Introduction
Thymomas are rare malignant tumors arising from
thymic epithelial cells (TEC). According to the current WHO
classification based on morphology of the tumors, thymomas are
divided into two groups (1). Type A
thymomas represent indolent tumors with slow growth and favorable
clinical course, comprised of spindle or oval epithelial cells with
a little or no admixture of non-neoplastic mature T lymphocytes.
Type B thymomas are subdivided into three entities with different
proportion of non-neoplastic immature T lymphocytes to neoplastic
TEC-type B1 (abundance of T cells), type B2, and type B3 (rich in
epithelial cells). Type B thymomas possess higher malignant
potential rising from type B1 up to type B3. In some cases, more
than one neoplastic component is present leading to a mixed
designation as thymoma type AB comprising both type A and type B
components or thymoma comprising two subtypes of type B.
The molecular pathogenesis of these rare tumors
remains widely unknown and only a couple of molecular events have
been related to tumor biology of thymomas so far (2–4).
Recently, Liang et al (5)
showed that induced overexpression of β-catenin in TEC of murine
models leads to higher incidence of thymomas exhibiting
histological and molecular characteristics of human B3 thymomas.
Additionally, this study identified upregulation of multiple
Wnt/β-catenin-targeted genes corroborating causality of this
pathway in the tumor development.
Since there is no data investigating the involvement
of Wnt signaling pathway in pathogenesis of human thymomas, we
analyzed the expression of molecules β-catenin, cyclin D1, c-myc,
and axin2, and of molecule E-cadherin in thymomas, and studied the
potential role of their detection for thymoma diagnosis and its
clinical relevance.
Materials and methods
Patient characteristics
A total of 112 thymoma cases (58 female and 54 male
patients) and 8 control subjects entered into our study.
The thymoma group consisted of 15 patients with
thymoma type A and 97 patients with thymoma type B undergoing
surgical resection of anterior mediastinal tumor at the Third
Department of Surgery, Motol University Hospital (Prague, Czech
Republic) between January 2008 and July 2017. Mean age was 54.3
years (range 22–86 years). Medical records of each patient were
reviewed in detail and the following features were recorded:
Gender, age at the time of surgery, size of tumor, presence of
myasthenia gravis (MG) or other autoimmune disorders, as well as
synchronous malignant neoplasms at the time of first presentation.
Since the age over 60 has been previously shown as a significant
prognostic factor in malignancies of hematopoietic system (6,7), we also
divided our group of patients according to their age to evaluate
potential age-specific features of the disease. All patients were
treated according to current guidelines for treatment of thymomas
(8) at the Department of Oncology,
General University Hospital (Prague, Czech Republic), and follow-up
data were retrieved from their files. Detailed clinical
characteristics of patients enrolled into the study are given in
Table I.
 | Table I.Detailed clinical characteristics of
patients with thymoma enrolled in the present study. |
Table I.
Detailed clinical characteristics of
patients with thymoma enrolled in the present study.
|
|
|
|
| Masaoka-Koga
stage |
|
|
|
|
|---|
|
|
|
|
|
|
|
|
|
|
|---|
| WHO type | Patients, n | F/M, n | Age, years | I | II | III | IV | MG, n (%) | Other AID, n
(%) | Recurrence, n
(%) | Synchronous
malignancy, n (%) |
|---|
| Type A | 15 | 5/10 | 55.3±13.1 | 13 | 2 | 0 | 0 | 11 (73) | 0 | 0 | 3 (20) |
| Type B1 | 19 | 9/10 | 52.2±15.0 | 11 | 4 | 4 | 0 | 13 (68) | 1 (5) | 0 | 0 |
| Type B2 | 41 | 26/15 | 56.9±14.0 | 13 | 18 | 2 | 8 | 26 (63) | 3 (7) | 5 (12) | 3 (7) |
| Type B3 | 37 | 14/23 | 52.1±14.1 | 4 | 17 | 11 | 6 | 19 (51) | 5 (14) | 4 (10) | 4 (11) |
| Total | 112 | 54/58 | 54.3±14.2 | 41 | 39 | 16 | 14 | 69 (62) | 9 (8) | 9 (8) | 10 (9) |
Since the thymus undergoes physiologically
involution during late childhood (9), the control thymic tissue for our study
was obtained from pediatric patients during cardiac surgery at the
Children's Heart Centre, Motol University Hospital; the control
group of non-neoplastic thymic tissue was retrieved from 2 female
patients and 6 male patients. Mean age was 1.5 years (range 1–3
years).
Written informed consent from each patient/guardian
was obtained prior to the enrollment, and the study was approved by
the Ethics committee of the Second Faculty of Medicine, Charles
University.
Histopathology and staging
All surgical pathology analyzes were performed at
the Department of Pathology and Molecular Medicine, Motol
University Hospital (Prague, Czech Republic). Resected tissues were
routinely fixed in 10% formalin and embedded in paraffin. Each
thymic tumor as well as the control thymic tissue were examined in
several tissue blocks; the most appropriate tissue block (e.g. with
the invasive component of the tumors) was used for further studies
in each case. From the tissue blocks, 4 µm sections were examined
microscopically (microscope BX51; Olympus) by routine
hematoxylin-eosin staining to ensure the quality and the relevance
of the harvested tissue. Further serial tissue sections were used
for immunohistochemistry and for the RNA isolation.
The resected specimens were reviewed to establish
the type of thymoma according to the actual WHO classification of
thymic tumors including the invasivity of tumors according to the
modified Masaoka-Koga clinical staging of thymomas (10). In 12 cases (11%), the tumor contained
both type B2 and B3 component; the sample entered the group
according to the predominant component in the tissue block. No
thymic carcinomas as well as micronodular thymomas or type AB
thymomas were enrolled into the study.
Immunohistochemistry
Each case of thymoma was evaluated
immunohistochemically. For immunohistochemical purposes, 4 µm thick
serial sections were recut from the tissue block. Tissue sections
were deparaffinized and rehydrated. Heat-induced epitope retrieval
was performed in sodium citrate buffer solution (pH 6.0) warming up
to 96°C in water bath for 40 min. Following cooling for 20 min and
blocking of endogenous peroxidase activity, sections were incubated
overnight at 4°C with mouse monoclonal antibody against β-catenin
(clone 14/β-catenin, BD Biosciences), diluted 1:1,500, and
E-cadherin (NCL-L-E-Cad; Novocastra Laboratories Ltd.), diluted
1:60. The antigen-antibody complexes were visualized by
biotin-streptavidin detection systems (N-Histofine Simple Stain MAX
PO; Nichirei Corporation); chromogenic development was performed
using 3,3-diaminobenzidine. All sections were counterstained
slightly with Harris' hematoxylin. Positive and negative controls
were used in each assay.
The results of immunohistochemical assays for both
molecules were evaluated in tumors and in controls considering
their localization (membranous, cytoplasmic or nuclear), as well as
intensity. The expression of the molecules was noted both in the
center of the tumor mass and in its periphery, especially in case
of invasive tumors.
Quantitative mRNA expression
analysis
RNA extraction and preparation of
complementary DNA (cDNA) by reverse transcription
Total RNA was isolated from paraffin sections of the
samples using extraction with High Pure RNA Paraffin kit (Roche
Diagnostic) according to the manufacturer's instructions. The
complementary DNA (cDNA) was synthesized using MMLV Reverse
Transcriptase (Invitrogen) from 10 µl total mRNA in a volume of 20
µl. The reaction mixture contained Tris-HCl 50 mM, pH 8.3; KCl 75
mM; MgCl2 3 mM; dithiothreitol 10 mM; dNTP 0.5 mM each;
random hexamers 12.5 mM and 50 units of MMLV Reverse Transcriptase
according to the manufacturer's instructions. Reverse transcription
included an incubation period of 60 min at 37°C.
Reverse transcription-quantitative PCR
(RT-qPCR)
RT-qPCR analyses were performed using
LightCycler® 480 Instrument II (Roche Diagnostics).
RT-qPCR for housekeeping gene B2M (β2-microglobulin) using
the hydrolyzation probe was utilized to evaluate the amount and
amplifiability of cDNA. The primers for B2M were designed as
reported by Bijwaard et al (11) and are given in Table II. Relative mRNA expressions of
CTNNB1 (β-catenin), CCND1 (cyclin D1), MYC
(c-myc), AXIN2 (axin2), and CDH1 (E-cadherin) were
evaluated by RT-qPCR using TaqMan Master Mix II and primers and
probes of TaqMan Assays (Applied Biosystems), as outlined by the
manufacturer's instructions. TaqMan Assays used in this study are
given in Table III. All analyses
were performed in duplicates and the mean values were taken for
further calculations.
 | Table II.Primers and probes used in the
present study. |
Table II.
Primers and probes used in the
present study.
| Target | Primers and probes
(5′-3′) or TaqMan Assays |
|---|
|
β2-microglobulin | Forward:
TGACTTTGTCACAGCCCAAGATA |
|
| Reverse:
AATCCAAATGCGGCATCTTC |
|
| Probe:
TGATGCTGCTTACATGTCTCGATCCCA |
 | Table III.TaqMan Assays used in the present
study. |
Table III.
TaqMan Assays used in the present
study.
| Molecule
(gene) | Assay ID |
|---|
| β-catenin
(CTNNB1) | Hs00355049_m1 |
| C-myc
(MYC) | Hs00153408_m1 |
| Cyclin D1
(CCND1) | Hs00765553_m1 |
| Axin2
(AXIN2) | Hs00610344_m1 |
| E-cadherin
(CDH1) | Hs01023894_m1 |
Evaluation of RT-qPCR results
The mRNA expressions of CTNNB1, CCND1, MYC,
AXIN2, and CDH1 were calculated using the relative
quantification, i.e. the ∆∆Cq methods, based on the expression
levels of a target gene versus the reference housekeeping gene
B2M (12). In brief,
fluorescence was detected continually after each cycle of PCR
reaction. Data were analyzed with the use of the
LightCycler® 480 Software, version 1.5 (Roche
Diagnostics). The software determines a threshold line based on the
baseline fluorescent signal, and the cycle where the fluorescent
signal crosses the threshold is recorded as the Cq value, which is
inversely proportional to the starting number of template copies.
The average Cq value for B2M was subtracted from the average
of Cq value of the gene of interest to yield the ΔCq value, which
is inversely proportional to the relative amount of target nucleic
acid in the sample. Next, the ΔCq value of the control sample was
subtracted from the ΔCq value of the studied sample to yield the
ΔΔCq value. The relative fold gene expression value level
[2−(ΔΔCq)] was subsequently obtained from the ΔΔCq
value.
Statistical analysis
Results are presented as means ± standard deviation
(SD). Differences of frequencies between specific categories were
tested via the Pearson's chi-squared test. Differences between the
numeric variables of the multiple groups of relative mRNA
expressions were tested by ANOVA followed by Tukey's post hoc test.
Other differences between the numeric variables of two subgroups of
thymomas were tested with Student's t-test. The analytical work was
performed using JMP IN 5.1 software (SAS Institute). P<0.05 was
considered to indicate a statistically significant difference.
Results
Clinical features
The clinical data of the studied group of 112
patients with thymomas is summarized in Table I. Thymomas of non-MG patients showed
significantly higher proportion of invasive tumors (n=34; 79%) than
those with MG (n=37; 54%; P=0.011). Autoimmune disorders other than
MG were present in 9 (8%) type B thymoma patients, representing
autoimmune thyroiditis in 7 cases, and autoimmune atrophic
gastritis and stiff man syndrome each in one case. A synchronous
malignant neoplasm at the time of diagnosis was present in 10
patients (9%) both with type A and type B thymomas; the spectrum of
concomitant malignant neoplasms was broad including melanoma,
colorectal and prostatic carcinoma, carcinomas of bladder, thyroid,
breast, and kidney. Type A thymomas were not significantly
different in size (mean 4.5±1.5 cm) than type B thymomas (5.0±2.9
cm; P=0.178). Thymic tumors of non-MG patients (5.6±3.5 cm) were
significantly larger than those with MG (4.5±2.1 cm; P=0.049) at
the time of primary surgery.
The age specific characteristics of the studied
group of patients with thymomas are given in Table IV. There were no significant
differences in frequency of specific WHO subtypes of thymomas as
well as in size of tumors between younger and older patients (data
not shown). MG positive patients were significantly younger at the
time of diagnosis of thymoma (n=69; 52.5±14.5 years) than the
non-MG patients (n=43; 57.0±13.4 years; P=0.047). We have detected
a higher proportion of invasive thymomas, as well as higher
recurrence rate and presence of synchronous malignancies in the age
group over 60 years compared to younger patients.
 | Table IV.Age specific characteristics of
patients with thymoma enrolled in the present study. |
Table IV.
Age specific characteristics of
patients with thymoma enrolled in the present study.
| Age, years | Patients, n | Invasive, n
(%) | MG, n (%) | Other AID, n
(%) | Recurrences, n
(%) | Synchronous
malignancy, n (%) |
|---|
| <60 | 65 | 39 (60) | 45 (69) | 4 (6) | 4 (6) | 3 (5) |
| >60 | 47 | 32 (68) | 24 (51) | 5 (11) | 5 (11) | 7 (15) |
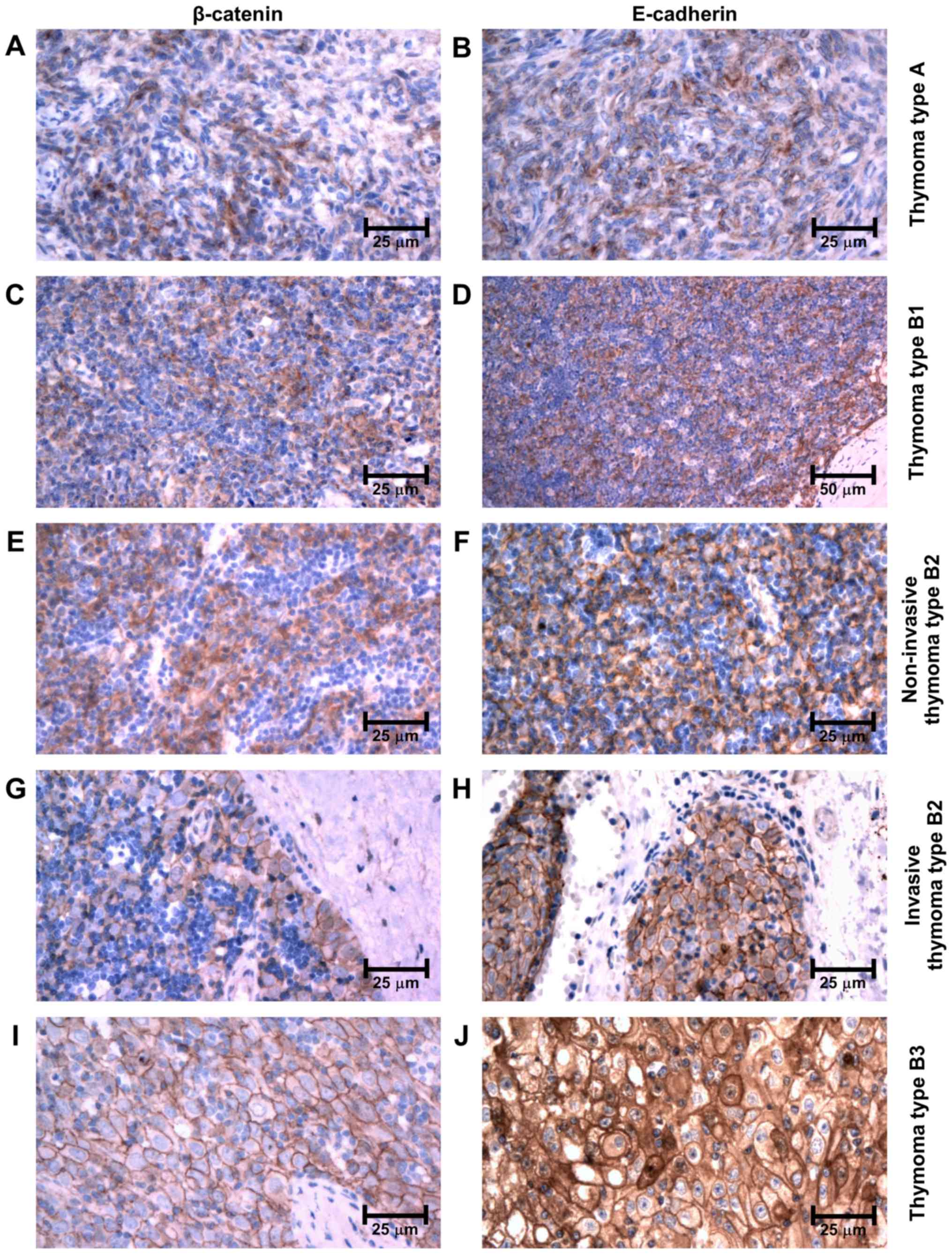
Immunoexpression of β-catenin and
E-cadherin
Immunohistochemically, β-catenin and E-cadherin were
both expressed in epithelial cells of all subtypes of thymomas as
well as in TEC in controls. However, its intracellular localization
and intensity varied among the subgroups. Both molecules retained
the same pattern of distribution in neoplastic tissues as well as
in controls. In type A thymomas, the immunoexpression was observed
only in the cytoplasm of neoplastic cells (Fig. 1A and B). In thymomas type B, the
intensity of immunolabeling increased, being only cytoplasmic in
type B1 and in non-invasive regions of type B2 (Fig. 1C-F). However, it was membranous
throughout the neoplastic tissue in type B3 thymomas, and in the
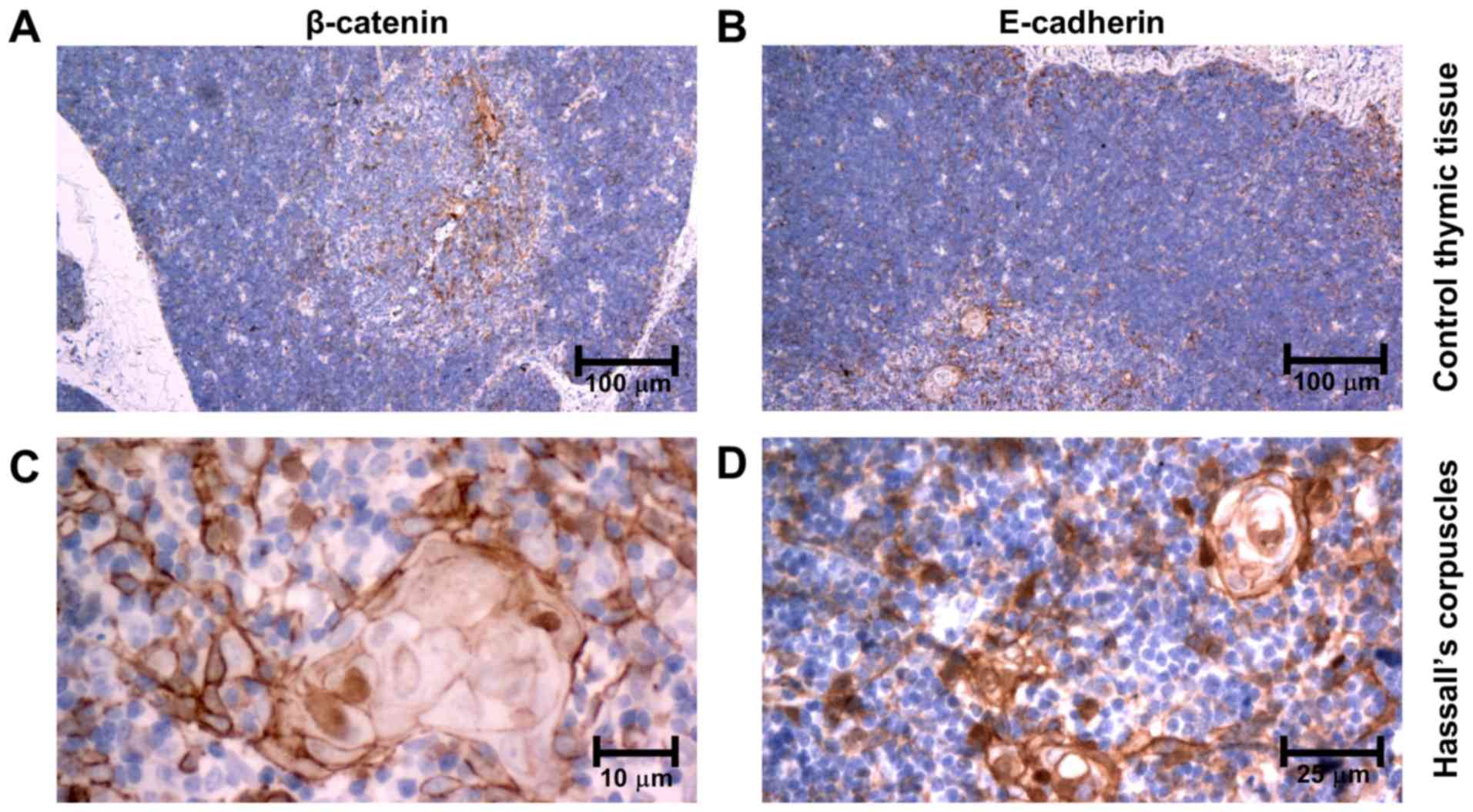
invasive front at the periphery of type B2 thymomas (Fig. 1G-J). In controls, only weak β-catenin
and E-cadherin expression was observed in the cytoplasm of
medullary TEC and on membranes of cortical TEC (Fig. 2A and B). No nuclear immunopositivity
of β-catenin was observed in tumor cells. Of note, an intense
membranous and nuclear positivity was revealed in TEC of Hassall's
corpuscles (Fig. 2C and D).
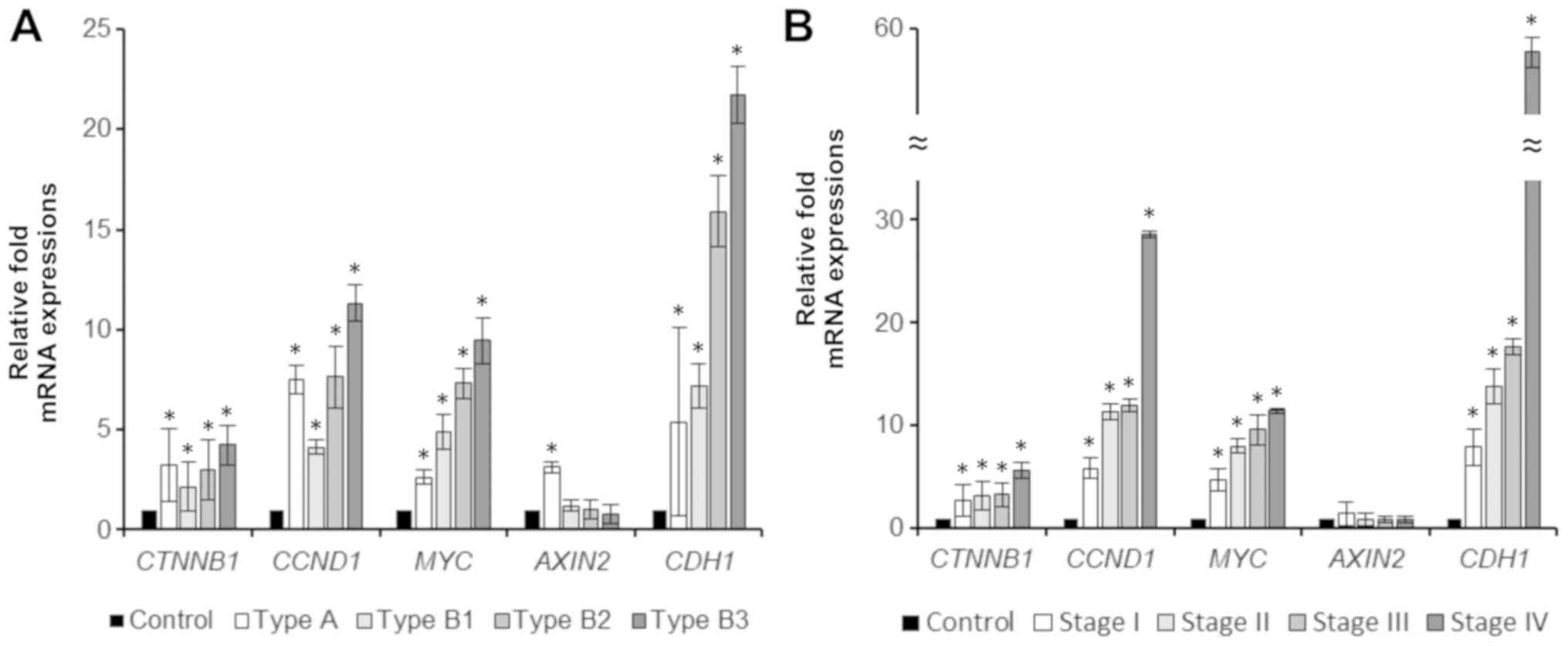
Relative mRNA expression of molecules
involved in the Wnt pathway and E-cadherin
mRNA expression according to the
histological subtype
Relative mRNA expression of molecules involved in
Wnt pathway (β-catenin-gene CTNNB1, cyclin D1-gene
CCND1, c-myc-gene MYC, axin2-gene AXIN2) and
E-cadherin (gene CDH1) according to the WHO histological
subtype is summarized in Table V and
Fig. 3A. Expression of all molecules
was significantly increased in thymomas when compared to controls,
except for the expression of axin2 in thymomas type B; the mRNA
expression increased gradually from type B1 to type B3 thymoma.
Only in thymomas type A, mRNA expression of axin2 was significantly
increased.
 | Table V.Relative fold mRNA expression value
level (2−ΔΔCq) of molecules involved in the Wnt
signaling pathway and E-cadherin based on the expression levels of
the target gene vs. the reference housekeeping gene B2M in
thymoma and control thymic tissue. |
Table V.
Relative fold mRNA expression value
level (2−ΔΔCq) of molecules involved in the Wnt
signaling pathway and E-cadherin based on the expression levels of
the target gene vs. the reference housekeeping gene B2M in
thymoma and control thymic tissue.
| A, WHO type |
|---|
|
|---|
|
|
| CTNNB1 | CCND1 | MYC | AXIN2 | CDH1 |
|---|
|
|
|
|
|
|
|
|
|---|
| Type | n | Value | P-value | Value | P-value | Value | P-value | Value | P-value | Value | P-value |
|---|
| A | 15 | 3.25±1.81 | 0.012a | 7.52±0.73 | 0.007a | 2.64±0.32 | 0.041a | 3.12±0.27 | 0.020a | 5.39±4.70 | 0.047a |
| B1 | 19 | 2.16±1.23 | 0.008a | 4.11±0.36 | 0.002a | 4.92±0.88 | 0.007a | 1.21±0.30 | 0.354 | 7.16±1.10 | 0.003a |
| B2 | 41 | 3.01±1.52 | 0.001a | 7.62±1.53 | 0.008a | 7.31±0.74 | 0.005a | 1.03±0.45 | 0.488 | 15.89±1.77 | 0.001a |
| B3 | 37 | 4.23±0.98 | 0.001a | 11.31±0.90 | 0.001a | 9.45±1.15 | 0.001a | 0.78±0.50 | 0.322 | 21.71±1.39 | 0.001a |
|
| B,
Stage |
|
|
|
|
CTNNB1 |
CCND1 |
MYC |
AXIN2 |
CDH1 |
|
|
|
|
|
|
|
|
| Stage | n | Value | P-value | Value | P-value | Value | P-value | Value | P-value | Value | P-value |
|
| I | 41 | 2.69±1.55 | 0.001a | 5.86±0.98 | 0.001a | 4.69±1.06 | 0.001a | 1.39±1.21 | 0.322 | 7.89±1.80 | 0.001a |
| II | 40 | 3.10±1.39 | 0.001a | 11.31±0.78 | 0.001a | 8.00±0.69 | 0.004a | 0.82±0.61 | 0.369 | 13.83±1.67 | 0.008a |
| III | 17 | 3.25±1.15 | 0.001a | 11.96±0.61 | 0.001a | 9.58±1.47 | 0.003a | 0.85±0.36 | 0.381 | 17.63±0.80 | 0.002a |
| IV | 14 | 5.66±0.77 | 0.001a | 28.64±0.31 | 0.003a | 11.47±0.24 | 0.004a | 0.82±0.32 | 0.354 | 57.68±1.46 | 0.001a |
mRNA expression according to the
Masaoka-Koga stage
Comparison of mRNA expression of the studied
molecules in invasive versus non-invasive tumors is given in
Table VI; the mRNA expression
according to Masaoka-Koga stage of thymomas is summarized in
Table V and Fig. 3B. Expression of mRNA of all studied
molecules except for axin2 was increased in invasive thymomas,
although the statistical significance was reached only for mRNA
expression of cyclin D1, c-myc, and E-cadherin. mRNA expression of
axin2 was not significantly different between invasive and
non-invasive tumors. However, expression of mRNA of axin2 differed
within the subgroup of non-invasive tumors-it was significantly
increased in non-invasive thymomas type A when compared to controls
[2−(ΔΔCq)=3.12±0.27; P=0.020], as well as to
non-invasive thymomas type B [2−(ΔΔCq)=3.58±1.02;
P=0.002].
 | Table VI.Relative fold mRNA expression value
level (2−ΔΔCq) of molecules involved in the Wnt
signaling pathway and E-cadherin based on the expression levels of
the target gene vs. the reference housekeeping gene B2M
between specific subgroups of thymomas. |
Table VI.
Relative fold mRNA expression value
level (2−ΔΔCq) of molecules involved in the Wnt
signaling pathway and E-cadherin based on the expression levels of
the target gene vs. the reference housekeeping gene B2M
between specific subgroups of thymomas.
|
|
| CTNNB1 | CCND1 | MYC | AXIN2 | CDH1 |
|---|
|
|
|
|
|
|
|
|
|---|
| Subgroups | n | Value | P-value | Value | P-value | Value | P-value | Value | P-value | Value | P-value |
|---|
| Invasivity,
Inv./Non-inv. | 71/41 | 1.28±0.30 | 0.144 | 2.28±0.94 | 0.006a | 1.85±0.53 | 0.017a | 0.64±0.43 | 0.113 | 2.55±1.69 | 0.0012a |
| Age,
<60/>60 | 65/47 | 1.49±0.31 | 0.027a | 1.57±1.10 | 0.087 | 1.88±0.70 | 0.020a | 1.21±0.21 | 0.316 | 1.42±0.99 | 0.102 |
| Recurrence, Rec./No
rec. | 9/103 | 2.28±0.85 | 0.044a | 2.64±0.67 |
<0.001a | 0.97±0.48 | 0.452 | 2.16±0.88 | 0.124 | 3.61±0.51 | 0.015a |
Increasing mRNA expression of β-catenin, cyclin D1,
c-myc, axin2, and E-cadherin was observed with increasing stage of
disease. An inverse tendency was shown for the mRNA expression of
axin2 (see Table V).
Association of the mRNA expression and
the clinical factors
No statistically significant differences in mRNA
expression of any of the studied molecules were observed when
comparing the tumors of MG patients to non-MG patients, as well as
when comparing patients with synchronous malignancy to those with
thymomas only (data not shown). The mRNA expression of all studied
molecules was higher in older patients' group (Table VI).
Follow-up
Median follow-up period was 80 months (range 12–150
months). In 9 patients (8%) a recurrence of the thymoma of the same
histological type was observed (Table
I) with the mean time to progression after the primary surgery
of 63 months (range 23–120 months).
Recurrences were only observed in type B thymomas.
All 5 cases of recurrent B2 thymomas, and 3 of 4 cases of recurrent
B3 thymomas were diagnosed as invasive, but one B3 thymoma was
evaluated as Masaoka-Koga stage I at the time of primary resection.
Immunohistochemically, all recurrent cases of B2 thymomas expressed
β-catenin and E-cadherin on membranes of neoplastic cells at the
invasive periphery of the tumor mass. Expression of mRNA of
β-catenin, cyclin D1 and E-cadherin was significantly increased in
patients with recurrent tumors in comparison to patients without
recurrence (Table VI).
Four patients (3%) died due to the generalization of
type B thymoma 44 to 92 months after the first diagnosis.
Discussion
The molecular pathogenesis of thymomas has remained
largely undiscovered (2,3). Few previous studies have shown
association of thymomas type B with loss of heterozygosity of
APC gene (4,13,14). The
APC molecule plays a key role in regulation of the canonical Wnt
signaling pathway by preventing the accumulation of molecule
β-catenin in cytoplasm. APC together with axin2 forms the
‘destruction complex’ leading to proteasomal degradation of
β-catenin (15–18). Inactivation of APC as well as Wnt
signaling activation blocks the degradation of β-catenin, and thus
increases its concentration in cytoplasm allowing translocation of
β-catenin to nucleus. Once in nucleus, β-catenin forms a
transcriptional complex. This complex increases the transcription
of cyclin D1 and c-myc, and of other molecules, leading to cell
growth. Activation of this pathway has been detected in various
tumors (19,20). but data concerning the involvement of
Wnt signaling in human thymomas are missing.
Liang et al (5) investigated a possible role of the Wnt
signaling pathway in initiation and progression of thymomas in mice
models by introducing the fusion gene of β-catenin together with
estrogen receptor to the mouse genome. Resulting overexpression of
β-catenin led to increased incidence of thymoma resembling human
type B3 thymomas in those mice.
Our results showed that all the respective molecules
are overexpressed also in human thymomas type B, but surprisingly,
in thymomas type A as well. Furthermore, we have detected an
increasing gradient of mRNA expression of these molecules with
increasing thymoma type from B1 up to B3, as well with Masaoka-Koga
stage I up to stage IV. This indicates that the levels of mRNA
expression correspond with aggressive behavior of thymomas type B.
Along with that, the recurrent thymoma cases (all of type B in our
study) displayed significantly increased levels of mRNA expression
of all molecules when compared to non-recurrent tumors.
Axin2 negatively regulates the Wnt pathway by
forming the ‘destruction complex’ of β-catenin, which inhibits the
Wnt signaling. Axin2 expression in type B thymomas was not
significantly different from the control group. However, axin2 was
significantly overexpressed in type A thymomas. Non-invasive
thymomas type A revealed significantly higher expression of this
molecules compared to non-invasive thymomas type B. Thus, the
expression of axin2 corresponds rather to indolent biological
nature and lower proliferative capacity of thymomas type A than to
Masaoka stage I. Despite the general activation of Wnt pathway in
thymomas type A, the negative feedback of axin2 seems to be
preserved.
The molecule of β-catenin also plays a crucial role
in the cell-to-cell adhesion by forming the adherens junction
complex together with the cytoplasmic tail of E-cadherin (21). Alteration of this complex in
neoplastic cells relates to increased proliferation and ability to
metastasize (22). Few previous
studies investigated the immunoexpression of β-catenin and
E-cadherin in thymomas (23–25). Pan et al (26) showed, that the pattern of
immunoexpression of β-catenin differs between thymomas type A
(medullary; cytoplasmic) and type B (cortical; membranous). Both
β-catenin and E-cadherin were overexpressed in our thymoma cases,
but the localization of expression differed-in thymomas type A, B1
and non-invasive type B2, the positivity of these molecules was
localized only in cytoplasm. In contrast, the invasive front of
thymomas type B2 and all thymomas type B3 showed intense membranous
positivity of both molecules. The membranous positivity was also
observed in all recurrent thymomas type B2. Thus, detection of this
pattern might be of a good diagnostic utility for detecting
potentially aggressive tumors in a group of histologically uniform
thymomas type B2.
Nuclear positivity of β-catenin as a result of
activated Wnt pathway has been previously detected in many other
tumors (27). However, more recent
studies show, that the translocation of β-catenin to nucleus is
more likely a multi-factorial process than just a result of
cytosolic accumulation of this molecule, even if the Wnt pathway is
activated (28). The nuclear
positivity was not detected in any neoplastic cells in our samples.
Interestingly, only a minor proportion of cells in Hassall's
corpuscles in control thymic tissue showed a nuclear positivity of
β-catenin (Fig. 2C and D).
In our control thymic tissue, low expression of
molecules of the Wnt pathway was also observed both on mRNA and
protein levels; probably due to the fact that this pathway was
shown to be essential for thymocyte development in a normal thymus
(29,30). Pongracz et al (31) showed, that Wnt ligands provided by
TEC are essential for development of thymocytes. As described by
van Loosdregt et al (32) the
overexpression of Wnt ligands and thus the activation of Wnt
signaling in thymic microenvironment represses function of
regulatory T cells. This change is speculated to be the reason for
the increased incidence of autoimmune disorders (33), which was also detected in some of our
patients with thymomas.
Clinical features of our thymoma cases including the
association with autoimmune disorders and the recurrence rate
correspond to previously published epidemiological data in thymomas
(34–36). Only, we observed slightly increased
proportion of MG patients in the thymoma group. The incidence of MG
in patients with thymoma was higher in younger population and lower
in older patients. Along with that, thymomas of younger patients
were less invasive and showed lower recurrence rate in our study.
Thus, similar to other malignancies of lymphoreticular organs
(6,37), the age over 60 years seems to be a
negative prognostic factor also in thymomas. The increased size of
non-myasthenic thymomas is probably due to delayed manifestation of
these tumors with the absence of the MG and corresponds to higher
age at manifestation.
In summary, the activation of Wnt pathway previously
detected in animal models is present also in human thymomas and may
contribute to the oncogenesis. But, the pattern of expression
differs among thymoma subtypes. The detection of some of these
molecules of the Wnt pathway might be of a diagnostic and
prognostic value.
Acknowledgements
Not applicable.
Funding
The present study was supported by Ministry of
Health, Czech Republic-DRO (University Hospital Motol; grant no.
00064203).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
JZ and PV conceived and designed the study. PV and
JS collected the tissue samples. JZ reviewed all enrolled tissue
samples and supervised the project. PV and JZ performed and
interpreted immunohistochemical experiments. LeK and IO performed
PCR experiments. LuK, ES and JS collected and evaluated patients'
data. PV and JZ were involved in final data analysis and writing
the final manuscript. All authors have read, reviewed and approved
the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee at the Second Faculty of Medicine, Charles University,
Prague. Written informed consent from each patient/guardian was
obtained prior to the enrollment in accordance with the Helsinki
protocol.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
TEC
|
thymic epithelial cells
|
|
MG
|
myasthenia gravis
|
|
F
|
female
|
|
M
|
male
|
|
AID
|
autoimmune disorder
|
References
|
1
|
Travis W, Brambilla E, Burke A, Marx A and
Nicholson A: WHO Classification of Tumours of the Lung, Pleura,
Thymus and Heart. IARC Press. (Lyon). 2015.
|
|
2
|
Li Q, Su YL and Shen WX: A novel
prognostic signature of seven genes for the prediction in patients
with thymoma. J Cancer Res Clin Oncol. 145:109–116. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Girard N: Thymic tumors: Relevant
molecular data in the clinic. J Thorac Oncol. 5:(10 Suppl 4).
S291–S295. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Inoue M, Starostik P, Zettl A, Ströbel P,
Schwarz S, Scaravilli F, Henry K, Willcox N, Müller-Hermelink HK
and Marx A: Correlating genetic aberrations with World Health
Organization-defined histology and stage across the spectrum of
thymomas. Cancer Res. 63:3708–3715. 2003.PubMed/NCBI
|
|
5
|
Liang CC, Lu TL, Yu YR, You LR and Chen
CM: β-catenin activation drives thymoma initiation and progression
in mice. Oncotarget. 6:13978–13993. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
International Non-Hodgkin's Lymphoma
Prognostic Factors Project, . A predictive model for aggressive
non-Hodgkin's lymphoma. N Engl J Med. 329:987–994. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sehn LH, Berry B, Chhanabhai M, Fitzgerald
C, Gill K, Hoskins P, Klasa R, Savage KJ, Shenkier T, Sutherland J,
et al: The revised International Prognostic Index (R-IPI) is a
better predictor of outcome than the standard IPI for patients with
diffuse large B-cell lymphoma treated with R-CHOP. Blood.
109:1857–1861. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Girard N, Ruffini E, Marx A, Faivre-Finn C
and Peters S; ESMO Guidelines Committee, : Thymic epithelial
tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment
and follow-up. Ann Oncol. 5 (Suppl 26):v40–v55. 2015. View Article : Google Scholar
|
|
9
|
Boehm T and Swann JB: Thymus involution
and regeneration: Two sides of the same coin? Nat Rev Immunol.
13:831–838. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
10
|
Detterbeck FC, Nicholson AG, Kondo K, Van
Schil P and Moran C: The Masaoka-Koga stage classification for
thymic malignancies: Clarification and definition of terms.
Zhongguo Fei Ai Za Zhi. 17:75–81. 2014.(In Chinese). PubMed/NCBI
|
|
11
|
Bijwaard KE, Aguilera NS, Monczak Y,
Trudel M, Taubenberger JK and Lichy JH: Quantitative real-time
reverse transcription-PCR assay for cyclin D1 expression: utility
in the diagnosis of mantle cell lymphoma. Clin Chem. 47:195–201.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Strobel P, Hohenberger P and Marx A:
Thymoma and thymic carcinoma: Molecular pathology and targeted
therapy. J Thorac Oncol. 5 (10 Suppl 4):S286–290. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhou R, Zettl A, Ströbel P, Wagner K,
Müller-Hermelink HK, Zhang S, Marx A and Starostik P: Thymic
epithelial tumors can develop along two different pathogenetic
pathways. Am J Pathol. 159:1853–1860. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hankey W, Frankel WL and Groden J:
Functions of the APC tumor suppressor protein dependent and
independent of canonical WNT signaling: Implications for
therapeutic targeting. Cancer Metastasis Rev. 37:159–172. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Stamos JL and Weis WI: The β-catenin
destruction complex. Cold Spring Harb Perspect Boil. 5:a0078982013.
View Article : Google Scholar
|
|
17
|
Yamulla RJ, Kane EG, Moody AE, Politi KA,
Lock NE, Foley AV and Roberts DM: Testing models of the APC tumor
suppressor/β-catenin interaction reshapes our view of the
destruction complex in Wnt signaling. Genetics. 197:1285–1302.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nakamura T, Hamada F, Ishidate T, Anai K,
Kawahara K, Toyoshima K and Akiyama T: Axin, an inhibitor of the
Wnt signalling pathway, interacts with beta-catenin, GSK-3beta and
APC and reduces the beta-catenin level. Genes Cells. 3:395–403.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang L and Shay JW: Multiple roles of APC
and its therapeutic implications in colorectal cancer. J Natl
Cancer Inst. 109:2017. View Article : Google Scholar
|
|
20
|
Hirschman BA, Pollock BH and Tomlinson GE:
The spectrum of APC mutations in children with hepatoblastoma from
familial adenomatous polyposis kindreds. J Pediatr. 147:263–266.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Huber AH, Stewart DB, Laurents DV, Nelson
WJ and Weis WI: The cadherin cytoplasmic domain is unstructured in
the absence of beta-catenin. A possible mechanism for regulating
cadherin turnover. J Boil Chem. 276:12301–12309. 2001. View Article : Google Scholar
|
|
22
|
Gloushankova NA, Rubtsova SN and Zhitnyak
IY: Cadherin-mediated cell-cell interactions in normal and cancer
cells. Tissue Barriers. 5:e13569002017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Yoshino I, Kase S, Yano T, Sugio K and
Sugimachi K: Expression status of E-cadherin and alpha-, beta-, and
gamma-catenins in thymoma. Ann Thorac Surg. 73:933–937. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang Y, Li L, Li Q, Xie C and Wang E and
Wang E: Expression of P120 catenin, Kaiso, and metastasis tumor
antigen-2 in thymomas. Tumour Biol. 33:1871–1879. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Riess JW, West R, Dean M, Klimowicz AC,
Neal JW, Hoang C and Wakelee HA: GLI1, CTNNB1 and NOTCH1 protein
expression in a thymic epithelial malignancy tissue microarray.
Anticancer Res. 35:669–676. 2015.PubMed/NCBI
|
|
26
|
Pan CC, Ho DM, Chen WY, Chiang H, Fahn HJ
and Wang LS: Expression of E-cadherin and alpha- and beta-catenins
in thymoma. J Pathol. 184:207–211. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kumar R and Bashyam MD: Multiple oncogenic
roles of nuclear beta-catenin. J Biosci. 42:695–707. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Morgan RG, Ridsdale J, Tonks A and Darley
RL: Factors affecting the nuclear localization of β-catenin in
normal and malignant tissue. J Cell Biochem. 115:1351–1361. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zuklys S, Gill J, Keller MP, Hauri-Hohl M,
Zhanybekova S, Balciunaite G, Na KJ, Jeker LT, Hafen K, Tsukamoto
N, et al: Stabilized beta-catenin in thymic epithelial cells blocks
thymus development and function. J Immunol. 182:2997–3007. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Staal FJ, Luis TC and Tiemessen MM: WNT
signalling in the immune system: WNT is spreading its wings. Nat
Rev Immunol. 8:581–593. 2008. View
Article : Google Scholar : PubMed/NCBI
|
|
31
|
Pongracz J, Hare K, Harman B, Anderson G
and Jenkinson EJ: Thymic epithelial cells provide WNT signals to
developing thymocytes. Eur J Immunol. 33:1949–1956. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
van Loosdregt J, Fleskens V, Tiemessen MM,
Mokry M, van Boxtel R, Meerding J, Pals CE, Kurek D, Baert MR,
Delemarre EM, et al: Canonical Wnt signaling negatively modulates
regulatory T cell function. Immunity. 39:298–310. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Evoli A and Lancaster E: Paraneoplastic
disorders in thymoma patients. J Thorac Oncol. 9 (9 Suppl
2):S143–S147. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Safieddine N, Liu G, Cuningham K, Ming T,
Hwang D, Brade A, Bezjak A, Fischer S, Xu W, Azad S, et al:
Prognostic factors for cure, recurrence and long-term survival
after surgical resection of thymoma. J Thorac Oncol. 9:1018–1022.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ruffini E, Detterbeck F, Van Raemdonck D,
Rocco G, Thomas P, Weder W, Brunelli A, Evangelista A and Venuta F;
European Association of Thoracic Surgeons (ESTS) Thymic Working
Group, : Tumours of the thymus: A cohort study of prognostic
factors from the European Society of Thoracic Surgeons database.
Eur J Cardiothorac Surg. 46:361–368. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Engels EA and Pfeiffer RM: Malignant
thymoma in the United States: Demographic patterns in incidence and
associations with subsequent malignancies. Int J Cancer.
105:546–551. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Buske C, Hutchings M, Ladetto M, Goede V,
Mey U, Soubeyran P, Spina M, Stauder R, Trnený M, Wedding U, et al:
ESMO consensus conference on malignant lymphoma: General
perspectives and recommendations for the clinical management of the
elderly patient with malignant lymphoma. Ann Oncol. 29:544–562.
2018. View Article : Google Scholar : PubMed/NCBI
|