Introduction
Lung cancer is the main cause of cancer death. The
incidence rate and mortality rate are the largest proportion of
malignant tumors in China (1).
According to statistics, there were 1.82 million new lung cancer
cases and 1.59 million deaths worldwide in 2012 (2). The global prevalence of tobacco has led
to a rapid increase in new lung cancer cases and deaths. It is
estimated that the death toll from lung cancer in the world will
increase to 3 million by 2035, with men increasing from 1.1 million
in 2012 to 2.1 million in 2035 and women from 500,000 in 2012 to
900,000 in 2035 (3). Second-hand
tobacco smoke is also an important cause of lung cancer. It is
estimated that 21,400 non-smokers die of lung cancer every year
(4). The extremely high morbidity
and mortality rate of lung cancer has caused heavy economic and
health burden. Although diagnosis and treatment have made great
progress, the 5-year overall survival rate is only approximately
15% (5), with poor prognosis.
Therefore, the diagnosis, treatment and prognosis of lung cancer
are still highly concerning issues.
At present, chemotherapy, radiotherapy and radical
resection of lung cancer are the main treatments for lung cancer in
clinic (6). Radical resection of
lung cancer is the first choice for patients who can be treated
surgically and can accept surgical risks although the risk is
relatively high (7). Anesthesia is
the decisive factor for the success of the operation, sevoflurane
inhalation anesthesia is the commonly used anesthesia method for
thoracotomy, and combined epidural anesthesia has higher
hemodynamic stability (8). Cognitive
dysfunction is a common adverse complication after anesthesia
surgery. Studies have found that S-100β is a calcium binding
protein of low molecular weight and is found in glial cells of
central and peripheral nervous systems (9,10).
S-100β in serum is at physiologically low concentration in healthy
population, and not easy to detect, but the expression in serum of
brain injured people is abnormally increased (11–13). The
level of S-100β in patients' serum can evaluate cognitive function,
but its prognostic value in lung cancer has not been studied.
ICAM-1 is an adhesion molecule and a member of the immunoglobulin
superfamily genes. It is related to cell migration and invasion,
plays a role in tumor metastasis (14), and can be used as a prognostic factor
for patients (15).
This study examined the concentration changes of
ICAM-1 and S-100β in sevoflurane combined with epidural anesthesia
for radical resection of lung cancer at different times to study
the predictive value of the two proteins for perioperative adverse
complications and patient prognosis.
Patients and methods
Collection of clinical data
In total, 172 lung cancer patients diagnosed and
treated in Tianjin Chest Hospital (Tianjin, China) from May 2014 to
January 2016 were collected as the therapy group (TG) and 160
normal healthy people who underwent physical examination in the
hospital during the same period were collected as the control group
(CG). The laboratory and imaging examinations of the patients in
the CG were normal without allergic diseases and autoimmune
diseases. This study was approved by the Ethics Committee of
Tianjin Chest Hospital.
Inclusion and exclusion criteria of
the patients
Inclusion criteria: The patients were diagnosed as
non-small cell lung cancer by thoracoscopic pleural biopsy. The
diagnostic criteria referred to the lung cancer guidelines of the
American College of Chest Physicians in 2013 (10). Tumor diameter was <5 cm and ASA-PS
grade (16) was ≥3. The patients did
not undergo radiotherapy or chemotherapy and were able to tolerate
one-lung ventilation. The patients had complete clinical data.
Patients and their families were informed and signed an informed
consent form.
Exclusion criteria: hypovolemia, shock, infection at
puncture site, mental disease, low coagulation, hepatic and kidney
function obstacle. Patients and their families had concerns.
Anesthesia methods
Before the operation, 8 ml/kg/h of lactated ringer's
solution (item number: H10983055, Shanghai Baite Medical Product
Co., Ltd.) was injected through the forearm vein approach.
Electrocardiogram, heart rate (HR), blood oxygen saturation
(SpO2) and double spectrum index (BIS) were monitored.
Arterial pressure was monitored by right invasive arterial puncture
and catheter check. Central venous pressure (CVP) was monitored by
right internal jugular vein puncture and catheter check. Epidural
puncture and catheterization were performed on T 7–8, followed by 3
ml and 2% lidocaine (Southwest Pharmaceutical Co., Ltd., SFDA
approval no. H50020038). It was confirmed that there were no
adverse reactions after anesthesia. Before skin incision for 30
min, 10 ml of 0.25% ropivacaine (Guangdong Jiabo Pharmaceutical
Co., Ltd., SFDA approval no. H20133178) and 2 µg/ml of fentanyl
(Yichang Humanwell Pharmaceutical Co., Ltd., SFDA approval no.
H20003688) were injected into the epidural space. Induction of
general anesthesia was inhalation of 8% sevoflurane (Shanghai
Hengrui Pharmaceutical Co., Ltd, SFDA approval no. H20070172) at a
high flow rate (oxygen flow rate 8–10 l/min). After losing
consciousness, the oxygen flow rate was adjusted to 2 l/min. The
end tidal sevoflurane concentration was kept at 2%. The tidal
volume of mechanical ventilation was 6–8 ml/kg. The respiratory
frequency was 12 times/min, with the exhalation: inhalation = 1:2.
The oxygen flow rate was 2.0 l/min. Anesthesia maintenance was
continuous inhalation of sevoflurane with an end tidal
concentration of 1.5–3.5%. Cisatracurium (0.05–0.1 Mg/kg) was
intermittently intravenously injected (Jiangsu Hengrui
Pharmaceutical Co., Ltd., SFDA approval no. H20060869). End tidal
CO2 partial pressure was 30–40 mmHg, BIS was 40–60 and
CVP was ≤12 cm H2O. The fluctuation of blood pressure
and HR did not exceed 20% of the baseline. Before the end of the
operation for 30 min, the muscle relaxant was stopped and 10 ml of
mixed anesthetic solution was injected into the epidural space.
Sevoflurane inhalation was stopped 10 min before the end of the
operation. The airway was flushed with oxygen at a high flow rate
(4 ml/min). PCIA was performed and VAS score ≤3 was maintained.
When swallowing reflux recovered, spontaneous respiration rate was
≥12 times/min, CO2 partial pressure was <45 mmHg and
SpO2 was ≥95%. Tracheal catheter was pulled out. The
patient was observed for 30 min. If SpO2 was <92%,
the oxygen mask was used at a speed of 5 l/min. There were no
routine preventive measures against nausea and vomiting. If
symptoms worsen, drugs should be prescribed. The patient returned
to the ward after reaching the corrected Aldrete score ≥9 (17).
Sample collection and detection
Venous blood (2 ml) was taken from the CG at fasting
and the four time points of T1, T2, T3 and T4. The blood was
allowed to stand at room temperature for 30 min and centrifuged at
3,000 × g at 4°C for 10 min. The supernatant was frozen in a
refrigerator at −80°C for centralized detection.
Detection of ICAM-1 concentration in
serum by ELISA
Blank, standard and sample wells to be tested were
set up. The SO standard sample with a concentration of 0 was added
into the blank well. The standard sample was added into the
standard well. The sample well was first added with the sample to
be tested. Sample diluent and horseradish peroxidase (HRP) labeled
detection antibody were added to all micropores except the sample
well. The unbound biotinylation antibodies were removed by full
washing. HRP-labeled avidin was added and TMB substrates were added
to color after washing again. TMB turned blue under catalysis and
yellow under the action of acid. The absorbance (OD value) was
measured by enzyme micro-plate reader at 450 nm wavelength. The
corresponding concentration was converted from the standard
curve.
Detection of S-100β concentration in
serum by RT-PCR
The collected serum was extracted with TRIzol kit
(Invitrogen™; Thermo Fisher Scientific, Inc., 15596026) for total
RNA. The purity, concentration and integrity of the extracted total
RNA were detected with ultraviolet spectrophotometer and agarose
gel electrophoresis. 5X TransScript® II All-in-One
SpuperMix for qPCR and gDNA Remover kit (belonging to TransScript
Green two-step qrt-pcr SuperMix) were used for reverse
transcription. The operation procedure was strictly in accordance
with the manufacturer's kit. Then TransScript Green Two-Step
qRT-PCR SuperMix (China TransGen Biotech, AQ201-01) and ABI7500
(Applied Biosystems™; Thermo Fisher Scientific, Inc.) were used for
PCR amplification. PCR reaction system was 1 µl of cDNA, each 0.4
µl of upstream and downstream primers, 10 µl of 2X
TransScript® Tip Green qPCR SuperMix and Passive
Reference Dye (50X). Finally, Nuclease-free Water was added to
replenish to 20 µl. PCR reaction conditions were pre-degeneration
at 94°C for 30 sec, degeneration at 94°C for 5 sec, annealing and
extention at 60°C for 30 sec, then followed a total of 40 cycles.
Then 3 repeated wells were set up of each sample. The experiment
was carried out 3 times. In this study, GAPDH was used as internal
parameters. 2−∆∆Ct was used to analyze the data.
Follow-up of patients
The survival of the patients was followed up for 3
years through outpatients' reexamination and by telephone.
Follow-up time was 1, 3, 6, 12, 24, 36 months from the patients'
radical resection of lung cancer to the follow-up time or the death
of the patients.
Observation indexes
Main outcome measures: The concentration changes of
ICAM-1 and S-100β before and after treatment. The predictive value
of ICAM-1 and S-100β for adverse complications during perioperative
period. The predictive value of ICAM-1 and S-100β for death of
patient prognosis within 3 years.
Secondary observation index: The survival curve was
drawn according to the survival of the patients. The median
concentration of ICAM-1 and S-100β before treatment was taken and
divided into high and low expression groups to draw the survival
curve of the patients.
Statistical analysis
In this study, SPSS20.0 (Shanghai Cabe Information
Technology Co., Ltd.) was used to carry out statistical analysis on
the collected data. GraphPad Prism 7 (Shenzhen Qiruitian Software
Technology Co., Ltd.) was used to draw the illustrations. Counting
data was expressed as a percentage (%). Chi-square test was used,
and expressed as χ2. All data conformed to normal
distribution and were expressed by mean number ± standard deviation
(mean ± SD). The independent sample t-test was used for inter-group
comparisons. Multiple time points were expressed by repetitive
measurement and analysis of variance, expressed as F. Then
Bonferroni test was used for inspection. P<0.05 was considered
to indicate a statistically significant difference.
Results
Comparison of baseline data of
patients in both groups
According to the data in Table I, there was no significant difference
in age, sex, BMI and place of residence between the TG and CG
(P>0.05), which were comparable.
 | Table I.Baseline data. |
Table I.
Baseline data.
| Factors | TG (n=172) | CG (n=160) | t/χ2
value | P-value |
|---|
| Age | 60.2±9.7 | 58.9±11.2 | 1.133 | 0.258 |
| Sex |
| Male | 115 (66.86) | 108 (67.50) | 0.015 | 0.901 |
|
Female | 57 (33.14) | 52 (32.50) |
|
|
| BMI
(kg/m2) | 21.8±1.6 | 22.1±1.2 | 1.922 | 0.056 |
| Place of
residence |
|
| 0.106 | 0.745 |
| City | 88 (51.16) | 79 (49.38) |
|
|
|
Rural | 84 (48.84) | 81 (50.62) |
|
|
| Differentiation
degree |
| Poorly
differentiated | 54
(31.40) | 0 (0.00) |
|
|
| Medium +
well differentiated | 118 (68.60) | 0 (0.00) |
|
|
| Lymphatic
metastasis |
|
Metastasis | 124 (72.09) | 0 (0.00) |
|
|
|
Non-metastasis | 48
(27.91) | 0 (0.00) |
|
|
| TNM stages |
| T1 | 67
(38.40) | 0 (0.00) |
|
|
| T2 | 105 (61.6) | 0 (0.00) |
|
|
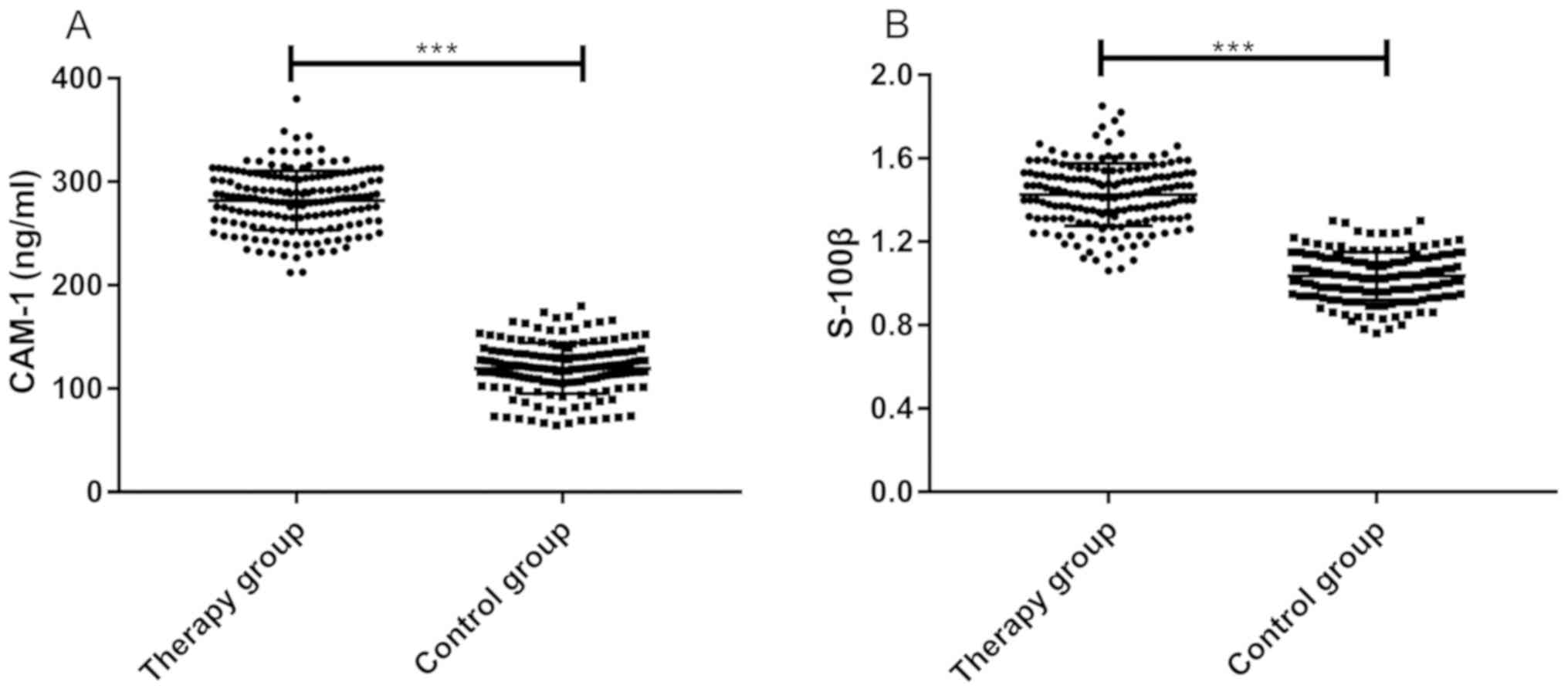
Comparison of ICAM-1 and S-100β
concentrations of patients in both groups
Comparing the concentration of ICAM-1 and S-100β in
the serum of the TG and the CG before treatment, it was found that
the concentration of ICAM-1 in the serum of TG (283.174±31.543) was
significantly higher than that of CG (119.281±24.615) (P<0.001).
The concentration of S-100β in the serum of TG (1.412±0.147) was
significantly higher than that of CG (1.031±0.112) (P<0.001), as
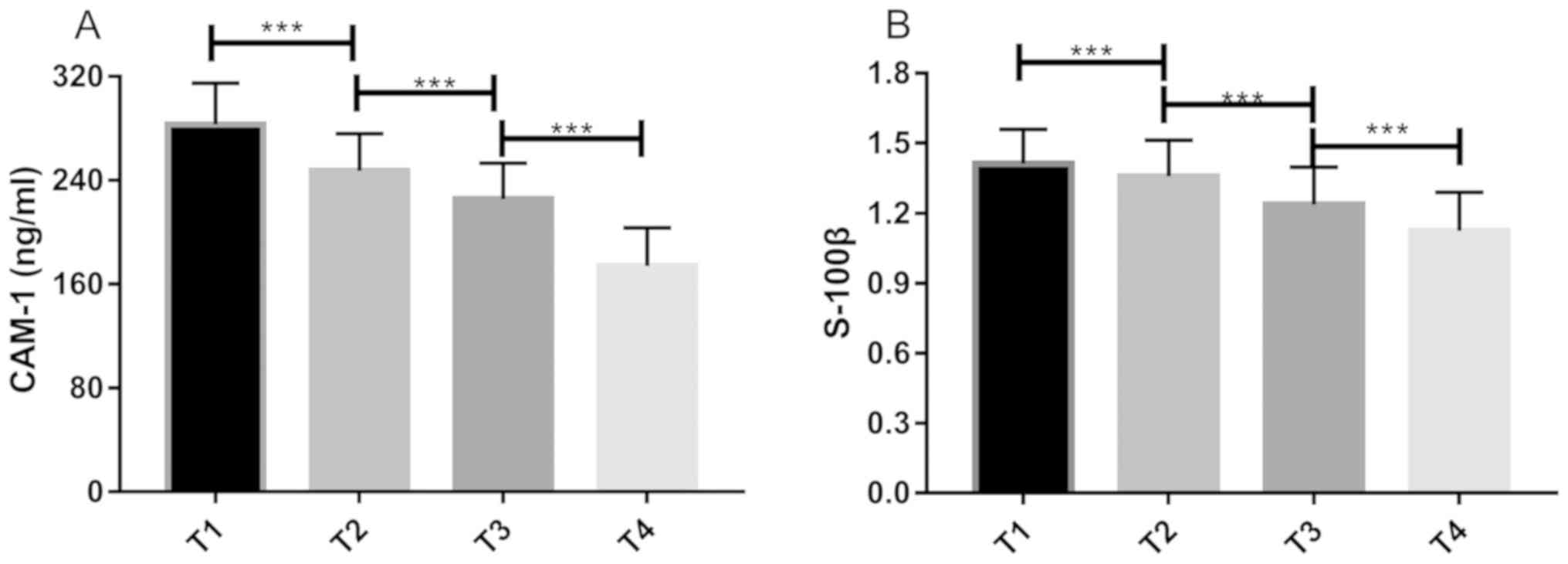
shown in Fig. 1. The concentration
of ICAM-1 in TG was highest at T1 (283.174±31.543) (P<0.001),
followed by T2 (247.246±28.714) (P<0.001). The concentration of
ICAM-1 at T3 (225.436±27.827) was higher than T4 (174.113±29.281)
(P<0.001). In TG, the concentration of S-100β at T1
(1.412±0.147) was the highest (P<0.001), followed by T2
(1.358±0.154) (P<0.001). The concentration of S-100β at T3
(1.236±0.161) was higher than T4 (1.124±0.165) (P<0.001), as
shown in Fig. 2.
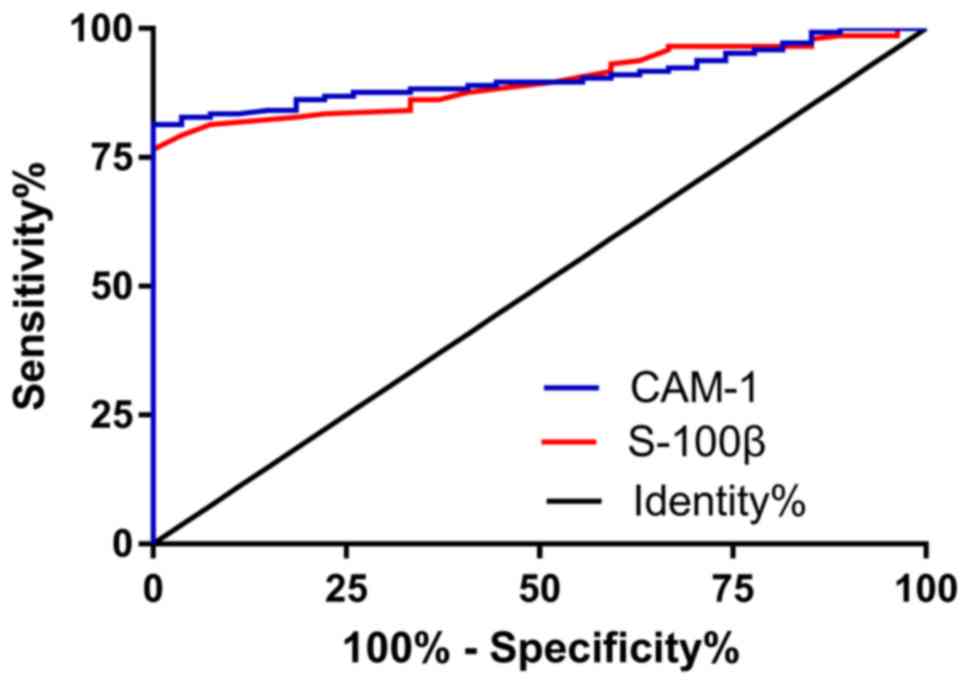
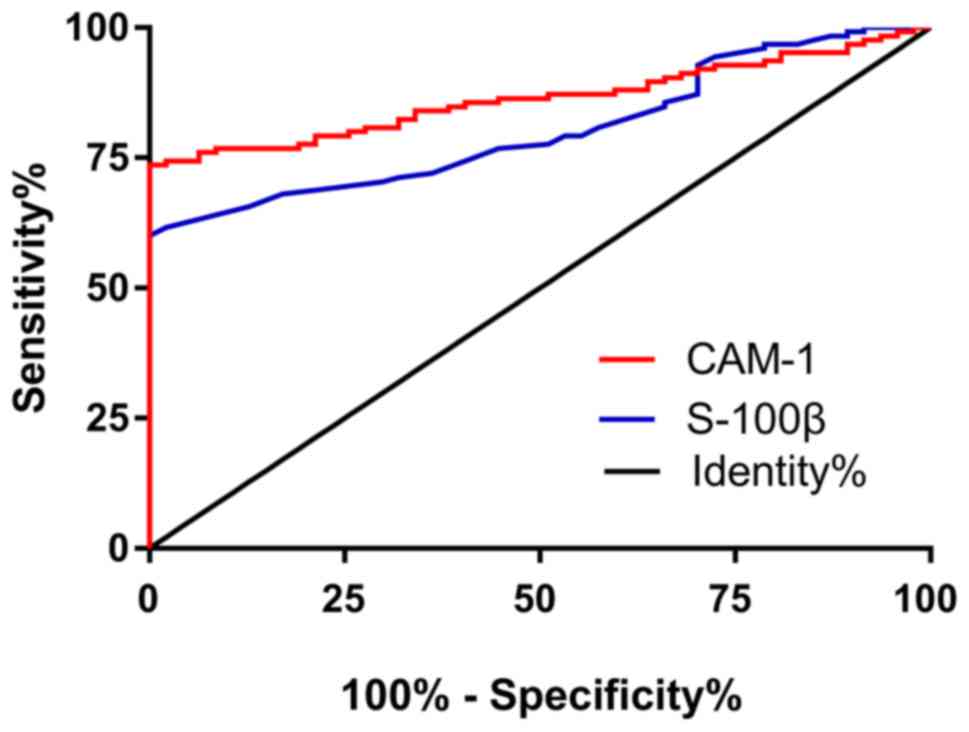
The predictive value of ICAM-1 and
S-100β for perioperative adverse complications of patients
According to statistics, a total of 27 patients in
TG had cognitive dysfunction during the perioperative period.
Patients with adverse complications and patients without adverse
complications were divided into two groups. Receiver operating
characteristics (ROC) curves were drawn according to the
concentrations of ICAM-1 and S-100β in the serum of patients in the
two groups before treatment. The results showed that the area under
ICAM-1 curve was 0.906 and the youden index was 81.38%. When
cut-off value was >266, the sensitivity and specificity of
ICAM-1 in predicting perioperative adverse complications were 81.38
and 100%, respectively. The area under the S-100β curve was 0.899
and the youden index was 76.55%. When cut-off value was >1.375,
the sensitivity and specificity of S-100β in predicting
perioperative adverse complications were 76.55 and 100%,
respectively, as shown in Fig.
3.
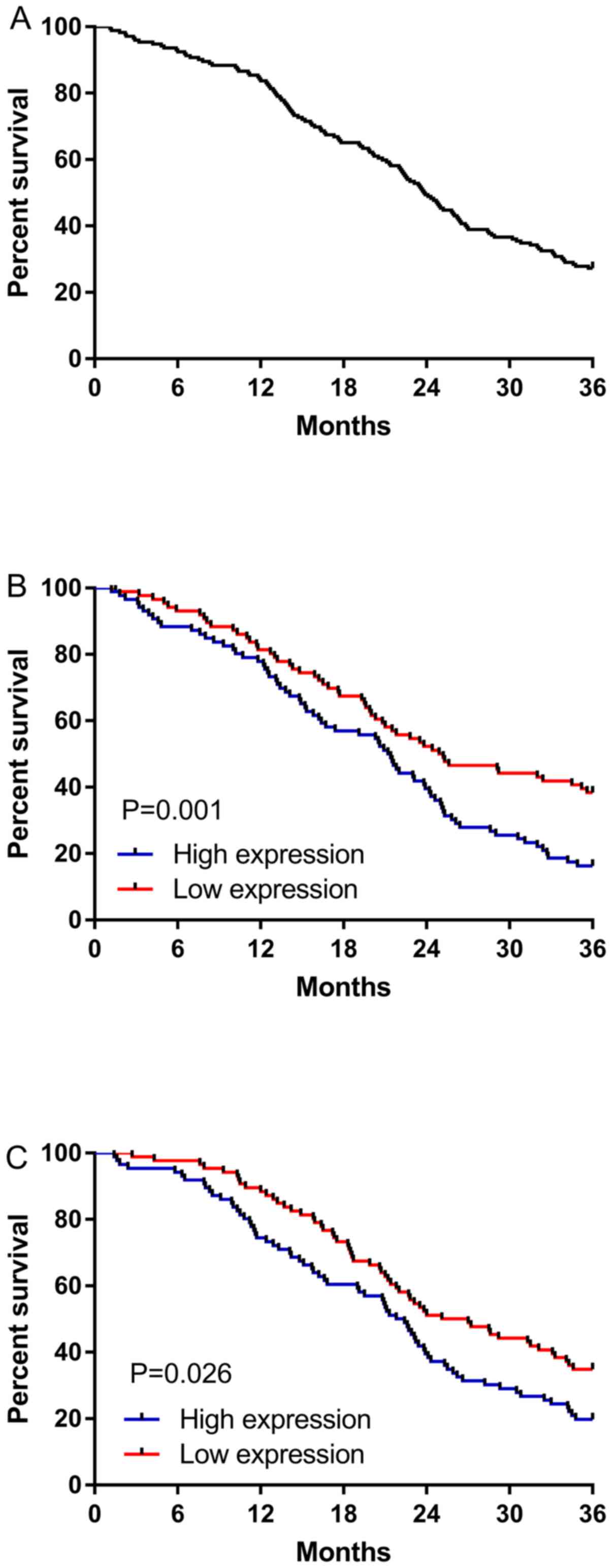
Relationship between survival of
patients, ICAM-1 and S-100β
According to statistics on the overall survival rate
of the patients, the results showed that the 172 patients were
followed up without any defects and the overall survival rate of
the patients was 37.60%. According to the median concentration of
ICAM-1 and S-100β before treatment, the patients were divided into
high and low concentration groups, respectively. Observation on the
overall survival rate of the two groups showed that the overall
survival rate of the ICAM-1 low concentration group (CLCG) was
significantly higher than that of the ICAM-1 high concentration
group (CHCG). There was a significant difference in survival
between the two groups (P=0.001). The overall survival rate of the
S-100β low concentration group (SLCG) was significantly higher than
that of the S-100β high concentration group (SHCG). There was a
significant difference in survival between the two groups
(P=0.026). The deceased and the surviving patients after the
follow-up were divided into two groups. ROC curves were drawn
according to the concentrations of ICAM-1 and S-100β in the serum
of the two groups before treatment. The results showed that the
area under ICAM-1 curve was 0.864 and the youden index was 73.60%.
When cut-off value was >280.9, the sensitivity and specificity
of ICAM-1 in predicting the prognosis of patients with death within
3 years were 73.60 and 100%, respectively. The area under the
S-100β curve was 0.804 and the youden index was 60%. When cut-off
value was >1.465, the sensitivity and specificity of S-100β in
predicting the prognosis of patients with death within 3 years were
60 and 100%, respectively, as shown in Figs. 4 and 5.
Discussion
With the prevalence of tobacco, lung cancer has
changed from a rare disease to a global and a public health
problem. From the perspective of public health, effective tobacco
control is the main strategy to prevent lung cancer. Although
smoking rate has begun to decline, lung cancer patients are still
increasing year by year. According to a study from South Korean,
the number of people who have never smoked with lung cancer has
increased (18). Therefore, the
treatment and prognosis of lung cancer is still a growing concern
in the whole society.
At present, chemotherapy, radiotherapy and lobectomy
are the main treatments for lung cancer in clinic. Surgery is the
best way to treat lung cancer for patients who meet the surgical
indications. Studies have found that at least 30% of patients with
primary resectable non-small cell lung cancer will relapse within 5
years after treatment (19). Relapse
is the main decisive factor of patient death. Therefore, it may
improve treatment allocation to find a good prognosis index, thus
providing adjuvant treatment for patients with high recurrence risk
after surgery. Inflammation is an important component of tumor
progression. Neutrophils and lymphocytes are commonly used as
prognostic indicators for lung cancer patients in clinic (20). However, tumor-related adverse
reactions, such as anorexia, can also promote the expression of
inflammatory factors, which cannot fully prove the biological basis
of systemic inflammatory prognosis. Therefore, it is particularly
important to find new serological prognostic indicators to improve
the current situation. Adhesion of tumor cells to endothelial cells
by ICAM-1 is a key step in metastasis, which indicates poor
prognosis of lung cancer patients to a large extent. However,
cognitive dysfunction usually occurs after surgery anesthesia.
Studies have found that S-100β can be used as a prognostic
indicator for patients with craniocerebral injury (21), but there are few studies on it as a
prognostic indicator for lung cancer. Therefore, this study
examined the concentration changes of ICAM-1 and S-100β in
sevoflurane combined with epidural anesthesia for radical resection
of lung cancer at different times to study the predictive value of
the two proteins for perioperative adverse complications and
patient prognosis.
In this study, we found that the concentration of
ICAM-1 and S-100β in patients' serum was significantly higher than
that in CG by comparing the concentration of ICAM-1 and S-100β in
the serum of the two groups before treatment. The differential
expression of the two proteins in patients and healthy people
suggested that they may be used as diagnostic indicators for lung
cancer. However, because this study focused on its significance for
the prognosis of patients, the diagnostic value has not been
thoroughly studied. Then we detected the concentration of ICAM-1
and S-100β in patients' serum at T1, T2, T3 and T4. It was found
that the concentration of ICAM-1 and S-100β decreased gradually.
Finzel et al (22) found that
after blocking endothelial soluble ICAM-1 with monoclonal antibody,
its expression levels and adhesion decreased significantly. It was
basically consistent with our research results. The results of Qiao
et al (23) showed that the
concentration of S-100β increased after sevoflurane anesthesia
alone, while this research showed that the concentration gradually
decreased. We speculated that the reason was that the operation
combined with epidural puncture anesthesia reduced the stress
response of patients and the cognitive dysfunction.
Anesthetic surgery is usually accompanied by adverse
complications. This study counted 27 cases of adverse complications
during perioperative period. Patients were divided into two groups
according to whether adverse complications occurred or not. ROC
curves were drawn according to the concentrations of ICAM-1 and
S-100β in the serum of patients in the two groups. The results
showed that ICAM-1 and S-100β had the best prediction specificity
and sensitivity when cut-off values were >266 and >1.375,
respectively, which suggested that ICAM-1 and S-100β might be used
as indicators to predict the occurrence of adverse complications in
patients during perioperative period. The high expression of ICAM-1
and S-100β indicates that tumor metastasis is accelerated, brain
injury is serious and it is significantly reduced after treatment.
According to the results of this study, it also showed that it has
high value in predicting adverse complications during the
perioperative period.
The prognosis of lung cancer patients is poor and
the 5-year survival rate is less than 18% (24). According to our statistics, the
3-year overall survival rate was only 37.6%. Although the treatment
of lung cancer has made great progress, the treatment results are
still unsatisfactory due to late diagnosis, older patients,
concomitant diseases and limited treatment options (25). According to the median concentration
of ICAM-1 and S-100β before treatment, the patients were divided
into high and low concentration groups. The value of the two
indexes in patients' survival was observed. The results showed that
the overall survival rate of CLCG and SLCG was significantly higher
than that of CHCG and SHCG. There was a significant difference in
survival between the two groups. It indicated that the two indexes
had predictive value in patients' short-term prognosis and could be
used as potential survival predictive indexes of patients.
Therefore, we further drew ROC curves for the survival of patients.
The results showed that when the concentrations of ICAM-1 and
S-100β were >280.9 and >1.465 respectively, the prediction
sensitivity was 73.60% and 60%, respectively, and the specificity
was 100%. We speculate that the reason may be that the
concentration of ICAM-1 and S-100β decreased significantly after
treatment, the adhesion decreased and the brain injury decreased,
thus slowing down the metastasis of tumor cells and improving the
disease. Moreover, patients with low concentration of ICAM-1 and
S-100β before treatment have better efficacy than patients with
high concentration. Therefore, we speculate that high or low
concentration of ICAM-1 and S-100β before treatment can predict the
survival of patients. The value of ICAM-1 as a prognostic indicator
was also reported by Kotteas et al (7).
Collectively, ICAM-1 and S-100β protein in
sevoflurane combined with epidural anesthesia for radical resection
of lung cancer can effectively predict the perioperative adverse
complications of patients, and have better monitoring significance
for the prognosis of patients.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
NZ wrote the manuscript and was responsible for
anesthesia. CL conceived and designed the study. LL was responsible
for the collection and analysis of the experimental data. PS
interpreted the data and drafted the manuscript. JH detected S-100β
concentration and revised the manuscript critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Tianjin Chest Hospital (Tianjin, China). Patients who participated
in this research had complete clinical data. Signed informed
consents were obtained from the patients and/or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cheng TY, Cramb SM, Baade PD, Youlden DR,
Nwogu C and Reid ME: The international epidemiology of lung cancer:
Latest trends, disparities, and tumor characteristics. J Thorac
Oncol. 11:1653–1671. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Didkowska J, Wojciechowska U, Mańczuk M
and Łobaszewski J: Lung cancer epidemiology: Contemporary and
future challenges worldwide. Ann Transl Med. 4:1502016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Oberg M, Jaakkola MS, Woodward A, Peruga A
and Prüss-Ustün A: Worldwide burden of disease from exposure to
second-hand smoke: A retrospective analysis of data from 192
countries. Lancet. 377:139–146. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Molina JR, Yang P, Cassivi SD, Schild SE
and Adjei AA: Non-small cell lung cancer: Epidemiology, risk
factors, treatment, and survivorship. Mayo Clin Proc. 83:584–594.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Vansteenkiste J, De Ruysscher D, Eberhardt
WE, Lim E, Senan S, Felip E and Peters S; ESMO Guidelines Working
Group, : Early and locally advanced non-small-cell lung cancer
(NSCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment
and follow-up. Ann Oncol. 24 (Suppl 6):vi89–vi98. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kotteas EA, Gkiozos I, Tsagkouli S, Bastas
A, Ntanos I, Saif MW and Syrigos KN: Soluble ICAM-1 levels in
small-cell lung cancer: Prognostic value for survival and
predictive significance for response during chemotherapy. Med
Oncol. 30:6622013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zhao L, Liu L, Dong Z and Xiong J: miR-149
suppresses human non-small cell lung cancer growth and metastasis
by inhibiting the FOXM1/cyclin D1/MMP2 axis. Oncol Rep.
38:3522–3530. 2017.PubMed/NCBI
|
|
9
|
Neselius S, Brisby H, Theodorsson A,
Blennow K, Zetterberg H and Marcusson J: CSF-biomarkers in Olympic
boxing: Diagnosis and effects of repetitive head trauma. PLoS One.
7:e336062012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rivera MP, Mehta AC and Wahidi MM:
Establishing the diagnosis of lung cancer: Diagnosis and management
of lung cancer, 3rd ed: American College of Chest Physicians
evidence-based clinical practice guidelines. Chest. 143
(Suppl):e142S–e165S. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Xianbao L, Hong Z, Xu Z, Chunfang Z and
Dunjin C: Dexmedetomidine reduced cytokine release during
postpartum bleeding-induced multiple organ dysfunction syndrome in
rats. Mediators Inflamm. 2013:6278312013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Qin B, Panickar KS and Anderson RA:
Cinnamon polyphenols attenuate the hydrogen peroxide-induced down
regulation of S100β secretion by regulating sirtuin 1 in C6 rat
glioma cells. Life Sci. 102:72–79. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ehrenreich H, Kästner A, Weissenborn K,
Streeter J, Sperling S, Wang KK, Worthmann H, Hayes RL, von Ahsen
N, Kastrup A, et al: Circulating damage marker profiles support a
neuroprotective effect of erythropoietin in ischemic stroke
patients. Mol Med. 17:1306–1310. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao LH, Shi ZH, Yin NN and Zhou JX: Use
of dexmedetomidine for prophylactic analgesia and sedation in
delayed extubation patients after craniotomy: A study protocol and
statistical analysis plan for a randomized controlled trial.
Trials. 14:2512013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Marenholz I, Heizmann CW and Fritz G: S100
proteins in mouse and man: From evolution to function and pathology
(including an update of the nomenclature). Biochem Biophys Res
Commun. 322:1111–1122. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Sankar A, Johnson SR, Beattie WS, Tait G
and Wijeysundera DN: Reliability of the American Society of
Anesthesiologists physical status scale in clinical practice. Br J
Anaesth. 113:424–432. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li R, Xu X, Wu XM, Xiong LZ, Guo QL, Lian
QQ, Heng XH, Zhang Y and Qing EM: Effect of dexmedetomidine on
responses to endotracheal extubation during recovery from general
anesthesia in patients with hypertension: A multicenter,
randomized, blind, placebo-controlled clinical trial. Chin J
Anesthesiol. 33:397–401. 2013.(In Chinese).
|
|
18
|
Park JY and Jang SH: Epidemiology of lung
cancer in Korea: Recent trends. Tuberc Respir Dis (Seoul).
79:58–69. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cedrés S, Torrejon D, Martínez A, Martinez
P, Navarro A, Zamora E, Mulet-Margalef N and Felip E: Neutrophil to
lymphocyte ratio (NLR) as an indicator of poor prognosis in stage
IV non-small cell lung cancer. Clin Transl Oncol. 14:864–869. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mercier E, Boutin A, Lauzier F, Fergusson
DA, Simard JF, Zarychanski R, Moore L, McIntyre LA, Archambault P,
Lamontagne F, et al: Predictive value of S-100β protein for
prognosis in patients with moderate and severe traumatic brain
injury: Systematic review and meta-analysis. BMJ. 346((apr04 1)):
f17572013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Pinato DJ, Shiner RJ, Seckl MJ, Stebbing
J, Sharma R and Mauri FA: Prognostic performance of
inflammation-based prognostic indices in primary operable non-small
cell lung cancer. Br J Cancer. 110:1930–1935. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Finzel AH, Reininger AJ, Bode PA and
Wurzinger LJ: ICAM-1 supports adhesion of human small-cell lung
carcinoma to endothelial cells. Clin Exp Metastasis. 21:185–189.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Qiao Y, Feng H, Zhao T, Yan H, Zhang H and
Zhao X: Postoperative cognitive dysfunction after inhalational
anesthesia in elderly patients undergoing major surgery: The
influence of anesthetic technique, cerebral injury and systemic
inflammation. BMC Anesthesiol. 15:1542015. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zappa C and Mousa SA: Non-small cell lung
cancer: Current treatment and future advances. Transl Lung Cancer
Res. 5:288–300. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Leppert W: Quality of life in patients
with advanced lung cancer at home palliative care at the in-patient
palliative care unit. Medycyna Paliatywna. 1:25–34. 2010.
|