Introduction
Tumors of the spinal cord and cauda equina have a
wide spectrum of histology and require care with diagnosis and
surgical intervention. The differential diagnosis for intradural
spinal tumors includes meningioma, nerve sheath tumors such as
schwannoma or neurofibroma, astrocytoma, ependymoma, and
metastasis. Spinal cord and cauda equina tumors are uncommon
neoplasms, and the majority is extramedullary tumors (1). Spinal involvement of extraskeletal
Ewing sarcoma in the epidural space or paravertebral area is also a
differential disease (2). Ewing
sarcoma is an aggressive bone and soft tissue tumor that usually
affects adolescents and young adults (3,4). The
Ewing sarcoma family of tumors are a group of high-grade small
round cell tumors, including primitive neuroectodermal tumor
(pPNET) and Askin tumor. Extraskeletal Ewing sarcoma is more likely
to arise in axial locations, compared to Ewing sarcoma of bone
(5). Most cases of Ewing sarcoma
occur in the long bones, pelvis, or ribs, and rarely in
extraskeletal regions such as the paravertebral or epidural space,
whereas a primary intradural extramedurally Ewing sarcoma (IEES) is
extremely rare. In general, Ewing sarcoma is treated with a
multimodal approach including surgery and/or focal radiotherapy, in
addition to systematic chemotherapy (4). However, because of its rarity and
limited evidence regarding the therapeutic aspects of IEES, there
are no standard treatment guidelines for these tumors even though
the aggressive malignant tumor causes severe neurologic morbidity
and mortality without appropriate treatment. In addition, the
initial imaging and clinical findings of IEES mimic those for
benign intradural spinal tumors. Therefore, it is important for
oncologists and neurosurgeons to be familiar with the clinical
presentation and evaluation of IEES. Here, we describe a case of
IEES with meningeal seeding, and we present a literature review of
the management and clinical course of this type of tumor.
Case report
A previously healthy 35-year-old woman developed
severe lumbago and radicular leg pain on both sides. The symptoms
gradually worsened for 2 months after appearance and paresthesia of
both legs progressed. Neurologically, straight leg raising and
femoral nerve stretch tests were negative on both sides. There was
hypoesthesia in the right-side dominant L5-S1 dermatomes. Patellar
tendon and Achilles tendon reflexes were normal and Babinski and
Chaddock reflexes were negative on both sides. The manual muscle
test score was 3 in the right gastrocnemius muscle. Bladder and
bowel functions were normal.
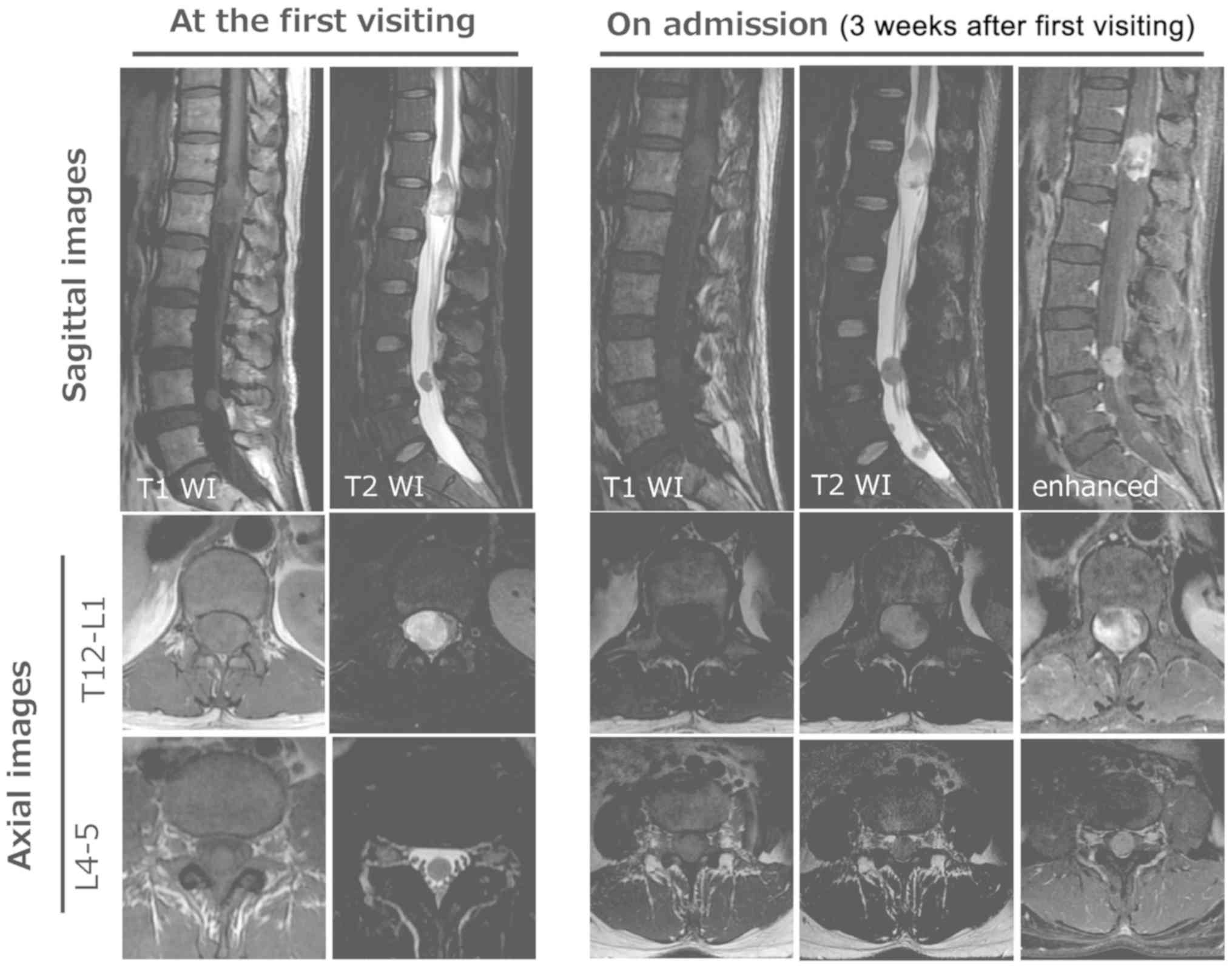
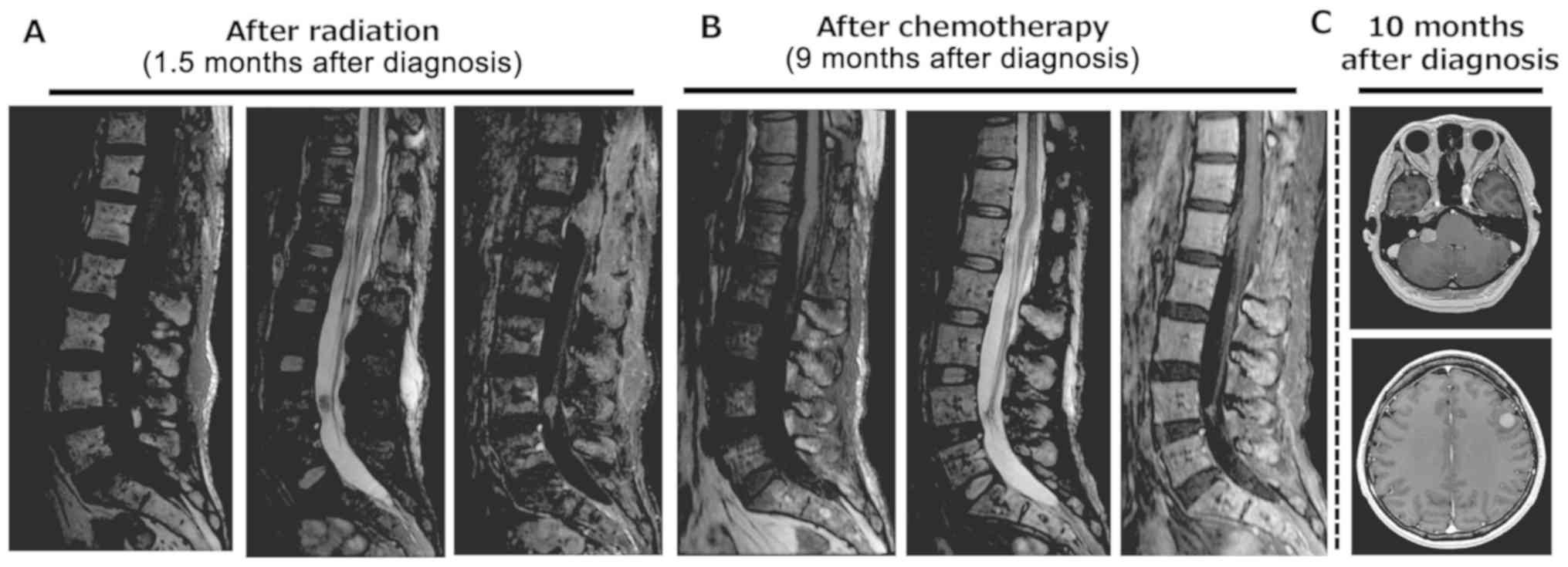
Magnetic resonance imaging (MRI) at a previous
hospital showed tumorous lesions at the T12-L1 and L4-5 levels
(Fig. 1). The lesion at L4-5 was
oval with an isointense signal on T1-weighted images and low-signal
intensity on T2-weighted images. The lesion at T12-L1 was semi-oval
with an isointense signal on T1-weighted images and low- to
high-signal inhomogeneous intensity on T2-weighted images. Surgical
treatment was planned based on suspicion of benign multiple
schwannoma and ependymoma, but MRI taken 3 weeks after the first
visit showed growth and an increased number of intradural tumors.
Gadolinium-contrast T1-weighted images showed diffuse enhancement
in the tumorous lesions (Fig.
1).
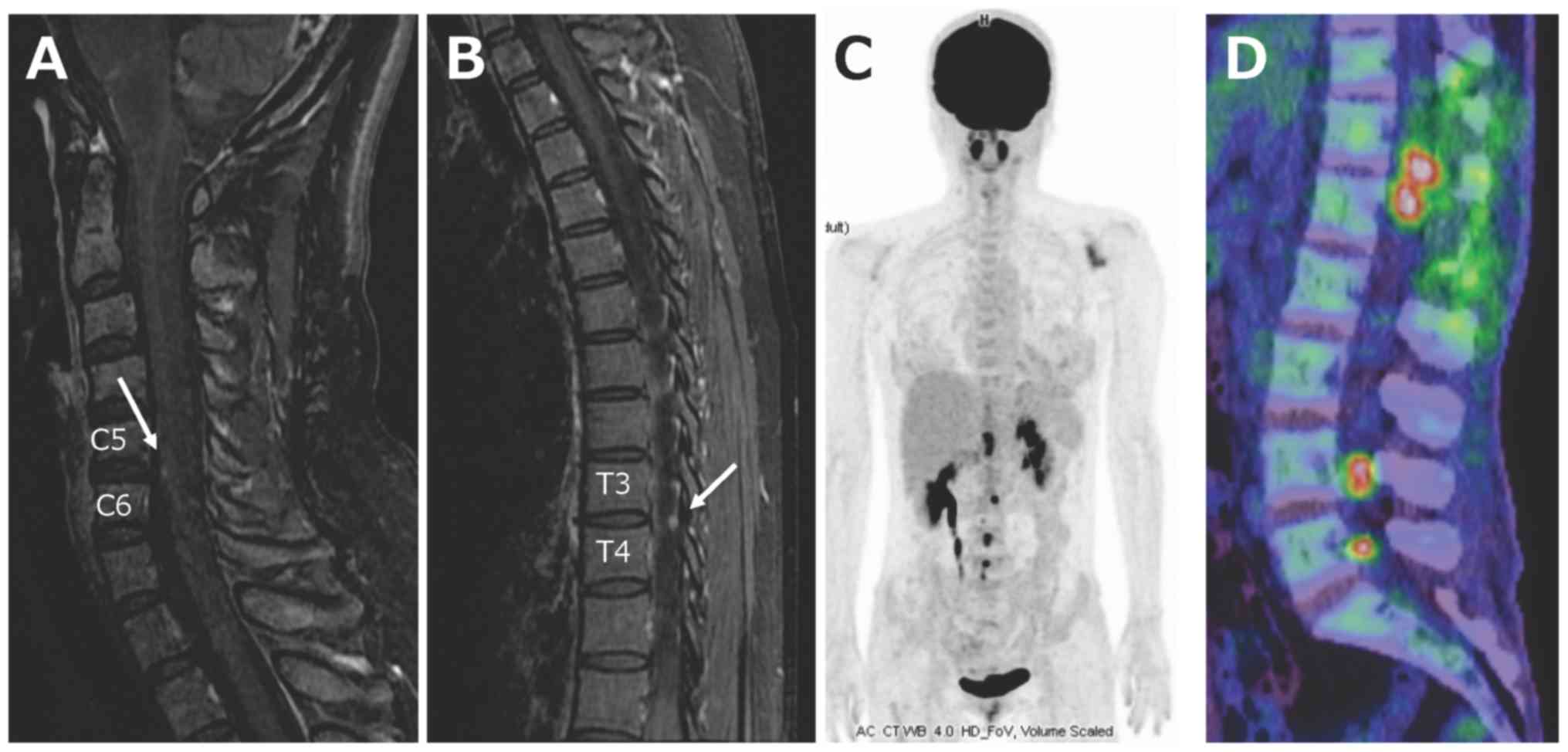
The rapid changes on MRI led us to strongly suspect
a malignant tumor, and we performed a whole-body imaging test. MRI
of the cervical and thoracic spinal cord showed enhanced skip
lesions on contrast-enhanced T1-weighted images, but brain MRI
showed no brain metastases. Computed tomography (CT) of the chest,
abdomen and pelvis, and whole-body positron emission tomography
(PET) showed no disease (Fig. 2).
From these findings, a malignant tumor was suspected, including
metastases of meningeal dissemination, malignant peripheral nerve
sheath tumor, malignant lymphoma, and anaplastic ependymoma (WHO
grade 3).
The tumor occupied the entire space within the dural
tube at the T12-L1 level on a transaxial MR image, and the right
leg-dominant neurological deficit had rapidly progressed. For
diagnosis and prevention of neurological deficits, laminectomy
between T12 and L1 and tumor resection were performed. The
amplitude of intraoperative neurologic monitoring (motor-evoked
potentials: MEPs) in the right quadriceps, tibialis anterior,
gastrocnemius muscles and sphincter dropped during tumor
detachment, and gross total resection was difficult due to severe
adhesion to the cauda equina and epiconus.
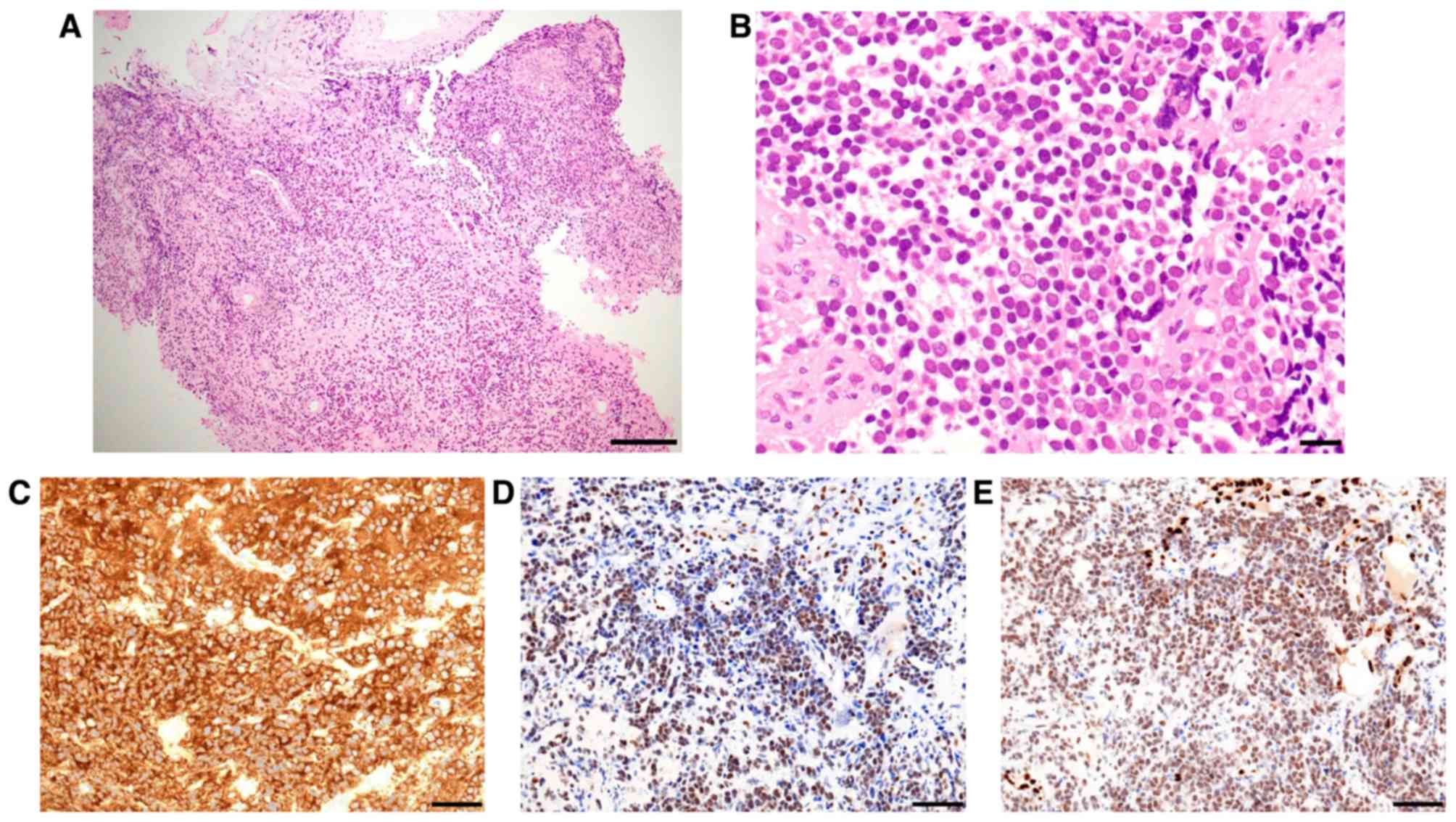
Microscopically, the tumor consisted of dense sheets
of small round cells based on hematoxylin-eosin staining.
Immunohistochemically, most tumor cells showed intense and diffuse
staining for CD99, ERG and FLI1, and were negative for GFAP, EMA,
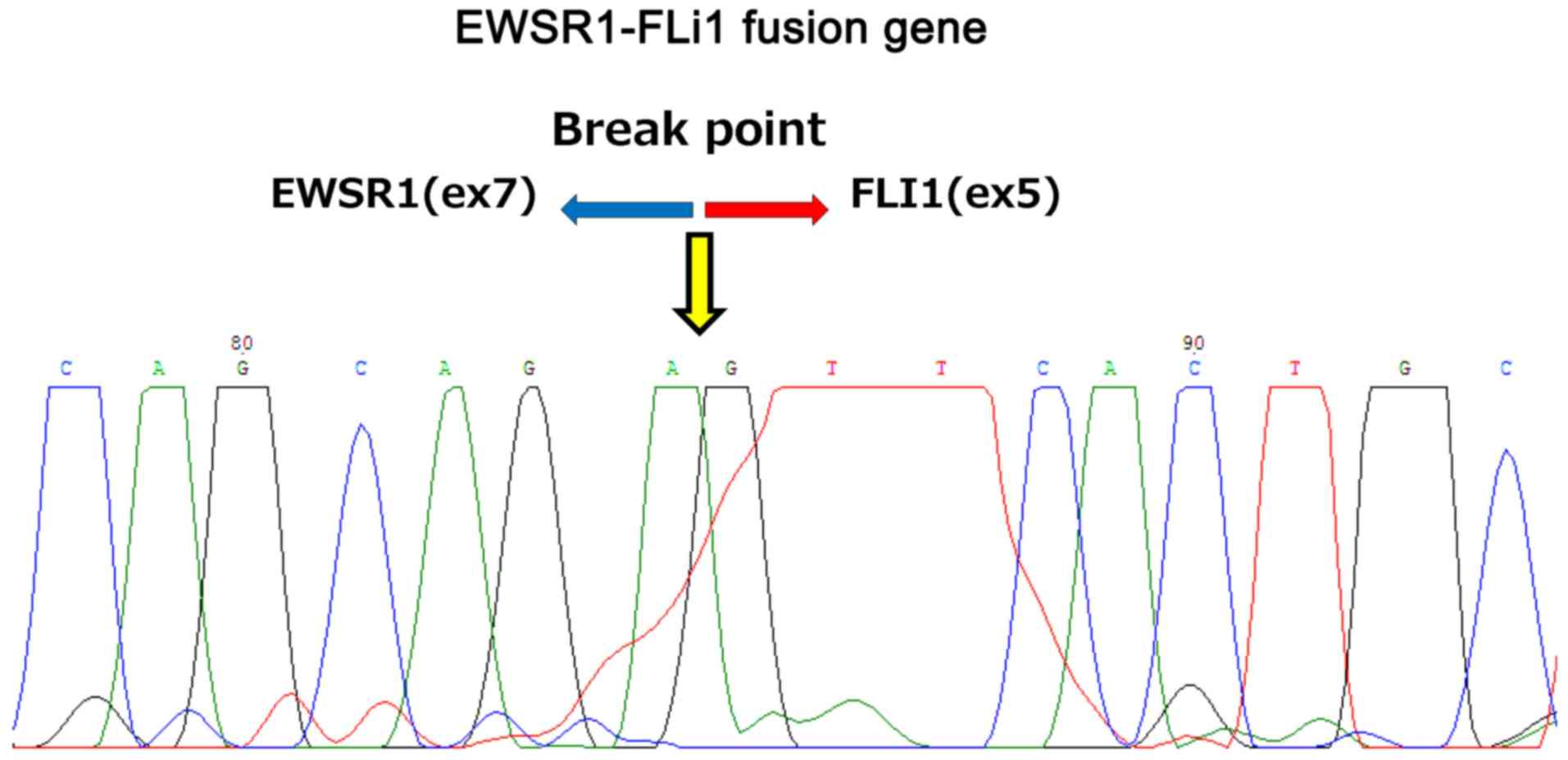
AE1/AE3, S-100, chromogranin A, and CD57 (Fig. 3). A nucleotide sequence analysis of
the reverse transcription-polymerase chain reaction (RT-PCR)
products confirmed that the gene fusion was formed between exon 7
of the EWSR1 gene and exon 5 of the FLI1 gene (Fig. 4). The lesion was diagnosed as primary
intradural Ewing sarcoma at the cauda equina with meningeal
seeding.
Chemotherapy (8 cycles of vincristine, doxorubicin
and cyclophosphamide (VDC) alternating with ifosfamide and
etoposide (IE)) following radiotherapy (total dose of 45 Gy in 25
fractions for the whole spinal lesion excluding the brain) were
performed after diagnosis. For Ewing sarcoma, we usually administer
vincristine (1.5 mg/m2 on day 1), doxorubicin (37.5
mg/m2 on days 1 and 2), and cyclophosphamide (1200
mg/m2 on day 1) (VDC) alternating with ifosfamide (1.8
g/m2 on days 1–5) and etoposide (100 mg/m2 on
days 1–5) (IE) every 3 weeks. The first course of VDC and second
course of IE were administered as full doses. However, we reduced
the dosage to 75% and delayed the start of chemotherapy for 1 week
in the 3rd to 6th courses due to severe myelosuppression, and we
reduced the dosages to 50% of standard chemotherapy in the 7th and
8th courses. Neurological symptoms improved with tumor shrinkage
after radiation and chemotherapy; however, multiple brain
metastases presenting with symptoms of double vision and hoarseness
were found at 10 months after diagnosis (Fig. 5). Whole-brain irradiation and
chemotherapy with another regimen were administered, but the
patient died of diffusely disseminated disease limited to the
central nervous system, without evidence of distant metastases, at
16 months after the initial diagnosis.
Histopathology
Histopathological examination was performed on
resected specimen fixed 10% formalin for 24 hours at room
temperature. Paraffin-embedded sections cut by 4 µm thickness were
performed hematoxylin and eosin (H&E) and following
immunohistological staining. For immunohistological examination, we
used CD99 antibody (cat. no. M3601, DAKO) (1:300 dilution), FLI1
antibody (cat. no. ab15289, abcam) (1:50 dilution) and ERG antibody
(cat. no. 41811, Nichirei). For CD99 immunostaining, we didnt
perform antigen activation after deparaffinization. For FLI1
immunostaining, we performed antigen activation at 95°C for 20
minutes at pH 6.0 using citrate buffer. For ERG immunostaining, we
performed antigen activation at 95°C for 20 minutes at pH 9.0 using
TE buffer. We adopted the protocol by using the BONDIII Fully
Automated IHC and ISH Stainer (Leica Microsysems, Japan) for all
immunohistological staining. Slides were observed under a light
microscope.
RT-PCR and sequencing analyses
Total RNA (53 ng/µl) was extracted from FFPE
sections using ISOGEN (Nippon Gene), according to the manufacturers
instructions. For specific amplification of the putative EWSR1-FLI1
junction regions, we performed a two-step PCR reaction. The
sequences of first primers are EWSR1(ex6) forward,
GAGACTAGTCAACCTCAATCTAGC and FLI1(ex6) reverse,
AAGCTCCTCTTCTGACTGTG, EWSR1(ex7s) forward CCCACTAGTTACCCACCCCAAA
and FLI1(ex8) reverse, GCCCAGGATCTGATACGGAT. The first PCR products
were used as template for subsequent PCR reaction using the
following nest primers; EWSR1(ex7s) forward, CCCACTAGTTACCCACCCCAAA
and FLI1(ex5) reverse, TCGGTGTGGGAGGTTGTATT and FLI1(ex7) reverse,
TGATCGTTTGTGCCCCTCCA. The first and nested PCR were performed with
the following cycling conditions: 94°C for 3 min, 40 cycles of
94°C, 60°C, and 72°C for 1 min, 72°C for 10 min. ABI PRIZM BigDye
Terminator Cycle Sequencing Ready Reaction kits (PE Biosystems) was
used for direct sequencing of the nested PCR products. EWSR1-FLI1
fusion gene analysis was performed using ABI PRISM 310 Genetic
Analyzer (PE Biosystems). Sequencing reaction products were
electrophoresed on 2% agarose gels and stained with ethidium
bromide.
Statistical analysis
The statistical analysis was conducted using SPSS
software (v24.0, SPSS). The Kaplan-Meier method was used for
calculation of survival. Overall survival (OS) was defined as the
time from diagnosis until the most recent follow-up or death of any
cause. Progression-free survival was defined as the time from
diagnosis until disease progression, death of any cause, or most
recent follow-up.
Discussion
We present an extremely rare case of primary
intradural extramedurally Ewing sarcoma (IEES). Clinical
information for 30 cases of primary IEES reported from 1997 to 2019
is summarized in Table I (6–30). Of
the 30 patients, 18 were male (60%) and 12 were female (40%). The
median age at diagnosis was 31 years. The lumbar-sacral region was
the most common location (n=20, 66.7%), and multiple lesions viewed
as meningeal dissemination were found in 8 patients (26.7%) at
diagnosis. The most common chief symptom was pain (n=25, 83.3%).
Motor disturbance of a lower or upper limb occurred in 15 patients
(50.0%), and bladder and rectal disturbance were present in 8
patients (26.7%).
 | Table I.Summary of reported cases of primary
intradural extramedurally Ewing sarcoma. |
Table I.
Summary of reported cases of primary
intradural extramedurally Ewing sarcoma.
| Case | Age, years | Sex | Location | IHC (+) | IHC (−) | EWS-FLI1 | Surgery | Chemotherapy
regimen | Radiation area | PFS, months | Recurrence | OS, months | Outcome | Refs. |
|---|
| 1 | 14 | M | Th12-L2 | NSE, synaptophysin,
S-100 | GFAP, Desimin,
actin | + | GTR | NA | NA | 3M | – | 3M | alive | (6) |
| 2 | 52 | M | L2-5 | CD99, synaptophysin,
vimentin | EMA, LCA lympho
marker | NA | GTR | NA | craniospinal | 12M | – | 12M | CDF 1M | (7) |
| 3 | 11 | F | C7-T1 | CD99, NSE
(weakly) | CD20, CD45, CD3,
Synaptophysin | NA | STR | NA | NA | NA | NA | NA | NA | (8) |
| 4 | 31 | F | L1-S2 | CD99, NSE,
synaptophysin, vimentin | LCA, desmin,
GFAP | NA | STR | VCR, CCNU, CDDP | focal | 2M | + | 4M | DOD 4M | (9) |
| 5 | 32 | M | L2-4 | CD99, vimentin | NA | + | STR | Act-D+VDC/IE | focal | 8M | + | 12M | DOD 12M | (10) |
| 6 | 26 | M | T11-S2 | MIC2 | LCA | NA | GTR | VAC, ICE | focal | 2M | + | 8M | AWD 8M | (11) |
| 7 | 32 | F | C3-C5 | CD99, Vimentin | NA | NA | STR | IE | focal | 12M | – | 12M | CDF 12M | (12) |
| 8 | 10 | M | L4-S2 | CD99,
synaptophysin | S100, CAM5.2 | NA | STR | VDC/IE | focal | 12M | – | 12M | CDF 12M | (13) |
| 9 | 10 | M | C2-3 | CD99, vimentin | GFAP, NSE, S-100,
LCA, lymphoid markers | NA | GTR | – | – | 1M | + | 1M | DOD 1M | (14) |
| 10 | 40 | F | T11-L4 | Fli1 | NA | + | STR | DXR, holoxan | focal | 6M | – | 6M | CDF 6M | (15) |
| 11 | 8 | M | L2-4 | CD99, NSE | Syn, CgA, L26, CD3,
GFAP | NA | + | NA | NA | NA | – | NA | alive | (16) |
| 12 | 25 | M | L2-3 | CD99, NSE,
S-100 | L26, UCHI, CD3,
CD30, Syn, CK | NA | + | NA | NA | 6M | + | 6M | AWD 6M | (16) |
| 13 | 56 | F | L1 | CD99, s-100,
synaptophysin, nurofilament protein | GFAP, EMA, CD20,
CD3, keratin, chromogranin, HMB45 | + | GTR | VDC/IE | NA | NA | NA | NA | CDF | (17) |
| 14 | 55 | M | L4-S2 | CD99,
cavelolin, | CD45, EMA, GFAP
chromogranin | + | GTR | VIDE | focal | 13M | – | 13M | CDF 13M | (18) |
| 15 | 25 | F | L2-3 | CD99, caveolin | CD45, CkAE1-AE3,
GFAP, chromogranin, p53 | + | GTR | – | – | 14M | + | 14M | alive | (18) |
| 16 | 28 | F | L5-S1 | S100,
Synaptophysin, CD99 | EMA, GFAP,
CD20 | + | GTR | VDC/IE | focal | 72M | – | 72M | CDF 72M | (19) |
| 17 | 44 | F | T6-7, L1-2 | CD99 | NA | NA | GTR | VDC/IE | focal | 31M | + | 31M | AWD 31M | (20) |
| 18 | 39 | F | C4-6 | CD99 | NA | NA | GTR | VCR, THR, CTX | focal | 36M | + | 36M | alive | (21) |
| 19 | 44 | F | L1-S3 | CD99,
vimentin, | NSE, Sinaptophysin,
GFAP, S-100, LCA, etc. | NA | GTR | VDC/IE | focal | 6M | – | 6M | CDF 6M | (22) |
| 20 | 14 | M | L2-S1 | CD99 | CD34, CD 20, S100,
NSE, GFAP, Desmin, myogenin | NA | STR | VDC | focal | NA | NA | 12M | CDF 12 M | (23) |
| 21 | 29 | M | C7 | MIC2, vimentin,
cytkeratin, synaptophysin | NA | + | GTR | VCR, IFO, DXR,
VP-16 | – | 1M | + | NA | NED 18M | (24) |
| 22 | 5 | M | T4-T7 | CD99, FLI-1,
NSE, | Desmin, Myogenin,
TdT, CKHMW synaptophysin | NA | STR | NA | NA | NA | NA | NA | NA | (25) |
| 23 | 50 | M | T10-L1 | MIC2(CD99), CD56
AE1/AE3 | CD45, S100,
GFAP | + | GTR | VDC/IE | focal | 48M | + | 60M | DOD 60M | (26) |
| 24 | 60 | M | L2-3 | MIC2, CAM5.2,
synaptophysin, vimentin | NA | + | partial | IE/AI | focal | 11M | + | 48M | DOD 48M | (26) |
| 25 | 25 | M | C4-7 | CD99 | Actin, MYOD1,
chromogranin, synaptophysin | + | STR | VDC/IE | focal | NA | + | 20M | NED 20M | (26) |
| 26 | 34 | M | L4-5/S1- | CD99, EMA,
synaptophysin | NA | + | biopsy | VDC/IE | craniospinal | 3M | – | 3M | CDF 3M | (26) |
| 27 | 14 | F | L2-3 | CD99, Fli1 | EMA, S100, CD20
synaptophysin | + | STR | VDC/IE | focal | 24M | – | 24M | CDF 24M | (27) |
| 28 | 31 | M | L2-L3, L5 | CD99 | GFAP, EMA,
cytokeratin, AE1/AE3, S-100 | + | partial | CPA,VCR, ADR,
Act-D,IFO,VP-16 | – | 24M | + | 42M | alive | (28) |
| 29 | 61 | M | L1-3 | AE1/AE3, CD99,
synaptophysin | GFAP, CD45 | + | GTR | VDC/IE | focal | NA | NA | NA | alive | (29) |
| 30 | 34 | F | C4-T3 | CD99, CD56 | Lymphoid, EMA,
GFAP, Chromogranin | + | partial | – | craniospinal | 9M | + | 11M | DOD 11M | (30) |
Ewing sarcoma is categorized as a small round cell
sarcoma with pathognomonic molecular findings and varying degrees
of neuroectodermal differentiation by immunohistochemistry. Classic
Ewing sarcoma lacks neural differentiation and typically has only
characteristic diffuse membranous CD99 (encoded by the MIC gene)
positivity (31). Almost all cases
in Table I (n=28, 93.3%) showed CD99
or MIC2 positivity. Ewing sarcoma has a specific translocation
involving the EWSR1 gene on chromosome 22, which produces an
EWSR1-FLI1 fusion gene transcript and oncoprotein. RT-PCR or
fluorescence in situ hybridization (FISH) can be used to detect the
fusion gene, and this was detected in 16 of the reported primary
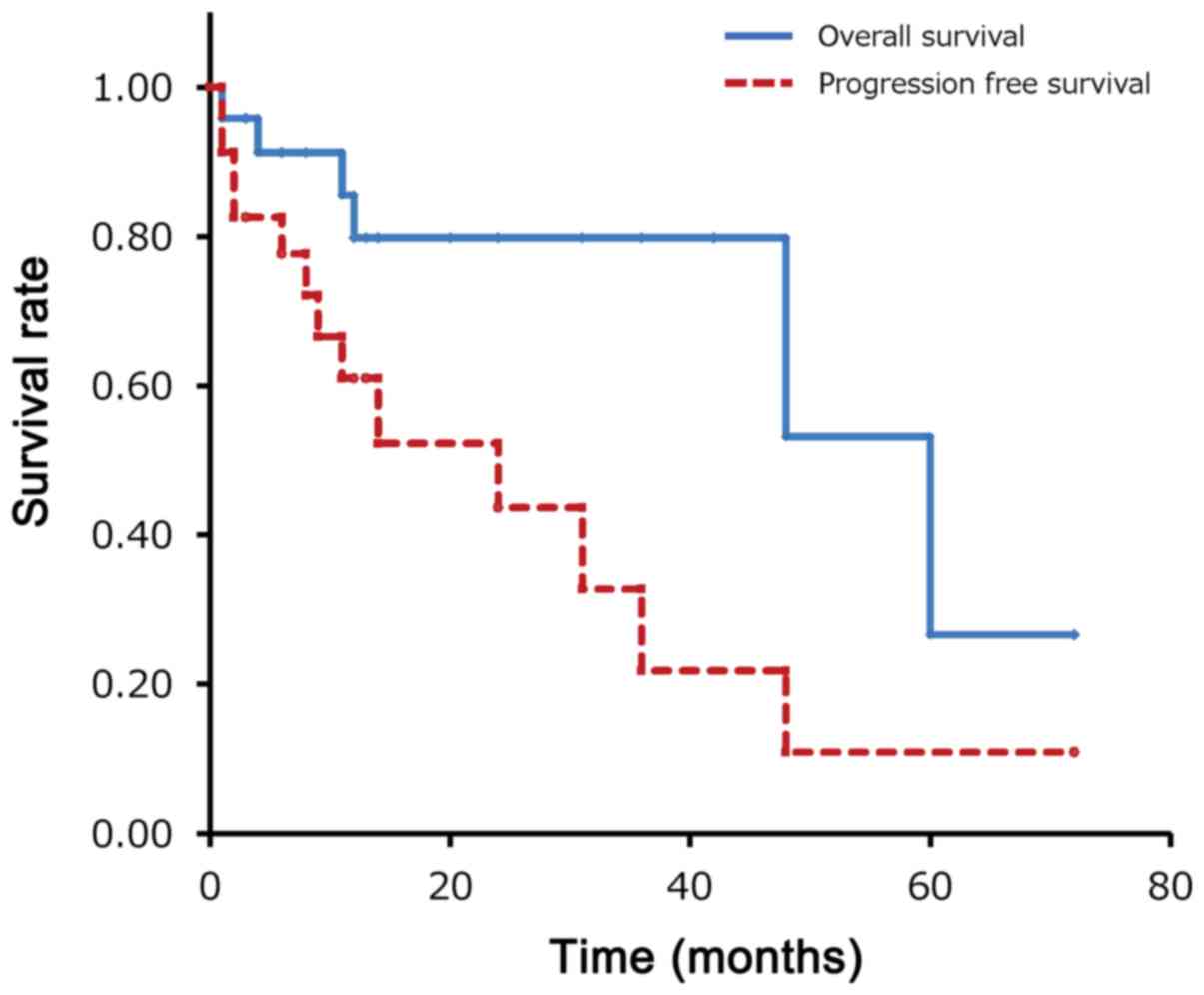
IEES cases. The 1- and 5-year OS rates were 79.8% and 26.6%, and
the 1-, 2- and 5-year progression free survival rates were 61.0%,
52.3% and 10.9% (Fig. 6). Although
the Kaplan-Meier survival analysis has certain limitation because
the patients in Table I had a short
duration of follow-up, these results suggest that IEES has a poorer
prognosis than conventional localized Ewing sarcoma, which has a
5-year OS of 65–75%. The prognosis of IEES was the same as that of
conventional Ewing sarcoma with metastases (4).
In general, patients with Ewing sarcoma receive
neoadjuvant chemotherapy upon diagnosis of Ewing sarcoma by biopsy.
However, spinal tumors are usually diagnosed after resection. All
patients in Table I also received
adjuvant chemotherapy after diagnosis. In the current case,
multiagent chemotherapy was given, including VDC alternating with
IE, as described above. However, we had to reduce the dosage and
delay the start of chemotherapy for 1 week after the 3rd course
because of severe myelosuppression. Zhang et al (32), suggested that adults with Ewing
sarcoma should be treated with adequate cycles of intensive
chemotherapy at appropriate intervals. Therefore, it is possible
that the effect of chemotherapy was not sufficient in our case.
Ewing sarcoma is radiosensitive (33), and in our case we used whole spine
radiotherapy without whole brain irradiation. Chihak et al
(26), suggested that craniospinal
radiotherapy, rather than focal radiotherapy, is critical for
preventing distant metastasis, and skip metastases of intradural
Ewing sarcoma to distant sites have been reported (11,20,26). The
patient in our case had a 2-year-old baby, and she refused
craniospinal radiotherapy because she was afraid of late cerebral
dysfunction. The outcome in this case suggests that craniospinal
radiotherapy might be more effective for local control than whole
spine radiotherapy.
In conclusion, IEES is an extremely rare malignant
tumor that requires multimodal therapy with surgery, craniospinal
radiotherapy and systematic chemotherapy. The poorer prognosis of
primary IEES compared to that of conventional Ewing sarcoma of bone
suggests that new agents and treatment strategies are needed.
Acknowledgements
The authors would like to acknowledge Mr. Manabu
Yamashita, laboratory technician at the Department of Pathology,
Kanazawa University, Kanazawa, Japan, for performing of FISH and
PCR tests.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors contributions
YIz and HN examined the patient, analyzed the
clinical, radiological and laboratory results, and wrote the
manuscript. KH assisted with data analysis. HN and KH were involved
in the surgical treatment. YIm and TN analyzed and interpreted the
pathological findings and FISH tests. AM designed the study,
including proofreading of the manuscript and revising it
critically. HN and AM proofread the manuscript and revised it
critically. AM made critical revisions of the article for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Human Ethics
Review Committee of Fukui University Medical Faculty (Histological
and biological analysis of disorders affecting the spine, bones and
joints; approval no. 2014046) and strictly followed the Clinical
Research Guidelines of the Ministry of Health, Labor, and Welfare
of the Japanese Government.
Patient consent for publication
The patient and parents provided written informed
consent for analysis and publication of the case.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Van Goethem JW, van den Hauwe L, Ozsarlak
O, De Schepper AM and Parizel PM: Spinal tumors. Eur J Radiol.
50:159–176. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Harimaya K, Oda Y, Matsuda S, Tanaka K,
Chuman H and Iwamoto Y: Primitive neuroectodermal tumor and
extraskeletal Ewing sarcoma arising primarily around the spinal
column: Report of four cases and a review of the literature. Spine.
28:E408–E412. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Balamuth NJ and Womer RB: Ewings sarcoma.
Lancet Oncol. 11:184–192. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gaspar N, Hawkins DS, Dirksen U, Lewis IJ,
Ferrari S, Le Deley MC, Kovar H, Grimer R, Whelan J, Claude L, et
al: Ewing sarcoma: Current management and future approaches through
collaboration. J Clin Oncol. 33:3036–3046. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Applebaum MA, Worch J, Matthay KK, Goldsby
R, Neuhaus J, West DC and Dubois SG: Clinical features and outcomes
in patients with extraskeletal Ewing sarcoma. Cancer.
117:3027–3032. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hisaoka M, Hashimoto H and Murao T:
Peripheral primitive neuroectodermal tumour with
ganglioneuroma-like areas arising in the cauda equina. Virchows
Arch. 431:365–369. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Isotalo PA, Agbi C, Davidson B, Girard A,
Verma S and Robertson SJ: Primary primitive neuroectodermal tumor
of the cauda equina. Hum Pathol. 31:999–1001, 200.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Uesaka T, Amano T, Inamura T, Ikezaki K,
Inoha S, Takamatsu M, Iwaki T and Fukui M: Intradural,
extramedullary spinal Ewings sarcoma in childhood. J Clin Neurosci.
10:122–125. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Akyüz M, Demiral AN, Gürer IE, Uçar T and
Tuncer R: Primary primitive neuro-ectodermal tumor of cauda equina
with intracranial seeding. Acta Neurochir (Wien). 146:525–528.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Mobley BC, Roulston D, Shah GV, Bijwaard
KE and McKeever PE: Peripheral primitive neuroectodermal
tumor/Ewings sarcoma of the craniospinal vault: Case reports and
review. Hum Pathol. 37:845–853. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Haresh KP, Chinikkatti SK, Prabhakar R,
Rishi A, Rath GK, Sharma DN and Julka PK: A rare case of intradural
extramedullary Ewings sarcoma with skip metastasis in the spine.
Spinal Cord. 46:582–584. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kim SW and Shin H: Primary intradural
extraosseous Ewings sarcoma. J Korean Neurosurg Soc. 45:179–181.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Klimo P Jr, Codd PJ, Grier H and
Goumnerova LC: Primary pediatric intraspinal sarcomas. Report of 3
cases. J Neurosurg Pediatr. 4:222–229. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yan Y, Xu T, Chen J, Hu G and Lu Y:
Intraspinal Ewings sarcoma/primitive neuroectodermal tumors. J Clin
Neurosci. 18:601–606. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Vincentelli F, Caruso G and
Figarella-Branger D: Primary intradural Ewings sarcoma of the cauda
equina presenting with acute bleeding. Acta Neurochir (Wien).
152:563–564. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Duan XH, Ban XH, Liu B, Zhong XM, Guo RM,
Zhang F, Liang BL and Shen J: Intraspinal primitive neuroectodermal
tumor: Imaging findings in six cases. Eur J Radiol. 80:426–431.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Karikari IO, Mehta AI, Nimjee S, Hodges
TR, Tibaleka J, Montgomery C, Simpson L, Cummings TJ and Bagley CA:
Primary intradural extraosseous Ewing sarcoma of the spine: Case
report and literature review. Neurosurgery. 69:E995–E999. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Pancucci G, Simal-Julian JA, Plaza-Ramirez
E, García-Marcos R, Mayordomo-Aranda E and Botella-Asunción C:
Primary extraosseous intradural spinal Ewings sarcoma: Report of
two cases. Acta Neurochir (Wien). 155:1229–1234. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Khalatbari MR, Jalaeikhoo H and Moharamzad
Y: Primary intradural extraosseous Ewings sarcoma of the lumbar
spine presenting with acute bleeding. Br J Neurosurg. 27:840–841.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bazzocchi A, Bacci A, Serchi E, Salerno A,
Salizzoni E and Leonardi M: Intradural extramedullary Ewings
sarcoma. Recurrence with acute clinical presentation and literature
review. Neuroradiol J. 26:476–481. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gong HS, Huang QS, Liu GJ, Chen FH and
Zhao HB: Cervical primary Ewings sarcoma in intradural and
extramedullary location and skip metastasis to Cauda Equina. Turk
Neurosurg. 25:943–947. 2015.PubMed/NCBI
|
|
22
|
Lozupone E, Martucci M, Rigante L, Gaudino
S, Di Lella GM and Colosimo C: Magnetic resonance image findings of
primary intradural Ewing sarcoma of the cauda equina: Case report
and review of the literature. Spine J. 14:e7–e11. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Zhao M, Zhang B, Liang F and Zhang J:
Primary spinal intradural extraskeletal Ewing sarcoma mimicking a
giant nerve sheath tumor: Case report and review of the literature.
Int J Clin Exp Pathol. 7:9081–9085. 2014.PubMed/NCBI
|
|
24
|
Bostelmann R, Leimert M, Steiger HJ,
Gierga K and Petridis AK: The importance of surgery as part of
multimodal therapy in rapid progressive primary extraosseous Ewing
sarcoma of the cervical intra- and epidural space. Clin Pract.
6:8972016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kartal A and Akatlı A: Primary intradural
extraosseous Ewings sarcoma in a young child. Childs Nerv Syst.
32:409–410. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chihak MA, Ahmed SK, Lachance DH,
Nageswara Rao AA and Laack NN: Patterns of failure and optimal
radiotherapy target volumes in primary intradural extramedullary
Ewing sarcoma. Acta Oncol. 55:1057–1061. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Scantland JT, Gondim MJ, Koivuniemi AS,
Fulkerson DH and Shih CS: Primary spinal intradural extraosseous
Ewing sarcoma in a pediatric patient: Case report and review of the
literature. Pediatr Neurosurg. 53:222–228. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Paterakis K, Brotis A, Tasiou A, Kotoula
V, Kapsalaki E and Vlychou M: Intradural extramedullary Ewings
sarcoma: A case report and review of the literature. Neurol
Neurochir Pol. 51:106–110. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Takami H, Kumar R, Brown DA and Krauss WE:
Histologic features and prognosis of spinal intradural
extramedullary ewing sarcoma: Case report, literature review, and
analysis of prognosis. World Neurosurg. 115:448–452.e2. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tan CH, Tan D, Phung TB and Lai LT:
Primary intradural extramedullary Ewing sarcoma of the cervical
spine: A case report and review of the literature. J Clin Neurosci.
66:280–284. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Fletcher CDM, Bridge JA, Hogendoorn PCW
and Mertens F: WHO Classification of Tumours of Soft Tissue and
Bone. 4th. IARC; Lyon, France: 2013
|
|
32
|
Zhang J, Huang Y, Sun Y, He A, Zhou Y, Hu
H, Yao Y and Shen Z: Impact of chemotherapy cycles and intervals on
outcomes of nonspinal Ewing sarcoma in adults: A real-world
experience. BMC Cancer. 19:11682019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
El Weshi A, Allam A, Ajarim D, Al Dayel F,
Pant R, Bazarbashi S and Memon M: Extraskeletal Ewings sarcoma
family of tumours in adults: Analysis of 57 patients from a single
institution. Clin Oncol (R Coll Radiol). 22:374–381. 2010.
View Article : Google Scholar : PubMed/NCBI
|