Introduction
Osteosarcoma is an osteoblastoma of mesenchymal
origin. It is the most common primary malignant tumor of the bone
and tends to occur in teenagers (1).
Although primary bone cancers account for only 0.2% of all
malignant tumors, the results are severe in children and adults
once they develop this cancer (1).
According to the National Cancer Institute Surveillance,
Epidemiology, and End Results program, cancer prevalence increased
at an annual rate of ~0.3% over the previous decade (2). Although osteosarcoma usually occurs at
the age between 5 and early adulthood, in recent years, the
incidence rate among elderly patients has increased, and ~60% of
osteosarcomas occur in patients <20 years old, and ~10% of
patients are >60 years old (3).
It has been reported that the emergence of this phenomenon may be
highly associated with a history of Paget's disease and
radiotherapy (4).
In the last decade, immunotherapy has been
considered as one of the most promising potential means of
treatments for patients with various types of cancer (5–8). The
emergence of immunotherapy for tumor treatment provides novel
insight, as this modality has been reported to activate the body's
immune system, enhance an antitumor immune response, kill
vulnerable tumor cells, and inhibit tumor proliferation and
metastasis. The reported results of immunotherapy are promising,
and clinical applications have indicated that immunotherapy is
effective, where a number of patients with cancer even achieve
long-term recovery (5). The immune
system recognizes novel tumor antigens usually as foreign
substances, therefore, eliminating tumors via an immune response
(6). When the body recognizes the
novel tumor antigen, the immune response starts (7). In this process, interactions between
different immune cells are critical for tumor elimination.
Nevertheless, a number of tumors, such as renal cell carcinoma,
pancreatic cancer, glioma and colorectal cancer, secrete proteins
called immunocheckpoint inhibitors via tumor-specific immune cells
(7). This combination activates an
inhibitory pathway that limits normal immune responses, thereby
allowing tumors to evade or suppress immune responses (5–7). The
most recent immunotherapeutic approaches target these mechanisms of
immune tolerance by blocking immune checkpoints to revive a
functionally suppressed immune response, reinvigorate T cells, and
promote antitumor immunity (9).
T-cell immunoglobulin and mucin domain-containing-3
(TIM-3), also known as HAVCR2, has been recognized as a member of
the TIM gene family, which includes TIM-1, TIM-3, and TIM-4 in
humans and Tim-1 through Tim-8 in mice (10). TIM-3 is expressed on T helper 1
(Th1), Th17, and CD8+ T cells (cells of myeloid
lineages) (11). Engagement of its
ligands by TIM-3 has been indicated to suppress Th1 and Th17
responses and to induce peripheral immune tolerance, supporting an
inhibitory role of TIM-3 in T-cell-mediated immune responses
(12). The expression levels of
programmed cell death 1 (PD-1) and TIM-3 in tumor tissues are
significantly associated with PD1 and TIM-3 polymorphisms, and
administration of TIM-3 and PD-1 synergistically promotes tumor
growth (13). The aforementioned
preclinical studies indicate an inhibitory effect of TIM-3 on
antitumor immunity.
However, the association between TIM-3 and
osteosarcoma, to the best of our knowledge, remains unclear.
Therefore, the aim of the present study was to analyze the
expression level of TIM-3 in primary osteosarcoma and its possible
association with survival of patients with osteosarcoma.
Materials and methods
Acquisition of human tissue
samples
The present study was approved by The Ethics
Committee of Union Hospital Tongji Medical College of Huazhong
University of Science and Technology (Wuhan, China) and conforms to
the provisions of the Declaration of Helsinki. Tissue collection
process was approved by the Ethics Committee, all patients and
legal guardians provided written informed consent regarding human
tissue acquisition used in the present study, in accordance with
National Regulations on the Use of Clinical Samples in China. A
total of 38 pairs of osteosarcoma tissue samples were obtained from
patients with osteosarcoma, who underwent surgical resection at the
Union Hospital between January 2011 and June 2016, and eight groups
of fresh tissue samples, including tumor and adjacent tissues were
obtained between January and November in 2016. Among the 38
patients, 26 were male and 12 were female, ranging in age from 8–72
years old, and the median age was 18 years old. The eight fresh
specimens included five male and three females, aged from 12–46
years, with a median age of 14 years. Patients receiving
chemotherapy or radiotherapy prior to surgical treatment were
excluded from the study. The diagnosis and Enneking stage of
osteosarcoma was assessed by two experienced pathologists
independently, (Union Hospital, Tongji Medical College, Huazhong
University of Science and Technology, Wuhan, China) in a blinded
manner, and according to the Enneking system and the 2015 World
Health Organization Classification of Tumors (14,15). All
patients and legal guardians provided written informed consent
regarding human tissue acquisition used in the present study, in
accordance with National Regulations on the Use of Clinical Samples
in China.
Cell culture
Human osteosarcoma cell lines U-2OS, MG63, and SAOS
and osteoblastic cell line hFOB1.19 were purchased from the Type
Culture Collection of the Chinese Academy of Sciences. The U-2OS,
MG63, and SAOS cells were cultured in Eagle's minimum essential
medium (ATCC) supplemented with 10% FBS (Thermo Fisher Scientific,
Inc.). hFOB1.19 cells were cultured in McCoy's 5a modified medium
(ATCC) containing 10% FBS. All cells were cultured at 37°C with 5%
CO2.
Immunohistochemical (IHC)
staining
Staining was performed on 4 µm tissue microarray
sections of formalin-fixed in 10% formalin at 4°C for 24 h and
subsequently paraffin-embedded. The slices were deparaffinized in
xylene and dehydrated in a graded series of ethanol solutions,
deparaffinized and hydrated in 100% alcohol for 5 min followed by
80% alcohol for 5 min. The endogenous peroxidase activity was
quenched with 0.3% hydrogen peroxide. Antigen retrieval was
performed with citrate buffer at 98°C for 10 min and endogenous
peroxidase activity was blocked using 0.3% hydrogen peroxide in
methanol for 15 min at room temperature. Antigen retrieval was
performed in 0.01 mol/l citric acid buffer and non-specific binding
was blocked with 10% normal goat serum (Wuhan Servicebio Technology
Co., Ltd., Wuhan, China) at 37°C for 30 min. Subsequently,
overnight incubation at 4°C was carried out with an anti-human
TIM-3 monoclonal antibody (dilution, 1:100; R&D Systems, Inc.,
Minneapolis, MN, USA), followed by a 30 min incubation at 37°C with
a horseradish peroxidase-labeled anti-rabbit IgG antibody
(dilution, 1:500; R&D Systems, Inc.). Samples were incubated
with the primary antibodies overnight at 4°C. Subsequently, the
samples were incubated with horseradish peroxidase universal
immunoglobulin G (IgG) secondary antibody (cat. no. sc69786;
1:1,000; Santa Cruz Biotechnology, Inc., Dallas, TX, USA) for 30
min at 37°C. A histostaining kit (cat. no. SP9001; OriGene
Technologies, Inc., Beijing, China) was used to visualize antibody
binding on the slides, according to the manufacturer's protocol.
The tissue slices were incubated with DAB (Wuhan Servicebio
Technology Co., Ltd., Wuhan, China) and lightly counterstained with
0.5% hematoxylin for 5 min at 37°C. Slides which had not been
treated with a primary antibody were used as the negative control
and the breast cancer tissues slides which had previously been
confirmed to overexpress the TIM-3 protein were used as the
positive controls. The slides were observed using a light
microscope at ×200 magnification (IX71; Olympus, Tokyo, Japan).
Tim-3 immunoreactivity was assessed independently by
two pathologists blinded to the origin of the tissue with the use
of a labeling index. A total of 100 cells were counted in 3 random
fields and the percentage of positive cells were calculated. The
extent of staining, calculated as the percentage of stained cells,
and the intensity of immunostaining were taken into consideration
in the analysis of data. The semi-quantitative immunoreaction
scoring system was evaluated based on the percentage of positive
cells added to the stain intensity. Regarding stain intensity,
negative staining was defined as 0, weakly positive was defined as
1, moderately positive as 2 and strongly positive as 3. The scores
of immuno-positive cells were defined as follows: <5% Positive
cells was defined as 0 (negative); 5–25% immuno-positive cells as 1
(low); 25–75% immuno-positive cells as 2 (moderate); and >75%
immuno-positive cells as 3 (high). The sum of the stain intensity
and positive cell scores was the final score given to each section
and defined as: -, 0; +, 1 or 2; ++, 3 or 4; and +++, 5 or 6. The
intensity of staining was scored between 0 and 3, and the extent of
staining was scored between 0 and 100%. The final quantitation of
IHC staining in each sample was obtained by multiplying the two
scores. TIM-3 expression was classified as high if the score was
>1.1 (median score), while a score of ≤1.1 was classified as low
expression of TIM-3.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR)
TRIzol® was used to extract total RNA
from the patients' frozen tissues and the osteosarcoma cell lines,
including U2OS, MG-63 and SAOS, and the osteoblast cell line,
hFOB1.19. Analysis of relative gene expression data from RT-qPCR
was performed using the 2−ΔΔCq method (16). Total RNA (1 µg) was
reverse-transcribed into cDNA in a total volume of 20 µl using the
RT Reaction kit (Promega Corporation, Madison, WI, USA), according
to the manufacturer's protocols. RT-qPCR was conducted with the
Express SYBR-GreenER qPCR Supermix Universal kit (Invitrogen;
Thermo Fisher Scientific, Inc., Waltham, MA, USA), according to the
manufacturer's protocols, on a Rotor-gene 6000 system (Qiagen China
Co., Ltd., Shanghai, China). A total of 25 µl PCR mixture contained
2 µl the reverse-transcribed product, 12.5 µl SYBR-Green Supermix,
8.5 µl RNase-free water, and 1 µl each of forward and reverse
primers. The reaction was run in a 72-well optical plate in
triplicate. The first step of the thermal-cycling program was
initial denaturation at 95°C for 10 sec, followed by 40 cycles of
95°C for 5 sec and 60°C for 30 sec as the second step. A
melting-curve analysis was performed to ensure specificity of the
PCR products. The following primers were employed: H-TIM-3 forward,
5′-GTGACTCTAGCAGACAGTGGGAT-3′ and reverse,
5′-TGACCTTGGCTGGTTTGATG-3′, and β-actin forward,
5′-CACCCAGCACAATGAAGATCAAGAT-3′ and reverse,
(5′-CCAGTTTTTAAATCCTGAGTCAAGC-3′). β-actin was used as the internal
control.
Western blot analysis
The osteosarcoma cell lines and osteoblast cell line
(2×106 cells/ml) were harvested and washed three times
with cold PBS. Cells were lysed in ice-cold lysis buffer (50 mM
Tris-HCl, pH 7.4, 250 mM NaCl, 50 mM NaF, 5 mM EDTA, 0.1% Triton
X-100 and 0.1 mM Na3VO4). Following
centrifugation at 12,000 × g for 15 min at 4°C to remove all
organelles, the supernatants were removed, and the protein levels
were estimated using a Super-Bradford Protein assay kit (CoWin
Biosciences Co., Ltd., Beijing, China), according to the
manufacturer's protocol. Equal amounts of proteins (20 µg/lane)
were denatured in SDS-PAGE buffer, resolved by SDS-PAGE on a 12%
Tris-glycine gel and transferred onto PVDF membranes. Membranes
were blocked with 5% skimmed milk in TBS containing 0.1% Tween-20
(TBST) for 1 h at room temperature. After washing with TBST three
times, membranes were incubated with a primary antibody against
TIM-3 (1:100; cat. no. 1315; Sigma-Aldrich; Merck KGaA; Darmstadt,
Germany) or β-actin (cat. no. abs20002; Absin Bioscience Co., Ltd.
Shanghai, China) overnight at 4°C in TBST. After incubation with
horseradish peroxidase-conjugated goat anti-rabbit IgG (1:10,000;
cat. no. BA1055; Boster Biological Technology) in TBST at room
temperature for 60 min, bands were detected using enhanced
chemiluminescence detection system (APG Bio Ltd., Shanghai, China).
ImageJ version 1.0 (National Institutes of Health, Bethesda, MD,
USA) was used for quantitative analysis of the bands. To account
for any differences in loading, target band densitometries were
divided by the density of β-actin obtained from the same lane.
Statistical analysis
The SPSS 20.0 software (IBM Corp., Armonk, NY, USA)
was used to analyze the data. Data are presented as the mean ±
standard deviation and categorical data were tested using a t-test
or a Wilcoxon signed-rank test. All the tests in the present study
were two-sided. The expression of TIM-3 and the clinical and
pathological factors were analyzed using a χ2 test or a
Fisher's exact test. Spearman's correlation analysis was performed
to investigate the correlation between TIM-3 mRNA and protein
expression levels. Overall survival time was defined as the time
from cancer diagnosis until the patient succumbed to the disease.
Survival was assessed by the Kaplan-Meier method, and differences
between curves were estimated by the log-rank test. P<0.05 was
considered to indicate a statistically significant difference.
Results
Baseline characteristics of
patients
The clinical characteristics of the 38 patients with
osteosarcoma are detailed in Table
I. TIM-3 expression levels were evaluated by tissue type, sex,
age, pathological type, Enneking stage, surgical status, and
survival (Table II). Table III presents the association between
TIM-3 expression and prognosis of the patients with osteosarcoma.
Significant associations were observed between TIM-3 expression and
the type of tissue (P<0.001), surgical status (P=0.008), and
survival (P<0.001), among the patients with osteosarcoma;
however, no significant associations between TIM-3 with the other
parameters, such as sex, age, Enneking stage and pathological
classification were detected (Table
III).
 | Table I.The clinical characteristics of the 38
patients with osteosarcoma. |
Table I.
The clinical characteristics of the 38
patients with osteosarcoma.
| Clinical
characteristics | Cases | Percent (%) |
|---|
| Age (years) |
|
>40 | 12 | 31.58 |
|
20-40 | 5 | 13.16 |
|
<20 | 21 | 55.26 |
| Sex |
| Male | 26 | 68.42 |
|
Female | 12 | 31.58 |
| WHO Pathological
classification |
|
Conventional osteosarcoma | 27 | 71.05 |
|
Telangiectatic
osteosarcoma | 3 | 7.89 |
| Parosteal
osteosarcoma | 2 | 5.26 |
| Small
round cell osteosarcoma | 2 | 5.26 |
| Fibrous
tissue osteosarcoma | 1 | 2.63 |
| Other |
| Tumor
location | 3 | 7.89 |
|
Femur | 20 | 52.63 |
| Shin | 11 | 28.95 |
|
Other | 7 | 18.42 |
| Enneking |
| IIB | 19 | 50.00 |
| III | 19 | 50.00 |
| Surgical |
|
Salvage | 11 | 28.95 |
|
Amputation | 27 | 71.05 |
| Overall survival
time |
| Yes | 16 | 42.11 |
| No | 22 | 57.89 |
 | Table II.Association between TIM-3 expression
and clinicopathological parameters. |
Table II.
Association between TIM-3 expression
and clinicopathological parameters.
|
| Immunohistochemical
staining score |
|---|
|
|
|
|---|
| Classification | − | + | ++ | +++ |
|---|
| Tissue types |
|
|
|
|
| Adjacent
tissues | 7 | 9 | 2 | 1 |
| Tumor
tissues | 2 | 6 | 6 | 24 |
| Sex |
|
|
|
|
| Male | 2 | 1 | 5 | 12 |
|
Female | 3 | 2 | 4 | 9 |
| Age (years) |
|
|
|
|
|
>40 | 2 | 1 | 4 | 8 |
|
20-40 | 0 | 2 | 4 | 6 |
|
<20 | 1 | 2 | 7 | 9 |
| WHO Pathological
classification |
|
|
|
|
|
Conventional osteosarcoma | 2 | 3 | 8 | 14 |
|
Telangiectatic
osteosarcoma | 0 | 0 | 1 | 2 |
|
Parosteal osteosarcoma | 0 | 1 | 0 | 1 |
| Small
round cell osteosarcoma | 0 | 0 | 1 | 1 |
| Fibrous
tissue osteosarcoma | 0 | 1 | 0 | 0 |
|
Other | 0 | 1 | 2 | 0 |
| Enneking |
|
|
|
|
|
IIB | 2 | 5 | 8 | 4 |
|
III | 1 | 2 | 5 | 11 |
| Surgical type |
|
|
|
|
|
Salvage | 3 | 5 | 2 | 1 |
|
Amputation | 2 | 4 | 9 | 12 |
| Overall survival
time |
|
|
|
|
|
Yes | 4 | 8 | 3 | 1 |
| No | 1 | 2 | 4 | 15 |
 | Table III.Association between TIM-3 expression
and prognosis in patients with osteosarcoma. |
Table III.
Association between TIM-3 expression
and prognosis in patients with osteosarcoma.
| Variables | Negative | Positive | P-value |
|---|
| Tissue types |
|
| <0.001 |
|
Adjacent tissues | 16 | 3 |
|
| Tumor
tissues | 8 | 30 |
|
| Sex |
|
| 0.438 |
|
Male | 3 | 17 |
|
|
Female | 5 | 13 |
|
| Age (years) |
|
| 1.000 |
|
>40 | 3 | 12 |
|
|
20-40 | 2 | 10 |
|
|
<20 | 3 | 16 |
|
| WHO Pathological
classification |
|
| 0.278 |
|
Conventional osteosarcoma | 5 | 22 |
|
|
Telangiectatic
osteosarcoma | 0 | 3 |
|
|
Parosteal osteosarcoma | 1 | 1 |
|
| Small
round cell osteosarcoma | 0 | 2 |
|
| Fibrous
tissue osteosarcoma | 1 | 0 |
|
|
Other | 1 | 2 |
|
| Enneking |
|
| 0.269 |
|
IIB | 7 | 12 |
|
|
III | 3 | 16 |
|
| Surgical type |
|
| 0.008 |
|
Salvage | 8 | 3 |
|
|
Amputation | 6 | 21 |
|
| Overall survival
time |
|
| <0.001 |
|
Yes | 12 | 4 |
|
| No | 3 | 19 |
|
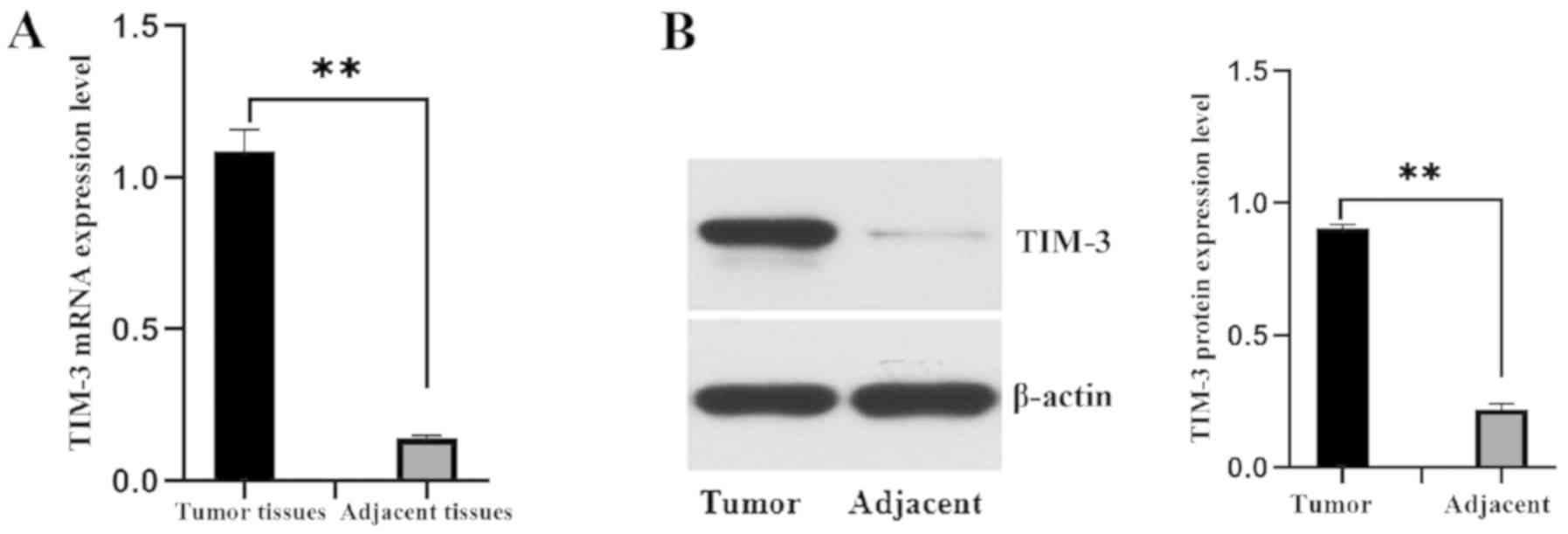
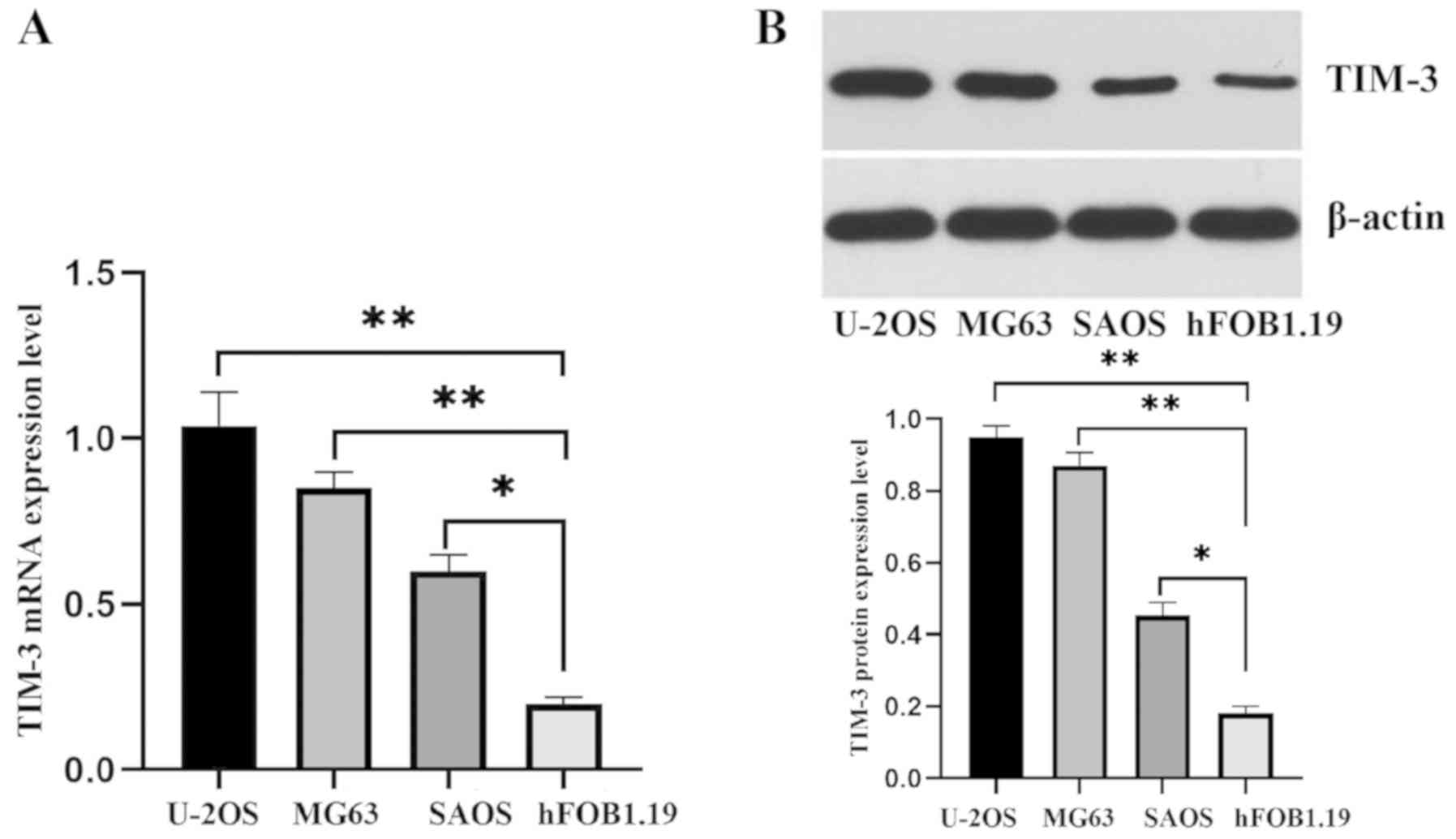
Detection of TIM-3 mRNA and protein
expressions in osteosarcoma tissues and cell lines
RT-qPCR and western blot analysis were conducted to
assess TIM-3 expression levels in fresh tumor tissue samples and
adjacent-tissue samples. TIM-3 was indicated to have an increased
expression in tumor tissue samples (P<0.001; Fig. 1). Subsequently, RT-qPCR and western
blot analysis were carried out to analyze the TIM-3 expression
levels in human osteosarcoma cell lines, U-2OS, MG63, and SAOS and
in osteoblastic cell line hFOB1.19. TIM-3 indicated an increased
expression level in U-2OS, MG63, and SAOS cells, however, not in
hFOB1.19 cells (P<0.001; Fig.
2).
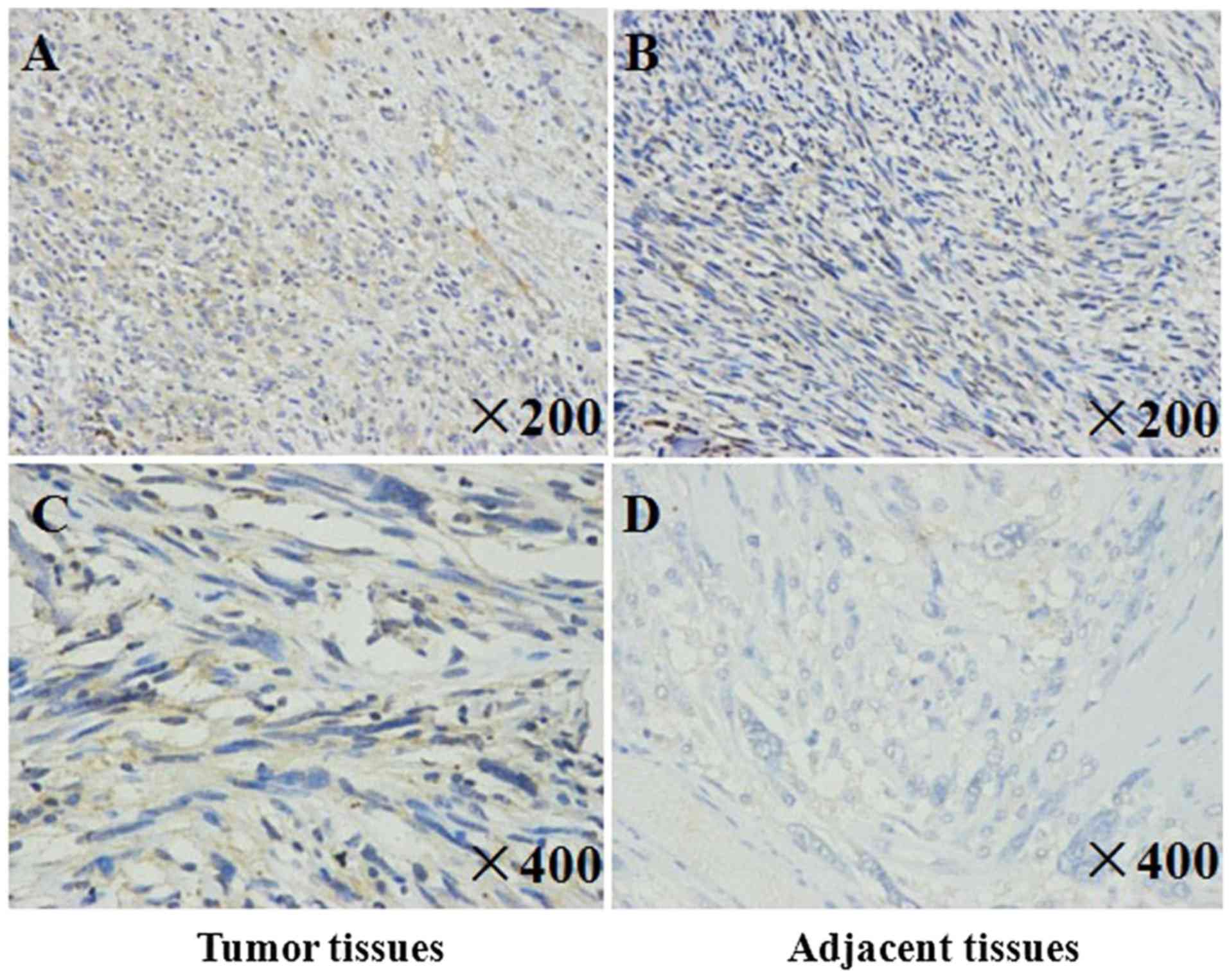
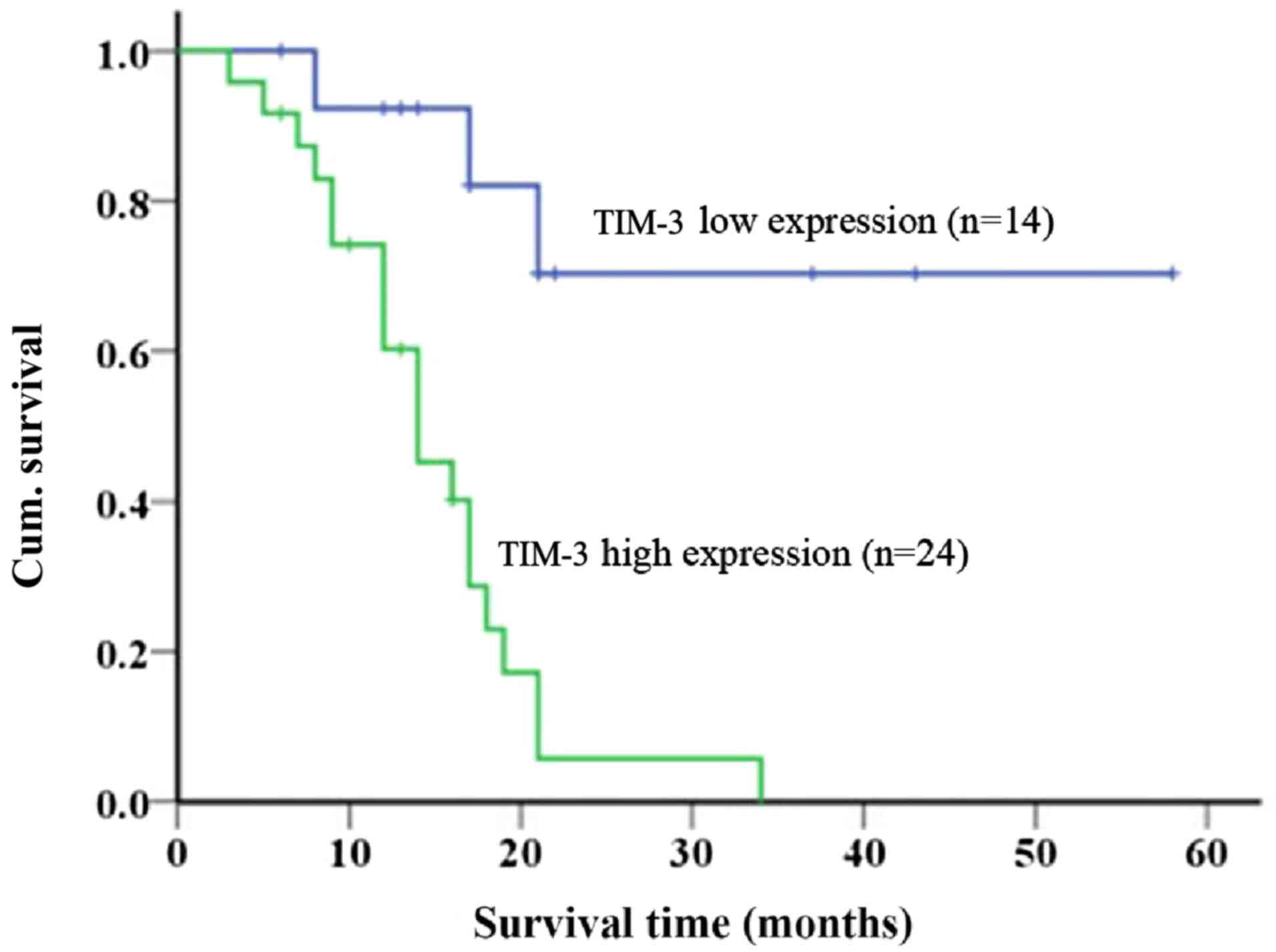
Immunohistochemistry of TIM-3 protein
expression and survival analysis
The positive expression of TIM-3 was showed as
brown-yellow granules and located in the cytoplasm and/or membrane
of tumor cells. Among 38 osteosarcoma tumor tissues, 36 tumor
tissues showed positive expression of TIM-3, with a positive
expression rate of 94.74%; among 19 adjacent-tissues, 12 specimens
showed positive expression of TIM-3, with a positive expression
rate of 63.16% (P<0.001). The IHC staining score of TIM-3
expression in primary osteosarcoma tissue samples was notably
higher compared with adjacent-tissue samples (Fig. 3). As presented in Fig. 4, the Kaplan-Meier analysis predicted
that patients with high TIM-3 expression (n=24) would have shorter
overall survival compared with patients with low TIM-3 expression
(n=14) (P<0.001). This result suggests that high TIM-3
expression is significantly associated with an increased risk of
mortality.
Discussion
Osteosarcoma is a cancer originating from primitive
mesenchymal cells and is the most common type of primary malignant
bone tumor in children and adolescents (17). With advances in multimodal treatments
consisting of adjuvant chemotherapy and surgical resection, the
prognosis and quality of life of patients with non-metastatic
osteosarcoma of the extremities have improved. However, the 5-year
progression-free survival of patients with high-grade osteosarcoma
is only 50%, due to a poor response to chemotherapy (18). Therefore, it is necessary to devise
novel therapeutic strategies for improving the overall rate of
survival.
In a study by Shang et al (19), TIM-3 expression resulted in tumor
cells acquiring features associated with aggressive
epithelial-mesenchymal transition and thus may be involved in the
pathogenesis of osteosarcoma (19).
A recent study revealed that aberrant expression of the TIM-3
antigen on peripheral blood T cells is associated with progressive
disease in patients with osteosarcoma, and TIM-3 may be a possible
diagnostic biomarker of osteosarcoma and/or a prognostic biomarker
of osteosarcoma progression (20).
In the present study, TIM-3 expression was assessed
by IHC staining in osteosarcoma tissue samples. The association
between TIM-3 expression and survival was examined. An increase in
TIM-3 expression was indicated to be associated with surgical
status and survival. Kaplan-Meier analysis indicated that TIM-3 is
an independent predictor of overall survival, and that its
overexpression is associated with poor survival among patients with
osteosarcoma. Piao et al (21) reported positive staining for TIM-3 in
prostate cancer tissues by IHC analysis, however, little or no
staining for TIM-3 has been observed in an epithelium containing
benign prostate hyperplasia (21).
TIM-3 may affect the development and progression of prostate
cancer, as this result may assist in the future use TIM-3 as a
novel therapeutic target for effective prostate cancer management
(21). Additionally, RT-qPCR and
western blot analysis were conducted in the present study to
evaluate TIM-3 expression levels in fresh tumor tissue samples,
adjacent-tissue samples, osteosarcoma cell lines, and in an
osteoblastic cell line. TIM-3 was increasing expressed in fresh
tumor tissue samples and osteosarcoma cells. Nonetheless, further
studies are required, in order to clarify the underlying biology of
TIM-3 in the development of osteosarcoma.
In conclusion, the results of the present study
revealed that high TIM-3 expression is significantly associated
with poor survival and may be an independent predictor of survival
among patients with osteosarcoma. TIM-3 expression was indicated to
be a valuable prognostic biomarker of osteosarcoma.
Acknowledgements
Not applicable.
Funding
The present study was supported by National Natural
Science Foundation of China (grant no. 81904231), the Scientific
Research Program of Wuhan Health and Family Planning (grant no.
WX17Q38 and WZ18Q05) and the Research Program of Wuhan No. 1
Hospital, Wuhan Integrated TCM and Western Medicine Hospital (grant
no. 2017Y01).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
FP, FC, ZZ and XQ performed the experiments and
wrote the manuscript. PX and ZS made substantial contributions to
conception and design of the manuscript. PX and ZWS were
responsible for the design of the experiments. HL and LZ analyzed
the experimental data. HL, LZ, ZZ and XQ assisted with the
statistical analysis. ZZ and XQ critically revised the manuscript
and provided final approval of the version to be published and also
made substantial contributions to conception and design. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by The Ethics
Committee of Union Hospital Tongji Medical College of Huazhong
University of Science and Technology (Wuhan, China) and conforms to
the provisions of the Declaration of Helsinki. All patients and
legal guardians provided written informed consent regarding human
tissue acquisition used in the present study, in accordance with
National Regulations on the Use of Clinical Samples in China.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Biermann JS, Adkins DR, Agulnik M,
Benjamin RS, Brigman B, Butrynski JE, Cheong D, Chow W, Curry WT,
Frassica DA, et al: Bone cancer. J Natl Compr Canc Netw.
11:688–723. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lindsey BA, Markel JE and Kleinerman ES:
Osteosarcoma overview. Rheumatol Ther. 4:25–43. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
He JP, Hao Y, Wang XL, Yang XJ, Shao JF,
Guo FJ and Feng JX: Review of the molecular pathogenesis of
osteosarcoma. Asian Pac J Cancer Prev. 15:5967–5976. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mirabello L, Troisi RJ and Savage SA:
Osteosarcoma incidence and survival rates from 1973 to 2004: Data
from the Surveillance, Epidemiology, and End Results Program.
Cancer. 115:1531–1543. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Liu S, Geng P, Cai X and Wang J:
Comprehensive evaluation of the cytotoxic T-lymphocyte antigen-4
gene polymorphisms in risk of bone sarcoma. Genet Test Mol
Biomarkers. 18:574–579. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Fan Y, Zhang C, Jin S, Gao Z, Cao J, Wang
A, Li D, Wang Q, Sun X and Bai D: Progress of immune checkpoint
therapy in the clinic (Review). Oncol Rep. 41:3–14. 2019.PubMed/NCBI
|
|
7
|
Wang SD, Li HY, Li BH, Xie T, Zhu T, Sun
LL, Ren HY and Ye ZM: The role of CTLA-4 and PD-1 in anti-tumor
immune response and their potential efficacy against osteosarcoma.
Int Immunopharmacol. 38:81–89. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ledford H, Else H and Warren M: Cancer
immunologists scoop medicine Nobel prize. Nature. 562:20–21. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gibney GT, Weiner LM and Atkins MB:
Predictive biomarkers for checkpoint inhibitor-based immunotherapy.
Lancet Oncol. 17:e542–e551. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Markwick LJ, Riva A, Ryan JM, Cooksley H,
Palma E, Tranah TH, Manakkat Vijay GK, Vergis N, Thursz M, Evans A,
et al: Blockade of PD1 and TIM3 restores innate and adaptive
immunity in patients with acute alcoholic hepatitis.
Gastroenterology. 148:590–602.e10. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Das M, Zhu C and Kuchroo VK: Tim-3 and its
role in regulating anti-tumor immunity. Immunol Rev. 276:97–111.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Sakuishi K, Ngiow SF, Sullivan JM, Teng
MW, Kuchroo VK, Smyth MJ and Anderson AC:
TIM3+FOXP3+ regulatory T cells are
tissue-specific promoters of T-cell dysfunction in cancer.
Oncoimmunology. 2:e238492013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li Z, Li N, Li F, Zhou Z, Sang J, Chen Y,
Han Q, Lv Y and Liu Z: Immune checkpoint proteins PD-1 and TIM-3
are both highly expressed in liver tissues and correlate with their
gene polymorphisms in patients with HBV-related hepatocellular
carcinoma. Medicine (Baltimore). 95:e57492016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Present D, Bertoni F, Hudson T and
Enneking WF: The correlation between the radiologic staging studies
and histopathologic findings in aggressive stage 3 giant cell tumor
of bone. Cancer. 57:237–244. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fletcher CDM, Bridge JA, Hogendoorn P and
Mertens F: WHO classification of tumours of soft tissue and
boneLyon: IARC Press; pp. 239–394. 2013
|
|
16
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sarsilmaz A, Argin M, Sezak M, Altay C and
Erdogan N: Primary osteosarcoma arising from subcutaneous tissue:
5-year follow-up. Clin Imaging. 36:402–405. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mavrogenis AF, Rossi G, Palmerini E,
Errani C, Rimondi E, Ruggieri P, Soucacos PN and Papagelopoulos PJ:
Palliative treatments for advanced osteosarcoma. J BUON.
17:436–445. 2012.PubMed/NCBI
|
|
19
|
Shang Y, Li Z, Li H, Xia H and Lin Z:
TIM-3 expression in human osteosarcoma: Correlation with the
expression of epithelial-mesenchymal transition-specific
biomarkers. Oncol Lett. 6:490–494. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu H, Zhi L, Duan N and Su P: Abnormal
expression of Tim-3 antigen on peripheral blood T cells is
associated with progressive disease in osteosarcoma patients. FEBS
Open Bio. 6:807–815. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Piao YR, Jin ZH, Yuan KC and Jin XS:
Analysis of Tim-3 as a therapeutic target in prostate cancer.
Tumour Biol. 35:11409–11414. 2014. View Article : Google Scholar : PubMed/NCBI
|