Introduction
Cystic renal cell carcinoma accounts for ~10% of
renal cancer, and it refers to the renal cancer confirmed by
pathology with mixed cystic-solid changes or cystic changes in
imageology (1). This disease appears
in people of any age, but is more common in elderly people and
males. If the tumor grading of cystic renal cell carcinoma is low,
the prognosis of patients can be improved by timely detection and
effective treatment (2). In clinic,
cystic renal cell carcinoma is rare, and patients with this disease
have no obvious clinical symptoms. It is often found by physical
examination. However, as cystic renal cell carcinoma is
insufficiently acquainted, it may be misdiagnosed as benign cystic
lesion of kidney (3). At present,
pathological diagnosis is the optimal standard for cystic renal
cell carcinoma, which is diagnosed by imageology in clinic
(4).
With the improvement of the diagnostic level and
imaging equipment, increased attention has been paid from
clinicians and radiologists on the diagnostic methods of cystic
renal cell carcinoma. Typical cystic renal cell carcinoma is easily
diagnosed by ultrasound sonograms, but a small number of atypical
cystic renal cell carcinomas with thin and regular cystic wall are
easily misdiagnosed as benign renal cysts (2). The CT manifestation of cystic renal
cell carcinoma has high density resolution. Thus, the
characteristics of cystic renal cell carcinoma can be analyzed by
imaging, which helps to accurately diagnose cystic renal cell
carcinoma (5). However, the CT
manifestation of cystic renal cell carcinoma is similar to that of
other benign cystic lesion. Therefore, cystic renal cell carcinoma
is easily misdiagnosed in clinic (6). Ultrasound is the preferred imaging
diagnostic method of cystic renal cell carcinoma. As a small amount
of new vessels appear in parenchymal part and septum of cystic
renal cell carcinoma, a little blood flow signal can be sometimes
seen in ultrasound, which is helpful for the diagnosis of cystic
renal cell carcinoma. However, the sensitivity and specificity of
ultrasound are poor in showing new microvascular vessels of tumors
(4). Studies have reported that the
combined diagnosis of imageology has a high diagnostic value in
Kawasaki disease (7), breast cancer
lesion (8) and early cervical cancer
(9). Baldari et al (10) found that ultrasound combined with CT
has a high diagnostic value in complex congenital heart diseases.
At present, the main diagnostic methods of cystic renal cell
carcinoma are ultrasound and CT. There are few reports on the
combined diagnosis of the two in cystic renal cell carcinoma.
The value of ultrasound combined with CT in the
diagnosis of cystic renal cell carcinoma was investigated in the
present study in order to provide an effective, sensitive and
accurate detection method for the diagnosis of cystic renal cell
carcinoma and improve the efficacy of the follow-up treatment and
prognosis of patients.
Patients and methods
General data
A total of 85 patients with cystic renal cell
carcinoma, who were admitted to the Oncology Department in Yantai
Yuhuangding Hospital Affiliated to Qingdao University (Yantai,
China) from December 2015 to April 2017, were selected as the study
group, with an average age of 47.89±5.12 years, including 68 males
and 17 females. The tumor diameter of patients was 50.13±11.76 mm,
and there were 49 cases with cystic renal cell carcinoma in left
kidney, 36 cases in right kidney, 47 cases with upper abdominal
discomfort, 23 cases with pain and discomfort in the waist, and 15
cases without obvious symptoms. A total of 70 patients with benign
renal cyst examined in Yantai Yuhuangding Hospital Affiliated to
Qingdao University during the same period were selected as the
benign group, with an average age of 46.21±4.85 years.
Inclusion criteria: i) patients >18 years of age;
ii) patients who actively cooperated with the research; and iii)
patients who had not received antitumor treatment before
examination.
Exclusion criteria: i) patients with mental illness
or a family history of mental illness in the past; ii) patients
with incomplete clinical data; iii) patients with severe diseases
in heart, liver and kidney; iv) patients who had contraindications
for ultrasound and CT; v) patients in gestation or lactation
period; and vi) patients with cystic renal cell carcinoma, severe
fungal infection, bacterial infection and virus infection.
The study was approved by the Ethics Committee of
Yantai Yuhuangding Hospital Affiliated to Qingdao University.
Patients who participated in this study had complete clinical data.
Signed informed consents were obtained from the patients or their
guardians.
Detection methods
All patients in both groups were examined by
ultrasound and CT, with an interval of <3 days. ATL HDI-5000
energy Doppler (Soma Technology, Inc.) and GE-LOGIQ9 color Doppler
(GE Healthcare) ultrasound diagnostic instruments were used. The
probe frequency was from 2.0 to 5.0 MHz. All patients fasted and
did not drink water for >8 h before ultrasound examination, and
in the next morning the patients with an empty stomach were
examined. A routine renal examination was carried out for the
patients, the echographic characteristics of the cystic lesions of
the kidneys were observed, and the size of the tumors was measured.
Energy Doppler and color Doppler ultrasound diagnostic instruments
were used to observe internal and peripheral blood flow of the
lesion part. The presence of swollen lymph nodes in renal hilus and
tumor thrombus in renal vein and postcava was checked, as well as
whether there was contralateral kidney and normal renal tissue
around the tumors.
Light speed 64-tier spiral CT instrument, produced
by GE Healthcare, was used to examine the patients. Plain scanning
and 3-phase dynamic enhanced scanning were carried out. The
patients were restricted from eating 8 h before the examination and
kept fasting. Before scanning, the patients were instructed to
drink purified water, and then the parameter of plain scanning was
set and the patients were scanned in supine position. The scanning
parameters were: tube current, 150–250 mA; tube voltage, 90–120 kV;
time product, 200 mAs; layer thickness, 5–10 mm; screw pitch, 1.0.
The vein mass in the anterior elbow of the patients was injected
with contrast agent by high-pressure automatic injectors. According
to the condition of the patients, the dosage of iohexol was
adjusted between 1.5 and 2.0 ml/kg (SFDA approval no. H19980218;
Beijing BeiLu Pharmaceutical Co., Ltd.) and the injection rate of
contrast agent was 2–3 ml/sec. The enhanced scanning was carried
out in renal cortex phase (delayed 25–30 sec), parenchymal phase
(delayed 60–90 sec), and renal pelvis phase (delayed 3–5 min).
The results were analyzed by the double-blind method
(at least four radiologists), and the final results were determined
after the radiologists came to an agreement.
Observation indicators
The scanning results of all patients were recorded
and graded. Bosniak grading (11):
Grade II: septum thickness was <1.0 mm. There was calcification
with the shape of filament and no enhancement of enhanced scanning.
Grade IIF: there were more complex features in Grade IIF compared
with Grade II. The calcification may be nodular, the septum wall
thickened, and there was no enhanced scanning or there was little
enhancement. Grade III: intracapsular signal was uneven, irregular
strip calcification could be seen, and cyst was characterized by
high density. Grade IV: intracapsular septum was distributed
irregularly, and substantial nodule could be seen. Clinical
observation indicators: the diagnostic results of surgery and
needle biopsy were used as reference. The sensitivity, specificity,
diagnostic coincidence rate, missed diagnosis rate and misdiagnosis
rate of ultrasound, CT and ultrasound combined with CT in diagnosis
of cystic renal cell carcinoma were calculated.
Statistical analysis
Experimental data were statistically analyzed by
SPSS 17.0 statistical software (SPSS, Inc.). Enumeration data were
expressed in the form of n (%) and Chi-square test was used for the
comparison between groups. Measurement data were expressed as mean
± standard deviation and paired t-test was used for the comparison
between two groups. ANOVA, with LSD post hoc test, was used for
comparison between multiple groups. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison of the general data between
the two groups
There were no significant differences in age, sex,
body mass index, smoking, drinking, history of diabetes, history of
hypertension, white blood cells, red blood cells, and platelet
count between the groups (P>0.05). The groups were comparable
(Table I).
 | Table I.Comparison of general data between the
two groups [n (%), mean ± standard deviation]. |
Table I.
Comparison of general data between the
two groups [n (%), mean ± standard deviation].
| Variables | Study group
(n=85) | Benign group
(n=70) | χ2/t | P-value |
|---|
| Age (years) | 47.89±5.12 | 46.21±4.85 | 0.842 | 0.401 |
| Sex |
|
| 0.048 | 0.827 |
| Male | 68 (80.0) | 55 (78.6) |
|
|
|
Female | 17 (20.0) | 15 (21.4) |
|
|
| Body mass index
(kg/m2) | 26.12±3.09 | 25.97±2.99 | 0.305 | 0.761 |
| Smoking |
|
|
|
|
| Yes | 43 (50.6) | 36 (51.4) | 0.011 | 0.917 |
| No | 42 (49.4) | 34 (48.6) |
|
|
| Drinking |
|
| 0.876 | 0.350 |
| Yes | 56 (65.9) | 41 (58.6) |
|
|
| No | 29 (34.1) | 29 (41.4) |
|
|
| History of
diabetes |
|
| 0.308 | 0.579 |
| Yes | 24 (28.2) | 17 (24.3) |
|
|
| No | 61 (71.8) | 53 (75.7) |
|
|
| History of
hypertension |
|
| 0.034 | 0.854 |
| Yes | 16 (18.8) | 14 (20.0) |
|
|
| No | 69 (81.2) | 56 (80.0) |
|
|
| White blood cells
(×109/l) |
6.24±3.67 |
6.37±3.77 | 0.829 | 0.217 |
| Platelets
(×109/l) | 173.23±21.09 | 169.26±23.87 | 1.099 | 0.274 |
| Red blood cells
(×1012/l) |
4.65±0.65 |
4.77±0.71 | 1.097 | 0.274 |
Comparison of diagnostic results
As shown in Table
II, 85 cases were diagnosed with cystic renal cell carcinoma by
pathology; 92 cases were diagnosed by CT, among which 65 cases were
true-positive; 88 cases were diagnosed by ultrasound, among which
74 cases were true-positive; and 99 cases were diagnosed by
ultrasound combined with CT, among which 84 cases were
true-positive.
 | Table II.Comparison of diagnostic results. |
Table II.
Comparison of diagnostic results.
| Detection
results | Pathological
results + | Pathological
results - | Summation |
|---|
| CT + | 65 | 27 | 92 |
| CT - | 20 | 43 | 63 |
| Summation | 85 | 70 | 155 |
| Ultrasound + | 74 | 14 | 88 |
| Ultrasound - | 11 | 56 | 67 |
| Summation | 85 | 70 | 155 |
| Ultrasound combined
with CT + | 84 | 15 | 99 |
| Ultrasound combined
with CT - | 1 | 55 | 56 |
| Summation | 85 | 70 | 155 |
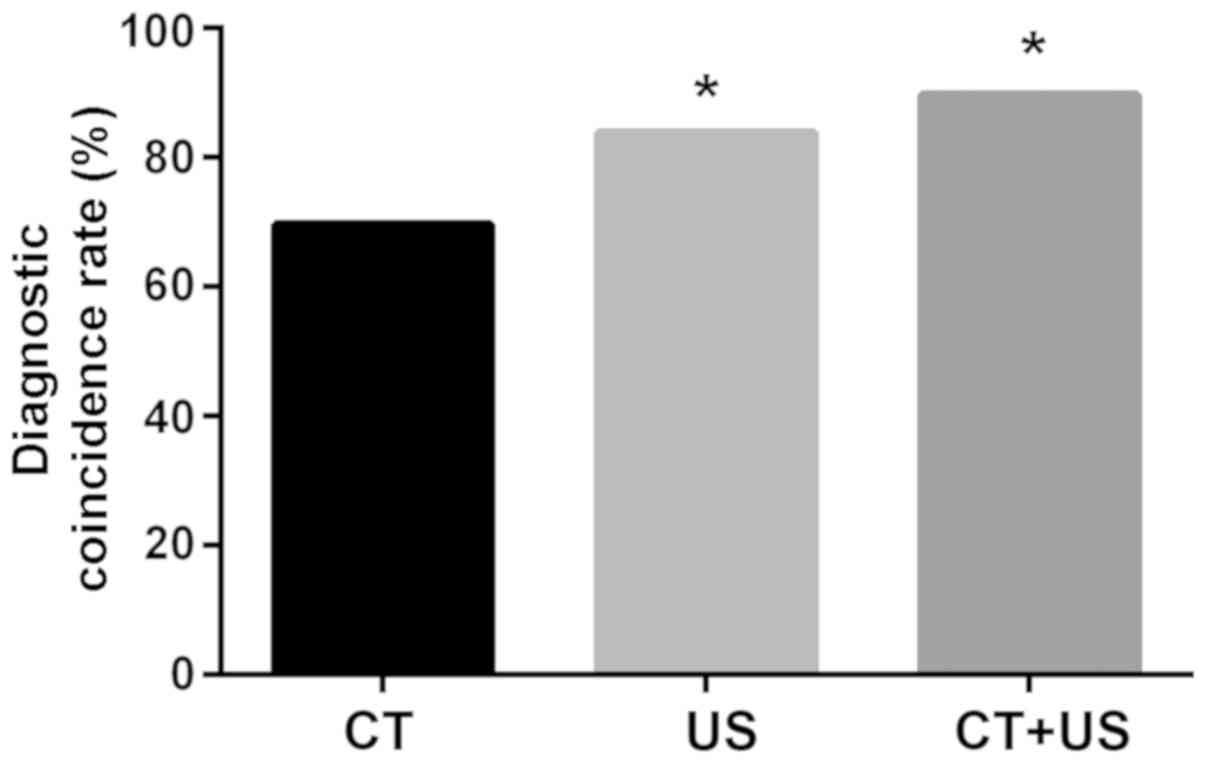
As shown in Table
III, the accuracy of the different methods was compared. The
sensitivity of ultrasound combined with CT was significantly higher
than that of CT and that of ultrasound (P<0.05). There was no
significant difference between the sensitivity of CT and the
sensitivity of ultrasound (P>0.05). The specificity of
ultrasound combined with CT and ultrasound alone was significantly
higher than that of CT (P<0.05). There was no significant
difference between the specificity of ultrasound combined with CT
and the specificity of ultrasound (P>0.05). It can be seen from
Fig. 1 that the diagnostic
coincidence rate of ultrasound was significantly higher than that
of CT and the diagnostic coincidence rate of ultrasound combined
with CT was significantly higher than that of CT (P<0.05).
 | Table III.Comparison of the accuracy of
different methods. |
Table III.
Comparison of the accuracy of
different methods.
| Variables | Sensitivity | Specificity |
|---|
| CT | 76.5% | 61.4% |
| Ultrasound | 87.1% | 80.0%a |
| Ultrasound combined
with CT | 98.8%a,b | 78.6%a |
| χ2 | 22.44 | 11.69 |
| P-value | <0.001 | 0.003 |
Comparison of the accuracy of the
different methods in the diagnosis of unicapsular and polycystic
kidney cancer
There were 39 cases diagnosed with unicapsular
kidney cancer and 46 cases diagnosed with polycystic kidney cancer.
The accuracy of the different methods in the diagnosis of
unicapsular and polycystic kidney cancer was compared. As seen in
Table IV, in terms of unicapsular
kidney cancer, there was no significant difference among
ultrasound, CT and ultrasound combined with CT in the diagnosis of
septum and wall nodule (P>0.05). In terms of polycystic kidney
cancer, there was no significant difference among ultrasound, CT
and ultrasound combined with CT in the diagnosis of the presence or
absence of septum (P>0.05), but the accuracy of ultrasound
combined with CT and that of CT alone was significantly higher than
the accuracy of ultrasound in the diagnosis of the presence or
absence of wall nodule (P<0.05).
 | Table IV.Comparison of the accuracy of
different methods in the diagnosis of unicapsular and polycystic
kidney cancer [n (%)]. |
Table IV.
Comparison of the accuracy of
different methods in the diagnosis of unicapsular and polycystic
kidney cancer [n (%)].
| Methods | Cases | Ultrasound | CT | Ultrasound combined
with CT | χ2 | P-value |
|---|
| Unicapsular kidney
cancer (n=39) |
| Absence
of septum | 10 | 10 (100.0) | 9 (90.0) | 10
(100.0) | 2.069 | 0.355 |
|
Presence of septum | 29 | 28 (96.6) | 26 (89.7) | 29
(100.0) | 3.669 | 0.160 |
| Absence
of wall nodule | 12 | 12 (100.0) | 11 (91.7) | 12
(100.0) | 2.057 | 0.358 |
|
Presence of wall nodule | 27 | 27 (100.0) | 25 (92.6) | 27
(100.0) | 4.101 | 0.129 |
| Polycystic kidney
cancer (n=46) |
| Absence
of septum | 13 | 12 (92.3) | 11 (84.6) | 13
(100.0) | 2.167 | 0.338 |
|
Presence of septum | 33 | 33 (100.0) | 31 (94.0) | 33
(100.0) | 4.082 | 0.130 |
| Absence
of wall nodule | 30 | 16 (53.3) | 28
(93.3)a | 30
(100.0)a | 26.150 | <0.001 |
|
Presence of wall nodule | 16 | 9 (56.3) | 14
(87.5)a | 15
(93.8)a | 7.832 | 0.020 |
Display rate of different
symptoms
In terms of the display of nidus and blood supply,
CT was significantly better than ultrasound in calcification and
blood supply of tumor (P<0.05). Ultrasound was significantly
better than CT in cyst wall confounding (P<0.05). Ultrasound
combined with CT was significantly better than ultrasound in
calcification and blood supply of tumor (P<0.05). Ultrasound
combined with CT was significantly better than CT in septum and
cyst wall confounding (P<0.05; Table
V).
 | Table V.Display rate of different symptoms [n
(%)]. |
Table V.
Display rate of different symptoms [n
(%)].
| Symptoms | Cases | Ultrasound | CT | Ultrasound combined
with CT | χ2 | P-value |
|---|
| Cyst wall slightly
irregular or completely irregular | 66 | 64 (97.0) | 66
(100.0) | 66
(100.0) |
4.041 |
0.133 |
| Septum | 62 | 61 (98.4) | 56 (90.3) | 62
(100.0)b |
9.20 |
0.010 |
| Calcification | 26 | 12 (46.2) | 24
(92.3)a | 26
(100.0)a | 27.05 | <0.001 |
| Wall nodule | 43 | 36 (83.7) | 39 (90.7) | 42 (97.7) |
4.962 |
0.084 |
| Cyst wall
confounding | 68 | 68
(100.0) | 62
(91.2)a | 68
(100.0)b | 12.36 |
0.002 |
| Blood supply of
tumor | 74 | 61 (82.4) | 73
(98.6)a | 74
(100.0)a | 23.94 | <0.001 |
Comparison of the results of Bosniak
grading diagnosis
Comparison of the results of Bosniak grading
diagnosis showed no significant difference between ultrasound and
CT (P<0.05). Ultrasound combined with CT was significantly
better than CT in the diagnosis of grades IIF and III (P<0.05).
Ultrasound combined with CT was significantly better than
ultrasound in the diagnosis of grade IIF (P<0.05; Table VI).
 | Table VI.Comparison of the results of Bosniak
grading diagnosis [n (%)]. |
Table VI.
Comparison of the results of Bosniak
grading diagnosis [n (%)].
| Bosniak
grading | No. | Ultrasound | CT | Ultrasound combined
with CT | χ2 | P-value |
|---|
| II | 37 | 36 (97.3) | 34 (92.0) | 37
(100.0) | 3.63 | 0.163 |
| IIF | 22 | 18 (81.8) | 14 (63.6) | 22
(100.0)a,b | 9.78 | 0.008 |
| III | 15 | 11 (73.3) | 8
(53.3) | 14
(93.3)b | 6.14 | 0.047 |
| IV | 11 | 9
(81.8) | 9
(81.8) | 11
(100.0) | 2.28 | 0.320 |
Discussion
Cystic renal cell carcinoma is a general term for
cystic space-occupying lesions of the kidney, which is separated
into four subtypes, i.e., the monolocular, multilocular, cystic
necrosis, and cyst epithelial-derived type (12). However, some scholars only separate
it into polycystic and unicapsular kidney cancers (13). Among the four pathological types,
polycystic kidney cancer accounts for ~33% of renal cystic tumors
(14). The main pathological feature
of cystic renal cell carcinoma is that there are multiple cysts
with different size in cancer tissue. The cyst wall is lined with
transparent cancer cells, there are agminated transparent cancer
cells in septum of the cyst. Cystic renal cell carcinoma is a renal
gland cancer, and a cyst is caused by cystic expansion of the
glandular cavity of adenocarcinoma (15). In the last 30 years, with the
popularization of B-ultrasound and CT, the detection rate of cystic
renal cell carcinoma has improved, which helps to accumulate
experience for preoperative diagnosis (16).
Accurate diagnosis is sometimes difficult because
there are similar imaging features among cystic renal cell
carcinoma, conventional renal cell carcinoma with cystic changes
and benign renal cystic diseases (17). Cystic small renal carcinoma is
generally graded and screened by ultrasound or CT. Bosniak grading
is mainly based on examination results of CT. It is divided into
four grades. Grades I and II represent benign nidus, grades III and
IV represent malignant nidus. Grade IIF is between grades II and
III. There are more lesions in grade IIF in clinic, so the
diagnosis is relatively difficult (18). Studies have shown that ultrasound
combined with Bosniak criteria can improve the diagnostic rate of
benign and malignant renal cystic lesions (19). Therefore, the accuracy of different
diagnostic methods in Bosniak grading diagnosis of cystic renal
cell carcinoma was compared in this study.
There were no significant differences in age, sex,
body mass index, smoking, drinking, history of diabetes, history of
hypertension, white blood cells, red blood cells, and platelet
count of the patients between the two groups, and thus, the groups
were comparable. Literature shows that generally CT and nuclear
magnetic resonance are consistent in the diagnostic classification
of cystic renal space-occupying lesions (20), but compared with CT, ultrasonic
contrast can help to improve the diagnostic accuracy of cystic
renal cell carcinoma (21).
Furthermore, studies have shown that enhanced ultrasound is
superior to unenhanced ultrasound and CT in the diagnosis of
complex cystic renal tumors (22).
This study showed that the sensitivity of ultrasound combined with
CT was significantly higher than that of CT and that of ultrasound
(P<0.05). The specificity and diagnostic coincidence rate of
ultrasound combined with CT were significantly higher than that of
CT (P<0.05). These results indicate that the combined diagnosis
can also improve the sensitivity, and the accuracy of the combined
diagnosis is high in the diagnosis of cystic renal cell carcinoma.
The accuracy of different methods in the diagnosis of unicapsular
and polycystic kidney cancer was also compared. For unicapsular
kidney cancer, there was no significant difference among
ultrasound, CT and ultrasound combined with CT in the diagnosis of
septum and wall nodule. For polycystic kidney cancer, there was no
significant difference among ultrasound, CT and ultrasound combined
with CT in the diagnosis of the presence or absence of septum. The
accuracy of CT and ultrasound combined with CT was significantly
higher than that of ultrasound in the diagnosis of the presence or
absence of wall nodule. The diagnosis of blood supply of the nidus
is an important aspect in the diagnosis of cystic renal cell
carcinoma and benign cystic renal diseases (23). The results of this study showed that
CT was significantly better than ultrasound in wall nodule,
calcification and blood supply of tumors. Ultrasound was
significantly better than CT in cyst wall confounding. Ultrasound
combined with CT was significantly better than ultrasound in
calcification and blood supply of tumors. Ultrasound combined with
CT was significantly better than CT in septum and cyst wall
confounding (P<0.05). Previous studies have demonstrated that CT
has a high display rate in showing wall nodule, calcification or
tumor, but compared with CT, ultrasound has a good display rate in
showing the number of septum, the enhancement of cystic tumors, the
thickness of septum or the thickness of the wall, and it can show
the internal structure of cystic tumors (24,25), in
agreement with the results of the present study. Ultrasound is a
better choice in showing specific nidus response. At the same time,
CT can effectively show the blood supply of the nidus in patients.
Therefore, the combination of the two methods can significantly
improve the diagnostic accuracy of cystic renal cell carcinoma and
help patients to receive timely treatment in order to reduce the
damage caused by cystic renal cell carcinoma (26,27).
Katabathina et al (28)
considered that the diagnosis of malignancy degree of renal cystic
lesion is particularly important. In terms of the comparison of the
results of Bosniak grading diagnosis, ultrasound combined with CT
is significantly superior to CT from grade IIF to III, and
ultrasound combined with CT is superior to ultrasound in grade IIF.
This study showed that the accuracy of the combined diagnosis is
higher than that of the other methods in the grading diagnosis. It
has been proven (29) that the
combination of imageology tests helps to improve space-occupying
diagnostic coincidence rate of cystic kidney in complex cyst which
is type II or above. Therefore, the combination of imageology tests
has a high value in clinical diagnosis.
Single imaging and multiple imaging techniques were
compared in the present study. The research presented is
innovative, however, the number of cases in the groups is not
sufficient, and the study is mainly retrospective, so there may
exist deviations in the study results. Therefore, future studies
confirming the above results are anticipated.
In summary, the accuracy of ultrasound combined with
CT is higher than that of ultrasound and that of CT in the
diagnosis of cystic renal cell carcinoma. Ultrasound combined with
CT can help to accurately carry out clinical diagnosis, reduce the
incidence of missed diagnosis and misdiagnosis caused by single
diagnosis and treatment. Ultrasound combined with CT is good for
clinical screening and can guide clinical symptomatic treatment,
and therefore is worthy of generalizing in clinic.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MS interpreted the data and drafted the manuscript.
CW conceived and designed the study. FJ and XF collected and
analyzed the data. BG was responsible for the ultrasound and CT
examination and revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Yantai Yuhuangding Hospital Affiliated to Qingdao University
(Yantai, China). Patients who participated in this study had
complete clinical data. Signed informed consents were obtained from
the patients or their guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gummadi S, Eisenbrey JR and Lyshchik A:
Contrast-enhanced ultrasonography in interventional oncology. Abdom
Radiol (NY). 43:3166–3175. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhou D, Quan Z and Wang J: Current status
of malignant mesothelioma with liver involvement in China: A brief
report and review of the literature. Intractable Rare Dis Res.
7:112–119. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liu B, Chen J, Jiang H, Wang S, Shen BH,
Jin BY and Xie LP: Diagnosis and treatment of cystic renal cell
carcinoma: A report of 14 cases. Zhonghua Yi Xue Za Zhi.
91:2861–2862. 2011.(In Chinese). PubMed/NCBI
|
|
4
|
Sirohi D, Smith SC, Agarwal N and Maughan
BL: Unclassified renal cell carcinoma: Diagnostic difficulties and
treatment modalities. Res Rep Urol. 10:205–217. 2018.PubMed/NCBI
|
|
5
|
Bindayi A, Mcdonald ML, Beksac AT,
Rivera-Sanfeliz G, Shabaik A, Hughes F, Aganovic L, Hansel DE and
Derweesh IH: Can multiphase CT scan distinguish between papillary
renal cell carcinoma type 1 and type 2? Turk J Urol. 44:316–322.
2018.PubMed/NCBI
|
|
6
|
Kim SH, Kwon WA, Joung JY, Seo HK, Lee KH
and Chung J: Clear cell papillary renal cell carcinoma: A case
report and review of the literature. World J Nephrol. 7:155–160.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mahajan A, Deshpande SS and Thakur MH:
Diffusion magnetic resonance imaging: a molecular imaging tool
caught between hope, hype and the real world of ‘personalized
oncology’. World J Radiol. 9:253–268. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Deng B, Lundqvist M, Fang Q and Carp SA:
Impact of errors in experimental parameters on reconstructed breast
images using diffuse optical tomography. Biomed Opt Express.
9:1130–1150. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Deán-Ben XL, Gottschalk S, Mc Larney B,
Shoham S and Razansky D: Advanced optoacoustic methods for
multiscale imaging of in vivo dynamics. Chem Soc Rev. 46:2158–2198.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Baldari D, Capece S, Mainenti PP, Tucci
AG, Klain M, Cozzolino I, Salvatore M and Maurea S: Comparison
between computed tomography multislice and high-field magnetic
resonance in the diagnostic evaluation of patients with renal
masses. Quant Imaging Med Surg. 5:691–699. 2015.PubMed/NCBI
|
|
11
|
Sevcenco S, Spick C, Helbich TH, Heinz G,
Shariat SF, Klingler HC, Rauchenwald M and Baltzer PA: Malignancy
rates and diagnostic performance of the Bosniak classification for
the diagnosis of cystic renal lesions in computed tomography - a
systematic review and meta-analysis. Eur Radiol. 27:2239–2247.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Aboagye EO and Kraeber-Bodéré F:
Highlights lecture EANM 2016: ‘Embracing molecular imaging and
multi-modal imaging: a smart move for nuclear medicine towards
personalized medicine’. Eur J Nucl Med Mol Imaging. 44:1559–1574.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chung SD, Liu SP and Lin HC: A
population-based study on the association between urinary calculi
and kidney cancer. Can Urol Assoc J. 7:E716–E721. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lévy P, Hélénon O, Merran S, Paraf F,
Méjean A, Cornud F and Moreau JF: Cystic tumors of the kidney in
adults: Radio-histopathologic correlations. J Radiol. 80:121–133.
1999.(In French). PubMed/NCBI
|
|
15
|
Sadiq M, Ahmad I, Shuja J, Ahmad Z, Ahmed
R and Ahmad K: Astroblastoma in a young female patient: A case
report and literature review of clinicopathological, radiological
and prognostic characteristics and current treatment strategies.
Brain Tumor Res Treat. 5:120–126. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gao XH, Hua YQ, Ding JG, Zhan JX, Song T,
Yin YL, Qian WQ and Song JD: Value of spiral CT in diagnosis of
cystic renal cell carcinoma. Zhonghua Zhong Liu Za Zhi. 28:130–133.
2006.(In Chinese). PubMed/NCBI
|
|
17
|
Bah I, Fahiminiya S, Bégin LR, Hamel N,
D'Agostino MD, Tanguay S and Foulkes WD: Atypical tuberous
sclerosis complex presenting as familial renal cell carcinoma with
leiomyomatous stroma. J Pathol Clin Res. 4:167–174. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Weibl P, Hora M, Kollarik B, Kalusova K,
Pitra T, Remzi M, Hübner W, Balzer P and Klatte T: A practical
guide and decision-making protocol for the management of complex
renal cystic masses. Arab J Urol. 15:115–122. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xu HX: Contrast-enhanced ultrasound: The
evolving applications. World J Radiol. 1:15–24. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Israel GM, Hindman N and Bosniak MA:
Evaluation of cystic renal masses: comparison of CT and MR imaging
by using the Bosniak classification system. Radiology. 231:365–371.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Park BK, Kim B, Kim SH, Ko K, Lee HM and
Choi HY: Assessment of cystic renal masses based on Bosniak
classification: Comparison of CT and contrast-enhanced US. Eur J
Radiol. 61:310–314. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Quaia E, Bertolotto M, Cioffi V, Rossi A,
Baratella E, Pizzolato R and Cov MA: Comparison of
contrast-enhanced sonography with unenhanced sonography and
contrast-enhanced CT in the diagnosis of malignancy in complex
cystic renal masses. AJR Am J Roentgenol. 191:1239–1249. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ragel M, Nedumaran A and Makowska-Webb J:
Prospective comparison of use of contrast-enhanced ultrasound and
contrast-enhanced computed tomography in the Bosniak classification
of complex renal cysts. Ultrasound. 24:6–16. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lal A, Naranje P and Pavunesan SK: What's
new in urologic ultrasound? Indian J Urol. 31:176–184. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bukhari S, Amodu A, Akinyemi M and Wallach
S: Persistent hematuria caused by renal cell carcinoma after aortic
valve replacement and warfarin therapy. Proc Bayl Univ Med Cent.
30:327–329. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Rafailidis V, Fang C, Yusuf GT, Huang DY
and Sidhu PS: Contrast-enhanced ultrasound (CEUS) of the abdominal
vasculature. Abdom Radiol (NY). 43:934–947. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Seyam RM, Alkhudair WK, Kattan SA,
Alotaibi MF, Alzahrani HM and Altaweel WM: The risks of renal
angiomyolipoma: Reviewing the evidence. J Kidney Cancer VHL.
4:13–25. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Katabathina VS, Garg D, Prasad SR and
Vikram R: Cystic renal neoplasms and renal neoplasms associated
with cystic renal diseases in adults: cross-sectional imaging
findings. J Comput Assist Tomogr. 36:659–668. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Xu L, Liang S, Yan N, Zhang L, Gu H, Fei
X, Xu Y and Zhang F: Metastatic gastric cancer from breast
carcinoma: A report of 78 cases. Oncol Lett. 14:4069–4077. 2017.
View Article : Google Scholar : PubMed/NCBI
|