Introduction
Breast cancer (BC) is a highly heterogeneous cancer
in both biological mechanisms and clinical treatment.
Triple-negative breast cancer accounts for ~15–30% of invasive
breast cancer, lacks the expression of estrogen receptors (ERs) and
progesterone receptors (PRs), and does not overexpress human
epidermal growth factor receptor 2 (HER2) (1). The lack of receptors on TNBC that can
be targeted by drugs has made the development of treatments for
TNBC challenging compared with other BC types. To date, to the best
of our knowledge, not a single targeted therapy has been approved
for the treatment of TNBC, and traditional chemotherapeutic
reagents remain the standard treatment. Patients who do not show a
pathologically complete response have a poor prognosis with a high
incidence of recurrence (2–4); thus, there is an urgent need to explore
new therapies and provide more patients with TNBC with other
treatment options (5,6).
Immune checkpoint inhibitors (ICIs), such as
antibodies targeting the checkpoints cytotoxic
T-lymphocyte-associated antigen-4 (CTLA-4; for example, ipilimumab)
and programmed cell death protein 1 (PDCD1; for example,
pembrolizumab and nivolumab), have shown remarkable achievements in
a variety of cancer types, such as melanoma, Hodgkin's lymphoma and
non-small-cell lung cancer (7–10). A
multicenter, nonrandomized phase I-b clinical trial named
KEYNOTE-012 (Clinical Trials.gov
identifier: NCT01848834) aims to investigate the safety,
tolerability and antitumor activity of pembrolizumab (a programmed
death-ligand 1, PDL1, inhibitor) in patients with TNBC and
adenocarcinoma of the stomach or gastro-oesophageal junction
(11). Among the 27 women with TNBC
who were evaluable for antitumor activity, the overall response
rate (ORR) was 18.5%, and the median time to response was 17.9
weeks (range, 7.3–32.4 weeks). Only a small fraction of patients
with TNBC exhibited satisfactory clinical responses compared with
patients with other solid tumors enrolled in KEYNOTE-012 (ORR:
Advanced gastric cancer, 22%; advanced or metastatic urothelial
cancer, 26%; and head and neck squamous cell carcinoma, 59%)
(12–16). Therefore, it has become a primary
priority to identify potential targetable biomarkers for ICI
therapy and to investigate strategies to increase patient response
rates.
Biomarkers, such as expression of the checkpoint
PDL1 (17,18), tumor mutation burden (TMB) (19), tumor-infiltrating lymphocytes (TILs)
(20), neoantigen load (21), and immune-regulatory mRNA expression
signatures (22), are potentially
applicable to predict the efficacy of ICIs. However, challenges in
defining a validated cut-off value, intratumoral heterogeneity,
test platform uniformities and dynamic changes have limited the
clinical application (19,23,24).
Furthermore, individual tumor clonal genotypes may require the
screening of patients with TNBC to determine who will benefit from
ICI therapy (25).
The present study aimed to verify the traditional
ICI biomarkers, to explore novel biomarkers of TNBC and screen the
patients who would benefit from ICI therapy.
Materials and methods
Data sources
The expression of the checkpoint molecules CTLA-4,
indoleamine 2, 3-dioxygenase 1 (IDO1), lymphocyte-activation gene 3
(LAG3), PDCD1, PDL1 and T cell immunoglobulin and mucin
domain-containing protein 3 (TIM3) across four types of BC (HER2,
luminal A, luminal B and TNBC) were obtained from a previous
comprehensive study of human breast cancer (26) in The Cancer Genome Atlas (TCGA)
database (cancer.gov/tcga) and
log2-transformed. Normalized RNA-sequencing (RNA-seq)
data were downloaded from the TCGA data portal. TMB data were also
retrieved from the database. All data were analyzed using R
(version 3.2.2) (27) and RStudio
version 1.1.463 (28), unless
otherwise stated.
Cytolytic activity (CYT)
In order to study immune effector activity in TNBC,
CYT was calculated as the log-average (geometric mean) of
perforin-1 (PRF1) and granzyme-A (GZMA) expression in transcripts
per million using RNA-seq data from TCGA.
Immune signature and single-sample
gene set enrichment analysis (ssGSEA)
To evaluate the immune signatures in the tumor
microenvironment of TNBC, ssGSEA was used to identify gene sets
from the Molecular Signatures Database (software.broadinstitute.org/gsea/msigdb/) that
were enriched in TNBC; 28 heterogeneous immune cells were
classified according to gene sets that share common biological
function, chromosomal location, or regulation. Based on the immune
signature spectrum, the degree of immune cell infiltration was
determined by the ssGSEA scores, which were computed using
R-package ‘Gene Set Variation Analysis’ version 1.34.0 (bioconductor.org/packages/GSVA/). The
immune signature was clustered into high-, medium- and
low-infiltration populations.
Random forests
To classify tumors of TNBC according to CYT, an
accurate classification method named random forests was introduced.
Random forests are comprised of a multitude of tree predictors such
that each tree depends on a random vector independently, and all
decision trees in the forests have the same distribution. A total
of 782 parameters were used to assess CYT according to the
importance score used to determine CYT. After
dimensionality-reduced visualization by the multidimensional
scaling (MDS) algorithm, the proximity of samples indicated their
similarity in immunophenotype.
Ethical approval and informed
consent
This study did not involve experiments on humans or
animals performed by any of the authors.
Statistical analysis
Statistical analysis was conducted by a two-way
Mann-Whitney test and one-way analysis of variance using the R
package. The correlation analysis between CYT and TMB was performed
by Pearson's correlation. Kaplan Meier-plotter (KM plotter)
(29) could assess the effect of
54,675 genes on survival of 5,143 patients with breast cancer with
a mean follow-up of 69 months. The hazard ratio (HR) with 95%
confidence intervals and log-rank P-value were calculated and
displayed on the plot. P<0.05 was considered to indicate a
statistically significant difference.
Results
Suppressive tumor immune
microenvironment in TNBC
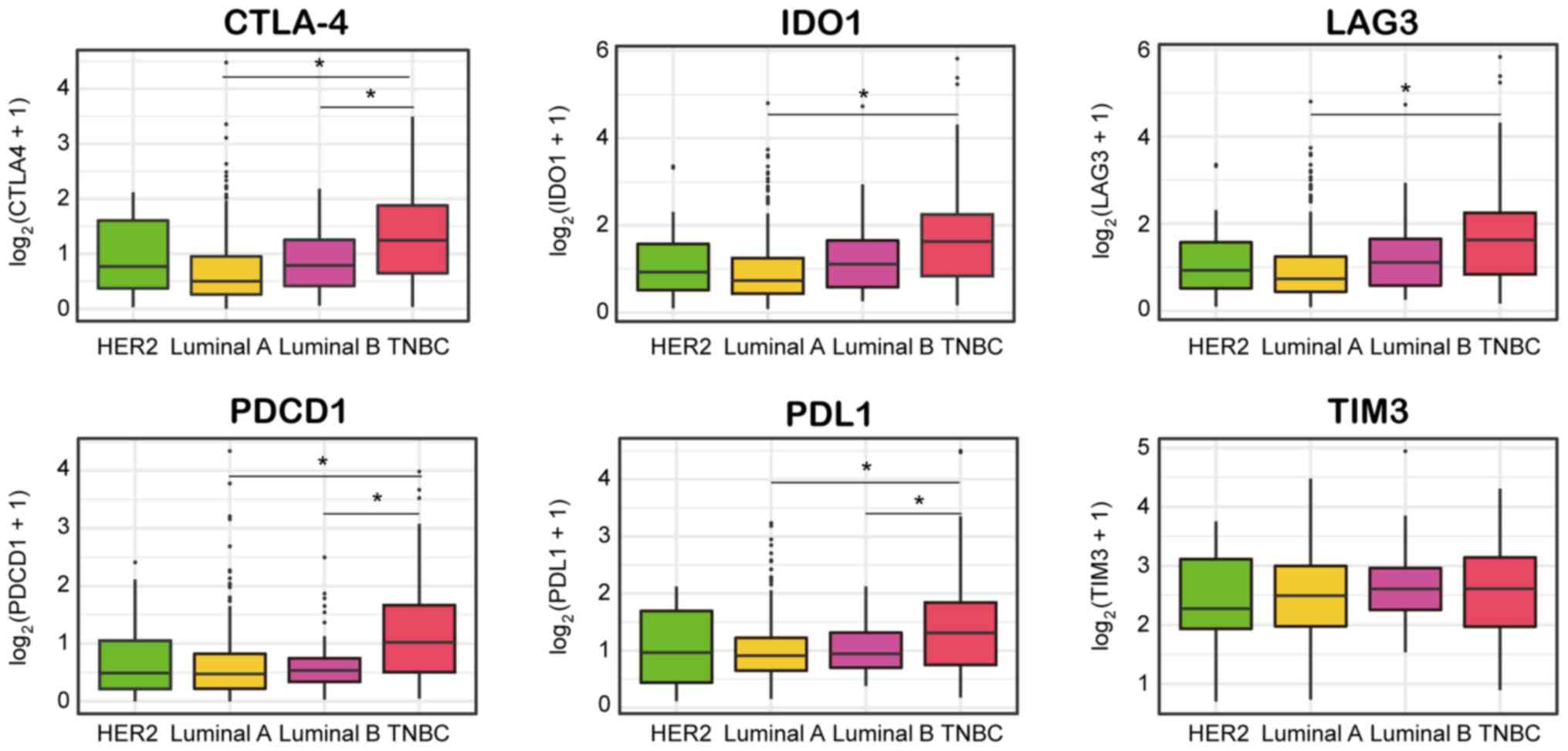
Pre-existing expression of immune regulatory
molecules is known as an indication of favorable responsiveness to
ICIs in solid tumors. To investigate the immunophenotype of TNBC in
comparison with other pathological types of BC, gene expression
profiling and luminal categorization data were used from the
publicly available TCGA database. Six immune regulatory molecules,
including CTLA-4, IDO1, LAG3, PDCD1, PDL1 and TIM3, were examined
in patients with each luminal type of BC. In this analysis, the
highest expression intensity of CTLA-4, IDO1, LAG3, PDCD1 and PDL1
was identified in patients with TNBC among the four types. TIM3
demonstrated the second highest expression level in TNBC among the
four types (Fig. 1). Moreover,
higher expression of these immune regulatory molecules, including
CTLA-4, IDO1, LAG3, PDCD1, PDL1 and TIM3, was not associated with
overall survival in patients with TNBC (Fig. S1). Thus, this enrichment of immune
regulatory molecules suggested a suppressive antitumor response and
poor prognosis in TNBC.
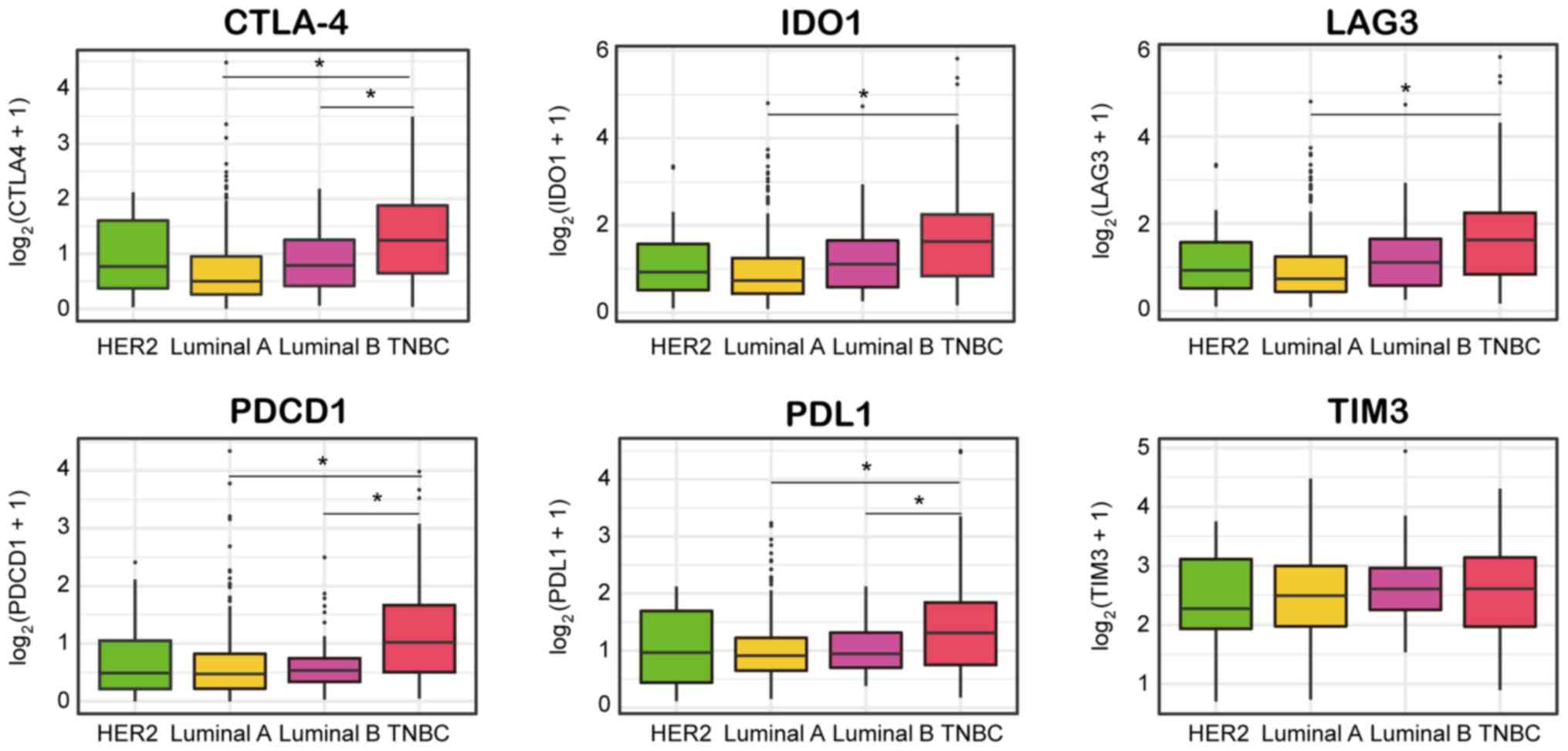 | Figure 1.Expression and prognostic value of
immune checkpoint genes of breast cancer. The relative expression
of six immune checkpoint genes across four subtypes,
HER2+, luminal A, luminal B and TNBC, is shown. The
expression of CTLA-4, IDO1, LAG3, PDCD1, PDL1 and TIM3 was
log2-transformed. *P<0.05. CTLA-4, cytotoxic
T-lymphocyte-associated antigen 4; IDO1, indoleamine 2,
3-dioxygenase 1; LAG3, lymphocyte-activation gene 3; PDCD1, PDL1,
programmed death-ligand 1; TIM3, T cell immunoglobulin and mucin
domain-containing protein 3; HER2, human epidermal growth factor
receptor 2; TNBC, triple negative breast cancer. |
Cytolytic immune response is
independent of TMB
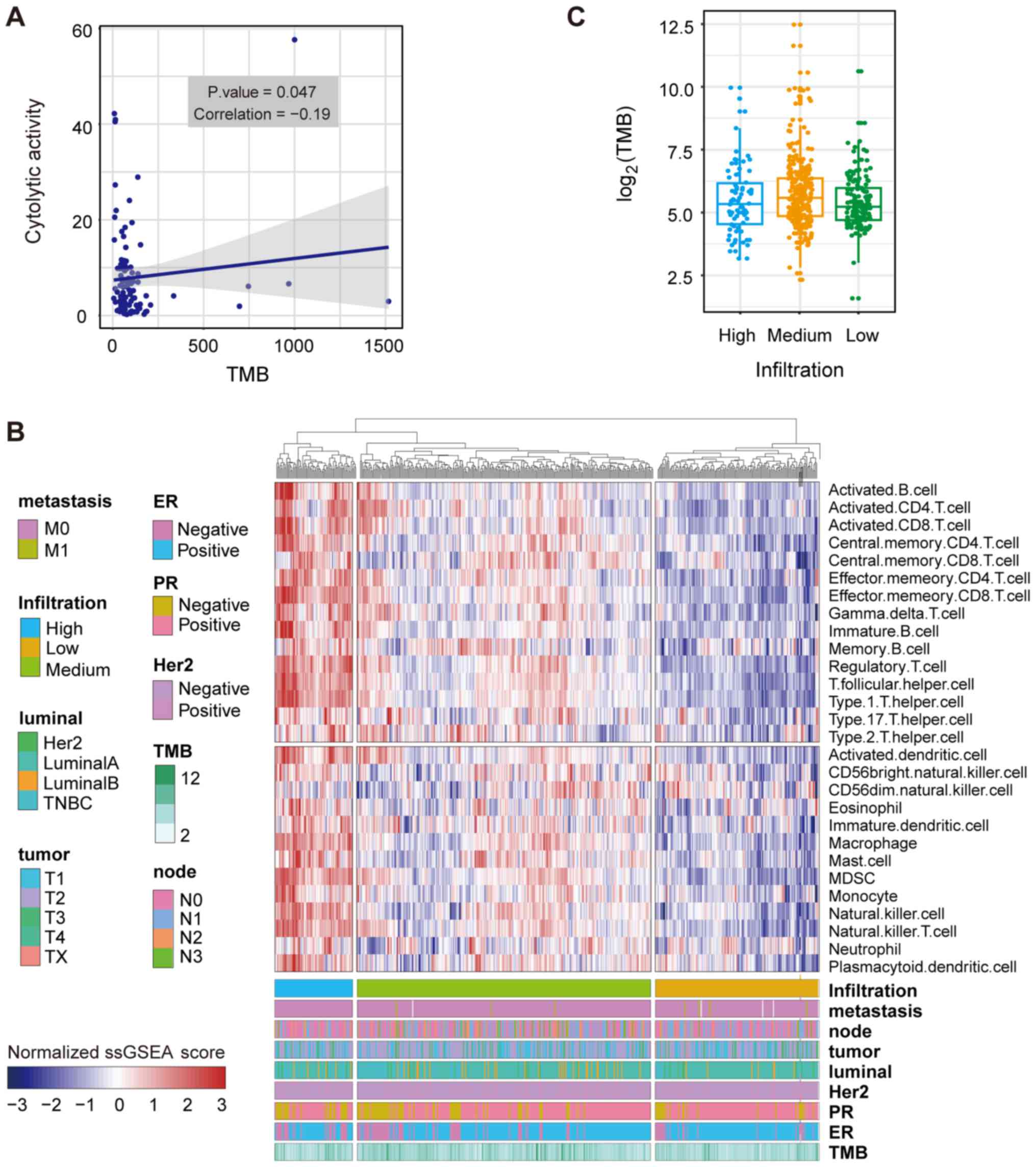
A comprehensive evaluation of the tumor
microenvironment of TNBC contributes to population selection.
Effective antitumor cytotoxic responses rely on the recognition and
presentation of newly generated and tumor-specific antigenic
peptides on the cancer cell surface (30). Thus, whether the TMB could indicate
the magnitude of the cytolytic immune response in the immune
microenvironment of TNBC was first examined. To this end, CYT, a
surrogate measurement of the magnitude of the cytolytic immune
response was used (31). CYT was
calculated as the geometric mean of GZMA and PRF1 expression, and
has served as a highly specific marker in human glioblastoma
(32). Based on this index, a very
weak correlation was observed between the TMB and CYT in patients
with TNBC (Fig. 2A), which strongly
suggested that TMB may not represent the magnitude of the cytolytic
immune response in TNBC.
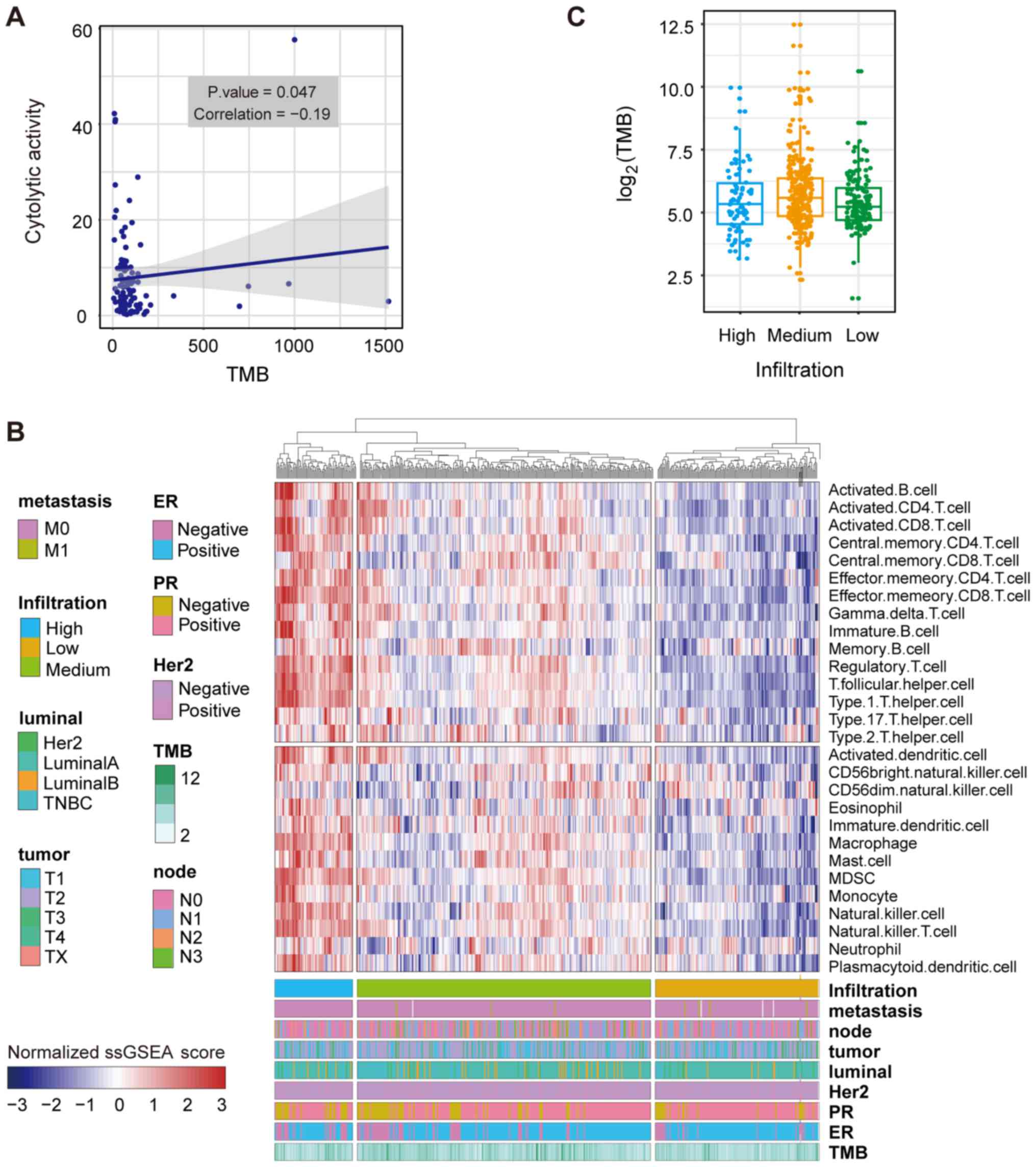 | Figure 2.TMB alone is not sufficient to assess
CYT. (A) Correlation between CYT and TMB in patients with TNBC. The
metric of CYT was quantified by mapping unmapped RNA-seq reads and
normalizing to the count of mapped reads. (B) ssGSEA contributes to
identifying the relative expression of immune cell populations and
classifies patients with TNBC into three categories according to
immune cell infiltration. The gradient of colors, from cool colors
to warm colors, represents scores of immune cell infiltration (from
−3 to 3, respectively). (C) There was no association between TMB
and different degrees of immune cell infiltration (high, medium and
low) in patients with TNBC. CYT, cytolytic activity; TNBC, triple
negative breast cancer; TMB, tumor mutation burden; ssGSEA,
single-sample gene set enrichment analysis; ER, estrogen receptor;
PR, progesterone receptor; HER2, human epidermal growth factor
receptor 2. |
In addition to CYT, immune cell infiltration in the
tumor immune microenvironment is directly correlated with the
magnitude of the cytolytic immune response (33). Furthermore, systemic characterization
of the pattern of tumor-infiltrating immune cell populations could
lead to a deeper understanding of the TNBC immune microenvironment.
Thus, whether a higher/lower TMB could predict the different
infiltration levels of immune cells was tested. To estimate the
relative infiltration of several intratumoral immune cell
populations, the ssGSEA method was employed. This bioinformatics
method translates the transcriptomic expression data as a
normalized score to represent the relative abundance of specific
cell types (34). Patients with TNBC
were classified into three categories according to the degree of
infiltration that was displayed by an unsupervised clustering
algorithm (Fig. 2B). The color of
each sample in the heatmap ranged from a cool color to a warm
color, which represented scores from −3 to 3, respectively, and
depicted infiltration of low, medium and high degrees. The
clinicopathological characteristics, such as Tumor-Node-Metastasis
stage, tissue type, and the expression of HER2, ER and PR, were
also annotated.
Among these characteristics, it was found that
clinical factors did not affect immune cell infiltration. TMB was
not associated with the degree of infiltration (Fig. 2C). This suggests that TMB was not the
only factor that determined the final immune response; further
research is required to identify other biomarkers.
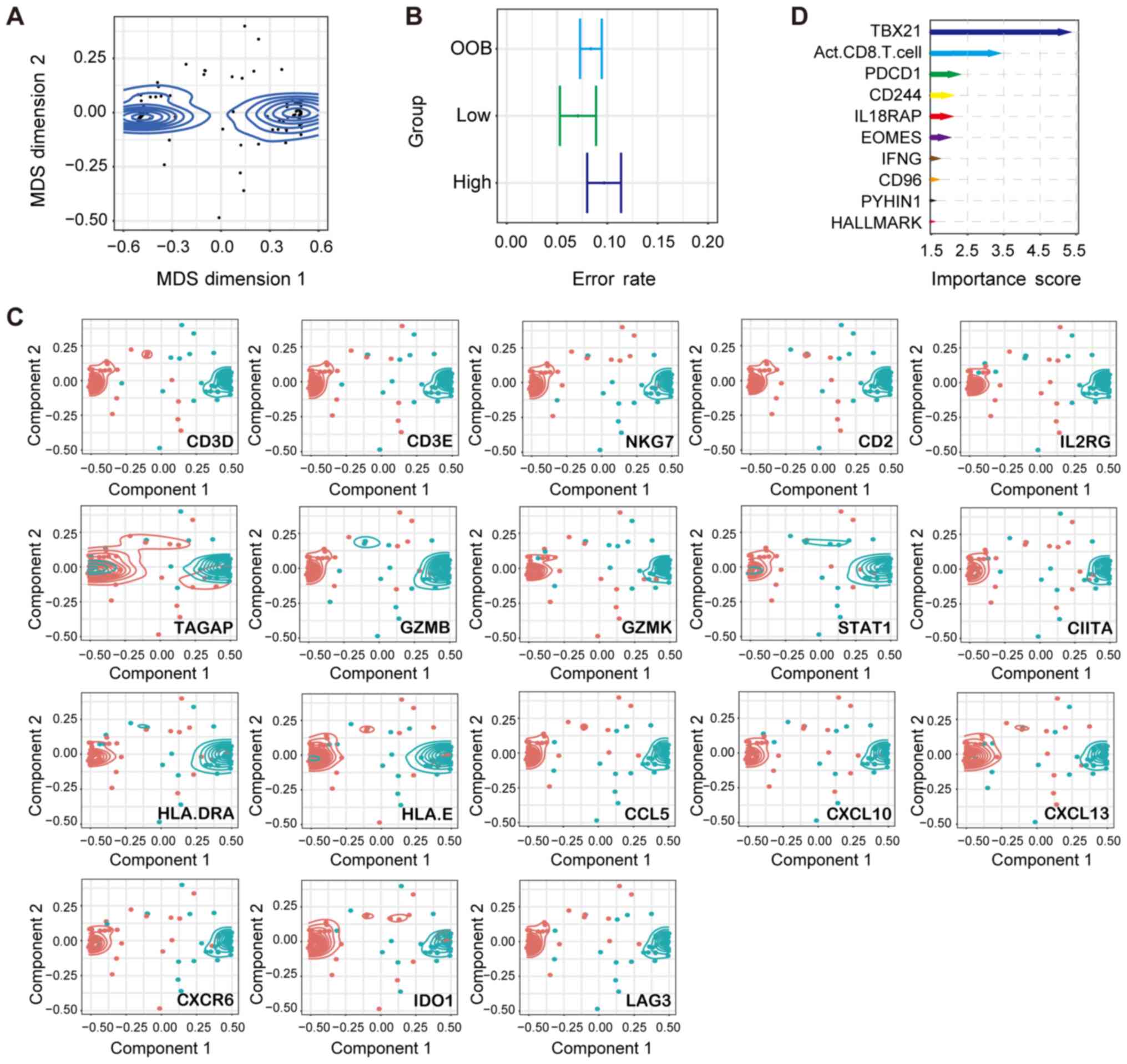
Machine learning identified dominant
factors in determining CYT
Given that the TMB is not directly correlated with
CYT in patients with TNBC, the optimization of the local immune
response by a systematic approach was explored. To this end, the
random forest method, a machine learning method based on multiple
random-built decision trees, was employed. Hundreds of variants
were employed as input parameters, including the relative
infiltration of 28 types of immune cells, somatic mutation counts,
78 immune-related molecules, and 50 signaling pathways from the
HALLMARK collection. By MDS algorithm, the close proximity of every
two patients was illustrated to determine the similarity of
immunological statuses between them. Two distinct immunological
statuses were clearly categorized when guided by the density
contour (Fig. 3A). To avoid
artificial bias, out-of-bag samples supported a rational and
acceptable error rate for the decision trees in the present
analysis (Fig. 3B). Recently, Ayers
et al (35) demonstrated that
an expanded panel with 18 genes could distinguish different
immunological statuses and predict a greater likelihood of response
to immune checkpoint inhibitors. The panel includes genes involved
in immune cell enrichment (CD3D, CD3E and NKG7), activation and
function (CD2, IL2RG, TAGAP, GZMB, GZMK and STAT1), antigen
presentation (CIITA, HLA-DRA, and HLA-E), chemokines and a
chemokine receptor (CCL5, CCL10, CXCL13, and CXCR6) and immune
checkpoint molecules (IDO1 and LAG3). Thus, these gene panels were
introduced to further characterize the immunological statuses and
ICI-responsive potential of patients with TNBC. Almost all 18 genes
showed higher expression in the immunologically hot compared with
the immunologically cold patients with TNBC, supporting an
ICI-responsive potential for immunologically hot patients (Fig. 3C).
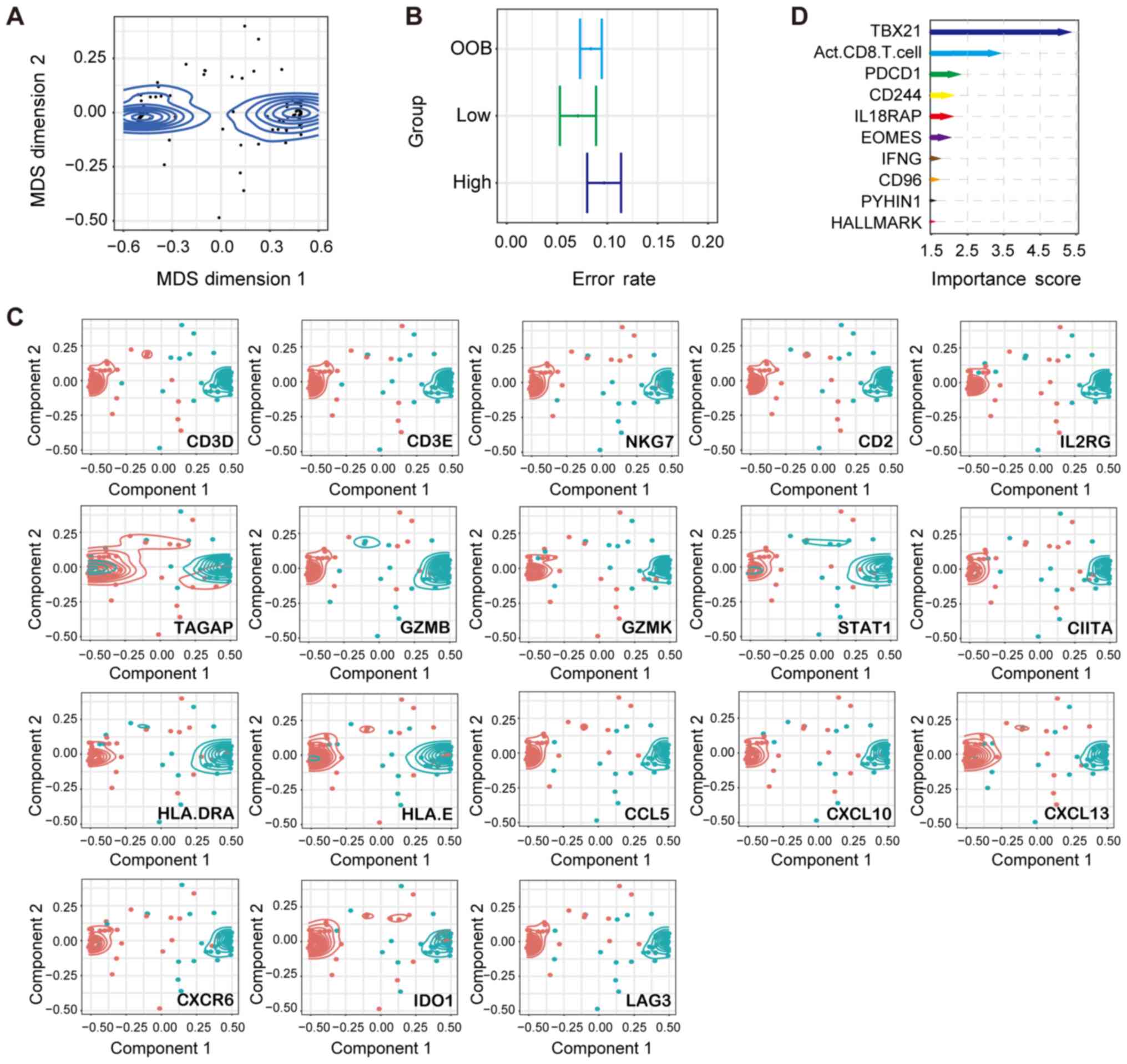 | Figure 3.Key immunological factors in
determining the nature of TMB. (A) Patients with TNBC were divided
into two categories, according to the level of cytolytic activity
determined by the density contour of Gaussian maximum fitting. (B)
OOB samples providing estimates of model error rate for the
decision trees validated the confidence of categories. (C) A total
of 18 immune-associated molecules were used to distinguish the
immunological statuses and predict the response to immune
checkpoint inhibitors of patients with TNBC. (D) The importance
score of ten most determinant signatures of the tumor
microenvironment: TBX21, activated CD8+ T cell, PDCD1,
CD244, IL18RAP, EOMES, IFNG, CD96, PYHIN1 and
Hallmark-Allograft-Rejection. CYT, cytolytic activity; TNBC, triple
negative breast cancer; TMB, tumor mutation burden; ssGSEA,
single-sample gene set enrichment analysis; OOB, out-of-bag;
multidimensional scaling. |
The most determining features in forming local CYT
were identified using the importance score over all the input
parameters (Fig. 3D). This score was
derived from the machine learning process and represented the
relative contribution of each factor to the resulting immune
response. Several effector molecules, key transcription factors in
the Th1/CTL response, were found in this analysis, which is
consistent with established knowledge on antitumor immunity.
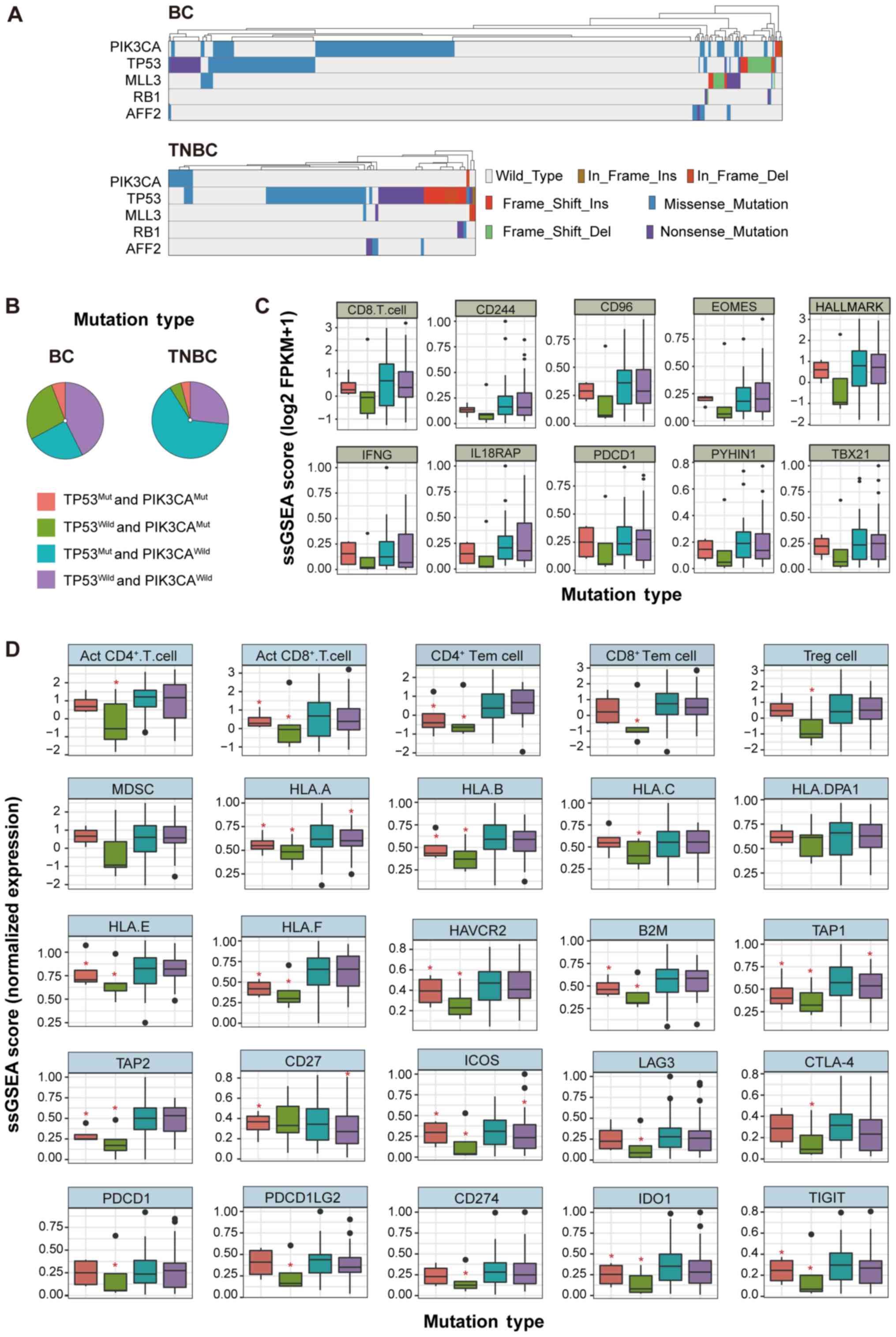
TP53MutPIK3CAWild genotype defines patients
with ICI-responsive potential
A previous study successfully demonstrated that
specific genomic alterations are correlated with different
efficacies of ICI treatment (36).
The present study aimed to test whether oncogenic mutations in TNBC
could cause different immunological statuses and sensitivities to
immunotherapy. It is known that mutations in TP53 and PIK3CA occur
frequently in patients with TNBC, and thus alterations in these
genes may involve as many clinic cases as possible (Fig. 4A). The ability of TP53/PIK3CA to
define a subset of the tumor immune microenvironment was firstly
examined. Four subsets were defined according to genomic
alterations in TP53 and PIK3CA (Fig.
4B). Among the four different genotypes, the top 10 dominant
factors in determining (Fig. 3D) CYT
were examined (Fig. 4C). TNBC
harboring wild-type PIK3CA had a significant abundance of all
factors in comparison with the wild-type counterparts, suggesting a
provoked antitumor response in patients with wild-type PIK3CA.
Moreover, when focusing on PIK3CAWild patients, it was
found that the TP53 mutation further indicated a subgroup with
higher expression of the dominant factors. These findings implied
that patients with genomic PIK3CAWild and
TP53Mut alterations exhibited an elicited pre-existing
CYT.
In recent years, new RNA-seq-derived biomarkers
characterizing the inflamed tumor immune microenvironment represent
one of the most exciting avenues for predicting the sensitivity of
ICI immunotherapies in the treatment of solid tumors (35–37). In
order to further evaluate the ICI-responsive potential, a scoring
system using an immunophenotype score over four typically
immunological factors was introduced: Effector cells (activated
CD4+ T cells and CD8+ T cells,
CD4+ Tem cells and CD8+ Tem cells),
suppressor cells (regulatory T cells and MDSCs), MHC molecules
(HLA-A, HLA-B, HLA-C, HLA-DPA1, HLA-E, HLA-F, HAVCR2, B2M, TAP1 and
TAP2), and immunomodulators (immunostimulatory: CD27 and ICOS; and
immune inhibitor molecules: LAG3, CTLA-4, PDCD1, PDCD1LG2, CD274,
IDO1 and TIGIT; Fig. 4D). An
elevated expression of the aforementioned immunological parameters
was demonstrated in general, suggesting the
TP53MutPIK3CAWild genotype as a potential
biomarker for ICI treatment in patients with TNBC. This finding
verified the hypothesis that patients with wild-type PIK3CA and
TP53 mutations may have an improved response to immunotherapy.
Discussion
The present study aimed to identify biomarkers that
would help to screen for patients with BC who were most likely to
benefit from ICI therapy. A large gene analysis suggested that
patients with TNBC might respond differently to ICIs based on their
inclusion in one of the four subtypes of BC. The machine learning
method facilitated the classification of TNBC according to its
heterogenicity; a panel of 18 immune-associated molecules further
divided TNBC into ‘hot’ and ‘cold’ tumors and indicated two
different treatment outcomes. Based on these findings, specific
gene mutations also affected the antitumor response, and patients
with the TP53MutPIK3CAWild genotype may have
an improved response to immunotherapy.
Gene analysis has proven to be a novel approach for
judging the potential clinical benefit of immunotherapy. The
expression of immune checkpoint genes, such as CTLA-4, IDO1, LAG3,
PDCD1, PDL1 or TIM3, which has traditionally been associated with
responsiveness to ICIs, was analyzed as an indicator for screening
tumors that were more suitable for immunotherapy (38). TNBC was identified as such a tumor,
with genes that were highly expressed. A recent study has shown
that PDL1 expression is associated with the presence of TILs
(39). The patients with TNBC were
divided into three groups, according to the infiltration of TILs:
High, medium and low infiltration.
Notably, there were no significant differences
between TMB and TILs. This finding suggested that in addition to
TMB, other factors, including the infiltration of immunosuppressive
cells, the state of blood vessels, the size of the lesion, and the
molecular typing of the lesion, also affected the TILs, which might
have caused the significant differences. Advances in technological
tools and high-throughput sequencing have increased the possibility
of comprehensive characterization of somatic mutations (40). TMB has an important impact on the
understanding of the efficacy of ICIs, as antigens that arise as a
consequence of TMB are often targets of anti-PDL1 and anti-CTLA-4
in mice (41). While TMB was not
strongly associated with CYT in TNBC, specific biomarkers are
needed to confirm these findings.
More than half of human tumors carry TP53 gene
mutations, and these mutations are also frequently found in BCs
(42). However, the prognostic
impact and response of the TP53 mutations across the different
molecular subtypes are still poorly understood. It was reported
that TP53 mutations were associated with poor prognosis and
increased mortality in patients with luminal B, HER2-enriched, and
normal-like tumors but not in patients with luminal A and
basal-like tumors (43). It was
found that patients with TP53 mutations had an improved response to
ICIs, in terms of higher expression of immune-associated molecules,
which meant a more suitable antitumor microenvironment. PIK3CA is
the second most frequently mutated gene, following the TP53 gene,
and is associated with different types of BC. PIK3CA mutations may
have favorable outcomes for patients with hormone receptor-positive
BCs but may also constitute a major mechanism of resistance to
trastuzumab treatment (44,45). The oncogene PIK3CA activates
multipotent genetic programs and influences intratumoral
heterogeneity (46).
In conclusion, the findings of the present study
suggested that patients with TNBC may be the best suited for
immunotherapy among the four subtypes of BC, and patients with the
TP53MutPIK3CAWild genotype will benefit most
from ICI treatment. However, the clinical significance needs to be
verified by further investigation.
Supplementary Material
Supporting Data
Acknowledgements
The abstract was presented at the 17th International
Congress of Immunology, 19th-23rd October 2019 in Beijing,
China.
Funding
This study was funded by the National Natural
Science Foundation of China (grant nos. 81472648, 81620108023 and
31700776).
Availability of data and materials
The datasets generated and/or analyzed during the
present study are available in the TCGA database (https://gdc-portal.nci.nih.gov/).
Authors' contributions
JC and QJ analyzed the data, constructed figures and
drafted the manuscript. JC, XD and SX were involved in data
collection and analysis. BZ and QJ contributed to the conception
and design of the study. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gluz O, Liedtke C, Gottschalk N, Pusztai
L, Nitz U and Harbeck N: Triple-negative breast cancer-current
status and future directions. Ann Oncol. 20:1913–1927. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Dent R, Trudeau M, Pritchard KI, Hanna WM,
Kahn HK, Sawka CA, Lickley LA, Rawlinson E, Sun P and Narod SA:
Triple-negative breast cancer: Clinical features and patterns of
recurrence. Clin Cancer Res. 13:4429–4434. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Liedtke C, Mazouni C, Hess KR, André F,
Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B,
Green M, et al: Response to neoadjuvant therapy and long-term
survival in patients with triple-negative breast cancer. J Clin
Oncol. 26:1275–1281. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Foulkes WD, Smith IE and Reis-Filho JS:
Triple-negative breast cancer. N Engl J Med. 363:1938–1948. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wahba HA and El-Hadaad HA: Current
approaches in treatment of triple-negative breast cancer. Cancer
Biol Med. 12:106–116. 2015.PubMed/NCBI
|
|
6
|
Mayer IA, Abramson VG, Lehmann BD and
Pietenpol JA: New strategies for triple-negative breast
cancer-deciphering the heterogeneity. Clin Cancer Res. 20:782–790.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Larkin J, Chiarion-Sileni V, Gonzalez R,
Grob JJ, Cowey CL, Lao CD, Schadendorf D, Dummer R, Smylie M,
Rutkowski P, et al: Combined nivolumab and ipilimumab or
monotherapy in untreated melanoma. N Engl J Med. 373:23–34. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wolchok JD, Kluger H, Callahan MK, Postow
MA, Rizvi NA, Lesokhin AM, Segal NH, Ariyan CE, Gordon RA, Reed K,
et al: Nivolumab plus ipilimumab in advanced melanoma. N Engl J
Med. 369:122–133. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ansell SM, Lesokhin AM, Borrello I,
Halwani A, Scott EC, Gutierrez M, Schuster SJ, Millenson MM, Cattry
D, Freeman GJ, et al: PD-1 blockade with nivolumab in relapsed or
refractory Hodgkin's lymphoma. N Engl J Med. 372:311–319. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Garon EB, Rizvi NA, Hui R, Leighl N,
Balmanoukian AS, Eder JP, Patnaik A, Aggarwal C, Gubens M, Horn L,
et al: Pembrolizumab for the treatment of non-small-cell lung
cancer. N Engl J Med. 372:2018–2028. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nanda R, Chow LQ, Dees EC, Berger R, Gupta
S, Geva R, Pusztai L, Pathiraja K, Aktan G, Cheng JD, et al:
Pembrolizumab in patients with advanced triple-negative breast
cancer: Phase Ib KEYNOTE-012 study. J Clin Oncol. 34:2460–2467.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Muro K, Chung HC, Shankaran V, Geva R,
Catenacci D, Gupta S, Eder JP, Golan T, Le DT, Burtness B, et al:
Pembrolizumab for patients with PD-L1-positive advanced gastric
cancer (KEYNOTE-012): A multicentre, open-label, phase 1b trial.
Lancet Oncol. 17:717–726. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Seiwert TY, Burtness B, Mehra R, Weiss J,
Berger R, Eder JP, Heath K, McClanahan T, Lunceford J, Gause C, et
al: Safety and clinical activity of pembrolizumab for treatment of
recurrent or metastatic squamous cell carcinoma of the head and
neck (KEYNOTE-012): An open-label, multicentre, phase 1b trial.
Lancet Oncol. 17:956–965. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Plimack ER, Bellmunt J, Gupta S, Berger R,
Chow LQ, Juco J, Lunceford J, Saraf S, Perini RF and O'Donnell PH:
Safety and activity of pembrolizumab in patients with locally
advanced or metastatic urothelial cancer (KEYNOTE-012): A
non-randomised, open-label, phase 1b study. Lancet Oncol.
18:212–220. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chow LQM, Haddad R, Gupta S, Mahipal A,
Mehra R, Tahara M, Berger R, Eder JP, Burtness B, Lee SH, et al:
Antitumor activity of pembrolizumab in biomarker-unselected
patients with recurrent and/or metastatic head and neck squamous
cell carcinoma: Results from the phase Ib KEYNOTE-012 expansion
cohort. J Clin Oncol. 34:3838–3845. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Liedtke C, Mazouni C, Hess KR, André F,
Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B,
Green M, et al: Response to Neoadjuvant therapy and Long-term
survival in patients with triple-negative breast cancer. J Clin
Oncol. 26:1275–1281. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Reck M, Rodriguez-Abreu D, Robinson AG,
Hui R, Csőszi T, Fülöp A, Gottfried M, Peled N, Tafreshi A, Cuffe
S, et al: Pembrolizumab versus chemotherapy for PD-L1-positive
non-small-cell lung cancer. N Engl J Med. 375:1823–1833. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Herbst RS, Baas P, Kim DW, Felip E,
Pérez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, et al:
Pembrolizumab versus docetaxel for previously treated,
PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010):
A randomised controlled trial. Lancet. 387:1540–1550. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Carbone DP, Reck M, Paz-Ares L, Creelan B,
Horn L, Steins M, Felip E, van den Heuvel MM, Ciuleanu TE, Badin F,
et al: First-line nivolumab in stage IV or recurrent non-small-cell
lung cancer. N Engl J Med. 376:2415–2426. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Diem S, Hasan Ali O, Ackermann CJ, Bomze
D, Koelzer VH, Jochum W, Speiser DE, Mertz KD and Flatz L: Tumor
infiltrating lymphocytes in lymph node metastases of stage III
melanoma correspond to response and survival in nine patients
treated with ipilimumab at the time of stage IV disease. Cancer
Immunol Immunother. 67:39–45. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hugo W, Zaretsky JM, Sun L, Song C, Moreno
BH, Hu-Lieskovan S, Berent-Maoz B, Pang J, Chmielowski B, Cherry G,
et al: Genomic and transcriptomic features of response to Anti-PD-1
therapy in metastatic melanoma. Cell. 165:35–44. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Connor AA, Denroche RE, Jang GH, Timms L,
Kalimuthu SN, Selander I, McPherson T, Wilson GW, Chan-Seng-Yue MA,
Borozan I, et al: Association of distinct mutational signatures
with correlates of increased immune activity in pancreatic ductal
adenocarcinoma. JAMA Oncol. 3:774–783. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gibney GT, Weiner LM and Atkins MB:
Predictive biomarkers for checkpoint inhibitor-based immunotherapy.
Lancet. 17:e542–e551. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Van Allen EM, Miao D, Schilling B, Shukla
SA, Blank C, Zimmer L, Sucker A, Hillen U, Foppen MHG, Goldinger
SM, et al: Genomic correlates of response to CTLA-4 blockade in
metastatic melanoma. Science. 350:207–211. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Shah SP, Roth A, Goya R, Oloumi A, Ha G,
Zhao Y, Turashvili G, Ding J, Tse K, Haffari G, et al: The clonal
and mutational evolution spectrum of primary triple-negative breast
cancers. Nature. 486:395–399. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cancer Genome Atlas Network: Comprehensive
molecular portraits of human breast tumours. Nature. 490:61–70.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
R Core Team, . R: A language and
environment for statistical computing. R Foundation for Statistical
Computing; Vienna, Austria: 2012, ISBN 3-900051-07-0. http://www.R-project.org/
|
|
28
|
RStudio Team, . RStudio: Integrated
development for R. RStudio, Inc.; Boston, MA: 2015, http://www.rstudio.com/
|
|
29
|
Nagy A, Lanczky A, Menyhart O and Győrffy
B: Validation of miRNA prognostic power in hepatocellular carcinoma
using expression data of independent datasets. Sci Rep. 8:92272018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yarchoan M, Johnson BA III, Lutz ER,
Laheru DA and Jaffee EM: Targeting neoantigens to augment
antitumour immunity. Nat Rev Cancer. 17:5692017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Finotello F and Trajanoski Z: Quantifying
tumor-infiltrating immune cells from transcriptomics data. Cancer
Immunol Immunother. 67:1031–1040. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bagley SJ, Hwang WT, Brem S, Linette GP,
O'Rourke DM and Desai AS: RNA-seq for identification of
therapeutically targetable determinants of immune activation in
human glioblastoma. J Neurooncol. 141:95–102. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mahmoud SM, Paish EC, Powe DG, Macmillan
RD, Grainge MJ, Lee AH, Ellis IO and Green AR: Tumor-infiltrating
CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin
Oncol. 29:1949–1955. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Pan S, Zhan Y, Chen X, Wu B and Liu B:
Bladder cancer exhibiting high immune infiltration shows the lowest
response rate to immune checkpoint inhibitors. Front Oncol.
9:11012019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ayers M, Lunceford J, Nebozhyn M, Murphy
E, Loboda A, Kaufman DR, Albright A, Cheng JD, Kang SP, Shankaran
V, et al: IFN-γ-related mRNA profile predicts clinical response to
PD-1 blockade. J Clin Invest. 127:2930–2940. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Havel JJ, Chowell D and Chan TA: The
evolving landscape of biomarkers for checkpoint inhibitor
immunotherapy. Nat Rev Cancer. 19:133–150. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sharma P, Retz M, Siefker-Radtke A, Baron
A, Necchi A, Bedke J, Plimack ER, Vaena D, Grimm MO, Bracarda S, et
al: Nivolumab in metastatic urothelial carcinoma after platinum
therapy (CheckMate 275): A multicentre, single-arm, phase 2 trial.
Lancet Oncol. 18:312–322. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Carbognin L, Pilotto S, Milella M, Vaccaro
V, Brunelli M, Caliò A, Cuppone F, Sperduti I, Giannarelli D,
Chilosi M, et al: Differential activity of nivolumab, pembrolizumab
and MPDL3280A according to the tumor expression of programmed
death-ligand-1 (PD-L1): Sensitivity analysis of trials in melanoma,
lung and genitourinary cancers. PLoS One. 10:e01301422015.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Taube JM, Klein A, Brahmer JR, Xu H, Pan
X, Kim JH, Chen L, Pardoll DM, Topalian SL and Anders RA:
Association of PD-1, PD-1 ligands and other features of the tumor
immune microenvironment with response to anti-PD-1 therapy. Clin
Cancer Res. 20:5064–5074. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Watson IR, Takahashi K, Futreal PA and
Chin L: Emerging patterns of somatic mutations in cancer. Nat Rev
Genet. 14:703–718. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gubin MM, Zhang X, Schuster H, Caron E,
Ward JP, Noguchi T, Ivanova Y, Hundal J, Arthur CD, Krebber WJ, et
al: Checkpoint blockade cancer immunotherapy targets
tumour-specific mutant antigens. Nature. 515:577–581. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Schon K and Tischkowitz M: Clinical
implications of germline mutations in breast cancer: TP53. Breast
Cancer Res Treat. 167:417–423. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Silwal-Pandit L, Vollan HK, Chin SF, Rueda
OM, McKinney S, Osako T, Quigley DA, Kristensen VN, Aparicio S,
Børresen-Dale AL, et al: TP53 mutation spectrum in breast cancer is
subtype specific and has distinct prognostic relevance. Clin Cancer
Res. 20:3569–3580. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Takeshita T, Yamamoto Y, Yamamoto-Ibusuki
M, Inao T, Sueta A, Fujiwara S, Omoto Y and Iwase H: Prognostic
role of PIK3CA mutations of cell-free DNA in early-stage triple
negative breast cancer. Cancer Sci. 106:1582–1589. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Black JD, Lopez S, Cocco E, Bellone S,
Altwerger G, Schwab CL, English DP, Bonazzoli E, Predolini F,
Ferrari F, et al: PIK3CA oncogenic mutations represent a major
mechanism of resistance to trastuzumab in HER2/neu overexpressing
uterine serous carcinomas. Br J Cancer. 113:1020–1026. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Van Keymeulen A, Lee MY, Ousset M, Brohée
S, Rorive S, Giraddi RR, Wuidart A, Bouvencourt G, Dubois C, Salmon
I, et al: Reactivation of multipotency by oncogenic PIK3CA induces
breast tumour heterogeneity. Nature. 525:119–123. 2015. View Article : Google Scholar : PubMed/NCBI
|