Introduction
Gastric cancer, which greatly endangers human
health, is a disease with high mortality and poor prognosis
(1,2). Studies have suggested that the
morbidity and mortality of gastric cancer will continue to increase
in the coming 2–3 decades in China, making it the number one killer
threatening the health of the Chinese (3,4). Due to
environmental pollution, food safety issues, unhealthy lifestyle
and other reasons, the incidence of gastric cancer shows a trend of
rejuvenation and normality. Most gastric cancer patients receive
preoperative chemotherapy, but chemotherapy drugs damage their
liver, heart and kidney (5,6). Therefore, gastric cancer patients
suffer from large trauma, severe pain and a series of severe stress
responses during surgical treatment, as well as more complications
after operation (7). The induction
period of anesthesia is the most easily fluctuating period of
respiration and circulation during the whole anesthesia period, so
it is beneficial to the recovery of patients to choose the
appropriate anesthetic drugs, helping them pass the anesthesia
period (8–10). Remifentanil, propofol and sevoflurane
are new short-acting anesthetics characterized by rapid action and
rapid recovery after anesthesia, suitable for surgical anesthesia
in cancer patients (11).
Sevoflurane is an inhaled anesthetic with muscle relaxant effect,
so it can reduce the dosage of muscle relaxant in operation;
propofol has a short-time effect on anesthesia, and patients
recover quickly after operation (12). Remifentanil is an opioid receptor
agonist with rapid onset and short duration of maintenance
(13). Study of Recart et al
(14) shows that the combined use of
inhaled anesthetics and opiates can reduce the dosage of
anesthetics, help to stabilize the vital signs of patients
undergoing surgery and reduce the incidence of postoperative
adverse reactions. In this study, a retrospective cohort study was
performed to analyze patients undergoing radical gastrectomy who
had received previous surgical treatment, and to observe the
anesthetic effect of propofol combined with remifentanil and
propofol combined with sevoflurane in cancer patients in order to
provide a basis for the selection of clinical anesthetic methods
for cancer patients.
Patients and methods
Study subjects
A retrospective cohort study was performed to
analyze the clinical data of 516 patients undergoing radical
gastrectomy in the First Bethune Hospital of Jilin University
(Changchun, China) between January 2011 and December 2017. Of the
patients 203 with propofol combined with remifentanil anesthesia
were group A, and 313 patients with propofol combined with
sevoflurane anesthesia were group B according to the anesthetic
methods accepted by patients.
The study was approved by the Ethics Committee of
the First Bethune Hospital of Jilin University (no. Jlsyd2011011).
Signed informed consents were obtained from the patients or the
guardians.
Inclusion criteria were: Patients whose ASA was
grade I or grade II, with no obvious abnormality in the function of
heart, lung, liver and kidney as well as respiratory system, no
history of taking opioids and drug abuse, no allergy history, no
contraindications for the use of anesthetics such as propofol and
sevoflurane, no history of long-term use of analgesic and sedative
were included. Under the guidelines for radical gastrectomy
(15), surgical procedures of all
patients were standardized. Exclusion criteria were: Patients with
perioperative large blood transfusion or hemorrhage, patients with
a history of endocrine and immune diseases, patients who received
hormone therapy, radiotherapy and chemotherapy before operation and
patients with cognitive dysfunction and mental illness.
Anesthetic methods
The venous access was opened after the patient
entered the operating room, and the vital signs, such as blood
pressure, heart rate, respiration and oxygen saturation were
closely monitored. Patients in the two groups were given general
anesthesia with tracheal intubation. The induction scheme was as
follows: midazolam 0.05 mg/kg and fentanyl 3.0 µg/kg. During
induction, the tidal volume was controlled at 8–10 ml/kg, the end
expiratory CO2 pressure was 30–40 mmHg, the ventilation
frequency was 12 min, and the breathing ratio was 1:2. When
bispectral index (BIS) was <60, 0.10 mg/kg of vecuronium bromide
was injected. Patients in group A were assisted to breathe after
falling asleep, and trace intravenous infusion of propofol 7.5
mg/kg/h and remifentanil 0.08 µg/kg/min were used to maintain
anesthesia. Drugs were withdrawn 5 min before the end of the
operation. Patients in group B were assisted to breathe after
falling asleep, and trace intravenous infusion of propofol 7.5
mg/kg/h and 2% of sevoflurane were used to maintain anesthesia.
During the operation, the doses of propofol and remifentanil were
adjusted according to patients' BIS and hemodynamic parameters.
Patient's BIS ranged from 40 to 55, and the blood pressure
fluctuated within 20% of the baseline value.
Observation indicators
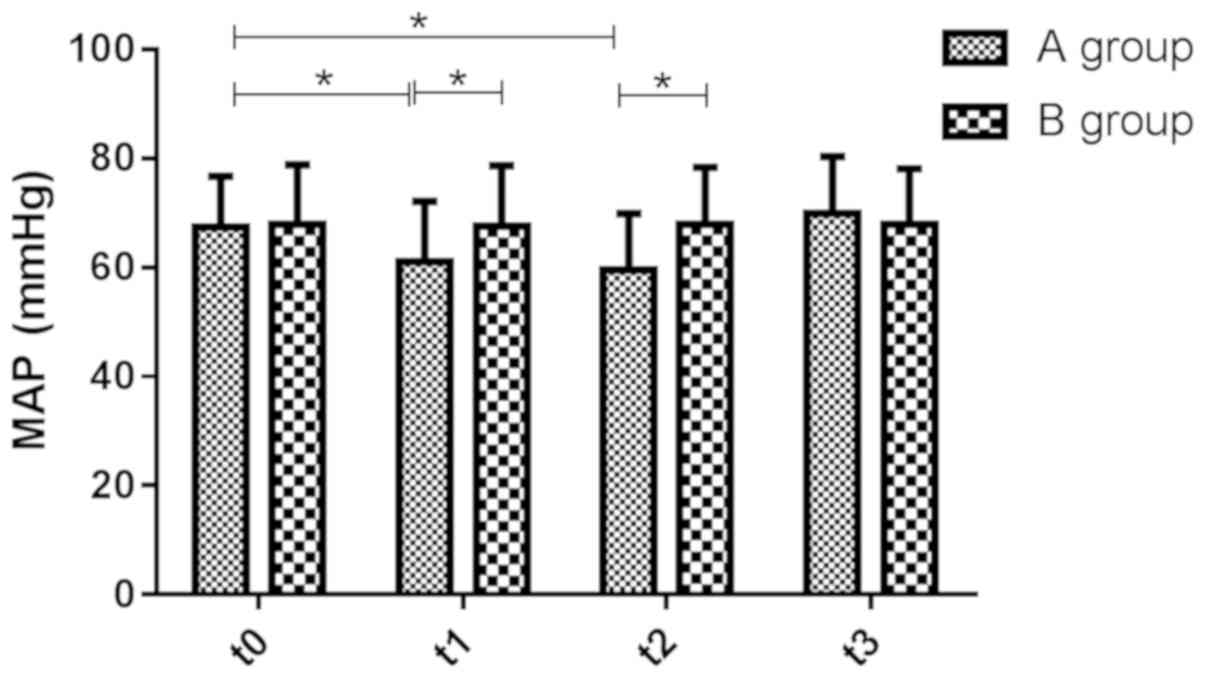
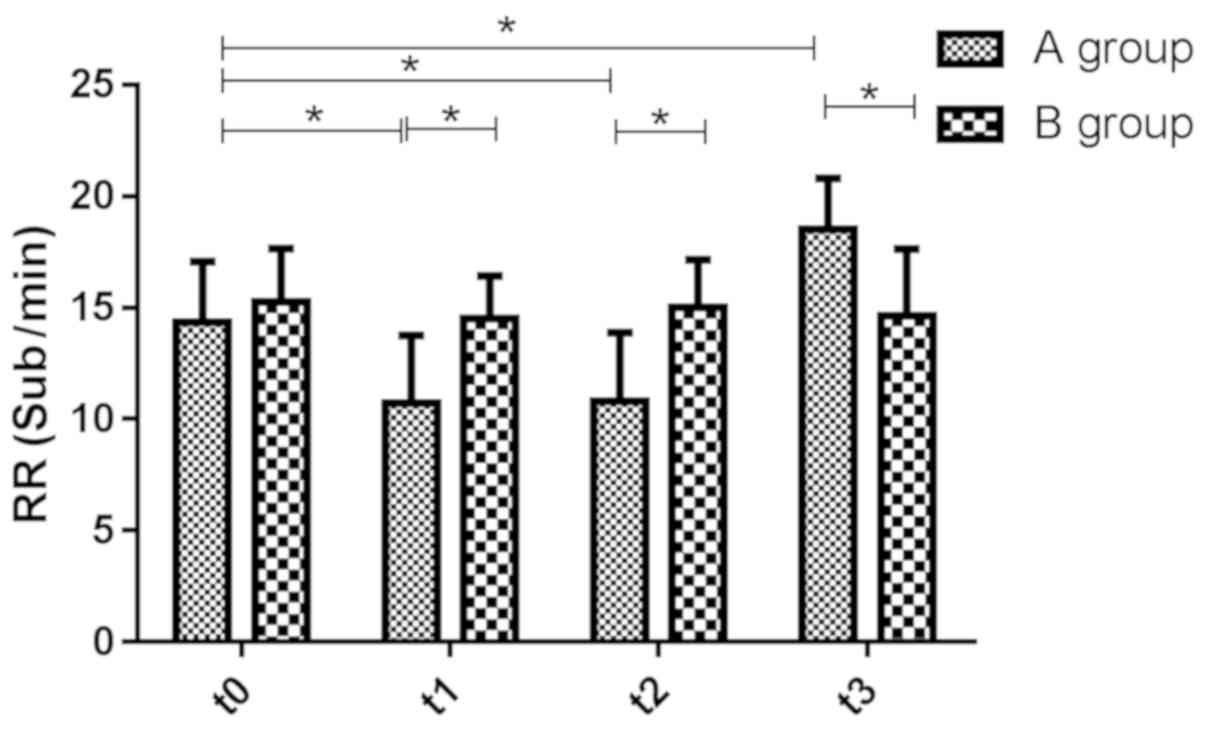
The mean arterial pressure (MAP), heart rate (HR)
and respiratory rate (RR) of patients in the two groups were
observed at the time of entering the operating room (t0), the
beginning of the operation (t1), 10 min after the beginning of the
operation (t2) and 10 min after the operation (t3). The onset time
of anesthesia, the total time of operation, the time of waking up
after operation and the time of leaving the operating room in the
two groups of patients were recorded.
Sedation and amnesia in patients 15 min after
operation were judged according to the standard (16). Ramsay sedation scale was used to
judge sedation effect. Patient is anxious and restless, 1 point;
patient coordinate, has orientation and is quiet, 2 points; patient
responds to instructions, 3 points; patient responds quickly to a
tap on the glabella or loud auditory stimuli, with sleepiness, 4
points; patient responds slowly to a tap on the glabella or loud
auditory stimuli, with sleepiness, 5 points; patient shows no
response, with sleepiness, 6 points. One point indicates
insufficient sedation; 2–4 points indicate appropriate sedation;
5–6 points indicate excessive sedation. Amnesia criteria: No
amnesia, can recall the surgical process when awake; incomplete
amnesia, can recall some with hints; complete amnesia, cannot
recall. The occurrence of adverse reactions within 24 h after
operation was recorded.
Statistical analysis
In this study, SPSS 19.00 (SPSS, Inc., Chicago, IL,
USA) software was used to perform statistical analysis on the data,
and Graph Pad 7 was used to draw illustrations. The count data were
presented as (%), and were analyzed using Chi-square test
(χ2). The grade data were presented as (%), and were
analyzed using the rank sum test (Z). The K-S test was used to
analyze the measurement data. Data conforming to the normal
distribution were tested by t-test, and were expressed as mean ±
standard deviation (mean ± SD). The independent sample t-test was
performed in the comparison between groups, while the paired t-test
was performed in the comparison within the group. The data that did
not conform to the normal distribution were expressed by quartiles
indicating P50 (P25-P75), and were analyzed using nonparametric
test (U). Repeated measures ANOVA was performed to analyze changes
in MAP, HR and RR during treatment. Bonferroni test was the post
hoc test. Statistically significant difference was set at
P<0.05.
Results
Basic patient data
There were 203 patients in group A, including 114
(56.16%) males with an average age of 63.41±4.52 years and an
average course of disease of 6.24±1.68 months; 313 patients in
group B, including 150 47.92% males with an average age of
65.39±3.61 years and an average course of disease of 6.48±1.51
months. The difference has no statistical significance between the
two groups in sex, age and course of disease (P>0.05) (Table I).
 | Table I.Comparison of basic data between two
groups of patients. |
Table I.
Comparison of basic data between two
groups of patients.
| Groups | Sex male, n (%) | Age (years) | Course of disease
(months) |
|---|
| A, n=203 | 114 (56.16) | 63.41±4.52 | 6.24±1.68 |
| B, n=313 | 150 (47.92) | 65.39±3.61 | 6.48±1.51 |
| t/χ2
value | 3.341 | 3.167 | 2.171 |
| P-value | 0.068 | 0.114 | 0.254 |
Changes of respiration and circulation
during perioperative period
The values of MAP (61.5 and 60.10 mmHg), HR (65.3
and 66.1 times/min) and RR (11.20 and 10.50 times/min) at t1 and t2
were lower than those at t0 (67.8, 77.2 and 14.6 times/min)
(P<0.05), and the value of RR (18.7 times/min) at t3 was higher
than that at t0 (P<0.05) in group A; the values of MAP (68.6,
67.8 and 67.9 mmHg), HR (76.8, 76.2 and 78.10 times/min) and RR
(14.6, 15.1 and 14.8 times/min) at t1, t2 and t3 were not different
from that at t0 (68.1 mmHg, 77.3 and 15.3 times/min) (P>0.05) in
group B. The values of MAP, HR and RR at t1 and t2 in group B were
higher than those in group A (P<0.05), and the value of RR at t3
was lower than that in group A (P>0.05) (Figs. 1–3).
Comparison of onset time of
anesthesia, total time of operation, time of waking up after
operation, and time of leaving the operating room between the two
groups
The onset time of anesthesia and the time of waking
up after operation in group B were shorter than those in group A,
and the difference has statistical significance (P<0.001,
P=0.011); the difference has no statistical significance (P=0.251,
P=0.611) between group A and group B in the total time of operation
and the time of leaving the operating room. Specific information is
shown in Table II.
 | Table II.Comparison of onset time of
anesthesia, total time of operation, time of waking up after
operation, and time of leaving the operating room between two
groups of patients (mean ± SD). |
Table II.
Comparison of onset time of
anesthesia, total time of operation, time of waking up after
operation, and time of leaving the operating room between two
groups of patients (mean ± SD).
| Groups | Onset time of
anesthesia (sec) | Total time of
operation (min) | Time of waking up
after operation (min) | Time of leaving the
operating room (min) |
|---|
| A, n=203 | 55.10±11.85 | 225.53±7.58 | 6.20±2.12 | 9.52±3.95 |
| B, n=313 | 35.20±8.26 | 224.71±7.01 | 4.06±1.84 | 9.31±4.32 |
| t value | 10.805 | 0.97 | 4.682 | 0.985 |
| P-value | <0.001 | 0.33 | 0.011 | 0.611 |
Sedation score and amnesia after
operation
The sedation score of patients in group A was lower
than that in group B, and the difference has statistical
significance (P<0.05); there was no statistical significance
difference between the two groups in amnesia (P>0.05) (Table III).
 | Table III.Comparison of sedation score, amnesia
and satisfaction of anesthesia after operation between the two
groups. |
Table III.
Comparison of sedation score, amnesia
and satisfaction of anesthesia after operation between the two
groups.
| Variables195/203 | Group A (n=203) | Group B (n=313) | t/Z value | P-value |
|---|
| Sedation score
(point) | 4.12±0.11 | 4.95±0.09 | 8.651 | <0.001 |
| Amnesia [n (%)] |
|
| −1.456 | 0.145 |
| Complete
amnesia | 195 (96.06) | 291 (92.98) |
|
|
|
Incomplete amnesia | 4 (1.97) | 12 (3.83) |
|
|
| No
amnesia | 4 (1.97) | 10 (3.19) |
|
|
| Satisfaction of
anesthesia |
|
| −5.076 | <0.001 |
| Very
satisfied | 142 (69.95) | 275 (87.86) |
|
|
|
Satisfied | 50 | 33 |
|
|
|
Neutral | 11 | 5 |
|
|
Occurrence of adverse reactions within
2 h after operation
There were 32 (15.76%) cases of dizziness, 6 (2.96%)
cases of nausea and 56 (27.59%) cases of pain after operation in
group A; In group B, 40 (12.78%) cases of dizziness, 9 (2.90%)
cases of nausea and 30 (9.58%) cases of pain. The difference has
statistical significance between the two groups in the occurrence
of pain (P<0.001), but it was not statistically significant in
the occurrence of dizziness and nausea (P>0.05) (Table IV).
 | Table IV.Comparison of the occurrence of
adverse reactions within 2 h after operation in two groups of
patients [n (%)]. |
Table IV.
Comparison of the occurrence of
adverse reactions within 2 h after operation in two groups of
patients [n (%)].
| Groups | Dizziness | Nausea | Pain |
|---|
| A, n=203 | 32 (15.76) | 6 (2.96) | 56 (27.59) |
| B, n=313 | 40 (12.78) | 9 (2.90) | 30 (9.58) |
| t/χ2
value | 0.913 | 0.003 | 28.73 |
| P-value | 0.339 | 0.958 | <0.001 |
Discussion
It has been pointed out by the World Health
Organization (WHO) that the global gastric cancer cases are
increasing year by year, by ~14 million new cases each year, and
the number of gastric cancer in China ranks first in the world
(17,18). Therefore, gastric cancer, which poses
a serious threat to human health and social and economic
development, is the major public health problem in China and the
world (19,20). Because multiple tissues and organs
are involved in radical gastrectomy, severe stress response will
occur to cancer patients during operation, bringing some
difficulties to anesthesia and postoperative management (21). At present, propofol combined with
opiates or propofol combined with inhaled anesthetics are commonly
used in patients undergoing radical gastrectomy. Propofol
anesthesia has a rapid effect but no analgesic effect, so it needs
to be used in combination with other analgesic drugs (5,22).
Remifentanil is a short-acting opioid analgesic with rapid onset of
anesthesia, good analgesic effect but short duration of action
(13). Sevoflurane is a new type of
inhaled anesthetic with the advantages of less stimulation, stable
hemodynamics during operation and easy control of anesthetic depth
(12). A study has shown that
patients with propofol combined with opiates have less
postoperative complications and faster spontaneous respiratory
recovery (23).
In this study, a retrospective cohort study was
performed to observe the anesthetic effect of propofol combined
with remifentanil and propofol combined with sevoflurane in cancer
patients. Scientific, standardized and strict internal quality
control was carried out in the process of data processing and
analysis, so the results have high accuracy and reliability. The
results showed that the difference was smaller in the values of
MAP, HR and RR at the four time points in group B; the values of
MAP and HR decreased at t1 and t2, and the value of RR decreased at
t1 and t2, but increased at t3 in group A when compared to t0; the
values of MAP, HR and RR at t1 and t2 in group B were higher than
those in group A, and the value of RR at t3 was lower than that in
group A; it indicated that propofol combined with sevoflurane
anesthesia had little effect on the respiration and circulation of
patients. The mechanism of propofol and remifentanil was related to
the stimulation of vagus nerve and the inhibition of sinus node
function, so the monitoring of heart rate should be strengthened
during anesthesia (20,24). Sevoflurane could cause peripheral
vasodilation and myocardial inhibition in patients and was suitable
for general anesthesia, because the time of waking up after
operation in patients was short and the respiratory tract secretion
was not increased (25).
It was found that patients' sedation score in group
A was lower than that in group B, and the incidence of pain in
group A was higher than that in group B, indicating that patients
had a high acceptance of propofol combined with sevoflurane
anesthesia and a low incidence of adverse reactions. Cancer
patients were prone to restlessness and other adverse reactions in
general anesthesia due to pain, so sedation and analgesia effect
were the main indicators to evaluate the anesthetic effect
(21,26). In addition to produce general
anesthesia, sevoflurane also had vasodilator and analgesic effects,
so it is more suitable for elderly patients and patients with
cardiovascular insufficiency (27).
In conclusion, a retrospective cohort study was
performed to analyze patients undergoing radical gastrectomy who
had been anesthetized by propofol combined with sevoflurane and
propofol combined with remifentanil. The results showed that
patients undergoing radical gastrectomy with the combination of
sevoflurane and propofol had stable respiration and circulation
during anesthesia, quick recovery of early consciousness and low
incidence of adverse reactions, having good sedation effects.
Therefore, the combination of sevoflurane and propofol could be
promoted in the clinical anesthesia of cancer patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
YF wrote the manuscript. YF and JL drafted the
manuscript and were mainly devoted to collecting and interpreting
the general data. HW and ZD recorded and analyzed the observation
indicators. All the authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the First Bethune Hospital of Jilin University (Changchun, China).
Signed informed consents were obtained from the patients or the
guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Lan L, Zhao F, Cai Y, Wu RX and Meng Q:
Epidemiological analysis on mortality of cancer in China, 2015.
Zhonghua Liu Xing Bing Xue Za Zhi. 39:32–34. 2018.(In Chinese).
PubMed/NCBI
|
|
2
|
He J: Strengthen the cancer surveillance
to promote cancer prevention and control in China. Zhonghua Zhong
Liu Za Zhi. 40:1–4. 2018.(In Chinese). PubMed/NCBI
|
|
3
|
Hayashi K, Murata K, Naito A, Kagawa Y,
Kawai K, Mori R, Nose Y, Akiyama Y, Sakamoto T, Murakami K, et al:
A case of resection of obstructive colon cancer associated with
aspiration pneumonia, under combined epidural-spinal anesthesia.
Gan To Kagaku Ryoho. 44:1970–1972. 2017.(In Japanese). PubMed/NCBI
|
|
4
|
Kim MH, Kim DW, Kim JH, Lee KY, Park S and
Yoo YC: Does the type of anesthesia really affect the
recurrence-free survival after breast cancer surgery? Oncotarget.
8:90477–90487. 2017.PubMed/NCBI
|
|
5
|
Lee KH, Rim SK, Lee JY, Lee SY, Lee SN,
Lee EJ and Lee JH: Effects of pretreatment with intravenous
palonosetron for propofol-remifentanil-based anesthesia in breast
and thyroid cancer surgery: A double-blind, randomized, controlled
study. Korean J Anesthesiol. 67:13–19. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hao Z, Yali H, Xiangjun L, Fusheng D and
Ruihua L: Comparison between propofol and propofol-remifentanil
sedation under target-controlled infusion for impacted
supernumerary teeth extraction surgery for children. Hua Xi Kou
Qiang Yi Xue Za Zhi. 35:408–412. 2017.(In Chinese). PubMed/NCBI
|
|
7
|
Peng K, Liu HY, Wu SR, Liu H, Zhang ZC and
Ji FH: Does propofol anesthesia lead to less postoperative pain
compared with inhalational anesthesia?: A systematic review and
meta-analysis. Anesth Analg. 123:846–858. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu S, Gu X, Zhu L, Wu G, Zhou H, Song Y
and Wu C: Effects of propofol and sevoflurane on perioperative
immune response in patients undergoing laparoscopic radical
hysterectomy for cervical cancer. Medicine (Baltimore).
95:e54792016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen Y, Liang M, Zhu Y and Zhou D: The
effect of propofol and sevoflurane on the perioperative immunity in
patients under laparoscopic radical resection of colorectal cancer.
Zhonghua Yi Xue Za Zhi. 95:3440–3444. 2015.(In Chinese). PubMed/NCBI
|
|
10
|
Hassan WM, Nasir YM, Zaini RH and Shukeri
WF: Target-controlled infusion propofol versus sevoflurane
anaesthesia for emergency traumatic brain surgery: Comparison of
the outcomes. Malays J Med Sci. 24:73–82. 2017.PubMed/NCBI
|
|
11
|
Zhang GH and Wang W: Effects of
sevoflurane and propofol on the development of pneumonia after
esophagectomy: A retrospective cohort study. BMC Anesthesiol.
17:1642017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Wang C, Ni C, Li G, Li Y, Tao L, Li N,
Wang J and Guo X: Effects of sevoflurane versus propofol on
cerebrovascular reactivity to carbon dioxide during laparoscopic
surgery. Ther Clin Risk Manag. 13:1349–1355. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kratzer S, Mattusch C, Garcia PS, Schmid
S, Kochs E, Rammes G, Schneider G, Kreuzer M and Haseneder R:
Propofol and sevoflurane differentially modulate cortical
depolarization following electric stimulation of the ventrobasal
thalamus. Front Comput Neurosci. 11:1092017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Recart A, Gasanova I, White PF, Thomas T,
Ogunnaike B, Hamza M and Wang A: The effect of cerebral monitoring
on recovery after general anesthesia: A comparison of the auditory
evoked potential and bispectral index devices with standard
clinical practice. Anesth Analg. 97:1667–1674. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kong J, Wu SD and Su Y: Translumenal
single-incision laparoscopy radical gastrectomy with D2 lymph node
dissection for early gastric cancer - primary experience with less
invasive surgery in China. J Laparoendosc Adv Surg Tech A.
23:141–145. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Andra E and Julie K: Bispectral index
monitoring during sedation with sevoflurane, mmifazolam, and
propofol. Anesthesiology. 95:112006.
|
|
17
|
Moradkhani MR and Karimi A: Role of drug
anesthesia and cancer. Drug Res (Stuttg). 68:125–131. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cho JS, Lee MH, Kim SI, Park S, Park HS,
Oh E, Lee JH and Koo BN: The effects of perioperative anesthesia
and analgesia on immune function in patients undergoing breast
cancer resection: A prospective randomized study. Int J Med Sci.
14:970–976. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sekandarzad MW, van Zundert AA, Doornebal
CW and Hollmann MW: Regional anesthesia and analgesia in cancer
care: Is it time to break the bad news? Curr Opin Anaesthesiol.
30:606–612. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Barela CA: The effect of anesthesia on
cancer metastasis. Gastroenterol Nurs. 40:75–76. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Han Y, Han L, Dong M, Sun Q, Ding K, Zhang
Z, Cao J and Zhang Y: Comparison of a loading dose of
dexmedetomidine combined with propofol or sevoflurane for
hemodynamic changes during anesthesia maintenance: A prospective,
randomized, double-blind, controlled clinical trial. BMC
Anesthesiol. 18:122018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhang L, Chen C, Wang L, Cheng G, Wu WW
and Li YH: Awakening from anesthesia using propofol or sevoflurane
with epidural block in radical surgery for senile gastric cancer.
Int J Clin Exp Med. 8:19412–19417. 2015.PubMed/NCBI
|
|
23
|
Annigeri RV and Patil RS: A retrospective
analysis on anesthetic management during rigid bronchoscopy in
children with foreign body aspiration: Propofol and sevoflurane
with controlled ventilation. Anesth Essays Res. 11:871–874. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tian HT, Duan XH, Yang YF, Wang Y, Bai QL
and Zhang X: Effects of propofol or sevoflurane anesthesia on the
perioperative inflammatory response, pulmonary function and
cognitive function in patients receiving lung cancer resection. Eur
Rev Med Pharmacol Sci. 21:5515–5522. 2017.PubMed/NCBI
|
|
25
|
De Oliveira GS Jr, Bialek J, Rodes ME,
Kendall MC and McCarthy RJ: The effect of sevoflurane compared to
propofol maintenance on post-surgical quality of recovery in
patients undergoing an ambulatory gynecological surgery: A
prospective, randomized, double-blinded, controlled, clinical
trial. J Clin Anesth. 43:70–74. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tang L, Liu H, Wu Y, Li M, Li W, Jiang M,
Hou J, Jiang Y, Xia Z and Meng Q: Sevoflurane may be more
beneficial than propofol in patients receiving endoscopic variceal
ligation and endoscopic variceal sclerotherapy: A randomized,
double-blind study. Exp Ther Med. 14:3145–3152. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Robba C, Qeva E, Borsellino B, Aloisio S,
Tosti G and Bilotta F: Effects of propofol or sevoflurane
anesthesia induction on hemodynamics in patients undergoing
fiberoptic intubation for cervical spine surgery: A randomized,
controlled, clinical trial. J Anaesthesiol Clin Pharmacol.
33:215–220. 2017.PubMed/NCBI
|