Introduction
Renal cell carcinoma (RCC) accounts for ~90% of all
renal malignancies (1). For
clinically localized RCC, nephrectomy remains the treatment method
of choice (2). Numerous studies
demonstrated that partial nephrectomy (PN) may provide a
recurrence-free and long-term benefit to patients with tumors <4
cm in diameter compared with radical nephrectomy (RN) (3–6). PN is
thus becoming a main alternative to RN for treating T1a disease
(RCC tumors <4 cm) (7–9), and the European Association of Urology
(EAU) guidelines recommended PN as the standard surgical procedure
for tumors measuring <4 cm (10).
However, for tumors measuring >4 cm, the EAU
guidelines do not recommend PN (10). Achieving patient benefit without
damaging renal function is the most important purpose of RCC
treatment. Mir et al (11)
observed that PN may provide oncological outcomes similar to those
of RN in clinical stage T1b patients (RCC tumors ≥4 and <7 cm).
In addition, other studies reported equivalent outcomes regarding
cancer control (individuals with no disease recurrence or
progression) for PN and RN (tumors >4 cm) (12,13). The
majority of those previous studies mostly focus on PN function,
regardless of age. Tan et al (14) observed similar long-term survival in
patients with T1 stage RCC who were treated with PN and RN;
however, subgroup analysis revealed improved survival in patients
>75 years of age treated with PN compared with RN.
The purpose of the present study was to investigate
the benefit of PN vs. RN on the cancer-specific survival (CSS) in
patients with T1b RCC, and to further assess the effects of age and
sex on the benefit of PN vs. RN. For that purpose, data from a
population database were analyzed.
Materials and methods
Data source
Case details were retrieved from the Surveillance,
Epidemiology, and End Results (SEER) database (https://seer.cancer.gov; code: kidney C64.9), which
covers ~28% USA population. The SEER program contains cancer
epidemiology information (15).
Study population
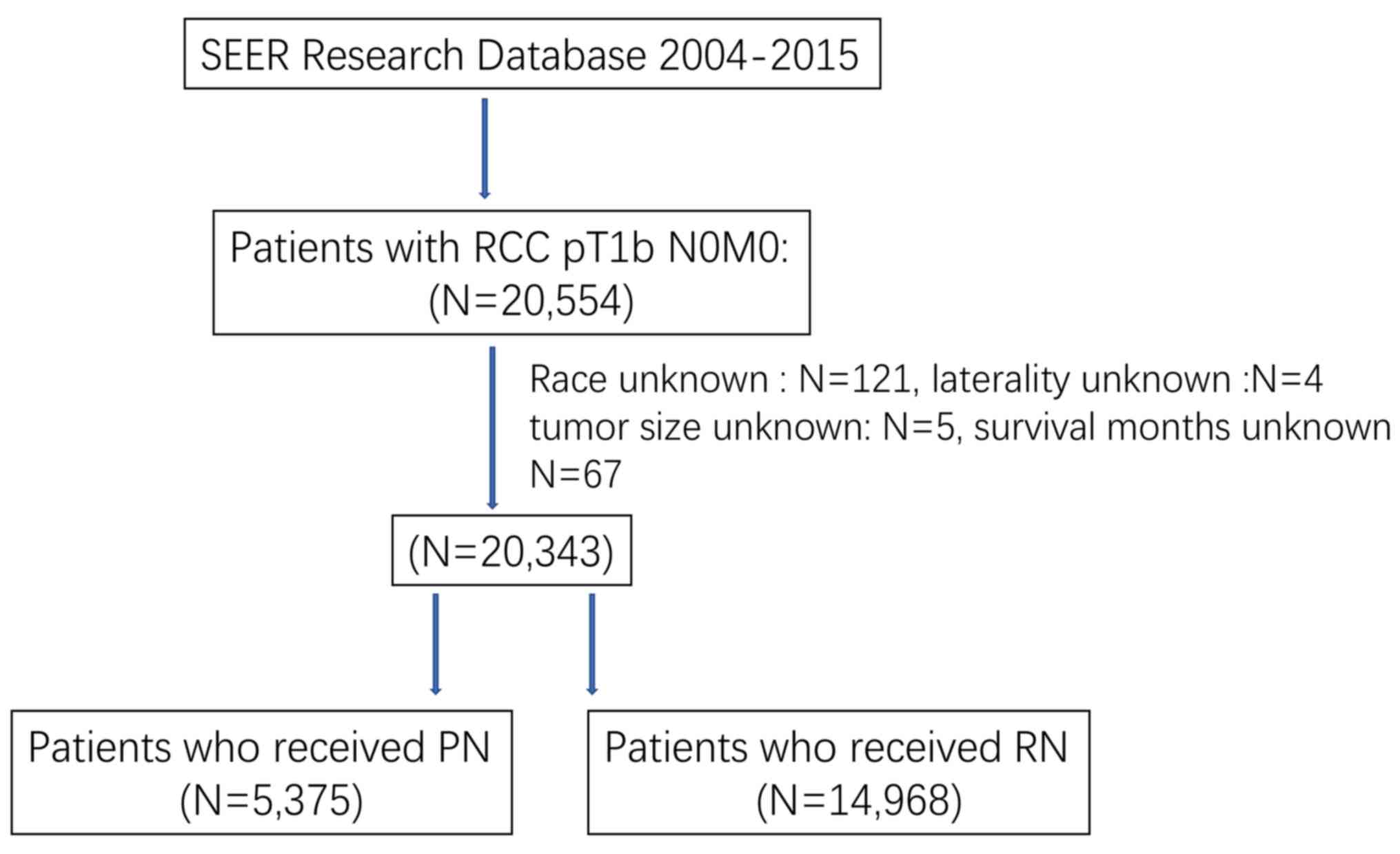
Patients who were histologically confirmed to have
RCC (stage pT1b N0M0) between the years 2004 and 2015 were
identified using SEER*Stat software (version 8.3.2; http://seer.cancer.gov/data-software/).
Variables including marital status, ethnicity, age at diagnosis,
sex, surgical method, tumor size, laterality and months of
follow-up were identified. TNM classification of RCC was based on
the 6th edition of the American Joint Committee on Cancer staging
system (16). In total, data from
20,554 patients with pT1b RCC who received PN or RN were collected.
Patients of unknown ethnicity (n=121), laterality (n=4), tumor size
(n=5) or survival months (n=67) were excluded. The remaining 20,343
patients were included in the present cohort study (Fig. 1). For data analysis, subgroups of
patients were created as follows: Males <75 years; males ≥75
years; females <75 years; and females ≥75 years.
Statistical analysis
Frequencies and proportions were used to describe
categorical variables. Means, medians and ranges were reported for
continuous variables. The χ2 test was used to assess
statistical significance in proportion differences, while the
t-test was used to evaluate statistical significances in the means
(Table I). The effect of surgery (PN
vs. RN) on the CSS was evaluated by Kaplan-Meier survival curves
with log-rank tests. Differences in CSS were assessed by
multivariate Cox proportional hazards regression analyses.
P<0.05 was considered to indicate a statistically significant
difference. Statistical analyses were performed using the
statistical package MASS for R (version 3.4.1; http://www.r-project.org/) or Empower software version
1.1 (www.empowerstats.com).
 | Table I.Baseline characteristics and
pathological characteristics of patients. |
Table I.
Baseline characteristics and
pathological characteristics of patients.
| Characteristics | Partial
nephrectomy | Radical
nephrectomy | P-value |
|---|
| n | 5,375 (26.4%) | 14,968 (73.6%) |
|
| Tumor size, (mm) | 50.9±7.6 | 54.5±8.5 | <0.001 |
| Marital status, n
(%) |
|
| 0.211 |
|
Single/widowed/divorced/unmarried | 1,859 (34.6%) | 5,319 (35.5%) |
|
|
Married | 3,516 (65.4%) | 9,649 (64.5%) |
|
| Age at diagnosis
(years), n (%) |
|
| <0.001 |
| ≥75 | 4,713 (87.7%) | 12,446 (83.2%) |
|
|
<75 | 662 (12.3%) | 2,522 (16.8%) |
|
| Period diagnosed, n
(%) |
|
| <0.001 |
|
2004–2008 | 1,545 (28.7%) | 7,758 (51.8%) |
|
|
2009–2015 | 3,830 (71.3%) | 7,210 (48.2%) |
|
| Sex, n (%) |
|
| <0.001 |
|
Male | 3,600 (67.0%) | 9,158 (61.2%) |
|
|
Female | 1,775 (33.0%) | 5,810 (38.8%) |
|
| Ethnicity, n
(%) |
|
| 0.001 |
|
Caucasian | 4,327 (80.5%) | 12,337 (82.4%) |
|
|
African-American | 722 (13.4%) | 1,726 (11.5%) |
|
| Other
(American Indian/AK Native, Asian) | 326 (6.1%) | 905 (6.1%) |
|
| Histology type, n
(%) |
|
| <0.001 |
|
Non-clear cell RCC | 2,457 (45.7%) | 5,562 (37.2%) |
|
| Clear
cell RCC | 2,918 (54.3%) | 9,406 (62.8%) |
|
| Grade, n (%) |
|
| <0.001 |
|
I+II | 3,034 (56.4%) | 8,939 (59.7%) |
|
|
III+IV | 1,561 (29.1%) | 4,264 (28.5%) |
|
|
Unknown | 780 (14.5%) | 1,765 (11.8%) |
|
| Laterality, n
(%) |
|
| 0.170 |
|
Left | 2,612 (48.6%) | 7,437 (49.7%) |
|
|
Right | 2,763 (51.4%) | 7,531 (50.3%) |
|
Results
In total, 5,375 (26.42%) and 14,968 (73.58%)
patients with pT1b RCC received PN and RN, respectively. The
baseline characteristics of the patients are presented in Table I. Of all patients, 45.73% were
diagnosed between 2004 and 2008 (mean follow-up time, 91 months),
while 54.27% were diagnosed between 2009 and 2015 (mean follow-up
time, 35 months). The mean follow-up time was 92 months (range,
0–143 months) for PN and 90 months (range, 0–143 months) for RN.
The mean overall age was 61.4 years [standard deviation (SD), 12.5
years], while the mean age for male patients was 61.2 years (SD,
12.1 years) and 61.7 years (SD, 13.0 years) for female
patients.
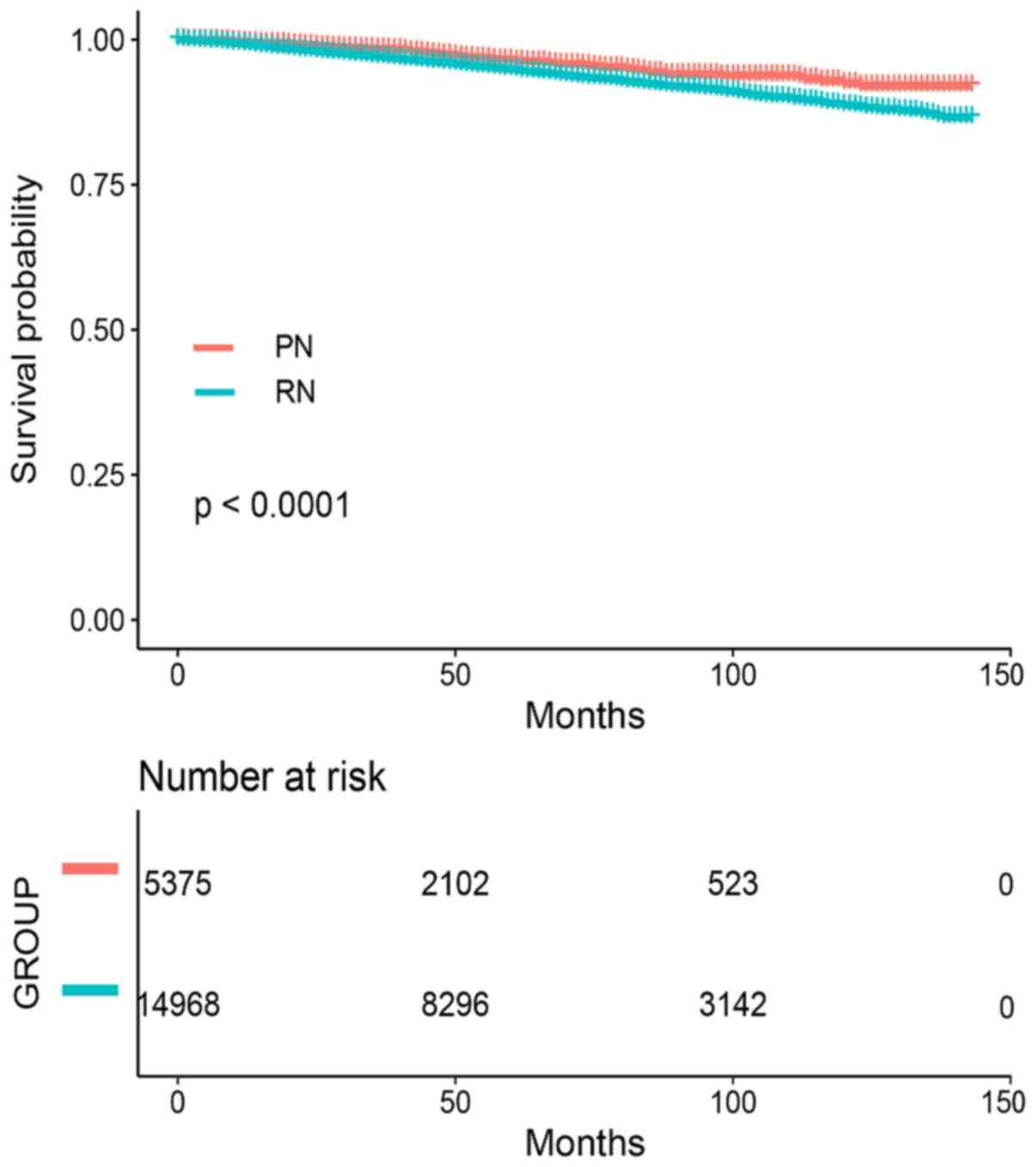
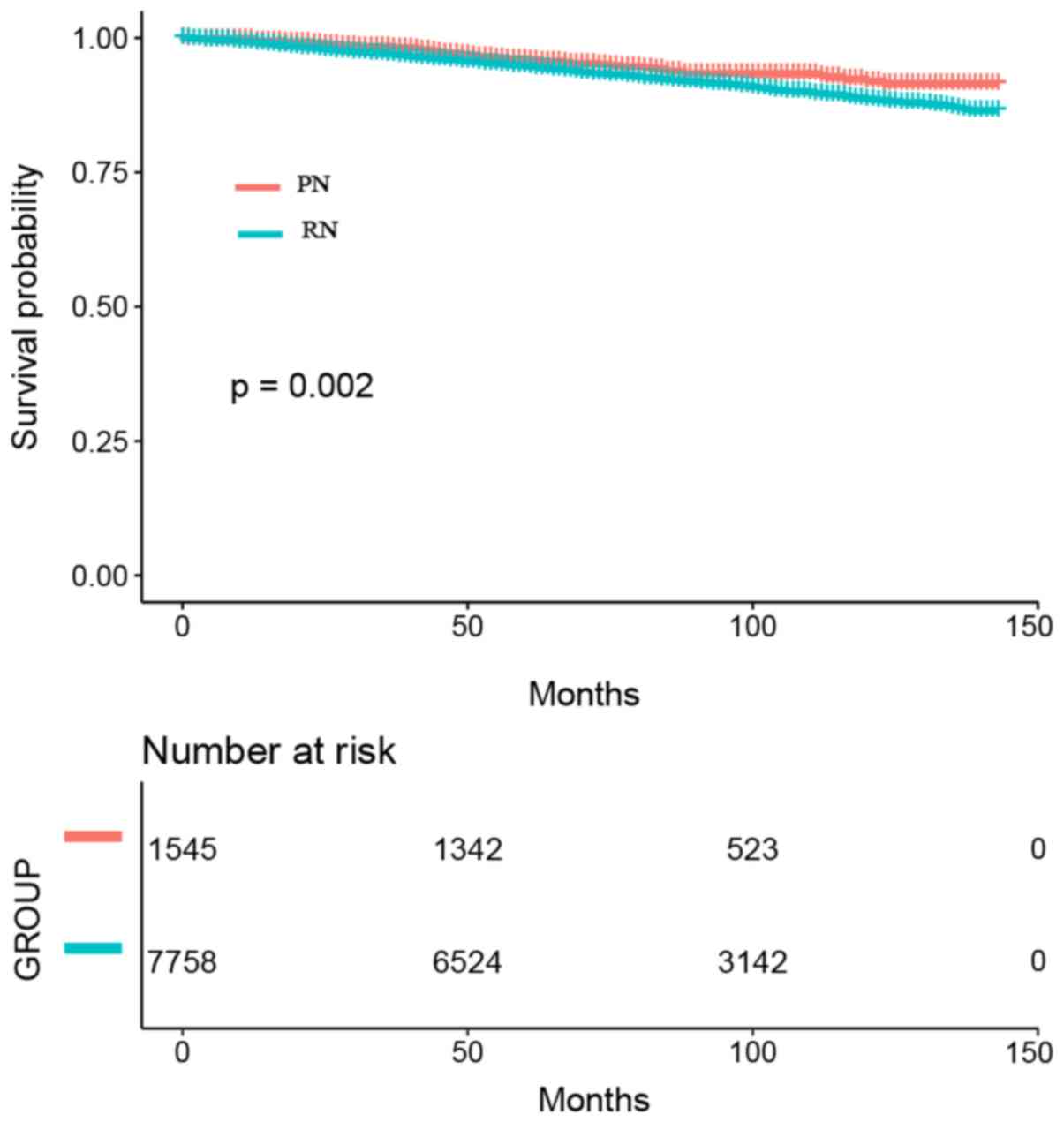
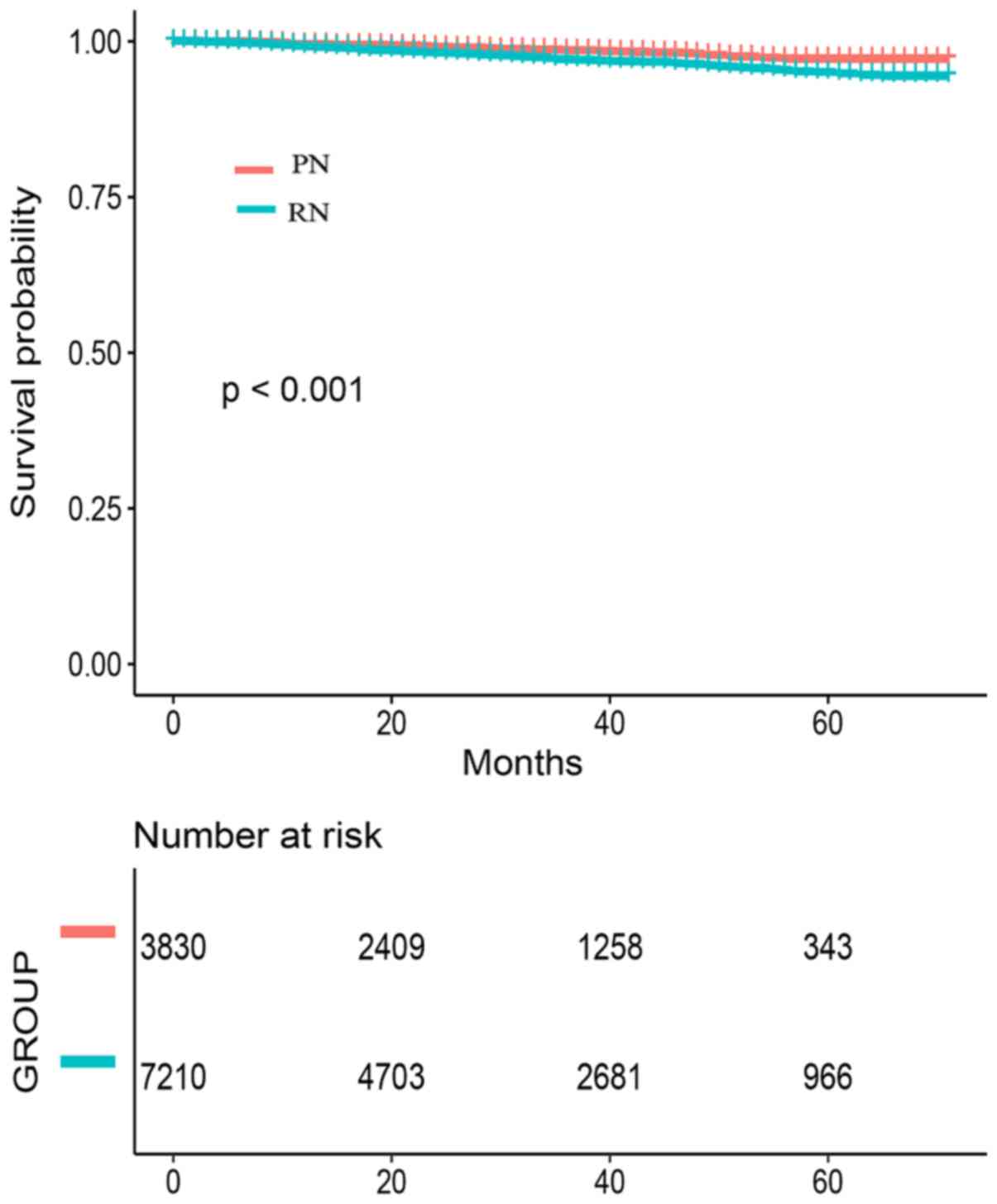
Regardless of their age or sex, there was an
improvement in CSS in all patients treated with PN (P<0.001;
Fig. 2). There was an improvement in
CSS in males (P<0.001) and females (P<0.001) regardless of
their age. Multivariable Cox regression analyses revealed that PN
was an independent predictor factor of CSS [hazard ratio (HR),
1.35; 95% confidence interval (CI), 1.13–1.62; P=0.001). In
addition, multivariate Cox regression analyses revealed that age at
diagnosis, marital status, tumor size and grade were associated
with outcomes (Table II).
 | Table II.Multivariable cox regression model in
the cohort of patients with renal cell carcinoma. |
Table II.
Multivariable cox regression model in
the cohort of patients with renal cell carcinoma.
| Variables | Hazard ratio (95%
confidence interval) | P-value |
|---|
| Surgery type | 1.35
(1.13–1.62) | 0.0010 |
| Marital status | 0.87
(0.76–0.99) | 0.0370 |
| Age at
diagnosis | 2.34
(2.03–2.69) | <0.0001 |
| Period
diagnosed | 0.87
(0.75–1.02) | 0.0958 |
| Sex | 0.88
(0.77–1.01) | 0.0698 |
| Ethnicity |
|
|
|
Caucasian | Reference |
|
|
African-American | 1.01
(0.83–1.24) | 0.9126 |
| Other
(American Indian/AK Native, Asian) | 1.09
(0.84–1.41) | 0.5207 |
| Histology type | 0.98
(0.86–1.11) | 0.7168 |
| Grade |
|
|
|
I+II | Reference |
|
|
III+IV | 1.97
(1.72–2.24) | <0.0001 |
|
Unknown | 1.09
(0.88–1.35) | 0.4355 |
| Laterality | 1.05
(0.92–1.18) | 0.4814 |
| Tumor size | 1.03
(1.02–1.04) | <0.0001 |
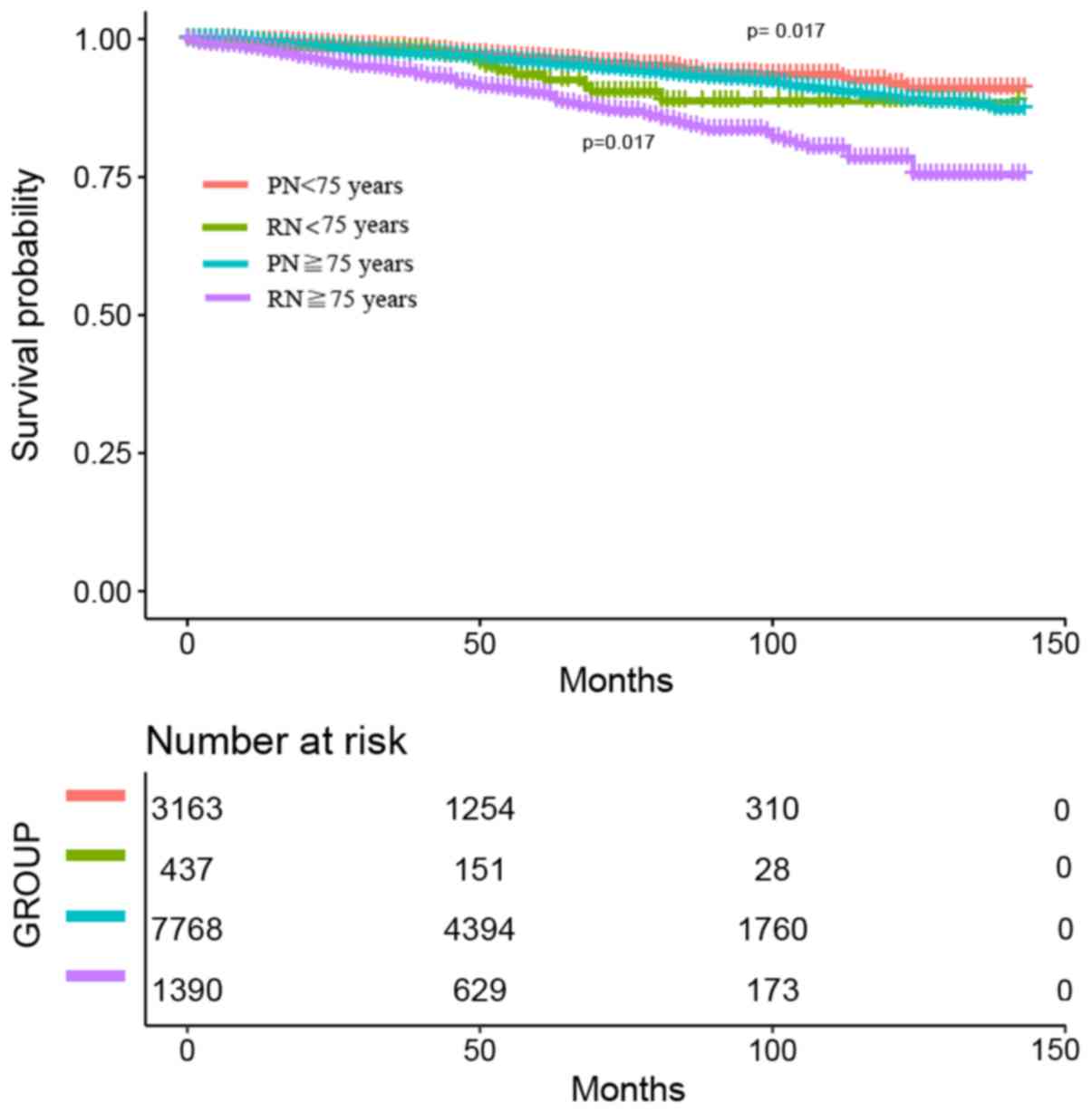
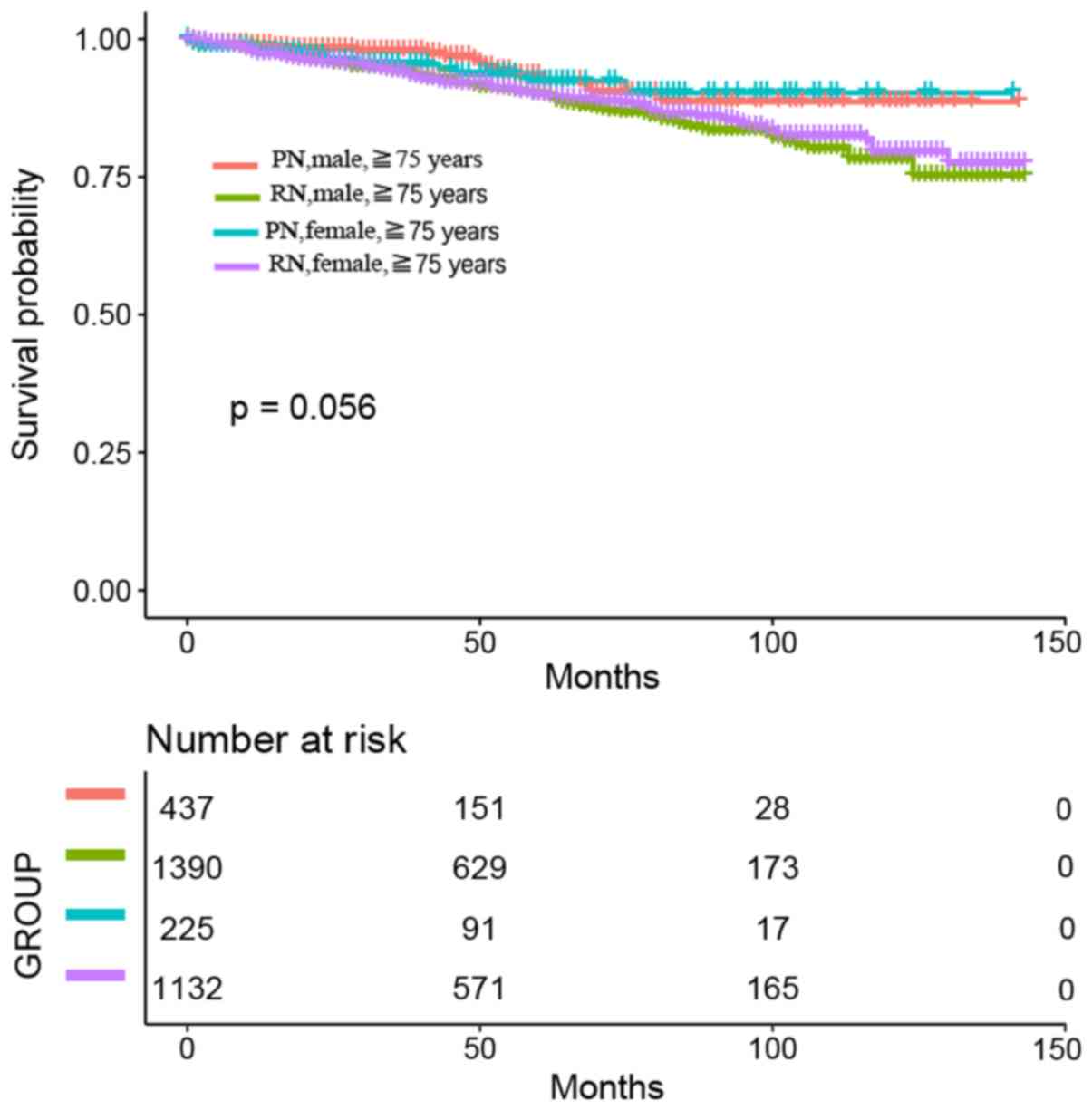
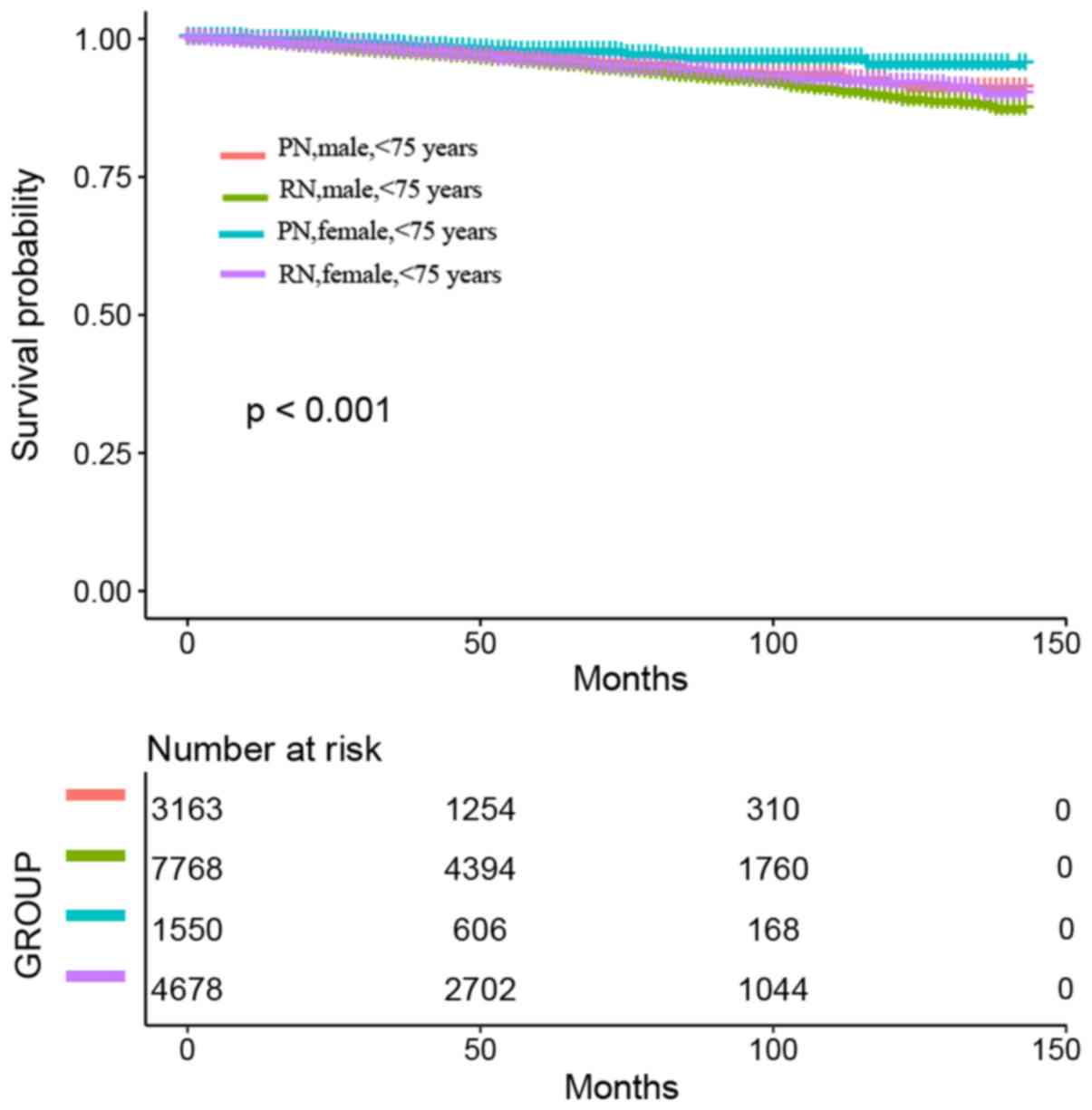
Considering the age of the patients, male patients
<75 and ≥75 years of age exhibited an improvement in CSS
following PN (P=0.017; Fig. 3).
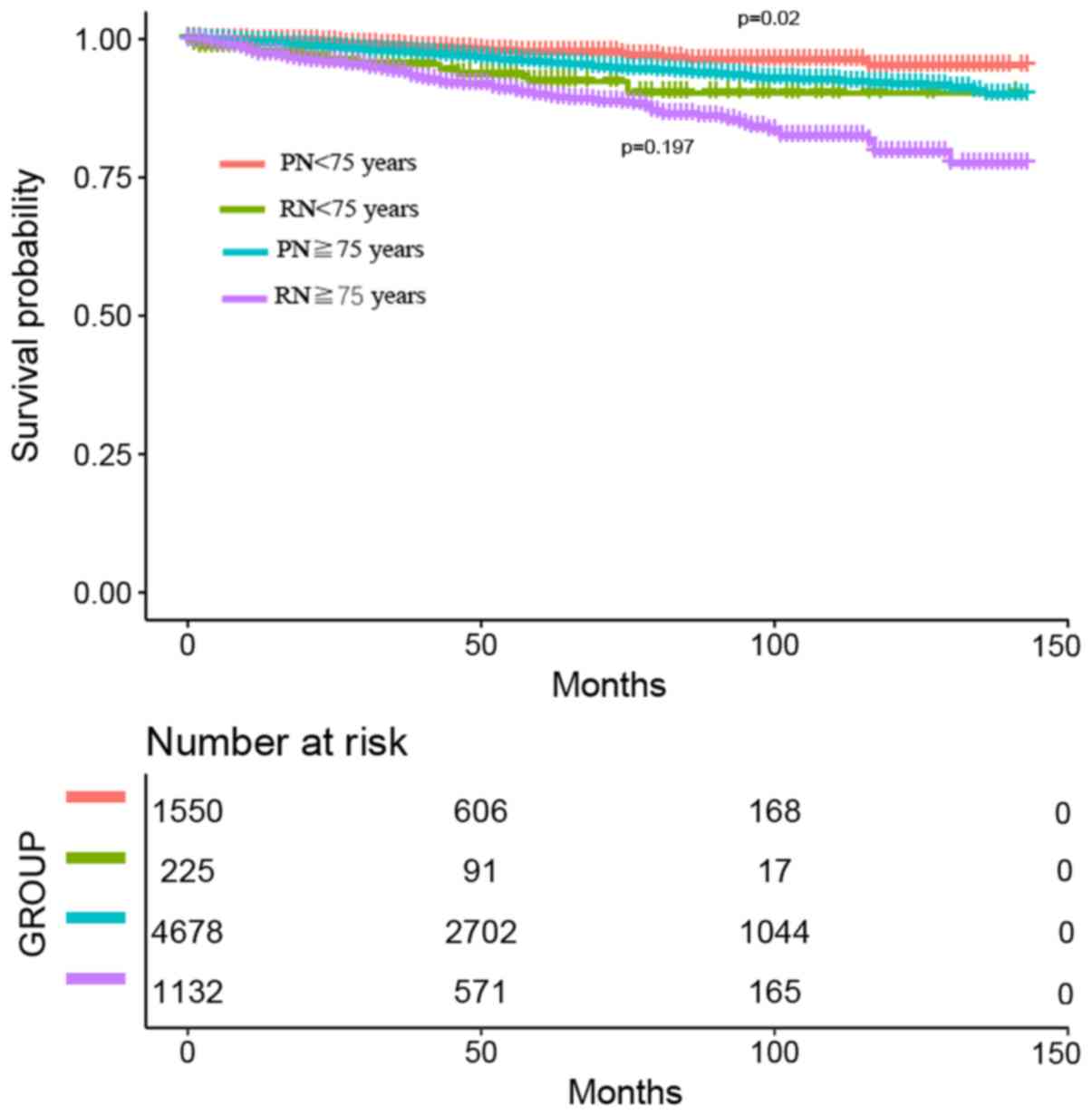
Among females, only patients <75 years exhibited a notable CSS
improvement (P=0.002) following PN. In patients treated by PN ≥75
years of age, no CSS improvement was observed (P=0.197; Fig. 4). Male and female patients ≥75 years
of age exhibited the same prognostic data for RN and PN, regardless
of their sex (Fig. 5). All male and
female patients <75 years exhibited improved CSS following PN.
Female patients <75 years exhibited improved CSS following PN
(P=0.029) compared with male patients <75 years. There were no
statistically significant differences for RN (P=0.066; Fig. 6).
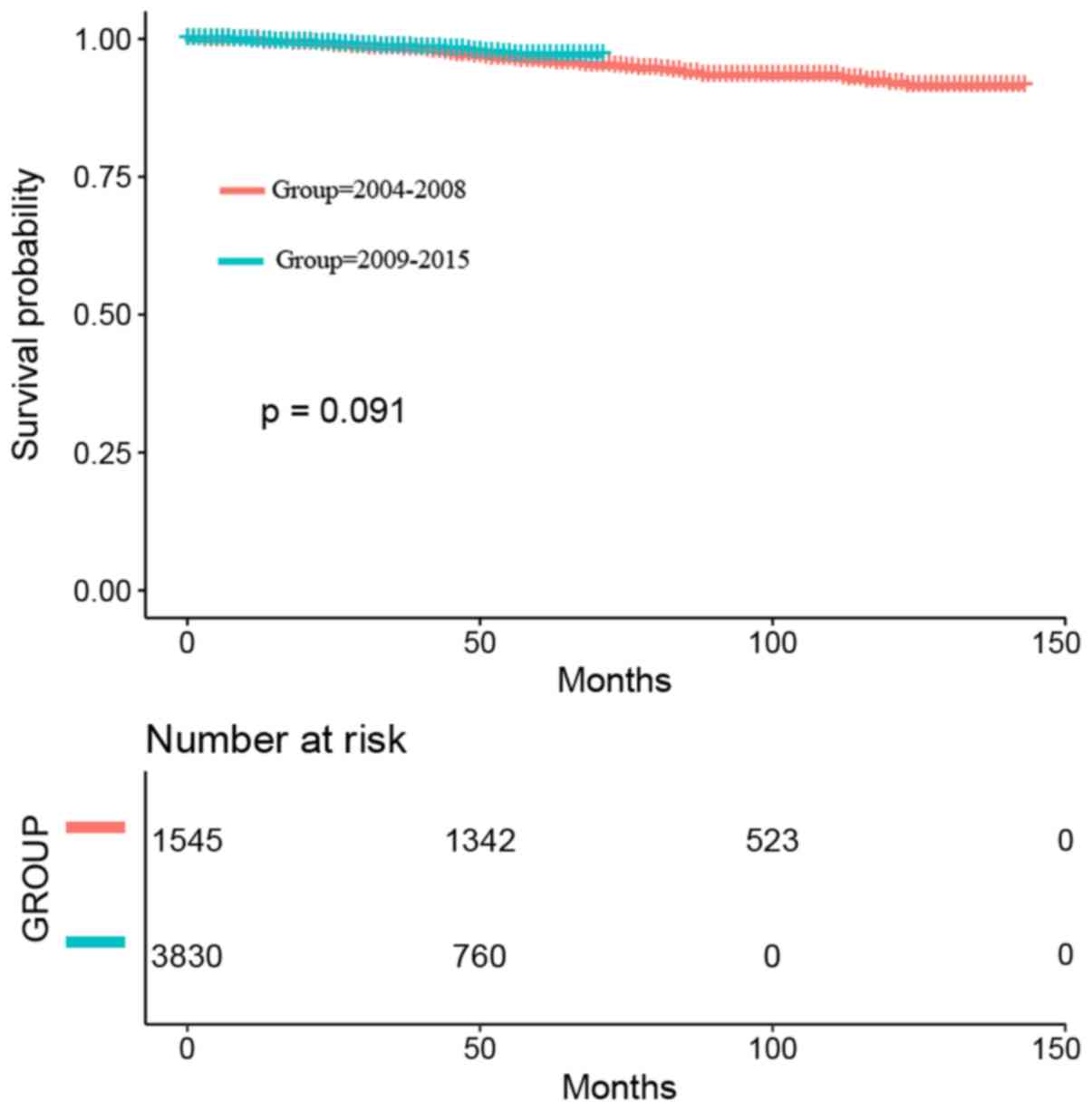
The contradistinction of the follow-up of patients
treated with PN (group 1, 2004–2008 and group 2, 2009–2015) is
presented in Fig. 7 (P=0.091). The
comparison of CSS following PN and RN during different periods of
time is presented in Figs. 8 and
9 (Fig.
8, 2004–2008; P=0.002; and Fig.
9, 2009–2015; P<0.001).
Discussion
The present study conducted a population-based
analysis with 20,343 cases to compare the benefits of PN vs. RN in
the treatment of pT1b RCC. The results obtained may clarify the
benefit of PN and aid evidence-based surgical decision-making.
Regardless of age and sex, a notable improvement in survival was
observed for all patients treated with PN, compared with those
treated with RN (HR, 1.35; P=0.001).
In terms of the improvement in CSS observed
following PN in patients with T1 clinical stage RCC across all age
groups, the results obtained in the current study are in accordance
with the literature (17–19). Tan et al (14) reported improved survival only in
patients with T1a RCC treated with PN who were <75 years of age.
Previously, PN was considered to be associated with an increased
probability of complications (20).
Thus, elderly patients with multiple comorbidities were deemed to
be more likely to suffer serious complications. However, according
to a study by Roos et al (21), PN may be performed with acceptable
complications on selected ≥65-year-old patients with a single,
small, unilateral, localized RCC. Similar studies revealed that
selected ≥80-year-old patients with RCC may benefit from PN
(22–24). However, the aforementioned studies
did not investigate the differences in the benefits of PN between
age groups according to sex. In the current study, in the male
group, patients <75 and ≥75 years of age experienced an improved
CSS (P=0.017) following PN compared with RN. Notably, in the female
group, only patients <75 years of age exhibited a marked CSS
improvement (P=0.002) following PN compared with RN, which may be
due to bias introduced by the small sample number. Dulabon et
al (25) revealed that female
patients had lower probability of undergoing PN compared with
males, and that female patients, particularly the elderly, may
prefer being subjected to active surveillance for renal disease
rather than to surgical extirpation. In a previous study, PN
decreased chronic kidney disease as well as nononcologic morbidity
and mortality compared with RN, and the complication rate did not
differ between the young and old patients (26).
To exclude bias introduced by the implementation of
new technologies, including laparoscopic robot-assisted procedures,
compared with open surgery (22,27,28),
different time periods were assessed for the PN group in the
present study. Notable differences in CSS following PN were not
observed between the groups treated during the periods 2004–2008
and 2009–2015 (P=0.091). According to these results, the
implementation of new technologies had no effect on CSS following
PN.
A statistically significant improvement in CSS
following PN was observed in patients treated during 2004–2008 who
were followed up for a long period (mean follow-up time, 91 months;
P=0.003). This was also observed in patients treated during the
2009–2015 period (mean follow-up time, 35 months; P<0.001).
Thus, it appears that CSS improvement following PN may not be
associated with follow-up time.
Tobert et al (29) reported that loss of kidney function
caused by surgery may have less effect on survival than chronic
kidney disease (CKD). Thus, the protective role of PN against
long-term complications such as cardiovascular disease in the
elderly may be overestimated (29,30).
However, Huang et al (31)
reported that patients who received PN had lower rates of damaging
glomerular filtration rate and CKD than those receiving RN.
However, other criteria, including tumor features, patients' wishes
and social support, remain important when deciding to perform PN or
RN surgery in elderly patients (21).
The present study had several limitations. The
analyses were based on an observational study design, and this
result obtained are limited by retrospective nature of the study.
Moreover, the impact of competing risk bias on PN was not
investigated (32). The SEER
database does not contain information on preoperative renal
function, which affects the selection of patients receiving partial
resection. Since poor renal function is associated with increased
risk of severe cardiovascular disease (33), if a large proportion of patients with
poor preoperative renal function is included in the PN group, this
may undervalue the role of PN. Furthermore, it is difficult to
select appropriate patients to receive partial resection due to the
absence of knowledge on the exact tumor location (34,35).
Altogether, the results obtained in the present
study, which was conducted on a large cohort, indicated that PN is
beneficial for patients with pT1b RCC compared with RN. Future
studies are required to clarify whether the patient age should be
taken into account when planning to perform PN in patients with T1b
RCC. According to the present study, female patients ≥75 years of
age appear to have limited benefit from PN. These results should be
corroborated in clinical trials.
Acknowledgements
Not applicable.
Funding
The present study was supported by the 1.3.5 Project
for Disciplines of Excellence, West China Hospital, Sichuan
University (grant no. ZY2016104).
Availability of data and materials
The datasets analyzed during the present study were
downloaded from the Surveillance, Epidemiology, and End Results
(SEER) database (https://seer.cancer.gov; code: kidney C64.9).
Authors' contributions
PaZ and PeZ analyzed the data and confirmed the
results' authenticity. XDL wrote the manuscript. XMH produced the
tables and figures, and together with XDL, interpreted the results
obtained. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2017. CA Cancer J Clin. 67:7–30. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Motzer RJ, Jonasch E, Agarwal N, Bhayani
S, Bro WP, Chang SS, Choueiri TK, Costello BA, Derweesh IH, Fishman
M, et al: Kidney cancer, version 2.2017, NCCN Clinical Practice
Guidelines in Oncology. J Natl Compr Canc Netw. 15:804–834. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Crépel M, Jeldres C, Sun M, Lughezzani G,
Isbarn H, Alasker A, Capitanio U, Shariat SF, Arjane P, Widmer H,
et al: A population-based comparison of cancer-control rates
between radical and partial nephrectomy for T1A renal cell
carcinoma. Urology. 76:883–888. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Patard JJ, Shvarts O, Lam JS, Pantuck AJ,
Kim HL, Ficarra V, Cindolo L, Han KR, De La Taille A, Tostain J, et
al: Safety and efficacy of partial nephrectomy for all T1 tumors
based on an international multicenter experience. J Urol.
171:2181–2185; quiz 2435. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Danzig MR, Ghandour RA, Chang P, Wagner
AA, Pierorazio PM, Allaf ME and McKiernan JM: Active surveillance
is superior to radical nephrectomy and equivalent to partial
nephrectomy for preserving renal function in patients with small
renal masses: Results from the DISSRM registry. J Urol.
194:903–909. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Plante K, Stewart TM, Wang D, Bratslavsky
G and Formica M: Treatment trends, determinants, and survival of
partial and radical nephrectomy for stage I renal cell carcinoma:
Results from the National Cancer Data Base, 2004–2013. Int Urol
Nephrol. 49:1375–1381. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Touijer K, Jacqmin D, Kavoussi LR,
Montorsi F, Patard JJ, Rogers CG, Russo P, Uzzo RG and Van Poppel
H: The expanding role of partial nephrectomy: A critical analysis
of indications, results, and complications. Eur Urol. 57:214–222.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wang DC, Plante K, Stewart T, Wang D,
Formica M, Daugherty M and Bratslavsky G: Comparison of survival
for partial vs. radical nephrectomy in young patients with T1a
renal cell carcinoma treated at commission on cancer-accredited
facilities and influence of comorbidities on treatment choice. Urol
Oncol. 35:660.e9–660.e15. 2017. View Article : Google Scholar
|
|
9
|
Larcher A, Sun M, Dell'Oglio P, Trudeau V,
Boehm K, Schiffmann J, Tian Z, Fossati N, Capitanio U, Briganti A,
et al: Mortality, morbidity and healthcare expenditures after local
tumour ablation or partial nephrectomy for T1A kidney cancer. Eur J
Surg Oncol. 43:815–822. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ljungberg B, Bensalah K, Canfield S,
Dabestani S, Hofmann F, Hora M, Kuczyk MA, Lam T, Marconi L,
Merseburger AS, et al: EAU guidelines on renal cell carcinoma: 2014
update. Eur Urol. 67:913–924. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mir MC, Derweesh I, Porpiglia F, Zargar H,
Mottrie A and Autorino R: Partial nephrectomy versus radical
nephrectomy for clinical T1b and T2 renal tumors: A systematic
review and meta-analysis of comparative studies. Eur Urol.
71:606–617. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Badalato GM, Kates M, Wisnivesky JP,
Choudhury AR and McKiernan JM: Survival after partial and radical
nephrectomy for the treatment of stage T1bN0M0 renal cell carcinoma
(RCC) in the USA: A propensity scoring approach. BJU Int.
109:1457–1462. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hadjipavlou M, Khan F, Fowler S, Joyce A,
Keeley FX and Sriprasad S: Partial vs. radical nephrectomy for T1
renal tumours: An analysis from the British Association of
urological surgeons nephrectomy audit. BJU Int. 117:62–71. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tan HJ, Norton EC, Ye Z, Hafez KS, Gore JL
and Miller DC: Long-term survival following partial vs. radical
nephrectomy among older patients with early-stage kidney cancer.
JAMA. 307:1629–1635. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lin CC, Virgo KS, Robbins AS, Jemal A and
Ward EM: Comparison of comorbid medical conditions in the National
Cancer Database and the SEER-medicare database. Ann Surg Oncol.
23:4139–4148. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Greene FP, Page DL, Fleming ID, Fritz A,
Balch CM, Haller DG and Morrow M: AJCC Cancer Staging Manual. 6.
Chicago: Springer; –Verlag. 2002, View Article : Google Scholar
|
|
17
|
Weight CJ, Larson BT, Gao T, Campbell SC,
Lane BR, Kaouk JH, Gill IS, Klein EA and Fergany AF: Elective
partial nephrectomy in patients with clinical T1b renal tumors is
associated with improved overall survival. Urology. 76:631–637.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zini L, Perrotte P, Capitanio U, Jeldres
C, Shariat SF, Antebi E, Saad F, Patard JJ, Montorsi F and
Karakiewicz PI: Radical versus partial nephrectomy: Effect on
overall and noncancer mortality. Cancer. 115:1465–1471. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sun M, Bianchi M, Trinh QD, Hansen J,
Abdollah F, Hanna N, Tian Z, Shariat SF, Montorsi F, Perrotte P and
Karakiewicz PI: Comparison of partial vs. radical nephrectomy with
regard to other-cause mortality in T1 renal cell carcinoma among
patients aged ≥75 years with multiple comorbidities. BJU Int.
111:67–73. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Novick AC: Laparoscopic and partial
nephrectomy. Clin Cancer Res. 10:S6322–S6327. 2004. View Article : Google Scholar
|
|
21
|
Roos FC, Brenner W, Jäger W, Albert C,
Müller M, Thüroff JW and Hampel C: Perioperative morbidity and
renal function in young and elderly patients undergoing elective
nephron-sparing surgery or radical nephrectomy for renal tumours
larger than 4 cm. BJU Int. 107:554–561. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Roos FC, Pahernik S, Melchior SW and
Thüroff JW: Renal tumour surgery in elderly patients. BJU Int.
102:680–683. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Thomas AA, Aron M, Hernandez AV, Lane BR
and Gill IS: Laparoscopic partial nephrectomy in octogenarians.
Urology. 74:1042–1046. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Guzzo TJ, Allaf ME, Pierorazio PM, Miller
D, McNeil BK, Kavoussi LR, Pavlovich CP and Schaeffer EM:
Perioperative outcomes of elderly patients undergoing laparoscopic
renal procedures. Urology. 73:572–576. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dulabon LM, Lowrance WT, Russo P and Huang
WC: Trends in renal tumor surgery delivery within the United
States. Cancer. 116:2316–2321. 2010.PubMed/NCBI
|
|
26
|
Huang WC, Elkin EB, Levey AS, Jang TL and
Russo P: Partial nephrectomy versus radical nephrectomy in patients
with small renal tumors-is there a difference in mortality and
cardiovascular outcomes? J Urol. 181:55–62. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Simmons MN, Chung BI and Gill IS:
Perioperative efficacy of laparoscopic partial nephrectomy for
tumors larger than 4 cm. Eur Urol. 55:199–207. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Patel MN, Krane LS, Bhandari A, Laungani
RG, Shrivastava A, Siddiqui SA, Menon M and Rogers CG: Robotic
partial nephrectomy for renal tumors larger than 4 cm. Eur Urol.
57:310–316. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tobert CM, Riedinger CB and Lane BR: Do we
know (or just believe) that partial nephrectomy leads to better
survival than radical nephrectomy for renal cancer? World J Urol.
32:573–579. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
An JY, Ball MW, Gorin MA, Hong JJ, Johnson
MH, Pavlovich CP, Allaf ME and Pierorazio PM: Partial vs. radical
nephrectomy for T1-T2 renal masses in the Elderly: Comparison of
complications, renal function, and oncologic outcomes. Urology.
100:151–157. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Huang WC, Levey AS, Serio AM, Snyder M,
Vickers AJ, Raj GV, Scardino PT and Russo P: Chronic kidney disease
after nephrectomy in patients with renal cortical tumours: A
retrospective cohort study. Lancet Oncol. 7:735–740. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bianchi M, Gandaglia G, Trinh QD, Hansen
J, Becker A, Abdollah F, Tian Z, Lughezzani G, Roghmann F, Briganti
A, et al: A population-based competing-risks analysis of survival
after nephrectomy for renal cell carcinoma. Urol Oncol.
32:46.e1–e7. 2014. View Article : Google Scholar
|
|
33
|
Capitanio U, Terrone C, Antonelli A,
Minervini A, Volpe A, Furlan M, Matloob R, Regis F, Fiori C,
Porpiglia F, et al: Nephron-sparing techniques independently
decrease the risk of cardiovascular events relative to radical
nephrectomy in patients with a T1a-T1b renal mass and normal
preoperative renal function. Eur Urol. 67:683–689. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Becker F, Siemer S, Hack M, Humke U,
Ziegler M and Stockle M: Excellent long-term cancer control with
elective nephron-sparing surgery for selected renal cell carcinomas
measuring more than 4 cm. Eur Urol. 49:1058–1064. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Weight CJ, Larson BT, Fergany AF, Gao T,
Lane BR, Campbell SC, Kaouk JH, Klein EA and Novick AC: Nephrectomy
induced chronic renal insufficiency is associated with increased
risk of cardiovascular death and death from any cause in patients
with localized cT1b renal masses. J Urol. 183:1317–1323. 2010.
View Article : Google Scholar : PubMed/NCBI
|