive value of each
independent variable. Kaplan-Meier survival curves were analyzed
for relevant variables. A log-rank test was used to analyze the
differences in survival times amongst different groups. A
Spearman's rank correlation coefficient test was used to test the
correlation of EBI3 and p35 in patients with PCA.
Results
General characteristics of the
participants
The clinical and pathological features of the
enrolled subjects are summarized in Table I. The mean age ± SD of each group was
as follows: Patients with PCA, 67.26±8.64 years; patients with BPH,
68.95±7.58 years; and the healthy control group, 69.30±10.71 years
(Table I; P=0.0631). The plasma PSA
expression levels in the patients with PCA, patients with BPH and
the HC group were 44.81±37.06, 9.92±10.41 and 1.40±1.39 µg/l,
respectively, and the plasma PSA expression levels were
significantly different across all three groups (Table I; P<0.0001). The mean PSA level in
the plasma of patients with PCA was significantly higher compared
with that in patients with BPH and in the healthy control group
(P<0.001). However, there was no significant difference in the
plasma PSA levels between patients with BPH and the healthy control
group (Table I; P=0.432).
 | Table I.Clinical characteristics of patients
with PCA, patients with BPH and the HC group. |
Table I.
Clinical characteristics of patients
with PCA, patients with BPH and the HC group.
| Characteristic | PCA | BPH | HC | F | P-value |
|---|
| n | 66 | 66 | 56 |
|
|
| Age, years | 67.26±8.64 | 68.95±7.58 | 69.30±10.71 | 2.805 | 0.0631 |
| PSA, µg/l | 44.81±37.06 | 9.92±10.41 | 1.40±1.39 | 63.950 |
<0.0001a |
| IL-35, pg/ml | 127.49±52.07 | 54.59±33.71 | 42.88±20.77 | 91.160 |
<0.0001a |
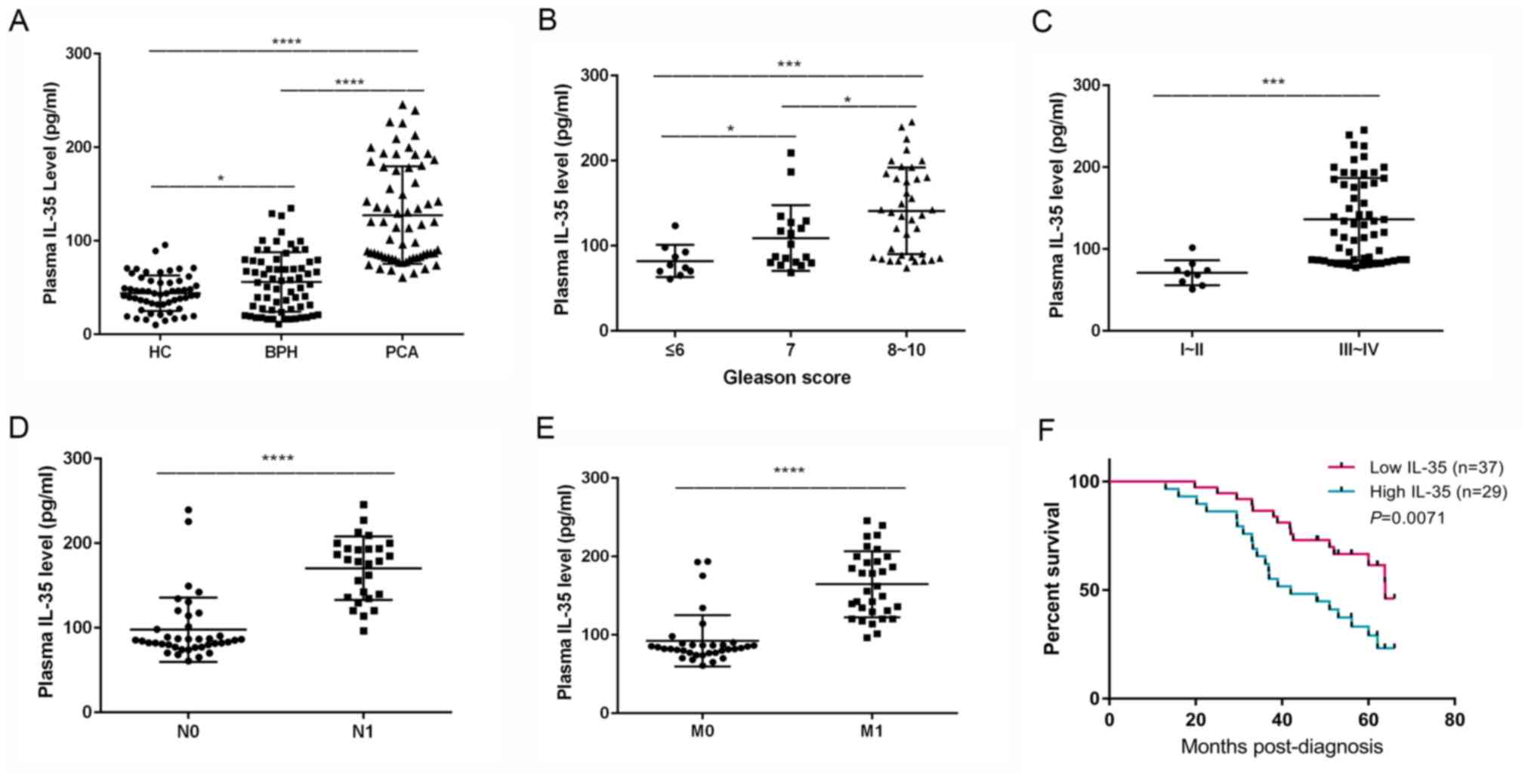
IL-35 plasma concentration in patients
with PCA and BPH, and healthy controls
The mean IL-35 plasma concentration of the three
groups was significantly different (P<0.0001). The mean IL-35
plasma concentration was significantly increased in patients with
PCA compared with the patients with BPH (127.49±52.07 vs.
54.59±33.71 pg/ml, respectively; P<0.0001; Table I). Similarly, the mean IL-35 plasma
concentration in the patients with BPH was significantly increased
compared with the healthy control group (54.59±33.71 vs.
42.88±20.77 pg/ml; P=0.0137; Table
I; Fig. 1A). The level of IL-35
in the PCA group was significantly higher compared with that in the
healthy control group (127.49±52.07 vs. 42.88±20.77 pg/ml;
P<0.0001; Table I; Fig. 1A).
Classification of patients with
PCA
The patients with PCA were classified into three
groups: Gleason score of ≤6, n=10; score 7, n=18; and score 8–10,
n=38 (Table II). The patients with
PCA were distributed according to their TNM stages with 9 patients
in stage I or II, and 57 patients in stage III or IV (Table II). There were 27 patients with PCA
with lymph node metastasis, compared with 39 patients without lymph
node metastasis. Additionally, there were 32 patients with PCA with
distant metastasis, including bone or lung metastasis compared with
34 patients without distant metastasis (Table II).
 | Table II.Demographic data and plasma
expression levels of IL-35 in patients with prostate cancer
according to different clinical and pathological
characteristics. |
Table II.
Demographic data and plasma
expression levels of IL-35 in patients with prostate cancer
according to different clinical and pathological
characteristics.
| Variables | Number of
cases | IL-35, pg/ml | t/F value | P-value |
|---|
| Age, years |
|
| 0.717 | 0.477 |
|
≥65 | 41 | 123.88±45.73 |
|
|
|
<65 | 25 | 134.09±61.55 |
|
|
| PSA, µg/l |
|
| 2.896 | 0.01a |
|
≥10 | 56 | 133.37±52.52 |
|
|
|
<10 | 10 | 94.55±36.13 |
|
|
| Gleason score |
|
| F=8.202 | 0.0007b |
| ≤6 | 10 | 82.07±18.92 |
|
|
| 7 | 18 | 109.12±38.67 |
|
|
|
8–10 | 38 | 141.05±51.07 |
|
|
| TNM stage |
|
| 3.831 | 0.0003b |
|
I–II | 9 | 70.87±15.26 |
|
|
|
III–IV | 57 | 136.26±50.54 |
|
|
| Lymph node
metastasis |
|
| 7.672 |
<0.000b |
|
Yes | 27 | 170.48±37.49 |
|
|
| No | 39 | 97.73±38.14 |
|
|
| Distant
metastasis |
|
| 7.784 |
<0.000b |
|
Yes | 32 | 164.64±42.15 |
|
|
| No | 34 | 92.53±32.77 |
|
|
Association of IL-35 plasma expression
levels with the clinicopathological characteristics of patients
with PCA
The IL-35 plasma concentrations of all the
individuals with PCA are presented in Table II. The IL-35 concentration in the
plasma of the individuals with Gleason scores of ≤6 (82.07±18.92),
7 (109.12±38.67) and 8–10 (141.05±51.07 pg/ml) were significantly
different (P<0.0001; Fig. 1B).
The concentration of plasma IL-35 in patients with PCA, with
Gleason scores of 7, was significantly higher compared with that in
those with a Gleason score of ≤6 (P=0.0489). The concentration of
plasma IL-35 in patients with PCA, with Gleason scores of 8–10, was
significantly higher compared with that of 7 (P=0.0225) and the
concentration of plasma IL-35 in patients with PCA with Gleason
scores of 8–10 was significantly higher compared with that of
patients with a score of ≤6 (P=0.0009). The IL-35 plasma
concentration was significantly increased in patients with PCA who
were classified with TNM stage III–IV (136.26±50.54 pg/ml) compared
with patients with TNM stage I–II (70.87±15.26 pg/ml; P=0.0003;
Table II; Fig. 1C). The IL-35 plasma concentration in
patients with PCA with lymph node metastasis was significantly
increased compared with individuals without lymph node metastasis
(170.48±37.49 vs. 97.73±38.14 pg/ml; P<0.0001; Table II; Fig.
1D). Similarly, the IL-35 plasma concentration was
significantly increased in patients with PCA with distant
metastasis compared with individuals without distant metastasis
(164.64±42.15 vs. 92.53±32.77 pg/ml; P<0.0001; Table II; Fig.
1E).
Furthermore, the overall survival rate of patients
with PCA with an increased IL-35 plasma concentration (greater than
the median value of 127.49 pg/ml; 42.0 months) was significantly
decreased compared with the patients with a decreased IL-35 plasma
concentration (less than the median value; 63.9 months; P=0.0071;
log-rank test; Fig. 1F).
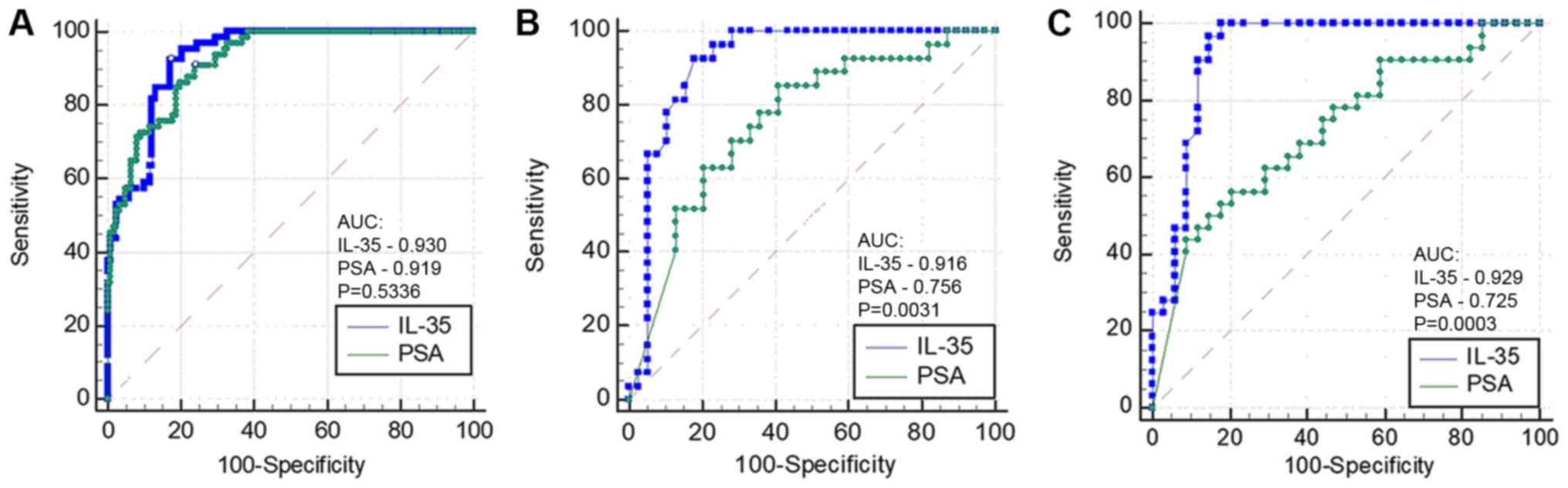
ROC curves of IL-35 and PSA expression
levels in plasma
The AUC of IL-35 did not differ significantly
compared with PSA in patients with PCA (AUC=0.930 vs. 0.919;
P=0.5336; Fig. 2A), and the
sensitivity, specificity and diagnostic accuracy were 92.42, 82.79
and 86.17%, respectively, at the best cut-off value of 70.99 pg/ml.
A significant difference was identified between IL-35 and PSA for
the detection of PCA with lymph node metastasis (AUC=0.916 vs.
0.756; P=0.0031; Fig. 2B), and at
the best cut-off value of 117.56 pg/ml, the sensitivity,
specificity and diagnostic accuracy of IL-35 were 92.59, 82.05 and
86.36%, respectively. A statistically significant difference was
observed between IL-35 and PSA in diagnosing PCA with distant
metastasis (AUC=0.929 vs. 0.725; P=0.0003; Fig. 2C), and at the best cut-off value of
90.43 pg/ml, the sensitivity, specificity and diagnostic accuracy
of IL-35 were 100, 82.35 and 90.91%, respectively.
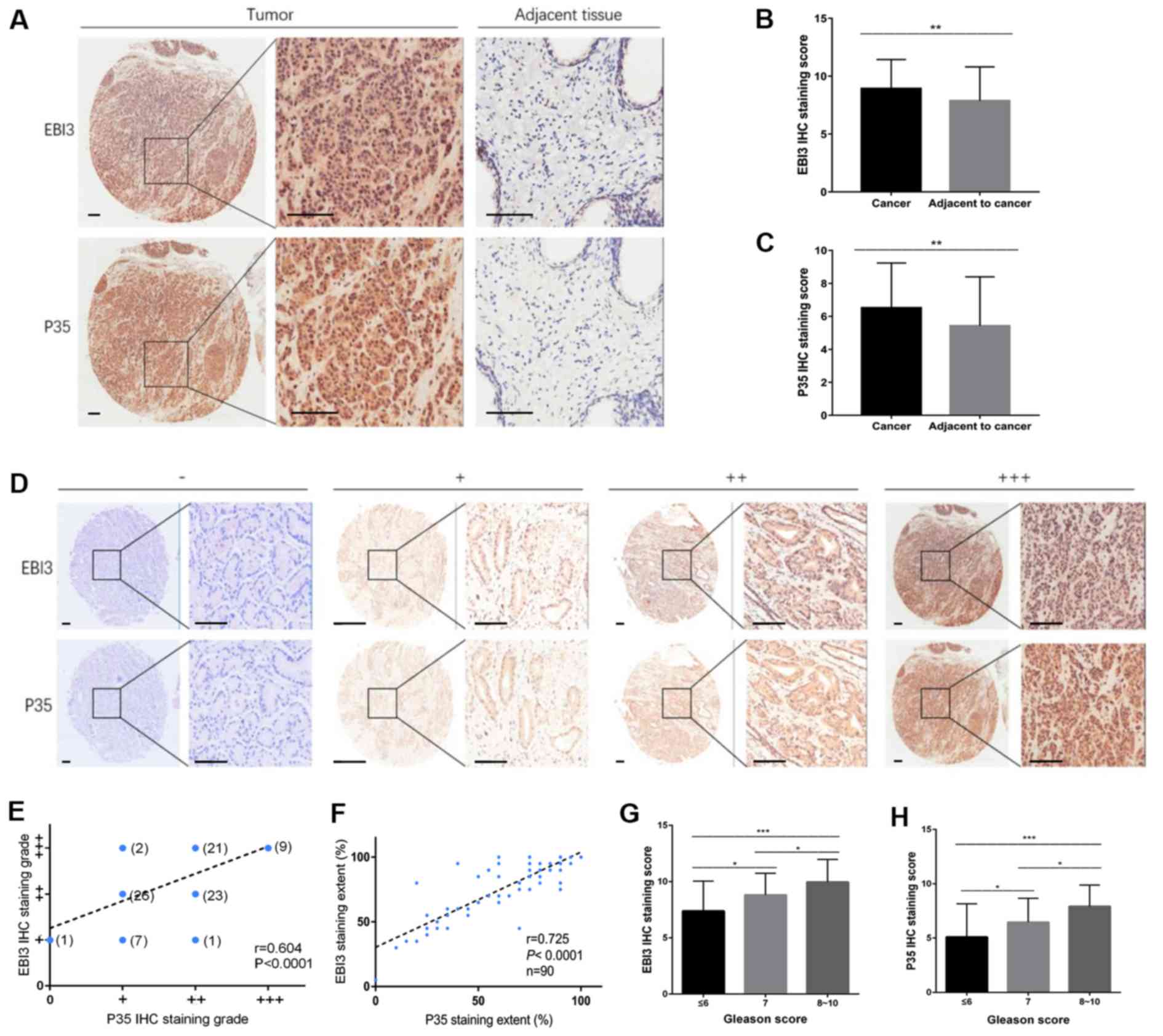
IL-35 expression levels in prostate
carcinoma tissues in patients with PCA
The protein expression levels of EBI3 and p35 were
used as a proxy for determining the protein expression level of
IL-35. A tissue microarray containing matched pairs of primary
prostate carcinoma tissue and adjacent tissues from 90 patients was
used for immunohistochemical analysis. A semi-quantitative method
was used to detect the expression of EBI3 and p35 by measuring the
density of positive staining. EBI3 and p35 expression was
significantly increased in tumor tissues compared with the adjacent
matching tissues, and positive staining was primarily localized to
the cytoplasm and the nucleus (Fig.
3A-C; P<0.01; Table III).
The extent of staining was divided into four grades: i) Negative,
-; ii) low staining, +; iii) medium staining, ++; and iv) high
staining, +++ (Fig. 3D). The final
staining grades of EBI3 and P35 were correlated (r=0.604;
P<0.0001; Fig. 3E), as was the
extent of staining of EBI3 and P35 (r=0.725; P<0.0001; Fig. 3F). Similarly, EBI3 and P35 staining
scores were associated with the Gleason score (P<0.001; Fig. 3G and H). As the Gleason score
increased, the EBI3 and P53 staining scores additionally increased.
The EBI3 staining scores of the PCA tissue with Gleason scores of 7
were significantly higher compared with those with a score of ≤6
(P=0.011). The EBI3 staining scores of the PCA tissue with Gleason
scores of 8–10 were significantly higher compared with those with a
score of 7 (P=0.049) and the EBI3 staining scores of the PCA tissue
with Gleason scores of 8–10 was significantly higher compared with
that in patients with a score of ≤6 (P<0.001). The p35 staining
scores of the PCA tissue with Gleason scores of 7 were
significantly higher compared with that of ≤6 (P=0.030). The p35
staining scores of the PCA tissue with Gleason scores of 8–10 were
significantly higher compared with those with a score of 7
(P=0.023), and the p35 staining scores of the PCA tissue with
Gleason scores of 8–10 was significantly higher compared with that
in patients with a score of ≤6 (P<0.001).
 | Table III.Expression of EBI3 and p35 in
patients with prostate cancer with different clinicopathological
characteristics. |
Table III.
Expression of EBI3 and p35 in
patients with prostate cancer with different clinicopathological
characteristics.
|
| EBI3
expression | p35 expression |
|---|
|
|
|
|
|---|
| Clinicopathological
characteristic | Mean ± standard
deviation | Mean ± standard
deviation | n | t/F-value | P-value | t/F-value | P-value |
|---|
| Position |
|
| 2.863 | 0.0052 |
| 2.850 | 0.0054a |
|
Cancer | 90 | 8.92±2.52 |
|
| 6.47±2.67 |
|
|
|
Adjacent to cancer | 90 | 7.87±2.94 |
|
| 5.42±2.98 |
|
|
| Age, years |
|
| 0.357 | 0.305 |
| 1.031 | 0.722 |
|
<65 | 21 | 9.10±2.36 |
|
| 7.57±3.14 |
|
|
|
≥65 | 69 | 8.87±2.58 |
|
| 6.09±2.96 |
|
|
| Gleason score |
|
| F=9.644 | 0.0002 |
| F=9.300 | 0.0002b |
| ≤6 | 29 | 7.38±2.67 |
|
| 5.24±3.27 |
|
|
| 7 | 34 | 8.82±1.91 |
|
| 6.47±2.21 |
|
|
|
8–10 | 27 | 9.96±2.01 |
|
| 7.93±1.96 |
|
|
Discussion
Cytokines serve an important role in promoting
malignant properties of cells, including tumor carcinogenesis,
angiogenesis and metastasis in the tumor microenvironment (20). In addition to stromal cells and
infiltrating immune cells, tumor cells produce and secrete various
types of cytokines, among which, tumor necrosis factor-α (21), transforming growth factor-β (22) and IL-6 (23) are well-studied. IL-35 is an important
mediator involved in regulating the function of T-cells, which
serve a potent immunosuppressive role, suppressing proliferation of
T-cells and inducing their transformation into suppressive
inducible regulatory T cells (Tregs) (24).
Based on the data in the present study, IL-35 may be
associated with the tumorigenesis and progression of PCA. IL-35
plasma concentration was significantly increased in patients with
PCA compared with patients with BPH or the healthy control group in
agreement with a recent study (25).
Plasma IL-35 expression levels in patients with PCA were
significantly increased in patients with higher Gleason scores.
Chatrabnous et al (26)
recently demonstrated that the genetic variations of a single
nucleotide polymorphism in the position of rs3761548, may have
affected the susceptibility to PCA and plasma IL-35 concentration,
although the study had a limitation of a small cohort. Furthermore,
plasma IL-35 concentrations were positively associated with disease
severity and clinical stage of tumors in patients with PCA, which
was additionally demonstrated in colorectal cancer (7), renal cell carcinoma (9) and nasopharyngeal carcinoma (27), suggesting that this cytokine may be
derived from tumors and may be regarded as a valuable biomarker for
evaluating tumor progression.
In the present study, IL-35 protein expression
levels in tumor tissues and matching adjacent non-tumor tissues of
patients with PCA were detected, and the association between IL-35
in PCA tissue and the Gleason score was analyzed. Co-expression of
the two subunits of IL-35 (EBI3 and p35) was used to determine the
IL-35 expression levels. EBI3 and p35 protein expression levels in
PCA tissues were highly correlated, thus, suggesting their
existence in PCA primarily as IL-35. The protein expression level
of IL-35 in the intra-tumoral zone was significantly increased
compared with the peritumoral zone. The Gleason score was
associated with the protein expression level of IL-35, and the
plasma IL-35 concentration in patients with Gleason scores of 8–10
were significantly increased compared with patients with a Gleason
scores of ≤6 and 7. Previous studies demonstrated that expression
of the p35 and EBI3 subunits was increased in a number of tumor
tissues, including PDAC (28) and
colorectal cancer (7). In addition,
elevated plasma IL-35 concentration and increased expression of
IL-35 in tumor tissues were associated with immunosuppression and
regarded as an unfavorable prognostic factor (28).
Furthermore, increased plasma IL-35 protein
expression levels may serve an important role in metastasis of PCA.
The IL-35 concentration in the plasma of patients with PCA with
lymph nodes metastasis was significantly increased compared with
patients with no evidence of lymph nodes metastasis. Similarly, in
patients with PCA with distant metastasis, IL-35 plasma expression
levels were significantly increased compared with patients with no
evidence of distant metastasis. IL-35 may promote the metastasis of
PCA, a role that was recently demonstrated in liver (16), breast (13) and pancreatic cancer (28). In addition, IL-35 may be a more
suitable biomarker compared with PSA in diagnosing PCA with lymph
nodes or distant metastasis.
Tumor growth and metastasis is a complicated process
involving multiple steps. At present, the mechanism of IL-35
promoting tumor development and metastasis has not yet been
determined. Huang et al (29)
suggested that tumor-derived IL-35 increases the microvessel
density in tumor tissues of PDAC. In a xenograft mouse model, IL-35
increased the recruitment of monocytes into PDAC tumors, which
required C-C motif chemokine ligand 5. Upon exposure to IL-35,
monocytes increased the expression of C-X-C motif chemokine ligand
(CXCL) 1 and CXCL8 genes whose products promoted angiogenesis
(29). Turnis et al (30) observed substantial enrichment of
IL-35+ Treg cells in tumors, and demonstrated
that treatment with an IL-35-specific antibody or restrictive
deletion of Treg cells limited the growth of tumors in
multiple murine models of human cancer.
Treg-cell-derived IL-35 promoted the expression of
multiple inhibitory receptors, including programmed cell death
protein 1, T-cell immunoglobulin mucin receptor 3 and lymphocyte
activation gene 3 protein, thereby facilitating the exhaustion of
intra-tumoral T-cells (30).
At present, the molecular mechanism of IL-35
promoting tumor development has not yet been determined. Previous
studies demonstrated the role of IL-35 in the transformation of
murine and human CD4+/CD25− T-cells into
IL-35-induced Treg cells (24,31).
Recently, Wang et al (32)
demonstrated that the number of IL-35-producing B-cells was
significantly increased in patients with advanced gastric cancer,
and that the frequency of IL-35-producing B-cells was associated
with the frequencies of Treg cells, myeloid derived
suppressor cells, IL-10-producing B-cells and CD14+
monocytes in the patients with gastric cancer.
Previous studies suggested that IL-35 recruited and
activated specific members of the signal transducer and activator
of transcription (STAT) family of transcription factors and
mediated their biological activities by binding to the IL-35
receptor (33,34). The IL-35 receptors in mice were
demonstrated to be comprised of IL-12Rβ2 and membrane glycoprotein
130 (gp130) subunits on T cells (35), or the IL-27Rα subunit on B-cells
(36). These differences may explain
the diversity of downstream responses of STAT activation observed
in T and B-cells in mice. Ma et al (37) demonstrated that STAT1 and STAT3 may
be activated by IL-35 in human CD4+ T-cells during
incubation and following temporary stimulation. However, STAT1 and
STAT3 were not activated by IL-35 in B-cells following temporary
stimulation, as IL-35R was not constitutively expressed in human
B-cells. Huang et al (29)
demonstrated that IL-35 activated transcription of genes whose
products promote angiogenesis by inducing gp130 signaling, through
IL12Rβ2, and phosphorylation of STAT1 and STAT4, in cells and mice
with xenograft tumors (29).
However, the present study has certain limitations.
Only a relatively small number of clinical samples were
retrospectively analyzed. A prospective analysis of a larger number
of samples is required to demonstrate the clinical significance of
IL-35 prior to examining the clinical significance. The majority of
the patients in the present study presented with high-stage PCA.
The majority of the patients with cancer in China, particularly in
rural areas, present with local invasion or metastasis when they
are diagnosed, which is different from European and American
countries. This may lead to a statistical bias. Since no
conformational antibodies specific to IL-35 are available at
present, the co-expression of EBI3 and p35 was detected for the IHC
staining. This method is inconvenient to use, and the result is
somewhat indirect. The functional role of increased protein
expression levels of IL-35 in patients with PCA in tumor
progression has not yet been determined, and requires further
investigation.
In summary, IL-35 expression was increased in the
plasma and tumors in patients with PCA. The plasma IL-35
concentration was associated with advanced stage PCA, suggesting
that IL-35 may promote the tumorigenesis and progression of PCA.
IL-35 may be an important biomarker for determining the presence
and progression of cancer in patients with PCA and may additionally
serve as a novel therapeutic target for PCA.
Acknowledgements
Not applicable.
Funding
The present study was funded by The National Natural
Science Foundation of China (grant nos. 81501568 and 81471761).
Availability of data and materials
The datasets used and analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ZG, JZ and XY conceived and designed the present
study. JZ, YW and HZ performed the experiments. JZ and XY wrote the
manuscript. ZG reviewed and edited the manuscript. All authors read
and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by The Medical Ethics
Committee of Tianjin Medical University Cancer Institute and
Hospital (Tianjin, China). All the procedures performed in the
present study involving human participants were in accordance with
the ethical standards of The Institutional and National Research
Committee and with The 1964 Helsinki Declaration and its later
amendments or comparable ethical standards. Informed consent was
obtained from all individual participants included in the present
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lilja H, Ulmert D and Vickers AJ:
Prostate-specific antigen and prostate cancer: Prediction,
detection and monitoring. Nat Rev Cancer. 8:268–278. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shariat SF, Semjonow A, Lilja H, Savage C,
Vickers AJ and Bjartell A: Tumor markers in prostate cancer I:
Blood-based markers. Acta Oncol. 50 (Suppl 1):S61–S75. 2011.
View Article : Google Scholar
|
|
4
|
Hwang JE, Joung JY, Shin SP, Choi MK, Kim
JE, Kim YH, Park WS, Lee SJ and Lee KH: Ad5/35E1aPSESE4: A novel
approach to marking circulating prostate tumor cells with a
replication competent adenovirus controlled by PSA/PSMA
transcription regulatory elements. Cancer Lett. 372:57–64. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cooperberg MR, Broering JM and Carroll PR:
Time trends and local variation in primary treatment of localized
prostate cancer. J Clin Oncol. 28:1117–1123. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Collison LW, Chaturvedi V, Henderson AL,
Giacomin PR, Guy C, Bankoti J, Finkelstein D, Forbes K, Workman CJ,
Brown SA, et al: IL-35-mediated induction of a potent regulatory T
cell population. Nat Immunol. 11:1093–1101. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zeng JC, Zhang Z, Li TY, Liang YF, Wang
HM, Bao JJ, Zhang JA, Wang WD, Xiang WY, Kong B, et al: Assessing
the role of IL-35 in colorectal cancer progression and prognosis.
Int J Clin Exp Pathol. 6:1806–1816. 2013.PubMed/NCBI
|
|
8
|
Jin P, Ren H, Sun W, Xin W, Zhang H and
Hao J: Circulating IL-35 in pancreatic ductal adenocarcinoma
patients. Hum Immunol. 75:29–33. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Jin L, Xu X, Ye B, Pan M, Shi Z and Hu Y:
Elevated serum interleukin-35 levels correlate with poor prognosis
in patients with clear cell renal cell carcinoma. Int J Clin Exp
Med. 8:18861–18866. 2015.PubMed/NCBI
|
|
10
|
Wu W, Jiang H, Li Yi and Yan MX: IL-35
expression is increased in laryngeal squamous cell carcinoma and in
the peripheral blood of patients. Oncol Lett. 13:3303–3308. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang Z, Liu JQ, Liu Z, Shen R, Zhang G, Xu
J, Basu S, Feng Y and Bai X: Tumor-derived IL-35 promotes tumor
growth by enhancing myeloid cell accumulation and angiogenesis. J
Immunol. 190:2415–2423. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nicholl MB, Ledgewood CL, Chen XH, Bai Q,
Qin CL, Cook KM, Herrick EJ, DiazArias A, Moore BJ and Fang YJ:
IL-35 promotes pancreas cancer growth through enhancement of
proliferation and inhibition of apoptosis: Evidence for a role as
an autocrine growth factor. Cytokine. 70:126–133. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhao Z, Chen X, Hao SN, Jia R, Wang N,
Chen S, Li M, Wang C and Mao H: Increased interleukin-35 expression
in tumor-infiltrating lymphocytes correlates with poor prognosis in
patients with breast cancer. Cytokine. 89:76–81. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tao Q, Pan Y, Wang Y, Wang H, Xiong S, Li
Q, Wang J, Tao L, Wang Z, Wu F, et al: Regulatory T cells derived
IL-35 promotes the growth of adult acute myeloid leukemia blasts.
Int J Cancer. 137:2384–2393. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gu X, Tian T, Zhang B, Liu Y, Yuan C, Shao
LJ, Guo Y and Fan K: Elevated plasma interleukin-35 levels predict
poor prognosis in patients with non-small cell lung cancer. Tumour
Biol. 36:2651–2656. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fu YP, Yi Y, Cai XY, Sun J, Ni XC, He HW,
Wang JX, Lu ZF, Huang JL, Cao Y, et al: Overexpression of
interleukin-35 associates with hepatocellular carcinoma
aggressiveness and recurrence after curative resection. Br J
Cancer. 114:767–776. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fan YG, Zhai JM, Wang W, Feng B, Yao GL,
An YH and Zeng Chao: IL-35 over-expression is associated with
genesis of gastric cancer. Asian Pac J Cancer Prev. 16:2845–2849.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Buyyounouski MK, Choyke PL, McKenney JK,
Sartor O, Sandler HM, Amin MB, Kattan MW and Lin DW: Prostate
cancer-major changes in the American Joint Committee on Cancer
eighth edition cancer staging manual. CA Cancer J Clin. 67:245–253.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Epstein JI, Egevad L, Amin MB, Delahunt B,
Srigley JR and Humphrey PA; Grading Committee, : The 2014
International Society of Urological Pathology (ISUP) Consensus
Conference on Gleason Grading of prostatic carcinoma: Definition of
grading patterns and proposal for a new grading system. Am J Surg
Pathol. 40:244–252. 2016.PubMed/NCBI
|
|
20
|
Whiteside TL: The tumor microenvironment
and its role in promoting tumor growth. Oncogene. 27:5904–5912.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Salomon BL, Leclerc M, Tosello J, Ronin E,
Piaggio E and Cohen JL: Tumor necrosis factor α and regulatory T
cells in oncoimmunology. Front Immunol. 9:4442018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Vivekanandhan S and Mukhopadhyay D:
Genetic status of KRAS influences transforming growth factor-beta
(TGF-β) signaling: An insight into Neuropilin-1 (NRP1) mediated
tumorigenesis. Semin Cancer Biol. 54:72–79. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Huang S, Liu Q, Liao Q, Wu Q, Sun B, Yang
Z, Hu X, Tan M and Li L: Interleukin-6/signal transducer and
activator of transcription 3 promotes prostate cancer resistance to
androgen deprivation therapy via regulating pituitary tumor
transforming gene 1 expression. Cancer Sci. 109:678–687. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Seyerl M, Kirchberger S, Majdic O, Seipelt
J, Jindra C, Schrauf C and Stöckl J: Human rhinoviruses induce
IL-35-producing Treg via induction of B7-H1 (CD274) and sialo
adhesin (CD169) on DC. Eur J Immunol. 40:321–329. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zhou C, Zhang J, Chen Y, Wang H and Hou J:
Interleukin-35 as a predictor of prostate cancer in patients
undergoing initial prostate biopsy. Onco Targets Ther.
10:3485–3491. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chatrabnous N, Ghaderi A, Ariafar A,
Razeghinia M S, Nemati M and Jafarzadeh A: Serum concentration of
interleukin-35 and its association with tumor stages and FOXP3 gene
polymorphism in patients with prostate cancer. Cytokine.
113:221–227. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang Y, Sun H, Wu H, Tan QD and Xiang K:
Interleukin 35 is an independent prognostic factor and a
therapeutic target for nasopharyngeal carcinoma. Contemp Oncol
(Pozn). 2:120–124. 2015.
|
|
28
|
Huang C, Li N, Li Z, Chang A, Chen Y, Zhao
T, Li Y, Wang X, Zhang W, Wang Z, et al: Tumour-derived Interleukin
35 promotes pancreatic ductal adenocarcinoma cell extravasation and
metastasis by inducing ICAM1 expression. Nat Commun. 8:140352017.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Huang C, Li Z, Li N, Li Y, Chang A, Zhao
T, Wang X, Wang H, Gao S, Yang S, et al: Interleukin 35 expression
correlates with microvessel density in pancreatic ductal
adenocarcinoma, recruits monocytes, and promotes growth and
angiogenesis of Xenograft tumors in mice. Gastroenterology.
154:675–688. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Turnis ME, Sawant DV, Szymczak-Workman AL,
Andrews LP, Delgoffe GM, Yano H, Beres AJ, Vogel P, Workman CJ and
Vignali DA: Interleukin-35 limits anti-tumor immunity. Immunity.
44:316–329. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Wang K, Liu J and Li J: IL-35-producing B
cells in gastric cancer patients. Medicine (Baltimore).
97:e07102018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Trinchieri G, Pflanz S and Kastelein RA:
The IL-12 family of heterodimeric cytokines: New players in the
regulation of T cell responses. Immunity. 19:641–644. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Sun L, He C, Nair L, Yeung J and Egwuagu
CE: Interleukin 12 (IL-12) family cytokines: Role in immune
pathogenesis and treatment of CNS autoimmune disease. Cytokine.
75:249–255. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Collison LW, Delgoffe GM, Guy CS, Vignali
KM, Chaturvedi V, Fairweather D, Satoskar AR, Garcia KC, Hunter CA,
Drake CG, et al: The composition and signaling of the IL-35
receptor are unconventional. Nat Immunol. 13:290–299. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang RX, Yu CR, Dambuza IM, Mahdi RM,
Dolinska MB, Sergeev YV, Wingfeld PT, Kim SH and Egwuagu CE:
Interleukin-35 induces regulatory B cells that suppress autoimmune
disease. Nat Med. 20:633–641. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ma YH, Chen L, Xie G, Zhou Y, Yue C, Yuan
X, Zheng Y, Wang W, Deng L and Shen L: Elevated level of
Interleukin-35 in colorectal cancer induces conversion of T cells
into iTr35 by activating STAT1/STAT3. Oncotarget. 7:73003–73015.
2016. View Article : Google Scholar : PubMed/NCBI
|