Introduction
Colorectal cancer is the most common malignant tumor
in the digestive tract and has a high incidence (1). According to statistics, more than 8
million new colorectal cancer cases were reported worldwide in
2016, and the cumulative number has reached ~300 million (2). In colorectal cancer patients,
intestinal obstruction is a very common tumor complication, and
there are studies indicating that the risk of colorectal cancer
patients with intestinal obstruction is as high as 10–30% (3). The body of patients with colon cancer
is in a very weak state, the occurrence of intestinal obstruction
at this time causes acid-base imbalance, water and electrolyte
disorders, and intestinal surgery cannot be performed routinely
(4). Edema and hyperemia are common
in the intestinal tract of obstruction segment. Patients with acute
tumor condition can only be operated by stages, which not only
increases the risk and cost of surgery, but also has a great
negative effect on the prognosis of patients (5). According to statistics, the effective
cure rate of colorectal cancer patients with intestinal obstruction
is only 60–80% (6) and intestinal
obstruction is one of the main reasons for the poor prognosis of
colorectal cancer patients. In the face of this situation,
continuous research and development of colorectal cancer in clinic
can effectively improve the prognosis of patients with intestinal
obstruction. With the application of neoadjuvant chemotherapy, the
tumor focus is first reduced by chemotherapy, and then resected by
surgery, which can significantly improve the curative effect of the
patients (7). Trans-anal ileus
catheter and intestinal metal stent implantation are the latest
laparoscopic surgery adjuvant therapy, which can not only
effectively improve the tumor resection rate, but also greatly
increase the rate of primary intestinal anastomosis and they have
been proved to have a very high application value in obstructive
colorectal cancer (8–10). However, the application of trans-anal
ileus catheter and intestinal metal stent implantation in
obstructive colorectal cancer worldwide is mostly used as guidance
study (11,12), and a relatively rare comparison
exists of the exact curative effect between them. Since 2016,
Taizhou Hospital has popularized the use of trans-anal ileus
catheter, intestinal metal stent implantation combined with cancer
laparoscopic surgery and neoadjuvant chemotherapy in the treatment
of obstructive colorectal cancer patients, and has achieved
significant results. There is still controversy on surgical
treatment of obstructive colorectal cancer worldwide. To the best
of our knowledge, there is no accurate research to propose which
method is most suitable for patients with obstructive colorectal
cancer. Therefore, this study compared the clinical effects of
intestinal stent and trans-anal ileus catheter combined with
laparoscopic surgery and neoadjuvant chemotherapy respectively in
patients with obstructive colorectal cancer to provide reference
and guidance for the selection of surgical schemes for patients
with obstructive colorectal cancer.
Patients and methods
General data
Patients with obstructive colorectal cancer treated
in Taizhou Hospital of Zhejiang Province, Wenzhou Medical
University (Taizhou, China), from February 2016 to March 2017 were
selected for retrospective analysis. Inclusion criteria: Patients
in accordance with the clinical manifestations of colorectal cancer
and highly suspected as colorectal cancer in Taizhou Hospital of
Zhejiang Province, Wenzhou Medical University (13), after pathological biopsy, confirmed
as colorectal cancer with intestinal obstruction. Patients had
trans-anal ileus catheter and intestinal metal stent implantation
combined with laparoscopic surgery and neoadjuvant chemotherapy in
the hospital after diagnosis. Patients aged 30 to 70 years;
patients who were willing to cooperate with the medical staff, and
patients with complete records. Exclusion criteria: Patients with
other tumors; patients with cardiovascular and cerebrovascular
diseases; patients with severe cardiopulmonary dysfunction;
pregnant patients; patients with chemotherapy tolerance; patients
with physical disabilities; long-term bedridden patients; patients
with mental illness; patients transferred to hospital in midway;
patients who had received radiotherapy and chemotherapy before
admission. In total, 89 cases were selected, including 67 males and
22 females with an age range of 38–67 years and an average age of
51.69±10.77 years. Forty-nine of 89 patients treated with
intestinal metal stent implantation combined with laparoscopic
surgery and neoadjuvant chemotherapy were the stent group. The
other 40 cases treated with trans-anal ileus catheter combined with
laparoscopic surgery and neoadjuvant chemotherapy were the catheter
group.
This study was approved by the Ethics Committee of
Taizhou Hospital of Zhejiang Province, Wenzhou Medical University.
Patients who participated in this research, signed an informed
consent and had complete clinical data.
Methods
Study design
Two groups of patients underwent intestinal
obstruction surgery followed by tumor resection and chemotherapy
after surgery. The clinical efficacy and prognosis of the two
groups were compared after all courses of treatment.
Surgical protocol in the stent
group
The patients were placed in a left lateral decubitus
position. When the enteroscope entered the body and reached the
stenotic part, an expansion catheter was used to send the guide
wire into the stenotic part under X-ray monitoring. Appropriate
stent was chosen according to the length and width of the tumor
invading intestine (NDS-20-080-230; Beijing YuLongKeTai Trading
Co., Ltd., Beijing, China). A stent pusher was used to drive the
stent along the wire to the stenotic part, both ends exceeding the
narrow point at least by 2 cm. The changes of vital signs were
closely monitored after stent placement.
Surgical protocol in the catheter
group
Endoscopy entered into the obstruction for
angiography after lavage of obstruction of the distal intestinal.
If the contrast agent was unable to pass through the narrow area,
the catheter placement was abandoned, if it passed, the guide wire
was inserted from the biopsy hole, and through the narrow part
under X-ray monitoring. A clamp expander was inserted along the
guide wire and the enteroscope was pulled out. The intestinal
obstruction catheter (D1407-0518; Dalian Create Medic International
Trade Co., Ltd.) was inserted into the airbag near the narrow area
along the clamp expander, and the guide wire and the clamp expander
were pulled out to complete the catheter placement. The vital signs
of the patients were closely monitored after catheterization, and
warm saline 1000–1500 ml was used daily to wash the obstruction
catheter.
Laparoscopic surgery
All the patients were operated by physicians with
secondary senior professional title or above in Oncological Surgery
of the hospital. The stents in the stent group were removed with
tumor resection during surgery, and the catheters in the catheter
group were removed before the surgery.
Neoadjuvant chemotherapy regimen
MFOLFOX6 protocol was used, including oxaliplatin
(EB01714; Shanghai Shifeng Biological Technology Co., Ltd.) 85
mg/m2, intravenous drip, d1. Calcium folinate
(RB768; Shanghai GuangRui Biological Technology Co., Ltd.) 200
mg/m2, intravenous drip, d1. Fluorouracil for
injection (0597-5G; Qingdao Jisskang Biotechnology Co., Ltd.) 400
mg/m2, venous injection, d1. Then
fluorouracil 2.0 g/m2 was added to the chemotherapeutic
pump for 48 h intravenous drip, repeated every 2 weeks, and the
duration of chemotherapy was 2–3 months.
Observation indicators
Preoperative indicators: Clinical information such
as sex, age, tumor stage and differentiation degree of patients in
the two groups. Intraoperative indicators: The intestinal
preparation time, surgical duration, intraoperative blood loss and
open surgery rate (open surgery was performed when the tumor was
not completely resected by laparoscopic surgery) of patients in the
two groups were observed. Postoperative indicators: postoperative
exhaust time and adverse reaction rate (including postoperative
anastomotic fistula, incision infection and lower extremity venous
thrombosis). Prognostic indicators: All the patients were included
in prognostic follow-up of reexamination at 1 year in hospital to
record the local recurrence rate and incision tumor implantation
rate.
Statistical analysis
The data were analyzed and processed by SPSS 24.0
statistical software (Beijing Bizinsight Information Technology
Co., Ltd.). The enumeration data were expressed in the form of a
rate. Chi-square test was used for comparison between the groups.
The measured data were expressed as mean ± standard deviation, and
t-test was used for comparison between the two groups. P<0.05
was considered statistically significant.
Results
Preoperative indicators
There was no significant difference in age, body
weight, disease course, the count of platelet, erythrocytes and
leukocytes, time interval after stent/tube insertion, sex, smoking,
alcohol consumption, exercise habit, ethnicity, pathological stage,
lymphatic metastasis, differentiation, intestinal obstruction
degree, primary tumor, histological type and lymph node dissection
between the two groups (P>0.05), which proved that the two
groups were comparable (Table
I).
 | Table I.Clinical data comparison [n (%)]. |
Table I.
Clinical data comparison [n (%)].
| Factors | Stent group
(n=49) | Catheter group
(n=40) | χ2 or
t-test | P-value |
|---|
| Age | 50.64±11.57 | 51.04±10.62 | 0.168 | 0.867 |
| Body weight (kg) | 76.24±8.67 | 75.14±8.32 | 0.606 | 0.546 |
| BMI
(kg/m2) | 26.13±4.38 | 27.05±5.15 | 0.911 | 0.365 |
| Disease course
(weeks) | 3.17±0.54 | 3.22±0.50 | 0.449 | 0.655 |
| Platelet
(×109/l) | 228.21±50.14 | 220.42±57.21 | 0.684 | 0.684 |
| Erythrocyte
(×109/l) | 4.66±0.64 | 4.72±0.51 | 0.481 | 0.632 |
| Leukocyte
(×109/l) | 8.15±1.17 | 7.96±1.34 | 0.714 | 0.477 |
| Time interval after
stent/tube insertion (days) | 12.85±2.36 | 11.92±2.05 | 1.960 | 0.053 |
| Sex |
|
| 0.192 | 0.661 |
| Male | 36 (73.47) | 31 (77.50) |
|
|
|
Female | 13 (26.53) | 9 (22.50) |
|
|
| Smoking |
|
| 0.103 | 0.748 |
| Yes | 34 (69.39) | 29 (72.50) |
|
|
| No | 15 (30.61) | 11 (27.50) |
|
|
| Alcohol
consumption |
|
| 0.577 | 0.448 |
| Yes | 40 (81.63) | 30 (75.00) |
|
|
| No | 9 (18.37) | 10 (25.00) |
|
|
| Exercise habit |
|
| 0.197 | 0.657 |
| Yes | 5 (10.20) | 3 (7.50) |
|
|
| No | 44 (89.80) | 37 (92.50) |
|
|
| Ethnicity |
|
| 0.485 | 0.486 |
| Han | 47 (95.92) | 37 (92.50) |
|
|
|
Minority | 2 (4.08) | 3 (7.50) |
|
|
| Pathological
stage |
|
| 0.320 | 0.572 |
| Stage
I–II | 24 (48.98) | 22 (55.00) |
|
|
| Stage
III–IV | 25 (51.02) | 18 (45.00) |
|
|
| Lymphatic
metastasis |
|
| 0.529 | 0.467 |
| Yes | 17 (34.69) | 11 (27.50) |
|
|
| No | 32 (65.31) | 29 (72.50) |
|
|
| Differentiation
degree |
|
| 0.231 | 0.891 |
|
Well-differentiated | 27 (55.10) | 20 (50.00) |
|
|
|
Moderately differentiated | 12 (24.49) | 11 (27.50) |
|
|
| Poorly
differentiated | 10 (20.41) | 9 (22.50) |
|
|
| Intestinal
obstruction degree |
|
| 0.047 | 0.828 |
|
Complete | 32 (65.31) | 27 (67.50) |
|
|
|
Incomplete | 17 (34.69) | 13 (32.50) |
|
|
| Primary tumor |
|
| 0.041 | 0.839 |
| Colon
cancer | 21 (42.86) | 18 (45.00) |
|
|
| Rectal
cancer | 28 (57.14) | 22 (55.00) |
|
|
| Histological
type |
|
| 0.136 | 0.934 |
|
Adenocarcinoma | 20 (40.82) | 15 (37.50) |
|
|
|
Mucinous carcinoma | 19 (38.78) | 14 (35.00) |
|
|
|
Undifferentiated
carcinoma | 10 (20.41) | 9 (22.50) |
|
|
| Lymph node
dissection |
|
| 0.054 | 0.816 |
| Total
mesangiectomy | 16 (32.65) | 14 (35.00) |
|
|
| Local
excision | 33 (67.35) | 26 (65.00) |
|
|
| Open surgery
rate | 2 (4.08) | 3 (7.50) | 0.485 | 0.486 |
| Incision
infection | 3 (6.12) | 2 (5.00) |
|
|
| Anastomotic
fistula | 1 (2.04) | 2 (5.00) |
|
|
| Lower extremity
venous thrombosis | 1 (2.04) | 0 (0.00) |
|
|
| Abdominal
infection | 2 (4.08) | 2 (5.00) |
|
|
| Abdominal pain | 4 (8.16) | 3 (7.50) |
|
|
| Fever | 3 (6.12) | 4
(10.00) |
|
|
| Incidence of
adverse reactions (%) | 28.57 | 32.50 | 0.161 | 0.688 |
| Hepatic
metastases | 1 (2.04) | 0 (0.00) |
|
|
| Pulmonary
metastasis | 0 (0.00) | 1 (2.56) |
|
|
| Brain
metastases | 0 (0.00) | 1 (2.56) |
|
|
| Gastric
metastasis | 1 (2.04) | 0 (0.00) |
|
|
| Local recurrence
rate (%) | 4.26 | 5.13 | 0.037 | 0.848 |
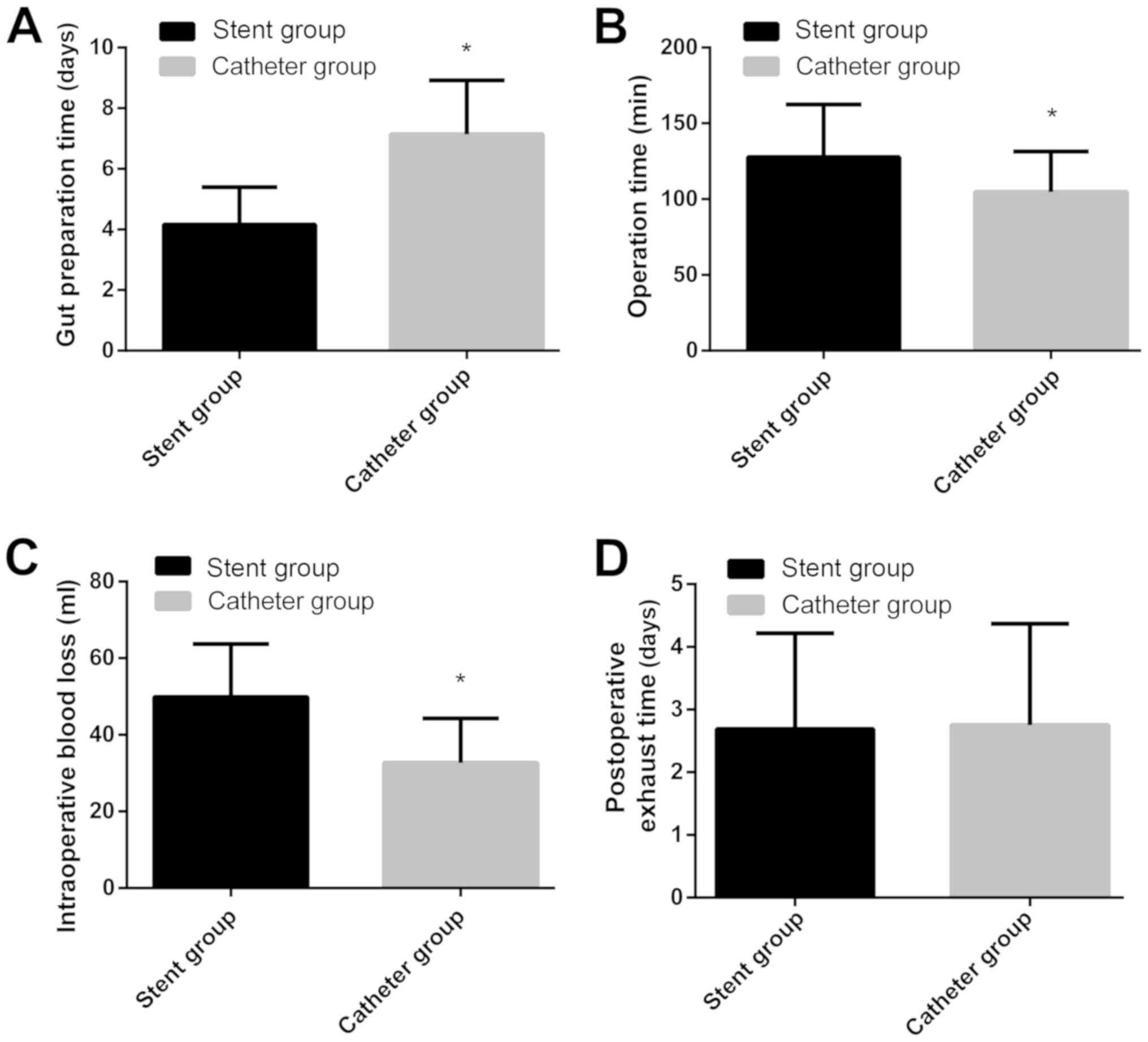
Intraoperative indicators
The intestinal preparation time in the stent group
(4.16±1.24 days) was shorter than that in the catheter group
(7.14±1.78 days) (P<0.001); The surgical duration in the stent
group (127.68±34.74 min) was longer than that in the catheter group
(104.67±26.77 min) (P<0.001). The intraoperative blood loss in
the stent group (49.87±13.81 ml) was higher than that in the
catheter group (32.73±11.57 ml) (P<0.001) (Fig. 1A-C). Two patients underwent open
surgery in the stent group, and the open surgery rate was 4.08%; 3
patients underwent open surgery in the catheter group, and the open
surgery rate was 7.50%. There was no significant difference in the
open surgery rate between the two groups (P>0.05) (Table II).
 | Table II.Open surgery rate comparison [n
(%)]. |
Table II.
Open surgery rate comparison [n
(%)].
| Factors | Stent group
(n=49) | Catheter group
(n=40) | χ2
test | P-value |
|---|
| Open surgery
rate | 2 (4.08) | 3 (7.50) | 0.485 | 0.486 |
| Incision
infection | 3 (6.12) | 2 (5.00) |
|
|
| Anastomotic
fistula | 1 (2.04) | 2 (5.00) |
|
|
| Lower extremity
venous thrombosis | 1 (2.04) | 0 (0.00) |
|
|
| Abdominal
infection | 2 (4.08) | 2 (5.00) |
|
|
| Abdominal pain | 4 (8.16) | 3 (7.50) |
|
|
| Fever | 3 (6.12) | 4
(10.00) |
|
|
| Incidence of
adverse reactions (%) | 28.57 | 32.50 | 0.161 | 0.688 |
| Hepatic
metastases | 1 (2.04) | 0 (0.00) |
|
|
| Pulmonary
metastasis | 0 (0.00) | 1 (2.56) |
|
|
| Brain
metastases | 0 (0.00) | 1 (2.56) |
|
|
| Gastric
metastasis | 1 (2.04) | 0 (0.00) |
|
|
| Local recurrence
rate (%) | 4.26 | 5.13 | 0.037 | 0.848 |
Postoperative indicators
The postoperative exhaust time in the stent group
was 2.69±1.53 days, which was not significantly different from that
in the catheter group (2.75±1.62 days) (P>0.05). In the stent
group, 6.12% (3 cases) of patients had incision infection; 2.04% (1
case) had anastomotic fistula; 2.04% (1 case) had lower extremity
venous thrombosis; 4.08% (2 cases) had abdominal infection; 8.16%
(4 cases) had abdominal pain; 6.12% (3 cases) had fever, and the
incidence of adverse reactions was 28.57% (14 cases). In the
catheter group, 5.00% (2 cases) of patients had incision infection;
5.00% (2 cases) had anastomotic fistula; 5.00% (2 cases) had
abdominal infection; 7.50% (3 cases) had abdominal pain; 10.00% (4
cases) had fever, and the incidence of adverse reactions was 32.50%
(13 cases). There was no significant difference in the incidence of
adverse reactions between the two groups (P>0.05) (Fig. 1D and Table II).
Prognostic indicators
Eighty-six of 89 subjects were followed up
successfully, and the success rate was 96.63%. Two participants
were lost to follow-up in the stent group and 1 case in the
catheter group. There was no incision tumor implantation in either
group. In the stent group, 2.13% (1 case) of patients had hepatic
metastasis, 2.13% (1 case) had gastric metastasis, and the local
recurrence rate was 4.26% (2 cases); In the catheter group, 2.56%
(1 case) of patients had pulmonary metastasis, 2.56% (1 1case) had
brain metastasis, and the local recurrence rate was 5.13% (2
cases). There was no significant difference in local recurrence
rate between the two groups (P>0.05) (Table II).
Discussion
There is a high probability of intestinal
obstruction in patients with colorectal cancer which may lead to
the reduction of resection rate, increase of intestinal orifice
rate, and a significant increase in risk of death after surgery
(14). Because of intestinal
obstruction, preoperative bowel preparation is not possible for
colorectal cancer patients. Patients were usually performed
proximal obstruction of intestinal fistula first and then resection
surgery, and an intestinal stoma reversion was conducted after the
surgery (15,16). Multiple trauma surgery causes more
damage to patients who are already suffering from cancer, and the
sequelae of trauma surgery multiplies (17,18).
With the widespread use of endoscopic stents and trans-anal ileus
catheterization in recent years, the clinical efficacy of patients
with obstructive colorectal cancer has significantly improved. At
present, endoscopic stent and trans-anal ileus catheterization
combined with laparoscopic surgery in the treatment of obstructive
colorectal cancer has achieved significant research results, which
has great value in improving the success rate of the surgery of
obstructive colorectal cancer. Through endoscopic stent and
trans-anal ileus catheterization, the intestinal obstruction of
colorectal cancer patients can be relieved by non-operative method
(19,20), which makes the tumor resection
surgery standard, and not only greatly increase the success rate of
resection surgery, but also effectively improve the prognosis of
patients.
The clinical value of endoscopic stent and
trans-anal ileus catheterization combined with neoadjuvant
chemotherapy in laparoscopic resection of obstructive colorectal
cancer was compared in this study, and the results showed that the
intestinal preparation time in the stent group was shorter than
that in the catheter group, which indicated that endoscopic stent
was more effective than trans-anal ileus catheterization in
relieving intestinal obstruction. The reason might be that the
small diameter of trans-anal ileus catheter, the poor effect of
defecation rate, disunited defecation of patients and higher stool
hardness in some patients can cause intestinal catheter
obstruction, resulting in the intestinal preparation time in the
catheter group being longer than the stent group. However, the
surgical duration and the intraoperative blood loss in the stent
group were higher than those in the catheter group, which suggested
that trans-anal ileus catheter had higher surgical safety than
endoscopic stent in patients with obstructive colorectal cancer.
The reason was that intestinal stents might lead to intestinal
perforation and bleeding, and stent displacement might lead to
abnormal intestinal metabolism in patients (18). During the operation, the doctor not
only needs to remove the tumor focus completely, but must also
remove the implanted stent, which would take more time and blood
loss during the surgery than in the catheter group. Catheterization
could indirectly improve intestinal edema and intestinal wall blood
flow in patients (21). The catheter
is removed preoperatively, allowing the doctor to focus on the
removal of the tumor during the surgery. Smooth environment of the
patient's intestine is beneficial to surgery. There was no
significant difference in open surgery rate, postoperative adverse
reactions, exhaust time and prognosis between the two groups, which
indicated that trans-anal ileus catheter and endoscopic stent had
high application value in patients with obstructive colorectal
cancer. Because of the presence of intestinal obstruction, patients
with obstructive colorectal cancer usually need to wash their
intestines before and after surgery the intestine is the largest
digestive organ in the human body, which contains a large amount of
feces and bacteria. Once the bacteria invade the body during
surgery, it is easy to cause infection, which directly results in
the decrease of the immune function of the patients, causes
postoperative complications and affects the prognosis. The
intestinal function of patients can be improved effectively with
trans-anal ileus catheter and endoscopic stent, and combined with
intravenous parenteral nutrition intervention can obtain effective
nutritional support after surgery, improve the stability and
balance of intestinal tract, reduce the occurrence of postoperative
adverse reactions, and greatly improve the prognosis of
patients.
The purpose of this study was to compare the
clinical efficacy of trans-anal ileus catheter and endoscopic stent
in patients with obstructive colorectal cancer, but there were
still some shortcomings due to the limited experimental conditions.
The number of subjects studied was small and the population was
relatively uniform. The materials of intestinal obstruction stents
are varied. The stents used in this study were all made of metal
materials, which did not exclude the possible differences in the
efficacy of other materials (such as stainless steel and
nickel-titanium alloy). A longer-term follow-up survey of the
subjects in this study will be conducted.
In conclusion, intestinal metal stent implantation
can effectively relieve intestinal obstruction, while trans-anal
ileus catheter offers higher safety in laparoscopic surgery. Their
combination with neoadjuvant chemotherapy and laparoscopic surgery
for obstructive colorectal cancer has high value and good clinical
effect. The best treatment plan should be selected according to the
patient's condition.
Acknowledgements
Not applicable.
Funding
This study was supported by Taizhou Science and
Technology Project. (no. 1701KY07).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LY and WM designed the study and drafted the
manuscript. LY, MW and RZ acquired the data. WM, TB and SZ analyzed
the data and revised the manuscript. All the authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Taizhou Hospital of Zhejiang Province, Wenzhou Medical University
(Taizhou, China). Patients who participated in this research,
signed an informed consent and had complete clinical data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD, Fedewa SA, Ahnen DJ,
Meester RG, Barzi A and Jemal A: Colorectal cancer statistics,
2017. CA Cancer J Clin. 67:177–193. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Arnold M, Sierra MS, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global patterns and trends in
colorectal cancer incidence and mortality. Gut. 66:683–691. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Takahashi H, Okabayashi K, Tsuruta M,
Hasegawa H, Yahagi M and Kitagawa Y: Self-expanding metallic stents
versus surgical intervention as palliative therapy for obstructive
colorectal cancer: A meta-analysis. World J Surg. 39:2037–2044.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Atsushi I, Mitsuyoshi O, Kazuya Y, Syuhei
K, Noriyuki K, Masashi M, Akira W, Kentaro S, Nobuyuki K, Natsuko
S, et al: Long-term outcomes and prognostic factors of patients
with obstructive colorectal cancer: A multicenter retrospective
cohort study. World J Gastroenterol. 22:5237–5245. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kegler MC, Beasley DD, Liang S, Cotter M,
Phillips E, Hermstad A, Williams R, Martinez J and Riehman K: Using
the consolidated framework for implementation research to
understand safety net health system efforts to increase colorectal
cancer screening rates. Health Educ Res. 33:315–326. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Baer C, Menon R, Bastawrous S and
Bastawrous A: Emergency presentations of colorectal cancer. Surg
Clin North Am. 97:529–545. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Khoo E, O'Neill S, Brown E, Wigmore SJ and
Harrison EM: Systematic review of systemic adjuvant, neoadjuvant
and perioperative chemotherapy for resectable colorectal-liver
metastases. HPB (Oxford). 18:485–493. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kwak MS, Kim WS, Lee JM, Yang DH, Yoon YS,
Yu CS, Kim JC and Byeon JS: Does stenting as a bridge to surgery in
left-sided colorectal cancer obstruction really worsen oncological
outcomes? Dis Colon Rectum. 59:725–732. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Haraguchi N, Ikeda M, Miyake M, Yamada T,
Sakakibara Y, Mita E, Doki Y, Mori M and Sekimoto M: Colonic
stenting as a bridge to surgery for obstructive colorectal cancer:
Advantages and disadvantages. Surg Today. 46:1310–1317. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cézé N, Charachon A, Locher C, Aparicio T,
Mitry E, Barbieux JP, Landi B, Dorval E, Moussata D and Lecomte T:
Safety and efficacy of palliative systemic chemotherapy combined
with colorectal self-expandable metallic stents in advanced
colorectal cancer: A multicenter study. Clin Res Hepatol
Gastroenterol. 40:230–238. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miłek T and Ciostek P: Implantation of a
new enteral stent in obstructive colorectal cancer using
interventional radiology in patients over 70 years of age.
Wideochir Inne Tech Malo Inwazyjne. 10:155–160. 2015.PubMed/NCBI
|
|
12
|
Kim EJ and Kim YJ: Stents for colorectal
obstruction: Past, present, and future. World J Gastroenterol.
22:842–852. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
De Rosa M, Pace U, Rega D, Costabile V,
Duraturo F, Izzo P and Delrio P: Genetics, diagnosis and management
of colorectal cancer (Review). Oncol Rep. 34:1087–1096. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mattar RE, Al-Alem F, Simoneau E and
Hassanain M: Preoperative selection of patients with colorectal
cancer liver metastasis for hepatic resection. World J
Gastroenterol. 22:567–581. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Enomoto T, Saida Y, Takabayashi K, Nagao
S, Takeshita E, Watanabe R, Takahashi A, Nakamura Y, Asai K,
Watanebe M, et al: Open surgery versus laparoscopic surgery after
stent insertion for obstructive colorectal cancer. Surg Today.
46:1383–1386. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yamada T, Okabayashi K, Hasegawa H,
Tsuruta M, Yoo JH, Seishima R and Kitagawa Y: Meta-analysis of the
risk of small bowel obstruction following open or laparoscopic
colorectal surgery. Br J Surg. 103:493–503. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cetinkaya E, Dogrul AB and Tirnaksiz MB:
Role of self expandable stents in management of colorectal cancers.
World J Gastrointest Oncol. 8:113–120. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zullig LL, Smith VA, Jackson GL, Danus S,
Schnell M, Lindquist J, Provenzale D, Weinberger M, Kelley MJ and
Bosworth HB: Colorectal cancer statistics from the veterans affairs
central cancer registry. Clin Colorectal Cancer. 15:e199–e204.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Shimizu H, Yamazaki R, Ohtsuka H, Osaka I,
Takuma K and Morita Y: Feasibility of laparoscopic surgery after
stent insertion for obstructive colorectal cancer. Asian J Endosc
Surg. 11:118–122. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Park SJ, Lee KY, Kwon SH and Lee SH:
Stenting as a bridge to surgery for obstructive colon cancer: Does
it have surgical merit or oncologic demerit? Ann Surg Oncol.
23:842–848. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang N, Zhou ZL and Xie JL: Application
of transanal ileus tube in acute obstructive left-sided colorectal
cancer. Int J Clin Exp Med. 8:14024–14029. 2015.PubMed/NCBI
|