Introduction
Prostate cancer (PCa) is a common malignant tumor of
genitourinary system in clinic (1).
In recent years, prostate-specific antigen (PSA) screening is
widely used in PCa examination, so the diagnosis rate and treatment
rate of early PCa also increase (2).
PCa is the second most common malignant tumor in men after lung
cancer. It is estimated that more than one million new cases are
diagnosed every year in the world (3), and the incidence rate is increasing
(4). After the primary treatment of
chemical or surgical castration for PCa patients, most cases would
develop into disease state, which is the metastatic
castration-resistant prostate cancer (CRPC), with median survival
less than 2 years (5). For the
treatment of CRPC, androgen pathway inhibitors have become the
mainstream treatment method in recent years, such as flutamide,
sipuleucel-T, enzalutamide, abiraterone acetate, radium-223 and
cabazitaxel, which can provide survival benefits for CRPC patients
(6).
Abiraterone is a selective and irreversible
cytochrome P450 c17 (CYP17) inhibitor. With potency 10 to 30 times
higher than ketoconazole, it is a non-selective inhibitor. CYP17
plays an important role in androgen synthesis and is a key enzyme
in testosterone synthesis (7).
Abiraterone acetate is a prodrug of abiraterone and a selective
inhibitor of androgen biosynthesis, which effectively blocks CYP17
and androgen synthesis in adrenal gland, testis and prostate tumors
(8). Flutamide is a non-steroidal
oral antiandrogen that blocks the effect of testosterone.
Testosterone is a natural hormone responsible for the growth and
diffusion of human PCa cells. Blocking the effect of testosterone
can slow down the growth and diffusion of PCa cells. Currently, it
has been widely used in treating patients with PCa (9,10).
MicroRNA (miRNA) is a newly discovered class of
highly conserved endogenous non-coding hairpin nucleotide
transcripts with a length of approximately 19–25 bases and widely
existing in eukaryotic cells (11,12).
Studies have found that some miRNAs are closely related to the
occurrence and development of cancer. For example, the research
results of Beebe-Dimmer et al (13) show that miR-195-5p is downregulated
in PCa cell lines DU145 and PC3. Overexpression of miR-195-5p
significantly inhibits the migration and invasion of PCa cells, and
they have proved that miR-195-5p can inhibit PCa cell movement by
regulating the expression of c-Met, MMP1 and MMP9. Research results
of Zhao et al (14) show that
miR-493-5p is downregulated in breast cancer cells and plays an
inhibitory role in invasion and tumorigenicity of breast cancer
cells. Human miR-493-5p belongs to DLK1-DIO3 imprinted miRNA
clusters and plays a role as a tumor inhibitor in human cancers
(14). Wang et al (15) showed that miR-493-5p is a tumor
suppressor gene and is downregulated in human liver cancer.
Overexpression of miR-493-5p promotes apoptosis and inhibits
proliferation and migration of liver cancer cells by negatively
regulating VAMP expression. The research results of Wang et
al (15) show that miR-493-5p is
downregulated in PCa cells and acts as a tumor inhibitor in PCa
cells.
At present, there are many studies on the treatment
of PCa patients with single drug use of abiraterone and flutamide,
but there are few on the treatment of PCa patients with abiraterone
combined with flutamide. This study aimed to find more effective
and safer treatment drugs for PCa patients, to prolong the survival
time of patients and improve the quality of life through the
efficacy and adverse reactions of abiraterone combined with
flutamide in the treatment of PCa patients, as well as the effects
on expression of miR-493-5p and miR-195-5p.
Patients and methods
General information
The medical records of 146 PCa patients were
selected, who were admitted to Longhua Hospital Shanghai University
of Traditional Chinese Medicine (Shanghai, China) from January 2011
to December 2013. Among them, 84 patients were treated with
abiraterone combined with flutamide as a study group, and 62
patients were treated with abiraterone alone as a control
group.
Inclusion and exclusion criteria
Inclusion criteria were as follows: Patients were
confirmed as PCa by pathological examination in both groups; PSA
progress was observed in both groups; both groups of patients were
male, aged 18–60 years. Exclusion criteria were as follows:
patients with mental illness and other serious diseases; patients
allergic to the drugs used in this study; patients who used
targeted therapy of enzarumine or other similar potent androgen
pathways.
Patients and their families were informed and signed
informed consent forms. This study was approved by the Medical
Ethics Committee of Longhua Hospital Shanghai University of
Traditional Chinese Medicine.
Main instruments and reagents
Human PSA kit (Cusabio); multifunctional microplate
reader (model: DLK0001622, BioTek Instruments, Inc.); real-time
fluorescence quantitative PCR instrument (model: 7300, Applied
Biosystems; Thermo Fisher Scientific, Inc.); spectrophotometer
(model: DR5000, Hach Company); high-speed refrigerated centrifuge
(Eppendorf); TRIzol kit (BioTek Instruments, Inc.); reverse
transcription kit (Takara); real-time fluorescence quantitative PCR
kit (Beijing BioDee BioTech Corporation Ltd.); miR-493-5p,
miR-195-5p and U6 small nuclear RNA (RNU6B) internal reference
primers were designed and synthesized by GeneCopoeia, Inc. The
detailed primer sequences are shown in Table I.
 | Table I.Sequence of primers. |
Table I.
Sequence of primers.
| Gene | Upstream primer
sequence | Downstream primer
sequence |
|---|
| miR-493-5p |
5′-TCCTACGGAGAGGCTCAG-3′ |
5′-TCCTCGTAGTCCAACACG-3′ |
| miR-195-5p |
5′-CGTAGCAGCACAGAAA-3′ |
5′-GTGCAGGGTCCGGGT-3′ |
| U6 |
5′-CTCGCTTCGGCAGCACA-3′ |
5′-AACGCTTCACGAATTTGCGT-3′ |
Treatment methods
Control group: patients were given 1,000 mg of
abiraterone acetate orally (Xian Janssen Pharmaceutical Ltd., SFDA
approval no. J20150112), once a day; study group: on the basis of
the control group, the patients in the study group were given 250
mg of flutamide orally (Tasly Diyi Pharmaceutical Co., Ltd., SFDA
approval no. H19990143) once a day. Altogether 28 days as a cycle,
two groups of patients were treated for 4 consecutive cycles.
Observation index and therapeutic
effect evaluation standard
The efficacy evaluation was divided into four parts
according to the World Health Organization solid tumor evaluation
standard (16): complete response
(CR) is defined as complete disappearance of tumor focus and no new
focus; partial response (PR) is defined as the degree of volume
reduction of tumor lesions >50%; stable disease (SD) is defined
as the reduction of tumor focus volume <50%; progressive disease
(PD) is defined as the degree of tumor lesion volume increase above
25%. The overall response rate (ORR) = (CR + PR)/Total cases ×100%.
The toxic and side effects of group A and group B during treatment
were observed. The main toxic and side effects were nausea,
vomiting, anemia, thrombocytopenia, myelosuppression, liver
function injury and renal function injury.
According to Karnofsky (KPS) score (17), the quality of life of patients after
treatment was evaluated. After treatment, KPS score was improved by
>10 points, which is classified as improvement. After treatment,
KPS score was decreased or increased by less than 10 points, which
is classified as stability. After treatment, KPS score was
decreased by >10 points, which is classified as deterioration.
Quality of Life Improvement Rate = (Improvement + Stability)/Total
cases ×100%.
Follow-up
The two groups of patients were followed up by
telephone and visit for 5 years. The follow-up was conducted once
every 3 months within 5 years, with the deadline of January 2019.
The overall survival (OS) was calculated from the beginning of drug
administration to the day of death or the last follow-up in both
groups.
Serum standard collection
A total of 5 ml fasting venous blood of the two
groups of patients was sampled and placed in EDTA-K2
anticoagulation tube three days before treatment (T1), one month
after treatment (T2), two months after treatment (T3) and six
months after treatment (T4). The samples were centrifuged at 1,500
× g at 4°C for 10 min, and 500 µl of upper serum was drawn and
stored in EP tube for later use.
Detection of serum PSA level
The serum PSA levels of the two groups of patients
were determined by radioimmunoassay at T1, T2, T3 and T4. The
detection process was strictly conducted according to the PSA kit
instructions.
Detection of serum miR-493-5p and
miR-195-5p
At T1, T2, T3 and T4, the serum of the two groups of
patients was taken for miR-493-5p and miR-195-5p detection, and the
specific steps were as follows: the serum total RNA was extracted
according to the instructions of the TRIzol serum extraction kit.
Total RNA purity, concentration and integrity were determined by UV
spectrophotometry and agarose gel electrophoresis. Total RNA (2 µl)
was taken to prepare cDNA according to the instruction manual of
the kit. The reverse transcription reaction conditions were as
follows: 42°C for 60 min and 95°C for 5 min; the synthesized cDNA
sample was stored at −20°C for later use. U6 was used as the
internal reference gene, and the reaction system of the total
volume (20 µl) was as follows: 1 µl of cDNA, 10 µl of PCR premix, 2
µl of upstream primer (×10), 2 µl of downstream primer (×10), and 5
µl of dd water (Rnase and Dnase free). PCR amplification cycle
conditions were as follows: 90°C for 5 min, 90°C for 5 sec, 60°C
for 30 sec, 72°C for 5 sec, a total of 40 cycles. Amplification
data were analyzed by ABI PRISM 7500 fluorescence quantitative PCR
instrument manufacturer software, and the results were expressed by
2−∆CT.
Statistical method
SPSS 21.0 (Easybio) was used for analysis, and
GraphPad Prism 7 was used to visualize the data. In this study, the
counting data were expressed by [n (%)], and Chi-square test was
used to compare the rates. The measurement data were expressed as
mean ± standard deviation (mean ± SD). t-test was used for
comparison of measurement data between two groups, and one-way
analysis of variance was used for the comparison of multiple
groups. Kaplan-Meier method was used to draw five-year OS curves of
the two groups of patients, and log-rank test for comparison.
P<0.05 was considered to indicate a statistically significant
difference.
Results
Comparison of general data between two
groups of patients
There was no significant difference between the
control group and the study group in age, smoking history,
exercise, residence, ethnicity, education level, weight, diet
preference, and alcohol consumption (P>0.05) (Table II).
 | Table II.Comparison of general data of both
groups [n (%)]. |
Table II.
Comparison of general data of both
groups [n (%)].
| Group | Control group
(n=62) | Study group
(n=84) | χ2
value | P-value |
|---|
| Age |
|
| 0.311 | 0.577 |
|
<45 | 23 (37.10) | 35 (41.67) |
|
|
|
≥45 | 39 (62.90) | 49 (58.33) |
|
|
| Smoking
history |
|
| 0.877 | 0.349 |
|
Yes | 47 (75.81) | 69 (82.14) |
|
|
| No | 15 (24.19) | 15 (17.86) |
|
|
| Exercise |
|
| 0.835 | 0.361 |
|
Yes | 36 (58.06) | 55 (65.48) |
|
|
| No | 26 (41.94) | 29 (34.52) |
|
|
| Residence |
|
| 1.086 | 0.297 |
|
Urban | 40 (64.52) | 47 (55.95) |
|
|
|
Rural | 22 (35.48) | 37 (44.05) |
|
|
| Ethnicity |
|
| 0.673 | 0.412 |
|
Han | 57 (91.94) | 80 (95.24) |
|
|
|
Minority | 5 (8.06) | 4 (4.76) |
|
|
| Education
level |
|
| 1.331 | 0.249 |
| <
High school | 46 (74.19) | 57 (67.86) |
|
|
| ≥ High
school | 16 (25.81) | 27 (32.14) |
|
|
| Weight |
|
| 1.041 | 0.308 |
| <55
kg | 25 (40.32) | 27 (32.14) |
|
|
| ≥55
kg | 37 (59.68) | 57 (67.86) |
|
|
| Diet
preference |
|
| 0.819 | 0.366 |
|
Light | 33 (53.23) | 51 (60.71) |
|
|
|
Spicy | 29 (46.77) | 33 (39.29) |
|
|
| Alcohol
consumption |
|
| 0.199 | 0.656 |
| Never
or seldom | 16 (25.81) | 19 (22.62) |
|
|
|
Frequent | 46 (74.19) | 65 (77.38) |
|
|
Clinical efficacy of two groups of
patients
In the control group after treatment, there were 8
cases of CR (12.91%), 15 cases of PR (24.19%), 29 cases of SD
(46.77%), 10 cases of PD (16.13%), response rate (RR) was 37.10%.
In the study group after treatment, there were 14 cases of CR
(16.66%), 34 cases of PR (40.48%), 26 cases of SD (30.95%), 10
cases of PD (11.91%), and RR was 57.14%. RR of study group was
significantly higher than that of control group (P<0.05)
(Table III).
 | Table III.Comparison of clinical efficacy
results of two groups of patients [n (%)]. |
Table III.
Comparison of clinical efficacy
results of two groups of patients [n (%)].
| Group | Control group
(n=62) | Study group
(n=84) | χ2
value | P-value |
|---|
| CR | 8
(12.90) | 14 (16.67) | – | – |
| PR | 15 (24.19) | 34 (40.48) | – | – |
| SD | 29 (46.77) | 26 (30.95) | – | – |
| PD | 10 (16.13) | 10 (11.91) | – | – |
| RR | 23 (37.10) | 48 (57.14) | 5.738 | 0.017 |
Comparison of toxic and side effects
between two groups of patients
During the treatment, toxic and side effects
occurred in both groups, and there was no allergic reaction. In the
control group, nausea and vomiting occurred in 3 cases (4.84%),
anemia in 4 cases (6.45%), thrombocytopenia in 3 cases (4.84%),
myelosuppression in 5 cases (8.06%), liver function injury in 2
cases (3.23%), renal function injury in 3 cases (4.84%), and the
total incidence of toxic and side effects was 32.26% (20/62). In
the study group, nausea and vomiting occurred in 3 cases (3.57%),
anemia in 2 cases (2.38%), thrombocytopenia in 2 cases (2.38%),
myelosuppression in 4 cases (4.76%), liver function injury in 1
case (1.19%), renal function injury in 1 case (1.19%), and the
total incidence of adverse reactions was 15.48% (13/84). There was
no significant difference in the incidence of nausea, vomiting,
anemia, thrombocytopenia, bone marrow suppression, liver function
injury and renal function injury between the two groups
(P>0.05), but the total incidence of adverse reactions in the
study group was significantly lower than that in the control group
(P<0.05) (Table IV).
 | Table IV.Comparison of adverse reactions
between two groups of patients [n (%)]. |
Table IV.
Comparison of adverse reactions
between two groups of patients [n (%)].
| Group | Control group
(n=62) | Study group
(n=84) | χ2
value | P-value |
|---|
| Nausea and
vomiting | 3 (4.84) | 3 (3.57) | 0.145 | 0.703 |
| Anemia | 4 (6.45) | 2 (2.38) | 1.500 | 0.221 |
|
Thrombocytopenia | 3 (4.84) | 2 (2.38) | 0.652 | 0.807 |
|
Myelosuppression | 5 (8.06) | 4 (4.76) | 0.673 | 0.412 |
| Liver function
injury | 2 (3.23) | 1 (1.19) | 0.734 | 0.392 |
| Renal function
injury | 3 (4.84) | 1 (1.19) | 1.782 | 0.128 |
| Total incidence
rate | 20 (32.26) | 13 (15.48) | 5.743 | 0.017 |
Comparison of quality of life between
two groups of patients
The quality of life in the control group was
improved in 10 cases (15.63%), stabilized in 25 cases (39.06%),
deteriorated in 29 cases (45.31%), and the improvement rate of
quality of life was 54.69% 30 days after discharge. In the study
group, the quality of life was improved in 16 cases (19.05%),
stabilized in 46 cases (54.76%), deteriorated in 22 cases (26.19%),
and the improvement rate of quality of life was 73.81% 30 days
after treatment. The improvement rate of quality of life in the
study group was significantly higher than that in the control group
(P<0.05) (Table V).
 | Table V.Comparison of quality of life between
two groups of patients [n (%)]. |
Table V.
Comparison of quality of life between
two groups of patients [n (%)].
| Group | n | Improved | Stabilized | Deteriorated | Improvement rate
(%) |
|---|
| Control group | 62 | 10 (15.63) | 25 (39.06) | 29 (45.31) | 54.69 |
| Study group | 84 | 16 (19.05) | 46 (54.76) | 22 (26.19) | 73.81 |
| χ2
value | – | – | – | – | 6.649 |
| P-value | – | – | – | – | 0.001 |
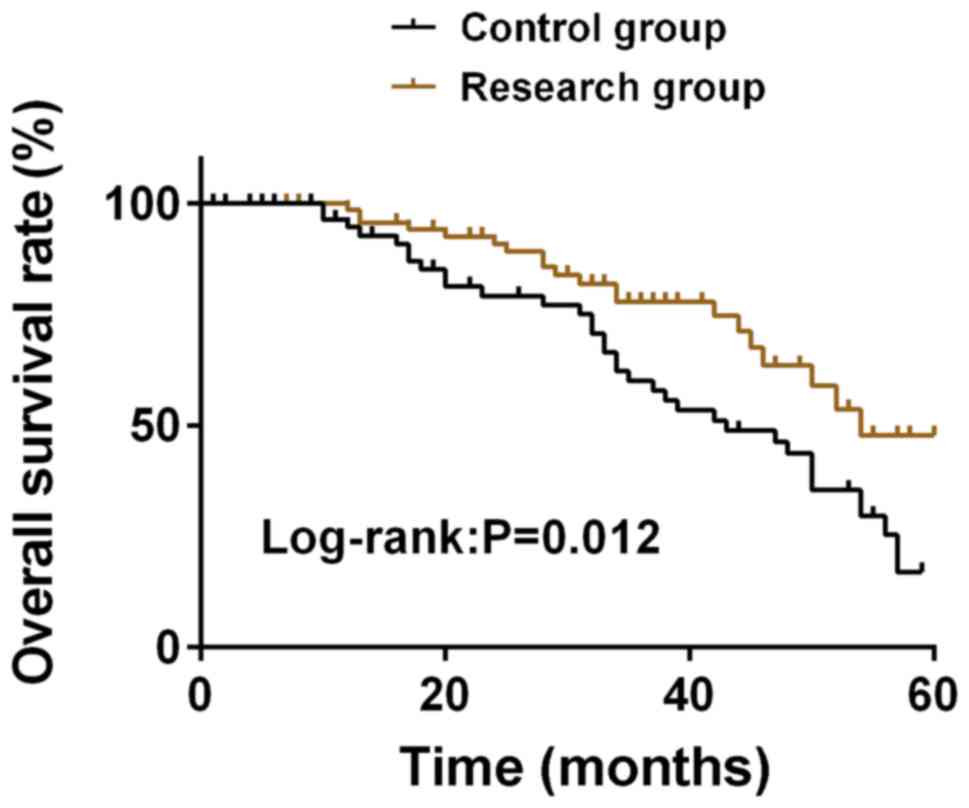
Comparison of 5-year survival rate
between two groups of patients
The follow-up results showed that OS in the study
group was 45.24% (38/84) at 5 years and OS in the control group was
20.97% (13/62) at 5 years. OS in the study group was significantly
higher than that in the control group at 5 years (P<0.05)
(Fig. 1).
Comparison of serum PSA levels of two
groups of patients at different time points
There was no significant difference in serum PSA
level between the two groups at T1 (P>0.05). Compared with T1,
serum PSA levels in T2, T3 and T4 groups were significantly
decreased (P<0.05). Compared with T2, the serum PSA level of the
two groups of patients decreased significantly at T3 (P<0.05),
while the serum PSA level of the study group decreased
significantly at T4 (P<0.05), and the serum PSA level of the
control group increased significantly (P<0.05). Compared with
T3, the serum PSA levels of the two groups at T4 were significantly
increased (P<0.05). At T2, T3 and T4, the serum PSA level in the
study group was significantly higher than that in the control group
(P<0.05). There was no significant difference in serum PSA level
between the two groups at T1 (P>0.05). Compared with T1, the
serum PSA levels of the two groups of patients at T2, T3 and T4
were significantly decreased (P<0.05), and the study group was
significantly lower than the control group (P<0.05) (Table VI).
 | Table VI.Comparison of serum PSA levels of two
groups of patients at different time points (mean ± SD, ng/ml). |
Table VI.
Comparison of serum PSA levels of two
groups of patients at different time points (mean ± SD, ng/ml).
| Group | n | T1 | T2 | T3 | T4 | F | P-value |
|---|
| Control group | 62 | 63.42±22.13 |
5.82±1.87a |
4.21±1.23a,b |
6.46±1.52a–c | 418.944 | <0.001 |
| Study group | 84 | 64.14±19.24 |
4.65±1.31a |
3.44±0.87a,b |
4.13±0.93a–c | 811.626 | <0.001 |
| t value | – | 0.210 |
4.446 |
4.431 | 11.450 | – | – |
| P-value | – | 0.834 | <0.001 | <0.001 | <0.001 | – | – |
Comparison of relative expression of
serum miR-493-5p in two groups of patients at different time
points
There was no significant difference in the relative
expression of serum miR-493-5p between the two groups at T1
(P>0.05). Compared with T1, the relative expression of
miR-493-5p in serum of the two groups of patients at T2, T3 and T4
were significantly increased (P<0.05). Compared with T2, the
relative expression levels of serum miR-493-5p at T3 and T4 were
significantly increased (P<0.05). Compared with T3, the relative
expression of serum miR-493-5p in the two groups at T4 was
significantly increased (P<0.05). At T2, T3 and T4, the relative
expression of serum miR-493-5p in the study group was significantly
higher than that in the control group (P<0.05) (Table VII).
 | Table VII.Comparison of relative expression
levels of serum miR-493-5p in two groups of patients at different
time points (mean ± SD). |
Table VII.
Comparison of relative expression
levels of serum miR-493-5p in two groups of patients at different
time points (mean ± SD).
| Group | n | T1 | T2 | T3 | T4 | F | P-value |
|---|
| Control group | 62 | 1.07±0.78 |
1.38±0.68a |
1.62±0.57a,b |
1.88±0.73a–c | 14.508 | <0.001 |
| Study group | 84 | 1.12±0.67 |
1.67±0.69a |
1.98±0.89a,b |
2.34±0.81a–c | 37.815 | <0.001 |
| t value | – | 0.416 | 2.526 | 2.789 | 3.535 | – | – |
| P-value | – | 0.678 | 0.013 | 0.006 | <0.001 | – | – |
Comparison of serum miR-195-5p
relative expression in two groups of patients at different time
points
There was no significant difference in the relative
expression of serum miR-195-5p between the two groups at T1
(P>0.05). Compared with T1, the relative expression of
miR-195-5p in serum at T2, T3 and T4 was significantly increased in
both groups (P<0.05). Compared with T2, the relative expression
of miR-195-5p in serum at T3 and T4 was significantly increased in
both groups (P<0.05). Compared with T3, the relative expression
of serum miR-195-5p in the two groups at T4 was significantly
increased (P<0.05). At T2, T3 and T4, the relative expression of
serum miR-195-5p in the study group was significantly higher than
that in the control group (P<0.05) (Table VIII).
 | Table VIII.Comparison of relative expression of
serum miR-195-5p between two groups of patients at different time
points (mean ± SD). |
Table VIII.
Comparison of relative expression of
serum miR-195-5p between two groups of patients at different time
points (mean ± SD).
| Group | n | T1 | T2 | T3 | T4 | F | P-value |
|---|
| Control group | 62 | 0.65±0.29 |
1.12±0.35a |
1.43±0.45a,b |
1.71±0.61a–c |
65.489 | <0.001 |
| Study group | 84 | 0.64±0.34 |
1.59±0.41a |
1.97±0.54a,b |
2.48±0.65a–c | 203.549 | <0.001 |
| t value | – | 0.187 | 7.278 | 6.401 | 7.261 | – | – |
| P-value | – | 0.852 | <0.001 | <0.001 | <0.001 | – | – |
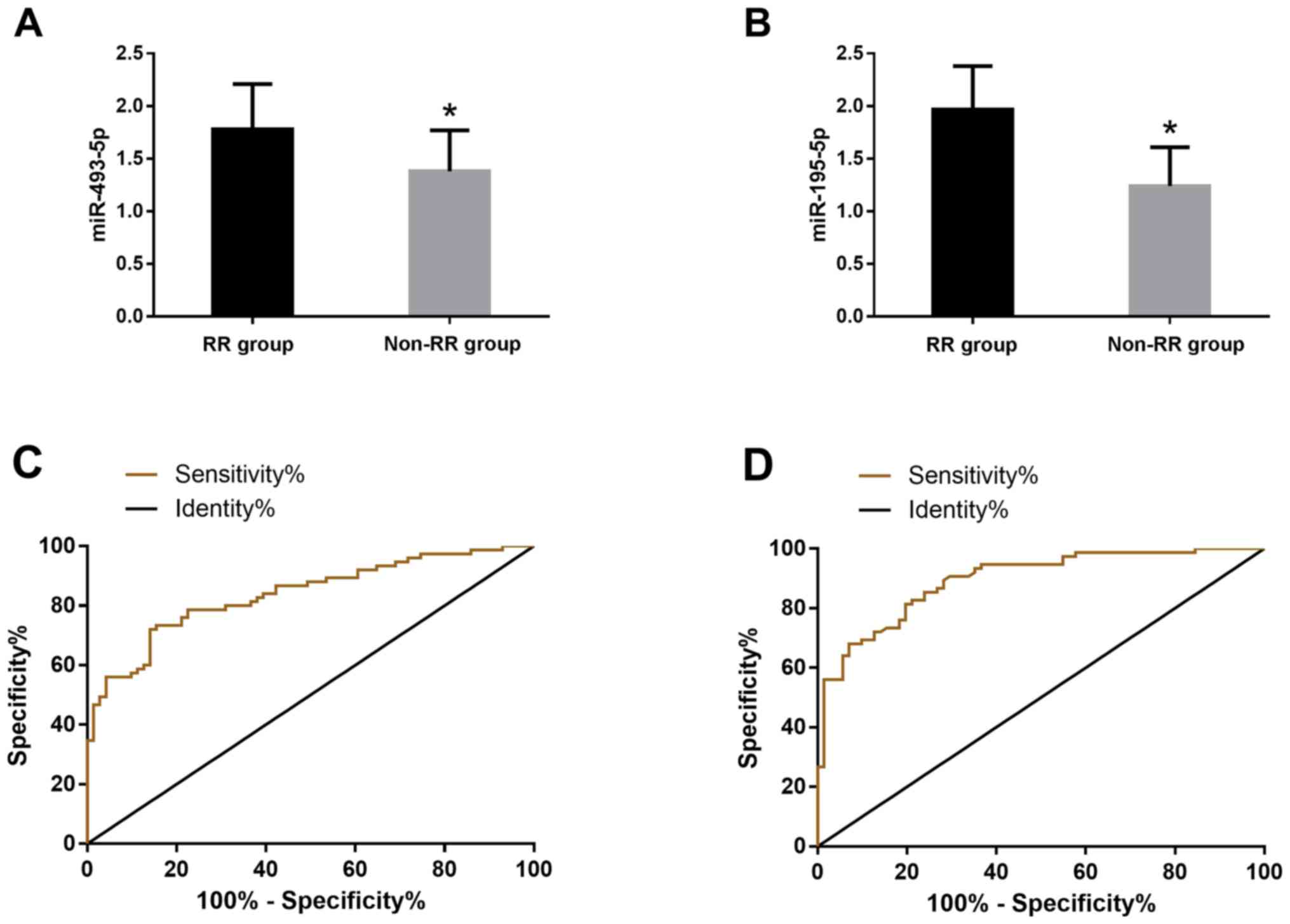
Diagnostic value of miR-493-5p and
miR-195-5p expression levels in patients
According to the clinical efficacy, the patients
were divided into RR group (n=71) and non-RR group (n=75). The
serum levels of miR-493-5p and miR-195-5p were detected in the two
groups. The expression levels of miR-493-5p in RR group and non-RR
group were 1.78±0.43 and 1.38±0.39, respectively, the difference
was statistically significant (P<0.05). The expression levels of
miR-195-5p in serum of RR group and non-RR group were 1.97±0.41,
1.24±0.37, the difference was statistically significant
(P<0.05). The receiver operating characteristic (ROC) curve of
the serum miR-493-5p and miR-195-5p expression levels in the
diagnosis of patients was drawn. The AUC value of the serum
miR-493-5p diagnosis was 0.829, the sensitivity was 72%, and the
specificity was 85.92%; the AUC of therapeutic effect of serum
miR-195-5p was 8.95, the sensitivity was 90.67%, and the
specificity was 71.83% (Fig. 2).
Discussion
PCa is one of the most common adult malignant
tumors. Approximately 220,000 American males are diagnosed with PCa
every year. Androgen deprivation therapy (ADT) is one of the main
methods for PCa treatment. Male patients with metastatic PCa almost
all develop drug resistance to primary ADT and develop CRPC
(18,19). In the past, treatment options for
CRPC patients were limited. In recent years, new androgen pathway
inhibitors are becoming the mainstream treatment methods for CRPC,
such as abiraterone acetate and enzalutamide (20). At present, there is no unified
administration method for treating CRPC through androgen pathway
inhibitor clinically, and the curative effect and side effects by
different administration methods are also different. It is of great
significance for CRPC patients to explore the administration method
with better curative effect and safety.
Serum PSA is widely used as a biomarker for PCa
diagnosis and is also a powerful prognostic marker for PCa
long-term risk (21,22). Some studies (23) show that the serum PSA level of CRPC
patients has significantly decreased after using abiraterone
acetate, and the early PSA change is related to the survival rate
of patients using abiraterone acetate, i.e. the increase of early
PSA leads to poor prognosis of early chemotherapy. The results of
this study show that the serum PSA levels of the two groups of
patients significantly decreased after treatment and the decrease
in the study group was greater. Similar to the above results, it
shows that the two administration methods in this study can
effectively reduce PSA levels, and the administration method of
abiraterone combined with flutamide could decrease the levels more
quickly.
Abiraterone acetate is the nursing standard of CRPC,
which can improve the overall survival time and progression-free
survival time of CRPC patients and reduce the deterioration of the
quality of life in metastatic CRPC patients. Currently, abiraterone
acetate has been approved by more than 70 countries (2014) for the
treatment of metastatic CRPC patients who have not received
chemotherapy (24,25). Research (26) results show that abiraterone acetate
also shows significant anti-tumor activity in CRPC patients after
receiving docetaxel, and has good effects on safety and tolerance.
Flutamide is the first nonsteroidal antiandrogen drug approved by
the U.S. Food and Drug Administration (FDA) for PCa, which can
block the action of androgen testosterone, prevent normal growth of
PCa cells and achieve the purpose of treating PCa (27). Basch et al (28) showed that compared with placebo
combined with prednisone, abiraterone combined with prednisone can
prolong the response pain progression and median time of CRPC
patients undergoing chemotherapy treatment, and the median time for
deterioration of health-related quality of life (HRQoL) is also
longer. Fizazi et al (29)
also used abiraterone combined with prednisone to treat CRPC
patients. The results are similar to those of Basch et al
(28). The median overall survival
time and radiological progression-free survival time of patients in
the abiraterone group (androgen deprivation therapy and abiraterone
conbined with prednisone) are significantly longer than those in
the placebo group (androgen deprivation therapy and double
placebo), and other indicators observed in the abiraterone group
are also better than those in the placebo group, such as the time
of pain progression, subsequent PCa treatment, chemotherapy
initiation and prostate specific antigen progression. In recent
years, it has been reported that the use of carbamide and flutamide
in patients with PCa prior to the use of abiraterone does not rule
out the effects of abiraterone (30). The results of this study show that RR
in the study group was significantly higher than that in the
control group after treatment, the total incidence of toxic and
side effects in the study group was significantly lower than that
in the control group, and OS in the study group was significantly
higher than that in the control group for 5 years. This indicates
that abiraterone combined with flutamide has better curative effect
and lower incidence of adverse reactions in CRPC patients than
single drug.
Wang et al (31) showed that miR-493-5p is downregulated
in PCa cells, c-Met, CREB1 and EGFR are downstream target genes of
miR-493-5p, and miR-493-5p inhibits cancer development through
AKT/GSK-3β/ Snail signaling in prostate cancer. Cai et al
(32) reported that the
downregulation of miR-195-5p in PCa tissue is significantly related
to high Gleason score, positive metastasis failure and biochemical
recurrence, and they confirmed the tumor inhibitory effect of
miR-195-5p through in vitro PCa cell invasion, migration and
apoptosis experiments. Linder et al (33) also reached the same conclusion as Cai
et al (32), that is,
miR-195-5p can inhibit PCa tumor, overexpression of miR-195-5p can
inhibit PCa cell migration, invasion and epithelial-mesenchymal
transition (EMT). They also pointed out that fibroblast growth
factor 2 (FGF2) is recognized as the direct target of miR-195-5p,
and miR-195-5p can inhibit PCa cell metastasis by downregulating
FGF2. After treatment, the relative expression of miR-493-5p and
miR-195-5p in the serum of the two groups of patients in this study
significantly increased. The above research shows that
overexpression of miR-493-5p and miR-195-5p significantly inhibits
the migration and invasion of PCa cells and acts as a tumor
inhibitor in PCa cells. Therefore, we speculate that abiraterone
and flutamide may inhibit the migration and invasion of PCa cells
by increasing the expression levels of miR-493-5p and miR-195-5p
and also their molecular mechanisms such as the antagonism of
androgen receptor miR-195-5p, thus, reducing the progress of PCa
and achieving the purpose of PCa treatment. At the end of the
study, we also examined the diagnostic value of miR-493-5p and
miR-195-5p expression levels in patients. The results showed that
the AUC values of the therapeutic effects of serum miR-493-5p and
miR-195-5p were respectively 0.829 and 0.895, indicating that they
both have a certain diagnostic value for the efficacy of PCa.
Collectively, abiraterone combined with flutamide
has better curative effect and lower incidence of adverse reactions
in CRPC patients than single drug, and can increase the expression
levels of miR-493-5p and miR-195-5p in patient serum.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
CY and YD conceived and designed the study, and
drafted the manuscript. CY, YD, SP and XG collected, analyzed and
interpreted the experimental data. XG revised the manuscript for
important intellectual content. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
The study was approved by the Ethics Committee of
Longhua Hospital Shanghai University of Traditional Chinese
Medicine (Shanghai, China). Signed informed consents were obtained
from the patients and/or guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Afshar-Oromieh A, Holland-Letz T, Giesel
FL, Kratochwil C, Mier W, Haufe S, Debus N, Eder M, Eisenhut M,
Schäfer M, et al: Diagnostic performance of 68Ga-PSMA-11 (HBED-CC)
PET/CT in patients with recurrent prostate cancer: Evaluation in
1007 patients. Eur J Nucl Med Mol Imaging. 44:1258–1268. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Watson PA, Arora VK and Sawyers CL:
Emerging mechanisms of resistance to androgen receptor inhibitors
in prostate cancer. Nat Rev Cancer. 15:701–711. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang Y, Chen R, Sun T, Zhao L, Liu F, Ren
S, Wang H, Lu X, Gao X, Xu C, et al: Efficacy and safety of
combined androgen blockade with antiandrogen for advanced prostate
cancer. Curr Oncol. 26:e39–e47. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kambale PR, Haldar D, Kabi BC and Kambale
KP: Study of vitamin D receptor gene polymorphism (FokI, TaqI and
ApaI) among prostate cancer patients in North India. J Clin Diagn
Res. 11:BC05–BC08. 2017.PubMed/NCBI
|
|
5
|
Benoist GE, Hendriks RJ, Mulders PF,
Gerritsen WR, Somford DM, Schalken JA, van Oort IM, Burger DM and
van Erp NP: Pharmacokinetic aspects of the two novel oral drugs
used for metastatic castration-resistant prostate cancer:
Abiraterone acetate and enzalutamide. Clin Pharmacokinet.
55:1369–1380. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yasui M, Uemura K, Yoneyama S, Kawahara T,
Hattori Y, Teranishi JI, Inoue M, Ohta JI, Yokomizo Y, Yao M, et
al: Predictors of poor response to secondary alternative
antiandrogen therapy with flutamide in metastatic
castration-resistant prostate cancer. Jpn J Clin Oncol.
46:1042–1046. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Reid AH, Attard G, Danila DC, Oommen NB,
Olmos D, Fong PC, Molife LR, Hunt J, Messiou C, Parker C, et al:
Significant and sustained antitumor activity in post-docetaxel,
castration-resistant prostate cancer with the CYP17 inhibitor
abiraterone acetate. J Clin Oncol. 28:1489–1495. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
de Bono JS, Logothetis CJ, Molina A,
Fizazi K, North S, Chu L, Chi KN, Jones RJ, Goodman OB Jr, Saad F,
et al COU-AA-301 Investigators, : Abiraterone and increased
survival in metastatic prostate cancer. N Engl J Med.
364:1995–2005. 2011. View Article : Google Scholar
|
|
9
|
Iguchi T, Tamada S, Kato M, Yasuda S,
Otoshi T, Hamada K, Yamasaki T and Nakatani T: Enzalutamide versus
flutamide for castration-resistant prostate cancer after combined
androgen blockade therapy with bicalutamide: A retrospective study.
Int J Clin Oncol. 24:848–856. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fukasawa S, Suzuki H, Kawaguchi K, Noguchi
H, Enjo K, Tran N, Todd M, Fizazi K and Matsubara N: Efficacy and
safety of abiraterone acetate plus prednisone in Japanese patients
with newly diagnosed, metastatic hormone-naïve prostate cancer: A
subgroup analysis of LATITUDE, a randomized, double-blind,
placebo-controlled, Phase 3 study. Jpn J Clin Oncol. 48:1012–1021.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nie W, Ge HJ, Yang XQ, Sun X, Huang H, Tao
X, Chen WS and Li B: LncRNA-UCA1 exerts oncogenic functions in
non-small cell lung cancer by targeting miR-193a-3p. Cancer Lett.
371:99–106. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fernandez S, Risolino M, Mandia N, Talotta
F, Soini Y, Incoronato M, Condorelli G, Banfi S and Verde P:
miR-340 inhibits tumor cell proliferation and induces apoptosis by
targeting multiple negative regulators of p27 in non-small cell
lung cancer. Oncogene. 34:3240–3250. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Beebe-Dimmer JL, Ruterbusch JJ, Bylsma LC,
Gillezeau C, Fryzek J, Schultz NM, Flanders SC, Barlev A, Heath E
and Quek RGW: Patterns of bicalutamide use in prostate cancer
treatment: A U.S. real-world analysis using the SEER-Medicare
database. Adv Ther. 35:1438–1451. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao L, Feng X, Song X, Zhou H, Zhao Y,
Cheng L and Jia L: miR-493-5p attenuates the invasiveness and
tumorigenicity in human breast cancer by targeting FUT4. Oncol Rep.
36:1007–1015. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wang G, Fang X, Han M, Wang X and Huang Q:
MicroRNA-493-5p promotes apoptosis and suppresses proliferation and
invasion in liver cancer cells by targeting VAMP2. Int J Mol Med.
41:1740–1748. 2018.PubMed/NCBI
|
|
16
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumours:
Revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tamada S, Iguchi T, Kato M, Asakawa J,
Kita K, Yasuda S, Yamasaki T, Matsuoka Y, Yamaguchi K, Matsumura K,
et al: Time to progression to castration-resistant prostate cancer
after commencing combined androgen blockade for advanced
hormone-sensitive prostate cancer. Oncotarget. 9:36966–36974. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Teoh JY, Ng CF and Poon DM: Chemohormonal
therapy for metastatic hormone-sensitive prostate cancer: An Asian
perspective. Asia Pac J Clin Oncol. 14 (Suppl 5):5–8. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Robinson D, Van Allen EM, Wu YM, Schultz
N, Lonigro RJ, Mosquera JM, Montgomery B, Taplin ME, Pritchard CC,
Attard G, et al: Integrative clinical genomics of advanced prostate
cancer. Cell. 161:1215–1228. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mittal RD, Mishra DK, Srivastava P,
Manchanda P, Bid HK and Kapoor R: Polymorphisms in the vitamin D
receptor and the androgen receptor gene associated with the risk of
urolithiasis. Indian J Clin Biochem. 25:119–126. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dong L, Zieren RC, Xue W, de Reijke TM and
Pienta KJ: Metastatic prostate cancer remains incurable, why? Asian
J Urol. 6:26–41. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shariat SF, Semjonow A, Lilja H, Savage C,
Vickers AJ and Bjartell A: Tumor markers in prostate cancer I:
Blood-based markers. Acta Oncol. 50 (Suppl 1):61–75. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Rescigno P, Lorente D, Bianchini D,
Ferraldeschi R, Kolinsky MP, Sideris S, Zafeiriou Z, Sumanasuriya
S, Smith AD, Mehra N, et al: Prostate-specific antigen decline
after 4 weeks of treatment with abiraterone acetate and overall
survival in patients with metastatic castration-resistant prostate
cancer. Eur Urol. 70:724–731. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Szmulewitz RZ, Peer CJ, Ibraheem A,
Martinez E, Kozloff MF, Carthon B, Harvey RD, Fishkin P, Yong WP,
Chiong E, et al: Prospective international randomized phase II
study of low-dose abiraterone with food versus standard dose
abiraterone in castration-resistant prostate cancer. J Clin Oncol.
36:1389–1395. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Nagai T, Naiki T, Iida K, Etani T, Ando R,
Hamamoto S, Sugiyama Y, Akita H, Kubota H, Hashimoto Y, et al:
Early abiraterone acetate treatment is beneficial in Japanese
castration-resistant prostate cancer after failure of primary
combined androgen blockade. Prostate Int. 6:18–23. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Xu L, Chen J, Liu W, Liang C, Hu H and
Huang J: Targeting androgen receptor-independent pathways in
therapy-resistant prostate cancer. Asian J Urol. 6:91–98. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ito Y and Sadar MD: Enzalutamide and
blocking androgen receptor in advanced prostate cancer: Lessons
learnt from the history of drug development of antiandrogens. Res
Rep Urol. 10:23–32. 2018.PubMed/NCBI
|
|
28
|
Basch E, Autio K, Ryan CJ, Mulders P,
Shore N, Kheoh T, Fizazi K, Logothetis CJ, Rathkopf D, Smith MR, et
al: Abiraterone acetate plus prednisone versus prednisone alone in
chemotherapy-naive men with metastatic castration-resistant
prostate cancer: Patient-reported outcome results of a randomised
phase 3 trial. Lancet Oncol. 14:1193–1199. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fizazi K, Tran N, Fein L, Matsubara N,
Rodriguez-Antolin A, Alekseev BY, Özgüroğlu M, Ye D, Feyerabend S,
Protheroe A, et al LATITUDE investigators, : Abiraterone plus
prednisone in metastatic, castration-sensitive prostate cancer. N
Engl J Med. 377:352–360. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zhao JG, Liu JD, Shen PF, Tang X, Sun GX,
Zhang XM, Chen JR, Shu KP, Shi M and Zeng H: Prior switching to a
second-line nonsteroidal antiandrogen does not impact the
therapeutic efficacy of abiraterone acetate in patients with
metastatic castration-resistant prostate cancer: A real-world
retrospective study. Asian J Androl. 20:545–550. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang S, Wang X, Li J, Meng S, Liang Z, Xu
X, Zhu Y, Li S, Wu J, Xu M, et al: c-Met, CREB1 and EGFR are
involved in miR-493-5p inhibition of EMT via AKT/GSK-3β/Snail
signaling in prostate cancer. Oncotarget. 8:82303–82313. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Cai C, Chen QB, Han ZD, Zhang YQ, He HC,
Chen JH, Chen YR, Yang SB, Wu YD, Zeng YR, et al: miR-195-5
inhibits tumor progression by targeting RPS6KB1 in human prostate
cancer. Clin Cancer Res. 21:4922–4934. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Linder S, van der Poel HG, Bergman AM,
Zwart W and Prekovic S: Enzalutamide therapy for advanced prostate
cancer: Efficacy, resistance and beyond. Endocr Relat Cancer.
26:R31–R52. 2018.PubMed/NCBI
|