Introduction
Melasma is an acquired disorder of hyperpigmentation
that typically presents as symmetric hyperpigmented macules on the
sun-exposed areas of skin, especially on the face (1). Although no race is spared, melasma is
particularly common in women at the reproductive age whose skin
types are Fitzpatrick III–V. Chronic sunlight exposure, genetic
factors, pregnancy, and sex hormones are generally believed to be
related to the occurrence of melasma (2). Moreover, improper use of cosmetic and
over-scrubbing of the face have been proposed (3), but the pathogenesis and etiology of
melasma have not yet been fully elucidated.
The treatment of melasma is challenging and
difficult since it is refractory and patients often suffer relapse.
Currently, the 1064-nm, low-fluence Q-switched neodymium-doped
yttrium aluminum garnet [QS Nd:YAG (QSNY)] laser is a commonly used
laser treatment of melasma. The ‘laser toning’ technique was used
for melasma treatment, and most of the studies have been conducted
in Asians (4–6). The technique includes large spot sizes,
low fluences, and multiple passes, and it is performed in five to
ten sessions at weekly to monthly interval. Subcellular-selective
photo-thermolysis was described as the mechanism that selectively
destroyed melanin while melanocytes were kept intact (7,8). Mild
treatment, lower incidence of complications and minimal downtime
are the advantages of this laser therapy.
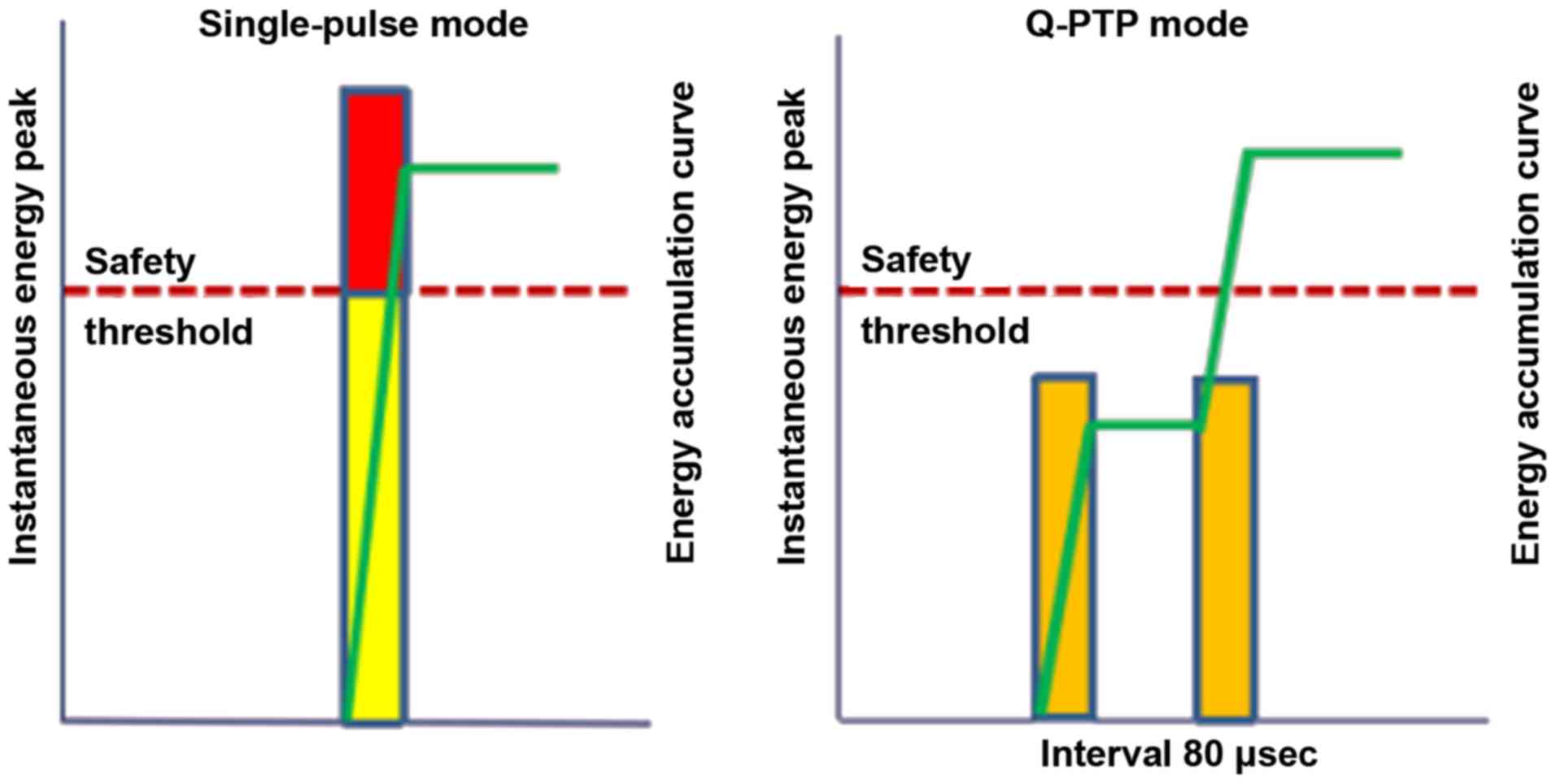
Quickly-pulse-to-pulse (Q-PTP) is the latest dual
pulse mode QS Nd:YAG laser technology that improves efficacy and
minimizes side effects by creating higher peak energy and more
effective photo-mechanical destruction of melanin particles
(Fig. 1). There are some previous
reports regarding the efficacy and safety of low-fluence Nd:YAG
laser therapy for melasma, but few studies have explored the laser
toning with Q-PTP laser mode (9,10).
We performed a prospective split-face study to
compare the degree of improvement and side effects of different
modes of laser toning with 1064-nm QS Nd:YAG laser in the treatment
of melasma. The aim of this study was to explore the advantages,
efficacy, and safety of laser toning with Q-PTP mode in treating
melasma in Chinese patients.
Patients and methods
Patients
From March 2016 to March 2017, twelve healthy women
ageed from 29 to 45 years with mild to severe symmetrical melasma
with skin types III or IV were consecutively enrolled. Subjects
were recruited from the Outpatient Department of Dermatology and
Aesthetic Surgery in Zhongshan Second People's Hospital (Zhongshan,
China). The exclusion criteria ruled out women with pregnancy or
breast feeding, any hormonal therapy, laser or intense pulsed light
therapy in the past 3 months, using topical bleaching agents in the
past 3 months, other medication treatments in the past 3 months,
inflammatory disease of the facial skin, history of
photosensitivity-related disorders, and over-expectation of the
treatment. QS 1064-nm Q-PTP laser mode was used to treat the right
side of the faces of the patients, while the single-pulse was used
on the left sides and the pre-treatment as control.
We explained the procedures, benefits, risks and
potential complications of the procedure to all the subjects.
Written informed consent was obtained from all patients or
guardians before the enrollment in accordance with the Declaration
of Helsinki. This clinical study was approved by the Ethics
Committee of Zhongshan Second People's Hospital. The patients
provided consent for the data to be published.
Laser treatment
This was a random study. The skin was cleansed using
a mild cleanser before treatment. Standard digital photographs
(Canon EOS 600D) were taken from the front and side of both cheeks
before and after each treatment session.
All subjects were assigned to the split-face study,
and treated with 1064-nm QS Nd:YAG laser (Spectra
VRMIII®, Lutronic Corp.), collimated homogeneous
flat-top beam profile, 5–7 nsec pulse width and 7 mm spot size.
Q-PTP and single-pulse laser mode were applied to the treatment
side and the control side, respectively. The fluence was 1.8
J/cm2 (0.9 J/cm2 each sub-pulse in Q-PTP
mode), and the treatments were repeated with 1,600 spots each side
with appropriate overlap (approximately 10%), regardless of the
development of erythema and swelling. The treatment was
administered for a total of five sessions at 4-week intervals. A
cooling collagen containing mask was applied after each session. To
ensure consistency, all laser treatments were performed by the same
therapist. Patients were followed up at the 4th and 12th week after
the final laser treatment.
Broad-spectrum Sunscreen with a sun protection
factor (SPF) 30+ and protection Ultraviolet A (PA)+++ was
instructed to be used on the whole face to avoid direct sun
exposure during the entire study period.
Immediate post-treatment
assessment
The patients and assessors were double-blinded. The
degree of erythema and the procedural pain were evaluated
immediately after the first treatment session in each side treated
with QS 1064-nm Q-PTP and single-pulse modes, by two assessors (one
dermatologist and one plastic surgeon), independently. Patients
were asked to rate treatment pain and chose a number that
represents their pain on both sides of the face based on a
numerical rating scale range 0–10 (0, no pain; 10, worst pain).
Pain scores were divided into four grades: 0, none (0); 1, mild
(1–3); 2, moderate (4–6); and 3,
severe (7–10). Skin erythema reaction assessment was
performed using a clinical assessment scale of 0, none; 1, mild; 2,
moderate; and 3, severe (swelling, petechiae, and other serious
skin reactions).
Clinical efficacy
Two assessors (one dermatologist and one plastic
surgeon) evaluated each half of the face used a modified melasma
area and severity index (mMASI) score based on the patients' photos
at baseline and after the final laser treatment at the 4th and 12th
week follow-up. The mMASI was used to score patients melasma based
on the percentage of the total area (A), darkness (D), and
homogeneity (H) of pigment lesions involving the forehead, cheek,
and chin on each side of the face. The sum of the severity grade
used three factors and the calculations as shown in Table I.
 | Table I.Modified melasma area and severity
index (mMASI) score. |
Table I.
Modified melasma area and severity
index (mMASI) score.
|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 |
|---|
| Area (A) | 0% | 1-9% | 10-29% | 30-49% | 50-69% | 70-89% | 90-100% |
| Darkness (D) | Absent | Slight | Mild | Marked | Severe |
|
|
| Homogeneity (H) | Absent | Slight | Mild | Marked | Severe |
|
|
| MASI = Area ×
(Darkness of pigment + Homogeneity) |
| Modified MASI score =
(f) 0.15A(D+H) + (m) 0.3A(D+H) + (c) 0.05A(D+H)a |
Physician's global assessment
Two blinded assessors (one dermatologist and one
plastic surgeon) assessed the results of treatment based on the
patients' photos. A six-grade VAS (visual analog scale) assessment
was designed to compare four weeks' follow-up records with the
baseline, and melasma clearance on both sides of the face.
Improvement of melasma as follows: excellent (melasma clearance
>75%); good (melasma clearance 50–75%); moderate (melasma
clearance 25–50%); minimal (melasma clearance <25%); unchanged
(no clearance); worsening (complications occurred).
Patients' self-assessment
Patients' subjective satisfaction with the results
rated through photos, using the same six-grade VAS assessment.
Safety assessment and recurrence
At each treatment and follow-up, adverse events (AE)
of patients were recorded. If adverse effects were detected, they
were treated promptly. At the same time, other side effects and
complications were recorded during and after the study including
swelling, petechiae, burning, itching, facial dryness,
hyperpigmentation and hypopigmentation or punctate leucoderma.
Patients were asked to use sun protection and avoid
sunlight exposure to reduce the effect of the sunlight on
treatment. At the 4th and 12th-week follow-up visits after the
final laser treatment, increase of the lesions or worsening of
hyperpigmentation was considered as a recurrence.
Statistical analysis
Data statistical analysis was conducted with
Statistical Package for Social Sciences (SPSS) software version
19.0 (IBM Corporation). mMASI scores were reported as the means ±
standard deviation. A paired t-test was used to compare mMASI
reductions. Differences in grades of procedural pain, skin erythema
reaction, physician and patients' self-assessments of both sides of
the face were tested using the Wilcoxon signed-rank test, before
and after the therapy. Two-tailed P<0.05 was considered to
indicate a statistically significant difference.
Results
Procedural pain and skin erythema
assessment
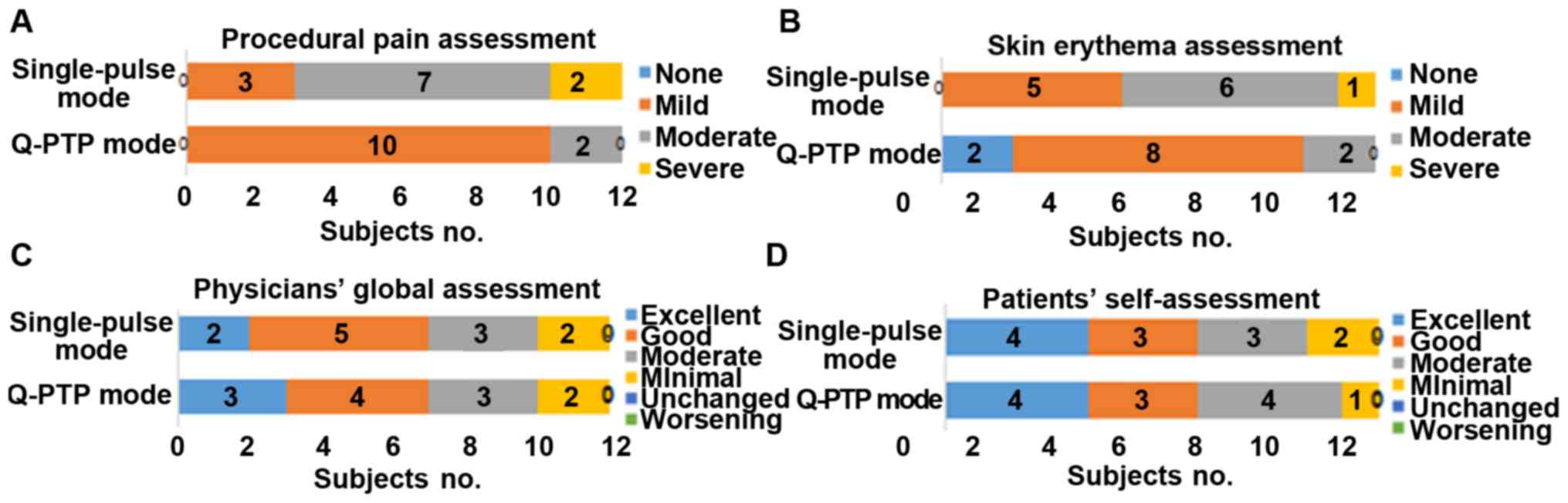
Treatment pain scores in QS 1064-nm Q-PTP and
single-pulse laser mode applied to the treatment side and the
control side, respectively, were none (0 vs. 0), mild (10 vs. 3),
moderate (2 vs. 7) and severe (0 vs. 2) (Fig. 2A). There was a statistically
significant difference (P<0.05). All the patients felt a
different degree of pain on both sides during laser treatment,
which was described as tingling sensation. Minor pain experience
and better patient acceptance were reported in the Q-PTP laser mode
treatment side. Q-PTP laser mode was significantly superior to
single-pulse laser mode in procedural pain assessment and skin
erythema assessment (Fig. 2).
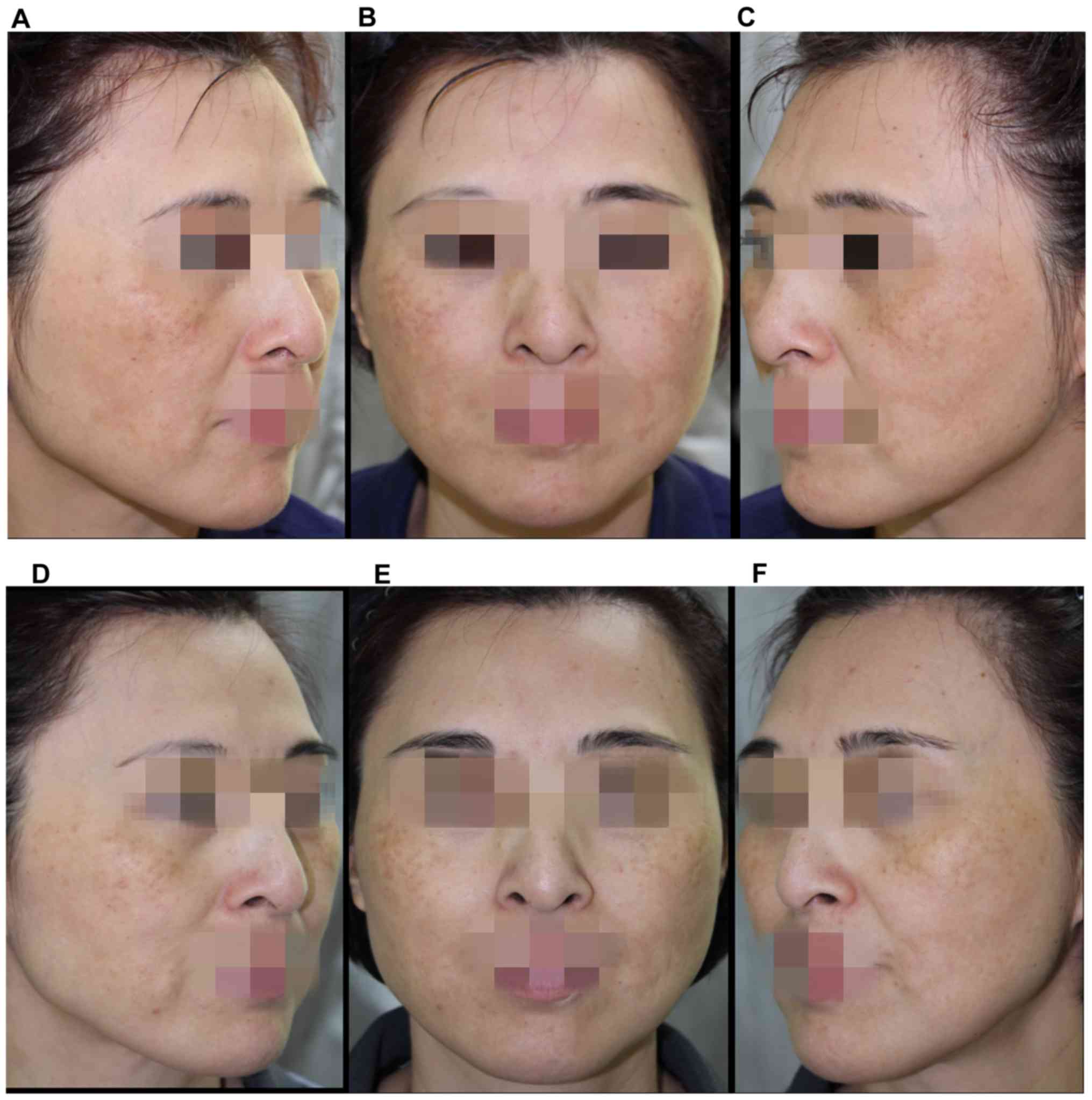
Post-treatment skin erythema assessment was
performed using a clinical assessment scale by two assessors.
Results in each side treated with QS 1064-nm Q-PTP and single-pulse
laser mode, respectively, were none (2 vs. 0), mild (8 vs. 5),
moderate (2 vs. 6), and severe (0 vs. 1) (Fig. 2B). There was a statistically
significant difference (P<0.05). Compared with before treatment
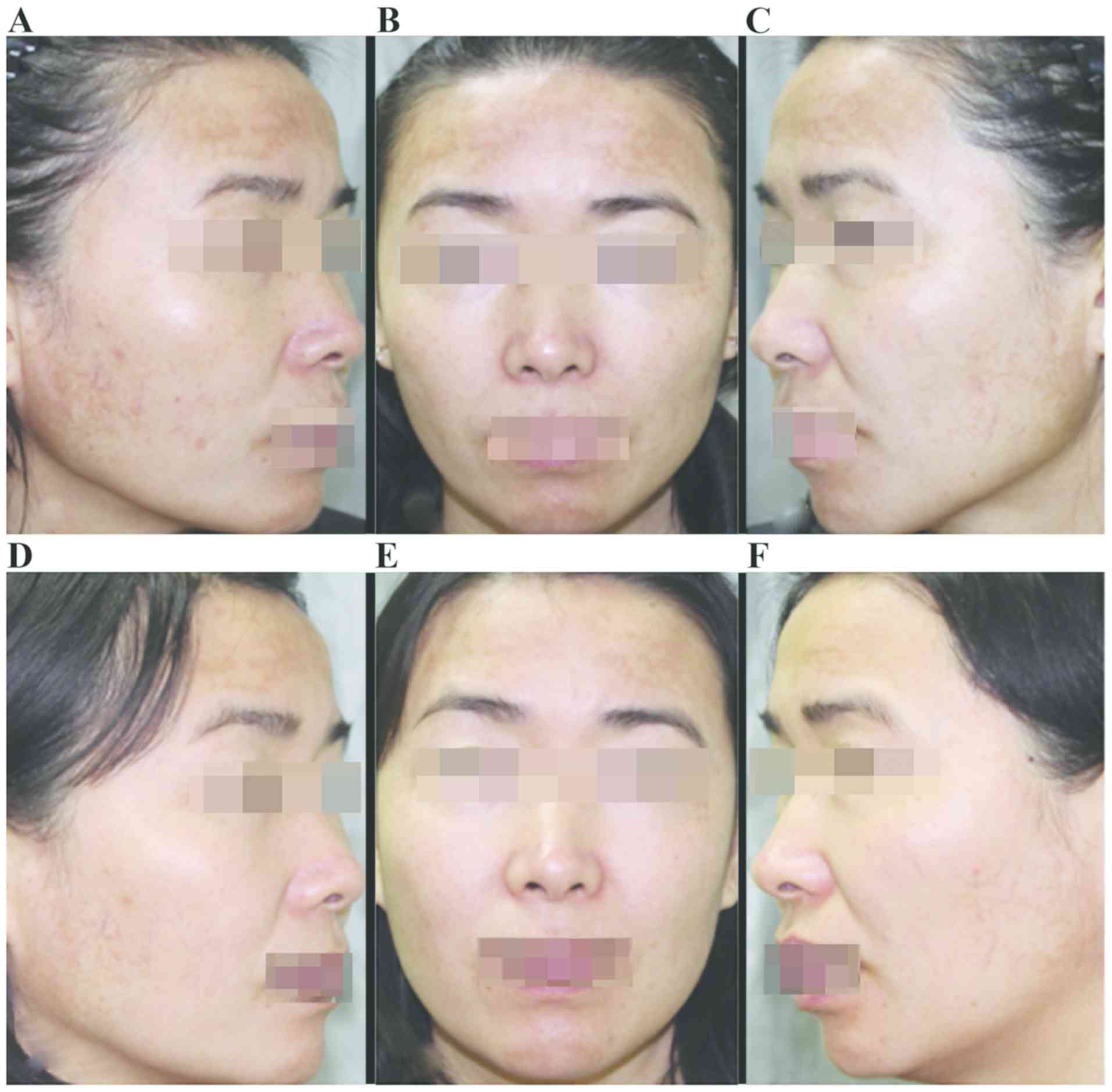
(Fig. 3A-C), lesser skin erythema
was observed in Q-PTP laser mode treatment after the treatment
(Figs. 3D-F and 4).
Modified melasma area and severity
index (mMASI)
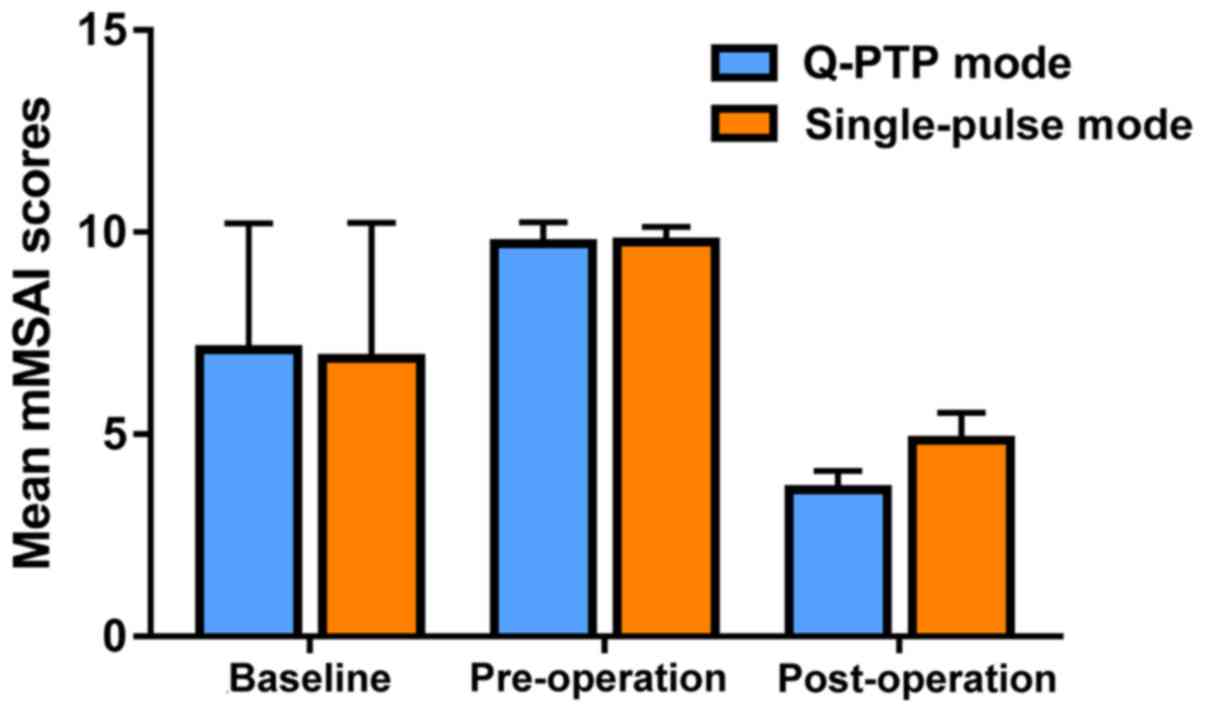
The mean mMASI score of each side of the face showed
improvement after the final laser treatment at the 4th and
12th-week follow-up visit compared to baseline (Fig. 5). Baseline mMASI scores were
7.09±3.13 on the side of the the face treated with Q-PTP mode and
6.89±3.35 on the other side treated with single-pulsed mode. There
was no significant difference between the two sides (P>0.05). At
the 4th week of follow-up, the mMASI scores were changed to
2.69±2.32 on the Q-PTP side and 2.75±2.38 on the single-pulsed
side. mMASI scores were 2.97±2.52 and 3.03±2.37 on the Q-PTP and
single-pulsed side, respectively, at the 12th week of follow-up.
The mMASI score was 3 when the melasma lesion clearance was 50%. In
our study, 7 out of 12 patients had mMASI scores of less than 3.
Mean mMASI scores were decreased significantly, as compared to the
baseline on both sides (P<0.05). However, the difference in
mMASI scores between the two laser modes was not statistically
significant (P>0.05).
Physician's global assessment and
Patients' self-assessment
QS 1064-nm Q-PTP and single-pulse laser mode were
used to treat each half-face group, melasma improvement showed a
positive treatment efficacy at the 4th week follow-up, compared
with pre-treatment baseline (Figs. 6
and 7). The patient's satisfaction
was good. However, both sides of the same patient showed similar
therapeutic effect, with no statistical significance
(P>0.05).
In PGA, improvement of melasma treated with Q-PTP
and single-pulse laser mode was as follows: excellent (3 vs. 2);
good (4 vs. 5); moderate (3 vs. 3); minimal (2 vs. 2); unchanged (0
vs. 0); worsening (0 vs. 0). Patients' self-assessment was as
follows: excellent (4 vs. 4); good (3 vs. 3); moderate (4 vs. 3);
minimal (1 vs. 2); unchanged (0 vs. 0); worsening (0 vs. 0)
(Fig. 2C and D).
Adverse effects and recurrence
One patient (approximately 8.33%) who was treated
with QS 1064-nm single-pulse modes experienced edema like acute
urticaria (wheal), little visible petechiae and severe skin
erythema for 24 h without specific treatment. Other serious
complications such as hyperpigmentation, hypopigmentation or
punctate leucoderma were not found in any other patient during the
treatment, except for tingling sensation and slight burning which
disappeared after a cooling collagen-containing mask was applied
for 20 min. Mild to moderate skin erythema in our study was
observed after the treatment session and disappeared in less than 2
h. Three patients (25%) had a relapse of the disease at the
12th-week follow-up visit.
Discussion
Melasma has a significant negative impact on the
quality of life because it is a refractory disease of pigmentation
disorders. Although there are still many challenges in the
treatment of melasma, some studies have shown efficacy of laser and
light therapy in the treatment of the disease (11–16).
Using Q-switched lasers for treating pigmentation disorders is
based on the theory of selective photothermolysis. The therapy
technique ‘laser toning’ is based on subcellular selective
photothermolysis (7,8) and its mechanism of action in melasma
remains unclear. Although the technique removed melanosomes without
damaging melanocytes, defects have been reported in the treatment
of melasma in recent literature (17–19).
In order to eliminate the disadvantages and risks in
the treatment of melasma, few side effects and good results of new
laser technology or treatment schedule are being explored (20–23).
Close attention should be paid to how to realize the balance of
‘thermal control’ to fit the target tissue in the laser and light
treatment of melasma. The therapy with minimal thermal damage to
melanocytes, achieves rapid elimination and metabolism rebalancing
of melanin. QS Nd:YAG laser, fractional-mode and PTP laser
technology as innovation was reported in recent studies. Q-PTP is
the latest dual-pulse mode QS Nd:YAG lasers technology in which one
pulse is split into successive two sub-pulses by very short
intervals (80 µsec, in our study) and two relatively weak energy
pulses are accumulated from photoacoustic to photothermal to
produce higher peak power than those produced by the current QS
single-pulse. Synergistic dual-pulse immediately led to pressure
changes and vibration of melanin, and peak energy was accumulated
to increase the temperature of the targets (20). Kim et al (24) conducted a study on the efficacy of
the QS 1064-nm Nd:YAG laser and found the shock-wave effect of
photoacoustic effectively destroys the melanin particles with less
thermal damage.
In this study, QS 1064-nm Nd:YAG laser Q-PTP and
single-pulse mode were used to treat each half-face of the
patients. Melasma improvement showed treatment efficacy at the 4th
week of follow-up, more than 50% of patients had higher lesion
clearance compared with pre-treatment baseline. The patient's
satisfaction was good. No serious complications were found in any
of the patients during or after treatment. From baseline to the 4th
week of follow-up after the final laser treatment, the mean mMASI
scores showed a 62% reduction for the side of the face treated with
Q-PTP mode vs. a 60% reduction for the single-pulsed mode. This
difference in mMASI scores between the two laser modes was not
statistically significant. In the 12th week of follow-up after the
final laser treatment, there was a slight increase in mean mMASI
for both sides. However, similar to the results at the 4th week of
follow-up, both sides of the face still had a significant
improvement from baseline. At a histological level, Fontana-Masson
staining of the human skin revealed a similar effect of pigment
destruction across the same parameters used in both modes of the QS
1064-nm Nd:YAG laser (24). In our
study, the modified melasma area and severity index (mMASI) scores
were used to quantify pigmentation changes in each side of the
face.
Moreover, close attention was paid to procedural
pain and post-treatment skin erythema reaction. From the feedback
of the patients who had moderate to excellent improvement, we were
pleased to find that their facial skin tone became healthier and
brighter, and facial skin became smoother with better improvement
of pores and fine wrinkles, possibly result of the increased type
III collagen levels (24). Similar
to our findings, Jang et al (21) found that dual-pulsed and
single-pulsed 1064-nm QSNY laser modes improved melasma
significantly but modified MASI score, and L value (the value of
brightness in the CIELAB color system) was not significantly
different. Lesser pain and shorter duration of post-laser erythema
were observed with the dual-pulsed mode. Compared to the
single-pulsed laser mode, fewer side effects combined with similar
efficacy may lead to Q-PTP being the preferred choice, especially
pain sensitive skin types in patients with melasma or pain
sensitive parts of the face such as periorbital treatment. Kim
et al (24) observed by
electron microscopy that dual-pulsed mode exhibited gentle
treatment delivery on the basis of less epidermal keratinocytes and
melanocytes damage. The relative lower expression levels of
protease-activated receptors-2, pro-inflammatory transcription
factors and pro-inflammatory cytokines were found in dual-pulsed
mode compared to the conventional mode. High expression of the
factors would cause skin erythema/inflammation or result to
dyspigmentation.
Our study was conducted in southern China, although
patients were required to use uniform sunscreen and given guidance
on avoiding sunlight exposure, the patients' individual differences
inevitably affected the treatment outcome. Three patients had a
relapse of the disease at the 12th week of follow-up. However,
there was no significant difference on either side of the face. We
believe that a larger sample would be needed to analyze the
recurrence of melasma. One patient suffered a relapse due to a
severe facial allergy for nine weeks after laser surgery, one case
was the result of sun exposure with outdoor working environment,
and one may be due to the daily bad skin care habits causing skin
rubbing damage. In our clinical practice, we found that
epidemiological changes in the etiology of melasma. Improper skin
care and the use of cosmetics lead to skin barrier damage, and
adversely affect the occurrence and development of melasma.
Impaired stratum corneum integrity and a delayed barrier recovery
rate in melasma skin were reported by Lee et al (25).
The current treatment of melasma is still a
comprehensive treatment and sequential treatment, and treatment
schedule is adjusted according to the different conditions of the
skin lesions. For the purpose of a comparative study, a laser
monotherapy to treat melasma was applied. The number of research
samples is small and the follow-up time is short, which are the
limitations of our study. From the view of improving psychological
condition through rapid reduction of pigment lesions, laser therapy
is an indispensable treatment method as part of a comprehensive
treatment program.
In conclusion, current laser physics technology and
treatment strategy in laser therapy of melasma were explored. As a
new technology of QS Nd:YAG laser, Q-PTP is a technical
optimization of laser therapy in the treatment of melasma. Although
there was no significant difference in the treatment outcome with
the same treatment parameters, a minor procedural pain experience,
lesser skin erythema reaction posttreatment and better patient
acceptance demonstrate greater treatment safety and superiority
than the current QSNY laser.
Acknowledgements
Not applicable.
Funding
This study was supported by the Science and
Technology Program of Zhongshan under grant (no. 2017B1075).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XG conceived and designed the study and provided
statistical methods. XC and YJ worked on laser treatment and
post-treatment assessment. TZ and BW were responsible for
physician's global assessment. QL helped with safety assessment.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Zhongshan Second People's Hospital (Zhongshan, China). Patients who
participated in this research, had complete clinical data. Signed
informed consents were obtained from the patients or the
guardians.
Patient consent for publication
The patients provided consent for the data to be
published.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sarkar R, Gokhale N, Godse K, Ailawadi P,
Arya L, Sarma N, Torsekar RG, Somani VK, Arora P, Majid I, et al:
Medical management of melasma: A review with consensus
recommendations by Indian pigmentary expert group. Indian J
Dermatol. 62:558–577. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ortonne JP, Arellano I, Berneburg M,
Cestari T, Chan H, Grimes P, Hexsel D, Im S, Lim J, Lui H, et al: A
global survey of the role of ultraviolet radiation and hormonal
influences in the development of melasma. J Eur Acad Dermatol
Venereol. 23:1254–1262. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wu S, Shi H, Wu H, Yan S, Guo J, Sun Y and
Pan L: Treatment of melasma with oral administration of tranexamic
acid. Aesthetic Plast Surg. 36:964–970. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kauvar AN: Successful treatment of melasma
using a combination of microdermabrasion and Q-switched Nd:YAG
lasers. Lasers Surg Med. 44:117–124. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wattanakrai P, Mornchan R and Eimpunth S:
Low-fluence Q-switched neodymium-doped yttrium aluminum garnet
(1,064 nm) laser for the treatment of facial melasma in Asians.
Dermatol Surg. 36:76–87. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zhou X, Gold MH, Lu Z and Li Y: Efficacy
and safety of Q-switched 1,064-nm neodymium-doped yttrium aluminum
garnet laser treatment of melasma. Dermatol Surg. 37:962–970. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mun JY, Jeong SY, Kim JH, Han SS and Kim
IH: A low fluence Q-switched Nd:YAG laser modifies the 3D structure
of melanocyte and ultrastructure of melanosome by
subcellular-selective photothermolysis. J Electron Microsc (Tokyo).
60:11–18. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kim JH, Kim H, Park HC and Kim IH:
Subcellular selective photothermolysis of melanosomes in adult
zebrafish skin following 1064-nm Q-switched Nd:YAG laser
irradiation. J Invest Dermatol. 130:2333–2335. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Na SY, Cho S and Lee JH: Intense pulsed
light and low-fluence Q-switched Nd:YAG laser treatment in melasma
patients. Ann Dermatol. 24:267–273. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sim JH, Park YL, Lee JS, Lee SY, Choi WB,
Kim HJ and Lee JH: Treatment of melasma by low-fluence 1064 nm
Q-switched Nd:YAG laser. J Dermatolog Treat. 25:212–217. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li YH, Chen JZ, Wei HC, Wu Y, Liu M, Xu
YY, Dong GH and Chen HD: Efficacy and safety of intense pulsed
light in treatment of melasma in Chinese patients. Dermatol Surg.
34:693–701. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tian WC: Novel technique to treat melasma
in Chinese: The combination of 2940-nm fractional Er:YAG and
1064-nm Q-switched Nd:YAG laser. J Cosmet Laser Ther. 18:72–74.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Geddes ER, Stout AB and Friedman PM:
Retrospective analysis of the treatment of melasma lesions
exhibiting increased vascularity with the 595-nm pulsed dye laser
combined with the 1927-nm fractional low-powered diode laser.
Lasers Surg Med. 49:20–26. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cheng CY, Huang YL, Lee MC, Chang SL, Lin
YF and Hu S: Pulsed alexandrite laser for treatment of melasma in
Asian patients. J Cosmet Laser Ther. 19:210–214. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tong LG, Wu Y, Wang B, Xu XG, Tu HD, Chen
HD and Li YH: Combination of fractional QSRL and IPL for melasma
treatment in Chinese population. J Cosmet Laser Ther. 19:13–17.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sugawara J, Kou S, Kou S, Yasumura K,
Satake T and Maegawa J: Influence of the frequency of laser toning
for melasma on occurrence of leukoderma and its early detection by
ultraviolet imaging. Lasers Surg Med. 47:161–167. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gokalp H, Akkaya AD and Oram Y: Long-term
results in low-fluence 1064-nm Q-Switched Nd:YAG laser for melasma:
Is it effective? J Cosmet Dermatol. 15:420–426. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hofbauer Parra CA, Careta MF, Valente NY,
de Sanches Osório NE and Torezan LA: Clinical and histopathologic
assessment of facial melasma after low-fluence Q-switched
neodymium-doped yttrium aluminium garnet laser. Dermatol Surg.
42:507–512. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ryu HJ and Kim J: A case of mottled
hypopigmentation after low-fluence 1,064-nm Q-switched
neodymium-doped yttrium aluminum garnet laser therapy. J Cosmet
Laser Ther. 15:290–292. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim JY, Choi M, Nam CH, Kim JS, Kim MH,
Park BC and Hong SP: Treatment of melasma with the photoacoustic
twin pulse mode of low-fluence 1,064 nm Q-switched Nd:YAG laser.
Ann Dermatol. 28:290–296. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Jang HW, Chun SH, Park HC, Ryu HJ and Kim
IH: Comparative study of dual-pulsed 1064 nm Q-switched Nd:YAG
laser and single-pulsed 1064 nm Q-switched Nd:YAG laser by using
zebrafish model and prospective split-face analysis of facial
melasma. J Cosmet Laser Ther. 19:114–123. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yue B, Yang Q, Xu J and Lu Z: Efficacy and
safety of fractional Q-switched 1064-nm neodymium-doped yttrium
aluminum garnet laser in the treatment of melasma in Chinese
patients. Lasers Med Sci. 31:1657–1663. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lee MC, Chang CS, Huang YL, Chang SL,
Chang CH, Lin YF and Hu S: Treatment of melasma with mixed
parameters of 1,064-nm Q-switched Nd:YAG laser toning and an
enhanced effect of ultrasonic application of vitamin C: a
split-face study. Lasers Med Sci. 30:159–163. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kim BW, Moon IJ and Chang SE: Cellular and
biomolecular comparison of a novel, dual-pulsed Q-switched 1064 nm
Nd:YAG laser with conventional Q-switched 1064 nm Nd:YAG laser.
Indian J Dermatol Venereol Leprol. 83:251–255. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lee DJ, Lee J, Ha J, Park KC, Ortonne JP
and Kang HY: Defective barrier function in melasma skin. J Eur Acad
Dermatol Venereol. 26:1533–1537. 2012.PubMed/NCBI
|