Introduction
Studies conducted in real and simulated microgravity
(SMG) have demonstrated that the physiological functions of living
organisms undergo substantial changes in different gravitational
conditions (1,2). These changes may have adverse effects,
including degenerative changes to bone and muscle, cephalic fluid
shifts and electrolyte disturbances, and dysfunction of the immune
and cardiovascular system (3,4). Based
on these studies, the influence of real and SMG on human
macroscopic tissue is relatively clear; however, the influence of
these conditions on cells, especially cancer cells, requires
further investigation.
The effect of real and SMG on different cancer cells
has been previously studied (5–10) and
alterations primiarly involved the morphological structure and
physiological function. For example, compared with the 2D monolayer
structure of cancer cells under normal gravity (NG), cells are more
rounded and form complex 3D spheroid structures under SMG (5–7).
Furthermore, G2/M and G2+M phases are key
mitotic check points, which are increased under SMG (8) and decreased proliferation and
increaseed apoptosis are also observed under decreased SMG
(9,10).
The influence of metabolism on cancer cells, which
functions in the synthesis of various cell substances such as cell
membrane, is of interest in the field of cancer. Under
physiological conditions, oxidative phosphorylation is the primary
process that generates ATP and glycolysis is dominant only when
oxygen is low; however, the opposite is observed in tumor cells
(11,12). This ability of tumor cells to undergo
glycolysis, even under aerobic conditions, is referred to as the
Warburg effect (11), and the
metabolic reprogramming of several tumor characteristics involved
has been previously investigated, including increased ATP synthesis
and uncontrolled tumor growth (13).
Previous studies have demonstrated that the levels of lactic acid
were increased and glucose levels decreased in gastric cancer
tissues compared with the control group (14,15). The
high levels of lactate may be due to the Warburg effect (11), whereas the low glucose levels may be
due to the elevated fructose-6-phosphokinase activity (16), high levels of glucose transporters
(17) and increased type II
hexokinase activity (18) in gastric
cancer tissues. High activity levels of pyruvate kinase and lactate
dehydrogenase are associated with cancer proliferation and poor
prognosis (19,20), whereas their downregulation in
vitro can impair tumor invasion (21,22).
Based on these reports, several studies have investigated the
influence of normal gravity on physiology and metabolism of cancer
(23–25); however, the effect of gravity
metabolism on cells, especially gastric cancer cells, is poorly
understood.
Previous studies investigating MDA-MB-231 and MCF-7
breast cancer cells have reported changes in energy metabolism and
increases in intracellular lactic acid and lactate dehydrogenase
activity (26). Metabolomic analysis
revealed several metabolic pathways affected and a number of
pathways involved in glycometabolism were significantly influenced
under SMG, including glycolysis, Kreb's cycle, the pentose
phosphate pathway, and the glycerol-phosphate and the
malate-aspartate shuttles. The following results were observed: The
glycolysis pathway was stimulated by increased levels of
glucose-6-phosphate and other glycolytic precursors, such as
3-phosphoglyceraldehyde and 1,3-diphosphoglyceric acid; the Kreb's
cycle was activated by the accumulation of acetyl-CoA and the
content of acyl-carnitine was decreased under SMG, reflected by
increased acyl-CoA levels, which suggests that the β-oxidation
pathway was decreased (27). Thus,
to demonstrate the effects of SMG on the metabolism of HGC-27
gastric cancer cells in the present study, liquid
chromatography-mass spectrometry (LC-MS) was used.
The present study aimed to improve the understanding
of the physiology and pathology of gastric cancer cells under SMG.
The metabolomics analysis of HGC-27 cells under SMG may promote
further understanding of the regularity of tumor occurrence and the
development and changes in physiological function, to provide a
novel therapeutic strategy for gastric cancer.
Materials and methods
Cell culture
The gastric cancer cell line HGC-27 was purchased
from the BeNa Culture Collection. Cells were cultured in RPMI 1640
medium and supplemented with 10% fetal bovine serum (both Thermo
Fisher Scientific, Inc), 100 units/ml penicillin and 100 mg/ml
streptomycin (Gibco; Thermo Fisher Scientific, Inc) and were
incubated at 37°C with 5% CO2. The medium was changed
three times a week.
Microgravity simulation
The RCCS bioreactor (Synthecon, Inc.) was developed
by the National Aeronautics and Space Administration to simulate
the effects of microgravity. A total of 12 bioreactors were used
(total volume, 55 ml), each equipped with a gas-exchange membrane
and incubated at 37°C with 5% CO2. The bottom of the
RCCS bioreactor was designed with a silicone membrane and prevented
the formation of bubbles (28).
Cells in the RCCS bioreactor were grown on cytodex-3 microcarrier
beads (Sigma-Alrich; Merck KGaA) to provide a solid support
pretreated with phosphate buffered saline (PBS) and 75% ethanol,
and stored at 4°C. After washing cytodex-3 microcarrier beads three
times with PBS, the beads were added to the rotating culture
vessel. Subsequently, 7×106 HGC-27 cells with 250 mg
cytodex-3 microcarrier beads were seeded into a 55 ml RCCS
bioreactor containing 500 ml of RPMI-1640 complete medium (Gibco;
Thermo Fisher Scientific, Inc.), and all air bubbles were removed
using a 5 ml syringe. The rotational speed of the high aspect ratio
vessel was 0.01 × g. Control groups (NG) of 1 g static cultures
were stored in the same incubator at 37°C with 5% CO2.
Both groups were cultured in the RCCS bioreactor for 1 and 3 days,
respectively.
Sample preparation and treatment
The cell-microcarrier complexes were washed with PBS
three times. A total of 4 ml Trypsin (0.25% EDTA) was added at 37°C
for 10 min and the cells were dislodged by intermittently tapping
the flask against a hard surface. This reaction was terminated by
adding 500 ml of RPMI-1640 complete medium followed by
centrifugation at 167.7 × g for 5 min at 37°C. The suspension was
obtained by filtering the mixture of cells and microcarriers with
70 µm cell sieves. The control group was washed twice using PBS,
with the addition of 2–3 ml 0.25% Trypsin-EDTA Solution (Gibco;
Thermo Fisher Scientific, Inc.) at 37°C for 5 min. The supernatant
was discarded following centrifugation at 167.7 × g for 5 min at
37°C. Cells collected from NG and SMG were stored at −80°C for ~1
week, prior to subsequent experimentation.
A total of 7×106 HGC-27 NG and SMG cells
were added to 400 µl cold methanol and the cell pellet was
dislodged using a high flux tissue crusher (MP Biomedicals Co.,
Ltd.) at 4°C. Subsequently, 100 µl of distilled water was added and
ultrasonic extraction (Ningbo Xinzhi Biotechnology Co., Ltd.) was
performed on ice three times (10 min each time).
Analysis of metabolites using LC-
MS
LC-MS was performed using a 100×2.1 mm2
Acquity 1.7 µm C18 column and a ACQUITY Ultra High-Performance
Liquid Chromatography system (both Waters Corporation). The
following conditions were used; Ionization mode, positive/negative;
nitrogen gas temperature, 500°C; nebulizer pressure, 50 psi and
flow rate, 0.40 ml/min. Each sample was analyzed six times and the
scanning range of mass spectrometry was 50–1,000 m/z and the
resolution was 30,000 dpi.
Data processing
MS data matrices were obtained using Progenesis QI
software (version 2.0; Waters Corporation). The data matrices were
imported into SIMCA-P+ software (version 14.0; Sartorius AG) and
unsupervised principal component analysis was used to observe the
overall distribution among samples and the degree of dispersion
between groups and supervised partial least square discriminant
analysis (PLS-DA) was used to distinguish the overall differences
of metabolic profiles among groups. For PLS-DA scores, a variable
importance (VIP) value >1 was considered to indicate a
statistically significant difference, whereas R2Y and Q2>0.5
were considered to indicate a strong prediction capability. The
Human Metabolme (HMDB; http://www.hmdb.ca) and the Kyoto Encyclopedia of
Genes and Genomes (KEGG; http://www.kegg.jp) databases were used to identify
potential metabolites.
Statistical analysis
Statistical analysis was performed using SPSS
software version 21.0 (IBM Corp.). Data are expressed as the mean ±
standard deviation for continuous variables and were analyzed using
an independent sample t-test or one-way ANOVA, followed by Tukey's
post-hoc test. P<0.05 was considered to indicate a statistically
significant difference. All experiments were performed in
triplicate.
Results
Metabolic alterations of HGC-27 cells
under NG and SMG
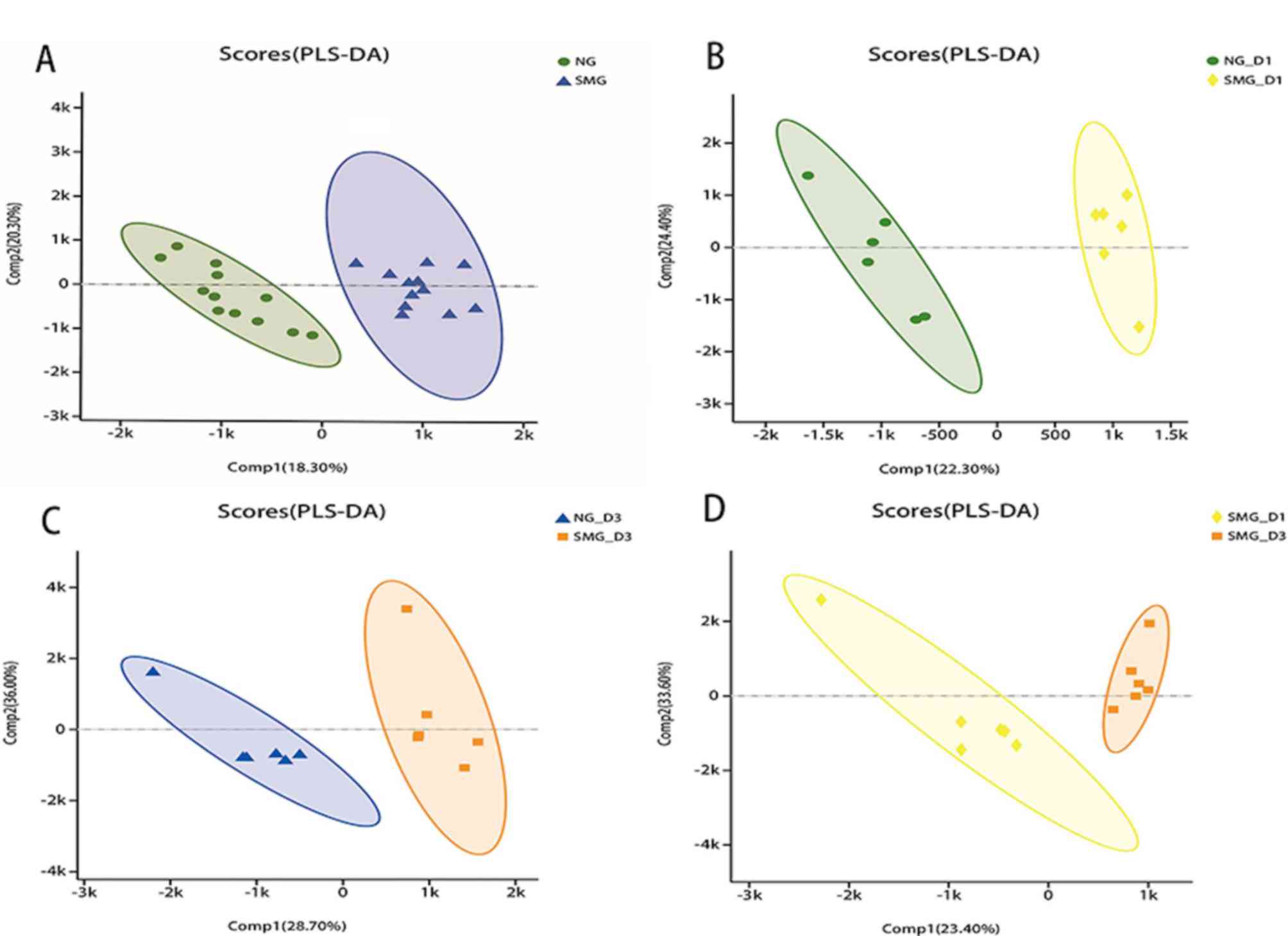
The PLS-DA scores in HGC-27 cells under NG and SMG
are presented in Fig. 1. The value
of the parameters R2Y and Q2 are >0.5,
which suggests that the model was good and that the prediction
capability was strong. The greater the separation degree between
the two groups, the more significant the classification effect.
Comp1 refers to the first principal component interpretation degree
and Comp2 refers to the second principal component interpretation
degree. The metabolites of NG and SMG cells were grouped,
indicating that there was a difference in metabolites between the
two groups. A total of 67 differentially regulated metabolites were
identified, including 36 upregulated and 31 downregulated
metabolites (all P<0.05, VIP>1). Compared with the NG group,
phosphatidyl ethanolamine (PE), phosphatidyl choline (PC),
arachidonic acid and sphinganine were significantly upregulated in
the SMG group, whereas sphingomyelin (SM), phosphatidyl serine
(PS), phosphatidic acid (PA), L-Proline, creatine, pantothenic
acid, oxidized glutathione (GSSG), adenosine diphosphate (ADP) and
adenosine triphosphate (ATP) were significantly downregulated.
Lipids and lipid-like metabolite
alterations of HGC-27 cells in NG and SMG
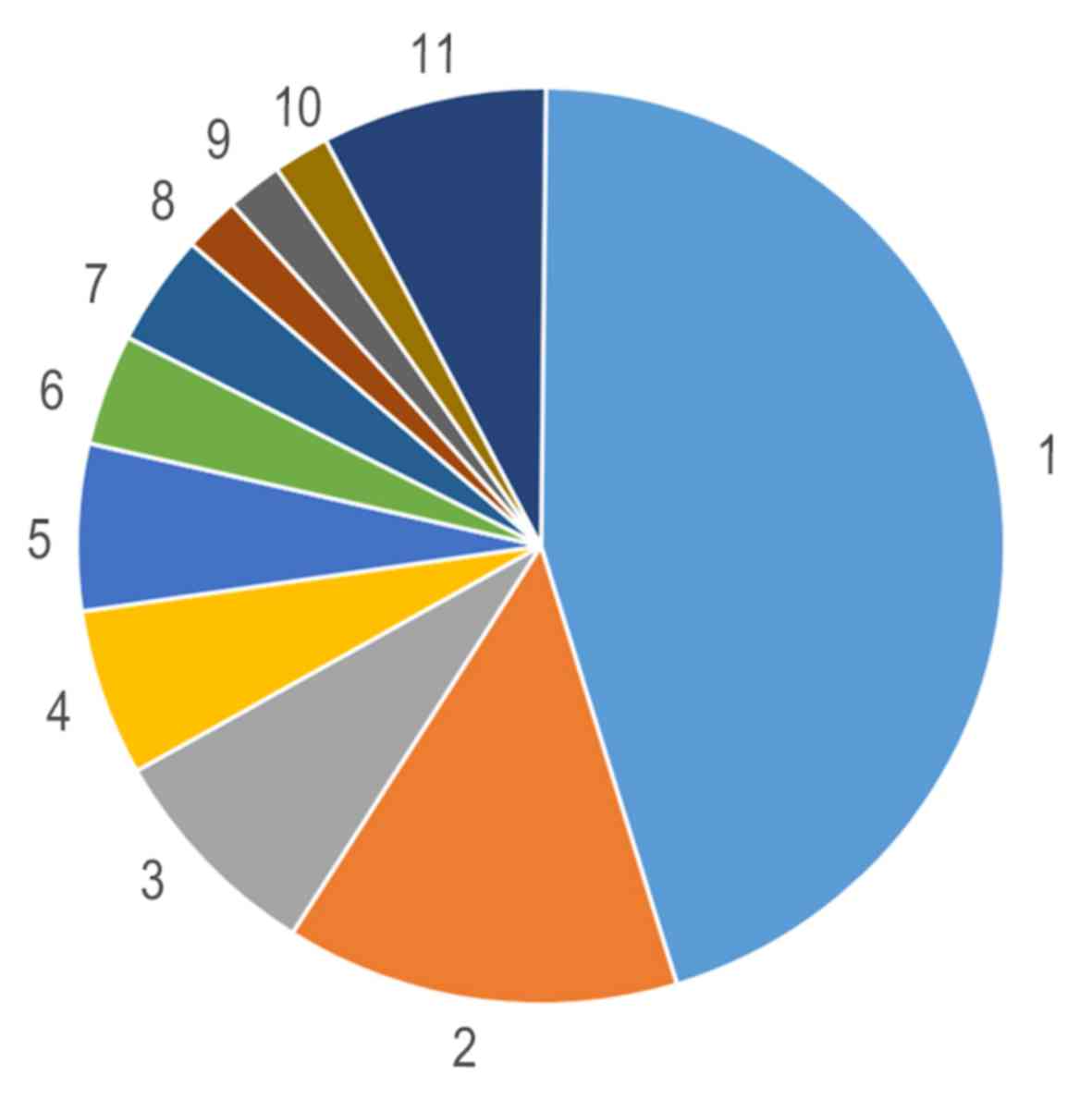
The HMDB method in LC-MS was used to assess compound
classification of HGC-27 cells. Compared with the NG groups, HMDB
compound analysis confirmed that glyceropholipids (45.10%) and
fatty acids (13.73%) were the most affected by SMG, followed by
nucleotides (Fig. 2). Of the 67
metabolites, LC-MS/MS profiling of HGC-27 cells detected 50 lipid
molecules, including 31 phospholipids and 7 sphingolipids, which
were upregulated in SMG (Table I).
These results suggest that these two types of lipids exhibited
special biological behaviors in HGC-27 cells under SMG.
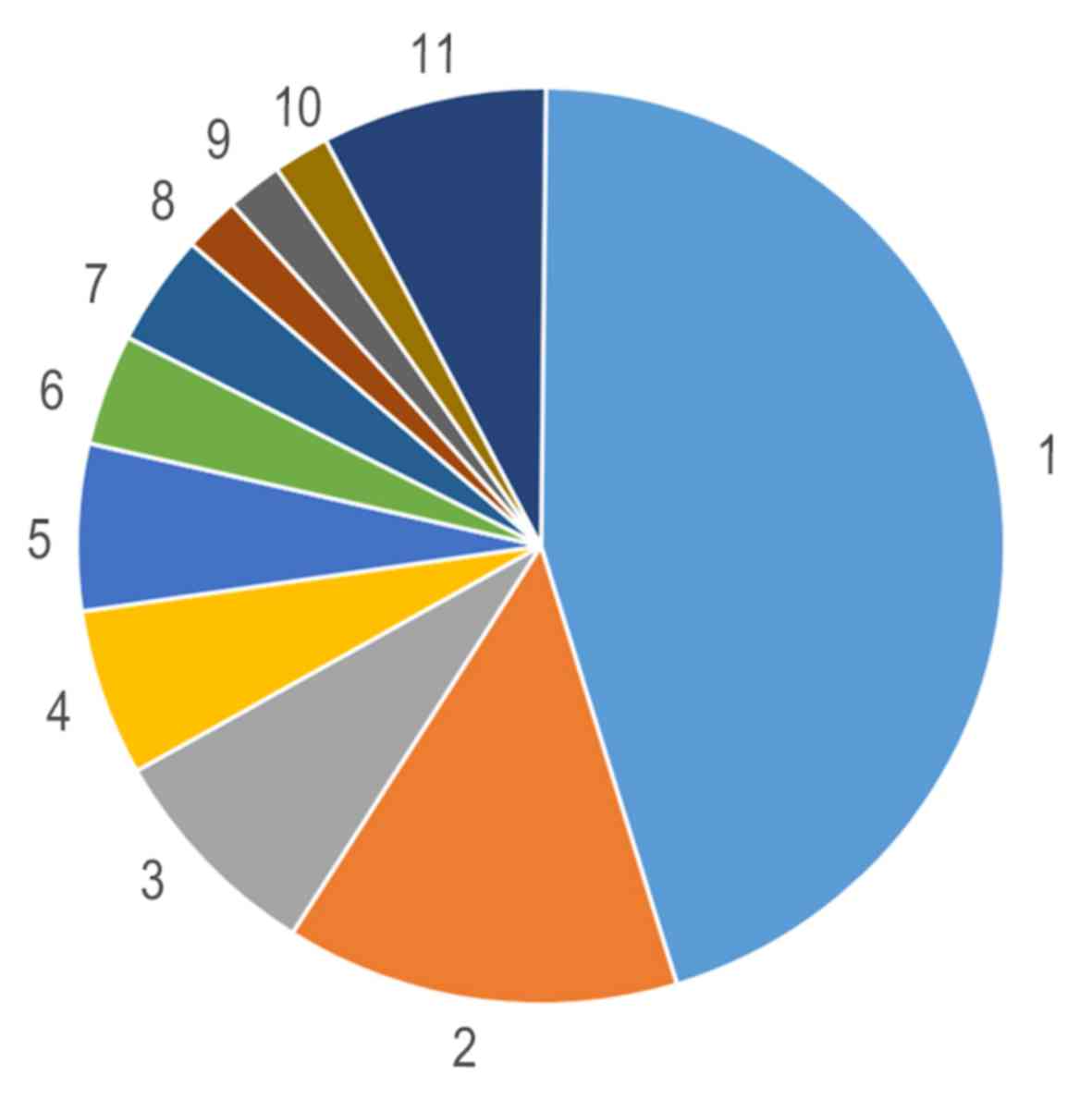 | Figure 2.Human Metabolme Database compound
classification analysis of the significantly altered metabolites
indicating that lipids were the mo st influenced metabolite under
simulated microgravity. 1, Glycerophospholipids (45.1%); 2, Fatty
Acids (13.73%); 3, Carboxylic acids and derivatives (7.84%); 4,
Prenol lipids (5.88%); 5, Sphingolipids (5.88%); 6, Organonitrogen
Compounds (3.92%); 7, Organooxygen compounds (3.92%); 8, Alcohols
and polyols (1.96%); 9, Carbonyl compounds (1.96%); 10, Flavonoids
(1.96%) and 11, Others (7.85%). |
 | Table I.Quantitated lipid classes and numbers
in HGC-27 cells under normal gravity and simulated
microgravity. |
Table I.
Quantitated lipid classes and numbers
in HGC-27 cells under normal gravity and simulated
microgravity.
| Lipid category | Lipid class | Number of lipid
species |
|---|
| Phospholipid |
Phosphatidylcholine | 13 |
|
|
Lysophospholipid | 1 |
|
|
Glycerophosphocholine | 1 |
|
|
Phosphatidylethanolamine | 12 |
|
|
Phosphatidylserine | 3 |
|
| Phosphatidic
acid | 1 |
| Sphingolipid | Sphingomyelin | 2 |
|
| Sphinganine | 1 |
|
| Oleamide | 1 |
|
| Linoleamide | 1 |
|
|
Dihydroceramide | 1 |
|
|
Lactosylceramide | 1 |
| Glycerolipide | Glycinoprenol
9 | 1 |
| Other lipids | Umbelliprenin | 1 |
|
| Sorbitan
stearate | 1 |
|
| Pantothenic
Acid | 1 |
|
|
Oleoylcarnitine | 1 |
|
| Isobutyryl
carnitine | 1 |
|
| Glycocholic
acid | 1 |
|
| Camelliagenin
B | 1 |
|
| Arachidonic
acid | 1 |
|
|
8-Hydroxyguanosine | 1 |
|
|
3-Hydroxyhexadecanoyl carnitine | 1 |
|
|
2-Methylbutyroylcarnitine | 1 |
| Total lipids |
| 50 |
A total of 38 significantly affected lipids,
particularly phospholipids and sphingolipids, were observed, which
characterized the differences between NG and SMG (VIP >1).
Detailed information concerning these lipids is presented in
Table II. Of these 38 lipids, 25
were upregulated and 13 were downregulated. The two predominant
downregulated lipid classes detected in SMG were SM and PS. It was
showed that PS [DiMe (11,3)/MonoMe (11,5)], PS
[18:3 (9Z,12Z,15Z)/22:1(13Z)], PS [14:1 (9Z)/24:0)],
PA[16:0/18:1(11Z)], SM (d18:0/16:1(9Z) and SM (d18: +B5:G321/14:0)
levels significantly decreased, whereas Sphinganine,
lactosylceramide (d18:1/12:0) and dihydroceramide levels increased
under SMG.
 | Table II.Identification of the significantly
altered metabolites in HGC-27 cells. |
Table II.
Identification of the significantly
altered metabolites in HGC-27 cells.
| Metabolite | Formula | M/Z | P-value | Regulation | VIP |
|---|
| SM
(d18:+B5:G321/14:0) |
C37H75N2O6P | 719,5313 |
8.951×10−6 | Downregulated | 1,5850 |
| SM
[d18:0/16:1(9Z)] |
C39H79N2O6P | 747,5634 |
2.004×10−2 | Downregulated | 1,8047 |
| PS
[DiMe(11,3)/MonoMe(11,5)] |
C47H80NO12P | 918,4877 |
1.500×10−8 | Downregulated | 1,1943 |
| PS
[18:3(9Z,12Z,15Z)/22:1(13Z)] |
C46H82NO10P | 822,5620 |
9.948×10−3 | Downregulated | 1,2988 |
| PS
[14:1(9Z)/24:0] |
C44H84NO10P | 800,5760 |
1.440×10−7 | Downregulated | 3,0884 |
| PE-NMe2
[14:1(9Z)/16:1(9Z)] |
C37H70NO8P | 732,4793 |
2.400×10−8 | Downregulated | 3,9878 |
| PE-NMe
[14:1(9Z)/16:1(9Z)] |
C36H68NO8P | 718,4649 |
4.190×10−6 | Downregulated | 1,0028 |
| PE
(15:0/P-16:0) |
C36H72NO7P | 706,4990 |
1.223×10−6 | Upregulated | 1,8137 |
| PE
[15:0/24:1(15Z)] |
C44H86NO8P | 832,6037 |
4.555×10−3 | Upregulated | 1,3361 |
| PE
[15:0/22:5(4Z,7Z,10Z,13Z,16Z)] |
C42H74NO8P | 796,5100 |
7.155×10−4 | Upregulated | 1,4220 |
| PE
[15:0/22:4(7Z,10Z,13Z,16Z)] |
C42H76NO8P | 798,5255 |
2.232×10−2 | Upregulated | 1,3835 |
| PE
[15:0/22:2(13Z,16Z)] |
C42H80NO8P | 802,5564 |
1.816×10−2 | Downregulated | 2,8050 |
| PE
[15:0/22:1(13Z)] |
C42H82NO8P | 804,5728 |
7.846×10−5 | Upregulated | 4,1810 |
| PE
[15:0/20:2(11Z,14Z)] |
C40H76NO8P | 774,5259 |
9.433×10−6 | Downregulated | 8,3376 |
| PE
[15:0/18:2(9Z,12Z)] |
C38H72NO8P | 746,4948 |
1.153×10−6 | Downregulated | 4,9712 |
| PE
[14:0/24:1(15Z)] |
C43H84NO8P | 818,5870 |
9.771×10−6 | Upregulated | 1,1963 |
| PE
[14:0/20:2(11Z,14Z)] |
C39H74NO8P | 757,5542 |
4.356×10−3 | Downregulated | 2,1212 |
| PC
[o-16:0/20:4(8Z,11Z,14Z,17Z)] |
C44H82NO7P | 812,5771 |
1.832×10−2 | Upregulated | 1,2528 |
| PC
[22:5(4Z,7Z,10Z,13Z,16Z)/16:0] |
C46H82NO8P | 852,5716 |
4.918×10−2 | Upregulated | 2,0817 |
| PC
[22:4(7Z,10Z,13Z,16Z)/14:0] |
C44H80NO8P | 826,5566 |
7.767×10−6 | Upregulated | 3,9909 |
| PC
[18:4(6Z,9Z,12Z,15Z)/P-18:0] |
C44H80NO7P | 810,5616 |
3.320×10−7 | Upregulated | 2,0711 |
| PC
[18:4(6Z,9Z,12Z,15Z)/P-16:0] |
C42H76NO7P | 782,5270 |
1.608×10−5 | Upregulated | 1,0437 |
| PC
[18:1(11Z)/22:6(4Z,7Z,10Z,13Z,16Z,19Z)] |
C48H82NO8P | 876,5722 |
2.134×10−4 | Upregulated | 1,7139 |
| PC
[18:0/20:4(5Z,8Z,11Z,14Z)] |
C46H84NO8P | 854,5879 |
9.655×10−6 | Upregulated | 1,5839 |
| PC
[18:0/18:2(9Z,12Z)] |
C44H84NO8P | 830,5881 |
6.867×10−4 | Upregulated | 2,3650 |
| PC
[16:1(9Z)/20:3(5Z,8Z,11Z)] |
C44H80NO8P | 826,5554 |
1.198×10−4 | Upregulated | 1,5843 |
| PC
[16:1(9Z)/16:1(9Z)] |
C40H76NO8P | 752,5196 |
2.971×10−2 | Downregulated | 4,8632 |
| PC
[16:0/20:5(5Z,8Z,11Z,14Z,17Z)] |
C44H78NO8P | 824,5400 |
9.291×10−3 | Upregulated | 3,4401 |
| PC
[16:0/20:3(5Z,8Z,11Z)] |
C44H82NO8P | 826,5554 |
6.358×10−3 | Upregulated | 1,4770 |
| PC
(16:0/18:3(6Z,9Z,12Z)] |
C42H78NO8P | 800,5412 |
9.244×10−4 | Upregulated | 2,2188 |
| PA
(16:0/18:1(11Z)] |
C37H71O8P | 719,4839 |
4.759×10−6 | Downregulated | 1,2779 |
| LysoPC
[20:4(8Z,11Z,14Z,17Z)] |
C28H50NO7P | 588,3274 |
5.778×10−5 | Upregulated | 1,7989 |
| Sphinganine |
C18H39NO2 | 302,3052 |
6.998×10−3 | Upregulated | 2,7342 |
| Oleamide |
C18H35NO | 563,5495 |
7.274×10−4 | Upregulated | 31,6443 |
| Linoleamide |
C18H33NO | 280,2632 |
1.702×10−2 | Upregulated | 10,9674 |
| Lactosylceramide
(d18:1/12:0) |
C42H79NO13 | 850,5563 |
5.000×10−9 | Upregulated | 3,5254 |
|
Glycerophosphocholine |
C8H20NO6P | 258,1098 |
1.328×10−2 | Upregulated | 1,5225 |
|
Dihydroceramide |
C19H39NO3 | 362,3264 |
2.622×10−2 | Upregulated | 1,9767 |
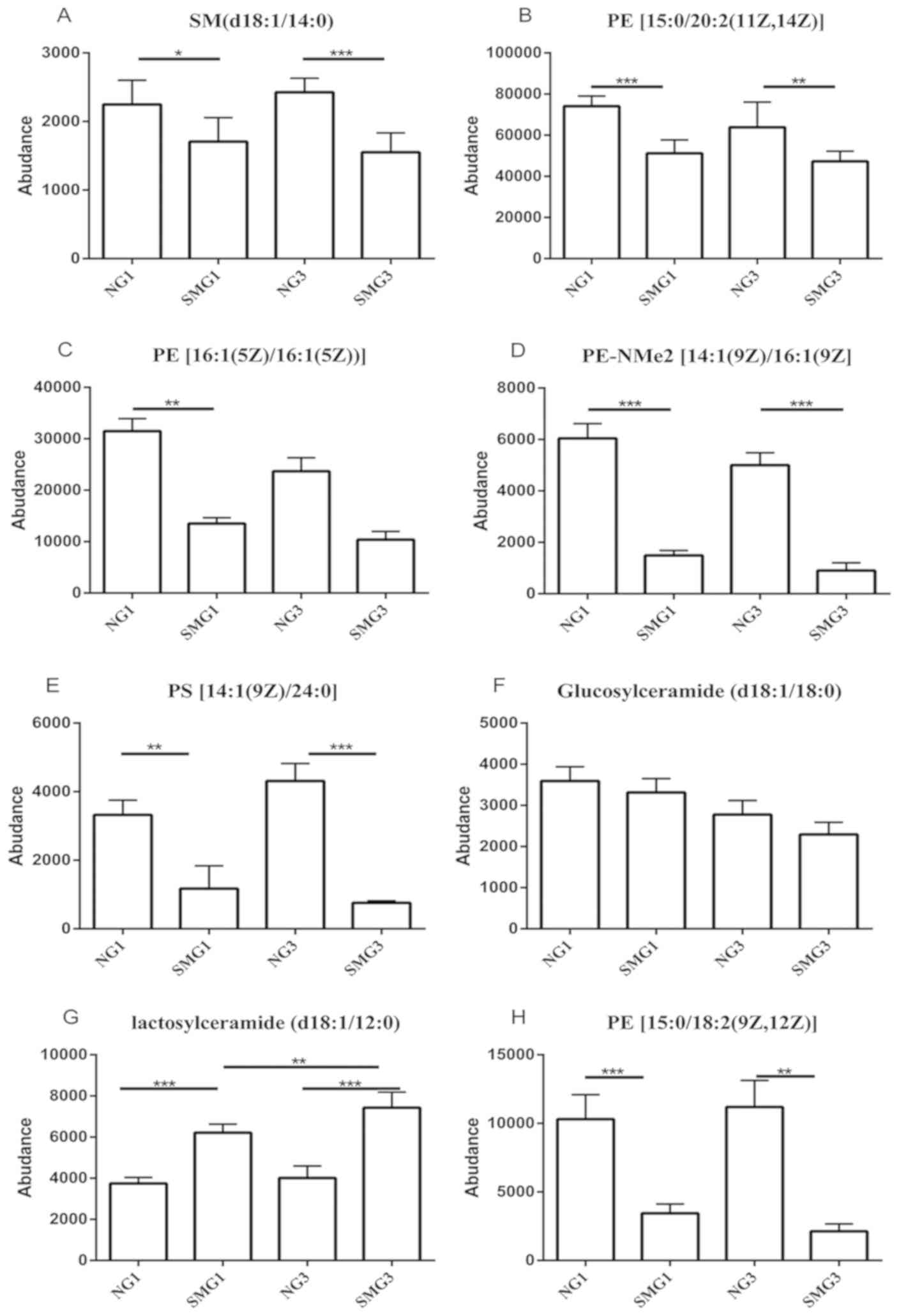
Among the 13 downregulated lipids one class of PS
[14:1(9Z)/24:0] (consisting of one chain of myristoleic acid at the
C-1 position and one chain of lignoceric acid at the C-2 position;
http://www.hmdb.ca/metabolites/HMDB0112319), one class
of SM (d18:1/14:0), three classes of PE, [15:0/18:2(9Z,12Z),
15:0/20:2(11Z,14Z), 16:1(5Z)/16:1(5Z) and PE-NMe2
14:1(9Z)/16:1(9Z)] were downregulated after 1 and 3 days of SMG
compared with the NG group, (P<0.05; Fig. 3). Glucosylceramide (d18:1/18:0) was
downregulated after 1 and 3 days of SMG compared with the NG group,
however there was no statistical significance (P>0.05; Fig. 3). Regarding lactosylceramide
(d18:1/12:0), there was a significant increase after 3 days of SMG
exposure compared with 1 day of SMG (Fig. 3).
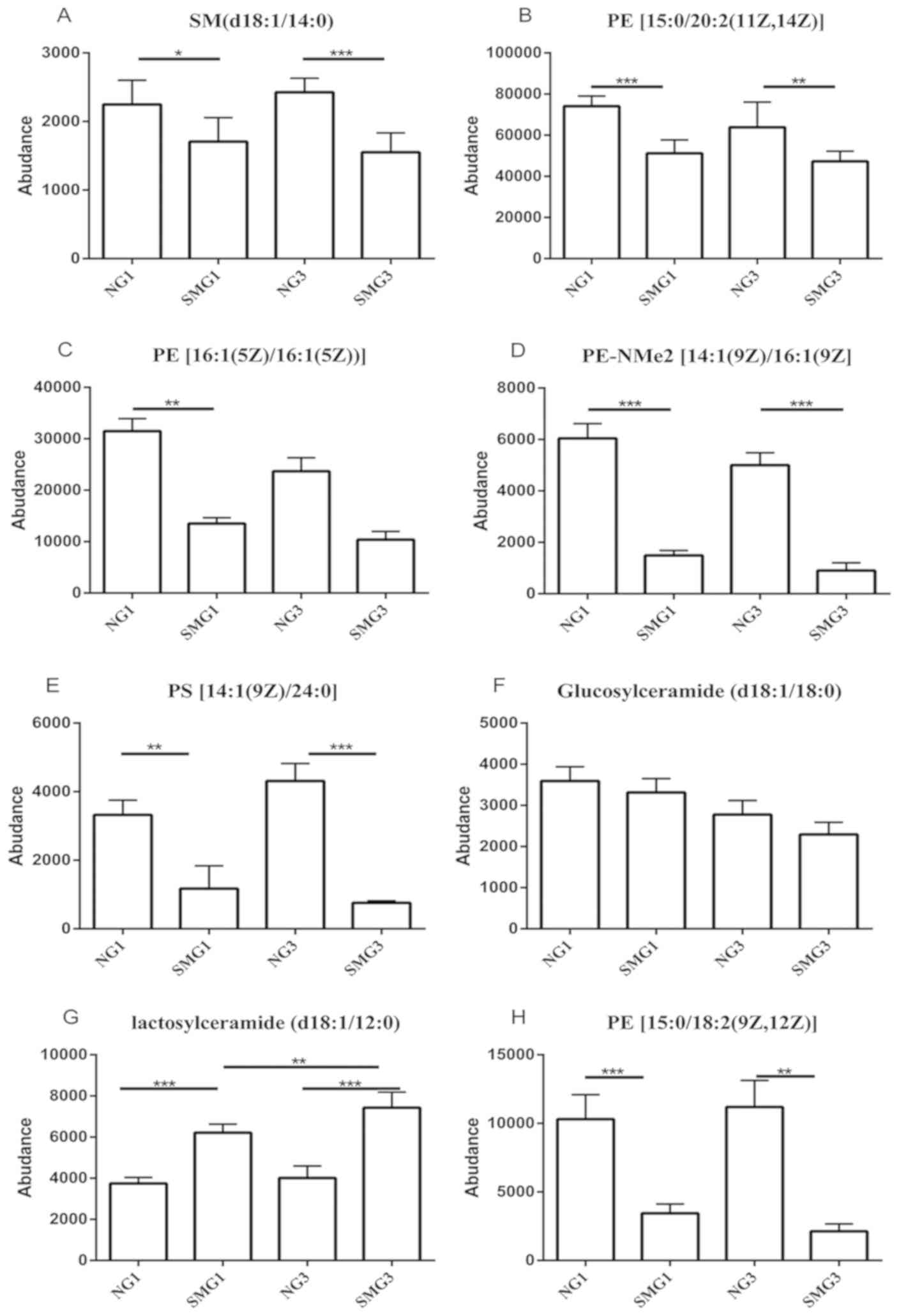 | Figure 3.Effects of SMG on the expression of
(A) SM (d18:1/14:0), (B) PE [15:0/20:2(11Z,14Z)], (C) PE
[16:1(5Z)/16:1(5Z)], (D) PE-NMe2 [14:1(9Z)/16:1(9Z)], (E) PS
[14:1(9Z)/24:0], (F) Glucosylceramide (d18:1/18:0), (G)
Lactosylceramide (d18:1/12:0) and (H) PE [15:0/18:2(9Z,12Z)].
*P<0.05, **P<0.01 and ***P<0.001. NG, normal gravity; SMG,
simulated microgravity; D1, 1 day duration; D3, 3 day duration; PE,
phosphatidyl ethanolamine; SM, sphingomyelin. |
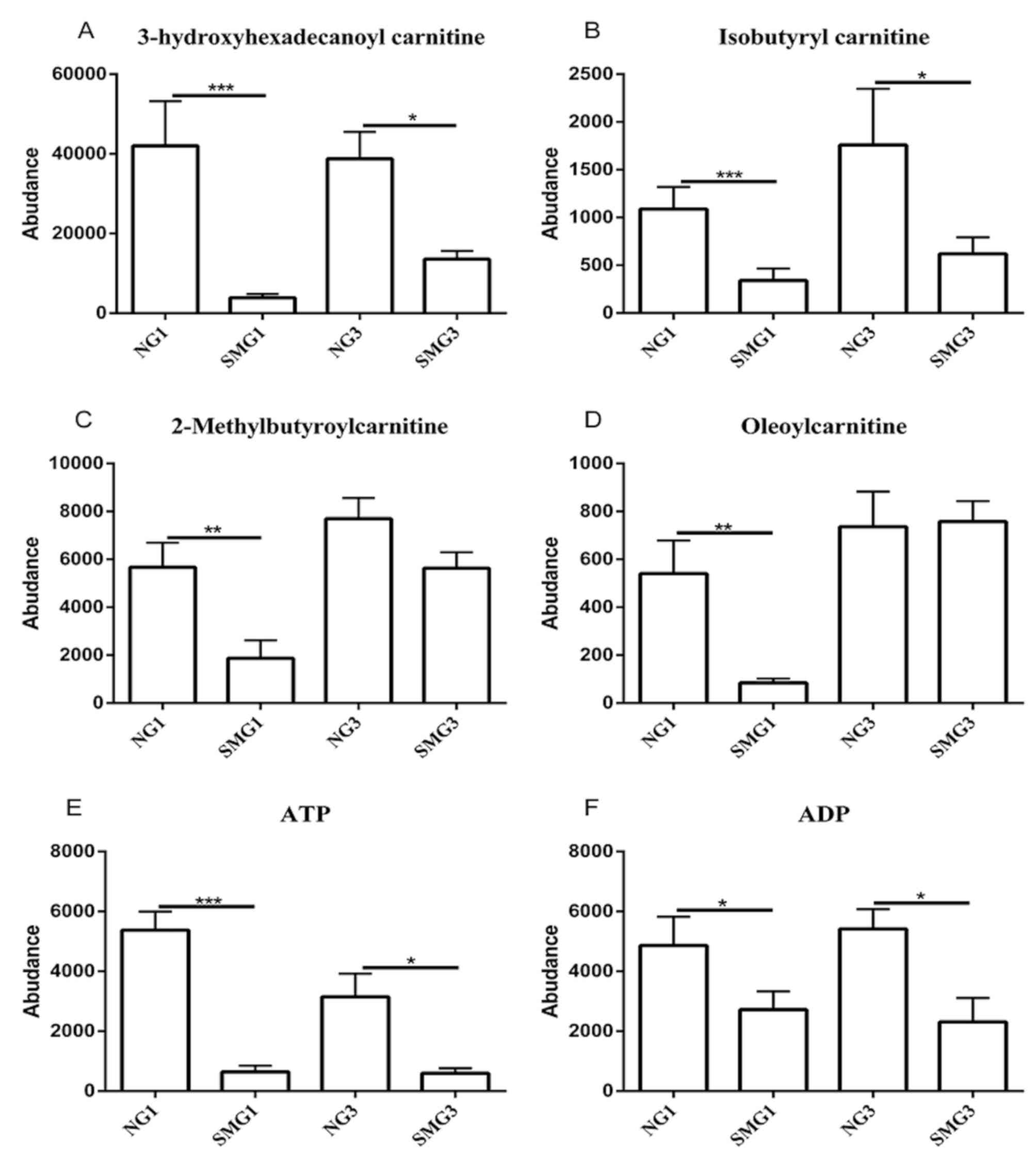
The influence of fatty acid
β-oxidation under SMG
Carnitines, including 3-hydroxyhexadecanoyl
carnitine, 2-methylbutyroylcarnitine, isobutyryl carnitine and
oleoylcarnitine, serve a role in the oxidation of fatty acids to
ATP (29). 3-hydroxyhexadecanoyl
carnitine and isobutyryl carnitine were downregulated after 1 and 3
days of SMG compared with the NG group. However,
2-methylbutyroylcarnitine and oleoylcarnitine were only
downregulated after 1 day of SMG. Furthermore, ATP and ADP were
downregulated after 1 and 3 days of SMG compared with the NG group
(Fig. 4).
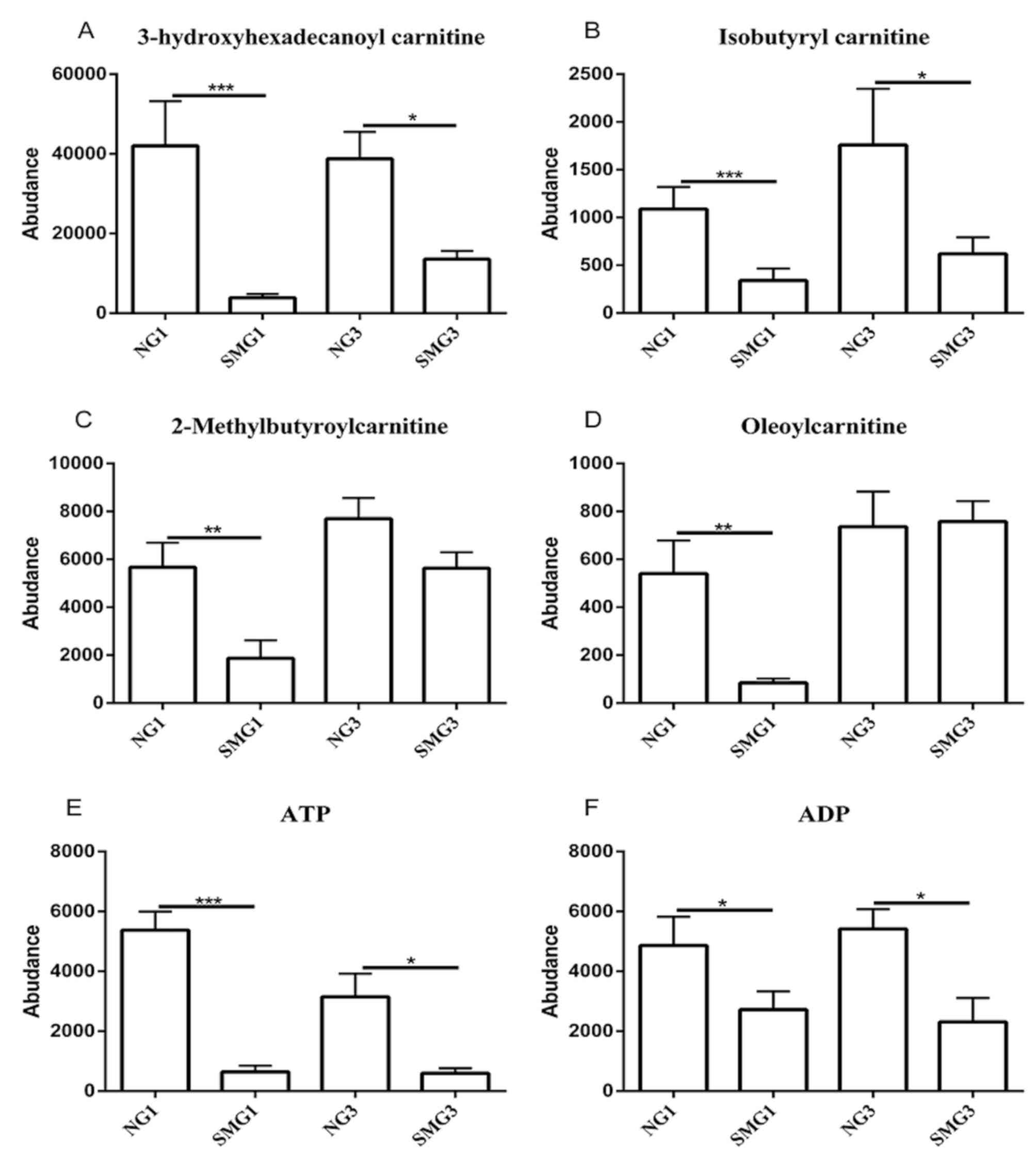 | Figure 4.Effects of SMG on the expression of
(A) 3-hydroxyhexadecanoyl carnitine, (B) Isobutyayl carnitine, (C)
2-Methylbutyroylcarnitine, (D) Oleoylcarbitine, (E) ATP and (F)
ADP. *P<0.05, **P<0.01 and ***P<0.001. NG, normal gravity;
SMG, simulated microgravity; D1, 1 day duration; D3, 3 day
duration; ATP, adenosine triphosphate; ADP, adenosine
diphosphate. |
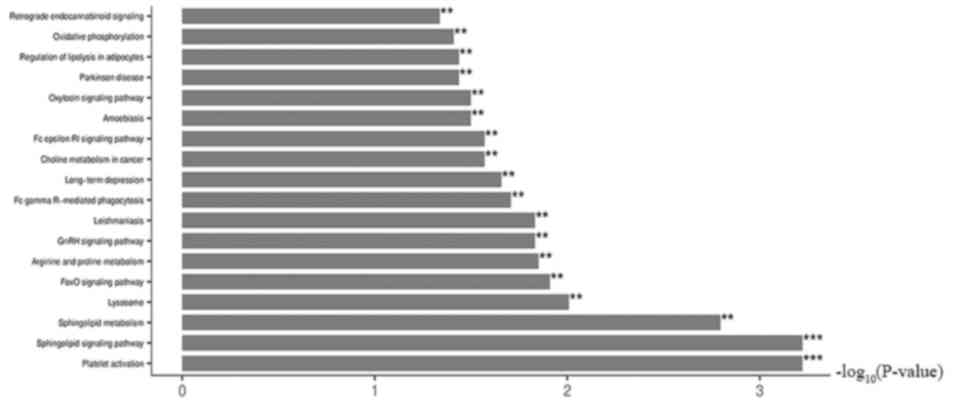
KEGG pathway enrichment analysis
Fig. 5 shows the KEGG
enrichment pathways under SMG. These pathways could be grouped into
six categories: Cellular processes; environmental information
processing; genetic information processing; human diseases;
metabolism; and organismal systems. The results show that SMG
significantly affected multiple pathways and KEGG pathway
enrichment analysis showed that the differentially expressed
metabolites were primarily associated with: Regulation of the
lysosome; ‘FoxO signaling pathway’; ‘leishmaniasis’; ‘GnRH
signaling pathway’; ‘platelet activation’; ‘sphingolipid signaling
pathway’; ‘Fc γ R-mediated phagocytosis’; ‘long-term depression’;
‘sphingolipid metabolism’; and ‘arginine and proline
metabolism’.
Discussion
Several studies have explored the effects of
different durations of NG and SMG on various types of cells,
ranging from a few seconds to dozens of days, reporting notable
effects on different types of cells, including thyroid, colorectal
and breast cancer cells (30–33). In
these studies cellular morphology was significantly altered (3D
spheroid structure formation and the alteration of the
cytoskeleton), the extracellular matrix (ECM) was increased, the
cell cycle was modified after 10 and 12 days of SMG (the number of
cells in the G1 phase increased, whilst the number of
cells in the S and G2/M phases decreased), proliferation
capacity was decreased and apoptosis was increased (30,31). The
clear alteration of physiological functions of different human
cancer cells were observed in our previous study (34). Chen et al (26) reported that different types of tumor
can reprogram their metabolic processes to fulfill particular
demands after 5 days of SMG, including processes involved in cancer
cell proliferation, metastasis, immunological escape and survival,
and shifting the aggressive phenotype of cancer cells. This
metabolic reprogramming is regarded as a novel characteristic of
tumors (35). Chen et al
(26) also proposed a novel point to
understand the Warburg effect in MDA-MB-231 and MCF-7 breast cancer
cells. Glycolysis is often induced by hypoxia; however, glycolysis
can also be induced by high levels of adrenomedullin under SMG,
which may be a novel mechanism inducing glycolysis. However, to the
best of our knowledge, the exact molecular mechanism of this
reprogramming in tumor cells remains unknown under SMG.
A previous study reported that 72 h exposure to SMG
induces changes in morphology, proliferation, cell cycle
distribution and apoptosis in human SGC-7901 gastric cancer cells
(36). Thus, the present study
investigated whether 1 and 3 days exposure to SMG could influence
the metabolites of human HGC-27 gastric cancer cells. Previous
studies have demonstrated that SMG influences several metabolic
pathways, stimulates lipid metabolism and interrupting the Krebs
cycle in human breast cancer cells, osteoblast and oligodendrocyte
after 5 d, 110 h and 3 d of SMG, respectively (26,27,37).
The present study demonstrated that SMG
significantly affected HGC-27 human gastric cancer cells in a
number of processes, in particular lipid metabolism. HGC-27 cells
are highly malignant tumor cells (38). Reprograming lipid metabolism is
associated with cancer invasion and metastasis (39); however, the influences of lipid
metabolism on HGC-27 cells remains unclear. In the present study,
HGC-27 lipid metabolites were measured using LC-MS and, to the best
of our knowledge, this is the first study to analyze the alteration
of lipid metabolic profiles of gastric cancer cells under SMG. As
evidenced by LC-MS metabolome analysis, it was revealed the
differential expression of 67 metabolites were altered during 1 and
3 days exposure to SMG compared with NG, according to the criteria
of a VIP>1 and P<0.05, suggesting several different
categories of membrane lipid components were affected by SMG. A
total of 50 significantly different lipid metabolites were
identified and 1 and 3 days exposure to SMG significantly increased
the levels of PE, PC, arachidonic acid and sphinganine, but
significantly decreased the levels of SM, PS, PA, pantothenic acid,
ADP and ATP (Table I, Fig. 4). These upregulated and downregulated
metabolites are associated with cellular processes, biological
regulation and metabolic processes. These metabolites, altered in
SMG, may have value as markers for the early diagnosis of gastric
cancer.
PC, PE, PS, SM and PA are the primary components of
membrane phospholipids, which play a significant role in cell
membranes (40). A previous study
showed that these phospholipids were upregulated in breast cancer
tissues (41). The high levels of PE
may serve as a biomarker of apoptosis in cancer (42) and PC has been considered as a
biomarker of membrane proliferation in ovarian cancer (43). The present study demonstrated that PE
and PC levels increased under SMG. Previous studies have indicated
that several cancer cell lines, including ML-1 and ONCO-DG1 thyroid
carcinoma cells, SGC-7901 gastric carcinoma cells, U251 glioma
cells and MDA-MB-231 breast cancer cells, exhibit high levels of
apoptosis under SMG after 48, 24, 36, 8 and 72 h of SMG (36,44–47).
These high levels of apoptosis may be due to elevated PC levels,
which indicates high membrane proliferation. These results are
consistent with previous findings that apoptosis in human SGC-7901
gastric cancer cells increase following treatment with SMG after 48
h (36). However, other PEs, such as
PE [15:0/18:2(9Z,12Z)], PE [15:0/20:2(11Z,14Z)], PE
[16:1(5Z)/16:1(5Z)] and PE-NMe2 [14:1(9Z)/16:1(9Z)] were
downegulated after 1 and 3 days of SMG compared with the NG group.
It is hypothesized that PE is an key molecule for the synthesis of
glycosylphosphatidylinositol anchors, which are glycolipids
identified in yeast, protozoa, plants and humans, enabling modified
proteins to be tethered to the outer leaflet of the plasma membrane
necessary for the immune response, cell-cell communication and
embryogenesis (48–51). Failure to attach can lead to
dysfunction in the immune response, cell-cell communication and
embryogenesis. As levels of PE were decreased in HGC-27 cells in
the present study after 1 and 3 days of SMG, an adverse effect,
such as gene mutations associated with cell cycle and apoptosis,
may occur.
Chang et al (52) and Qian et al (53) observed that the invasive ability of
A549 human lung adenocarcinoma and MCF-7 breast cells decreases
following treatment with SMG after 72 h. A previous study reported
that PS is associated with invasion of colorectal cancer cells
(54). In the present study, it was
demonstrated that PS [DiMe (11,3)/MonoMe
(11,5)], PS [18:3 (9Z,12Z,15Z)/22:1(13Z)] and PS
[14:1 (9Z)/24:0)] significantly decreased, suggesting that the the
invasive ability of HGC-27 cells was weakened under SMG. This
indicates that these phospholipids may have value as biomarkers for
metastasis.
SM is located in the plasma membrane of most
mammalian cells, which is the primary component of the pulp. The
metabolic products of SM, including Cer and sphingosine (Sph), are
signalling molecules with biological activity and act as first
and/or second messengers controlling the vital activity of cells,
such as cell growth, differentiation, aging, and apoptosis
(55–57). The present study observed that SM
(d18:0/16:1(9Z) and SM (d18: +B5:G321/14:0) levels were decreased,
whereas Sphinganine, lactosylceramide (d18:1/12:0) and
dihydroceramide levels increased under SMG (Table II). These results suggest that SMG
may decrease the formation of sphingomyelin and increase its
metabolism. Cer and Sph metabolic products function in the
regulation of tumor proliferation and apoptosis, and are negative
regulators of proliferation, which can inhibit cell growth and
promote apoptosis (58). PE and the
metabolic products of SM (Cer and Sph) can contribute to the
increase in apoptosis under SMG (59,60).
Previous studies have demonstrated a decrease in the proliferation
capacity in SGC-7901 gastric cancer cells, U251 glioma cells and
A549 lung adenocarcinoma cells, and increased apoptosis after 12,
48 and 72 h of SMG, respectively (36,47,53).
SM metabolism can regulate the function of K-Ras,
which was the first human oncogene identified in human cancer and
is a member of the Ras superfamily (61). Considering cellular signalling
networks in the Ras-Raf-mitogen-activated protein kinase (MAPK)
pathways, the role of K-Ras is associated with cell physiological
functions, such as proliferation, apoptosis and survival (62). Relevant mutations in pathway
components, such as serine/threonine-protein kinase B-raf,
epidermal growth factor receptor and neurofibromin, are associated
with progression in colon cancer and melanomas (63–65). The
present study demonstrated that PA[16:0/18:1(11Z)] levels were
decreased after SMG compared with the NG group (Table II). This may be associated with the
high levels of phospholipase D2 (PLD2) after 3 days of SMG
(66). PLD2 is an enzyme which
hydrolyzes PA, promoting local invasion by regulating MT1-matrix
metalloproteinase (MMP) (66). Based
on the role of PLD2-generated PA in breast cancer metastasis, PLD2
may be regarded as a potential therapeutic target for metastatic
breast cancer, and as a plasma membrane target (67). MT1-MMP, tethered to the plasma
membrane, is a key protein associated with the migration of cancer
cells (67). PLD2 generates small
lipid molecules, such as phosphatidic acid, which can regulate the
movement of the cytoskeleton, proliferation and migration (68–70).
Therefore, it has been suggested that PLD2 and its small lipid
molecules can regulate MT1-MMP for invasion and metastasis.
However, this result contradicts the data of the present study,
which demonstrates that some lipid levels, including PS
[DiMe(11,3)/MonoMe(11,5)], PS [18:3(9Z,12Z,15Z)/22:1(13Z)] and PS
[14:1(9Z)/24:0], were significantly decreased under SMG, suggesting
that the invasive abilities of HGC-27 cells are weakened under SMG.
It was hypothesized that the environment of cell proliferation may
account for these contradicting results. Furthermore, the different
devices used to simulate microgravity, such as random positioning
machine and RCCS are speculated to account for the alteration in
cell migration; however, further studies are required.
L-Proline, creatine, ADP and ATP levels were
decreased after 1 and 3 days of SMG compared with the NG group in
the present study. The downregulation of L-Proline in HGC-27 cells
under SMG may be due to decreased activation of MMPs and
degradation of the microenvironment for the ECM (71), rather than the degradation of
collagen, which is regulated under conditions of nutrient stress
assoicated with the mTOR signaling pathway, is blocked (72). However, the mTOR pathway participates
in the process of apoptosis and autophagy (73).
The present study demonstrated that
3-hydroxyhexadecanoyl carnitine, 2-methylbutyroylcarnitine,
isobutyryl carnitine and oleoylcarnitine, associated with
β-oxidation, were significantly downregulated under SMG. Creatine
is a key component in muscle contraction and can be transported
between the mitochondria and cellular ATP utilization sites, acting
as a spatial energy buffer (74).
The function of creatine in cancer has been studied, reporting that
some physiological functions of cancer, such as metabolism, are
associated with the creatine kinase system, by regulating ATP
provisions (75). The anticancer
role of creatine has been demonstrated in vitro and in
vivo experimental models (76,77). The
downregulation of creatine, ADP and ATP in present study indicates
that SMG may influence energy metabolism, an important process in
physiological functions, including proliferation, cell cycle,
migration and apoptosis after 5 d of expose (26). ATP is produced primarily in the
mitochondria. SMG may have interferred with the normal
mitochondrial function of HGC-27 gastric cancer cells, which has
been illustrated in skeletal muscle tissue and cardiomyocytes
(78,79). Mitochondrial function alteration
might be an adaptive response for HGC-27 cells to reprogram their
metabolism for particular requirements under SMG (80). A previous study reported that
glycolysis and the pentose phosphate pathways were dominant,
whereas the Krebs cycle was interrupted, which resulted in the
downregulation of ATP, after 110 h of SMG (27). Similarly, complex II, a primary
protein of the mitochondrial respiratory chain, was decreased and
ATP was influenced by a reduction in proton transport when measured
by proteomics (27).
Pantothenic acid is associated with cell migration
(81). The downregulation of
pantothenic acid in the present study may be due to the decreased
migration ability, which was consistent with our previous
discussion that the invasive ability decreased from downregulating
PS [DiMe(11,3)/MonoMe(11,5)], PS [18:3(9Z,12Z,15Z)/22:1(13Z)] and
PS [14:1(9Z)/24:0]. Furthermore, the downregulation of pantothenic
acid, the key precursor for the biosynthesis of coenzyme A (CoA),
can inhibit the synthesis of CoA and, in the Krebs cycle, CoA is a
key enzyme for the transformation of α-ketoglutarate to
succinyl-CoA (82).
Meanwhile, the KEGG pathway enrichment analysis of
the present study revealed that the metabolites associated with the
regulation of physiological functions were differentially expressed
in SMG compared with NG. When the sphingolipid signaling pathway,
sphingolipid metabolism, and arginine and proline metabolism were
altered under SMG, their associated physiological functions, such
as proliferation, cell cycle, apoptosis and migration, may also
have been affected. Therefore, the mechanism of the effect of SMG
on these functions in human HGC-27 cells requires further
investigation. In addition, KEGG pathway enrichment analysis
indicated that the differentially expressed metabolites were
primarily associated with the Forkhead box O (FOXO) signaling
pathway. FOXO is an important transcription factor that determines
cell fate and is associated with a broad range of cellular
physiological functions, such as differentiation, apoptosis, cell
proliferation, DNA damage and repair and mediating oxidative stress
among a wide range of cancers (83,84). The
intracellularly initiation pathway of apoptosis induced by the FOXO
protein is associated with oxidative stress, which occurs when ROS
is released into the cytoplasm (85). The FOXO1 and FOXO3a transcription
factors typically actived during oxidative stress causing apoptotic
cell injury (86,87). Under other oxidative stresses, FOXO3a
translocates from the cytoplasm to the nucleus where it triggers
cell death, thus activating the cell apoptosis pathway mediated by
the Fas protein (88). In addition,
FOXO4 and FOXO3a can mediate cell cycle arrest in mice and
cyclin-dependent kinases (CDK) expression through DNA damage
(89). The transcription factor,
E2F1 forms a complex with FOXO1 and FOXO3a, promoting the
transition from G1 to S phase, eventually resulting in
cell cycle arrest (90). Notably,
knockdown of FOXO3a, in combination with the oncogene c-myc,
nuclear factor and p27, results in the initiation of the cell
cycle, alteration of malignant mouse cells and activation of
carcinogenesis (91).
In summary, the investigation of cancer cells under
SMG may provide novel insight into the development of cancer and
subsequent changes in physiological function. The present study
revealed that human HGC-27 gastric cancer cells have a major effect
on lipid metabolism and that SMG may be valuble for cell and cancer
research. Ground-based weightlessness simulators like the RCCS,
used in the present study, have improved the understanding of how
SMG may affect humans. Although the present study is the first to
show the changes in metabolic expression of human HGC-27 gastric
cancer cells induced by SMG, to the best of our knowledge, the
understanding is far from complete. However, the results of the
present study may inform future development of novel targets for
gastric cancer therapy.
Acknowledgements
Not applicable.
Funding
The present study was funded by The Key Program
Grants of PLA Planning Technology Research (grant no.
SYFD1500128).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
ZC performed the experiments and drafted the initial
manuscript. HS, SG, JZ and BL performed the majority of the
experiments and statistical analyses. JY, SC, HFY, PS and TZ
performed certain experiments and collected the samples. NJ, SG, JZ
and HMY interpreted the data. YC designed the study and revised the
initial manuscript. All authors read and approved the final
manuscript.
Ethical approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
RCCS
|
rotary cell culture system
|
|
LC-MS
|
liquid chromatography-mass
spectrometry
|
|
SMG
|
simulated microgravity
|
|
NG
|
normal gravity
|
|
PE
|
phosphatidyl ethanolamine
|
|
PC
|
phosphatidyl choline
|
|
SM
|
sphingomyelin
|
|
PS
|
phosphatidyl serine
|
|
PA
|
phosphatidic acid
|
|
ECM
|
extracellular matrix
|
|
Cer
|
ceramide
|
|
Sph
|
sphingosine
|
|
PLD2
|
phospholipase D2
|
|
MMP
|
matrix metalloproteinase
|
|
FOXO
|
forkhead box O
|
References
|
1
|
Fedotov AA, Akulov SA and Akulova AS:
Alterations in cardiovascular system under artificially simulated
microgravity: Preliminary study. Conf Proc IEEE Eng Med Biol Soc.
2016:204–206. 2016.PubMed/NCBI
|
|
2
|
Atomi Y: Gravitational Effects on human
physiology. Subcell Biochem. 72:627–59. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hughes-Fulford M: Changes in gene
expression and signal transduction in microgravity. J Gravit
Physiol. 8:P1–4. 2001.PubMed/NCBI
|
|
4
|
Ulbrich C, Wehland M, Pietsch J,
Aleshcheva G, Wise P, van Loon J, Magnusson N, Infanger M, Grosse
J, Eilles C, et al: The impact of simulated and real microgravity
on bone cells and mesenchymal stem cells. Biomed Res Int.
2014:9285072014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Riwaldt S, Bauer J, Wehland M, Slumstrup
L, Kopp S, Warnke E, Dittrich A, Magnusson NE, Pietsch J, Corydon
TJ, et al: Pathways regulating spheroid formation of human
follicular thyroid cancer cells under simulated microgravity
conditions: A genetic approach. Int J Mol Sci. 17:5282016.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Svejgaard B, Wehland M, Ma X, Kopp S,
Sahana J, Warnke E, Aleshcheva G, Hemmersbach R, Hauslage J, Grosse
J, et al: Common effects on cancer cells exerted by a
randompositioning machine and a 2D clinostat. PLoS One.
10:e01351572015. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sahana J, Nassef MZ, Wehland M, Kopp S,
Krüger M, Corydon TJ, Infanger M, Bauer J and Grimm D: Decreased
E-cadherin in MCF-7 human breast cancer cells forming multicellular
spheroids exposed to simulated microgravity. Proteomics.
18:e18000152018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vidyasekar P, Shyamsunder P, Arun R,
Santhakumar R, Kapadia NK, Kumar R and Verma RS: Genome wide
expression profiling of cancer cell lines cultured in microgravity
reveals significant dysregulation of cell cycle and MicroRNA gene
networks. PLoS One. 10:e01359582015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dietz C, Infanger M, Romswinkel A, Strube
F and Kraus A: Apoptosis induction and alteration of cell adherence
in human lung cancer cells under simulated microgravity. Int J Mol
Sci. 20(pii): E36012019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kim YJ, Jeong AJ, Kim M, Lee C, Ye SK and
Kim S: Time-averaged simulated microgravity (taSMG) inhibits
proliferation of lymphoma cells, L-540 and HDLM-2, using a 3D
clinostat. Biomed Eng Online. 16:482017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Warburg O: On respiratory impairment in
cancer cells. Science. 124:269–272. 1956.PubMed/NCBI
|
|
12
|
Nath S and Villadsen J: Oxidative
phosphorylation revisited. Biotechnol Bioeng. 112:429–437. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–74. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hu JD, Tang HQ, Zhang Q, Fan J, Hong J, Gu
JZ and Chen JL: Prediction of gastric cancer metastasis through
urinary metabolomics investigation using GC/MS. World J
Gastroenterol. 17:727–734. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen JL, Tang HQ, Hu JD, Fan J, Hong J and
Gu JZ: Metabolomics of gastric cancer metastasis detected by gas
chromatography and mass spectrometry. World J Gastroenterol.
16:5874–5880. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gatenby RA and Gillies RJ: Why do cancers
have high aerobic glycolysis. Nat Rev Cancer. 4:891–899. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Koukourakis MI, Pitiakoudis M,
Giatromanolaki A, Tsarouha A, Polychronidis A, Sivridis E and
Simopoulos C: Oxygen and glucose consumption in gastrointestinal
adenocarcinomas: Correlation with markers of hypoxia, acidity and
anaerobic glycolysis. Cancer Sci. 97:1056–1060. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pedersen PL, Mathupala S, Rempel A,
Geschwind JF and Ko YH: A key player in the growth and survival of
many cancers and an ideal prospect for therapeutic intervention.
Biochim Biophys Acta. 1555:14–20. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tech K, Tikunov AP, Farooq H, Morrissy AS,
Meidinger J, Fish T, Green SC, Liu H, Li Y, Mungall AJ, et al:
Pyruvate kinase inhibits proliferation during postnatal cerebellar
neurogenesis and suppresses medulloblastoma formation. Cancer Res.
77:3217–3230. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
An J, Zhang Y, He J, Zang Z, Zhou Z, Pei
X, Zheng X, Zhang W, Yang H and Li S: Lactate dehydrogenase A
promotes the invasion and proliferation of pituitary adenoma. Sci
Rep. 7:47342017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Israelsen WJ and Vander Heiden MG:
Pyruvate kinase: Function, regulation and role in cancer. Semin
Cell Dev Biol. 43:43–51. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Wu J, Hu L, Chen M, Cao W, Chen H and He
T: Pyruvate kinase M2 overexpression and poor prognosis in solid
tumors of digestive system: Evidence from 16 cohort studies. Onco
Targets Ther. 9:4277–4288. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Jové M, Collado R, Quiles JL,
Ramírez-Tortosa MC, Sol J, Ruiz-Sanjuan M, Fernandez M, de la Torre
Cabrera C, Ramírez-Tortosa C, Granados-Principal S, et al: A plasma
metabolomic signature discloses human breast cancer. Oncotarget.
8:19522–19533. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pandey R, Caflisch L, Lodi A1, Brenner AJ
and Tiziani S: Metabolomic signature of brain cancer. Mol Carcinog.
56:2355–2371. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Navas-Carrillo D, Rodriguez JM,
Montoro-García S and Orenes-Piñero E: High-resolution proteomics
and metabolomics in thyroid cancer: Deciphering novel biomarkers.
Crit Rev Clin Lab Sci. 54:446–457. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chen L, Yang X, Cui X, Jiang MM, Gui Y,
Zhang YN and Luo XD: Adrenomedullin is a key protein mediating
rotary cell culture system that induces the effects of simulated
microgravity on human breast cancer Cells. Microgravity Sci
Technol. 27:417–426. 2015. View Article : Google Scholar
|
|
27
|
Michaletti A, Gioia M, Tarantino U and
Zolla L: Effects of microgravity on osteoblast mitochondria: A
proteomic and metabolomics profile. Sci Rep. 7:153762017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Morabito C, Steimberg N, Mazzoleni G,
Guarnieri S, Fanò-Illic G and Mariggiò MA: RCCS bioreactor-based
modelled microgravity induces significant changes on in vitro 3D
neuroglial cell cultures. Biomed Res Int. 2015:7542832015.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Longo N, Frigeni M and Pasquali M:
Carnitine transport and fatty acid oxidation. Biochim Biophys Acta.
1863:2422–2435. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Pietsch J, Ma X, Wehland M, Aleshcheva G,
Schwarzwälder A, Segerer J, Birlem M, Horn A, Bauer J, Infanger M
and Grimm D: Spheroid formation of human thyroid cancer cells in an
automated culturing system during the Shenzhou-8 Space mission.
Biomaterials. 34:7694–705. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Riwaldt S, Pietsch J, Sickmann A, Bauer J,
Braun M, Segerer J, Schwarzwälder A, Aleshcheva G, Corydon TJ,
Infanger M and Grimm D: Identification of proteins involved in
inhibition of spheroid formation under microgravity. Proteomics.
15:2945–2952. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Arun RP, Sivanesan D, Vidyasekar P and
Verma RS: PTEN/FOXO3/AKT pathway regulates cell death and mediates
morphogenetic differentiation of Colorectal Cancer Cells under
Simulated Microgravity. Sci Rep. 7:59522017. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kopp S, Sahana J, Islam T, Petersen AG,
Bauer J, Corydon TJ, Schulz H, Saar K, Huebner N, Slumstrup L, et
al: The role of NFκB in spheroid formation of human breast cancer
cells cultured on the random positioning machine. Sci Rep.
8:9212018. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chen ZY, Guo S, Li BB, Jiang N, Li A, Yan
HF, Yang HM, Zhou JL, Li CL and Cui Y: Effect of weightlessness on
the 3D structure formation and physiologic function of human cancer
cells. Biomed Res Int. 2019:48940832019.PubMed/NCBI
|
|
35
|
Marín de Mas I, Aguilar E, Jayaraman A,
Polat IH, Martín-Bernabé A, Bharat R, Foguet C, Milà E, Papp B,
Centelles JJ and Cascante M: Cancer cell metabolism as new targets
for novel designed therapies. Future Med Chem. 6:1791–1810. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Zhu M, Jin XW, Wu BY, Nie JL and Li YH:
Effects of simulated weightlessness on cellular morphology and
biological characteristics of cell lines SGC-7901 and HFE-145.
Genet Mol Res. 13:6060–6069. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Espinosa-Jeffrey A, Nguyen K, Kumar S,
Toshimasa O, Hirose R, Reue K, Vergnes L, Kinchen J and Vellis J:
Simulated microgravity enhances oligodendrocyte mitochondrial
function and lipid metabolism. J Neurosci Res. 94:1434–1450. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Akagi T and Kimoto T: Human cell line
(HGC-27) derived from the metastatic lymph node of gastric cancer.
Acta Med Okayama. 30:215–219. 1976.PubMed/NCBI
|
|
39
|
Kawakami H, Zaanan A and Sinicrope FA:
Microsatellite instability testing and its role in the management
of colorectal cancer. Curr Treat Options Oncol. 16:302015.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Zalba S and Ten Hagen TL: Cell membrane
modulation as adjuvant in cancer therapy. Cancer Treat Rev.
52:48–57. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kim HY, Lee KM, Kim SH, Kwon YJ, Chun YJ
and Choi HK: Comparative metabolic and lipidomic profiling of human
breast cancer cells with different metastatic potentials.
Oncotarget. 7:67111–67128. 2016.PubMed/NCBI
|
|
42
|
Elvas F, Stroobants S and Wyffels L:
Phosphatidylethanolamine targeting for cell death imaging in early
treatment response evaluation and disease diagnosis. Apoptosis.
22:971–987. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Iorio E, Ricci A, Bagnoli M, Pisanu ME,
Castellano G, Di Vito M, Venturini E, Glunde K, Bhujwalla ZM,
Mezzanzanica D, et al: Activation of phosphatidylcholine cycle
enzymes in human epithelial ovarian cancer cells. Cancer Res.
70:2126–2135. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Grimm D, Bauer J, Kossmehl P, Shakibaei M,
Schöberger J, Pickenhahn H, Schulze-Tanzil G, Vetter R, Eilles C,
Paul M and Cogoli A: Simulated microgravity alters differentiation
and increases apoptosis in human follicular thyroid carcinoma
cells. FASEB J. 16:604–606. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kossmehl P, Shakibaei M, Cogoli A,
Infanger M, Curcio F, Schönberger J, Eilles C, Bauer J, Pickenhahn
H, Schulze-Tanzil G, et al: Weightlessness induced apoptosis in
normal thyroid cells and papillary thyroid carcinoma cells via
extrinsic and intrinsic pathways. Endocrinology. 144:4172–4179.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Masiello MG, Cucina A, Proietti S, Palombo
A, Coluccia P, D'Anselmi F, Dinicola S, Pasqualato A, Morini V and
Bizzarri M: Phenotypic switch induced by simulated microgravity on
MDA-MB-231 breast cancer cells. Biomed Res Int. 2014:6524342014.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Zhao J, Ma H, Wu L, Cao L, Yang Q, Dong H,
Wang Z, Ma J and Li Z: The influence of simulated microgravity on
proliferation and apoptosis in U251 glioma cells. In Vitro Cell Dev
Biol Anim. 53:744–751. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Paulick MG and Bertozzi CR: The
glycosylphosphatidylinositol anchor: a complex membrane-anchoring
structure for protein. Biochemistry. 47:6991–7000. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Ferguson MA, Homans SW, Dwek RA and
Rademacher TW: Glycosyl-phosphatidylinositol moiety that anchors
Trypanosoma brucei variant surface glycoprotein to the membrane.
Science. 239:753–759. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Ferguson MA: The structure, biosynthesis
and functions of glycosylphosphatidylinositol anchors, and the
contributions of trypanosome research. J Cell Sci. 112:2799–2809.
1999.PubMed/NCBI
|
|
51
|
Tsai YH, Liu X and Seeberger PH: Chemical
biology of glycosylphosphatidylinositol anchors. Angew Chem Int Ed
Engl. 51:11438–11456. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Chang D, Xu H, Guo Y, Jiang X, Liu Y, Li
K, Pan C, Yuan M, Wang J, Li T and Liu C: Simulated microgravity
alters the metastatic potential of a human lung adenocarcinoma cell
line. In Vitro Cell Dev Biol Anim. 49:170–177. 2019. View Article : Google Scholar
|
|
53
|
Qian A, Zhang W, Xie L, Weng Y, Yang P,
Wang Z, Hu L, Xu HY, Tian ZC and Shang P: Simulated weightlessness
alters biological characteristics of human breast cancer cell line
MCF-7. Acta Astronautica. 63:947–958. 2008. View Article : Google Scholar
|
|
54
|
Peng W, Tan S, Xu Y, Wang L, Qiu D, Cheng
C, Lin Y, Liu C, Li Z, Li Y, et al: LC-MS/MS metabolome analysis
detects the changes in the lipid metabolic profiles of dMMR and
pMMR cells. Oncol Rep. 40:1026–1034. 2018.PubMed/NCBI
|
|
55
|
Toshima K, Nagafuku M, Okazaki T,
Kobayashi T and Inokuchi JI: Plasma membrane sphingomyelin
modulates thymocyte development by inhibiting TCR-induced
apoptosis. Int Immunol. 31:211–223. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Hogan PG: Sphingomyelin, ORAI1 channels,
and cellular Ca2+ signaling. J Gen Physiol. 146:195–200. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Matanes F, Twal WO and Hammad SM:
Sphingolipids as biomarkers of disease. Adv Exp Med Biol.
1159:109–138. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Kohama T, Olivera A, Edsall L, Nagiec MM,
Dickson R and Spiegel S: Molecular cloning and functional
characterization of murine sphingosine kinase. J Biol Chem.
273:23722–23728. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Li J, Gray BD, Pak KY and Ng CK: Targeting
phosphatidylethanolamine and phosphatidylserine for imaging
apoptosis in cancer. Nucl Med Biol. 78:23–30. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Andrieu-Abadie N and Levade T:
Sphingomyelin hydrolysis during apoptosis. Biochim Biophys Acta.
1585:126–134. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
van der Hoeven D, Cho KJ, Zhou Y, Ma X,
Chen W, Naji A, Montufar-Solis D, Zuo Y, Kovar SE, Levental KR, et
al: Sphingomyelin metabolism is a regulator of K-Ras function. Mol
Cell Biol. 38(pii): e00373–17. 2018.PubMed/NCBI
|
|
62
|
Fernández-Medarde A and Santos E: Ras in
cancer and developmental diseases. Genes Cancer. 2:344–358. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Cacev T, Radosević S, Spaventi R, Pavelić
K and Kapitanović S: NF1 gene loss of heterozygosity and expression
analysis in sporadic colon cancer. Gut. 54:1129–1135. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Dhomen N and Marais R: New insight into
BRAF mutations in cancer. Curr Opin Genet Dev. 17:31–39. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Khoukaz T: Administration of anti-EGFR
therapy: A practical review. Semin Oncol Nurs. 22:20–27. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Baek MO, Ahn CB, Cho HJ, Choi JY, Son KH
and Yoon MS: Simulated microgravity inhibits C2C12 myogenesis via
phospholipase D2-induced Akt/FOXO1 regulation. Sci Rep.
9:149102019. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Wang Z, Zhang F, He J, Wu P, Tay LWR, Cai
M, Nian W, Weng Y, Qin L, Chang JT, et al: Binding of
PLD2-generated phosphatidic acid to KIF5B promotes MT1-MMP surface
trafficking and lung metastasis of mouse breast cancer cells. Dev
Cell. 43:186–197. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Zeiller C, Mebarek S, Jaafar R, Pirola L,
Lagarde M, Prigent AF and Némoz G: Phospholipase D2 regulates
endothelial permeability through cytoskeleton reorganization and
occludin downregulation. Biochim Biophys Acta. 1793:1236–1249.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Ngo Thai Bich V, Hongu T, Miura Y,
Katagiri N, Ohbayashi N, Yamashita-Kanemaru Y, Shibuya A, Funakoshi
Y and Kanaho Y: Physiological function of phospholipase D2 in
anti-tumor immunity: Regulation of CD8+ T lymphocyte proliferation.
Sci Rep. 8:62832018. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Kandori S, Kojima T, Matsuoka T, Yoshino
T, Sugiyama A, Nakamura E, Shimazui T, Funakoshi Y, Kanaho Y and
Nishiyama H: Phospholipase D2 promotes disease progression of renal
cell carcinoma through the induction of angiogenin. Cancer Sci.
109:1865–1875. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Guo L, Cui C, Zhang K, Wang J, Wang Y, Lu
Y, Chen K, Yuan J, Xiao G, Tang B, et al: Kindlin-2 links
mechano-environment to proline synthesis and tumor growth. Nat
Commun. 10:8452019. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Phang JM, Donald SP, Pandhare J and Liu Y:
The metabolism of proline, a stress substrate, modulates
carcinogenic pathways. Amino Acids. 35:681–690. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Liu W, Wang X, Liu Z, Wang Y, Yin B, Yu P,
Duan X, Liao Z, Chen Y, Liu C, et al: SGK1 inhibition induces
autophagy-dependent apoptosis via the mTOR-Foxo3a pathway. Br J
Cancer. 117:1139–1153. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wallimann T, Tokarska-Schlattner M and
Schlattner U: The creatine kinase system and pleiotropic effects of
creatine. Amino Acids. 40:1271–1296. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Campos-Ferraz PL, Gualano B, das Neves W,
Andrade IT, Hangai I, Pereira RT, Bezerra RN, Deminice R,
Seelaender M and Lancha AH: Exploratory studies of the potential
anti-cancer effects of creatine. Amino Acids. 48:1993–2001. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Martin KJ, Chen SF, Clark GM, Degen D,
Wajima M, Von Hoff DD and Kaddurah-Daouk R: Evaluation of creatine
analogs as a new class of anticancer agents using freshly explanted
human tumor cells. J Natl Cancer Inst. 86:608–613. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Miller EE, Evans AE and Cohn M: Inhibition
of rate of tumor growth by creatine and cyclocreatine. Proc Natl
Acad Sci USA. 90:3304–3308. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Hoppeler H and Fluck M: Plasticity of
skeletal muscle mitochondria: Structure and function. Med Sci
Sports Exerc. 35:95–104. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Adams SH, Hoppel CL, Lok KH, Zhao L, Wong
SW, Minkler PE, Hwang DH, Newman JW and Garvey WT: Plasma
acylcarnitine profiles suggest incomplete long-chain fatty acid
beta-oxidation and altered tricarboxylic acid cycle activity in
type 2 diabetic African-American women. J Nutr. 139:1073–1081.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Chen WW, Freinkman E, Wang T, Birsoy K and
Sabatini DM: Absolute quantification of matrix metabolites reveals
the dynamics of mitochondrial metabolism. Cell. 166:1324–1337.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Hutschenreuther A, Birkenmeier G, Bigl M,
Krohn K and Birkemeyer C: Glycerophosphoglycerol, Beta-alanine, and
pantothenic acid as metabolic companions of glycolytic activity and
cell migration in breast cancer cell lines. Metabolites.
3:1084–1101. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Leonardi R and Jackowski S: Biosynthesis
of pantothenic acid and coenzyme A. EcoSal Plus. 2:2007. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Vurusaner B, Poli G and Basaga H: Tumor
suppressor genes and ROS: Complex networks of interactions. Free
Radic Biol Med. 52:7–18. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Gomes AR, Brosens JJ and Lam EW: Resist or
die: FOXO transcription factors determine the cellular response to
chemotherapy. Cell Cycle. 7:3133–3136. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Hou YQ, Yao Y, Bao YL, Song ZB, Yang C,
Gao XL, Zhang WJ, Sun LG, Yu CL, Huang YX, et al: Juglanthraquinone
C induces intracellular ROS increase and apoptosis by activating
the Akt/Foxo signal pathway in HCC cells. Oxid Med Cell Longev.
2016:49416232016. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Maiese K, Chong ZZ, Hou J and Shang YC:
Erythropoietin and oxidative stress. Curr Neurovasc Res. 5:125–142.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Nakamura T and Sakamoto K: Forkhead
transcription factor FOXO subfamily is essential for reactive
oxygen species-induced apoptosis. Mol Cell Endocrinol. 281:47–55.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Barthélémy C, Henderson CE and Pettmann B:
Foxo3a induces motoneuron death through the Fas pathway in
cooperation with JNK. BMC Neurosci. 5(48)2004.
|
|
89
|
Maiese K, Chong ZZ, Li F and Shang YC:
Erythropoietin: Elucidating new cellular targets that broaden
therapeutic strategies. Prog Neurobiol. 85:194–213. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Nowak K, Killmer K, Gessner C and Lutz W:
E2F-1 regulates expression of FOXO1 and FOXO3a. Biochim Biophys
Acta. 1769:244–252. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Liu Y, Ao X, Ding W, Ponnusamy M, Wu W,
Hao X, Yu W, Wang Y, Li P and Wang J: Critical role of FOXO3a in
carcinogenesis. Mol Cancer. 17:1042018. View Article : Google Scholar : PubMed/NCBI
|