Introduction
Lung cancer is the most commonly diagnosed malignant
tumor and one of the leading causes of cancer-associated mortality
worldwide and in China (1,2). Non-small-cell lung cancer (NSCLC)
represents ~85–90% of the total number of lung cancer cases
(3) and may be divided into three
pathological subtypes: Adenocarcinoma, squamous cell carcinoma and
large cell carcinoma (4). Among
these, lung adenocarcinoma (LUAD) is the most common pathological
subtype and accounts for ~40% of all lung cancer cases (5). Despite progress in diagnosis and
treatment, the 5 year survival rate of patients with NSCLC remains
low (~15%), which is mainly attributed to the low rate of diagnosis
in the early stages of the disease and a high rate of cancer
recurrence and metastasis (3,6).
Therefore, the identification and validation of novel biomarkers
may improve the prognosis of patients with LUAD.
Interleukin-enhancer binding factor 3 (ILF3) plays
an important role in modulating numerous aspects of RNA metabolism,
primarily due to its double-stranded RNA-binding motifs (7). Consequently, ILF3 participates in
various cellular biological processes, including cell cycle
regulation, DNA metabolism, transcription, translation, mRNA
stability, microRNA expression and circular RNA (circRNA)
regulation (8–13). Moreover, ILF3 has been linked to the
occurrence and progression of various malignant tumors (14–18). For
example, ILF3 has been shown to contribute to the occurrence of
breast cancer by maintaining the expression of the urokinase-type
plasminogen activator (14).
Importantly, ILF3 was found to be highly expressed in advanced
breast cancer tissues, and the upregulation of ILF3 was negatively
associated with the distant metastasis-free survival of patients
with breast cancer (15). In human
epithelial ovarian cancer, the expression level of ILF3 was
increased in tumor tissues compared with peri-tumor tissues and was
significantly higher in serous carcinomas compared with mucinous,
endometrial and clear cell carcinomas (16). Furthermore, compared with early-stage
or well-differentiated ovarian cancer, the expression level of ILF3
was increased in late-stage or poorly-differentiated ovarian cancer
(17). It has also been reported
that ILF3 sustains the epidermal growth factor receptor-mediated
signaling pathway in NSCLC, indicating that ILF3 may serve an
important role in the occurrence of cancer (18).
To the best of our knowledge, the prognostic value
of ILF3 and its potential predictive significance for guiding
clinical practice have not yet been investigated. Therefore, the
aim of the present study was to assess the prognostic value of ILF3
and to apply this knowledge to avoid excessive medical treatment of
patients with LUAD. The results revealed the prognostic value of
ILF3 and established a new prognostic model for overall survival
(OS) time in patients with LUAD.
Materials and methods
Study cohorts
The current present involved two independent sets of
patients with LUAD. The discovery set consisted of 143 patients,
with pathologically confirmed LUAD, who did not receive
chemotherapy or radiotherapy prior to surgical resection of the
tumor. A total of 143 LUAD and 40 adjacent non-cancerous tissues (2
cm from the tumor margin) were collected following surgery at the
Affiliated Hospital of Nantong University (Jiangsu, China) between
January 2009 and December 2011. All samples were pathologically
confirmed by two pathologists from the Department of Pathology,
Affiliated Hospital of Nantong University (Nantong, China). Of the
143 patients, 73 were men while 70 were women, and the mean age of
patients at the time of surgery was 61 years (range, 39–83 years).
The patient clinical data, including gender, smoking status, age,
tumor differentiation and tumor-node-metastasis (TNM) stage, were
retrieved from the hospital records. All patients were staged
according to the 8th edition of the TNM staging system for lung
cancer (19). The OS time was
defined as the time between surgery and mortality from any cause.
The present retrospective study was approved by the Clinical
Research Ethics Committee of The Affiliated Hospital of Nantong
University (Jiangsu, China; approval no. 2017-K025) and all
patients provided written informed consent.
The validation set was downloaded from The Cancer
Genome Atlas (TCGA) database (20),
accessed on November 1st, 2017. The patient inclusion
criteria for the present study were as follows: Availability of
clinical data (including TNM stage, survival status, follow-up
time, smoking status, gender, age and ethnicity), a diagnosis of
pathologically confirmed LUAD and the availability of mRNA-seq data
for ILF3. Patients who died on the day of surgery were excluded
from the study. A total of 501 tumor and 59 peri-tumor unpaired
samples were selected for subsequent study. A total of 228 patients
were men while 273 were women, and the mean age of patients at the
time of surgery was 65.40 years (range, 33–88 years).
Tissue microarrays (TMAs) and
immunohistochemistry (IHC)
Surgical tissue samples was fixed with 10% formalin
for 24 h at room temperature. Formalin-fixed paraffin-embedded
surgical tissue samples were used for TMAs and IHC. To construct
the TMAs, tissue cylinders (2 mm in diameter) were removed from
each sample and selected tissue cylinders were grouped into a
single array block using an Unitma Quick-Ray tissue microarrayer
(cat. no. UT06; Unitma Co., Ltd). Each TMA specimen was
subsequently cut into 4 µm tissue sections, which were mounted on
microscope slides. IHC staining was performed as previously
described (21), except an anti-ILF3
antibody (ab92355; 1:400; Abcam) was used as the primary antibody.
A total of two pathologists blindly evaluated the percentage of
ILF3-positive samples using the NDP.view2 software (version 2.6.13;
Japan SLC, Inc.), as well as the intensity of ILF3 IHC staining. A
semi-quantitative immunoreactivity scoring system was used to
evaluate the staining (22). The
semi-quantitative H-score (0–300) was calculated as the product of
the intensity (0, negative; 1, weak; 2, moderate; 3, strong) and
the percentage of ILF-3-positive samples (0–100).
Statistical analysis
X-tile (version 3.6.1; Yale University), GraphPad
Prism (version 7.00; GraphPad Software), SPSS (version 20.0; IBM
Corp.) and R (version 3.5.2; R Foundation for Statistical
Computing) software were used for the statistical analyses.
Patients in the discovery and validation sets were stratified into
high and low expression groups according to cut-off points (80 and
1,1628.1 for the discovery and validation sets, respectively) that
were computed using X-tile as previously described (23). Differential expression of ILF3
between tumor and peri-tumor samples was analyzed using the
Mann-Whitney-Wilcoxon test. Survival curves and forest plots were
plotted using GraphPad Prism, and the difference in survival
between the groups was evaluated using the log-rank test. The
χ2 or Fisher's exact tests were used to analyze the
association between ILF3 expression and clinicopathological
parameters. The Cox proportional hazards regression model was used
for univariate and multivariate analyses of factors affecting
patient prognosis. The factors that were associated with prognosis
in the univariate analysis were subsequently included in a
multivariate analysis. Nomograms and calibration curves were
plotted using R software with the regression modeling strategies
package (version 5.0.0; http://www.r-project.org). Harrell's concordance index
(C-index) and the Akaike information criterion (AIC) were
calculated to assess and compare the accuracy of the prognostic
models (24). All data are expressed
as the mean ± standard error mean. P<0.05 was considered to
indicate a statistically significant difference.
Results
Association between ILF3 expression,
clinicopathological parameters and OS time in patients with
LUAD
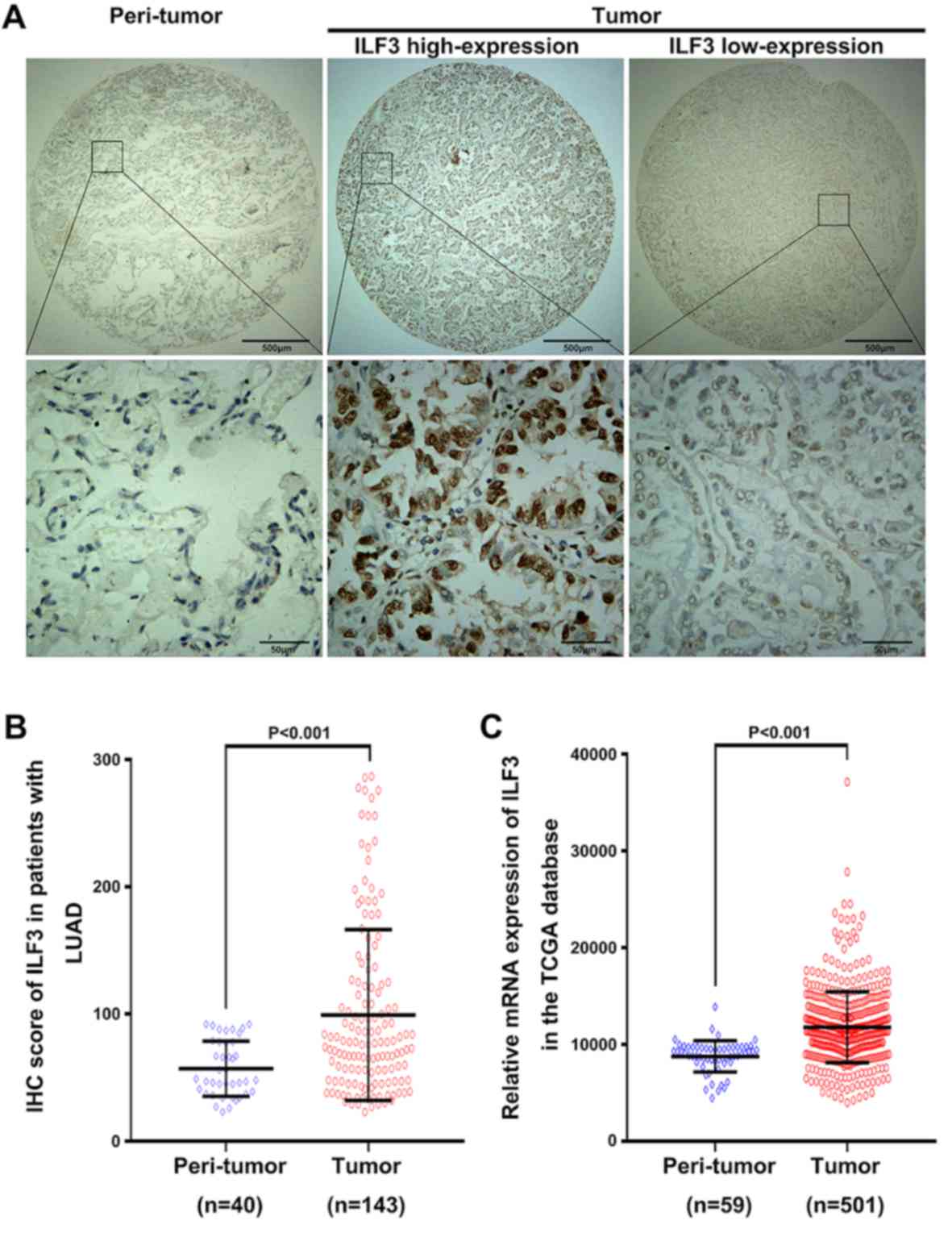
ILF3-positive staining was predominantly observed in
the cytoplasm and nucleus of the LUAD tissue samples (Fig. 1A). The mean expression level of ILF3
in the 143 tumor samples was significantly increased compared with
the 40 peri-tumor samples (P<0.001; Fig. 1B). Furthermore, the mRNA level of
ILF3 was analyzed in 501 tumor and 59 peri-tumor tissue samples in
TCGA database. In line with the IHC staining data, the mRNA level
of ILF3 was increased in the tumor samples compared with the
peri-tumor samples (P<0.001; Fig.
1C).
The association between ILF3 expression and
clinicopathological parameters in patients with LUAD is presented
in Table I. In the discovery set, a
high ILF3 expression level was associated with the TNM stage
(P=0.041). However, no significant association was found between
ILF3 expression and the other clinical parameters examined (tumor
differentiation, gender, age and smoking status). Furthermore, no
significant association between ILF3 expression and the clinical
parameters examined in the TCGA validation set was observed.
 | Table I.Association between ILF3 expression
and clinical characteristics in patients with lung
adenocarcinoma. |
Table I.
Association between ILF3 expression
and clinical characteristics in patients with lung
adenocarcinoma.
| A, Discovery
set |
|---|
|
|---|
|
Characteristics | Low ILF3
expression, n (%) | High ILF3
expression, n (%) | P-value |
|---|
| Sex |
|
| 0.661 |
|
Female | 39 (27.3) | 31 (21.7) |
|
|
Male | 38 (26.6) | 35 (24.5) |
|
| Age (years) |
|
| 0.080 |
|
<60 | 38 (26.6) | 23 (16.1) |
|
|
≥60 | 39 (27.3) | 43 (30.1) |
|
| Smoking |
|
Yes | 14 (9.8) | 18 (12.6) | 0.193 |
|
No/unknown | 63 (44.1) | 48 (33.6) |
|
| TNM stage |
|
| 0.041a |
| I | 49 (34.3) | 28 (19.6) |
|
| II | 19 (13.3) | 22 (15.4) |
|
|
III | 9 (6.3) | 14 (9.8) |
|
| IV | 0 (0.0) | 2 (1.4) |
|
|
Differentiation |
|
| 0.711 |
|
Well | 17 (11.9) | 11 (7.7) |
|
|
Moderately | 44 (30.8) | 41 (28.7) |
|
|
Poorly | 16 (11.2) | 14 (9.8) |
|
|
| B, Validation
set (TCGA) |
|
|
Characteristics | Low ILF3
expression, n (%) | High ILF3
expression, n (%) | P-value |
|
| Gender |
|
| 0.445 |
|
Female | 153 (30.5) | 120 (24.0) |
|
|
Male | 120 (24.0) | 108 (21.6) |
|
| Age (years) |
|
| 0.329 |
|
<60 | 65 (13.0) | 63 (12.6) |
|
|
≥60 | 208 (41.5) | 165 (32.9) |
|
| Smoking status |
|
| 0.591 |
|
Yes | 99 (19.8) | 88 (17.6) |
|
|
No/unknown | 174 (34.7) | 140 (27.9) |
|
| TNM stage |
|
| 0.590 |
| I | 144 (28.7) | 128 (25.6) |
|
| II | 72 (14.4) | 49 (9.8) |
|
|
III | 45 (9.0) | 38 (7.6) |
|
| IV | 12 (2.4) | 13 (2.6) |
|
| Ethnicity |
|
| 0.665 |
|
Caucasian | 68 (13.6) | 53 (10.6) |
|
|
Non-caucasian | 205 (40.9) | 175 (34.9) |
|
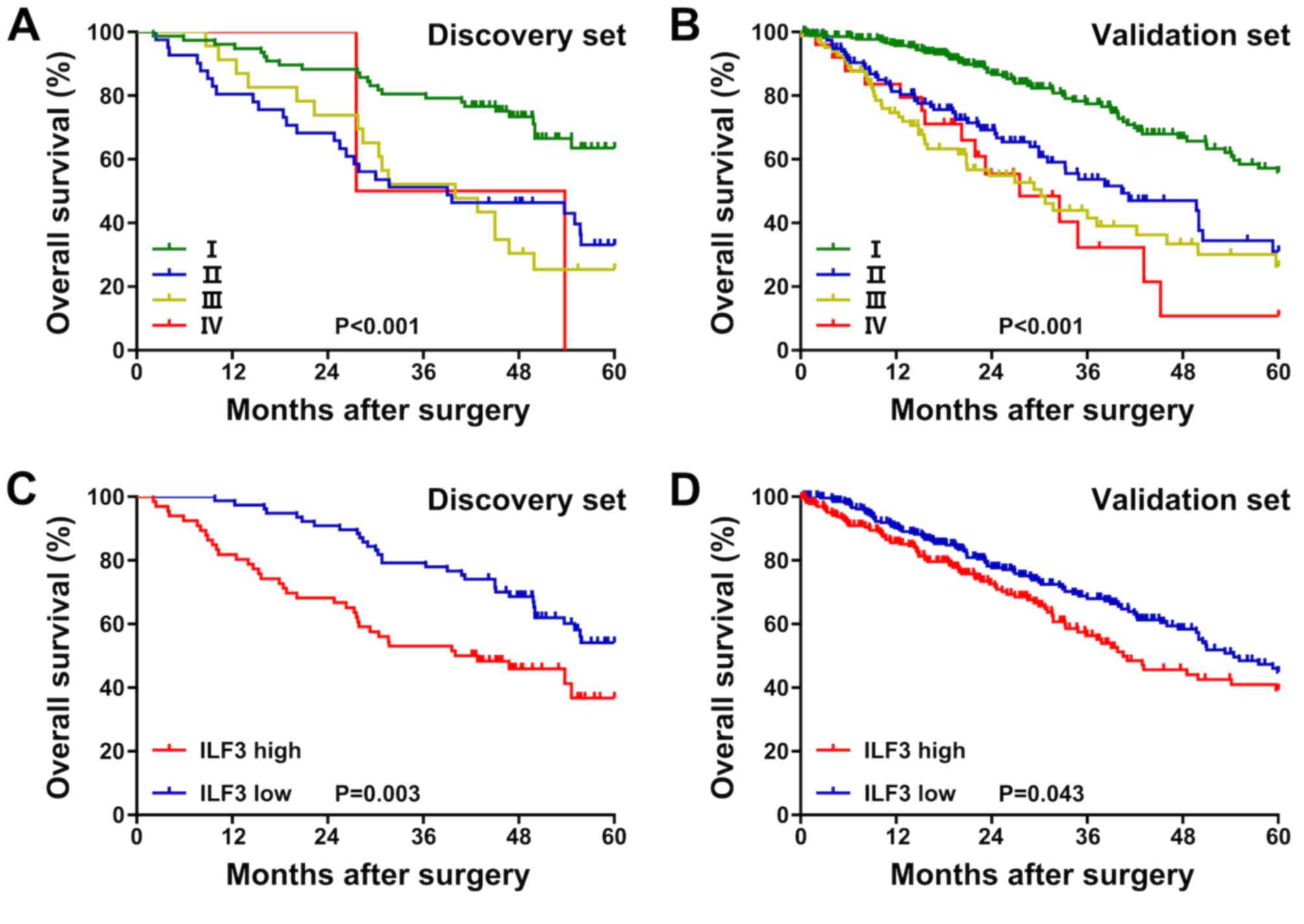
Moreover, in the discovery set, the OS time of
patients with TNM stage I was longer than that of patients with TNM
stages II–III (P<0.001; Fig. 2A).
In the validation set, the OS time of patients with TNM stage I was
longer than that of patients with TNM stages II–IV (P<0.001;
Fig. 2B). Patients with a low ILF3
expression level exhibited an increased OS time compared with
patients with high expression, both in the discovery (P=0.003;
Fig. 2C) and validation (P=0.043;
Fig. 2D) sets.
Subgroup analysis of the association
between ILF3 expression and the OS time in patients with different
TNM stages
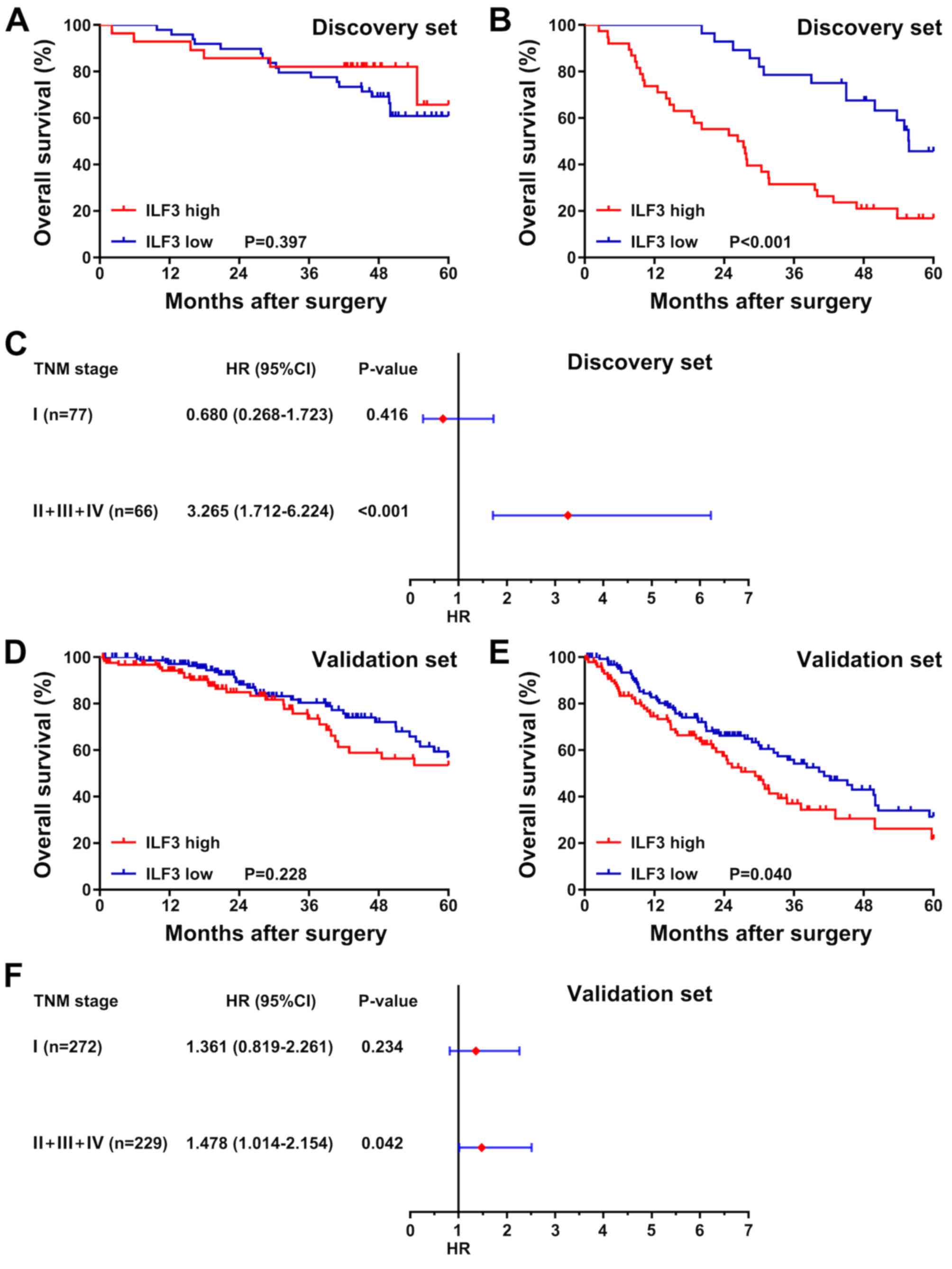
To determine whether the OS time of patients with
LUAD with different TNM stages was associated with the ILF3
expression level, the patients in the discovery and validation sets
were divided into two subgroups based on TNM stage. The first
subgroup consisted of patients with TNM stage I, and the second
subgroup consisted of patients with TNM stages II–IV. Survival
analysis was subsequently performed for each subgroup, and the
association between ILF3 expression and the OS time of patients was
presented as a forest plot based on the univariate analysis. In the
discovery set, no significant difference in survival time was
observed between patients with high or low ILF3 expression in the
TNM stage I subgroup (P=0.397; Fig.
3A). However, in the TNM stages II–IV subgroup, the OS time of
patients with high ILF3 expression was shorter than that of
patients with low ILF3 expression (P<0.001; Fig. 3B). Furthermore, the ILF3 expression
level was significantly associated with the OS time of patients in
the TNM stages II–IV subgroup (P<0.001; Fig. 3C), but not in the TNM stage I
subgroup (P=0.416).
In the validation set, as in the discovery set, ILF3
expression was not associated with the OS time of patients in the
TNM stage I subgroup (P=0.228; Fig.
3D). By contrast, in the TNM stages II–IV subgroup, patients
with low ILF3 expression had an improved OS time than those with
high ILF3 expression (P=0.040; Fig.
3E). Moreover, in the validation set, the ILF3 expression level
was significantly associated with the OS time of patients with TNM
stages II–IV (P=0.042; Fig. 3F), but
not TNM stage I (P=0.234).
Subgroup analysis of the association
between ILF3 expression and the OS time in patients with different
tumor differentiation
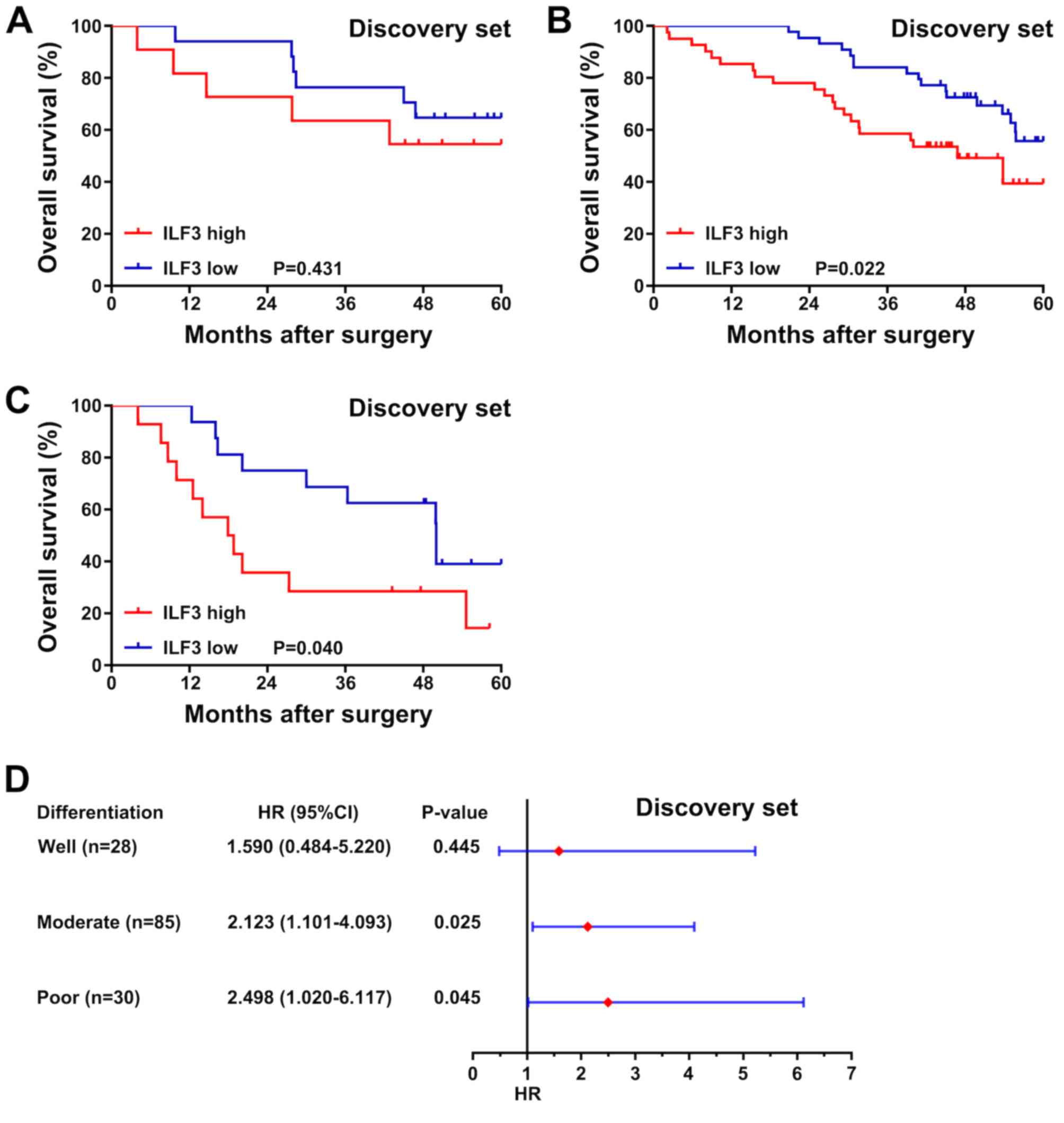
In the discovery set, no significant association
between ILF3 expression and the OS time was observed in patients
with well-differentiated tumors (P=0.431; Fig. 4A). Nevertheless, among patients with
moderately or poorly differentiated tumors, those with a low ILF3
expression level had an increased OS time compared with patients
with high expression (P=0.022 and P=0.040, respectively; Fig. 4B and C). Moreover, a forest plot
based on a univariate analysis revealed that ILF3 expression was
associated with the OS time of patients with moderate or poor tumor
differentiation (P=0.025 and P=0.045, respectively; Fig. 4D), but not with well-differentiated
tumors (P=0.445).
ILF3 expression is an independent risk
factor for patients with LUAD
The results of univariate and multivariate analyses
are presented in Table II. In the
univariate analysis, ILF3 expression (P=0.003 and P=0.044, for the
discovery and validation sets, respectively) and the TNM stage
(P<0.001, for both discovery and validation sets) were
significant risk factors for OS time. Moreover, tumor
differentiation (P=0.017) and smoking status (P=0.033) in the
discovery set and ethnicity (P=0.013) in the validation set were
identified as significant risk factors for OS time.
 | Table II.Univariate and multivariate analyses
of overall survival time in patients with lung adenocarcinoma. |
Table II.
Univariate and multivariate analyses
of overall survival time in patients with lung adenocarcinoma.
| A, Univariate
analysis |
|---|
|
|---|
|
| Discovery set | Validation set
(TCGA) |
|---|
|
|
|
|
|---|
| Variable | HR (95% CI) | P-value | HR (95% CI) | P-value |
|---|
| Age, years |
| ≥60 vs.
<60 | 0.868
(0.541–1.394) | 0.558 | 0.882
(0.627–1.240) | 0.470 |
| Sex |
| Male
vs. female | 1.437
(0.890–2.320) | 0.138 | 1.062
(0.785–1.436) | 0.697 |
| Smoking |
| Yes vs.
no/unknown | 1.765
(1.048–2.972) | 0.033a | 1.209
(0.884–1.653) | 0.236 |
| Ethnicity |
|
Caucasian vs.
non-caucasian |
|
| 1.610
(1.103–2.350) | 0.013a |
|
Differentiation |
| Poor
and moderate vs. well | 1.599
(1.087–2.350) | 0.017a |
|
|
| TNM stage |
| II, III
and IV vs. I | 1.682
(1.300–2.175) |
<0.001a | 1.648
(1.428–1.903) |
<0.001a |
| ILF3
expression |
| High vs. low | 2.050
(1.270–3.311) | 0.003a | 1.363
(1.008–1.844) | 0.044a |
|
| B, Multivariate
analysis |
|
|
| Discovery
set | Validation set
(TCGA) |
|
|
|
|
|
Variable | HR (95%
CI) | P-value | HR (95%
CI) | P-value |
|
| Smoking status |
| Yes vs.
no | 1.512
(0.893–2.561) | 0.124 |
|
|
| Ethnicity |
|
| 1.594
(1.093–2.326) | 0.016a |
|
Caucasian vs.
Non-caucasian |
|
|
|
|
|
Differentiation |
| Poor and moderate
vs. well | 1.542
(1.042–2.283) | 0.030a |
|
|
| TNM stage |
| II, III
and IV vs. I | 1.544
(1.184–2.015) | 0.001a | 1.634
(1.417–1.883) |
<0.001a |
| ILF3
expression |
| High
vs. low | 1.761
(1.075–2.885) | 0.025a | 1.376
(1.017–1.862) | 0.038a |
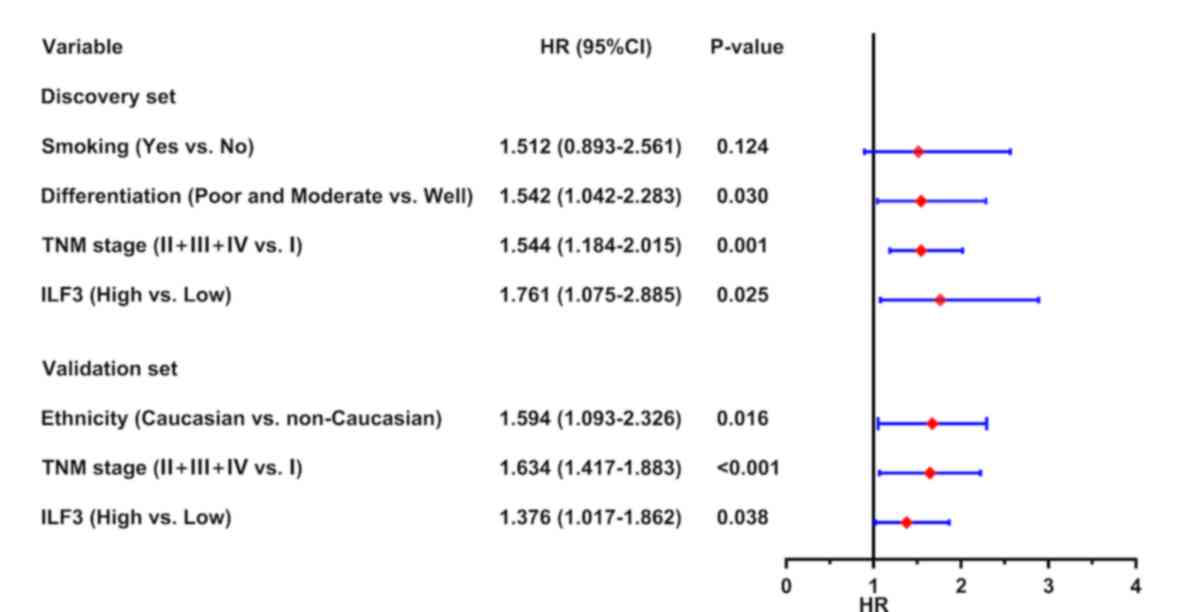
Subsequently, all the significant risk factors for
OS time identified in the univariate analysis were used for
multivariate analysis, and the results were presented as a forest
plot showing risk factors for prognosis in patients with LUAD. This
analysis revealed that ILF3 expression was an independent risk
factor for OS time in the discovery (P=0.025) and validation
(P=0.038) sets. Furthermore, the TNM stage (P=0.001 and P<0.001,
for the discovery and validation sets, respectively), tumor
differentiation (P=0.030, for the discovery set) and ethnicity
(P=0.016, for the validation set) were identified as underlying
independent risk factors for OS time in patients with LUAD
(Fig. 5).
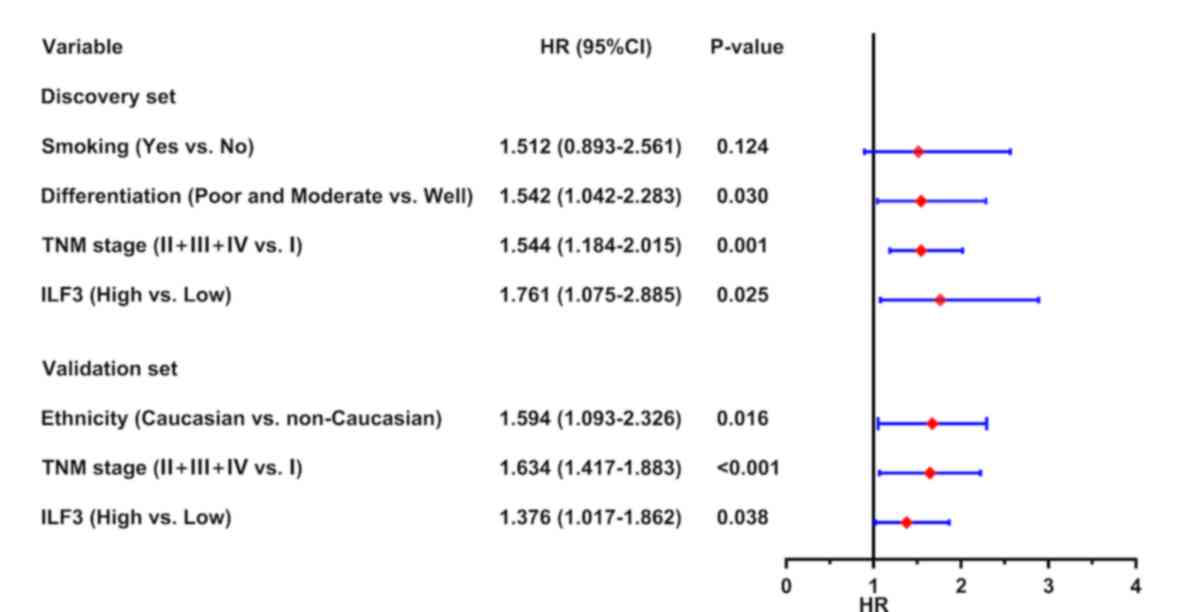 | Figure 5.Forest plot based on ILF3 expression
and other risk factors. In the discovery set, ILF3 expression
(based on immunohistochemistry), tumor differentiation and TNM
stage were identified as independent risk factors for OS time in
patients with LUAD. In the validation set, ILF3 expression (based
on the mRNA level), TNM stage and ethnicity were identified as
independent risk factors for OS time in patients with LUAD. ILF3,
interleukin-enhancer binding factor 3; TNM, tumor-node-metastasis;
OS, overall survival; LUAD, lung adenocarcinoma; HR, hazard ratio;
CI, confidence interval. |
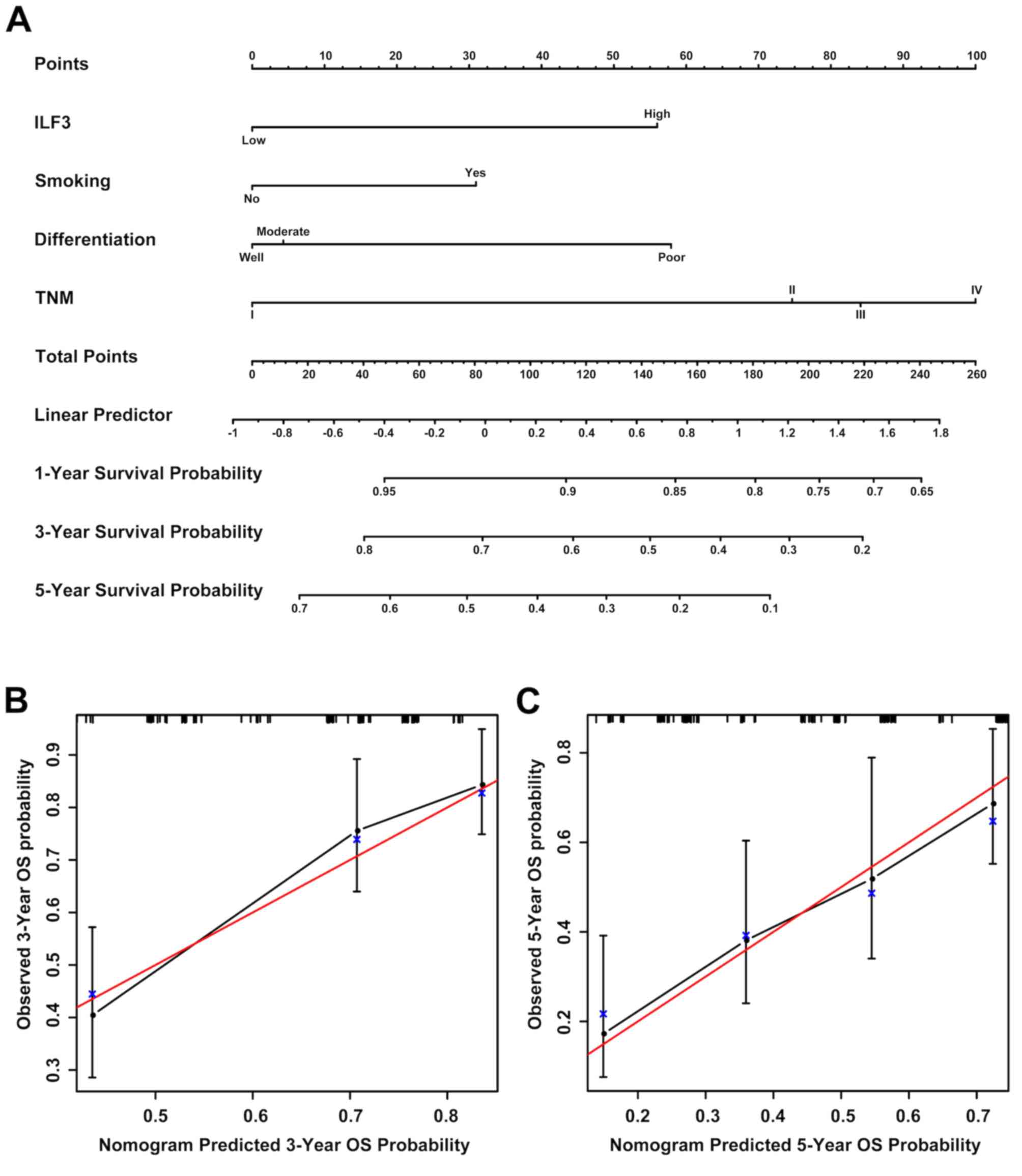
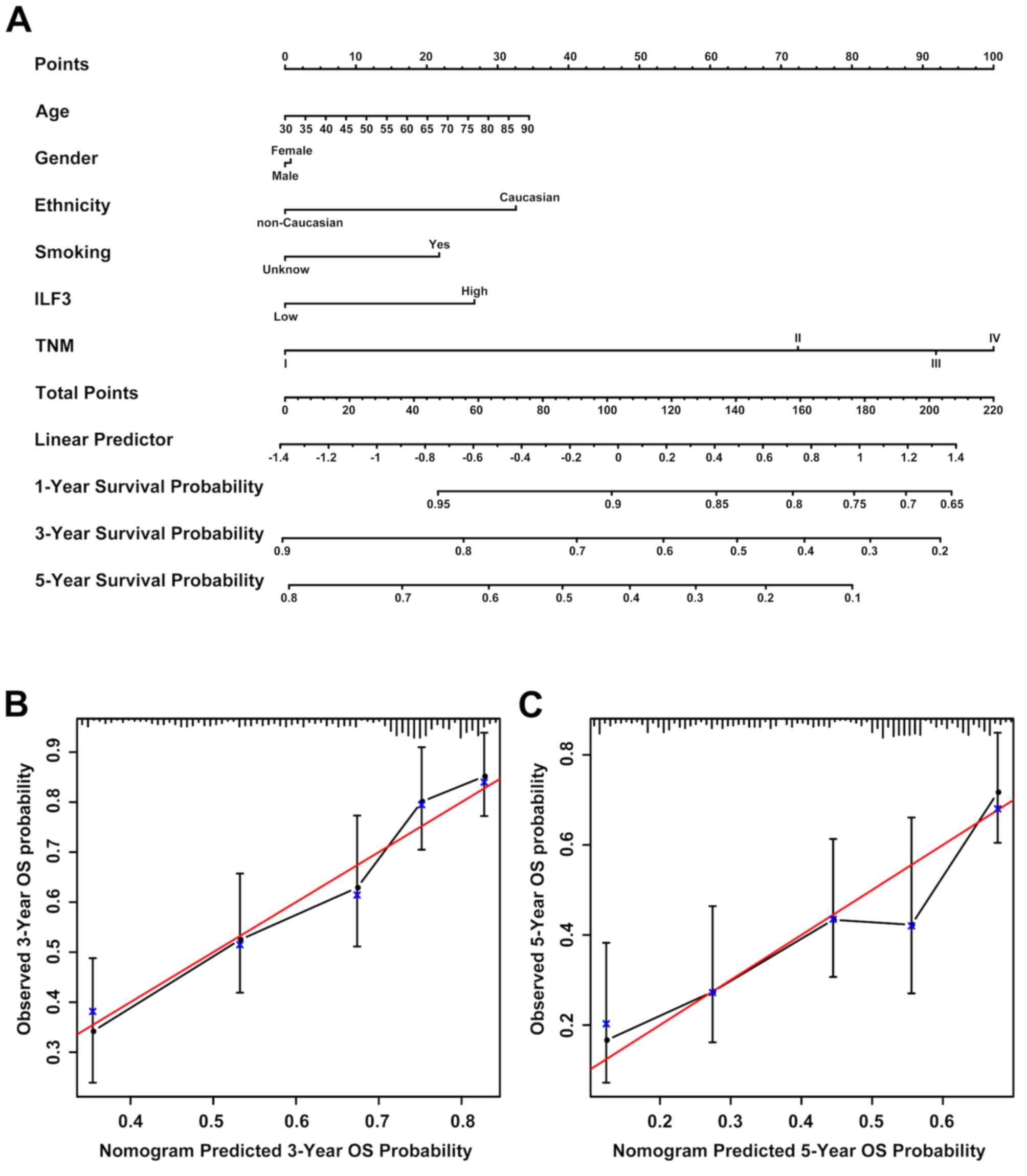
Prognostic nomograms for OS time in
patients with LUAD
Prognostic nomograms estimating the OS time of
patients with LUAD were generated for the discovery (Fig. 6A) and validation (Fig. 7A) sets based on the results obtained
in the univariate and multivariate analyses. The nomogram based on
the discovery set data integrated ILF3 expression, TNM stage, tumor
differentiation and smoking status, whereas the nomogram based on
the validation set data integrated all the risk factors, including
ILF3 expression, TNM stage, age, gender, ethnicity and smoking
status. Each patient received points based on each risk factor, and
the total number of points (i.e., the sum of the points received
for each risk factor) was used to predict the OS time. A high
number of total points were associated with advanced age, smoking,
high ILF3 expression, poor differentiation, females and the
Caucasian race. It was also associated with a high risk and poor
prognosis. The calibration curve for the probability of survival
time at 3 or 5 years revealed a strong association between the
predicted outcome from the nomogram and the actual observed outcome
for the discovery (Fig. 6B and C)
and validation (Fig. 7B and C)
sets.
The predictive accuracy of the prognostic nomograms
based on ILF3 expression was evaluated using the C-index and AIC.
The results of the comparison between the prognostic model based on
ILF3 expression and the conventional prognostic model based on the
TNM stage are presented in Table
III. For the discovery set, the C-index for the probability of
survival at 3 and 5 years was increased to 0.7045 and 0.6823,
respectively, for the model based on ILF3 expression, while the AIC
was decreased to 433.0039 and 624.1688, respectively. Similarly,
for the validation set, the C-index for the probability of survival
time at 3 and 5 years was increased to 0.6970 and 0.6909,
respectively, for the model based on ILF3 expression, while the AIC
was decreased to 1506.3810 and 1827.3640, respectively. Therefore,
the nomogram based on ILF3 expression provided an improved
predictive accuracy compared with the prognostic model based on the
TNM stage in both the discovery and validation sets.
 | Table III.Comparison of the accuracy of the
prognostic models. |
Table III.
Comparison of the accuracy of the
prognostic models.
| A, Discovery
set |
|---|
|
|---|
|
| 3-year OS time | 5-year OS time |
|---|
|
|
|
|
|---|
| Model | C-index | AIC | C-index | AIC |
|---|
| TNM | 0.6263 | 445.7592 | 0.6269 | 619.0112 |
| ILF3-based
model | 0.7045 | 443.0039 | 0.6823 | 624.1688 |
|
| B, Validation
set (TCGA) |
|
|
| 3-year OS
time | 5-year OS
time |
|
|
|
|
| Model | C-index | AIC | C-index | AIC |
|
| TNM | 0.6679 | 1506.5460 | 0.6613 | 1831.0630 |
| ILF3-based
model | 0.6970 | 1506.3810 | 0.6909 | 1827.3640 |
As presented in Fig.
S1, a decision curve analysis for the prediction of OS time was
performed. Compared with the model based on the TNM stage, a model
combining the analysis of the TNM stage and ILF3 expression
benefited patients with a survival probability of <49 or
>74%. For example, if a survival probability of 80% was used as
a threshold, the net benefit of the combined model was ~0.05, which
was greater than the net benefit of the model based on the TNM
stage (0.01).
Discussion
The ILF3 family consists of four members (NF90a,
NF90b, NF110a and NF110b), which result from the mutually exclusive
alternative splicing of the ILF3 gene transcript (25–27).
NF90 and NF110 serve important roles in the regulation of circRNA
biogenesis and the antiviral immune response (13). Furthermore, ILF3 interacts with Nanog
homeobox mRNA to regulate pluripotency in embryonic stem cells and
has potential roles in sustaining embryonic stem cell self-renewal
and cell fate determination (28).
While a previous study indicated that ILF3 expression may be a
novel risk factor for venous thromboembolism, stroke and coronary
artery disease (29), ILF3
autoantibodies have been identified as potential diagnostic
biomarkers for human autoimmune disease (30). Furthermore, ILF3 interacts with
interleukin-2 in T cells to upregulate synoviolin in rheumatoid
synovial cells and is therefore a potential therapeutic target for
rheumatoid arthritis (31). To the
best of our knowledge, the current study is the first to report
that ILF3 was an independent risk factor for OS time in patients
with LUAD.
Increasing evidence suggests that ILF3 may
contribute to the aggressiveness and progression of certain
malignant tumors, including hepatocellular carcinoma, NSCLC and
breast and ovarian cancer (14,16,32,33). In
the current study, ILF3 expression was significantly associated
with the TNM stage and OS time of patients with LUAD. Furthermore,
subgroup analyses revealed that patients with TNM stages II–IV and
poor or moderate tumor differentiation may be stratified according
to ILF3 expression. Collectively, these results suggested that ILF3
expression may significantly affect the prognosis of patients with
LUAD.
Moreover, when the conventional prognostic model
based on the TNM stage was applied to patients with LUAD, the
C-index of the discovery set was low compared with that of the
validation set. This phenomenon may be associated with differences
in the levels of economic development and medical services provided
in different regions. Nevertheless, compared with the conventional
prognostic model based on the TNM stage, the nomogram model based
on ILF3 expression exhibited improved predictive accuracy for the
OS time of patients with LUAD, in both the discovery and validation
sets.
LincIN, a novel NF90-binding long non-coding RNA, is
upregulated in advanced breast tumors and is involved in metastasis
(34). NF90 is a member of ILF3
family, and LincIN is a novel long non-coding RNA which binding
NF90. So LincIN is associated with the current study. Upregulated
expression of ILF2 in NSCLC is associated with tumor cell
proliferation and poor prognosis (35). The present study suggested that ILF3
is a potential independent adverse prognostic factor for
post-operative survival time in patients with LUAD and may be
beneficial for the postoperative hierarchical management of
patients with the disease.
Further work is required to strengthen the results
obtained in the present study. First, due to a lack of information
on disease recurrence or progression, the present study only
reported the analysis of the association between ILF3 expression
and OS time. Additional work is required to establish further
associations with disease recurrence and progression. Secondly, the
prognostic value of ILF3 expression for patients with LUAD requires
further validation in more extensive prospective multi-center
clinical trials, which may improve the reliability of the
prognostic nomogram based on ILF3 expression. Thirdly, the ILF3
expression level was not investigated in patients with suspected
LUAD and this requires further investigation. Furthermore, the
present study lacked differentiation data of patients in the
validation set, which may have affected the predictive accuracy of
the nomogram, based on ILF3. Finally, the role of ILF3 in the
development and progression of LUAD remains unclear, and further
studies are required to elucidate the underlying mechanisms.
Overall, the present study identified ILF3 as a
predictor of adverse prognosis in patients with LUAD. Furthermore,
determining the expression level of ILF3 may improve the
hierarchical post-operative management of patients with LUAD based
on the TNM stage or tumor differentiation. Moreover, the prognostic
nomogram based on ILF3 expression and other risk factors presented
a significant improvement in the predictive accuracy of the
survival time of patients with LUAD compared with the model based
on the TNM stage and may avoid excessive medical treatment for
patients with the disease.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was funded by the National Natural
Science Foundation of China (grant no. 81770266) and the ‘Six-One’
Project for High-Level Health Talents of the Jiangsu Province
(grant no. LGY2016037).
Availability of data and materials
The datasets generated and/or analyzed during the
present study are available in TCGA database (https://www.cancer.gov).
Authors' contributions
JS and HZ designed the present study. YL, JZ and ZW
acquired the data. XL, ZX, YL, JZ, ZW and HH analyzed and
interpreted the data. CJ and XJL performed statistical analysis. ZX
drafted the initial manuscript. HZ and XL revised the initial
manuscript for important intellectual content. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The current study was approved by the Clinical
Research Ethics Committee of The Affiliated Hospital of Nantong
University (Jiangsu, China) and written informed consent was
obtained from all patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ILF3
|
interleukin-enhancer binding factor
3
|
|
LUAD
|
lung adenocarcinoma
|
|
TCGA
|
The Cancer Genome Atlas
|
|
OS
|
overall survival
|
|
TNM
|
tumor-node-metastasis
|
|
NSCLC
|
non-small-cell lung cancer
|
|
circRNA
|
circular RNA
|
|
TMA
|
tissue microarray
|
|
IHC
|
immunohistochemistry
|
|
C-index
|
the Harrell's concordance index
|
|
AIC
|
Akaike information criterion
|
References
|
1
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Molina JR, Yang P, Cassivi SD, Schild SE
and Adjei AA: Non-Small cell lung cancer: Epidemiology, risk
factors, treatment, and survivorship. Mayo Clin Proc. 83:584–594.
2008. View
Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yao S, Zhong L, Liu J, Feng J, Bian T,
Zhang Q, Chen J, Lv X, Chen J and Liu Y: Prognostic value of
decreased GRK6 expression in lung adenocarcinoma. J Cancer Res Clin
Oncol. 142:2541–2549. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chang JT, Lee YM and Huang RS: The impact
of the cancer genome atlas on lung cancer. Transl Res. 166:568–585.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Minguet J, Smith KH and Bramlage P:
Targeted therapies for treatment of non-small cell lung
cancer-recent advances and future perspectives. Int J Cancer.
138:2549–2561. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Castella S, Bernard R, Corno M, Fradin A
and Larcher JC: Ilf3 and NF90 functions in RNA biology. Wiley
Interdiscip Rev RNA. 6:243–256. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Xu YH, Leonova T and Grabowski GA: Cell
cycle dependent intracellular distribution of two spliced isoforms
of TCP/ILF3 proteins. Mol Genet Metab. 80:426–436. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhuang J, Shen L, Yang L, Huang X, Lu Q,
Cui Y, Zheng X, Zhao X, Zhang D, Huang R, et al: TGFβ1 promotes
gemcitabine resistance through regulating the
LncRNA-LET/NF90/miR-145 signaling axis in bladder cancer.
Theranostics. 7:3053–3067. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Larcher JC, Gasmi L, Viranaicken W, Edde
B, Bernard R, Ginzburg I and Denoulet P: Ilf3 and NF90 associate
with the axonal targeting element of tau mRNA. FASEB J.
18:1761–1763. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pei Y, Zhu P, Dang Y, Wu J, Yang X, Wan B,
Liu JO, Yi Q and Yu L: Nuclear export of NF90 to stabilize IL-2
mRNA is mediated by AKT-dependent phosphorylation at Ser647 in
response to CD28 costimulation. J Immunol. 180:222–229. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shi L, Zhao G, Qiu D, Godfrey WR, Vogel H,
Rando TA, Hu H and Kao PN: NF90 regulates cell cycle exit and
terminal myogenic differentiation by direct binding to the
3′-untranslated region of MyoD and p21WAF1/CIP1 mRNAs. J Biol Chem.
280:18981–18989. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li X, Liu CX, Xue W, Zhang Y, Jiang S, Yin
QF, Wei J, Yao RW, Yang L and Chen LL: Coordinated circRNA
biogenesis and function with NF90/NF110 in viral infection. Mol
Cell. 67:214–227. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hu Q, Lu YY, Noh H, Hong S, Dong Z, Ding
HF, Su SB and Huang S: Interleukin enhancer-binding factor 3
promotes breast tumor progression by regulating sustained
urokinase-type plasminogen activator expression. Oncogene.
32:3933–3943. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhang Y, Yang C, Zhang M, Liu H, Gong C,
Zhang J, Xu S, Zou J, Kai Y and Li Y: Interleukin enhancer-binding
factor 3 and HOXC8 co-activate cadherin 11 transcription to promote
breast cancer cells proliferation and migration. Oncotarget.
8:107477–107491. 2017.PubMed/NCBI
|
|
16
|
Guo Y, Fu P, Zhu H, Reed E, Remick SC,
Petros W, Mueller MD and Yu JJ: Correlations among ERCC1, XPB,
UBE2I, EGF, TAL2 and ILF3 revealed by gene signatures of
histological subtypes of patients with epithelial ovarian cancer.
Oncol Rep. 27:286–292. 2012.PubMed/NCBI
|
|
17
|
Zhu H and Yu JJ: Gene expression patterns
in the histopathological classification of epithelial ovarian
cancer. Exp Ther Med. 1:187–192. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cheng CC, Chou KF, Wu CW, Su NW, Peng CL,
Su YW, Chang J, Ho AS, Lin HC, Chen CG, et al: EGFR-mediated
interleukin enhancer-binding factor 3 contributes to formation and
survival of cancer stem-like tumorspheres as a therapeutic target
against EGFR-positive non-small cell lung cancer. Lung Cancer.
116:80–89. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Detterbeck FC, Chansky K, Groome P,
Bolejack V, Crowley J, Shemanski L, Kennedy C, Krasnik M, Peake M,
Rami-Porta R, et al: The IASLC lung cancer staging project:
Methodology and validation used in the development of proposals for
revision of the stage classification of NSCLC in the forthcoming
(Eighth) edition of the TNM classification of lung cancer. J Thorac
Oncol. 11:1433–1446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tomczak K, Czerwinska P and Wiznerowicz M:
The cancer genome atlas (TCGA): An immeasurable source of
knowledge. Contemp Oncol (Pozn). 19:A68–A77. 2015.PubMed/NCBI
|
|
21
|
Liu K, Wang S, Liu Y, Gu J, Gu S, Xu Z,
Zhang R, Wang Z, Ma H, Chen Y and Ji L: Overexpression of MYCN
promotes proliferation of non-small cell lung cancer. Tumour Biol.
37:12855–12866. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ji L, Li H, Gao P, Shang G, Zhang DD,
Zhang N and Jiang T: Nrf2 pathway regulates
multidrug-resistance-associated protein 1 in small cell lung
cancer. PLoS One. 8:e634042013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Camp RL, Dolled-Filhart M and Rimm DL:
X-tile: A new bio-informatics tool for biomarker assessment and
outcome-based cut-point optimization. Clin Cancer Res.
10:7252–7259. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Weiss A, Chavez-MacGregor M, Lichtensztajn
DY, Yi M, Tadros A, Hortobagyi GN, Giordano SH, Hunt KK and
Mittendorf EA: Validation study of the American joint committee on
cancer eighth edition prognostic stage compared with the anatomic
stage in breast cancer. JAMA Oncol. 4:203–209. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Duchange N, Pidoux J, Camus E and Sauvaget
D: Alternative splicing in the human interleukin enhancer binding
factor 3 (ILF3) gene. Gene. 261:345–353. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Reichman TW, Parrott AM, Fierro-Monti I,
Caron DJ, Kao PN, Lee CG, Li H and Mathews MB: Selective regulation
of gene expression by nuclear factor 110, a member of the NF90
family of double-stranded RNA-binding proteins. J Mol Biol.
332:85–98. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chaumet A, Castella S, Gasmi L, Fradin A,
Clodic G, Bolbach G, Poulhe R, Denoulet P and Larcher JC: Proteomic
analysis of interleukin enhancer binding factor 3 (Ilf3) and
nuclear factor 90 (NF90) interactome. Biochimie. 95:1146–1157.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Guo C, Xue Y, Yang G, Yin S, Shi W, Cheng
Y, Yan X, Fan S, Zhang H and Zeng F: Nanog RNA-binding proteins
YBX1 and ILF3 affect pluripotency of embryonic stem cells. Cell
Biol Int. 40:847–860. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hinds DA, Buil A, Ziemek D, Martinez-Perez
A, Malik R, Folkersen L, Germain M, Malarstig A, Brown A, Soria JM,
et al: Genome-Wide association analysis of self-reported events in
6135 individuals and 252 827 controls identifies 8 loci associated
with thrombosis. Hum Mol Genet. 25:1867–1874. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Bremer HD, Landegren N, Sjoberg R,
Hallgren A, Renneker S, Lattwein E, Leonard D, Eloranta ML,
Ronnblom L, Nordmark G, et al: ILF2 and ILF3 are autoantigens in
canine systemic autoimmune disease. Sci Rep. 8:48522018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Izumi T, Fujii R, Izumi T, Nakazawa M,
Yagishita N, Tsuchimochi K, Yamano Y, Sato T, Fujita H, Aratani S,
et al: Activation of synoviolin promoter in rheumatoid synovial
cells by a novel transcription complex of interleukin enhancer
binding factor 3 and GA binding protein alpha. Arthritis Rheum.
60:63–72. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jiang W, Huang H, Ding L, Zhu P, Saiyin H,
Ji G, Zuo J, Han D, Pan Y, Ding D, et al: Regulation of cell cycle
of hepatocellular carcinoma by NF90 through modulation of cyclin E1
mRNA stability. Oncogene. 34:4460–4470. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Guo NL, Wan YW, Tosun K, Lin H, Msiska Z,
Flynn DC, Remick SC, Vallyathan V, Dowlati A, Shi X, et al:
Confirmation of gene expression-based prediction of survival in
non-small cell lung cancer. Clin Cancer Res. 14:8213–8220. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Jiang Z, Slater CM, Zhou Y, Devarajan K,
Ruth KJ, Li Y, Cai KQ, Daly M and Chen X: LincIN, a novel
NF90-binding long non-coding RNA, is overexpressed in advanced
breast tumors and involved in metastasis. Breast Cancer Res.
19:622017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ni T, Mao G, Xue Q, Liu Y, Chen B, Cui X,
Lv L, Jia L, Wang Y and Ji L: Upregulated expression of ILF2 in
non-small cell lung cancer is associated with tumor cell
proliferation and poor prognosis. J Mol Histol. 46:325–335. 2015.
View Article : Google Scholar : PubMed/NCBI
|