Introduction
The number of smokers is increasing with the
increase of modern life pressure (1). In daily social life, people are forced
to absorb second-hand smoke from people around them, and studies
have shown that the risk of being forced to absorb second-hand
smoke is much higher than that of normal smoking (2). Lung cancer has the highest mortality
and morbidity rates worldwide (3).
Patients with non-small cell lung cancer (NSCLC) account for
>80% of the total number of lung cancer patients (4), and lung adenocarcinoma is the most
common in NSCLC (5). Lung
adenocarcinoma has a high degree of malignancy, short survival time
and high mortality (6). Due to the
mild early symptoms that are difficult to detect, most lung
adenocarcinoma patients have entered advanced stage when diagnosed
(7). Clinically, chemotherapy is
still the preferred treatment regimen for patients with advanced
malignant tumors (8). However,
patients with malignant tumors, generally have reduced immune
function, with many adverse reactions to chemotherapeutics, and
often have limited tolerance and efficacy to the drugs (9).
As a receptor tyrosinase inhibitor against epidermal
growth factor, icotinib has high specificity for tyrosine kinase on
epidermal growth factor (10), which
prolongs the survival time of lung adenocarcinoma patients, but
drug resistance is prone to occur with prolonged treatment time
(11). Pemetrexed, a newly developed
anti-folate agent with multiple targets and few toxic and side
effects, can effectively inhibit tumor cell proliferation (12). At present, chemotherapeutics in
combination with platinum drugs is an often used standard
first-line chemotherapy regimen (13). Some studies have shown that the
efficacy of pemetrexed in combination with platinum drugs is
better, which can improve adverse reactions of drugs and clinical
efficacy, prolonging patients' survival time (14). In this study, the clinical efficacy
of icotinib and pemetrexed in combination with cisplatin in the
first-line treatment of lung adenocarcinoma was compared, and the
correlation of different treatment regimens with the prognosis and
survival of patients was evaluated.
Patients and methods
Experimental subjects
A retrospective analysis was performed in 132 lung
adenocarcinoma patients who were treated in the Affiliated Hospital
of Weifang Medical University (Weifang, China) from July 2010 to
July 2015. Among them, 69 patients were treated with icotinib as
the icotinib group, including 45 males and 24 females, aged 35–71
years, with an average age of (54.32±6.46) years. The other 63
patients were treated with pemetrexed as the pemetrexed group,
including 42 males and 21 females, aged 36–67 years, with an
average age of (53.85± 6.83) years.
Inclusion criteria were: i) Lung adenocarcinoma
patients (with stages IIIA, IIIB and IV) diagnosed by the pathology
department of the Affiliated Hospital of Weifang Medical University
and unable or unwilling to undergo operation, or recurrent patients
6 months after operation and radiotherapy and chemotherapy; ii)
patients with US Eastern Cancer Cooperative Group (ECOG) score
(15) ≤1 point and initial expected
survival time >3 months; iii) patients with observable tumor
lesion ≥1, and iv) The amplification refractory mutation system
(ARMS) kit was used to detect EGFR genic mutations at exon 18, exon
19 or exon 2l.
Exclusion criteria were: i) Patients with systemic
immune system diseases or extremely low immune ability who were
intolerant to chemotherapy; ii) patients with severe heart
insufficiency or liver and kidney dysfunction, and iii) patients
allergic to drugs used in this experiment.
The study was approved by the Ethics Committee of
the Affiliated Hospital of Weifang Medical University. Signed
informed consents were obtained from the patients or the
guardians.
Experimental reagents and
instruments
Icotinib hydrochloride (Beida Pharmaceutical Co.,
Ltd., H20110060), pemetrexed disodium for injection (Shanghai
Kaimao Biomedical Co., Ltd., H20123010), cisplatin (Jinzhou Jiutai
Pharmaceutical Co., Ltd., H21020751) and folic acid tablet
(Hangzhou Australian Medical Baoling Pharmaceutical Co., Ltd.,
H20123159). ARMS kit was purchased from MSK Biotechnology Co.,
Ltd.
Experimental methods
All patients were given routine treatment such as
anti-emesis, stomach protection and fluid infusion on the first 3
days of chemotherapy. Patients in the pemetrexed group were
additionally orally administered 1 folic acid tablet (0.4
mg/tablet) daily for 3 weeks from the first 7 days of chemotherapy
to the last administration of chemotherapy for enhancing the
efficacy. The drug regimen of patients in the icotinib group was:
icotinib 125 mg/time, 3 times/day orally, days 1–28. The drug
regimen of patients in the pemetrexed group was: pemetrexed 500
mg/m2, day 1, intravenous drip; cisplatin, 25
mg/m2, days 1–3. Patients in the icotinib group were not
given medicine during continuous drug use if progressive tumor or
intolerable toxic and side effects occurred. The first evaluation
of patients was performed 4 weeks after the last administration,
and then evaluation was performed once every six weeks. A total of
21 days for 1 chemotherapy cycle, patients in the pemetrexed group
were continuously administered for 4 cycles. After each two
chemotherapy cycles, patient was reviewed to evaluate the efficacy
of drugs. If progressive tumor or severe adverse reactions
occurred, medication was stopped.
Evaluation criteria for efficacy as
well as toxic and side effects (16)
Patients with different medications in the two
groups were observed and their conditions after medication were
recorded. The efficacy of drugs was evaluated based on the Response
Evaluation Criteria in Solid Tumors (RECIST), divided into:
complete response (CR): all target lesions of patients disappeared
for >28 consecutive days; partial response (PR): the total
diameter of the target lesion of patients reduced by 30%,
maintaining for >28 days; stable disease (SD): the total
diameter of the target lesion of patients increased by ≤20%, or
reduced ≤30%; progressive disease (PD): the total diameter of the
target lesion of patients increased by ≥20%, or new target lesions
appeared. The observation indicator was progression-free survival
time when progressive tumor or death occurred in patients. Overall
response rate (ORR) = (CR+PR) / total number × 100%. Disease
control rate (DCR) = (CR+PR+SD) / total number × 100%. The toxic
and side effects of drugs were evaluated based on the National
Cancer Institute General Toxicity Standard (NCI-CTC.4.0) (17).
Statistical analysis
SPSS 19.0 statistical software (SPSS Inc.) was used
for statistical analysis of the experimental data. Enumeration data
were expressed as %, and Chi-square (χ2) test was used
for comparison between the groups and pairwise comparisons were
made followed by Bonferroni post hoc test. χ2 test was
used when the total number of cases was n≥40 and all theoretical
frequencies T≥5. Fisher's exact test was used when n≥40, but ≥1
T<5. Measurement data were expressed as mean ± SD, and t-test
was used for comparison between the groups. Kaplan-Meier test was
used for survival analysis. The log-rank test was used to compare
the survival distribution between the two samples. At P<0.05,
the difference was considered statistically significant.
Results
Comparison of clinical basic data
As shown in Table I,
there were no differences in age, body mass index and blood
pressure between the icotinib and pemetrexed groups of patients
(P>0.05).
 | Table I.Comparison of clinical basic data
(mean ± SD) [n (%)]. |
Table I.
Comparison of clinical basic data
(mean ± SD) [n (%)].
| Clinical
features | Icotinib group
(n=69) | Pemetrexed group
(n=63) | t/χ2 | P-value |
|---|
| Age (years) | 54.32±6.46 | 53.85±6.83 | 0.406 | 0.685 |
| Body mass index
(kg/m2) | 20.63±2.58 | 21.22±2.41 | 1.354 | 0.178 |
| Systolic pressure
(mmHg) | 126.47±12.39 | 128.38±8.25 | 1.032 | 0.304 |
| Diastolic pressure
(mmHg) | 74.53±3.58 | 73.68±5.39 | 1.076 | 0.284 |
| Sex | 0.031 | 0.861 |
|
|
| Male | 45 (65.22) | 42 (66.67) |
|
|
|
Female | 24 (24.78) | 21 (33.33) |
|
|
| Clinical stages | 0.049 | 0.976 |
|
|
| IIIA | 2 (2.90) | 2 (3.17) | 0.009 | 0.926 |
| IIIB | 5 (7.25) | 4 (6.35) | 0.042 | 0.838 |
| IV | 62 (89.85) | 57 (90.48) | 0.014 | 0.905 |
| Performance
status | 0.128 | 0.938 |
|
|
| 0 | 3 (4.35) | 2 (3.17) | 0.124 | 0.724 |
| 1 | 65 (94.20) | 60 (95.24) | 1.513 | 0.219 |
| 2 | 1 (1.45) | 1 (1.59) | 0.004 | 0.948 |
Comparison of clinical efficacy
The clinical efficacy was evaluated in the two
groups of patients. Patients in the icotinib group were treated for
>28 days, and patients in the pemetrexed group for at least 2
cycles. There was no treatment-related death in the two groups. ORR
was 34.78% in the icotinib group and 28.57% in the pemetrexed
group, and DCR was 75.36% in the icotinib group and 69.84% in the
pemetrexed group, with no statistically significant differences
(P>0.05) (Table II).
 | Table II.Comparison of clinical efficacy
between icotinib and pemetrexed in treatment of lung
adenocarcinoma. |
Table II.
Comparison of clinical efficacy
between icotinib and pemetrexed in treatment of lung
adenocarcinoma.
| Groups | CR (complete
remission) | PR (partial
remission) | SD (stable
disease) | PD (progressive
disease) | ORR (overall response
rate) | DCR (disease control
rate) |
|---|
| Icotinib group
(n=69) | 2 (2.90) | 22 (31.88) | 28 (40.58) | 17 (24.64) | 24 (34.78) | 52 (75.36) |
| Pemetrexed group
(n=63) | 1 (1.59) | 17 (26.98) | 26 (41.27) | 19 (30.16) | 18 (28.57) | 44 (69.84) |
| χ2 | 0.006 | 0.380 | 0.006 | 0.506 | 0.586 | 0.506 |
| P-value | 0.937 | 0.048 | 0.936 | 0.477 | 0.444 | 0.477 |
Comparison of toxic and side
effects
The main toxic and side effects of icotinib were
rash (39.13%), constipation or diarrhea (20.29%), hepatotoxicity
(17.39%) and nausea and vomiting (13.04%), with generally less
toxic and side effects at grades III–IV (Table III). Those of pemetrexed were
leukopenia (47.62%), neutropenia (63.49%), thrombocytopenia
(36.51%), nausea and vomiting (73.02%), fatigue (55.56%) and
peripheral nerve toxicity (34.92% (Table IV). The toxic and side effects of
the two groups were compared by χ2 test. The incidence
of leukopenia, neutropenia, thrombocytopenia, anemia, nausea and
vomiting, fatigue and peripheral nerve toxicity was higher in the
pemetrexed group than that in the icotinib group, but that of rash
was higher in the icotinib group than that in the pemetrexed group
(P<0.05). The comparison of other toxic and side effects was not
significant (P>0.05) (Table
V).
 | Table III.Toxic side effects of icotinib in
treatment of lung adenocarcinoma [n (%)]. |
Table III.
Toxic side effects of icotinib in
treatment of lung adenocarcinoma [n (%)].
|
| Icotinib group
(n=69) |
|---|
|
|
|
|---|
| Toxic and side
effects | I | II | III | IV | Total number of
cases |
|---|
| Leukopenia | 4
(5.80) | 2 (2.90) | 2 (2.90) | 0 (0.00) | 8
(11.59) |
| Neutropenia | 2
(2.90) | 1 (1.45) | 1 (1.45) | 0 (0.00) | 4
(5.80) |
|
Thrombocytopenia | 3
(4.35) | 2 (2.90) | 0 (0.00) | 0 (0.00) | 5
(7.25) |
| Anemia | 2
(2.90) | 1 (1.45) | 0 (0.00) | 0 (0.00) | 3
(4.35) |
| Nausea and
vomiting | 6
(8.70) | 2 (2.90) | 1 (1.45) | 0 (0.00) | 9
(13.04) |
| Constipation or
diarrhea | 8
(11.59) | 3 (4.35) | 2 (2.90) | 1 (1.45) | 14 (20.29) |
| Rash | 24 (34.78) | 3 (4.35) | 0 (0.00) | 0 (0.00) | 27 (39.13) |
| Alopecia | 2
(2.90) | 1 (1.45) | 0 (0.00) | 0 (0.00) | 3
(4.35) |
| Fatigue | 7
(10.14) | 3 (4.35) | 0 (0.00) | 0 (0.00) | 7
(10.14) |
| Peripheral nerve
toxicity | 1
(1.45) | 5 (7.25) | 0 (0.00) | 0 (0.00) | 6
(8.70) |
| Stomatitis | 3
(4.35) | 2 (2.90) | 0 (0.00) | 0 (0.00) | 5
(7.25) |
| Hepatotoxicity | 8
(11.59) | 3 (4.35) | 1 (1.45) | 0 (0.00) | 12 (17.39) |
| Neurotoxicity | 1
(1.45) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 1
(1.45) |
 | Table IV.Toxic side effects of pemetrexed in
the treatment of lung adenocarcinoma [n (%)]. |
Table IV.
Toxic side effects of pemetrexed in
the treatment of lung adenocarcinoma [n (%)].
|
| Pemetrexed group
(n=63) |
|---|
|
|
|
|---|
| Toxic and side
effects | I | II | III | IV | Total number of
cases |
|---|
| Leukopenia | 12 (19.05) | 9
(14.29) | 8 (12.70) | 1 (1.59) | 30 (47.62) |
| Neutropenia | 18 (28.57) | 10 (15.87) | 8 (12.70) | 4 (6.35) | 40 (63.49) |
|
Thrombocytopenia | 12 (19.05) | 6
(9.52) | 5 (7.94) | 0 (0.00) | 23 (36.51) |
| Anemia | 8
(12.70) | 4
(6.35) | 3 (4.76) | 0 (0.00) | 15 (23.81) |
| Nausea and
vomiting | 27 (42.86) | 16 (25.40) | 3 (4.76) | 0 (0.00) | 46 (73.02) |
| Constipation or
diarrhea | 11 (17.46) | 3
(4.76) | 1 (1.59) | 0 (0.00) | 15 (23.81) |
| Rash | 3
(4.76) | 2
(3.17) | 0 (0.00) | 0 (0.00) | 5
(7.94) |
| Alopecia | 4
(6.35) | 1
(1.59) | 0 (0.00) | 0 (0.00) | 5
(7.94) |
| Fatigue | 23 (36.51) | 10 (15.87) | 2 (3.17) | 0 (0.00) | 35 (55.56) |
| Peripheral nerve
toxicity | 17 (16.98) | 5
(7.94) | 0 (0.00) | 0 (0.00) | 22 (34.92) |
| Stomatitis | 4
(6.35) | 1
(1.59) | 0 (0.00) | 0 (0.00) | 5
(7.94) |
| Hepatotoxicity | 8
(12.70) | 3
(4.76) | 2 (3.17) | 0 (0.00) | 13 (20.63) |
| Neurotoxicity | 1
(1.59) | 0
(0.00) | 0 (0.00) | 0 (0.00) | 1
(1.59) |
 | Table V.Comparison of toxic and side effects
between icotinib and pemetrexed in the treatment of lung
adenocarcinoma [n (%)]. |
Table V.
Comparison of toxic and side effects
between icotinib and pemetrexed in the treatment of lung
adenocarcinoma [n (%)].
|
| Total number of
cases |
|---|
|
|
|
|---|
| Toxic and side
effects | Icotinib group
(n=69) | Pemetrexed group
(n=63) | χ2 | P-value |
|---|
| Leukopenia | 8
(11.59) | 30
(47.62)a | 20.850 | <0.001 |
| Neutropenia | 4
(5.80) | 40
(63.49)a | 49.330 | <0.001 |
|
Thrombocytopenia | 5
(7.25) | 23
(36.51)a | 16.870 | <0.001 |
| Anemia | 3
(4.35) | 15
(23.81)a | 10.590 | <0.001 |
| Nausea and
vomiting | 9
(13.04) | 46
(73.02)a | 48.730 | <0.001 |
| Constipation or
diarrhea | 14 (20.29) | 15 (23.81) |
0.238 |
0.626 |
| Rash | 27 (39.13) | 5
(7.94)a | 17.450 | <0.001 |
| Alopecia | 3
(4.35) | 5
(7.94) |
0.278 |
0.619 |
| Fatigue | 7
(10.14) | 35
(55.56)a | 31.300 | <0.001 |
| Peripheral nerve
toxicity | 6
(8.70) | 22
(34.92)a | 13.550 | <0.001 |
| Stomatitis | 5
(7.25) | 5
(7.94) |
0.024 |
0.878 |
| Hepatotoxicity | 12 (17.39) | 13 (20.63) |
0.226 |
0.635 |
| Neurotoxicity | 1
(1.45) | 1
(1.59) |
0.420 |
0.517 |
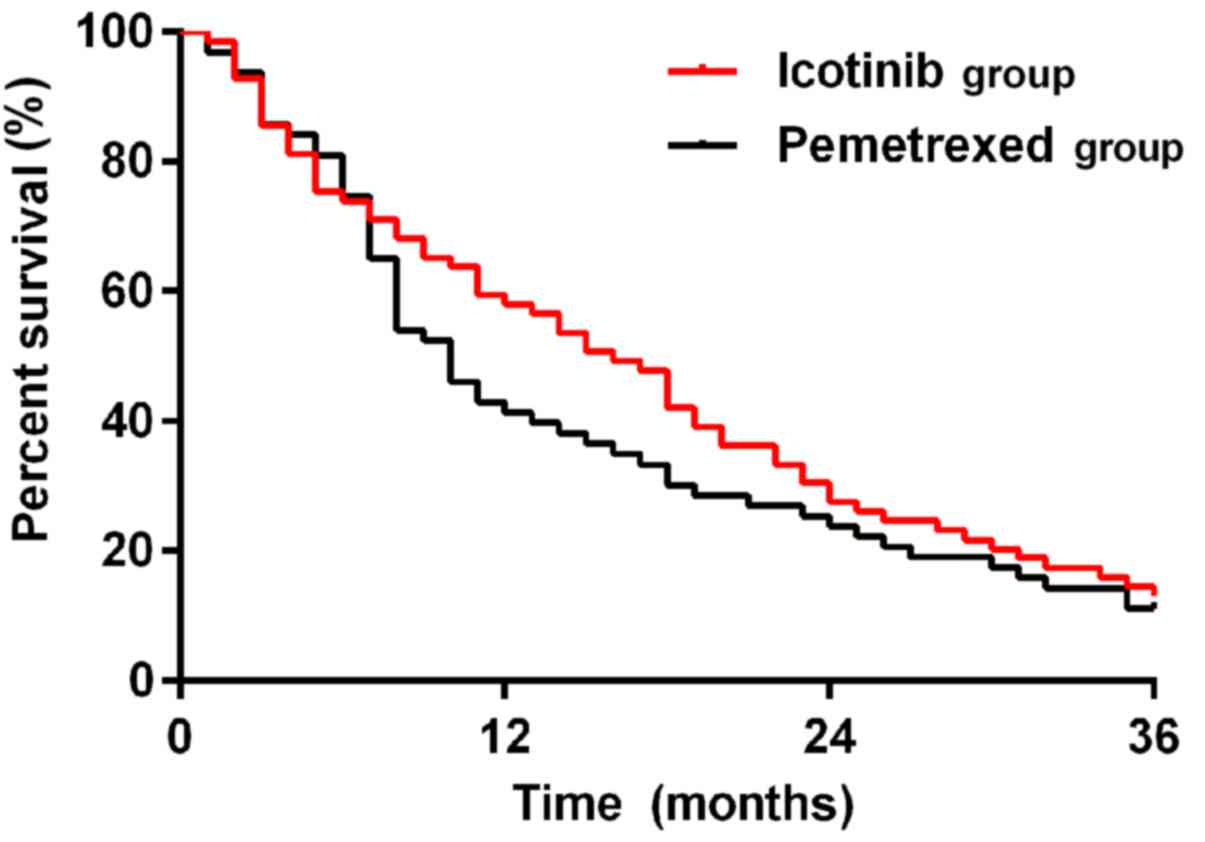
Survival
Patients in the two groups were followed up until
July 2018. The median survival time of patients was 16 months in
the icotinib group, higher than that in the pemetrexed group (10
months), with a statistically significant difference (P<0.05).
The 1-year survival rate was higher in the icotinib group than that
in the pemetrexed group (P<0.05). There were no differences in
2- and 3-year survival rates between the two groups (P>0.05)
(Table VI and survival curve in
Fig. 1).
 | Table VI.Comparison of survival rate between
the icotinib and pemetrexed groups [n (%)]. |
Table VI.
Comparison of survival rate between
the icotinib and pemetrexed groups [n (%)].
| Case
number/ratio | 1-year | 2-years | 3-years |
|---|
| Icotinib group
(n=69) | 44 (63.77) | 23 (33.33) | 9 (13.04) |
| Pemetrexed group
(n=63) | 29 (46.03) | 17 (26.98) | 7 (11.11) |
| χ2 | 4.191 | 0.364 | 0.005 |
| P-value | 0.041 | 0.546 | 0.942 |
Discussion
Lung cancer is a malignant tumor mostly occurring in
the middle-aged and elderly (18).
Most patients miss the best treatment time of operation because of
untimely treatment, so its main clinical treatment is chemotherapy
(19). Having various organ
dysfunction with poor stress ability, middle-aged and elderly
patients cannot well tolerate chemotherapeutics (20). Thus, more complications and lesion
metastasis occur in them, seriously threatening their life and
health (21). In order to prolong
the survival time of patients, the most important point for the
treatment of malignant tumors is to find chemotherapeutics with
good efficacy and few adverse reactions.
Icotinib is a small molecule targeted anti-cancer
drug independently developed in China, which is suitable for
patients with middle and advanced NSCLC and easy to use, with fewer
toxic and side effects (22).
Currently, clinical studies have shown that pemetrexed can
significantly prolong the survival time of adenocarcinoma patients
and better control progressive disease (23). However, the incidence of its toxic
and side effects such as myelosuppression (leukopenia, neutropenia
and thrombocytopenia) and gastrointestinal reactions is high,
therefore it is difficult to achieve the desired efficacy (24). Long-term pemetrexed combination
treatment still has high requirements for patients' physical
quality, but there are extremely few studies on the efficacy
comparison between icotinib and pemetrexed in clinical practice. In
this study, the efficacy, safety and survival rate were compared
between the two groups of drugs to help the first-line treatment of
lung adenocarcinoma.
The results of this study showed that the
progression-free survival time of icotinib was significantly higher
than that of pemetrexed in the treatment of lung adenocarcinoma
(P<0.05). ORR was 34.78% in icotinib group and 28.57% in the
pemetrexed group, and DCR was 75.36% in the icotinib group and
69.84% in the pemetrexed group, with no statistically significant
differences (P>0.05). It is suggested that both drugs have good
efficacy. The median survival time of patients was 16 months in the
icotinib group, higher than 10 months in the pemetrexed group, with
a statistically significant difference (P<0.05). The 1-year
survival rate was higher in the icotinib group compared with that
in the pemetrexed group (P<0.05). There were no differences in
2- and 3-year survival rates between the two groups (P>0.05).
Gefitinib, the tyrosinase inhibitor of epidermal growth factor
receptor (EGFR), which is currently the most commonly used in
clinic, inhibits the invasion, infiltration, proliferation and
angiogenesis of tumor cells (25).
It can prolong the survival time of lung adenocarcinoma patients,
especially the median and progression-free survival time, improving
patients' quality of life (26).
Studies have shown that icotinib, as a small molecule EGFR
tyrosinase inhibitor independently developed in China, can be
equivalent to gefitinib, which has been confirmed in clinical
applications (27). Even for
patients with EGFR mutations, icotinib can selectively inhibit the
binding of ATP and EGFR tyrosine kinase to reduce the biological
activity of EGFR-TKI, thereby inhibiting the proliferation,
invasion and metastasis of cancer cells (28). Pemetrexed is a novel anti-folate drug
that inhibits multiple enzyme targets depending on folate
metabolism. It can enable tumor cells to synthesize pyrimidine and
purine disorders, stopping tumor cell growth in S phase, so as to
inhibit the growth and proliferation of tumor cells (29). Several studies have shown that
pemetrexed tends to achieve better ORR and DCR than other
first-line chemotherapeutics in the treatment of non-squamous
cancer malignant tumors such as adenocarcinoma (30). Both icotinib and pemetrexed have good
efficacy in lung adenocarcinoma. It may be considered clinically
that icotinib combined with pemetrexed can be used to inhibit tumor
growth and proliferation, prolonging the survival time of lung
adenocarcinoma patients, to obtain better efficacy.
The main toxic and side effects of icotinib were
rash (39.13%), constipation or diarrhea (20.29%), hepatotoxicity
(17.39%) and nausea and vomiting (13.04%), with generally less
toxic and side effects at grades III–IV. Those of pemetrexed were
leukopenia (47.62%), neutropenia (63.49%), thrombocytopenia
(36.51%), nausea and vomiting (73.02%), fatigue (55.56%) and
peripheral nerve toxicity (34.92%). It is suggested that the
incidence of toxic and side effects of pemetrexed is significantly
higher than that of icotinib. Literature (31) shows that after a short-term
withdrawal or symptomatic treatment, the toxic and side effects of
icotinib, rash and diarrhea, can be alleviated to a great extent.
Even for milder toxic and side effects at grades I–II, symptoms
disappear on their own within a certain period of time (31). Therefore, lung adenocarcinoma
patients with poor physical quality may have longer tolerance time
to treatment with icotinib and higher quality of life.
However, in this study, there are also some
limitations. First, the sample size of patients is still
insufficient. When survival analysis was performed, the time span
was not long enough. It is necessary to collect more cases for a
long-term follow-up study. Second, the mechanism of action of
icotinib and pemetrexed in lung adenocarcinoma tumor cells is still
not clear enough. In this study, we did not compare icotinib with
other drugs such as gefitinib or erlotinib, so whether the efficacy
of icotinib in lung adenocarcinoma is optimal remains to be further
explored.
In conclusion, there is no difference in short-term
clinical efficacy between icotinib and pemetrexed in the treatment
of patients with lung adenocarcinoma. However, the median survival,
progression-free survival and one-year survival of patients with
lung adenocarcinoma treated with icotinib are higher than those
treated with pemetrexed, and icotinib has significantly less toxic
and side effects than pemetrexed, which is worthy of further
research.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XZ and LW helped with analysis of the toxic and side
effects. XZ, CG and YZ were responsible for the collection and
analysis of the experimental data. DH and LQ were responsible for
the follow-up of the patients and drafted the manuscript. All the
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
the Affiliated Hospital of Weifang Medical University (Weifang,
China). Signed informed consents were obtained from the patients or
the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Black CN, Bot M, Scheffer PG, Cuijpers P
and Penninx BW: Is depression associated with increased oxidative
stress? A systematic review and meta-analysis.
Psychoneuro-endocrinology. 51:164–175. 2015. View Article : Google Scholar
|
|
2
|
National Center for Chronic Disease
Prevention and Health Promotion (US) Office on Smoking and Health:
The Health Consequences of Smoking—50 Years of Progress: A Report
of the Surgeon General. Centers for Disease Control and Prevention
(US); Atlanta, GA: 2014
|
|
3
|
Thomas PA, Berbis J, Baste JM, Le
Pimpec-Barthes F, Tronc F, Falcoz PE, Dahan M and Loundou A;
EPITHOR group, : Pneumonectomy for lung cancer: Contemporary
national early morbidity and mortality outcomes. J Thorac
Cardiovasc Surg. 149:73–82. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zeng Y, Zhu J, Shen D, Qin H, Lei Z, Li W,
Liu Z and Huang JA: MicroRNA-205 targets SMAD4 in non-small cell
lung cancer and promotes lung cancer cell growth in vitro and in
vivo. Oncotarget. 8:30817–30829. 2017.PubMed/NCBI
|
|
5
|
Girard N, Corral J, Cortinovis D and
Heigener DF: Second-line treatment selection in patients with
non-small-cell lung cancer of adenocarcinoma histology: Findings
from a European survey of treating physicians. Clin Lung Cancer.
18:e89–e97. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Meaney CL, Zingone A, Brown D, Yu Y, Cao L
and Ryan BM: Identification of serum inflammatory markers as
classifiers of lung cancer mortality for stage I adenocarcinoma.
Oncotarget. 8:40946–40957. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wagland R, Brindle L, Ewings S, James E,
Moore M, Rivas C, Esqueda AI and Corner J: Promoting help-seeking
in response to symptoms amongst primary care patients at high risk
of lung cancer: A mixed method study. PLoS One. 11:e01656772016.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sha F, Zhuang S, Zhou L, Zhang L, Yang Y,
Zhang S, Jiang Y, Qiu G, Chen C, Zheng J, et al: Biomarkers for
cancer-related fatigue and adverse reactions to chemotherapy in
lung cancer patients. Mol Clin Oncol. 3:163–166. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shaw AT, Kim DW, Nakagawa K, Seto T, Crinó
L, Ahn MJ, De Pas T, Besse B, Solomon BJ, Blackhall F, et al:
Crizotinib versus chemotherapy in advanced ALK-positive lung
cancer. N Engl J Med. 368:2385–2394. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yao S, Zhi X, Wang R, Qian K, Hu M and
Zhang Y: Retrospective study of adjuvant icotinib in postoperative
lung cancer patients harboring epidermal growth factor receptor
mutations. Thorac Cancer. 7:543–548. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen YT, Feng B and Chen LB: Update of
research on drug resistance in small cell lung cancer chemotherapy.
Asian Pac J Cancer Prev. 13:3577–3581. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liew SC: Folic acid and diseases -
supplement it or not? Rev Assoc Med Bras 1992. 62:90–100. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li B, Li MY, Sun LL, Wang J, Zheng YQ and
Hao J: Impact of anticancer drugs price cut on physician's
prescription choices on first-line chemotherapy regimens and health
expenditure for advanced non-small cell lung cancer in China. J
Thorac Dis. 8:2832–2842. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mok TS, Wu YL, Ahn MJ, Garassino MC, Kim
HR, Ramalingam SS, Shepherd FA, He Y, Akamatsu H, Theelen WS, et al
AURA3 Investigators, : Osimertinib or platinum-pemetrexed in EGFR
T790M-positive lung cancer. N Engl J Med. 376:629–640. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
de Kock I, Mirhosseini M, Lau F, Thai V,
Downing M, Quan H, Lesperance M and Yang J: Conversion of Karnofsky
Performance Status (KPS) and Eastern Cooperative Oncology Group
Performance Status (ECOG) to Palliative Performance Scale (PPS),
and the interchangeability of PPS and KPS in prognostic tools. J
Palliat Care. 29:163–169. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Guenther LM, Rowe RG, Acharya PT, Swenson
DW, Meyer SC, Clinton CM, Guo D, Sridharan M, London WB, Grier HE,
et al: Response Evaluation Criteria in Solid Tumors (RECIST)
following neoadjuvant chemotherapy in osteosarcoma. Pediatr Blood
Cancer. 65:652018. View Article : Google Scholar
|
|
17
|
Luo Y, Li J, Wang Y, Hao X and Qu F:
Nimotuzumab combined with chemotherapy as second- or later-line in
the treatment of advanced lung squamous cell carcinoma. Zhongguo
Fei Ai Za Zhi. 19:665–669. 2016.(In Chinese). PubMed/NCBI
|
|
18
|
Fritz I and Olsson H: Lung cancer in young
women in southern Sweden: A descriptive study. Clin Respir J.
12:1565–1571. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Murphy RA, Mourtzakis M, Chu QS, Baracos
VE, Reiman T and Mazurak VC: Supplementation with fish oil
increases first-line chemotherapy efficacy in patients with
advanced nonsmall cell lung cancer. Cancer. 117:3774–3780. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kanesvaran R, Roy Chowdhury A and Krishna
L: Practice pearls in the management of lung cancer in the elderly.
J Geriatr Oncol. 7:362–367. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gutschner T, Hämmerle M, Eissmann M, Hsu
J, Kim Y, Hung G, Revenko A, Arun G, Stentrup M, Gross M, et al:
The noncoding RNA MALAT1 is a critical regulator of the metastasis
phenotype of lung cancer cells. Cancer Res. 73:1180–1189. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhou L, He J, Xiong W, Liu Y, Xiang J, Yu
Q, Liang M, Zhou X, Ding Z, Huang M, et al: Impact of whole brain
radiation therapy on CSF penetration ability of Icotinib in
EGFR-mutated non-small cell lung cancer patients with brain
metastases: Results of phase I dose-escalation study. Lung Cancer.
96:93–100. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Song Z, Su H and Zhang Y: Patients with
ROS1 rearrangement-positive non-small-cell lung cancer benefit from
pemetrexed-based chemotherapy. Cancer Med. 5:2688–2693. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Scheinpflug K, Menzel C, Koch A, Kahl C
and Achenbach HJ: Toxic epidermal necrolysis related to cisplatin
and pemetrexed for metastatic non-small cell lung cancer.
Onkologie. 35:600–603. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ping W, Gao Y, Fan X, Li W, Deng Y and Fu
X: MiR-181a contributes gefitinib resistance in non-small cell lung
cancer cells by targeting GAS7. Biochem Biophys Res Commun.
495:2482–2489. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ding T, Zhou F, Chen X, Zhang S, Liu Y,
Sun H, Ren S, Li X, Zhao C, Wang H, et al: Continuation of
gefitinib plus chemotherapy prolongs progression-free survival in
advanced non-small cell lung cancer patients who get acquired
resistance to gefitinib without T790M mutations. J Thorac Dis.
9:2923–2934. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Liu Y, Zhang Y, Feng G, Niu Q, Xu S, Yan
Y, Li S and Jing M: Comparison of effectiveness and adverse effects
of gefitinib, erlotinib and icotinib among patients with non-small
cell lung cancer: A network meta-analysis. Exp Ther Med.
14:4017–4032. 2017.PubMed/NCBI
|
|
28
|
Lee JK, Hahn S, Kim DW, Suh KJ, Keam B,
Kim TM, Lee SH and Heo DS: Epidermal growth factor receptor
tyrosine kinase inhibitors vs conventional chemotherapy in
non-small cell lung cancer harboring wild-type epidermal growth
factor receptor: A meta-analysis. JAMA. 311:1430–1437. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fennell DA, Gaudino G, O'Byrne KJ, Mutti L
and van Meerbeeck J: Advances in the systemic therapy of malignant
pleural mesothelioma. Nat Clin Pract Oncol. 5:136–147. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chen M, Cao H, Ji Y, Mao Y, Shen S and Li
X: Association between the ALK Gene Status and the efficacy of
first-line pemetrexed chemotherapy in patients with advanced lung
adenocarcinoma. Zhongguo Fei Ai Za Zhi. 20:732–736. 2017.(In
Chinese). PubMed/NCBI
|
|
31
|
Shi Y, Zhang L, Liu X, Zhou C, Zhang L,
Zhang S, Wang D, Li Q, Qin S, Hu C, et al: Icotinib versus
gefitinib in previously treated advanced non-small-cell lung cancer
(ICOGEN): A randomised, double-blind phase 3 non-inferiority trial.
Lancet Oncol. 14:953–961. 2013. View Article : Google Scholar : PubMed/NCBI
|