Introduction
Keratocystic odontogenic tumor (KOT), which has
recently been renamed as odontogenic keratocyst (OKC), is one of
the most controversial pathologic entities in maxillofacial
pathology (1–3). OKC is characterized by a thin and
regular lining of parakeratinized stratified squamous epithelium
with palisading hyperchromatic basal cells (1). The unique features of OKCs comprise a
locally aggressive behavior with a high recurrence rate and a
tendency to multiply (4,5). Recurrence occurs following inadequate
treatment methods, incomplete removal of the cyst or epithelial
islands appearing after enucleation, a high mitotic index of the
epithelial cells, large size of the cyst and a lesion location
associated with difficult surgical access (4,6,7).
The treatment method for OKCs remains controversial.
To the best of our knowledge, there is no evidence in the
literature that would guide surgeons in selecting the best
treatment options. Clinicians continue to rely on their own
experience when deciding for the most appropriate treatment.
Surgical approaches vary between conservative to more aggressive
treatments (8,9). Enucleation is the most commonly used
treatment method (6) and is
associated with a high recurrence rate (10,11).
Decompression and marsupialization has been used as a conservative
treatment of OKCs (12). Some
clinicians do not approve these techniques because the potential
remnant cystic tissues left behind can facilitate the recurrence
(13). A more aggressive approach
may therefore lower the risk of recurrence (14). It has been suggested that aggressive
resection should be limited to OKCs that have recurred more than
twice or to those that have undergone malignant transformation
(4,15). In addition, Worrall (16) recommended radical excision as the
treatment of choice for OKCs that had cortically perforated,
whereas Gosau et al (17)
reported that enucleation plus curettage with carnoy's solution
results in a recurrence rate statistically comparable to that of
resection excision. Jackson et al (18) highlighted that complete excision
should be performed for OKCs associated with any sign of soft
tissue involvement. There is therefore high variability in the
decision-making process for the resection of OKCs. Although radical
resection offers the highest cure rate, it produces significant
morbidity, including the loss of jaw continuity or facial
disfigurement. Evaluation of patients following such aggressive
treatment is therefore necessary. The present study reported the
clinical outcomes of 35 patients who were treated with radical
resection followed by immediate defect reconstruction.
Materials and methods
Patients
A retrospective review of well-documented cases of
OKCs that were treated between April 2003 and May 2015 at the
Department of Oral and Maxillofacial Surgery of the School and
Hospital of Stomatology, Wuhan University was conducted. The
involvement sites of the lesions were divided into the mandibular
anterior-premolar and the mandibular molar-ramus regions. Data were
obtained from the pathological department and comprised the
orthopantomogram radiographs or CT scans performed prior to and
following the treatment, and medical record notes. Patients were
excluded if the data records were incomplete, if the follow-up
period was ≤12 months or if they had multiple cysts that were
associated with nevoid basal cell nevus syndrome.
Treatment procedures
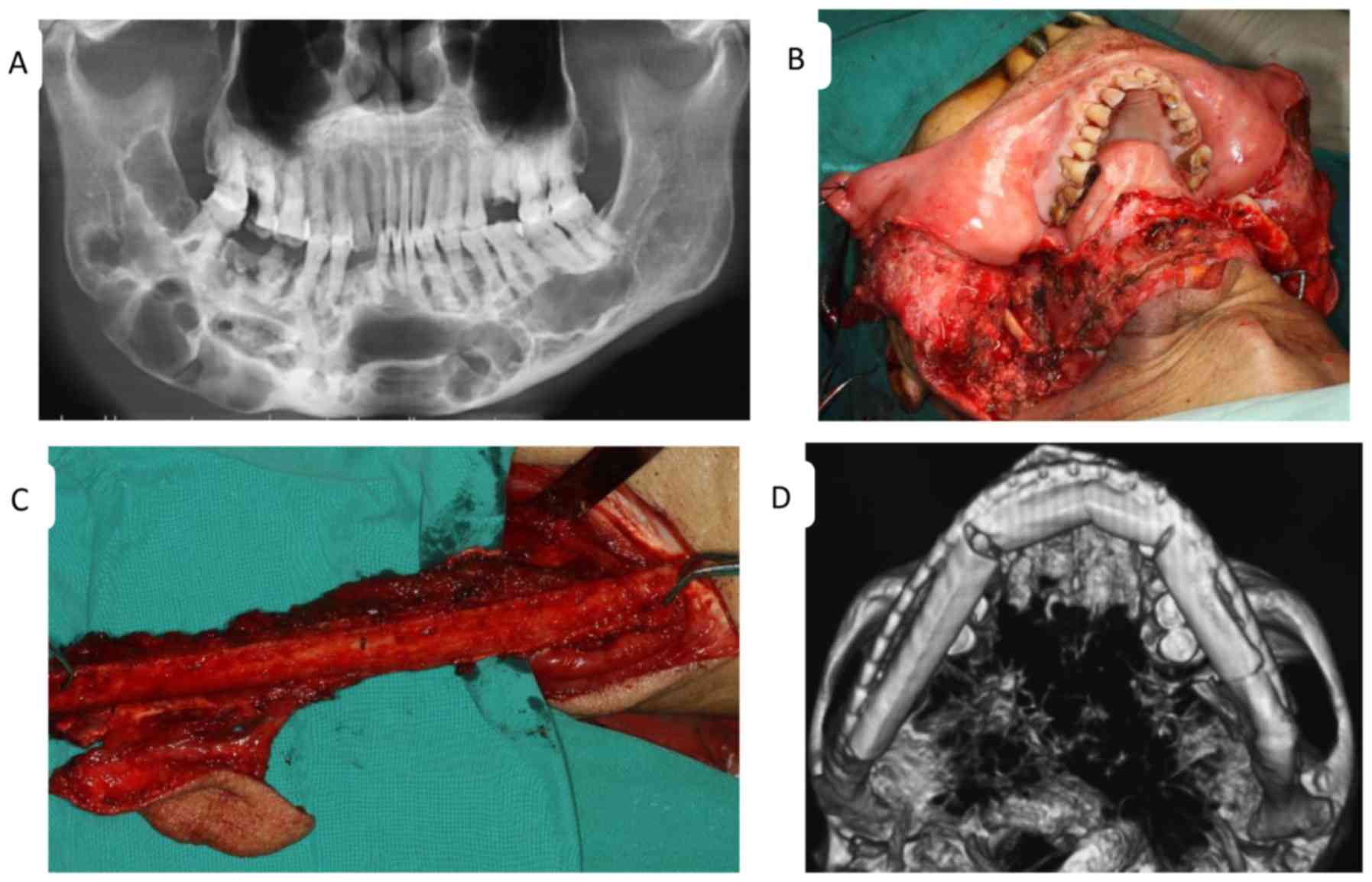
The treatment plans were based on clinical or
radiographic evidence of cortical perforation of the inferior or
posterior mandibular borders and subsequent soft tissue
involvement, multilocular large cysts and a history of previous
recurrence of the same lesion. All cases associated with any of
these features were considered to have a more aggressive behavior
and were therefore treated with radical resection, followed by
immediate reconstruction of the defect with autogenous bone grafts
(Fig. 1). In contrast, marginal
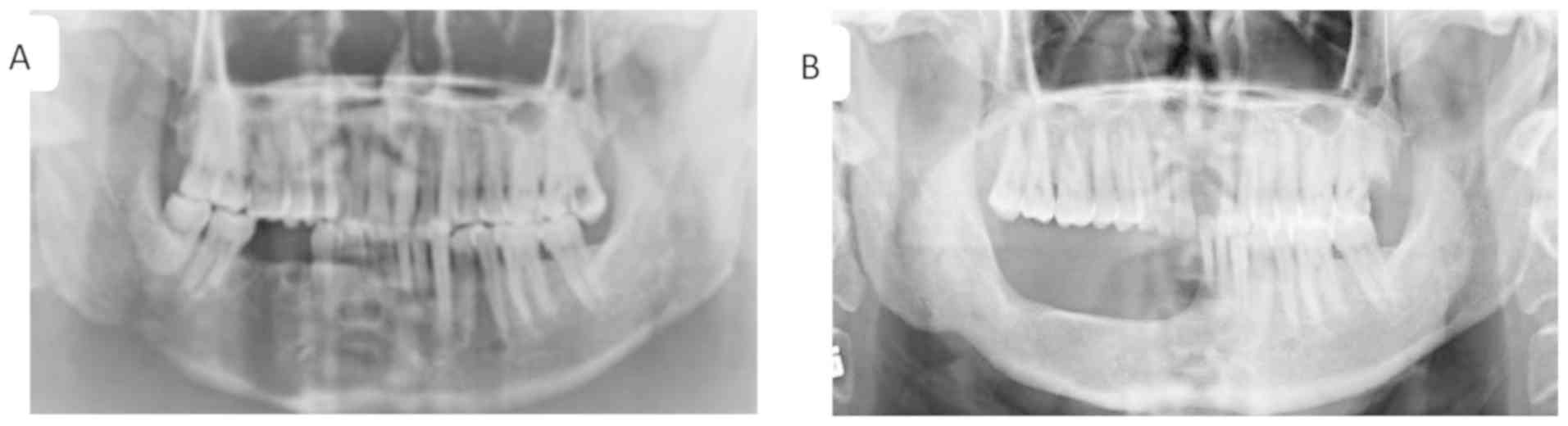
mandibulectomy was used with ~1 cm margin around the lesion,
whereas the lower border of the mandible and/or the posterior
border of the ramus was maintained intact (Fig. 2). When the soft tissue adjacent to
the cyst was involved, excision of the soft tissue up to the next
anatomical boundary was recommended and the excised tissue was
frozen and observed to determine adequacy of surgical margins.
Resection and reconstruction procedures were performed via
transmandibular approach with general anesthesia and
naso-endotracheal intubation. Two surgical teams simultaneously
operated on these patients, for whom immediate defect
reconstruction was performed. One team performed the mandible
resection and prepared the recipient site for flap transfer,
whereas the other team handled the vascularized flap. The length of
the follow-up period for patients that underwent radical resection
followed by reconstruction ranged from 2 to 17 years following
surgery (average, 5.82 years).
The justifications for resection were systematically
and carefully analyzed to identify the common major factor. The
functional results of patients with mandibular reconstruction were
evaluated using a self-assessment questionnaire that was completed
6 months after surgery. The questionnaire consisted in questions
regarding social activities, diet, speech, oral continence and
facial appearance. The cosmetic appearance following reconstruction
was assessed by the patients (patients perception) using their own
pre and post-reconstruction photographs (frontal and/or profile
views) and also by two experienced doctors. Postoperative
complications, including plate breakage, plate exposure, failure of
the flap, infection and recurrence were also evaluated. The
judgement criteria were the presence or absence of recurrence, jaw
function and cosmetic outcome.
Statistical analysis
Descriptive statistics, including frequency
distribution and percentage, measures of central tendency (average,
median) and measures of dispersion (range) were used to report the
data. The questionnaire was approved by the Medical Ethic Committee
of the School and Hospital of Stomatology, Wuhan University, and
written informed consent was obtained from all patients.
Results
Clinical characteristics of
patients
The present retrospective study evaluated 565
patients with OKCs. A total of 43 patients treated with a radical
approach were selected. Among them, two patients diagnosed with
basal cell nevus syndrome, one patient with a primary OKC and ≤12
months follow-up, and five patients with OKCs that occurred in the
maxilla were excluded. The remaining 35 patients (6.19%) underwent
OKCs resection. Table I presents the
patient demographics, lesion characteristics, treatments and
outcomes. The age of the patients ranged from 20 to 77 years old,
with a median age of 39.6 years. There were 27 men (77.14%) and
eight women (22.86%). Among the 35 patients, 26 had OKCs in the
mandibular molar-ramus region (74.29%), eight had OKCs in the
mandibular anterior-premolar area (22.86%) and one had OKCs in the
mandibular molar-ramus and anterior-molar regions (2.9%). A total
of 18 patients experienced cortical perforation with subsequent
soft tissue involvement or extension into the adjacent tissues.
Furthermore, 20 patients had primary OKCs (57.14%) and 15 patients
experienced recurrent OKCs (42.86%). Patients suffered from
recurrent OKCs for 1–34 years prior to resection (average, 8.8
years). The size of the OKCs varied from 7 to 15 cm, with an
average size of 9.40 cm.
 | Table I.Patient demographics, lesion
characteristics, treatments and outcomes. |
Table I.
Patient demographics, lesion
characteristics, treatments and outcomes.
| Patient no. | Sex | Age (years) | Location | Nature of OKC | Previous surgery
prior to resection | Surgery
management | Result at last
follow-up |
|---|
| 1 | F | 27 | Mandible
molar-ramus | Recurrent (3
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 2 | M | 30 | Mandible
anterior-premolar | Primary | None | Seg.
mandibulectomy | NERC |
| 3 | M | 31 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 4 | M | 77 | Mandible
molar-ramus | Recurrent (2
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 5 | F | 42 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 6 | M | 27 | Mandible
anterior-premolar | Primary | None | Seg.
mandibulectomy | NERC |
| 7 | F | 36 | Mandible
molar-ramus | Recurrent (3
times) | Decompression,
Enucleation | Seg.
mandibulectomy | NERC |
| 8 | F | 42 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 9 | M | 37 | Mandible
molar-ramus | Recurrent (3
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 10 | M | 44 | Mandible
molar-ramus | Recurrent (3
times) | Enucleation | Marg.
mandibulectomy | NERC |
| 11 | F | 22 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 12 | M | 20 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 13 | M | 49 | Mandible
molar-ramus | Recurrent (3
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 14 | F | 28 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 15 | M | 32 | Mandible
anterior-premolar | Recurrent (3
times) | Enucleation | Marg.
mandibulectomy | NERC |
| 16 | M | 66 | Mandible
molar-ramus | Primary | None | Marg.
mandibulectomy | ERC |
| 17 | M | 47 | Mandible
molar-ramus | Recurrent (3
times) | Decompression,
Enucleation | Seg.
mandibulectomy | NERC |
| 18 | M | 71 | Mandible
anterior-remolar | Primary | None | Marg.
mandibulectomy | NERC |
| 19 | M | 65 | Mandible
molar-ramus and anterior-molar | Primary | None | Seg.
mandibulectomy | NERC |
| 20 | M | 32 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 21 | M | 42 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 22 | M | 65 | Mandible
molar-ramus | Recurrent (3
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 23 | M | 48 | Mandible
anterior-premolar | Recurrent (1
time) | Decompression | Seg.
mandibulectomy | NERC |
| 24 | M | 35 | Mandible
anterior-premolar | Primary | None | Seg.
mandibulectomy | NERC |
| 25 | F | 36 | Mandible
molar-ramus | Recurrent (2
times) | Decompression,
Curettage | Seg.
mandibulectomy | NERC |
| 26 | M | 23 | Mandible
anterior-premolar | Recurrent (1
time) | Enucleation | Seg.
mandibulectomy | NERC |
| 27 | M | 32 | Mandible
anterior-premolar | Recurrent (2
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 28 | F | 53 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 29 | M | 28 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 30 | M | 49 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 31 | M | 45 | Mandible
molar-ramus | Recurrent (2
times) | Enucleation | Seg.
mandibulectomy | NERC |
| 32 | M | 52 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 33 | M | 54 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 34 | M | 50 | Mandible
molar-ramus | Primary | None | Seg.
mandibulectomy | NERC |
| 35 | M | 61 | Mandible
molar-ramus | Recurrent (2
times) | Enucleation,
Segmental mandibulectomy | Seg. mandibulectomy
+ Excision of the tumor from the deep surface of the masseter
muscle | NERC |
Treatment
Segmental mandibulectomy was completed in 31
patients (88.57%). Following resection, 28 patients (90.32%) were
immediately reconstructed with a vascularized fibula flap (11
patients), a vascularized iliac crest flap (16 patients) or frozen
autogenous bone replantation (one patient). No reconstruction was
completed in three patients due to economic constraints. Marginal
mandibulectomy was performed in four patients (11.43%), and one
patient underwent immediate reconstruction with an alloplastic
plate to prevent postoperative pathological fracture. In total, 18
patients had 7–9 cm in length of bone harvested, whereas 10
patients had 10–15 cm in length of bone harvested.
Functional outcomes
The functional outcomes of patients were evaluated
and the results revealed that diet and oral continence were normal,
speech was easily understood for all patients, but social
activities were diminished for three patients. Following mandibular
reconstruction, no patients experienced complications of flap
failure, plate exposure or plate breakage. Three patients
experienced moderate infections that were treated with local wound
care and antibiotic (Table II). The
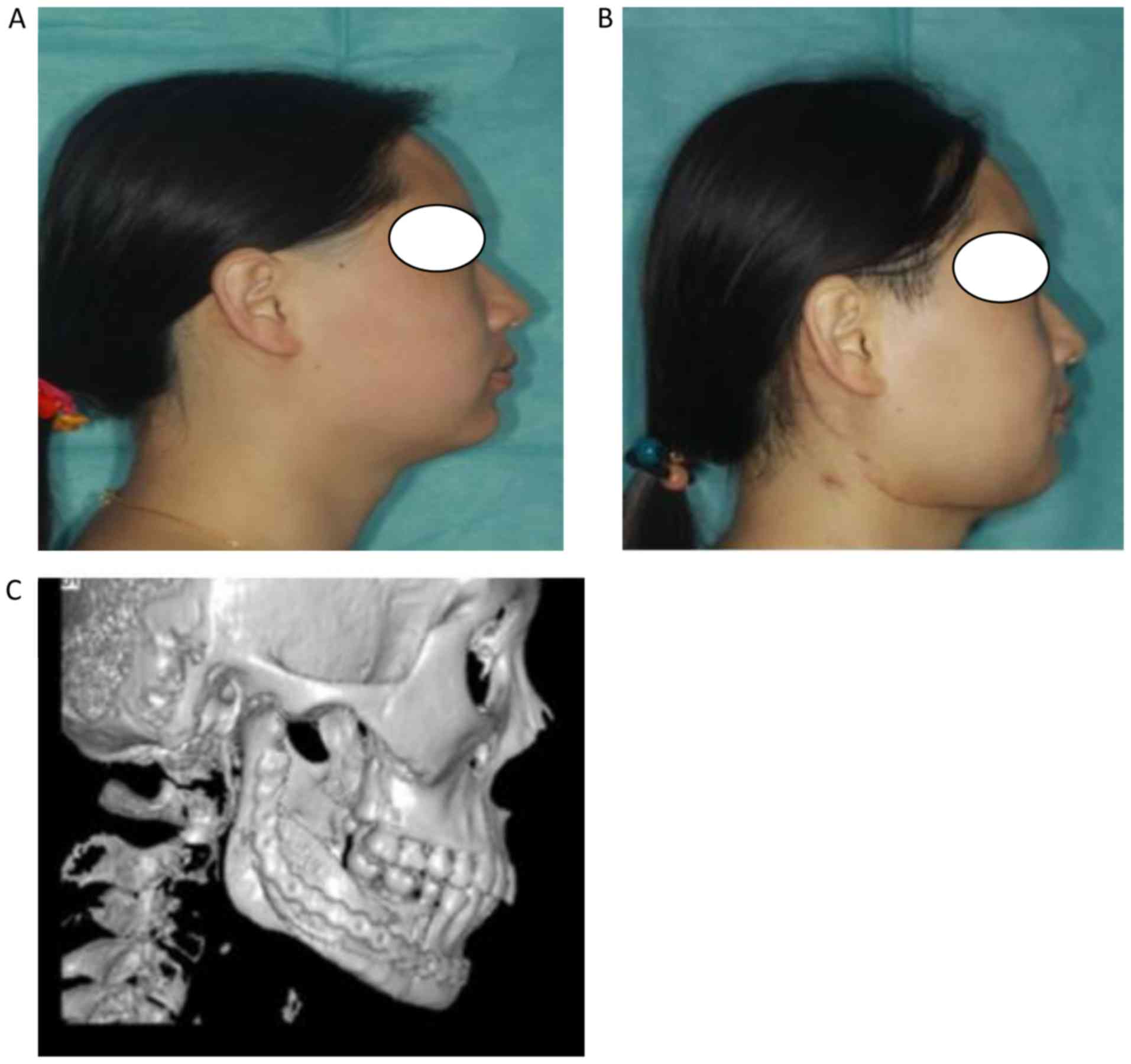
facial appearance of all patients following surgical intervention
was evaluated as good by the surgeons, and six of the patients
rated their facial appearance as acceptable (Fig. 3). There was one recurrence in a
patient treated with marginal mandibulectomy after a period of 5
years follow-up.
 | Table II.Complication, functional and esthetic
outcomes of patients following treatment. |
Table II.
Complication, functional and esthetic
outcomes of patients following treatment.
| Variables | Mandibular
reconstruction (n=28) | Percentage |
|---|
| Diet |
|
|
|
Normal | 28 | 100 |
|
Soft | – | – |
| Speech |
|
|
| Easily
understood | 28 | 100 |
|
Understood with effort | – | – |
|
Unintelligible | – | – |
| Social
activities |
|
|
|
Normal | 25 | 89.29 |
|
Diminished | 3 | 10.71 |
| Oral
continence |
|
|
|
Norma | 28 | 100 |
|
Slight/severe drooling | – | – |
| Facial
appearance |
|
|
|
Excellent/good |
|
|
|
Patient | 24 | 85.71 |
| Surgeon
team | 28 | 100 |
|
Acceptable |
|
|
|
Patient | 6 | 21.43 |
| Surgeon
team | – | – |
|
Poor |
|
|
|
Patient | – | – |
| Surgeon
team | – | – |
| Complications |
|
|
| Flap
failure | 0 | 0 |
| Plate
exposure | 0 | 0 |
| Plate
breakage | 0 | 0 |
|
Infection | 3 | 7.7 |
Discussion
The understanding of OKCs treatment modalities has
increased over the past few decades; however, the outcome remains
controversial. Enucleation is the most commonly used method for
surgical treatment of OKCs, although it presents a significantly
higher recurrence rate compared with other treatment options
(4,6,19). Since
OKCs lining is typically thin and friable, cyst removal in one
piece can therefore be difficult, in particular for large OKCs with
multilocular lesions. The use of adjunctive therapies usually
follows enucleation and reduces the recurrence rate to ≤10%
(20). Decompression and
marsupialization have been also used as a conservative treatment
method and both are beneficial in certain cases (13). These two techniques offer the
advantages of considerably reducing the cyst volume and diminishing
the risks of injuries to certain structures, including teeth or
inferior dental nerve (12). The OKC
wall after marsupialization commonly undergoes histological and
immunohistochemical changes and may transform into normal oral
mucosa without inherent aggressive features (21), which could explain the lower
recurrence rates in patients with OKCs treated by this approach
(22). However, both methods require
a longer treatment period with multiple-staged procedures. The high
degree of OKCs recurrence explains the inclination of certain
surgeons to eliminate the disease through a single radical surgical
approach; however the morbidity associated with this radical
approach guides other clinicians to select more conservative
techniques. Well-conducted randomized controlled clinical trials
analyzing the management of OKCs are therefore required. To the
best of our knowledge, no conclusions on the effectiveness of the
treatments for OKCs have yet been made (23) and there is no strong evidence that
can guide surgeons to select the best treatment option. In the
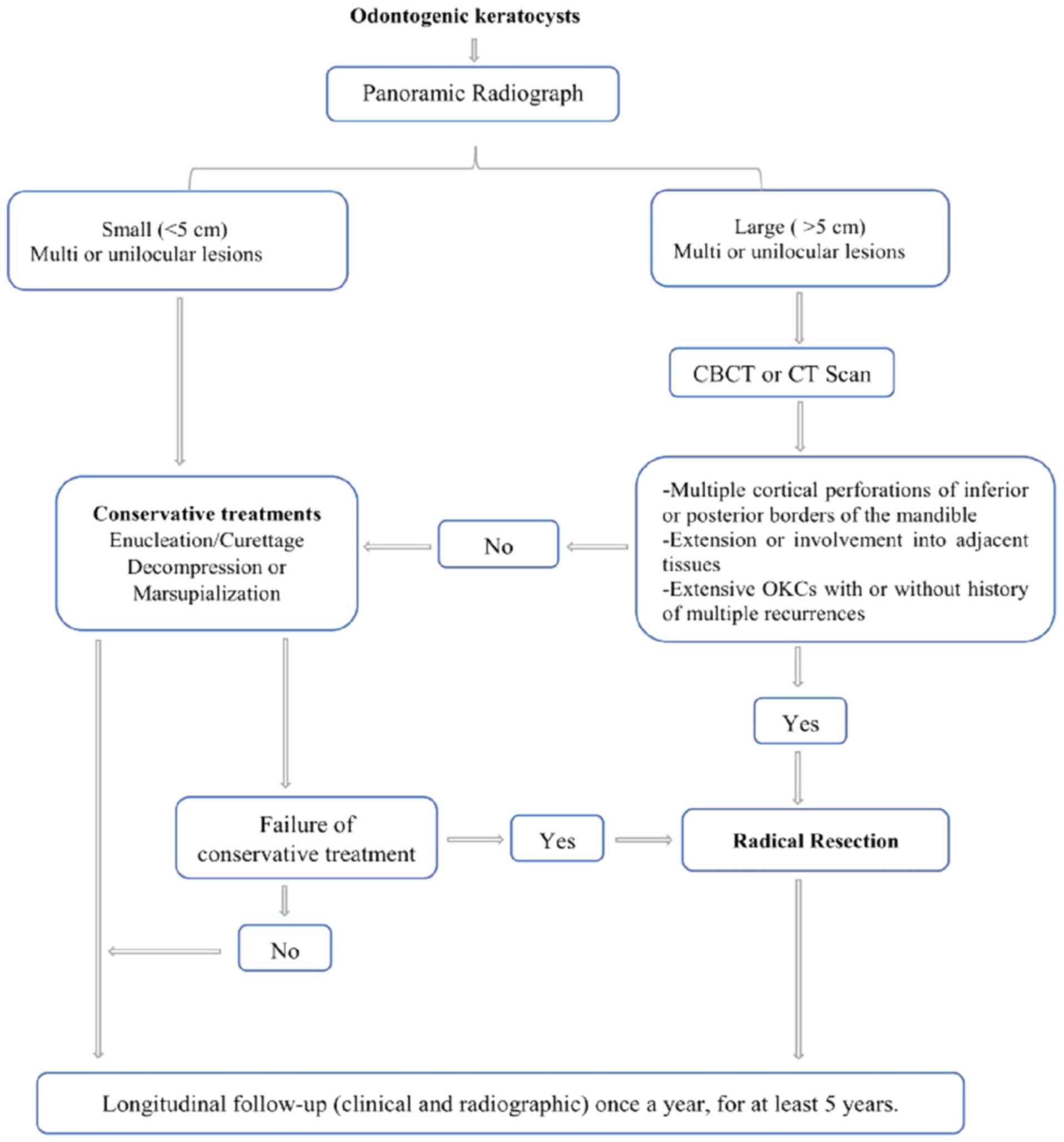
present study of 565 patients with OKCs, only 35 patients (6.19%)
underwent segmental or marginal resection, and immediate
reconstruction was performed in 28 of them (93.32%). Based on the
aforementioned results, a protocol for managing OKCs was
established (Fig. 4). Segmental
resection should be considered in the following situations: i)
Primary OKC with any radiologic appearance, exhibiting aggressive
clinical behavior such as multiple perforations of the jaws
cortical plates or extension into adjacent tissues, the involvement
of any location (particularly in the mandibular molar-ramus
region), and multilocular large lesions; and ii) recurrent OKC with
or without cortical perforation, or failure to comply with the
interval time follow-up schedule and with a size either similar or
larger than the primary lesion, particularly the multiple recurrent
OKCs in any location. If the primary lesion or recurrent lesion
with multiple radiolucencies does not grow sizable or without the
thinned inferior border of the mandible) and is located in the
mandible anterior region, marginal mandibulectomy is preferred.
Previous studies have demonstrated that mandibular
molar-ramus is the most common region with frequent perforation of
the overlying bone by OKCs and with firm cysts adhesion to the
overlying mucosa (19,20,24,25).
Excision of the overlying mucosa with the cysts and curettage with
carnoy's solution or electrocautery has been recommended in this
area (20). However, conservative
treatment methods are inadequate when OKCs have extended and
involve muscles with cortical perforation (18,26). In
addition, OKCs that occur in the mandibular molar-ramus region have
significantly higher recurrence rates (75%) compared with those in
other sites (27). Perforation of
the cortical plates and extension of the lesions from the masseter,
as presented in patient no. 35 of the present study, or extension
of the lesions from the pterygoid or the temporalis muscle to the
infratemporal fossa or orbit-skull base are possible at this stage,
and elimination of these OKCs requires a heavy wide surgery. The
thinned inferior border does not serve any purpose as chances of
pathological fracture occur. Subsequently, it is may be crucial to
treat primary OKC associated with aggressive behaviors more
radically in order to avoid a severe recurrent lesion.
Most studies emphasize that radical resection should
be limited to multiple recurrent OKCs, or to those that have
undergone malignant transformation (4,15,28).
Worrall (16) and Jackson et
al (18) recommended radical
excision as the treatment of choice for OKCs with bone perforation
or unpredictable lesions with any signs of soft tissue involvement.
Ahlfors et al (29) suggested
that in order to reduce the high recurrence rate of OKCs, surgery
should include marginal resection, including a rim of uninvolved
bone, which is similar to the treatment suggested in cases of
unicystic ameloblastoma. In the present study, the pathological
sign that influenced the decision to perform radical resection was
primary and recurrent OKCs that had clinically aggressive behavior
and that mostly occurred in the mandible molar-ramus region.
Segmental or marginal mandibulectomy was performed for those OKCs,
which was in agreement with previous studies that demonstrated that
~100% of recurrent OKCs contain epithelial islands and microcysts
in the overlying mucosa areas (20,30). The
absence of microcysts has been demonstrated in the surrounding bone
following block resections of recurrent OKCs (30).
OKCs recurrence within the bone graft following
segmental resection has also been reported (6,24,26). The
involvement of the surrounding soft tissues is common in mandibular
molar-ramus OKCs, and the bone perforation caused by OKCs ranges
from 39 to 50.8% (6), which was also
demonstrated in the present study. This may be considered as the
main cause of recurrence in patients following marginal
mandibulectomy observed in the present study. The presence of
multifocal cysts disease may also explain the recurrence rate.
Stoelinga (20) reported 3/80
patients and Boyne et al (31) reported seven cases with multiple
recurrent OKCs, of which six underwent segmental mandibulectomy
over 10–21 years. Their histologic examination revealed cyst
formation at distant sites from the original cyst in all cases,
which suggest that the lesions were multifocal. There are numerous
confounding factors associated with the recurrence and
clinicopathologic behavior of OKCs (13). Surgical management is the most
influential factor on recurrence. In the present study, one patient
with OKC that involved deep surface of the masseter muscle after
segmental mandibulectomy had also been reported in our previous
study (24).
The major sequelae of radical resection affect the
cosmetic and functional outcomes. Recently, the development of free
vascularized bone graft has facilitated the decision-making process
for surgical ablation in oral and maxillofacial surgery, and has
led to a high success rate of ~100% (32). In the present study, a large number
of patients who underwent segmental mandibulectomy were immediately
reconstructed with a vascularized flap, which was not the case in
our previous study (19). Immediate
reconstruction with a vascularized flap allowed good healing and
reduced the risk of bone resorption. Free fibula and iliac crest
flaps were the most widely used techniques in the present study, as
also reported in a previous study (33). The fibula flap is the only donor site
that allows reconstruction of entire mandibular defects. The free
iliac crest flap offers more choices for mandible reconstruction
when the length of bone harvested is ≤8 cm, in particular when used
for reconstruction of the mandibular body. In the present study,
most patients were greatly satisfied by their treatment, with
regards to resumption of normal diet, good speech, oral continence
and good facial appearance.
Conservative treatment methods of OKC are still
preferred by most surgeons. There is ongoing debate over the
preservation structure and reduction of the recurrence, and
numerous surgical approaches have been applied to OKCs. The
understanding of OKC treatment is clear to some extent; the overall
recurrence rate of ≤20% is not discouraging and there is a low
recurrence rate following resection.
The present study demonstrated that radical
resection was only suitable for OKCs with locally aggressive
features. Immediate reconstruction of the defect with vascularized
fibula or crest iliac flaps allowed positive functional and
cosmetic outcomes for patients who underwent an aggressive
treatment. Multiples recurrent lesions and primary OKCs with
aggressive clinical behavior, including perforation of the cortical
plates of the jaws or extension into the adjacent tissues,
extensive lesions, and presence in the mandibular molar-ramus
region were the main factors in the decision-making process for
radical resection. When possible, it was acceptable to start with a
conservative approach, including marsupialization followed by
enucleation, in particular in young patients or elderly patients
who are medically compromised. Long-term follow-up remains
important to monitor possible disease recurrence.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NBF contributed to the design of the study and wrote
the manuscript. NBF, YS, TW and YYZ collected the clinical samples.
YFZ, TW and LB performed the data analysis and revised the
manuscript. All authors have read and approved the manuscript.
Ethics approval and consent to
participate
The questionnaire survey was approved by The Medical
Ethic Committee of the School and Hospital of Stomatology, Wuhan
University (Hubei, China). Written informed consent was obtained
from the patients.
Patient consent for publication
Written informed consent was obtained from the
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Speight PM and Takata T: New tumour
entities in the 4th edition of the World Health Organization
Classification of Head and Neck tumours: Odontogenic and
maxillofacial bone tumours. Virchows Arch. 472:331–339. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Philipsen HP: Pathology and Genetics of
Head and Neck Tumours. World Health Organization Classification of
Tumours. Barnes L, Eveson JW, Reichart P and Sidransky D: IARC.
(Lyon). 306–307. 2005.
|
|
3
|
Peacock ZS: Controversies in oral and
maxillofacial pathology. Oral Maxillofac Surg Clin North Am.
29:475–486. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Al-moraissi EA, Dahan AA, Alwadeai MS,
Oginni FO, Al-jamali JM, Alkhutari AS, Al-Tairi NH, Almaweri AA and
Al-Sanabani JS: What surgical treatment has the lowest recurrence
rate following the management of keratocystic odontogenic tumor?: A
large systematic review and meta-analysis. J Craniomaxillofac Surg.
45:131–144. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pitak-Arnnop P, Chaine A, Oprean N,
Dhanuthai K, Bertrand JC and Bertolus C: Management of odontogenic
keratocysts of the jaws: A ten-year experience with 120 consecutive
lesions. J Craniomaxillofac Surg. 38:358–364. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Chirapathomsakul D, Sastravaha P and
Jansisyanont P: A review of odontogenic keratocysts and the
behavior of recurrences. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 101:5–9. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yagyuu T, Kirita T, Sasahira T, Moriwaka
Y, Yamamoto K and Kuniyasu H: Recurrence of keratocystic
odontogenic tumor: Clinicopathological features and
immunohistochemical study of the Hedgehog signaling pathway.
Pathobiology. 75:171–176. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sánchez-Burgos R, González-Martín-Moro J,
Pérez-Fernández E and Burgueño-García M: Clinical, radiological and
therapeutic features of keratocystic odontogenic tumours: A study
over a decade. J Clin Exp Dent. 6:e259–e264. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Al-Moraissi EA, Pogrel MA and Ellis E III:
Enucleation with or without adjuvant therapy versus
marsupialization with or without secondary enucleation in the
treatment of keratocystic odontogenic tumors: A systematic review
and meta-analysis. J Craniomaxillofaciac Surg. 44:1395–1403. 2016.
View Article : Google Scholar
|
|
10
|
Zecha JA, Mendes RA, Lindeboom VB and van
der Waal I: Recurrence rate of keratocystic odontogenic tumor after
conservative surgical treatment without adjunctive therapies-A
35-year single institution experience. Oral Oncol. 46:740–742.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cunha JF, Gomes CC, de Mesquita RA,
Andrade Goulart EM, de Castro WH and Gomez RS: Clinicopathologic
features associated with recurrence of the odontogenic keratocyst:
A cohort retrospective analysis. Oral Surg Oral Med Oral Pathol
Oral Radiol. 121:629–635. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pogrel MA and Jordan RC: Marsupialization
as a definitive treatment for the odontogenic keratocyst. J Oral
Maxillofac Surg. 62:651–655; discussion 655–656. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Mendes RA, Carvalho JF and van der Waal I:
Characterization and management of the keratocystic odontogenic
tumor in relation to its histopathological and biological features.
Oral Oncol. 46:219–225. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Blanas N, Freund B, Schwartz M and Furst
IM: Systematic review of the treatment and prognosis of the
odontogenic keratocyst. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod. 90:553–558. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kolokythas A, Fernandes RP, Pazoki A and
Ord RA: Odontogenic keratocyst: To decompress or not to decompress?
A comparative study of decompression and enucleation versus
resection/peripheral ostectomy. J Oral Maxillofac Surg. 65:640–644.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Worrall SF: Recurrent odontogenic
keratocyst within the temporalis muscle. Br J Oral Maxillofac Surg.
30:59–62. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gosau M, Draenert FG, Müller S, Frerich B,
Bürgers R, Reichert TE and Driemel O: Two modifications in the
treatment of keratocystic odontogenic tumors (KCOT) and the use of
carnoy's solution (CS)-a retrospective study lasting between 2 and
10 years. Clin Oral Investig. 14:27–34. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Jackson IT, Potparic Z, Fasching M,
Schievink WI, Tidstrom K and Hussain K: Penetration of the skull
base by dissecting keratocyst. J Craniomaxillofac Surg. 21:319–325.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhao YF, Wei JX and Wang SP: Treatment of
odontogenic keratocysts: A follow-up of 255 Chinese patients. Oral
Surg Oral Med Oral Pathol Oral Radiol. 94:151–156. 2002. View Article : Google Scholar
|
|
20
|
Stoelinga PJ: Long-term follow-up on
keratocysts treated according to a defined protocol. Int J Oral
Maxillofac Surg. 30:14–25. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
August M, Faquin WC, Troulis MJ and Kaban
LB: Dedifferentiation of odontogenic keratocyst epithelium after
cyst decompression. J Oral Maxillofac Surg. 61:678–683; discussion
683–684. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Chrcanovic BR and Gomez RS: Recurrence
probability for keratocystic odontogenic tumors: An analysis of
6427 cases. J Craniomaxillofac Surg. 45:244–251. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sharif FN, Oliver R, Sweet C and Sharif
MO: Interventions for the treatment of keratocystic odontogenic
tumours. Cochrane Database Syst Rev CD008464. 2015. View Article : Google Scholar
|
|
24
|
Liu B, Cai Y, Wang SP and Zhao YF:
Recurrent keratocystic odontogenic tumor in the masseter muscle
overlying the boney perforations: A case report. Oral Surg Oral Med
Oral Pathol Oral Radiol. 113:e1–e5. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Stoelinga PJ: Etiology and pathogenesis of
keratocysts. Oral Maxillofac Surg Clin North Am. 15:317–324. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Warburton G, Shihabi A and Ord RA:
Keratocystic odontogenic tumor (KCOT/OKC)-clinical guidelines for
resection. J Maxillofac Oral Surg. 14:558–564. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Myoung H, Hong SP, Hong SD, Lee JI, Lim
CY, Choung PH, Lee JH, Choi JY, Seo BM and Kim MJ: Odontogenic
keratocyst: Review of 256 cases for recurrence and
clinicopathologic parameters. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 91:328–333. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Giuliani M, Grossi GB, Lajolo C, Bisceglia
M and Herb KE: Conservative management of a large odontogenic
keratocyst: Report of a case and review of the literature. J Oral
Maxillofac Surg. 64:308–316. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ahlfors E, Larsson A and Sjögren S: The
odontogenic keratocyst: A benign cystic tumour? J Oral Maxillofac
Surg. 42:10–19. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Stoelinga PJ and Bronkhorst FB: The
incidence, multiple presentation and recurrence of aggressive cysts
of the jaws. J Craniomaxillofac Surg. 16:184–195. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Boyne PJ, Hou D, Moretta C and Pritchard
T: The multifocal nature of odontogenic keratocysts. J Calif Dent
Assoc. 33:961–965. 2005.PubMed/NCBI
|
|
32
|
Hidalgo DA and Pusic AL: Free-flap
mandibular reconstruction: A 10-year follow-up study. Plast
Reconstr Surg. 110:438–449; discussion 450–451. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Lyons AJ, James R and Collyer J: Free
vascularised iliac crest graft: An audit of 26 consecutive cases.
Br J Oral Maxillofac Surg. 43:210–214. 2005. View Article : Google Scholar : PubMed/NCBI
|