Estrogens, including estrone, estriol and the
biologically active metabolite 17β-estradiol (E2), have long been
considered important regulators of female reproductive functions
and are primarily produced in the ovaries. In addition to the
ovaries, several extragonadal tissues, such as the mesenchymal
cells in the adipose tissue of the breast, osteoblasts,
chondrocytes, aortic smooth muscle cells, vascular endothelium and
numerous parts of the brain also produce estrogens (1). Estrogens have been demonstrated to
serve functions outside of the female reproductive system,
including in the cardiovascular system and the central nervous
system, and function to regulate bone density, brain function,
cholesterol mobilization and electrolyte balance (2,3). In
contrast to women, men are largely dependent on the local synthesis
of estrogens in extragonadal target tissues. This local production
of estrogens encompasses the signaling modality from endocrine to
paracrine, autocrine and intracrine signaling (4). Both estrogen and estrogen receptors
have numerous effects on various organs and diseases specific to
the gastrointestinal (GI) tract. For example, estrogen and estrogen
receptors have been demonstrated to serve pathophysiological roles
in gastroesophageal reflux disease, esophageal cancer, peptic ulcer
disease, gastric cancer, irritable bowel syndrome, inflammatory
bowel disease and colon cancer (5–7).
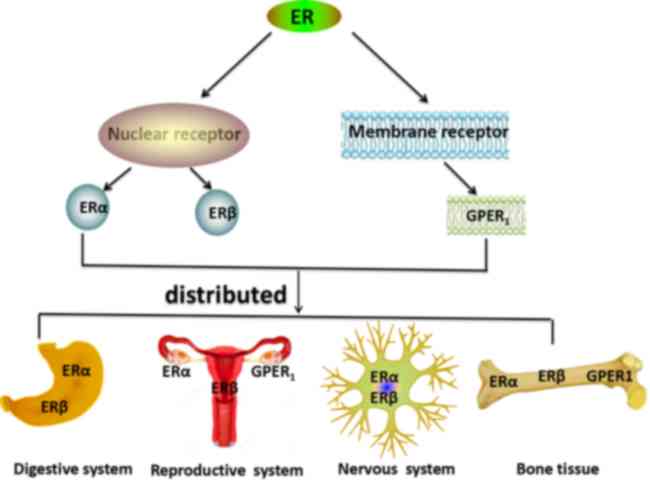
The estrogen receptor has three subtypes; estrogen
receptor α (ERα), estrogen receptor β (ERβ), which belong to
nuclear receptors and membrane receptors, such as G protein-coupled
estrogen receptor 1 (GPER1, also known as GPR30), which mediate all
of estrogens effects, and the expression of each receptor is
largely tissue-type specific (3)
(Fig. 1).
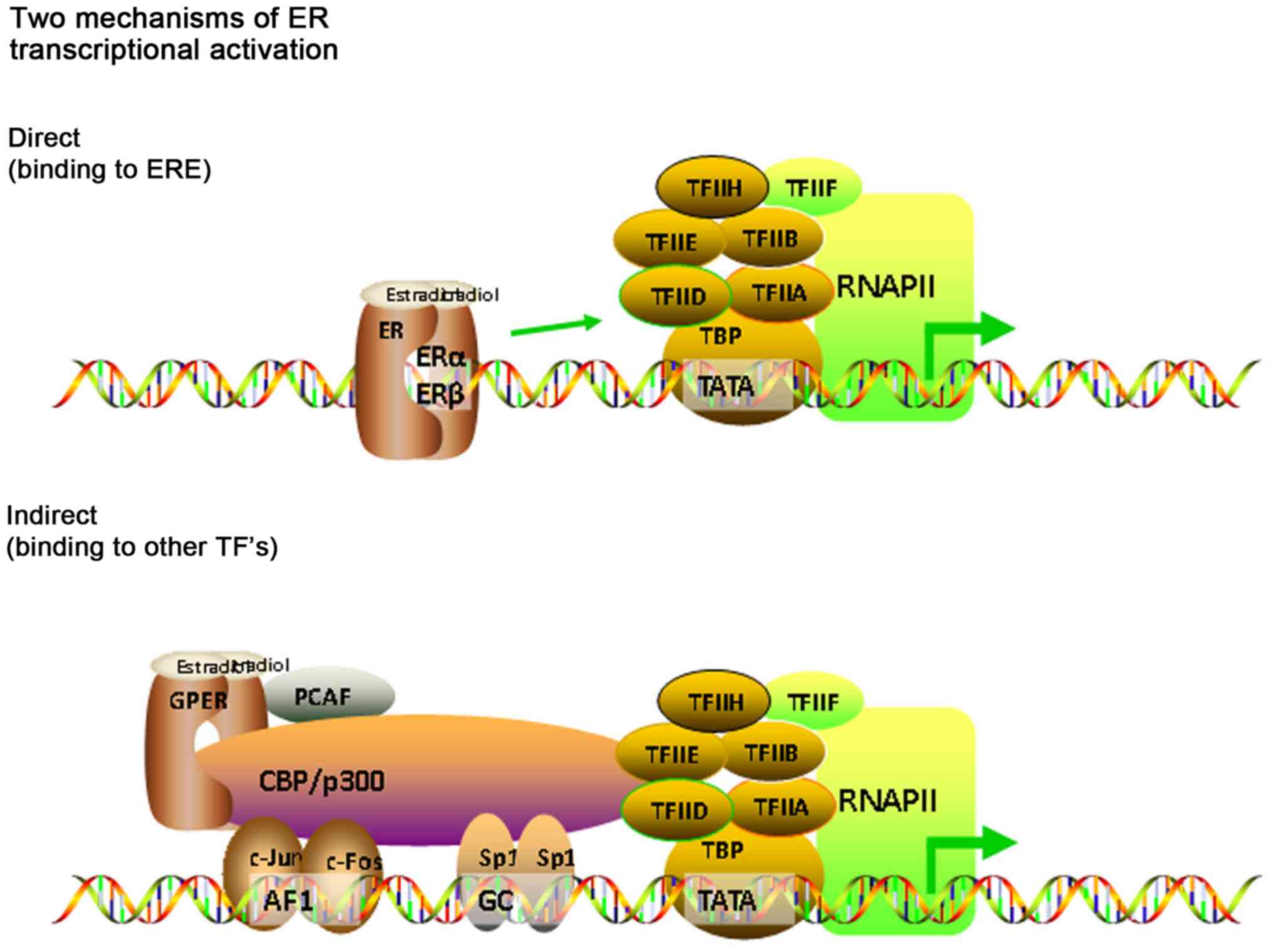
ERα and ERβ have similar structures, and were
respectively identified and cloned in 1986 and 1996 (8). Both ERα and ERβ have distinct cellular
distributions and regulate separate sets of genes (9). ERα is encoded by estrogen receptor 1
which is located on chromosome 6q25.1, and ERβ is encoded by
estrogen receptor 2 or estrogen receptor 2, which is located on
chromosome 14q22-24 (10). ERα is
primarily expressed in female sex organs, such as the breast,
uterus and ovaries. ERα has three known isoforms; two shorter ERα
isoforms which lack the N-terminal domain, and a full-length ERα
isoform. The truncated isoforms can heterodimerize with the
full-length ERα isoform and repress ERα activity. ERβ is expressed
in different types of tissues and cells, and to a higher degree in
females compared with males (11).
ERβ has at least five different isoforms; four shorter ERβ isoforms
and a full-length ERβ isoform. The four shorter ERβ isoforms
exhibit reduced ligand binding activity (12). The ERβ isoforms are neither
homodimerizable nor transcriptionally active (12). However, they can preferentially
dimerize with ERα. The ERα and ERβ isoforms have different effects
on estrogen signaling and target gene regulation (12) (Fig.
2).
Although, ERα, ERβ and GPER1 possess a similar
structure, they regulate divergent functions. In the present
review, the role of estrogen and ERs in the physiology and
pathology of the digestive system are explored.
However, contradictory studies have shown that
estrogen and estrogen receptor agonists are associated with an
increased risk of gastroesophageal reflux disease symptoms
(28–31). Female sex hormones can relax the
lower esophageal sphincter and increase the risk of
gastroesophageal reflux symptoms (32). Previously, it has been demonstrated
that there is a positive correlation between gastroesophageal
reflux symptoms and postmenopausal hormone replacement therapy
(HRT) (31).
Furthermore, women whom have never taken
postmenopausal hormone therapies, have a lower risk of reflux
symptoms compared with women who have or are still taking estrogen
replacement therapy (28). There is
a positive correlation between the risk of reflux symptoms,
increased estrogen dose and increased duration of estrogen use.
Jacobson et al (28) showed
an odds ratio of 1.39 for reflux symptoms that used a selective
estrogen receptor modulator, and an odds ratio of 1.37 for women
who used over-the-counter hormone preparations (28). Therefore, it is important to
understand the role of estrogen and estrogen receptors in the
pathogenesis of GERD.
EC is one of the deadliest malignancies of the GI
tract and causes >400,000 deaths each year. The two most common
histological subtypes are esophageal adenocarcinoma (EAC) and
esophageal squamous cell carcinoma (ESCC) (33). The incidence of EAC was 6–10× lower
in women compared with men, and that ESCC incidence was 2–3× lower
(34). Mathieu et al
(35) analyzed the prevalence of EC
by histology and gender differences between 1973 and 2008 in nine
population-related cancer studies, and the incidence of EAC
increased in both males and females over this time period.
Furthermore, the ratio of EAC in male vs. female was highest in
individuals aged 50–54. The risk of EAC age-based incidence rate in
postmenopausal females aged 80 increased significantly, and this
trend was not seen in similarly aged males. Overall,
estrogen-related endocrine milieu in premenopausal and
perimenopausal females serves as a protective factor in the
prevention of EAC, and with loss of estrogen in the body or an
increase in time without estrogen-mediated maintenance, the
prevalence of EAC incidence increases in older postmenopausal
females. A total of 16 independent studies were analyzed by Wang
et al (36), and the results
showed that estrogen can lower the risk of EC. The relative risks
were pooled and they showed a negative correlation between the risk
of EC and hormone replacement therapy. In addition, menopausal
women were at an increased risk of EAC compared with EC (36). The serum levels of estradiol in a
healthy cohort from a high-incidence area (HIA) and a low-incidence
area for esophageal cancer, as well as that of patients with ESCC
from a HIA in Hena, China were assessed, and it showed that lower
serum levels of estradiol were associated with a higher
predisposition for developing ESCC (37). Furthermore, Zhang et al
(38) demonstrated that 17β-E2, but
not 17α-E2, decreased proliferation of human ESCC cells in a
dose-dependent manner, and this was attenuated by ICI1 82780 (an
estrogen receptor antagonist). 17β-E2 promotes intracellular
calcium mobilization and extracellular calcium entry into ESCC
cells, and estrogen exerted an antiproliferative effect on human
ESCC cells, likely through an estrogen receptor-calcium signaling
pathway. According to Hennessy et al (39), the antiproliferative effects of
17β-E2 may occur through the ERβ estrogen receptor. Zuguchi et
al (40) examined the expression
status of both ERα and ERβ in 90 Japanese patients with ESCC and
demonstrated that both ERα and ERβ were upregulated in ECGI-10
cells (an ESCC cell line). Additionally, the status of ERβ in ESCC
was closely associated with unfavorable outcomes, possibly through
increasing proliferation of carcinoma cells.
Taken together, these results indicate that estrogen
and estrogen receptors inhibit growth of esophageal cancer by
estradiol (41). Furthermore,
estrogen replacement in postmenopausal women serves as a protective
factor against esophageal cancer by reducing the degree of damage
to esophageal tissues caused by gastric acid (42). Estrogen can reduce the risk of
esophageal cancer. Therefore, a reduction or lack of estrogen may
be an important factor in the high incidence of esophageal cancer
in men and postmenopausal women.
Peptic ulcers include both gastric and duodenal
ulcers, and complications include upper GI bleeding, GI perforation
and gastric outlet obstruction (43). Peptic ulcer disease is a
multifactorial and complex digestive disease, and its pathogenesis
is unclear (44). Gastric protective
factors include mucous, endogenous bicarbonate, prostaglandins and
antioxidant agents; whereas, pepsin, gastric acid, bile acids and
endogenous oxidant agents are recognized as risk factors that could
cause damage to the stomach (45).
Acid secretion, and the pH values of the stomach and duodenum did
not differ between males and females (46). Peptic ulcers are relatively rare
during pregnancy, and estrogen exhibits a protective effect against
the incidence and severity of peptic ulcers, and the risk of ulcers
is lower in women compared with men (6,47). Okada
et al (48) found that
individuals >70 years in age, had an increased prevalence of
ulcers and this was also true in postmenopausal women. The decrease
in the serum levels of estrogen induced a reduction in gastric
mucosal defenses. Additionally, another study suggested that
estrogen exerts an antioxidant effect, which directly scavenges
free oxygen radicals, activates antioxidant enzymes, represses the
production of superoxides and reduces the formation of peptic
ulcers (49).
Therefore, estrogen exhibits a protective effect
from peptic ulcers, which may be achieved through its antioxidant
effects. However, the specific mechanisms underlying its protective
effects require further study.
GC is a malignant tumor and the fifth highest
incidence and third highest mortality rates in the world (50). Epidemiological studies have suggested
that the prevalence of gastric cancer is higher in men than women
with a ratio of 1.2:1.0 male:female. However, the differences
between male and females becomes negligible when compared with
postmenopausal women (51). Tokunaga
et al (52) first reported
the relationship between hormone receptors and GC, and they
highlighted the fact that estrogens may serve a protective role
against gastric cancer. Lindblad et al (53) found that the probability of
developing gastric cancer was not increased in patients with
prostate cancer. In addition, Furukawa et al (54) found that female, castrated male and
estrogen-treated male rats had a lower incidence of gastric cancer
with lower histological differentiation compared with that in
non-treated male rats after administration of the carcinogen,
N-methyl-N0-nitro-N-nitrosoguanidine, and untreated male rats had
increased rates of morbidity as a result of gastric cancer compared
with castrated or estrogen-treated male rats.
The expression of ERα and ERβ in gastric cancer has
been previously demonstrated (55).
It has been hypothesized that ERs serve an important role in the
occurrence and development of gastric cancer (56). Studies have demonstrated that ERβ,
but not ERα, is abundantly expressed in GC (57–61).
However, other researchers have demonstrated the expression of both
receptors in GC (62–64). Zhou et al (65) found that the expression of β-catenin
was reduced when ERα was overexpressed, and this resulted in a
decrease in growth and proliferation of GC cells, and an increase
in the apoptotic rate by preventing entry into the
G1/G0 phase. ER-α is considered a rare
subtype of estrogen receptor ERα, which is associated with
increased lymph node metastasis and invasion in GC. Non-genomic
estrogen signaling mediated by ER-α was involved in the c-Src
signaling pathway in SGC7901 GC cells (66). A recent study found that ERα
expression in gastric cancer cells was increased by low
concentrations of 17β-estradiol, which in turn resulted in
increased proliferation by activating mitogen-activated protein
kinase signaling pathway (67). In
addition, knock down of ERα did not affect the proliferation,
migration and invasion of gastric cancer cells (67). Compared with expression of ERα,
expression of ERβ in noncancerous tissues was significantly higher
in female rats compared with male rats (68). Ryu et al (61) evaluated the presence of ERβ in
gastric cancer and showed that ERβ was likely not a contributing
factor for the invasiveness of gastric cancer.
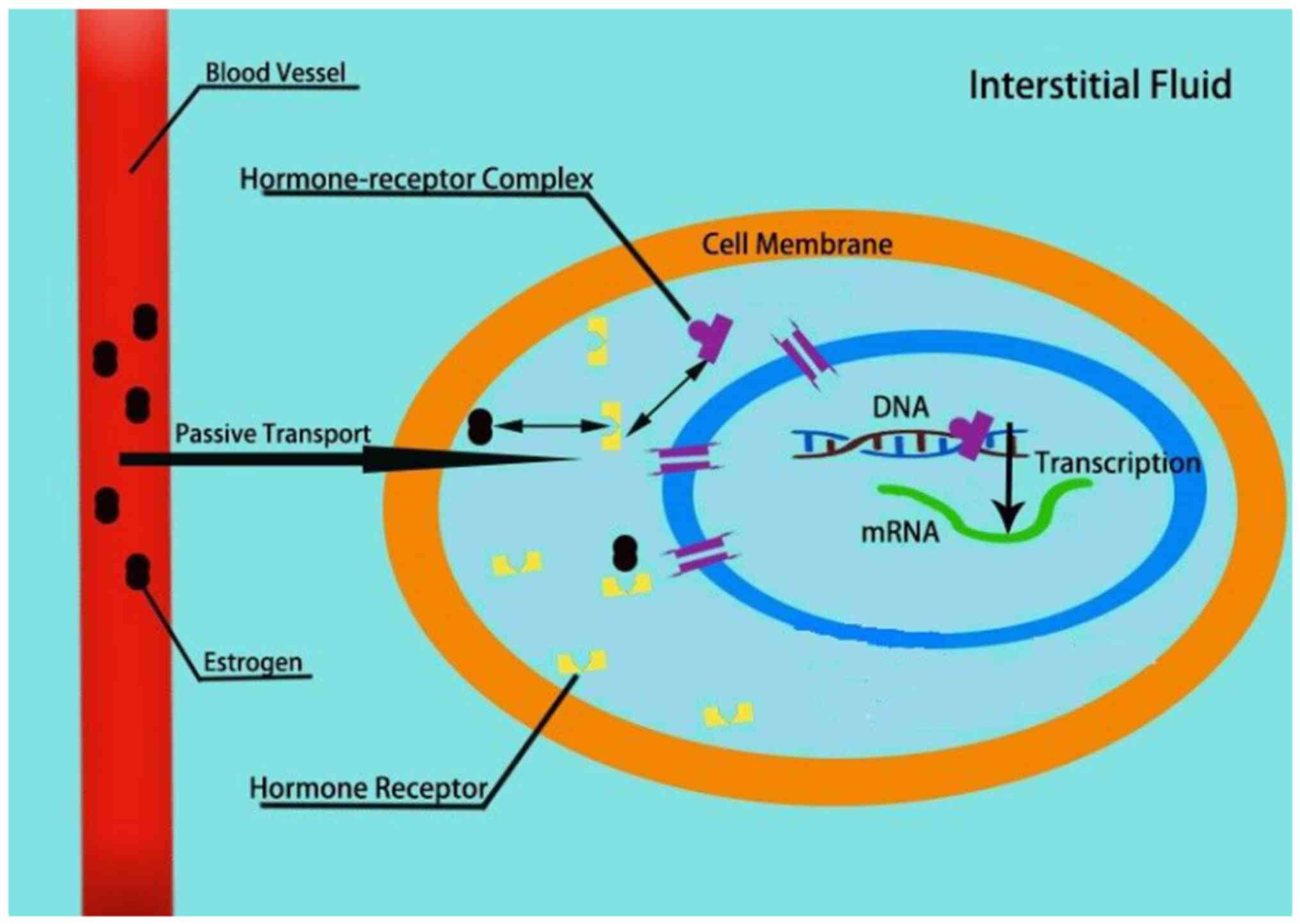
Therefore, investigating the roles and mechanisms of
ER and its receptors may highlight potential mechanisms to improve
management of the disease (Fig.
3).
Irritable bowel syndrome is one of the most common
GI disorders, and is typically characterized by disorderly bowel
movements and chronic abdominal pain (69). Based on epidemiological studies
(70–72), irritable bowel syndrome is more
prevalent in women than men, with a ratio range of 2–4:1,
highlighting the possibility of the involvement of estrogen serving
a role in the pathophysiology of IBS (7). IBS symptoms were determined to be
associated with hormonal status, and the role of sex steroid
hormones in the pathophysiology of IBS is gaining increasing
attention (73). Studies have
demonstrated that estrogen participates in modulating visceral
sensitivity and regulating motor and sensory functions in IBS
animal models (74,75). Additionally, Jacenik et al
(76) determined the estrogen
receptor engagement in the IBS subtypes, constipation predominant
IBS and diarrhea predominant IBS (IBS-D). The authors analyzed
whether estrogen signaling was accompanied by alterations in the
expression of pro-inflammatory and anti-inflammatory cytokines and
microRNAs, which regulate genes associated with the immune
response. Both ERα and GPER expression were upregulated in IBS.
There was a correlation between the expression of GPER in patients
with IBS-D and the severity of abdominal pain, and an association
between the GPER-mediated estrogenic effects on IBS pathogenesis
and activation of mast cells in the colon, thus highlighting a
novel avenue for understanding the pathogenesis of sex differences
in IBS (77). GPER-mediated
estrogenic effects were involved in the regulation of visceral pain
and GI motility (78).
IBD is an intestinal inflammatory disease, which is
incompletely understood. There is a lack of clear understanding of
the pathogenesis of IBD and established effective treatments
(79). Previously, patients with IBD
were diagnosed primarily in North America and Europe (80). As lifestyle, environment and diets of
individuals has changed overtime, the prevalence of IBD has
increased worldwide, particularly in children and adult populations
(81). IBD includes both ulcerative
colitis (UC) and Crohn's disease (CD). The differences in cancer
risk between male and female mice were evaluated for patients with
IBD, and the results showed that IBD conferred a higher risk of
developing colorectal cancer (CRC) in males compared with females.
Colitis is hypothesized to be associated with the development of
IBD (82).
ERβ is the predominant ER subtype expressed in colon
tissues, and it maintains a normal epithelial architecture
protecting against chronic colitis (83–85). Men
present with a higher risk of developing colitis than women,
implicating estrogen as a protective factor against developing
colitis. Armstrong et al (86) found that E2 treatment reduced
inflammation in the colon in control mice. The expression of
interleukins (ILs; particularly IL-6, IL-12 and IL-17),
granulocyte-macrophage colony-stimulating factor, interferon-γ,
monocyte chemotactic proteins-1, macrophage inflammatory protein-1α
and tumor necrosis factor-α were not significantly increased in
control mice following treatment with E2. The extent of damage was
higher in the control ERβ knockout mice compared with the
E2-treated ERβ knockout mice. Additionally, ERβ mRNA expression
levels were decreased in a colitis mouse model of intestinal
inflammation (87). ERβ knockout
mice presented with colitis of increased severity compared with the
wild-type group (88). Therefore, E2
may protect against acute colitis through the activation of
ERβ.
Colon cancer is one of the most common types of
malignant tumor of the GI tract and the second leading cause of
cancer-associated death worldwide. An epidemiological study of
colon cancer prevalence found that females exhibited a higher
prevalence of colon cancer. However, women aged 18–44 with colon
cancer had an improved prognosis compared with men of the same age
and women >50 years (89).
Upregulated expression of ERβ1 in colon cancer is associated with
an improved survival outcome (90).
Similarly, downregulated expression of ERβ1 is associated with
poorer survival outcome (90).
Numerous studies have demonstrated that hormone replacement therapy
(HRT) in postmenopausal women did not serve a protective role
(91,92), contradicting previous studies
(93,94). The Women's Health Initiative showed
that the prevalence of colon cancer decreased by 30% following
treatment with HRT in postmenopausal women (95).
E2 treatment reinforced hypoxia-associated migration
and proliferation of colon cancer cells, whereas in an aerobic
environment, cell migration and proliferation were decreased by E2
treatment (89). The effects of E2
on the cellular responses in an aerobic environment and anoxic
conditions were mediated by GPER. Therefore, in order to fully
predict the estrogenic response in patients with colon cancer, it
is necessary to understand not only the status of estrogen receptor
expression in tumor cells, but also the aerobic/anoxic conditions
of the local tumor microenvironment (89).
Estrogen is a sex hormone that regulates the
development and function of the reproductive systems in all
mammalian species, and increasing evidence demonstrates the
multifaceted nature of its effects on non-reproductive organs
during physiological and pathophysiological conditions.
Understanding the effects of estrogen and estrogen receptor
function may provide an important theoretical basis for improving
clinical treatments of GI disease.
The authors would like to thank Professor Biguang
Tuo (Department of Gastroenterology, Affiliated Hospital to Zunyi
Medical University) for suggestions for the manuscript.
This study was supported by research grants from the
National Natural Science Foundation of China (grant nos. 81660099
and 81770610).
Data sharing is not applicable to the present study,
as no datasets were generated or analyzed during the current
study.
CMC, XG, XXY, XHS, QD, QSL and RX conceived, wrote
and revised the paper. YSC and JYX wrote and revised the paper. All
authors approved the final version of the manuscript for
submission.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Simpson ER: Sources of estrogen and their
importance. J Steroid Biochem Mol Biol. 86:225–230. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Guyton AC and Hall J: Guyton and Hall
Textbook of Medical Physiology. 957–999. 2011.
|
|
3
|
Nilsson S and Gustafsson JA: Estrogen
receptors: Therapies targeted to receptor subtypes. Clin Pharmacol
Ther. 89:44–55. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Labrie F: Extragonadal synthesis of sex
steroids: Intracrinology. Ann Endocrinol (Paris). 64:95–107.
2003.PubMed/NCBI
|
|
5
|
Kim YS, Kim N and Kim GH: Sex and gender
differences in gastroesophageal reflux disease. J
Neurogastroenterol Motil. 22:575–588. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kurt D, Saruhan BG, Kanay Z, Yokus B,
Kanay BE, Unver O and Hatipoglu S: Effect of ovariectomy and female
sex hormones administration upon gastric ulceration induced by cold
and immobility restraint stress. Saudi Med J. 28:1021–1027.
2007.PubMed/NCBI
|
|
7
|
Meleine M and Matricon J: Gender-related
differences in irritable bowel syndrome: Potential mechanisms of
sex hormones. World J Gastroenterol. 20:6725–6743. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Batistatou A, Stefanou D, Goussia A,
Arkoumani E, Papavassiliou AG and Agnantis NJ: Estrogen receptor
beta (ERbeta) is expressed in brain astrocytic tumors and declines
with dedifferentiation of the neoplasm. J Cancer Res Clin Oncol.
130:405–410. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang H, Sukocheva OA, Hussey DJ and Watson
DI: Estrogen, male dominance and esophageal adenocarcinoma: Is
there a link? World J Gastroenterol. 18:393–400. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Enmark E, Pelto-Huikko M, Grandien K,
Lagercrantz S, Lagercrantz J, Fried G, Nordenskjold M and
Gustafsson JA: Human estrogen receptor beta-gene structure,
chromosomal localization, and expression pattern. J Clin Endocrinol
Metab. 82:4258–4265. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Rochira V, Granata AR, Madeo B, Zirilli L,
Rossi G and Carani C: Estrogens in males: What have we learned in
the last 10 years? Asian J Androl. 7:3–20. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Heldring N, Pike A, Andersson S, Matthews
J, Cheng G, Hartman J, Tujague M, Strom A, Treuter E, Warner M and
Gustafsson JA: Estrogen receptors: How do they signal and what are
their targets. Physiol Rev. 87:905–931. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Carmeci C, Thompson DA, Ring HZ, Francke U
and Weigel RJ: Identification of a gene (GPR30) with homology to
the G-protein-coupled receptor superfamily associated with estrogen
receptor expression in breast cancer. Genomics. 45:607–617. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Filardo EJ and Thomas P: Minireview: G
protein-coupled estrogen receptor-1, GPER-1: Its mechanism of
action and role in female reproductive cancer, renal and vascular
physiology. Endocrinology. 153:2953–2962. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sanden C, Broselid S, Cornmark L,
Andersson K, Daszkiewicz-Nilsson J, Martensson UE, Olde B and
Leeb-Lundberg LM: G protein-coupled estrogen receptor 1/G
protein-coupled receptor 30 localizes in the plasma membrane and
traffics intracellularly on cytokeratin intermediate filaments. Mol
Pharmacol. 79:400–410. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Filardo EJ, Quinn JA, Bland KI and
Frackelton AR Jr: Estrogen-induced activation of Erk-1 and Erk-2
requires the G protein-coupled receptor homolog, GPR30, and occurs
via trans-activation of the epidermal growth factor receptor
through release of HB-EGF. Mol Endocrinol. 14:1649–1660. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Revankar CM, Cimino DF, Sklar LA,
Arterburn JB and Prossnitz ER: A transmembrane intracellular
estrogen receptor mediates rapid cell signaling. Science.
307:1625–1630. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Thomas P, Pang Y, Filardo EJ and Dong J:
Identity of an estrogen membrane receptor coupled to a G protein in
human breast cancer cells. Endocrinology. 146:624–632. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sharma G and Prossnitz ER:
G-protein-coupled estrogen receptor (GPER) and sex-specific
metabolic homeostasis. Adv Exp Med Boil. 1043:427–453. 2017.
View Article : Google Scholar
|
|
20
|
Vakil N, van Zanten SV, Kahrilas P, Dent J
and Jones R; Globale Konsensusgruppe, : The Montreal definition and
classification of gastroesophageal reflux disease: A global,
evidence-based consensus paper. Z Gastroenterol. 45:1125–1140.
2007.(Article in German). View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Katzka DA, Pandolfino JE and Kahrilas PJ:
Phenotypes of gastroesophageal reflux disease: Where rome, lyon,
and montreal meet. Clin Gastroenterol Hepatol. July 15–2019.(Epub
ahead of print). View Article : Google Scholar
|
|
22
|
Nam SY, Choi IJ, Ryu KH, Park BJ, Kim YW,
Kim HB and Kim JS: The effect of abdominal visceral fat,
circulating inflammatory cytokines, and leptin levels on reflux
esophagitis. J Neurogastroenterol Motil. 21:247–254. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pohl H, Wrobel K, Bojarski C, Voderholzer
W, Sonnenberg A, Rosch T and Baumgart DC: Risk factors in the
development of esophageal adenocarcinoma. Am J Gastroenterol.
108:200–207. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Asanuma K, Iijima K and Shimosegawa T:
Gender difference in gastro-esophageal reflux diseases. World J
Gastroenterol. 22:1800–1810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Iijima K and Shimosegawa T: Involvement of
luminal nitric oxide in the pathogenesis of the gastroesophageal
reflux disease spectrum. J Gastroenterol Hepatol. 29:898–905. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Masaka T, Iijima K, Endo H, Asanuma K, Ara
N, Ishiyama F, Asano N, Koike T, Imatani A and Shimosegawa T:
Gender differences in oesophageal mucosal injury in a reflux
oesophagitis model of rats. Gut. 62:6–14. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Boeckxstaens G, El-Serag HB, Smout AJ and
Kahrilas PJ: Symptomatic reflux disease: The present, the past and
the future. Gut. 63:1185–1193. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jacobson BC, Moy B, Colditz GA and Fuchs
CS: Postmenopausal hormone use and symptoms of gastroesophageal
reflux. Arch Intern Med. 168:1798–1804. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Van Thiel DH, Gavaler JS and Stremple J:
Lower esophageal sphincter pressure in women using sequential oral
contraceptives. Gastroenterology. 71:232–234. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Nilsson M, Lundegardh G, Carling L, Ye W
and Lagergren J: Body mass and reflux oesophagitis: An
oestrogen-dependent association? Scand J Gastroenterol. 37:626–630.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nilsson M, Johnsen R, Ye W, Hveem K and
Lagergren J: Obesity and estrogen as risk factors for
gastroesophageal reflux symptoms. JAMA. 290:66–72. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Nordenstedt H, Zheng Z, Cameron AJ, Ye W,
Pedersen NL and Lagergren J: Postmenopausal hormone therapy as a
risk factor for gastroesophageal reflux symptoms among female
twins. Gastroenterology. 134:921–928. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
el-Serag HB: The epidemic of esophageal
adenocarcinoma. Gastroenterol Clin North Am. 31421–440. (viii)2002.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Vizcaino AP, Moreno V, Lambert R and
Parkin DM: Time trends incidence of both major histologic types of
esophageal carcinomas in selected countries, 1973–1995. Int J
Cancer. 99:860–868. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mathieu LN, Kanarek NF, Tsai HL, Rudin CM
and Brock MV: Age and sex differences in the incidence of
esophageal adenocarcinoma: Results from the surveillance,
epidemiology, and end results (SEER) registry (1973–2008). Dis
Esophagus. 27:757–763. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang BJ, Zhang B, Yan SS, Li ZC, Jiang T,
Hua CJ, Lu L, Liu XZ, Zhang DH, Zhang RS and Wang X: Hormonal and
reproductive factors and risk of esophageal cancer in women: A
meta-analysis. Dis Esophagus. 29:448–454. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang QM, Qi YJ, Jiang Q, Ma YF and Wang
LD: Relevance of serum estradiol and estrogen receptor beta
expression from a high-incidence area for esophageal squamous cell
carcinoma in China. Med Oncol. 28:188–193. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhang Z, He Q, Fu S and Zheng Z: Estrogen
receptors in regulating cell proliferation of esophageal squamous
cell carcinoma: Involvement of intracellular Ca(2+) signaling.
Pathol Oncol Res. 23:329–334. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hennessy BA, Harvey BJ and Healy V:
17beta-Estradiol rapidly stimulates c-fos expression via the MAPK
pathway in T84 cells. Mol Cell Endocrinol. 229:39–47. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zuguchi M, Miki Y, Onodera Y, Fujishima F,
Takeyama D, Okamoto H, Miyata G, Sato A, Satomi S and Sasano H:
Estrogen receptor α and β in esophageal squamous cell carcinoma.
Cancer Sci. 103:1348–1355. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ueo H, Matsuoka H, Sugimachi K, Kuwano H,
Mori M and Akiyoshi T: Inhibitory effects of estrogen on the growth
of a human esophageal carcinoma cell line. Cancer Res.
50:7212–7215. 1990.PubMed/NCBI
|
|
42
|
Menon S, Nightingale P and Trudgill N: Is
hormone replacement therapy in post-menopausal women associated
with a reduced risk of oesophageal cancer? United European
Gastroenterol J. 2:374–382. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lanas A and Chan FKL: Peptic ulcer
disease. Lancet. 390:613–624. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Kanotra R, Ahmed M, Patel N, Thakkar B,
Solanki S, Tareen S, Fasullo MJ, Kesavan M, Nalluri N, Khan A, et
al: Seasonal variations and trends in hospitalization for peptic
ulcer disease in the United States: A 12-year analysis of the
nationwide inpatient sample. Cureus. 8:e8542016.PubMed/NCBI
|
|
45
|
Suleyman H, Albayrak A, Bilici M, Cadirci
E and Halici Z: Different mechanisms in formation and prevention of
indomethacin-induced gastric ulcers. Inflammation. 33:224–234.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Feldman M, Richardson CT and Walsh JH:
Sex-related differences in gastrin release and parietal cell
sensitivity to gastrin in healthy human beings. J Clin Invest.
71:715–720. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Sangma TK, Jain S and Mediratta PK: Effect
of ovarian sex hormones on non-steroidal anti-inflammatory
drug-induced gastric lesions in female rats. Indian J Pharmacol.
46:113–116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Okada K, Inamori M, Imajyo K, Chiba H,
Nonaka T, Shiba T, Sakaguchi T, Atsukawa K, Takahashi H, Hoshino E
and Nakajima A: Gender differences of low-dose aspirin-associated
gastroduodenal ulcer in Japanese patients. World J Gastroenterol.
16:1896–1900. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Speir E, Yu ZX, Takeda K, Ferrans VJ and
Cannon RO III: Antioxidant effect of estrogen on
cytomegalovirus-induced gene expression in coronary artery smooth
muscle cells. Circulation. 102:2990–2996. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jiang F and Shen X: Current prevalence
status of gastric cancer and recent studies on the roles of
circular RNAs and methods used to investigate circular RNAs. Cell
Mol Biol Lett. 24:532019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Chung HW, Noh SH and Lim JB: Analysis of
demographic characteristics in 3242 young age gastric cancer
patients in Korea. World J Gastroenterol. 16:256–263. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Tokunaga A, Kojima N, Andoh T, Matsukura
N, Yoshiyasu M, Tanaka N, Ohkawa K, Shirota A, Asano G and Hayashi
K: Hormone receptors in gastric cancer. Eur J Cancer Clin Oncol.
19:687–689. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Lindblad M, Ye W, Rubio C and Lagergren J:
Estrogen and risk of gastric cancer: A protective effect in a
nationwide cohort study of patients with prostate cancer in Sweden.
Cancer Epidemiology Biomarkers Prev. 13:2203–2207. 2004.
|
|
54
|
Furukawa H, Iwanaga T, Koyama H and
Taniguchi H: Effect of sex hormones on the experimental induction
of cancer in rat stomach-a preliminary study. Digestion.
23:151–155. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kim MJ, Cho SI, Lee KO, Han HJ, Song TJ
and Park SH: Effects of 17β-estradiol and estrogen receptor
antagonists on the proliferation of gastric cancer cell lines. J
Gastric Cancer. 13:172–178. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chandanos E and Lagergren J: Oestrogen and
the enigmatic male predominance of gastric cancer. Eur J Cancer.
44:2397–2403. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sunakawa Y, Cao S, Berger MD, Matsusaka S,
Yang D, Zhang W, Ning Y, Parekh A, Stremitzer S, Mendez A, et al:
Estrogen receptor-beta genetic variations and overall survival in
patients with locally advanced gastric cancer. Pharmacogenomics J.
17:36–41. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Matsuyama S, Ohkura Y, Eguchi H, Kobayashi
Y, Akagi K, Uchida K, Nakachi K, Gustafsson JA and Hayashi S:
Estrogen receptor beta is expressed in human stomach
adenocarcinoma. J Cancer Res Clin Oncol. 128:319–324. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Takano N, Iizuka N, Hazama S, Yoshino S,
Tangoku A and Oka M: Expression of estrogen receptor-alpha and
-beta mRNAs in human gastric cancer. Cancer Lett. 176:129–135.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Wang M, Pan JY, Song GR, Chen HB, An LJ
and Qu SX: Altered expression of estrogen receptor alpha and beta
in advanced gastric adenocarcinoma: Correlation with prothymosin
alpha and clinicopathological parameters. Eur J Surg Oncol.
33:195–201. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ryu WS, Kim JH, Jang YJ, Park SS, Um JW,
Park SH, Kim SJ, Mok YJ and Kim CS: Expression of estrogen
receptors in gastric cancer and their clinical significance. J Surg
Oncol. 106:456–461. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Qin J, Liu M, Ding Q, Ji X, Hao Y, Wu X
and Xiong J: The direct effect of estrogen on cell viability and
apoptosis in human gastric cancer cells. Mol Cell Biochem.
395:99–107. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Zhang BG, Du T, Zang MD, Chang Q, Fan ZY,
Li JF, Yu BQ, Su LP, Li C, Yan C, et al: Androgen receptor promotes
gastric cancer cell migration and invasion via AKT-phosphorylation
dependent upregulation of matrix metalloproteinase 9. Oncotarget.
5:10584–10595. 2014.PubMed/NCBI
|
|
64
|
Wesolowska M, Pawlik P and Jagodzinski PP:
The clinicopathologic significance of estrogen receptors in human
gastric carcinoma. Biomed Pharmacother. 83:314–322. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Zhou J, Teng R, Xu C, Wang Q, Guo J, Xu C,
Li Z, Xie S, Shen J and Wang L: Overexpression of ERα inhibits
proliferation and invasion of MKN28 gastric cancer cells by
suppressing β-catenin. Oncol Rep. 30:1622–1630. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wang X, Deng H, Zou F, Fu Z, Chen Y, Wang
Z and Liu L: ER-α36-mediated gastric cancer cell proliferation via
the c-Src pathway. Oncol Lett. 6:329–335. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Tang W, Liu R, Yan Y, Pan X, Wang M, Han
X, Ren H and Zhang Z: Expression of estrogen receptors and androgen
receptor and their clinical significance in gastric cancer.
Oncotarget. 8:40765–40777. 2017.PubMed/NCBI
|
|
68
|
Wakui S, Motohashi M, Muto T, Takahashi H,
Hano H, Jutabha P, Anzai N, Wempe MF and Endou H: Sex-associated
difference in estrogen receptor β expression in
N-methyl-N′-nitro-N-nitrosoguanidine-induced gastric cancers in
rats. Comp Med. 61:412–418. 2011.PubMed/NCBI
|
|
69
|
Choung RS and Locke GR III: Epidemiology
of IBS. Gastroenterol Clin North Am. 40:1–10. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Heitkemper M, Jarrett M, Bond EF and Chang
L: Impact of sex and gender on irritable bowel syndrome. Biol Res
Nurs. 5:56–65. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Longstreth GF and Wolde-Tsadik G:
Irritable bowel-type symptoms in HMO examinees. Prevalence,
demographics, and clinical correlates. Dig Dis Sci. 38:1581–1589.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Toner BB and Akman D: Gender role and
irritable bowel syndrome: Literature review and hypothesis. Am J
Gastroenterol. 95:11–16. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Heitkemper MM and Chang L: Do fluctuations
in ovarian hormones affect gastrointestinal symptoms in women with
irritable bowel syndrome? Gender Med. 2 (Suppl 6):152–167. 2009.
View Article : Google Scholar
|
|
74
|
Chaloner A and Greenwood-Van Meerveld B:
Sexually dimorphic effects of unpredictable early life adversity on
visceral pain behavior in a rodent model. J Pain. 14:270–280. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Cao DY, Ji Y, Tang B and Traub RJ:
Estrogen receptor β activation is antinociceptive in a model of
visceral pain in the rat. J Pain. 13:685–694. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Jacenik D, Cygankiewicz AI, Fichna J,
Mokrowiecka A, Malecka-Panas E and Krajewska WM: Estrogen signaling
deregulation related with local immune response modulation in
irritable bowel syndrome. Mol Cell Endocrinol. 471:89–96. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Qin B, Dong L, Guo X, Jiang J, He Y, Wang
X, Li L and Zhao J: Expression of G protein-coupled estrogen
receptor in irritable bowel syndrome and its clinical significance.
Int J Clin Exp Pathol. 7:2238–2246. 2014.PubMed/NCBI
|
|
78
|
Zielinska M, Fichna J, Bashashati M,
Habibi S, Sibaev A, Timmermans JP and Storr M: G protein-coupled
estrogen receptor and estrogen receptor ligands regulate colonic
motility and visceral pain. Neurogastroenterol Motil. 29:2017.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Mizoguchi A, Takeuchi T, Himuro H, Okada T
and Mizoguchi E: Genetically engineered mouse models for studying
inflammatory bowel disease. J Pathol. 238:205–219. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Xavier RJ and Podolsky DK: Unravelling the
pathogenesis of inflammatory bowel disease. Nature. 448:427–434.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Molodecky NA, Soon IS, Rabi DM, Ghali WA,
Ferris M, Chernoff G, Benchimol EI, Panaccione R, Ghosh S, Barkema
HW and Kaplan GG: Increasing incidence and prevalence of the
inflammatory bowel diseases with time, based on systematic review.
Gastroenterology. 142:46–54.e42; quiz e30. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Cook LC, Hillhouse AE, Myles MH, Lubahn
DB, Bryda EC, Davis JW and Franklin CL: The role of estrogen
signaling in a mouse model of inflammatory bowel disease: A
Helicobacter hepaticus model. PLoS One. 9:e942092014. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Barzi A, Lenz AM, Labonte MJ and Lenz HJ:
Molecular pathways: Estrogen pathway in colorectal cancer. Clin
Cancer Res. 19:5842–5848. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Principi M, Barone M, Pricci M, De Tullio
N, Losurdo G, Ierardi E and Di Leo A: Ulcerative colitis: From
inflammation to cancer. Do estrogen receptors have a role? World J
Gastroenterol. 20:11496–11504. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Pierdominici M, Maselli A, Varano B,
Barbati C, Cesaro P, Spada C, Zullo A, Lorenzetti R, Rosati M,
Rainaldi G, et al: Linking estrogen receptor β expression with
inflammatory bowel disease activity. Oncotarget. 6:40443–40451.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Armstrong CM, Allred KF, Weeks BR, Chapkin
RS and Allred CD: Estradiol has differential effects on acute
colonic inflammation in the presence and absence of estrogen
receptor β expression. Dig Dis Sci. 62:1977–1984. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Looijer-van Langen M, Hotte N, Dieleman
LA, Albert E, Mulder C and Madsen KL: Estrogen receptor-β signaling
modulates epithelial barrier function. Am J Physiol Gastrointest
Liver Physiol. 300:G621–G626. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Saleiro D, Murillo G, Benya RV,
Bissonnette M, Hart J and Mehta RG: Estrogen receptor-β protects
against colitis-associated neoplasia in mice. Int J Cancer.
131:2553–2561. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Bustos V, Nolan AM, Nijhuis A, Harvey H,
Parker A, Poulsom R, McBryan J, Thomas W, Silver A and Harvey BJ:
GPER mediates differential effects of estrogen on colon cancer cell
proliferation and migration under normoxic and hypoxic conditions.
Oncotarget. 8:84258–84275. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Konstantinopoulos PA, Kominea A, Vandoros
G, Sykiotis GP, Andricopoulos P, Varakis I, Sotiropoulou-Bonikou G
and Papavassiliou AG: Oestrogen receptor beta (ERbeta) is
abundantly expressed in normal colonic mucosa, but declines in
colon adenocarcinoma paralleling the tumour's dedifferentiation.
Eur J Cancer. 39:1251–1258. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Delellis Henderson K, Duan L,
Sullivan-Halley J, Ma H, Clarke CA, Neuhausen SL, Templeman C and
Bernstein L: Menopausal hormone therapy use and risk of invasive
colon cancer: The california teachers study. Am J Epidemiol.
171:415–425. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Manson JE, Chlebowski RT, Stefanick ML,
Aragaki AK, Rossouw JE, Prentice RL, Anderson G, Howard BV, Thomson
CA, LaCroix AZ, et al: Menopausal hormone therapy and health
outcomes during the intervention and extended poststopping phases
of the Women's Health Initiative randomized trials. JAMA.
310:1353–1368. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Design of the Women's Health Initiative
clinical trial and observational study. The Women's Health
Initiative Study Group. Control Clin Trials. 19:61–109. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Calle EE, Miracle-McMahill HL, Thun MJ and
Heath CW Jr: Estrogen replacement therapy and risk of fatal colon
cancer in a prospective cohort of postmenopausal women. J Natl
Cancer Inst. 87:517–523. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Simon MS, Chlebowski RT, Wactawski-Wende
J, Johnson KC, Muskovitz A, Kato I, Young A, Hubbell FA and
Prentice RL: Estrogen plus progestin and colorectal cancer
incidence and mortality. J Clin Oncol. 30:3983–3990. 2012.
View Article : Google Scholar : PubMed/NCBI
|