Introduction
In locally advanced renal cell carcinoma (RCC),
4–10% of patients have vein tumour thrombus (VTT) (1). Radical nephrectomy and thrombectomy are
the standard surgical procedures for the treatment of RCC with VTT
and can effectively improve the prognosis. The 5-year
tumour-specific survival rate is 40–65% for patients with
non-metastatic disease and 6–28% for those with metastatic disease
at presentation globally (2).
Open radical nephrectomy and venous tumour
thrombectomy are traditional surgical procedures that are safe and
effective (3). Compared with
laparoscopic surgery, open surgery has wider indications, for
example the liver needs to be freely exposed in the surgery of
patients with Mayo classification (1) III–IV tumour thrombus, which is
difficult to achieve laparoscopically. However, open radical
nephrectomy and thrombectomy also have some disadvantages,
including the need for a larger incision, more bleeding and
postoperative pain, and longer hospital stays compared with
laparoscopic surgery (2).
With the popularisation of laparoscopic and robotic
techniques in urology, laparoscopic or robotic-assisted inferior
vena cava (IVC) thrombectomy has been used in some centres
(2–6). Compared with open surgery, laparoscopic
surgery has the same efficacy and safety (3); however, laparoscopic IVC thrombectomy
has limited operating space and requires high professional skills,
especially vascular suture skills (4).
In view of the similar efficacy of laparoscopic and
open surgery and the minimally invasive advantages of laparoscopic
surgery, laparoscopic surgery is usually more beneficial to
patients. Thus, the type of patient most suitable for laparoscopic
surgery must be determined. To the best of our knowledge, there are
no surgical approach prediction models to aid with this
decision-making. The choice of surgical approach is primarily based
on the experience of the surgeon, which means that some patients
undergoing laparoscopic surgery have to transfer to open surgery,
whilst some patients who could have undergone laparoscopic surgery
undergo open surgery instead and do not have the advantage of the
minimally invasive approach. To better assess which patients can
undergo laparoscopic surgery, the present study aimed to construct
a scoring system, which was named the Peking University Third
Hospital Laparoscopic Probability (PKUTHLP) score, to predict the
likelihood of using laparoscopic surgery in radical nephrectomy and
RV or IVC thrombectomy.
Materials and methods
Patient selection
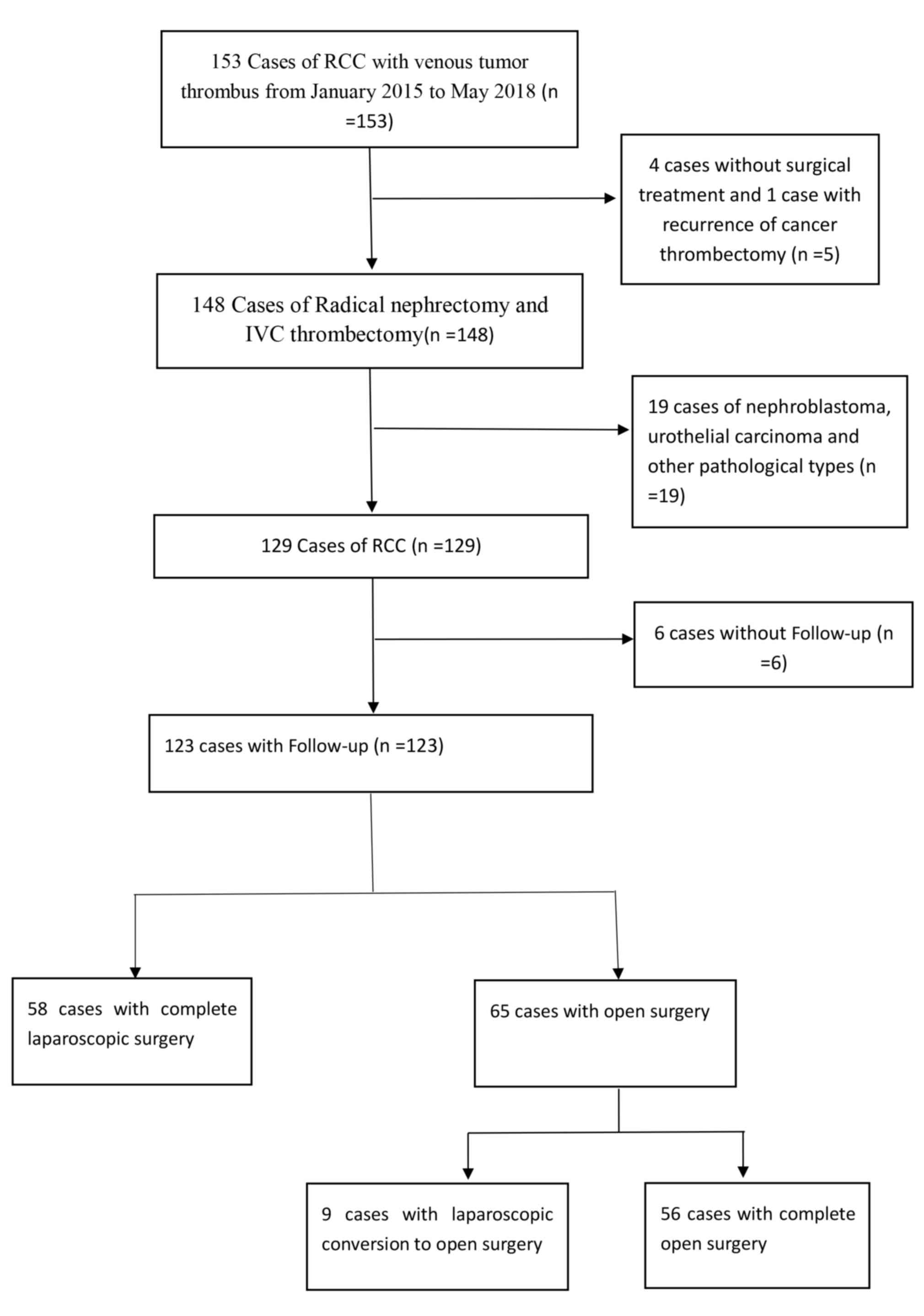
The clinical data of 153 patients with renal mass
with RV or IVC tumour thrombus admitted to the Department of
Urology at the Peking University Third Hospital (Beijing, China)
between January 2015 and May 2018 were retrospectively analysed.
The following patients were excluded: i) Patients without surgical
treatment; and ii) patients with recurrence of tumour thrombectomy,
nephroblastoma, urothelial carcinoma or other pathological types.
Overall, 123 cases with follow-up data were included in the present
study. Patient selection is shown in Fig. 1. The present study was approved by
the Ethics Committee of Peking University Third Hospital (approval
no. IRB00006761-M2018178; Beijing, China). All patients and their
families agreed to participate in the present study and provided
written informed consent.
Clinical and pathological
information
Clinical data, including age, sex, laterality, body
mass index, serum haemoglobin (Hb), albumin, corrected serum
calcium, alkaline phosphatase, serum creatinine (SCr), glomerular
filtration rate, American Society of Anesthesiologists grading
system score (7), nodal and
metastasis status, and pathological features, were collected. SCr
was retested 1 week after surgery.
Preoperative magnetic resonance imaging (MRI) or
computed tomography (CT) data were reviewed by two radiologists
blinded to the patient surgery data. The length of the tumour
thrombus and the width of the tumour thrombus were measured, and
the presence of bland thrombus and the relationship with the vessel
wall were observed. To define the level of venous tumour thrombus
extension, the Mayo classification system was used (1). Preoperative distant metastasis status
was routinely confirmed by positron emission tomography-CT or chest
CT, abdominal CT, cranial MRI and bone scans. Postoperative
immunotherapy or targeted molecular therapies were suggested if
distant metastasis existed before surgery.
Surgery and complications
The surgical approach of IVC tumour thrombectomy at
Peking University Third Hospital has been described previously
(6,8). In level 0 tumour thrombus, the IVC was
freed at the junction of the RV. The entrance of the RV was
clamped. In level I tumour thrombus, the IVC was freed at the
junction of the RV with non-invasive forceps. The blood flow of the
IVC was partially blocked. Following removal of the tumour
thrombus, a Prolene vascular suture was used to continuously suture
the wall of the IVC. In level II tumour thrombus, the contralateral
RV and the distal and proximal end of the IVC were freed via the
retroperitoneal approach combined with or without the abdominal
approach before the incision of the IVC wall and removal of the
tumour thrombus. If the tumour thrombus invaded the vessel wall,
the invaded portion was removed. In level III tumour thrombus, the
tumour thrombus is higher compared with the level of the hepatic
vein. The short hepatic vein was cut off, and the liver was pulled
down to the left to fully expose the IVC.
In the procedure of open radical nephrectomy and
thrombectomy, right RCC was treated with a chevron incision from
xiphoid process to axillary midline at 2 cm below the right rib
margin, extending ~5 cm below the left rib margin. For left renal
tumours, the open incision was symmetrical to the right renal
tumours. The surgical procedure of level 0-II tumour thrombus is
similar to that of laparoscopic surgery. In level III tumour
thrombus, the ligamentum teres hepatis left and right triangular
ligament, the sagittal ligament and the coronal ligament were cut
off to fully expose the retrohepatic IVC and hepatic vein. Then, a
Foley catheter was used to assist in thrombectomy (9). Intraoperative ultrasonography was used
to detect the superior pole of the tumour thrombus. In level IV
tumour thrombus, the central tendon of the diaphragm was cut around
the IVC, and the tumour thrombus was gently pushed into the IVC, so
that the thrombus became a level III thrombus. Conventional right
atrial thrombectomy was required to open the chest to establish
cardiopulmonary bypass under beating or non-beating conditions.
The modified Clavien grading system was used to
evaluate the postoperative complications (10). Complications higher than grade III
were defined as severe complications (11).
Monitoring and follow-up
The first follow-up was conducted 1 month after
surgery, and then every 3 months in the first 2 years, and every 6
months after that. Appropriate treatments were provided in cases of
local recurrence or distant metastasis, including sunitinib,
axitinib and other targeted therapy drugs. Follow-up information
was obtained from phone interviews and outpatient records. The
median follow-up time was 14.0 months (range, 0–44.0 months). The
last follow-up was completed in December 2018. If a patient died
during follow-up, the cause of death was confirmed by the death
certificate provided by the hospital.
Statistical analysis
In Table I continuous
parametric variables are presented as the mean value ± standard
deviation, and were analysed using Student t-tests (normally
distributed data) and Mann-Whitney U tests (non-normally
distributed data). Categorical variables (except Mayo
classification, which was analysed using the Mann-Whitney U test)
are presented as percentages, and were compared using χ2
test. For data pertaining to a small number of patients (<5),
the Fisher's exact test was used instead of the χ2 test.
In Table II statistically
significant patient and tumour characteristics in different
surgical approaches were included in regression analysis, where
odds ratios (ORs) and 95% confidence intervals (CIs) were
calculated. For easier interpretation of results in association
analysis, continuous variables were categorised based on
approximate sample tertiles (size of renal mass and width of tumour
thrombus) or predefined cut-offs of interest (age, ≥60 years; and
Hb divided by anaemia, 120 g/dl for males and 110 g/dl for
females). Although the aim of the present study was to develop an
accurate preoperative scoring system to predict the probability of
using laparoscopic surgery, the laparoscopic surgery group was used
as the control group during the analysis for the convenience of
calculation. For example, in Table
II, OR=25.667 for Mayo classification III–IV represents a very
high chance of using open surgery rather than laparoscopic surgery.
Given that the aim was to construct a scoring system that
effectively predicted which patients were suitable for laparoscopic
surgery, a forward selection approach was used, with a focus on the
percentage accuracy in classification of the given logistic
regression model. To create a scoring algorithm that classified
patients based on the likelihood of laparoscopic surgery, a
multivariate logistic regression model was developed with an
emphasis on the area under (AUC) the receiver operating
characteristic curve (ROC). The survival time was calculated from
the date of operation to death or the date of last follow-up (when
the patient was confirmed to be alive). The Kaplan-Meier method was
used to analyse the survival curve, and differences between groups
were tested using the log-rank test (12). The statistical tests were performed
using SPSS version 24.0 (IBM Corp.). All tests were two-sided, and
P<0.05 was considered to indicate a statistically significant
difference.
 | Table I.Comparison of clinicopathological
characteristics between the laparoscopic surgery and open surgery
groups of patients with renal cell carcinoma. |
Table I.
Comparison of clinicopathological
characteristics between the laparoscopic surgery and open surgery
groups of patients with renal cell carcinoma.
| Clinicopathological
characteristic | Laparoscopic surgery
(n=58) | Open surgery
(n=65) | P-value |
|---|
| Age, years | 61.2±10.9 | 56.4±11.1 | 0.018 |
| BMI,
kg/m2 | 23.5±4.4 | 23.8±3.5 | 0.639 |
| Tumor diameter,
cm | 7.9±2.3 | 9.5±4.0 | 0.007 |
| Tumor thrombus width,
mm | 17.4±8.4 | 26.7±8.7 | <0.001 |
| Hemoglobin, g/l | 125.9±21.5 | 116.8±24.3 | 0.029 |
| Serum calcium,
mg/dl | 8.5±1.5 | 8.7±0.5 | 0.181 |
| Albumin, g/l | 38.6±5.6 | 38.0±6.1 | 0.595 |
| Preoperative serum
creatinine, µmol/l | 91.8±20.7 | 105.1±69.7 | 0.167 |
| Serum creatinine one
week after operation, µmol/l | 104.9±51.8 | 138.1±166.1 | 0.131 |
| Alkaline phosphatase,
U/l | 87.1±45.1 | 102.3±52.7 | 0.091 |
| Operative time, min,
median (IQR) | 249.0 (190.5,
332.0) | 380.0 (304.5,
478.5) | <0.001 |
| Surgical bleeding
volume, ml, median (IQR) | 300.0 (100.0,
600.0) | 2000.0 (750.0,
3000.0) | <0.001 |
| Surgical blood
transfusion volume, ml, median (IQR) | 0 (0, 400.0) | 1200.0 (0,
2000.0) | <0.001 |
| Plasma transfusion
volume, ml, median (IQR) | 0 (0, 0) | 0 (0, 600.0) | <0.001 |
| Sex, n (%) |
|
|
|
| Male | 44 (75.9) | 48 (73.8) | 0.838 |
|
Female | 14 (24.1) | 17 (26.2) |
|
| Side, n (%) |
|
|
|
| Left | 23 (39.7) | 24 (36.9) | 0.923 |
|
Right | 35 (60.3) | 40 (61.5) |
|
| Both | 0 (0.0) | 1 (1.5) |
|
| KPS score, n (%) |
|
|
|
| ≥80 | 54 (93.1) | 51 (78.5) | 0.039 |
|
<80 | 4 (6.9) | 14 (21.5) |
|
| Clinical symptoms, n
(%) |
|
|
|
| No | 21 (36.2) | 12 (18.5) | 0.041 |
|
Yes | 37 (63.8) | 53 (81.5) |
|
| cN stage, n
(%) |
|
|
|
|
cN0 | 33 (56.9) | 22 (33.8) | 0.012 |
|
cN1 | 25 (43.1) | 43 (66.2) |
|
| cM stage, n
(%) |
|
|
|
|
cM0 | 45 (77.6) | 42 (64.6) | 0.164 |
|
cM1 | 13 (22.4) | 23 (35.4) |
|
| Mayo
classification, n (%) |
|
|
|
| 0 | 22 (37.9) | 6 (9.2) | <0.001 |
| I | 23 (39.7) | 13 (20.0) |
|
| II | 10 (17.2) | 25 (38.5) |
|
|
III | 3 (5.2) | 10 (15.4) |
|
| IV | 0 (0.0) | 11 (16.9) |
|
| IVC
brand thrombus, n (%) |
|
|
|
| No | 54 (93.1) | 48 (73.8) | 0.007 |
|
Yes | 4 (6.9) | 17 (26.2) |
|
| IVC resection, n
(%) |
|
|
|
| No | 55 (94.8) | 49 (75.4) | 0.005 |
|
Yes | 3 (5.2) | 16 (24.6) |
|
| Ipsilateral
adrenalectomy, n (%) |
|
|
|
| No | 34 (58.6) | 25 (38.5) | 0.031 |
|
Yes | 24 (41.4) | 40 (61.5) |
|
| Pathological type,
n (%) |
|
|
|
| Clear
cell carcinoma | 52 (89.7) | 51 (78.5) | 0.141 |
|
Non-clear cell carcinoma | 6 (10.3) | 14 (21.5) |
|
| Fuhrman's grade, n
(%) |
|
|
|
|
1-2 | 26 (44.8) | 19 (29.2) | 0.092 |
|
3-4 | 32 (55.2) | 46 (70.8) |
|
| Sarcomatoid
differentiation, n (%) |
|
|
|
| No | 49 (84.5) | 53 (81.5) | 0.811 |
|
Yes | 9 (15.5) | 12 (18.5) |
|
| Postoperative
complications, n (%) |
|
|
|
| No | 45 (77.6) | 38 (58.5) | 0.034 |
|
Yes | 13 (22.4) | 27 (41.5) |
|
| Severe
postoperative complications, n (%) |
|
|
|
| No | 54 (93.1) | 61 (93.8) | 1.000 |
|
Yes | 4 (6.9) | 4 (6.2) |
|
| Postoperative
targeted therapy, n (%) |
|
|
|
| No | 25 (43.1) | 25 (38.5) | 0.713 |
|
Yes | 33 (56.9) | 40 (61.5) |
|
 | Table II.Univariate and multivariate analysis
of laparoscopic surgery and open surgery. |
Table II.
Univariate and multivariate analysis
of laparoscopic surgery and open surgery.
|
| Univariate
analysis | Multivariate
logistic regression analysis |
|
|---|
|
|
|
|
|
|---|
| Variable | P-value | OR | 95% Cl | P-value | OR | 95% CI | PKUTHL score |
|---|
| Tumor diameter,
cm | 0.002 |
|
| 0.011 |
|
|
|
|
<7 |
| 1.000 |
|
| 1.000 |
| 0 |
|
7-10 | 0.135 | 0.504 | 0.205–1.237 | 0.268 | 0.531 | 0.173–1.629 | 0 |
|
≥10 | 0.045 | 2.662 | 1.024–6.918 | 0.014 | 4.801 | 1.381–16.693 | 1 |
| Mayo
classification | <0.001 |
|
| <0.001 |
|
|
|
| 0 |
| 1.000 |
|
| 1.000 |
| 0 |
| I | 0.206 | 2.072 | 0.669–6.417 | 0.760 | 1.219 | 0.343–4.324 | 0 |
| II | <0.001 | 9.167 | 2.865–29.330 | 0.001 | 9.773 | 2.629–36.336 | 2 |
|
III–IV | <0.001 | 25.667 | 5.673–116.116 | <0.001 | 31.145 | 6.059–160.095 | 3 |
| cN stage, cN1 vs.
cN0 | 0.011 | 2.580 | 1.242–5.358 | 0.030 | 2.790 | 1.107–7.302 | 1 |
| Age, ≥60 vs.
<60, years | 0.022 | 0.959 | 0.926–0.994 | 0.059 | 1.543 | 0.477–4.992 |
|
| Hemoglobin, anemia
vs. normal | 0.344 | 1.419 | 0.687–2.931 | 0.938 | 1.029 | 0.363–2.913 |
|
| KPS score, <80
vs. ≥80 | 0.029 | 3.706 | 1.144–12.003 | 0.302 | 2.551 | 0.456–14.262 |
|
| Clinical symptoms,
yes vs. no | 0.029 | 2.507 | 1.099–5.716 | 0.183 | 1.746 | 0.545–5.599 |
|
| IVC brand thrombus,
yes vs. no | 0.008 | 4.781 | 1.504–15.199 | 0.234 | 2.269 | 0.487–10.576 |
|
| Tumor thrombus
width, mm | <0.001 | 1.133 | 1.076–1.192 | 0.152 |
|
|
|
|
<17 |
| 1.000 |
|
| 1.000 |
|
|
|
17-27 | <0.001 | 9.067 | 3.246–25.324 | 0.280 | 3.259 | 0.781–13.604 |
|
|
≥27 | <0.001 | 16.190 | 5.373–48.786 | 0.647 | 2.773 | 0.459–16.762 |
|
Results
Clinicopathological
characteristics
The clinical data of the present cohort are shown in
Table I. In 123 patients, 58 (47.2%)
patients underwent complete laparoscopic surgery and 65 (52.8%)
patients underwent open surgery, including 9 (7.3%) patients who
underwent laparoscopic conversion to open surgery (data not shown).
Open surgery and laparoscopic surgery had statistically significant
differences for a number of factors, including Karnofsky
Performance Status score, clinical symptoms, age, Hb, tumour
diameter, tumour thrombus width, clinical node (cN) stage (13), Mayo classification, IVC bland
thrombus, IVC resection, ipsilateral adrenalectomy, operative time,
surgical bleeding volume, surgical blood transfusion volume, plasma
transfusion volume and postoperative complications. The open
surgery group had a longer operative time (380.0 vs. 249.0 min;
P<0.001), greater surgical bleeding volume (2,000.0 vs. 300.0
ml; P<0.001), greater blood transfusion volume (1,200.0 vs. 0
ml; P<0.001), greater plasma transfusion volume (0 vs. 0 ml;
P<0.001), and higher postoperative complication rates (41.5 vs.
22.4%; P=0.034) compared with the laparoscopic surgery group.
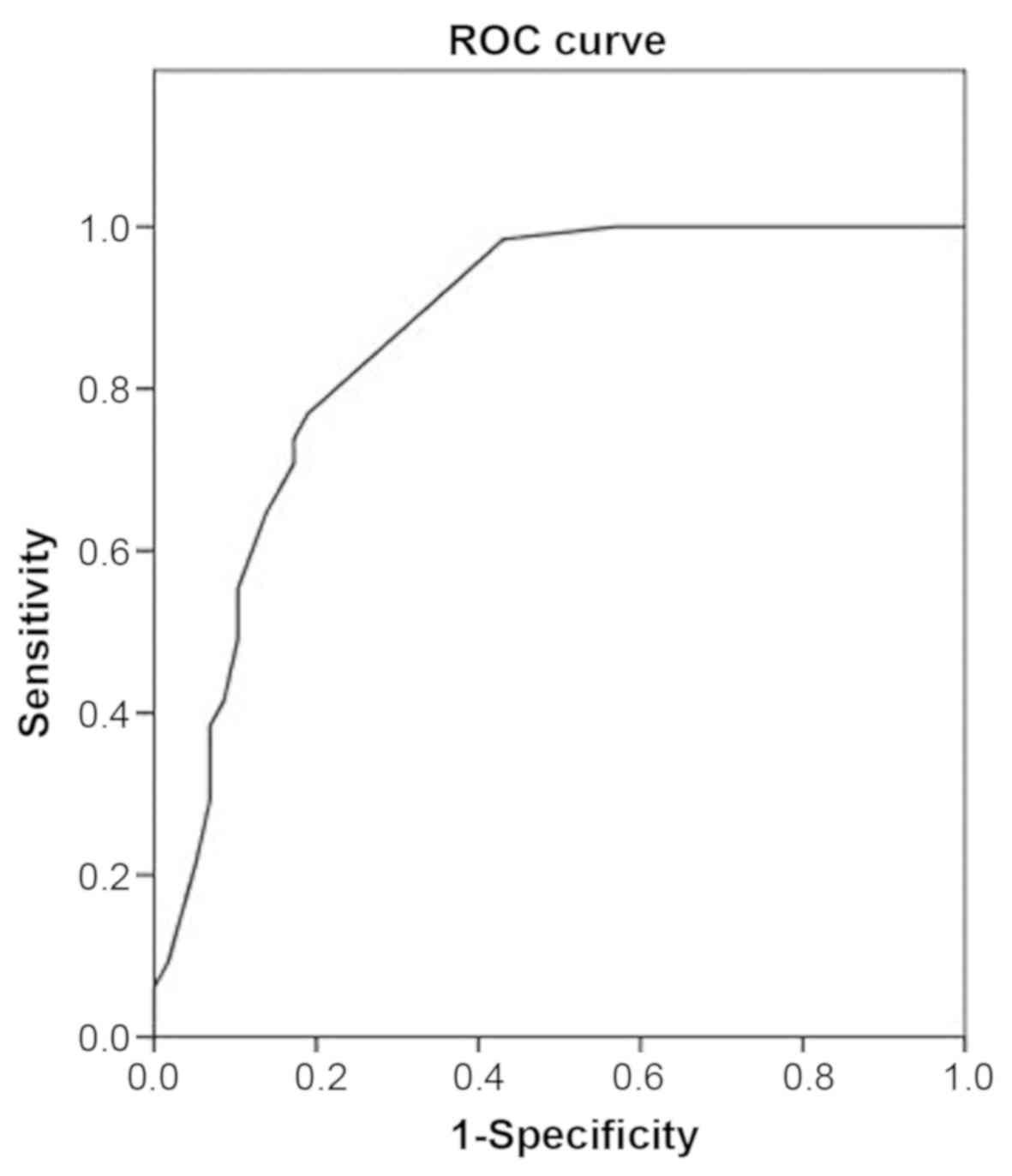
Logistic regression analyses and the
PKUTHLP score
Univariate and multivariate logistic regression
analyses of preoperative clinical and radiographic factors
associated with laparoscopic surgery are shown in Table II. Univariate analysis confirmed
that the aforementioned factors were significantly associated with
laparoscopic surgery. In multivariate analysis, only three factors
were associated with laparoscopic surgery: cN stage (OR=2.790;
P=0.030), Mayo classification (levels 0, I, II and III–IV;
OR=1.000, 1.219, 9.773 and 31.145, respectively; P<0.001), and
tumour diameter (<7, 7–10 and ≥10 cm; OR=1.000, 0.531, 4.801,
respectively; P=0.011). The ROC curve depicting the relationship
between the final model and laparoscopic surgery had an AUC of
0.862 (Fig. 2), which achieved a
sensitivity of 81.0% and a specificity of 76.9%.
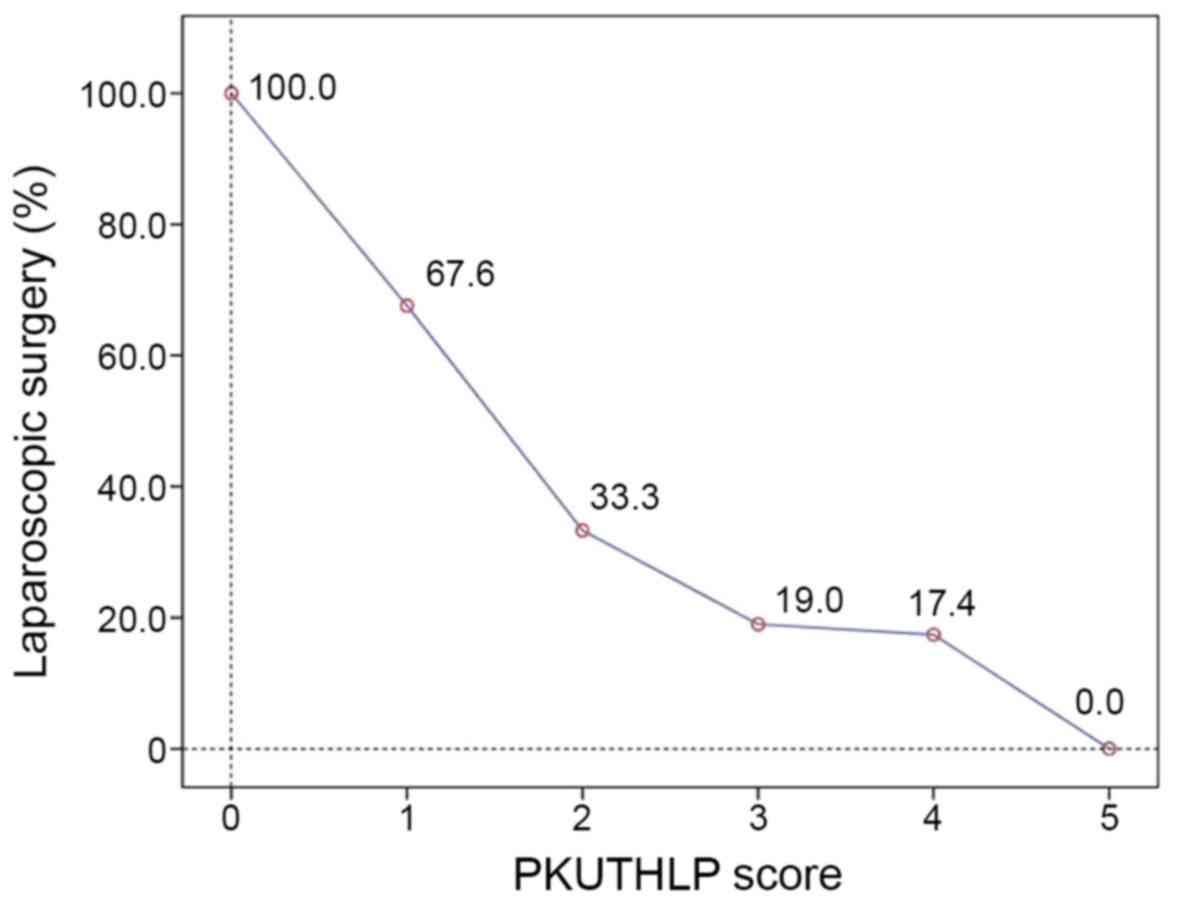
The PKUTHLP risk score was constructed based on cN
stage, Mayo classification and tumour diameter as follows. The OR
estimates from the multivariable logistic regression model were
used to create an individual score for each different level of
these three variables. These logistic regression results and
variable-specific scores are displayed in Table II. The individual scores for these
three variables were then summed to create the PKUTHLP score, which
ranges from 0–5. As shown in Table
III and Fig. 3, the proportion
of patients undergoing laparoscopic surgery for each level of the
PKUTHLP scores was as follows: 0 (n=20), 100%; 1 (n=34), 67.6%; 2
(n=21), 33.3%; 3 (n=21), 19.0%; 4 (n=23), 17.4%; and 5 (n=4),
0.0%.
 | Table III.Proportion of patients undergoing
laparoscopic surgery for each level of the PKUTHLP score. |
Table III.
Proportion of patients undergoing
laparoscopic surgery for each level of the PKUTHLP score.
| PKUTHLP score | Laparoscopic
surgery, n (%) | Open surgery, n
(%) |
|---|
| 0 | 20 (100) | 0 (0.0) |
| 1 | 23 (67.6) | 11 (32.4) |
| 2 | 7 (33.3) | 14 (66.7) |
| 3 | 4 (19.0) | 17 (81.0) |
| 4 | 4 (17.4) | 19 (82.6) |
| 5 | 0 (0.0) | 4 (100.0) |
Nine of the present cases were converted from
laparoscopic to open surgery. The PKUTHLP scores of these patients
were 1 point in one case, 2 points in two cases, 3 points in four
cases and 4 points in two cases. Most of these patients had a
relatively high PKUTHLP score.
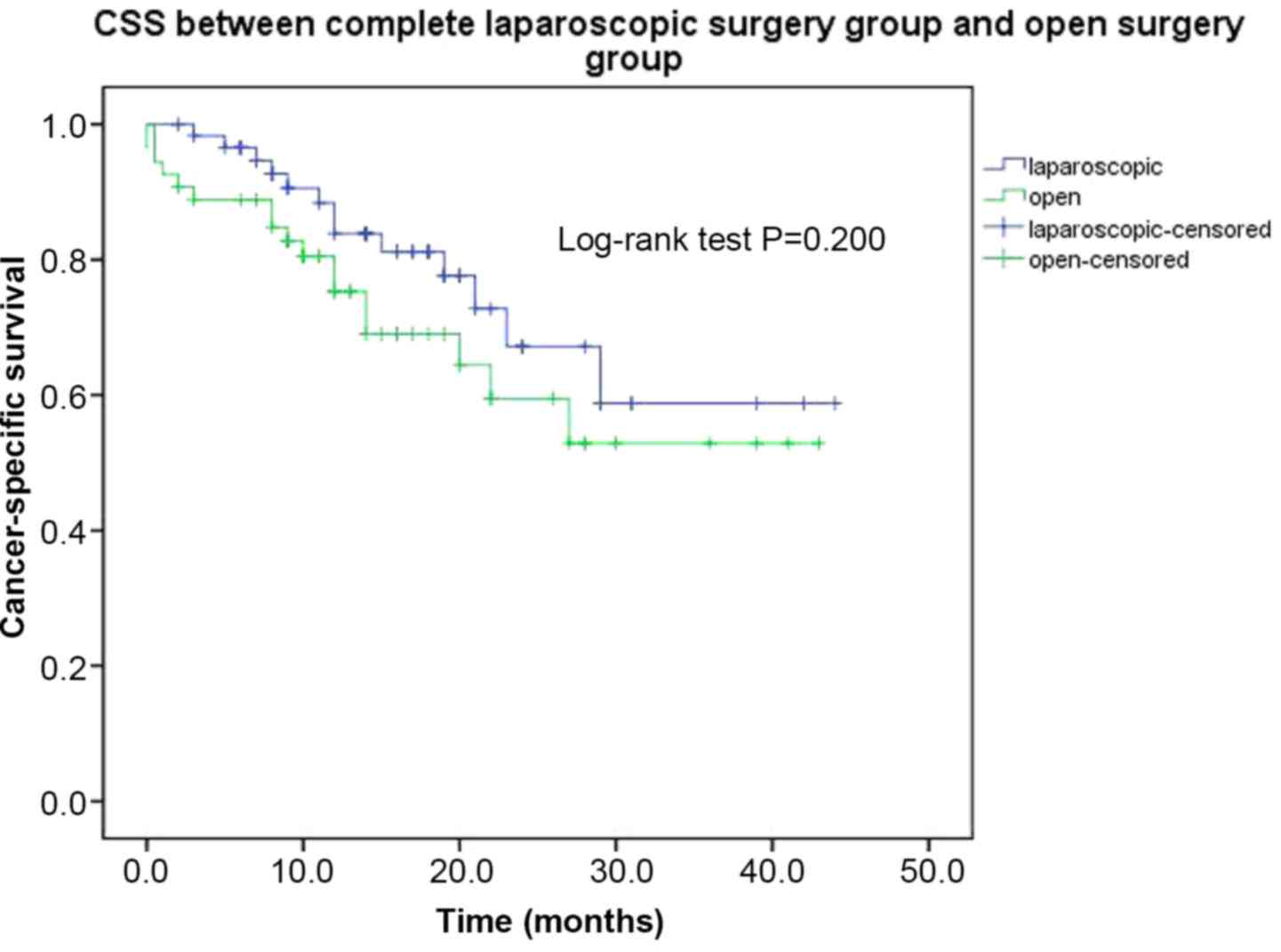
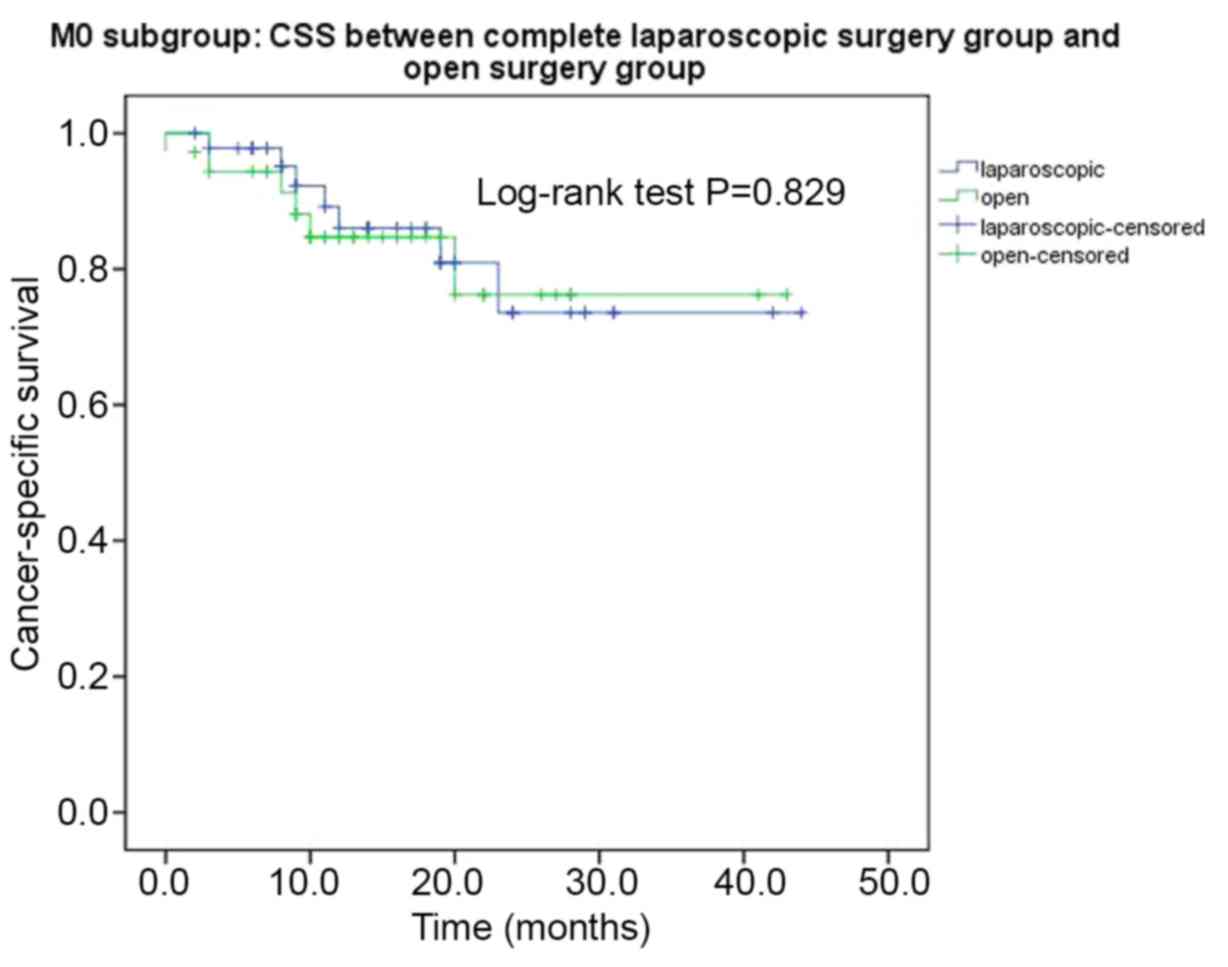
Follow-up and survival
The survival information of all patients was
available. At the last follow-up, 32 patients were deceased, and
all of them were cancer-associated deaths. The cancer-specific
survival (CSS) times of RCC with VTT between the complete
laparoscopic surgery group and the open surgery group is shown in
Fig. 4. The estimated mean CSS times
of the two groups were 33.1±2.6 months and 28.9±2.7 months between
the laparoscopic and open surgery groups, respectively, and a
non-significant difference was noted between the two groups
(P=0.200). In the metastasis (M)0 subgroup, the estimated mean CSS
times of the complete laparoscopic surgery group and the open
surgery group were 36.3±2.6 and 35.4±2.9 months, respectively,
although this difference was not significant (P=0.829; Fig. 5).
Discussion
Radical nephrectomy and thrombectomy are the
standard surgical procedures for the treatment of RCC with VTT and
can effectively improve prognosis. Open surgery and laparoscopic
surgery demonstrate no significant difference in terms of long-term
tumour survival (14). Patients can
have increased complications due an incorrect choice of surgical
procedure. Therefore, the present aimed to develop a user-friendly
scoring system to predict the probability of undergoing
laparoscopic surgery based on preoperative clinicopathological
characteristics. Finally, three predictive factors, including Mayo
classification, cN stage and tumour diameter, were used to create a
PKUTHLP score accurately classifying patients according to the
likelihood of undergoing laparoscopic surgery.
A previous study demonstrated that the level of Mayo
classification is the most important factor affecting the surgical
approach (15), consistent with the
results of the present study. Tumour thrombectomy for grade III and
IV tumours is difficult to perform laparoscopically because the
upper edge of the grade III tumour thrombus has reached the hepatic
vein. It is necessary to cut off some of the short hepatic veins or
use the piggyback hepatic method or the Pringle technique to
completely free the liver (16).
Furthermore, some patients with grade IV tumour thrombosis also
require a venous bypass shunt or cardiopulmonary bypass shunt; for
these patients, complete laparoscopic surgery is very difficult
(2).
Tumour diameter is also one of the factors
influencing the surgical approach. Although the large diameter of
the tumour is not an absolute contraindication for laparoscopic
surgery, a large tumour affects the establishment of the
pneumoperitoneum, reduces the operating space and increases the
difficulty of laparoscopic surgery (17). Huge tumours can sometimes seriously
affect the laparoscopic field of view, making the surgery
difficult. Therefore, tumour diameter also affects the choice of
surgical approach. The present study found that the proportion of
patients undergoing laparoscopic surgery was reduced when the
tumour diameter was >10 cm.
Lymph node enlargement suggested by preoperative
imaging is also one of the factors that affects the surgical
approach. Lymph node enlargement may require lymphadenectomy, and
it has been reported that lymphadenectomy is less common in
laparoscopic surgery (18). This may
be due to the surgeon's technical concerns about laparoscopically
excising nodal tissue adjacent to the major vessels. Furthermore,
retroperitoneal lymphadenopathy usually indicates a high
probability of intraoperative adhesion and difficulty in separating
the renal pedicle, which is not conducive to a laparoscopic
operation (19).
The PKUTHLP model constructed in the present study
demonstrated promise; however, it did not predict prognosis. There
was no difference in prognosis between the laparoscopic and open
surgery groups, but the incidence of complications in laparoscopic
surgery was lower compared with that of open surgery, which is
consistent with previous studies (20,21).
Although the PKUTHLP score appeared promising, the
present study had some limitations. It was a single-centre study,
and it is well known that the surgical approach has a lot to do
with the individual choice of the surgeon. In addition, the sample
size and number of patients with RCC and VTT are relatively small,
and the number of patients for each PKUTHLP score level is small,
which may have resulted in inaccuracy of the PKUTHLP score.
Furthermore, the present study was retrospective, and the score was
developed using a data-driven approach. Therefore, the PKUTHLP
score needs to be further validated in a prospective large-sample
study.
It was demonstrated that Mayo classification, cN
stage and tumour diameter were independently associated with the
surgical approach of nephrectomy and thrombectomy. Based on these
variables, the PKUTHLP score was constructed, which is an
easy-to-calculate preoperative scoring system accurately predicting
the probability of using laparoscopic surgery during radical
nephrectomy and thrombectomy. PKUTHLP may be used as a surrogate
marker for surgical complexity and may encourage less experienced
laparoscopic surgeons to select an alternative approach, such as an
open surgery, for treating patients with small RCC with VTT.
However, the present risk score requires prospective validation in
a larger patient cohort.
Acknowledgements
Not applicable.
Funding
The present study was funded by The Beijing Health
Promotion Association (grant. no. A76475-04).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
XZ drafted the manuscript. XZ, ZL, HZ and LM
conceived and designed the study. XZ, ZL, HZ, LM, LL, ST, GW, SZ,
SW and XT were responsible for the collection, analysis and
interpretation of the data. LM revised the manuscript critically
for important intellectual content. All authors read and approved
the final manuscript.
Ethics approval and consent to
participate
The study was approved by The Ethics Committee of
Peking University Third Hospital (approval no. IRB00006761-
M2018178; Beijing, China). All patients and their families agreed
to participate in the present study and provided written informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
VTT
|
vein tumour thrombus
|
|
RCC
|
renal cell carcinoma
|
|
IVC
|
inferior vena cava
|
|
ROC
|
receiver operating characteristic
|
References
|
1
|
Blute ML, Leibovich BC, Lohse CM, Cheville
JC and Zincke H: The Mayo Clinic experience with surgical
management, complications and outcome for patients with renal cell
carcinoma and venous tumour thrombus. BJU Int. 94:33–41. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pouliot F, Shuch B, Larochelle JC, Pantuck
A and Belldegrun AS: Contemporary management of renal tumors with
venous tumor thrombus. J Urol. 184:833–841. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Shao P, Li J, Qin C, Lv Q, Ju X, Li P,
Shao Y, Ni B and Yin C: Laparoscopic radical nephrectomy and
inferior vena cava thrombectomy in the treatment of renal cell
carcinoma. Eur Urol. 68:115–122. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bansal RK, Tu HY, Drachenberg D, Shayegan
B, Matsumoto E, Whelan JP and Kapoor A: Laparoscopic management of
advanced renal cell carcinoma with renal vein and inferior vena
cava thrombus. Urology. 83:812–816. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Al Otaibi M, Abou Youssif T, Alkhaldi A,
Sircar K, Kassouf W, Aprikian A, Mulder D and Tanguay S: Renal cell
carcinoma with inferior vena caval extention: Impact of tumour
extent on surgical outcome. BJU Int. 104:1467–1470. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Liu Z, Ma LL, Tian XJ, Wang GL, Zhang SD,
Huang Y, Hou XF, Zhao L, Lu J, et al: Clinical experience of Mayo
0-IV tumor thrombus treated with radical nephrectomy and inferior
vena cava thrombectomy. Chin J Urol. 11:842–847. 2017.(In
Chinese).
|
|
7
|
Davenport DL, Bowe EA, Henderson WG, Khuri
SF and Mentzer RM Jr: National surgical quality improvement program
(NSQIP) risk factors can be used to validate American society of
anesthesiologists physical status classification (ASA PS) levels.
Ann Surg. 243:636–644. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu Z, Ma LL, Tian XJ, Wang GL, Hou XF,
Zhang SD and Deng SH: Radical nephrectomy and thrombectomy for Mayo
clinic stage III tumor thrombus: A surgical technique and clinical
experience. Beijing Da Xue Xue Bao Yi Xue Ban. 49:597–602. 2017.(In
Chinese). PubMed/NCBI
|
|
9
|
Liu Z, Tang S, Tian X, Zhang S, Wang G,
Zhang H and Ma L: Foley catheter-assisted six-step thrombectomy
technique in the surgical management of renal cell carcinoma with
Mayo level II to IV tumor thrombus. J Int Med Res. 47:2104–2115.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mandal S, Sankhwar SN, Kathpalia R, Singh
MK, Kumar M, Goel A, Singh V, Sinha RJ, Singh BP and Dalela D:
Grading complications after transurethral resection of prostate
using modified Clavien classification system and predicting
complications using the Charlson comorbidity index. Int Urol
Nephrol. 45:347–354. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Inoue T, Kinoshita H, Satou M, Oguchi N,
Kawa G, Muguruma K, Murota T and Matsuda T: Complications of
urologic laparoscopic surgery: A single institute experience of
1017 procedures. J Endourol. 24:253–260. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
De Bruyne B, Pijls NH, Kalesan B, Barbato
E, Tonino PA, Piroth Z, Jagic N, Möbius-Winkler S, Rioufol G, Witt
N, et al: Fractional flow reserve-guided PCI versus medical therapy
in stable coronary disease. N Engl J Med. 367:991–1001. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Martinez-Salamanca JI, Huang WC, Millan I,
Bertini R, Bianco FJ, Carballido JA, Ciancio G, Hernández C,
Herranz F, Haferkamp A, et al: Prognostic impact of the 2009
UICC/AJCC TNM staging system for renal cell carcinoma with venous
extension. Eur Urol. 59:120–127. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang W, Xu J, Adams TS, Tian Y and Lv W:
Pure retroperitoneal laparoscopic radical nephrectomy for left
renal cell carcinoma with differential extensions of level I renal
vein tumor thrombus. J Endourol. 28:312–327. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lardas M, Stewart F, Scrimgeour D, Hofmann
F, Marconi L, Dabestani S, Bex A, Volpe A, Canfield SE, Staehler M,
et al: Systematic review of surgical management of nonmetastatic
renal cell carcinoma with vena caval thrombus. Eur Urol.
70:265–280. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lawindy SM, Kurian T, Kim T, Mangar D,
Armstrong PA, Alsina AE, Sheffield C, Sexton WJ and Spiess PE:
Important surgical considerations in the management of renal cell
carcinoma (RCC) with inferior vena cava (IVC) tumour thrombus. BJU
Int. 110:926–939. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Luciani LG, Porpiglia F, Cai T, D'Elia C,
Vattovani V, Giusti G, Tiscione D, Chiodini S, Peschechera R, Fiori
C, et al: Operative safety and oncologic outcome of laparoscopic
radical nephrectomy for renal cell carcinoma >7 cm: A
multicenter study of 222 patients. Urology. 81:1239–1244. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Filson CP, Miller DC, Colt JS, Ruterbusch
J, Linehan WM, Chow WH and Schwartz K: Surgical approach and the
use of lymphadenectomy and adrenalectomy among patients undergoing
radical nephrectomy for renal cell carcinoma. Urol Oncol.
30:856–863. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Capitanio U, Stewart GD, Larcher A, Ouzaid
I, Akdogan B, Roscigno M, Marszalek M, Dell'Oglio P, Salagierski M,
Volpe A, et al: European temporal trends in the use of lymph node
dissection in patients with renal cancer. Eur J Surg Oncol.
43:2184–2192. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ebbing J, Wiebach T, Kempkensteffen C,
Miller K, Bachmann A, Günzel K, Rieken M, Friedersdorff F, Baumunk
D and Weikert S: Evaluation of perioperative complications in open
and laparoscopic surgery for renal cell cancer with tumor thrombus
involvement using the Clavien-Dindo classification. Eur J Surg
Oncol. 41:941–952. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xu B, Zhao Q, Jin J, He ZS, Zhou LQ and
Zhang Q: Laparoscopic versus open surgery for renal masses with
infrahepatic tumor thrombus: The largest series of retroperitoneal
experience from China. J Endourol. 28:201–207. 2014. View Article : Google Scholar : PubMed/NCBI
|